Abstract
Objective:
This study sought to determine whether parenting styles predict long-term psychosocial outcomes after traumatic brain injury in young children.
Methods:
The study involved a concurrent cohort, prospective design, with longitudinal assessments up to early adolescence. Participants included 126 children with moderate to severe traumatic brain injury or orthopaedic injury, ages 3 to 6 years 11 months, recruited between 2003 and 2006. Parents rated children’s pre-injury behavioral adjustment, social competence, and executive functioning shortly after injury, and again 6.8 years post injury. Parents also rated their parenting styles (permissive, authoritarian, authoritative) at both occasions.
Results:
After controlling for pre-injury functioning, the groups differed significantly on all three outcomes (ΔR2 .07 to .13). Later but not early parenting styles predicted outcomes in all groups (ΔR2 .06 to .17): more permissive parenting predicted worse outcomes in all domains (β = −0.18, 0.20, 0.27); and more authoritative parenting predicted better social competence and executive functioning (β = −0.17, 0.46). Severe traumatic brain injury interacted with parenting style for several outcomes, with ineffective parenting exacerbating the negative sequelae.
Conclusions:
Parenting style predicts children’s long-term psychosocial functioning after early childhood injury, and may moderate the effects of early traumatic brain injury.
Keywords: behaviour, social competence, executive functioning, youth, concussion, pediatric
Introduction
Childhood traumatic brain injury (TBI) is a major public health concern (1, 2). Preschool age children are especially vulnerable to TBI (3). Previous research has shown that childhood TBI is associated with a range of negative outcomes in multiple domains. including executive functioning (4), social and adaptive functioning (5), and emotional and behavioural adjustment (6, 7). These difficulties persist over time (8–11), sometimes into adulthood (12).
One of the major advances in research on TBI in recent years has been the recognition of the importance of non-injury related influences on recovery (6). Research to date has highlighted a variety of non-injury factors that can affect outcomes: preinjury factors (e.g. demographics, pre-injury cognitive ability, premorbid behavioural or psychiatric problems, genetic and epigenetic factors), comorbid conditions (e.g. post-traumatic stress disorder, pain), contextual factors (e.g. family and home environment, socioeconomic status), and medical and non-medical intervention (e.g. acute medical care, education and workplace accommodations), although the evidence for the effectiveness of these interventions remains limited (6).
Contextual factors play a particularly important role in determining the outcomes of childhood TBI. Notably, the home environment is known to moderate the impact of childhood TBI by buffering or exacerbating its consequences, such that the effects of severe TBI tend to be more pronounced among children from dysfunctional families (i.e., those characterized by poor quality home environments, fewer interpersonal and financial resources, higher levels of stress, more ineffective parenting, and greater parental psychological distress) and less pronounced among children from higher-functioning families (6, 13–20). The family environment may be especially influential in moderating behavioural and functional outcomes, as opposed to cognitive outcomes (6, 19). Both the immediate post-injury home environment, as well as the home environment long after injury, have roles to play in determining long-term behavioural and functional outcomes of early childhood TBI. Durber et al. (2017) assessed early (about 1 month post-injury) and late (on average 6.83 years postinjury, at an average age of 11.91 years of age) home environments using the early childhood and early adolescent versions of the HOME Inventory, respectively, which use home observations and semistructured interviews with primary caregivers to assess multiple dimensions of the quality of the home environment(21, 22).They found that higher quality early and late home environments predict better school performance and behaviour, respectively, after early childhood TBI (23). Durish et al. (2017) further found that the quality of the later home environment moderated the effects of early childhood TBI on long-term executive functioning (24).
Parenting style is a specific aspect of the family environment that has been linked with psychosocial outcomes in typically developing children (25, 26) and in recovery following TBI in childhood (27). Baumrind (28) outlined three parenting styles: authoritative, permissive, and authoritarian. Authoritative parenting is characterized by effective behaviours, such as strong communication, positive reinforcement, warmth, and responsiveness. Both permissive parenting and authoritarian parenting are characterized by ineffective behaviours, such as physical punishment, harsh discipline, and negativity (authoritarian parenting) and overindulgence, lax discipline, and neglect (permissive parenting). Parenting plays an important role during early adolescence, when parents and children are learning how to navigate a changing relationship that allows for increased adolescent independence (29) and decreased parental monitoring (30). Adolescent behaviour problems tend to be associated both with fewer positive parenting behaviours and more negative parenting behaviours (31–34).
Parenting style likely plays a role in recovery following TBI. In one study, the effect of TBI on children’s behavioural adjustment was more pronounced over the first-year post-injury at higher levels of authoritarian and permissive parenting; however, among children with severe TBI, even those from homes with lower levels of permissive parenting showed increased behavioural problems (19). Thus, early parenting may moderate psychosocial outcomes after TBI in young children, but its moderating influence may wane with time among children with severe TBI. Parenting style also moderates behavioural aspects of executive functioning following TBI in young children, such that higher levels of authoritarian parenting predict greater executive difficulties at 12 and 18 months post-injury relative to children with orthopaedic injuries (OI) (7).
Most previous research on the association of parenting style with the outcomes of early childhood TBI has focused on the first year post-injury. Few studies have examined the relationship between parenting style and children’s outcomes after TBI over a longer period of time, to determine if parenting style remains a significant moderator of outcomes years after the injury. The objective of the current study, therefore, was to determine whether parenting style moderates long-term psychosocial outcomes in children who sustained TBI during early childhood and are now entering adolesence. Consistent with our previous research, we predicted that young children hospitalized for moderate to severe TBI would display long-term deficits in behavioural adjustment (35), social competence (5), and everyday executive functioning (24, 36) relative to children with OI, and that the deficits would be most pronounced after severe TBI. We also expected that long-term deficits in psychosocial outcomes after early TBI would be more pronounced among children whose parents reported less effective parenting styles (i.e., more permissive and authoritarian parenting) and less pronounced among children whose parents reported more effective parenting styles (i.e., more authoritative parenting). We also explored whether early parenting, as measured shortly after the injury, and later parenting, measured contemporaneously, was associated with long-term outcomes.
