Abstract
Curcumin, when used in a combination regimen in multiple myeloma patients, has comparable progression‐free survival without the adverse effects of steroid‐based combination therapies that is curcumin may be a viable alternative to corticosteroids in combination with an immunomodulatory drug or proteasome inhibitor.
Keywords: curcumin, dexamethasone intolerance, multiple myeloma
Curcumin, when used in a combination regimen in multiple myeloma patients, has comparable progression‐free survival without the adverse effects of steroid‐based combination therapies that is curcumin may be a viable alternative to corticosteroids in combination with an immunomodulatory drug or proteasome inhibitor.
1. INTRODUCTION
There are currently many promising strategies for management of MM, including immunomodulatory drugs (IMiDs), proteasome inhibitors (PIs), or histone deacetylase inhibitors, but also novel strategies, such as small‐molecule inhibitors, monoclonal antibodies, or chimeric antigen receptor (CAR) T cells.1, 2 Treatment regimens typically involve a steroid, such as dexamethasone (Dex), used in combination with either an ImiD (ie, thalidomide, lenalidomide, or pomalidomide) or a PI (ie, bortezomib, carfilzomib, or ixazomib).3, 4, 5, 6, 7 Despite its demonstrated effectiveness in treating MM, the administration of Dex remains a challenge, particularly in elderly patients, due to its side effects: fatigue, weight gain, fluid retention, poor impact on mental health, osteoporosis and hyperglycemia, or poor diabetic control.5
A randomized controlled trial of 1623 transplant‐ineligible MM patients has shown that continuous lenalidomide (revlimid) and Dex (Rd) were superior to either 18 cycles of Rd or a combination of melphalan, prednisone, and thalidomide (MPT).6 Compared to 18 Rd cycles, a 30% reduction in the risk of progression or death was observed when patients were treated with continuous Rd.6 Continuous therapy was also shown to be associated with a longer duration of response and a longer median time to second‐line antimyeloma therapy. However, continuous Rd for greater than 72 weeks was associated with an augmentation of adverse effects such as infection(s), thromboembolic events, and cataracts. These adverse effects were, at least partly, attributable to the Dex component of the regimen.6 Dex‐related side effects have also been observed in other studies.4
Consequently, the challenge in MM management is to retain the prolonged duration of response and median time to second‐line chemotherapy associated with continuous therapy while simultaneously avoiding the adverse effects associated with corticosteroid administration. Often, patients can be supported through induction therapy with high‐dose steroids, but prolonged continuous therapy is more challenging. The clinical benefit associated with prolonged response duration and extended median time to the requirement for second‐line chemotherapy is particularly significant in elderly patients who, in general, respond poorly to rescue therapy. The aim of this study, therefore, is to report our experience with curcumin, combined with either an IMiD or PI, in the treatment of older (>55 years) MM patients intolerant of Dex.
Curcumin is the primary active component of turmeric. It is a hydrophobic polyphenol extracted from the rhizomes.8 Curcumin displays a wide range of biological activities including anti‐oxidant, anti‐inflammatory, and cytotoxicity to numerous cancer cell types.9 Its anticancer effect has been attributed to regulation of multiple cell signalling pathways involved in cell proliferation and apoptosis.10, 11 Curcumin has a demonstrated cytotoxic effect on myeloma activity12, 13 as well as a synergistic effect when used in combination with an IMiD or PI.14, 15 In a study by Wong et al,16 curcumin was shown to enhance the cytotoxic and chemo‐sensitizing effects of lenalidomide by suppressing the expression of the cereblon (CRBN) gene, which is a primary target for IMiD drugs like thalidomide and lenalidomide.17 The same study also reported an enhanced reduction in the expression of the MRP gene, which encodes the multidrug resistant protein, when lenalidomide and curcumin are used together on H929 myeloma cell line. Recently, Allegra et al18 reported a synergism between carfilzomib and curcumin toward induction of cytotoxicity on U266 myeloma cells. A combination of carfilzomib with curcumin leads to a significantly stronger downregulation of the NF‐kB pathway.18
Banerjee et al19 report that eight different “proteasome‐adapted” cell lines (multiple myeloma and triple‐negative breast cancer) exhibit strong synergistic toxicity upon treatment with a carfilzomib and curcumin combination. However, noncancerous cells did not exhibit the similar levels of cytotoxicity thus conveying the fact that cancer cells with acquired proteasome resistance could be selectively targeted by the curcumin‐carfilzomib combination.
