Abstract
Objective The main aim of this article is to report 10-year outcomes after Essex-Lopresti injury (ELI).
Study Design Retrospective case series. Two level I trauma centers and one associated community hospital from 2003 to 2016.
Patients Sixteen patients who sustained an ELI and were treated at one of our three regional hospitals.
Intervention Initially, 4 patients (25%) were treated nonoperatively by immobilization and 12 patients (75%) were treated operatively. Proximal surgery included radial head open reduction and internal fixation (ORIF), radial head arthroplasty, radial head excision and forearm ORIF, and wound debridement. Ten patients (63%) were acutely identified with longitudinal forearm instability. Of these, four patients had the distal radioulnar joint pinned. In the other six patients, the forearm was immobilized. Overall, 16 patients underwent a total of 32 revision surgeries.
Main Outcome Measure Performance of Patient-Reported Outcomes Measurement Information System Upper Extremity (PROMIS UE) Physical score, Numeric Rating Scale (NRS) score for pain-severity, and NRS score for satisfaction of overall outcome.
Results Follow-up for outcome evaluation was available for 10 patients, at a median of 10 (interquartile range [IQR]: 8.0–12) years after date of injury. The median PROMIS UE Physical score was 36 (IQR: 33–38). Median NRS score for pain-severity on average was 5 (IQR: 0–6). The median NRS score for satisfaction of overall outcome was 7 (IQR: 5–8).
Conclusion Patients who sustain an ELI generally have substantial deficits of upper extremity function as measured by PROMIS UE. Early radial head arthroplasty may be beneficial, but further study in a larger cohort is needed. Outcomes of nonoperative treatment and operative treatment were similar and suggest that current surgical treatments are incomplete.
Keywords: distal radioulnar joint disruption, Essex-Lopresti, interosseous membrane rupture, longitudinal forearm dissociation
Introduction
The Essex-Lopresti injury (ELI) consists of a fracture of the radial head and disruption of the soft tissue restraints between the radius and the ulna, including the interosseous ligament (IOL). 1 There is a general consensus that acute surgery is preferred, but not always feasible. 1 2 3 4 5 6 7 8 9 10 11 Because diagnosis is not always immediately clear and this injury involves multiple structures, multiple surgeries are common. 4 11 12 13 14
Surgical treatment of the proximal forearm ranges from radial head fixation to replacement, and treatment of the distal forearm ranges from simple immobilization to distal radioulnar joint (DRUJ) stabilization with pins. Late reconstruction may involve IOL reconstruction, or may involve late salvage such as Sauvé-Kapandji or creation of a single bone forearm. 3 6 7 8 9 10 11
We sought to describe patient, injury, and treatment characteristics and to report long-term outcomes after treatment of patients presenting with ELI at a metropolitan health system encompassing two tertiary level academic medical centers.
Methods
Patient Selection
This retrospective case series was approved by our institutional review board. International Classification of Diseases (ICD) codes for radial head fracture and subluxation/dislocation of the DRUJ were used to identify patients. Sixteen patients were treated for an ELI at one of our three regional hospitals: two level I trauma centers and one associated community hospital between January 2003 and December 2016.
All clinical, operative, and radiologist reports were assessed for (variations and misspellings of) “Essex-Lopresti”/”longitudinal forearm dissociation.” Patients who had a mention of any of these terms were reviewed for inclusion and were characterized by the triad of radial head fracture, interosseous membrane (IOM) rupture, and DRUJ disruption. The diagnosis of an ELI was established by a combination of clinical signs and radiographic evidence: widening of the DRUJ, proximal migration of the radius, or dorsal subluxation of the ulna on radiographs of the wrist ( Fig. 1 ).
Fig. 1.
Radiographs of the wrist ([A] posteroanterior, [B] lateral) at day of presentation, with evident widening of distal radioulnar joint and dorsal subluxation on the ulna.