Methods
Study Design
The parent study that provided the data for the current analyses employed a concurrent cohort, prospective design. The broad study objectives were to characterize differences in outcomes of children, 3 to 7 years of age, who were hospitalized for either OI or moderate to severe TBI, and to examine various aspects of the home environment (e.g., parenting) as potential moderators of outcomes. Children with OI were selected as a comparison group to control for the impact of acute hospitalization and for background characteristics that increase children’s risk of unintentional injury.
Participants
A total of 221 participants (23 severe TBI, 64 complicated mild/moderate TBI, 15 uncomplicated mild, 119 OI) were recruited from four sites: Children’s Hospital Medical Center, Cincinnati OH; Nationwide Children’s Hospital, Columbus OH; Rainbow Babies and Children’s Hospital, Cleveland OH; and Metro Health Medical Center, Cleveland, OH. The Institutional Review Boards at each site provided study approval, and parents gave written consent at the time of recruitment. Because the focus of this study was on children with moderate to severe TBI, the small group of children with uncomplicated mild TBI was excluded from analysis. Thus, the total study population included 206 participants.
Children were eligible if they met the following general inclusion criteria: hospitalization overnight for traumatic injury sustained between 3 years and 6 years 11 months of age, no evidence of child abuse as cause of injury, no history of documented neurological problems or developmental delays before the injury, and English as primary language in the home. Severity of TBI was characterized using the lowest post-resuscitation Glasgow Coma Scale (GCS; (37)), with GCS scores of 8 or less considered severe TBI, and scores of 9-12 considered moderate TBI. Participants with a GCS score of 13-15, but abnormal brain imaging, were considered to have a complicated mild TBI. The latter two groups were combined into a single complicated mild/moderate TBI group because past research has suggested that complicated mild and moderate TBI have similar outcomes (24, 38). The OI group included children with a bone fracture (excluding skull fractures) but no alterations in consciousness or other signs or symptoms of head trauma or brain injury.
Procedures
Participants were followed from shortly after injury (M = 40.26 days post-injury, SD = 20.13) to late childhood/early adolescence (years post-injury M = 6.84, SD = 1.12; age at testing M = 11.97 years, SD = 1.14), completing six assessments over that time (i.e., baseline, 6-months, 12-months, 18-months, 3.5 years, and 6.8 years after injury). Assessments were conducted with both children and their parents. The current study examined parenting as rated shortly after injury and again at the end of follow up as a predictor of long-term psychosocial outcomes, about 7 years post-injury. The sample for the current study was restricted to the 126 participants who completed the final follow up (61% of the total study sample), including 71 with OI, 40 with complicated mild/moderate TBI, and 15 with severe TBI. Children who completed the long-term follow up did not differ from those who did not do so with respect to group membership, sex, race (white vs non-white), age at injury, average median census tract income at time of study entry, maternal education, or baseline ratings of pre-injury parenting style or pre-injury psychosocial adjustment. Table 1 presents demographic data for the severe TBI, complicated mild/moderate TBI, and OI groups. The groups did not differ significantly in age at injury, sex, race, average census tract median income, or maternal education.
Table 1.
Participant demographics
| Group | |||
|---|---|---|---|
| Severe TBI (N=15) | Complicated mild/moderate TBI (N=40) | OI (N=71) | |
| Age at injury (years), M (SD) | 5.12 (0.97) | 5.21 (1.21) | 5.07 (1.06) |
| Age at last assessment (years), M (SD) | 12.13 (1.57) | 11.99 (1.09) | 11.92 (1.08) |
| Male, n (%) | 9 (60.0%) | 23 (58.0%) | 37 (52.1%) |
| White race, n (%) | 10 (66.7%) | 31 (77.5%) | 55 (77.5%) |
| Census tract median family income, M (SD) | 56,720 (20,729) | 69,999 (25,944) | 68,608 (24,335) |
| Maternal education, n (%) | |||
| < High school | 3 (20.0%) | 4 (10.0%) | 5 (7.0%) |
| High school/GED | 8 (53.3%) | 14 (35.0%) | 26 (36.6%) |
| Partial college | 3 (20.0%) | 9 (%) | 14 (19.7%) |
| College graduate | 1 (6.7%) | 13 (32.5%) | 26 (36.6%) |
Measures
Parents rated their pre-injury parenting styles, as well as children’s pre-injury psychosocial functioning, shortly after injury. They rated their parenting and the children’s post-injury psychosocial functioning again at the final assessment. Parenting styles were measured using the Parenting Practices Questionnaire (PPQ) (39), which is a 62-item rating scale that assesses three dimensions of parenting (i.e., authoritarian, authoritative and permissive). Consistent with Baumrind’s characterization (28), permissive and authoritarian parenting are regarded as less effective forms of parenting, whereas authoritative parenting is regarded as more effective. The scales for each dimension represent composites of subscales derived through factor analysis. For the purpose of the current study, we used total scores for each dimension as predictors. The PPQ has shown satisfactory reliability and validity in previous research (19, 40).