In this report, we describe our experience with the use of curcumin instead of Dex in combination therapy in MM patients intolerant of Dex.
2. METHODS
A total of 15 patients (>55 years) with multiple myeloma who were being treated with either an IMiD or PI plus Dex, who developed side effects determined to be due to the Dex, were selected to replace the Dex with curcumin and continue with their treatment. Patients were advised to take curcumin at a dose of 3‐4 g daily of C3 complex curcumin. They were monitored at intervals ranging from 1 to 3 months. At each visit, blood and urine samples were collected and analyzed for markers of myeloma activity (ie, paraprotein, Hb, calcium, eGFR, and B2 microglob). Paraprotein levels were used as a measure of disease stability or progression. Bone marrow biopsies were performed at intervals as determined by the treating hematologist. Conventional cytogenetic analysis for each patient was performed at intervals as well as fluorescent in situ hybridization (FISH). Data are expressed as a mean (±1 SD).
3. RESULTS
There were fifteen MM patients intolerant of Dex in whom curcumin was used in combination with IMiD’s or PI’s. Of the fifteen, seven patients had a history of diabetes and three were grossly obese with a BMI > 40. Six patients had a history of mental health issues including anxiety/depression. Two patients with poorly controlled hypertension and significant renal impairment (eGFR < 25) could not tolerate dexamethasone therapy. The characteristics of each patient at time of diagnosis, their treatment, and follow‐up outcomes as of June 2019 are illustrated in Table 1. There were six females and nine males with a mean age of 72 years (range 57‐86) included in the study. There were 12 patients with IgG paraproteinemia (nine kappa and three lambda) and three patients with IgA paraproteinemia (two lambda and one kappa). The mean duration of disease was 6.9 (±2.9) years, and the average duration of curcumin therapy was 6.1 (±2) years.
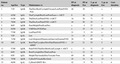
Table 1.
Individual clinical data, therapy, paraprotein levels, and plasmacytosis at diagnosis and end of study (June 2019) of multiple myeloma patients intolerant of Dex in whom curcumin was used in combination with IMiD’s or PI’s
| Patient no. | Age/Sex | Type | Maintenance rx | PP at diagnosis | PP at Eos | % pc at diagnosis | % pc at Eos | Curc duration |
|---|---|---|---|---|---|---|---|---|
| 1 | 71/F | IgGK | Tha/Dex/Bort/Cycloph/Clexane/Len/Pam/IVIG/Pom | 40 | 38 | 7 | x | 7 |
| 2 | 62/M | IgGL | Tha/Cycloph/Bort/Len/Pom/Ixazo + ASCT | 8 | 30 | 10 | 31 | 5 |
| 3 | 61/M | IgGL | Tha/Dex/Len/Pam/IVIG/ +ASCT | 16 | 20 | 71 | 37 | 6 |
| 4 | 78/M | IgGK | Tha/Dex/Len/Pam/IVIG/ +ASCT | 44 | 50 | 52 | 5 | 3 |
| 5 | 86/F | IgGK | Pam/Melph/Pred/Len/Dex | x | 4 | 27 | x | 9 |
| 6 | 82/M | IgGK | VMP/Dex/IVIG/Pam | x | 19 | 15 | 14 | 6 |
| 7 | 77/M | IgGK | Len/Pam/IVIG | 21 | 5 | 19 | x | 3 |
| 8 | 72/F | IgAL | Len. | 11 | 14 | 27 | 17 | 6 |
| 9 | 71/M | IgGK | Len/Alloprinol/Diamicron/Janovia/Zometa/IVIG | 20 | 3 | 60 | x | 7 |
| 10 | 58/F | IgAK | Bort/Tha/Cycophos/Dex/Pam/Pamisol/IVIG + ABMT | 33 | 21 | 55 | 5 | 6 |
| 11 | 57/M | IgGK | Pam/IVIG/Tha/Dex/Bort/Len/Cycloph + ASCT | x | 11 | 71 | 15 | 9 |
| 12 | 64/F | IgGK | Bort/Cycloph/Dex/Tha/Len/Pom | x | 12 | 35 | x | 4 |
| 13 | 85/F | IgGL | Melph/Tha/Aredia/Dex/Velcade/ Pom | 69 | 30 | 45 | 11 | 9 |