Outcome Evaluation
Patients were sent a letter of invitation to participate in or opt-out of the study. We approached participating patients to complete patient-rated outcomes surveys administered over the Internet or over the phone. 15 16 The level of pain on average in both the elbow and the wrist was assessed using a Numeric Rating Scale (NRS), with 0 indicating no pain and 10 indicating the worst pain imaginable. Satisfaction with the overall outcome of their treatment was also assessed using a NRS, with 0 indicating not satisfied at all and 10 indicating highly satisfied. Patients were asked to complete the Performance of Patient-Reported Outcomes Measurement Information System (PROMIS) Upper Extremity Physical Function computed tomography to evaluate physical function and upper extremity disability. In this questionnaire, a T-score of 50 represents the norm in the US population, and every 10 points represent a standard deviation from the norm. 17
Statistical Analysis
We described discrete data using frequencies and percentages, and non-normally distributed continuous data through medians and interquartile ranges (IQRs). For our bivariate analysis, we used the Mann–Whitney U -test.
Results
Patient Characteristics
There were 14 men and 2 women with a mean age of 42 ± 10 years at the time of injury ( Table 1 ). Six patients (38%) were treated at outside facilities before presenting to us. Three of these six patients underwent surgical intervention at the radial head (one open reduction and internal fixation (ORIF) of the radial head, one radial head prosthesis, and one radial head excision). These patients presented to our institution after late complaints of wrist pain following initial treatment. The other three patients were treated conservatively initially and were diagnosed with longitudinal forearm instability after delayed development of wrist and elbow symptoms.
Table 1. Patient and injury characteristics.
| Patient | Age at injury | Sex | Side injury | Mechanism of injury | Type a | Additional injury to upper limb |
|---|---|---|---|---|---|---|
| Abbreviations: LCL, lateral collateral ligament; MC, metacarpal; MVA, motor vehicle accident; TFCC, triangular fibrocartilage complex. a Classification by Edwards and Jupiter (1988). b Based on available data in charts. | ||||||
| 1 | 65 | F | Left | Fall | 1 | TFCC tear |
| 2_right | 40 b | M | Right | Fall from height | 3 | Not extractable from chart |
| 2_left | 40 b | Left | Fall from height | 3 | TFCC tear | |
| 3 | 36 | M | Left | Fall from height | 2 | None |
| 4 | 40 b | M | Left | Fall from height | 1 | Unstable MCL and LCL |
| 5 | 44 | M | Left | Fall from height | 1 | None |
| 6 | 24 b | M | Left | Fall | 3 | Not extractable from chart |
| 7 | 34 | M | Right | Fall | 2 | Unstable LCL |
| 8 | 43 | M | Right | Fall from height | 1 | None |
| 9 | 46 | F | Right | Fall | 1 | None |
| 10 | 36 | M | Left | Fall | 1 | TFCC tear, hamate hook fracture |
| 11 | 41 | M | Left | Fall from height | 2 | Unstable LCL, index MC fracture |
| 12 | 49 | M | Left | Fall from height | 1 | Unstable LCL, scaphoid fracture |
| 13 | 52 | M | Left | Fall from height | 2 | Unstable LCL |
| 14 | 45 | M | Right | MVA | 2 | None |
| 15 | 27 | F | Left | Fall from height | 1 | Distal radius fracture |
| 16 | 53 | M | Left | Fall from height | 2 | None |
Injury Characteristics
Ten patients (63%) had falls from a height, four (25%) had a simple fall, one (6.3%) was injured playing sports, and one (6.3%) was injured in a motor vehicle accident ( Table 1 ). Nine (56%) patients had additional injuries to the upper limb, five (31%) had injuries in other limbs or organ systems, and four (25%) had an isolated ELI. One patient (6.3%) presented with bilateral longitudinal forearm instability. Of the five patients that underwent ORIF, in three cases there were greater than three radial head fragments present and in two cases, the operative notes did not describe the number of fragments. The type of ELI was based on the previously described classification by Edwards and Jupiter: type I—radial head fracture with a large displaced fragment amenable to ORIF; type II—comminuted radial head fracture not amenable to ORIF; and type III—irreducible proximal migration of the radius. 4 Eight patients (50%) had a type I injury, six (38%) had a type II injury, and two (13%) had a type III injury.