Three psychosocial outcomes were examined in the current study: 1) behavioural adjustment, 2) social competence, and 3) everyday executive functioning. Behavioural adjustment was measured using the total problem T score from the Child Behaviour Checklist (CBCL) (41, 42). Parents rated pre-injury behavior at the initial assessment using the preschool version for children less than 6 years of age and the school age version for children ages 6 years of age and older; all ratings of adjustment at the long-term assessment were made using the school-age version. Both versions ask parents for ratings of behavior problems. Responses are recorded on a 3-point scale (0=not true, 1=somewhat/sometimes true, and 2= very true/often true). The CBCL was standardized on a large sample of community and clinic referred children, and has demonstrated satisfactory reliability and validity in previous research(42)
Pre-injury social competence was measured by asking parents to complete either the Preschool and Kindergarten Behaviour Scales-Second Edition (PKBS-2) (43, 44) or Home and Community Social Behaviour Scale (HCSBS) (45) at the initial assessment. All parents completed the HCSBS at the long-term assessment. The PKBS and HCSBS are similar in structure and content but are normed for younger (ages 3-6 years) and older (ages 5-18 years) children, respectively. The PKBS includes a social skills scale that includes 34 items that constitute three subscales: social cooperation, social interaction, and social independence. The HCSBS has two subscales, one measuring social competence and another measuring antisocial behaviour. For the current analyses, we used the social competence composites from each measure, rescaled to both be z scores based on normative data, with higher scores indicating higher social competence. Both measures have demonstrated satisfactory reliability and validity (46, 47).
Lastly, everyday executive functioning was measured using two versions of the Behaviour Rating Inventory of Executive Function (BRIEF) (48) for preinjury ratings, depending on the age of the child at the initial assessment, and using the school-age version for all children at the long-term assessment. The BRIEF requires parents to rate everyday executive behaviours on 3-point scales (0=never, 1=sometimes, 2=often). The global executive composite (GEC) represents the child’s overall level of everyday executive functioning, with higher scores representing greater executive dysfunction. We used the GEC standard score for the current analyses.
Statistical Analyses
A series of hierarchical linear regression analyses were conducted to test our hypotheses about group differences in psychosocial outcomes and the contribution of early and later parenting to those outcomes. A six-step regression analysis was conducted for each of the three dependent variables: CBCL total problem score, PKBS-2/HCSBS social competence score, and BRIEF GEC. In step one, children’s pre-injury functioning on the outcome of interest, as rated by parents shortly after injury, was entered into the model. In step two, group was entered into the model using dummy variables for complicated mild/moderate TBI versus OI and severe TBI versus OI. Then the three early parenting style measures (authoritarian, authoritative, & permissive parenting), as rated shortly after injury, were added to the model in step three. Step four added the same parenting style variables, but as rated later, at the final assessment about 6.8 years post injury. To explore potential moderation of group differences by parenting style, we then entered interaction terms for both early (step 5) and late (step 6) parenting by group, created by multiplying each group dummy variable by each of the parenting style measures. All analyses were conducted using SPSS Statistics 22 (49).
Results
Table 2 summarizes the results of the hierarchical regression analyses. In the first step, pre-injury functioning was a significant predictor of all three psychosocial outcomes, accounting for between 21% and 32% of the variance. In step two, the two dummy variables representing group differences accounted for significant additional variance across all three outcomes, ranging from 7% to 13%. The contrast between the severe TBI and OI groups was significant for all three psychosocial outcomes. The contrast between the complicated mild/moderate TBI and OI groups was significant for behavioural adjustment (CBCL) and everyday executive functioning (BRIEF), but not for social competence (HCSBS). Estimated group means and standard errors for all three outcomes, adjusted for pre-injury functioning, are presented in Table 3.
Table 2.
Summary of hierarchical regression analyses with early and long-yerm parenting practices as predictors of long-term psychosocial outcomes.
| Step and variable: | Behavioural Adjustment (CBCL Total) | Executive Functioning (BRIEF GEC) | Social Competence (PKBS Total) |
|---|---|---|---|
| Step 1: Pre-injury psychosocial outcomes | |||
| CBCL Total score (β) | 0.56* | NI | NI |
| BRIEF GEC (β) | NI | 0.52* | NI |
| PKBS Total score (β) | NI | NI | 0.46* |
| ΔR2 | 0.32* | 0.27* | 0.21* |
| Step 2: Group | |||
| Complicated mild/moderate TBI (β) | 0.22* | 0.23* | −0.13 |
| Severe TB (β) | 0.29* | 0.34* | −0.28* |
| ΔR2 | 0.10* | 0.13* | 0.07* |
| Step 3: Early parenting | |||
| Early authoritative(β) | 0.03 | 0.03 | 0.03 |
| Early authoritarian(β) | 0.05 | 0.14 | −0.03 |
| Early permissive(β) | −0.04 | 0.08 | −0.15 |
| ΔR2 | 0.00 | 0.03 | 0.03 |
| Step 4: Late parenting | |||
| Late Authoritative (β) | −0.13 | −0.17* | 0.46* |
| Late Authoritarian_T6 (β) | 0.13 | 0.14 | −0.04 |
| Late Permissive_T6(β) | 0.20* | 0.27* | −0.18* |
| ΔR2 | 0.06* | 0.09* | 0.17 |
| Step 5: Group x Early parenting | |||
| Moderate x Early Authoritativ (β) | 1.01 | 0.55 | 0.31 |
| Moderate x Early Authoritarian (β) | 0.58 | 0.55 | 0.00 |
| Moderate x Early Permissive (β) | −0.47 | −0.12 | 0.02 |
| Severe x Early Authoritative (β) | −0.30 | −0.51 | 0.31 |
| Severe x Early Authoritarian (β) | −0.26 | 0.05 | 0.48 |
| Severe x Early Permissive (β) | 0.22 | −0.32 | −0.13 |
| ΔR2 | 0.02 | 0.01 | 0.01 |
| Step 6: Group x Late parenting | |||
| Moderate x Late Authoritative(β) | −1.18 | −0.65 | 1.15 |
| Moderate x Late Authoritarian (β) | −0.54 | −0.735 | −0.14 |
| Moderate x Late Permissive (β) | 0.70 | 0.858 | −0.32 |
| Severe x Late Authoritative (β) | 0.68 | −0.607 | 1.75* |
| Severe x Late Authoritarian (β) | −0.74 | −1.24* | 0.76 |
| Severe x Late Permissive (β) | 1.23* | 0.51 | −0.70 |
| ΔR2 | 0.06 | 0.04 | 0.04 |
NOTE. Standardized beta weights reported for variables added at each step of the analysis. Complicated mild/moderate TBI group = Moderate TBI. NI= not included. CBCL = Child Behaviour Checklist. BRIEF GEC + Behaviour Rating Inventory of Executive Functioning General Executive Composite; PKBS = Preschool and Kindergarten Behaviour Scale.