| 14 | 75/M | IgGK | CyBorD/Velcade/Revlimid | 25 | 14 | 16 | 23 | 7 |
| 15 | 66/M | IgAL | CyBord/ABMT/ Rev | 42 | 9 | 70 | 2 | 6 |
Abbreviations: %pc, percentage plasma cells; ABMT, Autologous Bone Marrow Transplant; ASCT, Autologous Stem Cell Transplant; Bort, Bortezomib (Velcade); Curc, curcumin; Cycloph, Cyclophosomide; Dex, Dexamethasone; Eos, end of study; IVIG, Intravenous Immunoglobulin Infusion; Len, Lenalidomide (Revlimid); Melp, Melphalan; Mitox, Mitoxantrone; Pam, Pamidronate; Pom, Pomalidomide; PP, Paraproteinaemia; Pred, Prednisolone; Tha. Thalidomide; Vin, Vincristine; VMP, Bortezomib + Melphalan +Prednisone; x, information not available.
Individual biochemistry and erythrocyte sedimentation rate (ESR) data of each patient at diagnosis and follow‐up are illustrated in Table 2. Table 3 illustrates mean (+SD) of the various markers of disease activity at diagnosis and at the end of the study period (June 2019). The mean paraprotein level at time of diagnosis was 29.9 (±18) g/L (n = 11) and at end of study was 18.7 (±13.3) g/L (n = 15). The mean peak paraprotein level observed throughout the course of care was 36.1 (±19) g/L (n = 15). Mean plasmacytosis at diagnosis was 39 (± 24.5)% (n = 15) and at end of study (June 19) was 16 (±11.5) % (n = 10). We demonstrate that curcumin in combination with other antimyeloma therapies was able to reduce paraprotein load by 38% and plasmacytosis by 59% over this study period. The mean hemoglobin at time of diagnosis was 123.3 (±14.9) g/L and at end of study period was 110.7 (+15.7) g/L. Baseline ESR was 65.3 (±40.1) mm/hr and at end of study period was 62.1 (±36) mm/h At diagnosis, estimated glomerular filtration rate (eGFR) was 70.1(±17.5) mL/min and at end of study was 58.7(±24.1) mL/min. At diagnosis, calcium (Ca) was 2.46 (±0.28) mmol/L and at end of study was 2.40 (±0.17) mmol/L. Baseline beta 2 microglobulin (B2M) was 3.9 (±2.4) mg/L and end of study was 5.3 (+4.5) mg/L.
Table 2.
Individual biochemistry at diagnosis and end of study (June 2019)
| Patient no. | Hb at dx | Eos Hb | Esr at dx | Eos esr | eGFR at dx | Eos eGFR | Ca at dx | Eos ca | B2M at dx | Eos B2M |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 122 | 102 | 73 | 16 | 58 | 50 | 2.51 | 2.52 | 3.9 | 6.9 |
| 2 | 126 | 101 | 52 | 94 | 90 | 90 | 2.46 | 2.37 | 2.1 | 3.3 |
| 3 | 118 | 113 | 38 | 88 | 90 | 90 | 2.09 | 2.34 | 1.8 | 3 |
| 4 | 97 | 85 | 98 | 120 | 67 | 24 | 2.64 | 2.95 | 6.9 | 19.4 |
| 5 | 123 | 121 | 49 | 61 | 62 | 30 | 2.42 | 2.33 | 2.7 | 3.6 |
| 6 | 125 | 98 | 26 | 120 | 65 | 38 | 2.22 | 2.33 | 1.8 | 6.4 |
| 7 | 98 | 91 | 95 | 62 | 87 | 42 | 2.3 | 2.19 | 3.8 | 4.9 |
| 8 | 143 | 103 | 31 | 38 | 84 | 44 | 2.4 | 2.29 | 2.9 | 2.4 |
| 9 | 130 | 112 | 19 | 30 | 71 | 31 | 2.5 | 2.4 | 1.8 | 3.6 |
| 10 | 116 | 109 | 120 | 90 | 74 | 77 | 2.66 | 2.33 | 3.7 | 2.2 |
| 11 | 143 | 124 | 111 | 56 | 57 | 86 | 2.23 | 2.38 | 2.7 | 1.9 |
| 12 | 126 | 108 | 30 | 27 | 90 | 90 | 2.34 | 2.35 | 8.6 | 6.5 |
| 13 | 126 | 119 | 111 | 79 | 24 | 50 | 2.41 | 2.39 | 9.1 | 10.2 |
| 14 | 148 | 148 | 7 | 3 | 71 | 65 | 2.44 | 2.45 | 3.7 | 3.3 |
| 15 | 108 | 126 | 120 | 48 | 62 | 73 | 3.3 | 2.34 | 3 | 2.2 |
Abbreviations: B2M, beta 2 microglobulin (normal range 0‐3 mg/L); Ca, calcium (normal range 2.15‐2.55 mmol/L); dx, diagnosis; eGFR, estimated glomerular filtration rate (normal range > 90 mL/min); Eos, end of study; esr, erythrocyte sedimentation rate (normal range 0‐29 mm/h); Hb, hemoglobin (normal range 119‐160 g/L).