Treatment
Initial Treatment
The initial treatment was defined as the treatment that was chosen as initial definitive management. Four patients (25%) were treated nonoperatively by immobilization and 12 patients (75%) were treated operatively ( Table 2 ). Three patients were treated nonoperatively because the injury was not recognized initially. One patient treated nonoperatively elected not to pursue intervention. Proximal surgery included radial head ORIF ( n = 5, 31%), radial head arthroplasty ( n = 5, 31%), radial head excision and forearm ORIF ( n = 1, 6.5%), and wound debridement ( n = 1, 6.5%). Ten patients (63%) were acutely identified with longitudinal forearm instability. Of the 10 who underwent radial head ORIF or arthroplasty, 4 had the DRUJ pinned. In the other six patients, the forearm was immobilized for a period between 3 and 8 weeks. Four patients had a chronic injury (defined as older than 6 weeks) at the time of their first surgical intervention.
Table 2. Treatment-related characteristics.
| Abbreviations: DRUJ, distal radioulnar joint; ECU, extensor carpi ulnaris; LCL, lateral collateral ligament; MC, metacarpal; MCL, medial collateral ligament; ORIF, open reduction internal fixation; PRUJ, proximal radioulnar joint; TFCC, triangular fibrocartilage complex. | |||||||
| 1 | No | 2 wk | ORIF radial head and DRUJ pinning | Open TFCC repair | Removal of hardware and arthrotomy left elbow with capsular excision | 2 | |
| 2_right | Yes | ORIF forearm and radial head excision | 12 y | Radial head prosthesis | Ulna shortening osteotomy and lateral epicondyle debridement | 1. Hardware removal ulnar shaft, revision radial head prosthesis, capitellum prosthesis, ulnar wrist release with flexor pronator Z lengthening with submuscular transposition 2. Median nerve release, elbow arthroscopy with synovectomy and osteectomy of posterolateral olecranon 3. Wrist arthroscopy and synovectomy, DRUJ arthroplasty with Aptis prosthesis |
5 |
| 2_left | Yes | ORIF forearm and radial head excision | 12 y | Radial head prosthesis and DRUJ stabilization with ECU tendon graft | Wrist arthroscopy, TFCC debridement, ulnar nerve release, flexor pronator z lengthening, lunate triquetral reconstruction using extensor retinaculum, pinning lunate triquetral | 1. Revision radial head prosthesis, distal ulnar resection, median and radial nerve release 2. DRUJ arthroplasty with Aptis prosthesis 3. Removal DRUJ prosthesis, DRUJ fusion with iliac crest bone grafting Redo DRUJ effusion with right side iliac crest bone grafting 4. Removal of hardware Left wrist arthroscopy with complete synovectomy, left elbow open arthrotomy with debridement and synovectomy 5. Left elbow and wrist arthroscopy with synovectomy and debridement |
9 |
| 3 | No | 2 wk | Radial head prosthesis | 1. Removal of radial head prosthesis and debridement of heterotopic ossification | 2 | ||
| 4 | No | 1 wk | ORIF radial head | Repair LCL and MCL, ulnar nerve neurolysis | 1. Radial head prosthesis 2. Ulna shortening osteotomy |
3 | |
| 5 | Yes | Nonoperative treatment | 8 mo | Debridement radial head with microfracturing | Anterior capsule release | 1. Radial head excision 2. Radial head prosthesis |
3 |
| 6 | Yes | Radial head prosthesis, removal prosthesis | 15 y | Debridement PRUJ | 1. Radial head prosthesis 2. Removal radial head prosthesis and fusion with iliac crest bone graft 3. Removal of hardware |
6 | |
| 7 | yes | Nonoperative treatment | 6 wk | Radial head prosthesis and DRUJ pinning | Repair LCL | 1 | |
| 8 | No | 1 wk | ORIF radial head | 1. Removal of hardware | 2 | ||
| 9 | No | n/a | Nonoperative treatment | 0 | |||
| 10 | No | n/a | Nonoperative treatment | 0 | |||
| 11 | No | 2 wk | Radial head prosthesis and DRUJ pinning | Repair LCL, ORIF index MC fracture | 1 | ||
| 12 | No | 1 d | ORIF radial head | Repair LCL | 1 | ||
| 13 | No | 3 d | Radial head prosthesis and DRUJ pinning | Repair LCL | 1. Removal of hardware (pins DRUJ) 2. Reconstruction DRUJ with free tendon graft 3. Sauvé-Kapandji arthrodesis |
4 | |
| 14 | Yes | Debridement wound and repair triceps laceration | 8 mo | Radial head excision | Excision heterotopic ossification PRUJ, excision distal ulna | 2 | |
| 15 | Yes | ORIF radial head and distal radius fracture, release compartment syndrome, removal pins | 8 mo | Removal of hardware | Excision heterotopic ossification, capsular release | 4 | |
| 16 | No | 2 wk | Radial head prosthesis and DRUJ pinning | 1. Excision scar and heterotopic ossification elbow | 2 | ||
Subsequent Operations
Overall, 16 patients underwent a total of 32 revision surgeries (median 1; interquartile range [IQR]: 1–3). The median time from the injury to final surgery was 8 months (IQR: 4–15).