p < .05
Table 3.
Estimated means and standard errors on psychosocial outcome measures by group.
| Group | |||
|---|---|---|---|
| Outcome | Severe TBI | Moderate TBI | OI |
| Behavioural adjustment (CBCL Total) | 57.781 (2.473) | 52.514 (1.556) | 46.760 (1.173) |
| Executive functioning (BRIEF GEC) | 62.170 (2.491) | 56.185 (1.558) | 50.068 (1.166) |
| Social competence (PKBS Total) | −0.417 (0.217) | 0.131 (0.136) | 0.397 (0.101) |
The addition of early parenting style variables in step 3 did not add significantly to the prediction of the later psychosocial outcomes, and none of the early parenting style variables contributed unique variance. When late parenting style variables were added in step 4, they made a significant contribution to all three psychosocial outcomes, accounting for between 6% and 17% additional variance. Higher levels of permissive parenting predicted worse outcomes in all three domains, and higher levels of authoritative parenting predicted better executive functioning and social competence, but did not significantly predict behavioural adjustment. Authoritarian parenting was not uniquely predictive of any outcome.
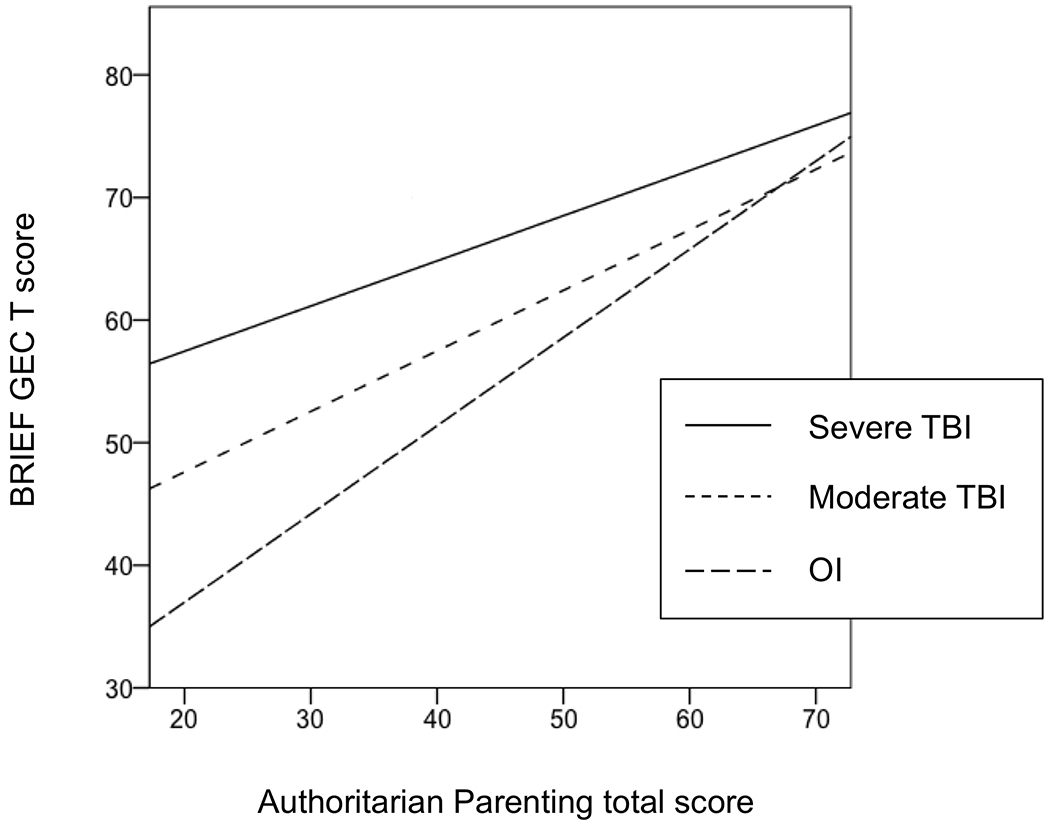
When interaction terms were added in steps 5 and 6, none of the interactions between early parenting style and group membership were significant. However, in step 6, although the six interaction terms did not collectively account for significant additional variance, significant interactions with late parenting style were found for each of the outcomes, all involving the contrast between the severe TBI and OI groups. For behavioural adjustment (CBCL), the severe TBI and OI groups differed more at higher than lower levels of permissive parenting (see Figure 1). For executive functioning (BRIEF), the severe TBI and OI groups differed more at lower than higher levels of authoritarian parenting, although higher authoritarian parenting predicted worse executive functioning in all groups (see Figure 2). For social competence, the severe TBI and OI groups differed more at lower than higher levels of authoritative parenting (see Figure 3).
Figure 1.