Table 3.
Disease progression markers and biochemistry of MM patients at diagnosis and at end of study period (Mean ± SD)
| Variables | At diagnosis | Eos (June 19) |
|---|---|---|
| Plasma cells (%) | 38.3 ± 23.4 | 15.6 ± 11.5 |
| Paraprotein (g/L) | 29.9 ± 18 | 18.7 ± 13.3 |
| Hemoglobin (119‐160 g/L) | 123.3 ± 14.9 | 110.7 ± 15.7 |
| B 2 microglobulin (0‐3 mg/L) | 3.9 ± 2.4 | 5.3 ± 4.5 |
| Calcium (2.15‐2.55 mmol/L) | 2.46 ± 0.28 | 2.4 ± 0.17 |
| ESR (0‐29 mm/h) | 65.3 ± 40.4 | 62.1 ± 36 |
| eGFR (>90 mL/min) | 70.1 ± 17.5 | 58.7 ± 24.1 |
Abbreviations: eGFR, estimated glomerular filtration rate; Eos, end of study; ESR, erythrocyte sedimentation rate.
Table 4 illustrates the conventional cytogenetics and FISH of each patient. No high‐risk cytogenetic abnormalities were detected in seven patients (1, 3, 4, 5, 9, 14, and 15). Eight patients had cytogenetic abnormalities that suggested higher risk disease (2, 6, 7, 8, 10, 11, 12, and 13).
Table 4.
Cytogenetics and FISH (fluorescent in situ hybridization) of each patient
| Patient no. | Cytogenetics | Findings |
|---|---|---|
| 1 | Normal | Cytogenetic studies and FISH analysis did not reveal any high‐risk abnormalities. |
| 2 | Normal |
Cytogenetic studies and FISH analysis consistent with high‐risk disease: Deletion of the TP53 locus at 17p13 detected (2019), but had not appeared on earlier studies (2017, 2016, 2014, and 2012). Gain of CKS1B with 3‐4 copies of 1q21 detected (2016) |
| 3 | Normal | Cytogenetic studies and FISH analysis did not reveal any high‐risk abnormalities. |
| 4 | Normal | Cytogenetic studies and FISH analysis did not reveal any high‐risk abnormalities. (trisomy p53 detected 2014 but lost by 2015) |
| 5 | Normal | Cytogenetic studies and FISH analysis did not reveal any high‐risk abnormalities. |
| 6 | 45,X,‐Y[4]/46,XY[26] | Cytogenetic studies and FISH analysis consistent with high‐risk disease: Gain of CKS1B with three copies of 1q21 detected (2014) and still present on most recent study (2017). |
| 7 | Normal | Cytogenetic studies and FISH analysis consistent with high‐risk disease: Gain of CKS1B with three copies of 1q21 detected (2016). |
| 8 | Normal |
Cytogenetic studies and FISH analysis consistent with high‐risk disease: Gain of CKS1B with three copies of 1q21 detected. Trisomy p53 detected (2014), but not detected on two prior studies (2014, 2013) or on subsequent studies (2016, 2017). |
| 9 | Normal | Cytogenetic studies and FISH analysis did not reveal any high‐risk abnormalities. |
| 10 | 45,X,‐X[4]/46,XX[26] | Cytogenetic studies and FISH analysis consistent with high‐risk disease: t(4;14) IGH/FGFR3 translocation detected (2016 ,2017, and 2019). Gain of CKS1B with 3‐4 copies of 1q21 was detected (2016). Tetrasomy (2019) |
| 11 | Normal | Cytogenetic studies and FISH analysis consistent with high‐risk disease: Deletion of the TP53 locus at 17p13 detected (2017) |
| 12 | Normal | Cytogenetic studies and FISH analysis consistent with high‐risk disease: Gain of CKS1B with three copies of 1q21 detected. A translocation involving the IGH locus at 14q32 was detected, but the translocation partner is unknown. t(4;14) and t(14;16) were not detected. These findings were not present in 2012 study but had developed by 2015 and were still present in 2016 and 2018 studies. |