Reoperation at the Proximal Forearm
Nine patients (56%) underwent a reoperation at the proximal forearm. Four of the five patients (80%) who underwent plate fixation of the radial head or neck underwent reoperation to remove the plates. Three patients had plates removed for hardware irritation. One patient had failure of fixation and underwent a revision to a radial head arthroplasty. Two of the five patients (40%) with radial head prostheses underwent resection arthroplasty because of pain and restricted motion of the elbow. Seven patients underwent late operative intervention at the elbow involving capsular release with joint debridement.
Reoperation at the Distal Forearm
Four patients (25%) underwent a reoperation at the distal forearm. DRUJ reconstruction was attempted in three forearms (two DRUJ replacements with implant arthroplasty, and one DRUJ reconstruction using a palmaris longus weave). Two of the three reconstructed DRUJs ultimately underwent further revision, with one of the implant arthroplasties being revised to a one-bone forearm, and the DRUJ reconstructed using a palmaris longus weave later underwent fusion through a Sauvé-Kapandji procedure. One additional patient with persistent pain and severe DRUJ arthritis also underwent creation of a one-bone forearm by DRUJ fusion with iliac crest bone graft ( Fig. 2 ). Three patients underwent ulnar shortening osteotomy. No patient underwent IOL reconstruction.
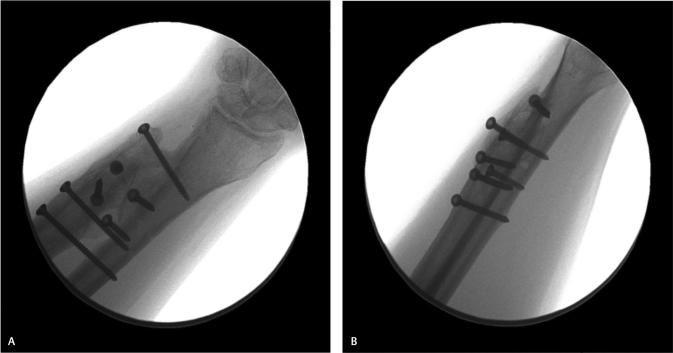
Fig. 2.
Radiographs of the wrist ([A] posteroanterior, [B] lateral) after distal radioulnar joint fusion with iliac crest bone graft.
Outcomes
Follow-up for outcome evaluation was available for 10 patients, at a median of 10 (IQR: 8.0–12) years after date of injury. The median PROMIS Upper Extremity Physical score was 36 (IQR: 33–38). Median NRS score for pain-severity on average was 5 (IQR: 0–6). The median NRS score for satisfaction of overall outcome was 7 (IQR: 5–8) ( Table 3 ).
Table 3. Outcome assessment categorized by initial treatment.