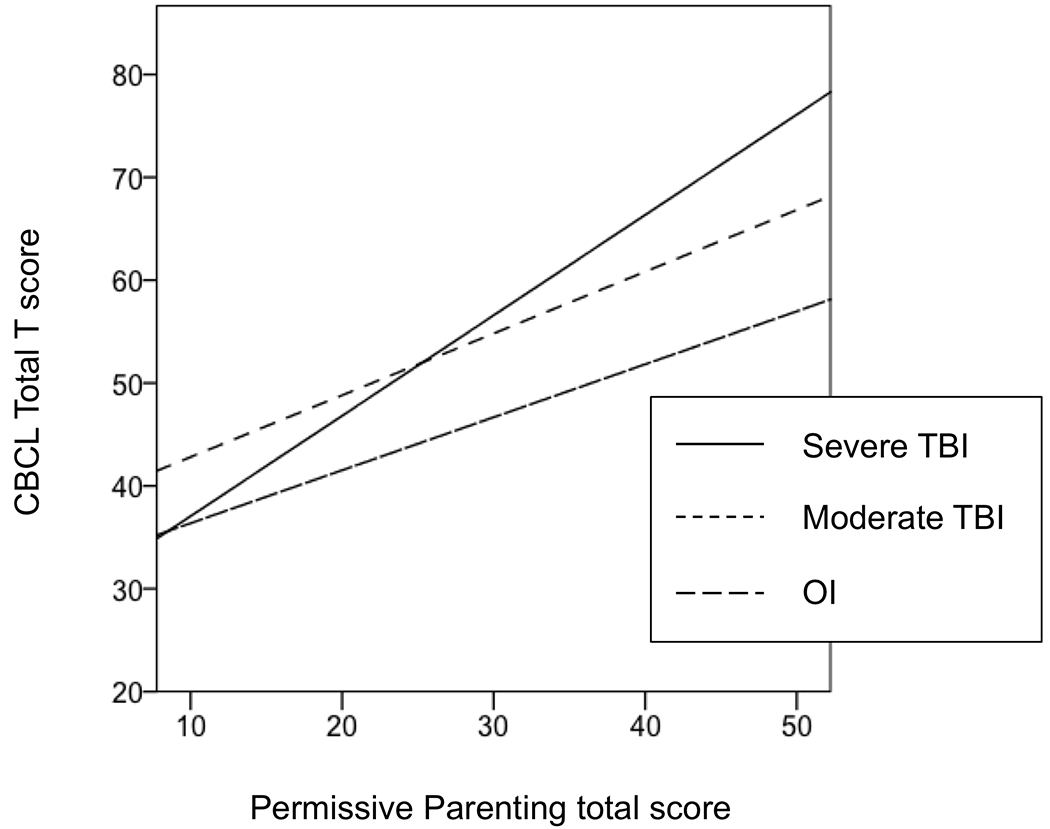
Interaction of group membership and permissive parenting in predicting behavioural adjustment.
Figure 2.
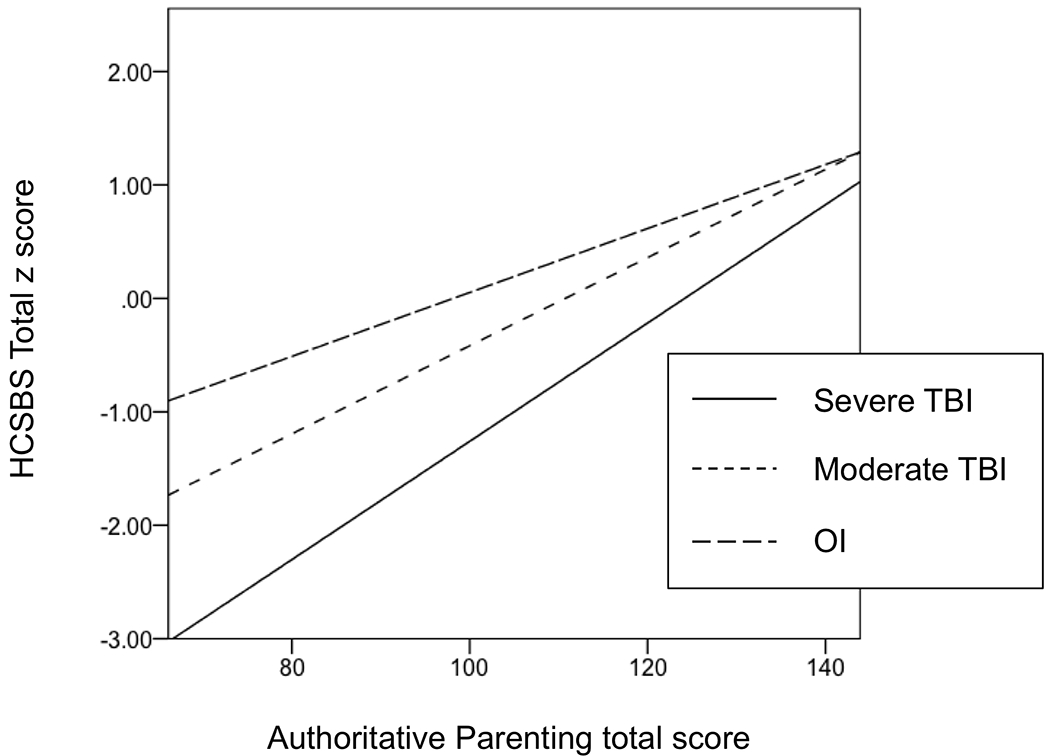
Interaction of group membership and authoritarian parenting in predicting executive functioning.
Figure 3.
Interaction of group membership and authoritative parenting in predicting social competence.