| 13 | 45,X,‐X[3]/46,XX[24] | Cytogenetic studies and FISH analysis consistent with high‐risk disease: Gain of CKS1B with three copies of 1q21 (2018), and also a translocation involving the IGH locus at 14q32 was detected, but the translocation partner is unknown. t(4;14) and t(14;16) were not detected. Earlier studies (2015, 2013, 2012, 2011, and 2009) were normal. |
| 14 | Normal | Cytogenetic studies and FISH analysis did not reveal any high‐risk abnormalities. |
| 15 | Normal | Cytogenetic studies and FISH analysis did not reveal any high‐risk abnormalities. |
Two patients (5, 9) developed diarrhea during the course of curcumin therapy. In patient 9, the diarrhea did not abate following curcumin suspension suggesting an alternative cause. When rechallenged with curcumin, the patient did not develop diarrhea. Patient no. 5 was managed by temporarily suspending curcumin therapy and reducing the dose.
Of the 15 patients, 12 remain alive at the time of writing up the case series (June 2019). Three patients (1, 3, 4) had died. One patient (no. 1) developed dementia and ceased therapy and died. She had been on curcumin therapy for 7 years. Patient no. 3 had spinal involvement of his disease and received radiation. He unfortunately progressed to paraplegia and subsequent death. He had been taking curcumin for 6 years. Patient no. 4 (age 79) had a poor prognosis due to cardiac issues. He had been taking curcumin for 3 years and died of an infection at the end of this period. The remaining 12 patients are considered to be in a stable condition and are progressing well.
4. DISCUSSION/CONCLUSION
Previous studies carried out in our clinics have demonstrated that oral administration of curcumin, even at high doses (up to 8 g daily), is well tolerated and can decrease the paraprotein load, free light chains, bone turnover, and % plasma cell dyscrasia in a selected group of patients with multiple myeloma precursor disease that is monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM).20, 21, 22, 23
The multitude of published studies, including an in vitro study carried out in our laboratory,16 suggest that curcumin can potentiate not only the cytotoxic effect of multiple agents used in the treatment of MM, but also enhance the chemo‐sensitizing effects of these agents. The implications arising from these observations may be of important clinical benefit: i) curcumin studies can be designed to assess the additive antimyeloma effects of curcumin to the current treatment protocols and ii) curcumin may be used as an alternative to corticosteroids in such protocols.
We show here that curcumin may act as a steroid‐sparing agent in patients with MM who are intolerant of Dex. We demonstrate that curcumin in combination with other antimyeloma therapies was able to reduce paraprotein load by 38% and plasmacytosis by 59% over this study period. Multiple myeloma is a heterogenous disease from a cytogenetic abnormalities point of view.24 Eight of the 15 patients demonstrated high‐risk cytogenetic and FISH abnormalities with many of these showing evolution during the course of their illness. While three patients died during the course of this study, none of these had high‐risk cytogenetic abnormalities. Some of the surviving patients do have high‐risk cytogenetic and FISH abnormalities and despite this, continue to do well on the combination therapy.