| Measurement | |||||
|---|---|---|---|---|---|
| Case number | PROMIS UE | Pain (0–10) | Satisfaction (0–10) | Number of surgeries | Follow-up (in years) |
| Nonoperative | |||||
| Abbreviations: ORIF, open reduction internal fixation; PROMIS UE, performance of patient-reported outcomes measurement information system upper extremity. | |||||
| 5 | 27.1 | 5 | 0 | 3 | 11 |
| 7 | 44.4 | 0 | 10 | 1 | 15 |
| 9 | 37.5 | 5 | 6 | 0 | 12 |
| 10 | 56.4 | 0 | 5 | 0 | 8.1 |
| Operative | |||||
| Radial head ORIF | |||||
| 1 | 30.4 | 6 | 2 | 2 | 12 |
| 15 | 32.9 | 4 | 5 | 4 | 2.2 |
| Radial head excision | |||||
| 2R | 32.9 | 6 | 7 | 5 | 24 |
| 2L | 32.9 | 6 | 7 | 9 | 24 |
| Radial head arthroplasty | |||||
| 11 | 36.0 | 0 | 10 | 1 | 9.8 |
| 13 | 37.4 | 5 | 7 | 4 | 8.0 |
| 16 | 36.7 | 2 | 8 | 2 | 3.8 |
Classifying by initial treatment (nonoperative vs. operative), we found for conservative treatment a median PROMIS Upper Extremity Physical score of 41 (IQR: 32–50), a median NRS score for pain-severity on average of 2.5 (IQR: 0–5), and a median NRS score for satisfaction of overall outcome of 5.5 (IQR: 2.5–8). For operative treatment, we found a median PROMIS Upper Extremity Physical score of 33 (IQR: 33–37), a median NRS score for pain-severity on average of 5 (IQR: 2–6), and a median NRS score for satisfaction of overall outcome of 7 (IQR: 5–8) ( Table 3 ). An additional analysis was performed to compare the patients initially treated with DRUJ pinning versus those not initially treated with DRUJ pinning. With our cohort, we did not identify differences when looking at PROMIS Upper Extremity Physical score (median of 36 vs. 33; p = 0.85), NRS score for pain-severity (median of 3.5 vs. 5; p = 0.85), and NRS score for satisfaction of overall outcome (median of 7.5 vs. 6; p = 0.39).
Discussion
Longitudinal forearm instability arises because of structural incompetence of the radial head, IOL, and DRUJ. 1 3 4 18 19 20 Treatment approaches vary widely. We aimed to describe a cohort of patients including the treatment course and long-term patient-reported outcomes for this difficult injury pattern. There is a high reoperation rate at both the proximal and distal forearm, persistent deficits in long-term physical function, and a high prevalence of residual pain. Regardless of treatment, it appears that most patients have residual upper limb disability, with a median PROMIS UE of 36 and a median NRS pain score of 5.
This study is limited in its retrospective nature. As no specific ICD code exists for ELI, we used a combination of codes for radial head fracture and subluxation/dislocation of the DRUJ, which introduces the possibility that patients were missed due to misclassification of their injury. Surveys were administered over the Internet or over the phone, so it was not possible to evaluate objective functional status such as range of motion and grip strength. Given the small sample size and the diversity of procedures used to treat these patients, limited conclusions can be drawn from this cohort. However, this report is unique in its inclusion of long-term patient-reported outcomes, with follow-up at a median of 10 years after date of injury. Further, this cohort consists of a variety of early and late diagnosed ELI patients whose treatment was based on timing and recognition of symptoms.
Research about the most optimal treatment for ELI remains inconclusive because of the complexity of the diagnosis, which is often overlooked. In a series of 20 patients, only 25% were fully recognized acutely, with 75% delayed diagnosis on an average of 7.92 years after injury. 11 Another study reported a correct diagnosis in the acute situation in 38% among 106 referral cases. 21 Often the radial head fracture is diagnosed and treated at initial presentation, but the injury of the IOM and DRUJ is missed. 4 5 Six patients (37%) in our series did not have immediate recognition of their injury.
In our series, 10 patients (63%) were acutely identified with longitudinal forearm instability and underwent DRUJ immobilization by pinning or splinting besides treatment of their elbow injury. Treatment options for reestablishing forearm stability continue to evolve, because of increasing knowledge about forearm anatomy and instability patterns. 20 A variety of augmentation techniques have been investigated for IOM reconstruction. In our cohort, there were no attempts to directly address IOM injury surgically. 2 18 22 23 24
In elbow fracture dislocations, radial head fractures with three or fewer articular fragments may be amenable to ORIF, but with multiple fragments in the unstable elbow, arthroplasty is recommended. 1 12 25 26 27 Edwards and Jupiter found that radial excision alone led to poor results, and recommended an ulna shortening procedure with radial head arthroplasty when not immediately recognized as an ELI. 4 In our series of ELI injuries, there was a trend toward better long-term function, higher satisfaction scores, and lower pain scores when the radial head was replaced as initial treatment, suggesting that arthroplasty may be a preferred route of treatment. However, regardless of treatment technique used at the proximal forearm, our cohort demonstrated a high rate of reoperation at this location. Two out of five radial head prostheses were removed because of pain and limited motion, and all four patients undergoing ORIF with plates ultimately underwent removal of hardware or radial head excision.