Discussion
The current study examined the association between parenting styles and long-term psychosocial outcomes following TBI in early childhood. As hypothesized, young children hospitalized for complicated mild/moderate to severe TBI displayed long-term deficits in behavioural adjustment, social competence, and everyday executive functioning relative to children with OI, with the most pronounced deficits apparent after severe TBI. Notably, these findings reflect persistent psychosocial deficits on average 6.8 years post-TBI. These results are consistent with previous studies of a variety of outcomes (e.g., cognitive abilities, adaptive functioning, executive functioning, social/behavioural skills) and their predictors (e.g., injury severity, family environment, preinjury child characteristics) after early childhood TBI up to ten years post injury (8, 9). Our findings highlight the importance of following children with early TBI over time to determine factors that may contribute to persistent deficits into adulthood.
Also as expected, parenting style was significantly associated with children’s psychosocial outcomes in both groups, although the association held true only for parenting measured later, at the time of the final assessment. At that time, higher levels of permissive parenting predicted worse outcomes in all three domains, and higher levels of authoritative parenting predicted better executive function and social competence. These findings are consistent with the previous research on the relationship of parenting style and children’s psychosocial functioning (19), and highlight the pervasive negative effects of permissive parenting, which provides little structure or support for children. Unfortunately, parenting appears to change over time after TBI in ways that may have detrimental effects (50). A recent analysis of the same participants in the current study indicated that parents of children with TBI, but not OI, show declines in warmth and involvement with their children over time, suggesting that they may become more disengaged during the transition to adolescence (26). Given changes in parenting over time, early parenting style may have less influence on later psychosocial outcomes, which are more likely to be associated with contemporaneous parenting style.
The results also provided some evidence for moderation of the effects of TBI by later but not early parenting style. Relative to children with OI, children with severe TBI displayed worse behavioural adjustment at higher levels of permissive parenting and better social competence at higher levels of authoritative parenting. These findings are consistent with previous research indicating that the long-term effects of early TBI are exacerbated by less effective parenting (e.g., permissive) and buffered by more effective parenting (e.g., authoritative) (16–20, 27). The current results also extend previous research by showing ongoing moderating effects of parenting style on psychosocial outcomes, more than 6 years after injury on average. The participants in our study are entering adolescence, which is a unique developmental period during which children and parents navigate changes in children’s independence. The current findings suggest that overly permissive parenting during adolescence may be especially detrimental.
The current results show an interesting continunity with a previous study of the same participants that showed that early permissive parenting moderated behavioural adjustment over the first 18 months post-injury (19). However, the previous study did not find early parenting to moderate social competence during the initial 18 months, in contrast to the moderation of long-term social competence by parenting found in the present study. As suggested earlier, the most likely explanation why later but not early parenting moderates later psychosocial outcomes may simply be temporal contiguity—that is, contemporaneous parenting shows a stronger association with children’s current psychosocial functioning than parenting in the past because the influence of early parenting likely wanes with time and contemporaneous parenting has a more immediate impact. We also acknowledge that the relationship between parenting and children’s functioning after TBI is likely to be bidirectional, and that early childhood social outocmes may themselves shape parenting, which in turn affecdts the same outcomes in later childhood. Indeed, we have provided evidence of bidirectional child–family influences on the outcomes of TBI in school-age children(15). Thus, parenting shapes children’s psychosocial outcomes over time, but the obverse is also true.
Surprisingly, our results also indicated that children with severe TBI demonstrated better everyday executive functioning relative to children with OI at higher levels of authoritarian parenting. These results are less consistent with previous research (19). One explanation for this finding may be that children with severe TBI, relative to those with OI, benefit from a more directive parenting style following injury, at least when it comes to their everyday executive functioning. However, given that all groups displayed an association between higher authoritarian parenting and worse everyday executive functioning (albeit of differing magnitudes), another potential account of the findings may be that the effects of severe TBI on everyday executive functioning are so pronounced that variance in that outcome is limited and the typical association of higher authoritarian parenting style with poorer executive function behaviors is reduced after severe TBI.
The current study has several strengths, including a prospective, longitudinal design, with an extended follow up period. The duration of the study allowed us to examine the long-term effect of TBI on outcomes during the critical developmental phase of emerging adolescence, as well as to contrast the association of early versus later parenting style with those outcomes. The recruitment of participants from four sites, and the retention of a representative sample over time, are also strengths. They increase the likelihood that our results are generalizable to the target population of children hospitalized for moderate-severe TBI or OI.
Nevertheless, the findings should also be interpreted in light of several study limitations. One is the small sample size, most notably for the severe TBI group, which likely reduced the power to detect group differences in psychosocial outcomes or evidence of moderation of those differences by parenting style. Shared rater variance is also a limitation in this study. Parents completed both the measures of parenting style and all of the psychosocial outcomes, and this may have led to overestimation of the strength of association between parenting and psychosocial outcomes.
The study’s findings have potential clinical implications, suggesting that interventions to promote more effective parenting may help foster better child outcomes. Although parenting interventions shortly after preschool TBI have already shown short-term benefits (51), the current finding that late but not early parenting moderated long-term psychosocial outcomes may indicate a need for ongoing monitoring of children and their parents after TBI in early childhood. For children who are experiencing persistent negative psychosocial outcomes, the findings suggest that the provision of interventions to promote more effective parenting may be beneficial to children with TBI even years after injury.
Implications for Rehabilitation:
Children with traumatic brain injury (especially those with severe injuries) are likely to require long-term monitoring and rehabilitation to address their psychosocial functioning
Interventions that focus on parenting may be an important avenue for promoting better psychosocial outcomes among children with severe traumatic brain injury
Footnotes
Declarations of Interest
The authors report no conflicts of interest.