This is the first reported case series of patients with MM who have been treated with adjuvant curcumin as opposed to Dex in combination with other antimyeloma agents. Curcumin‐based combination therapies may be capable of stabilizing disease progression without the adverse effects associated with steroid use. In our experience, the only observed side effect of curcumin is diarrhea which can be managed by either temporarily suspending therapy or reducing the dose. Therefore, curcumin can be considered to have comparatively minimal adverse effects and superior tolerability to typical steroid medications, such as commonly used dexamethasone.
Curcumin has been reported to induce anticancer and antiproliferative activity via multiple pathways including induction of apoptosis by caspase activation, downregulation of essential transcription factors like NF‐kB, inhibition of c‐Jun N‐terminal kinase (JNK), and protein tyrosine kinases and downregulation of growth factor receptors like HER2 and EGFR.10 Banerjee et al19 establish that impairment of proteasome activity by DYRK2 inhibition is a major mechanism of action for curcumin in the context of the alleviation of proteasome‐dependent neoplastic malignancies such as MM.
Consequently, curcumin possesses the potential to impede myeloma activity and improve the quality of life in MM patients. Further randomized controlled trials should aim to elucidate and replicate the findings of this study.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTION
RR: recruited study patients, monitored follow‐up visits, and assisted with analysis of results and study write‐up. TD: consulted on study methodology and assisted with study write‐up. AM: recruited patients, monitored follow‐up visits, and assisted with analysis of results and study write‐up. WA: assisted with collection of research data and study analysis. TG: provided study concept, monitored follow‐up visits, analyzed results, and wrote up the study.
Ramakrishna R, Diamond TH, Alexander W, Manoharan A, Golombick T. Use of Curcumin in Multiple Myeloma patients intolerant of steroid therapy. Clin Case Rep. 2020;8:739–744. 10.1002/ccr3.2735
REFERENCES
- 1. Cavo M, Terpos E, Bargay J, et al. The multiple myeloma treatment landscape: international guideline recommendations and clinical practice in Europe. Expert Rev Hematol. 2018;11:219‐237. [DOI] [PubMed] [Google Scholar]
- 2. Köhler M, Greil C, Hudecek M, et al. Current developments in immunotherapy in the treatment of multiple myeloma. Cancer. 2018;124:2075‐2085. [DOI] [PubMed] [Google Scholar]
- 3. Hideshima T, Raje N, Richardson PG, Anderson KC. A review of lenalidomide in combination with dexamethasone for the treatment of multiple myeloma. Ther Clin Risk Manag. 2008;4:129‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rajkumar SV, Hayman SR, Lacy MQ, et al. Combination therapy with lenalidomide plus dexamethasone (Rev/Dex) for newly diagnosed myeloma. Blood. 2005;106:4050‐4053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rajkumar SV, Blood E, Vesole H, Fonseca R, Greipp PR. Phase III clinical trial of thalidomide plus dexamethasone compared with dexamethasone alone in newly diagnosed multiple myeloma: a clinical trial coordinated by the Eastern Cooperative Oncology Group. J Clin Oncol. 2006;24:431‐436. [DOI] [PubMed] [Google Scholar]
- 6. Benboubker L, Dimopoulos MA, Dispenzieri A, et al. Lenalidomide and dexamethasone in transplant‐ineligible patients with myeloma. N Engl J Med. 2014;371:906‐917. [DOI] [PubMed] [Google Scholar]
- 7. Dimopoulos MA, Chen C, Spencer A, et al. Long‐term follow‐up on overall survival from the MM‐009 and MM‐010 phase III trials of lenalidomide plus dexamethasone in patients with relapsed or refractory multiple myeloma. Leukemia. 2009;23:2147‐2152. [DOI] [PubMed] [Google Scholar]