Late treatment may be more problematic because the proximal migration of the radius and persistent dislocation of the DRUJ may be difficult once tissues stretch or contract permanently. 3 6 7 10 11 28 Suggested treatment for chronic or untreated ELI includes salvage procedures such as the ulna-shortening or Sauvé-Kapandji procedure, IOL reconstruction, or creation of a one-bone forearm as the ultimate salvage for a painful and unstable forearm. 2 3 6 7 10 11 19 20 21 28 In our cohort, 4 out of 16 patients (25%) underwent some form of salvage procedure. IOL reconstruction in our metropolitan area has not been widely utilized.
Previous studies that included patient-reported outcomes after treatment of ELI demonstrated comparable persistent deficits in upper extremity physical function, with DASH scores (Disabilities of the Arm, Shoulder and Hand Outcome Measure) ranging between 20.5 and 55 (mean 33.7; Table 4 ). 5 7 10 23 24 29 Similar DASH scores can be found after upper extremity amputation. A study from Pet et al reported a mean DASH score of 24.6 in replantation patients and a mean DASH score of 39.8 in patients with prosthetic rehabilitation. 30 The median PROMIS UE score in our study was 36 (IQR: 33–38). Scores for residual pain are slightly lower than shown in our study, ranging between 2 and 3.3 (mean 2.6). 3 10 Our study found a median NRS score for pain-severity on average of 5 (IQR: 0–6). We found similar outcomes for physical function and pain, when comparing nonoperative versus operative initial treatment, with the exception of one patient treated nonoperatively who had a PROMIS UE of 56. This patient had a partial articular fracture of the radial head and a DRUJ dislocation, but it is possible that this was a complete ELI. Overall, regardless of treatment course, ELI generally results in a substantial functional deficit for long term.
Table 4. Overview studies that include “patient-reported outcomes” after treatment of Essex-Lopresti injury.
| Study | Number of patients | Mean follow-up (in months) | Initial treatment radial head | Initial treatment DRUJ | Number of patients that underwent revision surgery | Patient-reported outcome |
|---|---|---|---|---|---|---|
| Abbreviations: ORIF, open reduction internal fixation; DASH, disability of the arm, shoulder, and hand; DRUJ, distal radioulnar joint; IOM, interosseous membrane; VAS, visual analog scale. | ||||||
| Jungbluth et al (2006) 7 | 12 | 29 | Radial head excision (3), radial head arthroplasty (8) | Sauvé-Kapandji (3) | 3 | DASH = 55 |
| Hii et al (2013) 29 | 1 | 6 | Radial head ORIF | Closed reduction | 0 | DASH = 44 |
| Grassmann et al (2014) 5 | 12 | 59 | Radial head ORIF (2), radial head arthroplasty (8) | DRUJ pinning (12) | 0 | DASH = 20.5 |
| Venouziou et al (2014) 3 | 7 | 33 | Radial head arthroplasty (7) | Ulna shortening osteotomy (5) | 2 | VAS pain = 3.3 |
| Gaspar et al (2016) 23 | 10 | 35 | Radial head ORIF (1), radial head excision (2), radial head arthroplasty (3) | – | 10 (all underwent IOM reconstruction) | DASH = 24 |
| Schnetzke et al (2017) 10 | 31 | 64 | Nonoperative (10), radial head ORIF (13), radial head excision (1), radial head arthroplasty (7) | DRUJ pinning (16) | 20 | DASH = 29, VAS pain elbow = 2, VAS pain wrist = 2.4 |
| Gaspar et al (2018) 24 | 33 | 131 | Radial head ORIF (6), radial head excision (12), radial head arthroplasty (5) | – | 33 (all underwent IOM reconstruction) | DASH = 29.8 |
In conclusion, patients who sustain an ELI generally have substantial deficits of upper extremity function as measured by PROMIS UE. Early radial head arthroplasty rather than radial head ORIF or excision may be beneficial, but further study in a larger cohort is needed. Outcomes of nonoperative treatment and operative treatment were similar and suggest that current surgical treatments are incomplete.