References:
- 1.Humphreys I, Wood RL, Phillips CJ, Macey S. The costs of traumatic brain injury: A literature review. . Clinicoecon Outcomes Res. 2013;5:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roozeneek B, Maas AI, Menon DK Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurosci . 2013;9:6. [DOI] [PubMed] [Google Scholar]
- 3.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Functional plasticity or vulnerability after early brain injury? Pediatrics 2005;116:9. [DOI] [PubMed] [Google Scholar]
- 4.Levin H, Hanten G. Executive functions after traumatic brain injury in children. Pediatr Neurol. 2005;33:14. [DOI] [PubMed] [Google Scholar]
- 5.Yeates KO, Swift E, Taylor HG, Wade SL, Drotar D, Stancin T, & Minich N Short-and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10:15. [DOI] [PubMed] [Google Scholar]
- 6.Yeates K, Levin HS, Ponsford J. The Neuropsychology of Traumatic Brain Injury: Looking Back, Peering Ahead. J INS. 2017;23:12. [DOI] [PubMed] [Google Scholar]
- 7.Potter J, Wade SL, Walz NC, Cassedy A, Yeates KO, Stevs HM, Taylor GH. Parenting style is related to executive dysfunction after brain injury in children. Rehabil Psychol. 2011;56(4):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson VGC, Rosenfeld JV, Catroppa C. Predictors of cognitive function and recovery 10 years after traumatic brain injury in young children. Pediatrics. 2012;129:8. [DOI] [PubMed] [Google Scholar]
- 9.Anderson VGC, Rosenfeld JV, Catroppa C. 10 years outcome from childhood traumatic brain injury. Int J Dev Neurosci. 2012;30:8. [DOI] [PubMed] [Google Scholar]
- 10.Beauchamp M, Catroppa C, Godfrey C, Morse S, Rosenfeld JF, Anderson V. Selective changes in executive functioning ten years after severe childhood traumatic brain injury. Dev Neuropsychol. 2011;36(5):18. [DOI] [PubMed] [Google Scholar]
- 11.Mangeot S, Armstrong K, Colvin AN, Yeates KO, Taylor GH. Long-term executive function deficits in children with traumatic brain injuries: Assessment using the Behaviour Rating Inventory of Executive Function (BRIEF). . Child Neuropsychol. 2010;8(4):14. [DOI] [PubMed] [Google Scholar]
- 12.Kuehn B Lasting Effects of Childhood TBI. JAMA. 2018;319(14). [DOI] [PubMed] [Google Scholar]
- 13.Taylor H, Yeates KO, Wade SL, Drotar D, Klein SK, Stancin T. Influences on first-year recovery from traumatic brain injury in children. . Neuropsychology. 1999;13:14. [DOI] [PubMed] [Google Scholar]
- 14.Yeates K, Taylor HG, Drotar D, Wade SL, Klein SK, Stancin T. Premorbid family environment as a predictor of neurobehavioral outcomes following pediatric TBI. J INS. 1997;3:14. [Google Scholar]
- 15.Taylor H, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury in children. J Int Neuropsychol Soc. 2001;7(6):13. [DOI] [PubMed] [Google Scholar]
- 16.Wade S, Borawski EA, Taylor HG, Drotar D, Yeates KO. The relationship of caregiver coping to family outcomes during the initial year following pediatric traumatic injury. J Consult Clin Psych. 2001;69(3):10. [DOI] [PubMed] [Google Scholar]
- 17.Wade S, Cassedy A, Walz NC, Taylor HG, Stancin T, Yeates KO. The relationship of parental warm responsivness and negativity to emerging behaviour problems following traumatci brain injury in young children. Dev Psychol. 2011;47(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yeates K, Taylor HG, Drotar D, Wade SL, Klein S, Stancin T, Schatschneider C. Preinjury family environment as a detererminant of recovery from traumatic brain injuries in school age children. J Int Neuropsychol Soc. 1997;3(6):14. [PubMed] [Google Scholar]
- 19.Yeates K, Taylor HG, Walz NC, Stancin T, Wade SL. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010;24(3):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wade S, Zhang N, Yeates KO, Stancin T, Taylor HG. Social Environmental Moderators of Long-term Functional Outcomes of Early Childhood Brain Injury. JAMA Pediatr. 2016;170(4):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bradley RH, Corwyn RF, Caldwell BM, Whiteside-Mansell L, Wasserman GA, & Mink IT. Measuring the home environments of children in early adolescence. J Res Adolesc. 2000;10:42. [Google Scholar]
- 22.Caldwell B, & Bradley R. . Home observation for measurement of the environment. Little Rock: University of Arkansas at Little Rock 1984. [Google Scholar]
- 23.Durber C, Yeates KO, Taylor HG, Walz NC, Stacin T, Wade SL The family environment predicts long-term academic achievement and classroom behavior following traumatic brain injury in early childhood. Neuropsychology. 2017;31(5):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Durish C, Yeates KO, Stancin T, Taylor HG, Walz NC, Wade SL. Home Environment as a Predictor of Long-Term Executive Functioning following Early Childhood Traumatic Brain Injury. . J Int Neuropsychol Soc. 2017;23:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glascoe F, Leew S. Parenting behaviors, perceptions, and psychosocial risk: impacts on young children’s development. Pediatrics. 2010;125(2):7. [DOI] [PubMed] [Google Scholar]