- 8. Aggarwal BB, Sundaram C, Malani N, Ichikawa H. Curcumin: the Indian solid gold. Adv Exp Med Biol. 2007;595:1‐75. [DOI] [PubMed] [Google Scholar]
- 9. Shishodia S. Molecular mechanisms of curcumin action: gene expression. BioFactors. 2012;39(1):37‐55. [DOI] [PubMed] [Google Scholar]
- 10. Aggarwal BB, Kumar A, Bharti AC. Anticancer potential of curcumin: preclinical and clinical studies. Anticancer Res. 2003;23:363‐398. [PubMed] [Google Scholar]
- 11. Ravindran J, Prasad S, Aggarwal BB. Curcumin and cancer cells: how many ways can curry kill tumor cells selectively? AAPS J. 2009;11:495‐510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bharti AC, Donato N, Singh S, Aggarwal BB. Curcumin (Diferuloylmethane) down‐regulates the constitutive activation of nuclear factor‐KB and IKBα kinase in human multiple myeloma cells, leading to suppression of proliferation and induction of apoptosis. Blood. 2003;101:1053‐1062. [DOI] [PubMed] [Google Scholar]
- 13. Vadhan‐Raj S, Weber DM, Wang M, et al. Curcumin downregulates NF‐KB and related genes in patients with Multiple Myeloma: results of a phase 1/11 study. Blood. 2007;110:1177a. [Google Scholar]
- 14. Sung B, Kunnumakkara AB, Sethi G, Anand P, Guha S, Aggarwal BB. Curcumin circumvents chemoresistance in vitro and potentiates the effect of thalidomide and bortezomib against human multiple myeloma in nude mice model. Mol Cancer Ther. 2009;8(4):959‐970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bai Q, Zhang X. Curcumin enhances cytotoxic effects of Bortezomib in human multiple myeloma H929. Int J Mol Sci. 2012;13(4):4831‐4838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wong R, Golombick T, Diamond TH, Ramakrishna R, Manoharan A. Curcumin enhances the cytotoxic and chemo‐sensitising effects of Lenalidomide in human myeloma cells. J Haematol Malign. 2013;3:2. [Google Scholar]
- 17. Zhu YX, Braggio E, Shi C‐X, et al. Cereblon expression is required for the antimyeloma activity of lenalidomide and pomalidomide. Blood. 2011;118:4771‐4779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Allegra A, Speciale A, Molonia MS, et al. Curcumin ameliorates the in vitro efficacy of carfilzomib in human multiple myeloma U266 cells targeting p53 and NF‐kappaB pathways. Toxicol In Vitro. 2018;47:186‐194. [DOI] [PubMed] [Google Scholar]
- 19. Banerjee S, Chenggong J, Mayfield JE, et al. Ancient drug curcumin impedes 26S proteasome activity by direct inhibition of dual‐specificity tyrosine‐regulated kinase 2. Proc Natl Acad Sci. 2018;115:8155‐8160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Golombick T, Diamond T, Badmaev V, et al. The potential role of curcumin in patients with monoclonal gammopathy of undetermined significance – Its effect on paraproteinemia and the urinary N‐Telopeptide of type 1 collagen bone turnover marker. Clin Cancer Res. 2009;15(18):5917‐5922. [DOI] [PubMed] [Google Scholar]
- 21. Golombick T, Diamond T, Manoharan A, Ramakrishna R. Monoclonal gammopathy of undetermined significance (MGUS), smoldering multiple myeloma (SMM) and curcumin: a randomised, double‐blind placebo‐controlled cross‐over 4g study and an open‐label 8g extension study. Am J Hematol. 2012;87:455‐460. [DOI] [PubMed] [Google Scholar]
- 22. Golombick T, Diamond T, Manoharan A. ,Response to Vermorken et al. – curcumin and free light chains. Am J Hematol. 2012;87:E80‐E81. [DOI] [PubMed] [Google Scholar]
- 23. Golombick T, Diamond T, Manoharan A, Ramakrishna R. Long term use of curcumin in two smoldering multiple myeloma (SMM) patients. J Hematol Malign. 2013;3(1):18‐23. [Google Scholar]
- 24. Rajan AM, Rajkumar SV. Interpretation of cytogenetic results in multiple myeloma for clinical practice. Blood Cancer J. 2015;5(10):e365. [DOI] [PMC free article] [PubMed] [Google Scholar]