Funding Statement
Funding None.
Footnotes
Ethical ApprovalConflict of Interest The Institutional Review Board of our institution approved this study under protocol no. 1999P008705.
None declared.
References
- 1.Essex-Lopresti P. Fractures of the radial head with distal radio-ulnar dislocation; report of two case. J Bone Joint Surg Br. 1951;33B(02):244–247. [PubMed] [Google Scholar]
- 2.Dodds S D, Yeh P C, Slade JF I I. Essex-Lopresti injurie. Hand Clin. 2008;24(01):125–137. doi: 10.1016/j.hcl.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Venouziou A I, Papatheodorou L K, Weiser R W, Sotereanos D G. Chronic Essex-Lopresti injuries: an alternative treatment metho. J Shoulder Elbow Surg. 2014;23(06):861–866. doi: 10.1016/j.jse.2014.01.043. [DOI] [PubMed] [Google Scholar]
- 4.Edwards G S, Jr, Jupiter J B. Radial head fractures with acute distal radioulnar dislocation. Essex-Lopresti revisite. Clin Orthop Relat Res. 1988;(234):61–69. [PubMed] [Google Scholar]
- 5.Grassmann J P, Hakimi M, Gehrmann S V et al. The treatment of the acute Essex-Lopresti injur. Bone Joint J. 2014;96-B(10):1385–1391. doi: 10.1302/0301-620X.96B10.33334. [DOI] [PubMed] [Google Scholar]
- 6.Heijink A, Morrey B F, van Riet R P, O’Driscoll S W, Cooney W P., III Delayed treatment of elbow pain and dysfunction following Essex-Lopresti injury with metallic radial head replacement: a case serie. J Shoulder Elbow Surg. 2010;19(06):929–936. doi: 10.1016/j.jse.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Jungbluth P, Frangen T M, Arens S, Muhr G, Kälicke T. The undiagnosed Essex-Lopresti injur. J Bone Joint Surg Br. 2006;88(12):1629–1633. doi: 10.1302/0301-620X.88B12.17780. [DOI] [PubMed] [Google Scholar]
- 8.Marcotte A L, Osterman A L. Longitudinal radioulnar dissociation: identification and treatment of acute and chronic injurie. Hand Clin. 2007;23(02):195–208. doi: 10.1016/j.hcl.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Matson A P, Ruch D S. Management of the Essex-Lopresti injur. J Wrist Surg. 2016;5(03):172–178. doi: 10.1055/s-0036-1584544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schnetzke M, Porschke F, Hoppe K, Studier-Fischer S, Gruetzner PA, Guehring T. Outcome of early and late diagnosed Essex-Lopresti injur. J Bone Joint Surg Am. 2017;99(12):1043–1050. doi: 10.2106/JBJS.16.01203. [DOI] [PubMed] [Google Scholar]
- 11.Trousdale R T, Amadio P C, Cooney W P, Morrey B F. Radio-ulnar dissociation. A review of twenty case. J Bone Joint Surg Am. 1992;74(10):1486–1497. [PubMed] [Google Scholar]
- 12.Geel C W, Palmer A K. Radial head fractures and their effect on the distal radioulnar joint. A rationale for treatmen. Clin Orthop Relat Res. 1992;(275):79–84. [PubMed] [Google Scholar]
- 13.Hotchkiss R N. Injuries to the interosseous ligament of the forear. Hand Clin. 1994;10(03):391–398. [PubMed] [Google Scholar]
- 14.Rabinowitz R S, Light T R, Havey R M et al. The role of the interosseous membrane and triangular fibrocartilage complex in forearm stabilit. J Hand Surg Am. 1994;19(03):385–393. doi: 10.1016/0363-5023(94)90050-7. [DOI] [PubMed] [Google Scholar]
- 15.Bot A GJ, Menendez M E, Neuhaus V, Mudgal C S, Ring D. The comparison of paper- and web-based questionnaires in patients with hand and upper extremity illnes. Hand (N Y) 2013;8(02):210–214. doi: 10.1007/s11552-013-9511-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bot A G, Becker S JE, Mol M F, Ring D, Vranceanu A M. Validation of phone administration of short-form disability and psychology questionnaire. J Hand Surg Am. 2013;38(07):1383–1387. doi: 10.1016/j.jhsa.2013.03.033. [DOI] [PubMed] [Google Scholar]