- 26.Narad M, Treble-Barna A, Zang H, Zhang N, Smith J, Yeates KO, Taylor HG, Stancin T, Wade SL Parenting Behaviors after Moderate – Severe Traumatic Injury in Early Childhood Dev Neurorehabil. 2018. 1(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Micklewright J, King TZ, O’Toole K, Henrich C, Floyd FJ. Parental distress, parenting practices, and child adaptive outcomes following traumatic brain injury. J Int Neuropsychol Soc. 2012;18(2):8. [DOI] [PubMed] [Google Scholar]
- 28.Baumrind D Current patterns of parental authority. Dev Psychol. 1971;4(1):104. [Google Scholar]
- 29.Allen JP, Hauser ST, Eickholt C, Bell KL, & O’Connor TG Autonomy and relatedness in family interactions as predictors of expressions of negative adolescent affect. J Res Adolesc. 1994;4(4):18. [Google Scholar]
- 30.Shaffer A, Lindhiem O, Kolko D, Trentacosta C Bidirectional Relations between Parenting Practices and Child Externalizing Behavior: A Cross-Lagged Panel Analysis in the Context of a Psychosocial Treatment and 3-Year Follow-up. J Abnorm Child Psychol. (2013).41(2):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burke J, Pardini D, Loeber R. Reciprocal Relationships Between Parenting Behavior and Disruptive Psychopathology from Childhood Through Adolescence. J Abnorm Child Psychol. 2008;36(5):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hipwell A, Keenan K, Kasza K, Loeber R, Stouthamer-Loeber M, Bean T Reciprocal influences between girls’ conduct problems and depression, and parental punishment and warmth: A six year prospective analysis. J Abnorm Child Psychol. 2008;36(5):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pardini DA, Fite PJ, & Burke JD Bidirectional associations between parenting practices and conduct problems in boys from childhood to adolescence: The moderating effect of age and African-American ethnicity. J Abnorm Child Psychol. 2008;36(5):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Serbin LA, Kingdon D, Ruttle PL, Stack DM . The impact of children’s internalizing and externalizing problems on parenting: Transactional processes and reciprocal change over time. Dev and Psychopathol. 2015;27(4). [DOI] [PubMed] [Google Scholar]
- 35.Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems after pediatric traumatic brain injury: Prevalence, predictors, and correlates. J Pediatr Psychol. 2003;28:14. [DOI] [PubMed] [Google Scholar]
- 36.Narad ME T-B A, Peugh J, Yeates KO, Taylor HG, Stancin T, Wade SL. Recovery trajectories of executive functioning after pediatric TBI: a latent class growth modeling analysis. J Head Trauma Rehab. 2017;32(2):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Teasdale G, & Jennett B. . Assessment of coma and impaired consciousness. A practical scale. . Lancet. 1974;2:5. [DOI] [PubMed] [Google Scholar]
- 38.Kashluba S, Hanks RA, Casey JE, & Mills SR . Neuropsychologic and functional outcome after complicated mild traumatic brain injury. Arch Phys Med Rehabil. 2008;89:8. [DOI] [PubMed] [Google Scholar]
- 39.Robinson C, Mandleco B, Olsen SF, Hart CH. Authoritative, authoritarian, and permissive parenting practices: development of a new measure. . Psychol Rep. 1995;77(3):12. [Google Scholar]
- 40.Robinson C, Mandleco B, Olsen SF, Hart CH. The Parenting Styles and Dimensions Questionnaire (PSDQ) . In: Perlmutter BFTJ, Holden GW, editor. Handbook of Family Measurement Techniques: Instruments & Index Vol 3 Thousand Oaks, CA: Sage; 2001. p. 3. [Google Scholar]
- 41.Achenbach T, Rescorla LA. Manual for ASEBA Preschool Forms & Profiles. Burlington: University of Vermont, Research Center for Children, Youth, & Families; ; 2000. [Google Scholar]
- 42.Achenbach T, Rescorla LA. Manual for ASEBA School- Aged Forms & Profiles. Burlington: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 43.Merrell K Social-emotional assessment in early childhood: The Preschool and Kindergarten Behavior Scales. . J Early Interv. 1996;20:14. [Google Scholar]
- 44.Merrell K. Preschool and Kindergarten Behavior Scales (2nd ed.). . Austin, TX: PRO-ED; 2002. [Google Scholar]
- 45.Merrell K, Caldarella P. Home & Community Social Behavior Scales. Eugene, OR: Assessment Intervention Resources; ; 2002. [Google Scholar]
- 46.Lund J, Merrell KW. Social and antisocial behavior of children with learning and behavioral disorders: Construct validity of the Home and Community Social Behavior Scales. J Psychoeduc Assess. 2001;19:11. [Google Scholar]
- 47.Merrell K, Streeter AL, Boelter EW. Validity of the Home and Community Social Behavior Scales: Comparisons with five behavior-rating scales. . Psychol Sch. 2001;38:13. [Google Scholar]
- 48.Gioia G, Isquith PK, Guy SC, Kenworthy L. Test Review: Behavior Rating Inventory of Executive Function. Child Neuropsychol. 2000;6(3):8. [DOI] [PubMed] [Google Scholar]
- 49.Corp. I. IBM SPSS Statistics for Mac, Version 22.0. Armonk, NY: IBM Corp; 2013. [Google Scholar]
- 50.Luyckx KTE, Soenens B, Andrews JA, Hampson SE, Peterson M, Duriez B. Parenting and trajectories of children’s maladaptive behaviors: a 12-year prospective community study. J Clin Child Adolesc. 2011;40(3):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wade S, Cassedy AE, Shultz EL, Zang H, Zhang N, Kirkwood MW, Stancin T, Yeates KO, Taylor HG. Randomized Clinical Trial of Online Parent Training for Behavior Problems After Early Brain Injury. J Am Acad Child Adolesc Psychiatry. 2017;56(11):10. [DOI] [PubMed] [Google Scholar]