- 17.Tyser A R, Beckmann J, Franklin J D et al. Evaluation of the PROMIS physical function computer adaptive test in the upper extremit. J Hand Surg Am. 2014;39(10):2047–2051. doi: 10.1016/j.jhsa.2014.06.130. [DOI] [PubMed] [Google Scholar]
- 18.Hutchinson S, Faber K J, Gan B S. The Essex-Lopresti injury: more than just a pain in the wris. Can J Plast Surg. 2006;14(04):215–218. doi: 10.1177/229255030601400410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adams J E. Forearm instability: anatomy, biomechanics, and treatment option. J Hand Surg Am. 2017;42(01):47–52. doi: 10.1016/j.jhsa.2016.10.017. [DOI] [PubMed] [Google Scholar]
- 20.Loeffler B J, Green J B, Zelouf D S. Forearm instabilit. J Hand Surg Am. 2014;39(01):156–167. doi: 10.1016/j.jhsa.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Adams J E, Culp R W, Osterman A L. Interosseous membrane reconstruction for the Essex-Lopresti injur. J Hand Surg Am. 2010;35(01):129–136. doi: 10.1016/j.jhsa.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 22.Pfaeffle H J, Fischer K J, Manson T T, Tomaino M M, Woo S L, Herndon J H. Role of the forearm interosseous ligament: is it more than just longitudinal load transfer. J Hand Surg Am. 2000;25(04):683–688. doi: 10.1053/jhsu.2000.9416. [DOI] [PubMed] [Google Scholar]
- 23.Gaspar M P, Kane P M, Pflug E M, Jacoby S M, Osterman A L, Culp R W. Interosseous membrane reconstruction with a suture-button construct for treatment of chronic forearm instabilit. J Shoulder Elbow Surg. 2016;25(09):1491–1500. doi: 10.1016/j.jse.2016.04.018. [DOI] [PubMed] [Google Scholar]
- 24.Gaspar M P, Adams J E, Zohn R C et al. Late reconstruction of the interosseous membrane with bone-patellar tendon-bone graft for chronic Essex-Lopresti injuries: outcomes with a mean follow-up of over 10 year. J Bone Joint Surg Am. 2018;100(05):416–427. doi: 10.2106/JBJS.17.00820. [DOI] [PubMed] [Google Scholar]
- 25.Geel C W, Palmer A K, Ruedi T, Leutenegger A F. Internal fixation of proximal radial head fracture. J Orthop Trauma. 1990;4(03):270–274. doi: 10.1097/00005131-199004030-00006. [DOI] [PubMed] [Google Scholar]
- 26.Ring D, Quintero J, Jupiter J B. Open reduction and internal fixation of fractures of the radial hea. J Bone Joint Surg Am. 2002;84(10):1811–1815. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Moro J K, Werier J, MacDermid J C, Patterson S D, King G J. Arthroplasty with a metal radial head for unreconstructible fractures of the radial hea. J Bone Joint Surg Am. 2001;83(08):1201–1211. doi: 10.2106/00004623-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Jungbluth P, Frangen T M, Muhr G, Kälicke T. A primarily overlooked and incorrectly treated Essex-Lopresti injury: what can this lead to. Arch Orthop Trauma Surg. 2008;128(01):89–95. doi: 10.1007/s00402-007-0431-7. [DOI] [PubMed] [Google Scholar]
- 29.Hii J W, Page M M, Prosser A.Bauer SAn uncommon Essex-Lopresti fracture dislocation with radial displacement in distal direction: diagnosis and surgical treatment of a rare cas BMJ Case Rep 201320132013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pet M A, Morrison S D, Mack J S et al. Comparison of patient-reported outcomes after traumatic upper extremity amputation: replantation versus prosthetic rehabilitatio. Injury. 2016;47(12):2783–2788. doi: 10.1016/j.injury.2016.10.004. [DOI] [PubMed] [Google Scholar]