Abstract
Background:
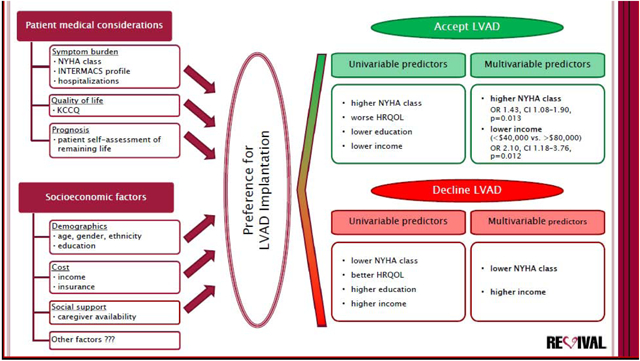
Worsening heart failure (HF) and health-related quality of life (HRQOL) have been shown to impact the decision to proceed with left ventricular assist device (LVAD) implantation, but little is known about how socioeconomic factors influence expressed patient preference for LVAD.
Methods and Results:
Ambulatory patients with advanced systolic HF (n=353) reviewed written information about LVAD therapy and completed a brief survey to indicate whether they would want an LVAD to treat their current level of HF. Ordinal logistic regression analyses identified clinical and demographic predictors of LVAD preference. Higher NYHA class, worse HRQOL measured by Kansas City Cardiomyopathy Questionnaire (KCCQ), lower education level, and lower income were significant univariable predictors of patients wanting an LVAD. In the multivariable model, higher NYHA class (OR 1.43, CI 1.08 – 1.90, p=0.013) and lower income level (OR 2.10, CI 1.18 – 3.76, p=0.012 for <$40,000 vs. >$80,000) remained significantly associated with wanting an LVAD.
Conclusion:
Among ambulatory patients with advanced systolic HF, treatment preference for LVAD was influenced by level of income independent of HF severity. Understanding the impact of socioeconomic factors on willingness to consider LVAD therapy may help tailor counseling towards individual needs.
Keywords: ventricular assist device, socioeconomic status, decision making, heart failure
Graphical Abstract
Introduction
Heart failure (HF) is a leading cause of increased cardiovascular morbidity and mortality. Poor health-related quality of life (HRQOL) and high rates of hospitalization impose significant burdens on both patients and society.1 Left ventricular assist devices (LVADs) improve survival, functional capacity and HRQOL in patients with end-stage systolic HF.2,3
However, this technologically advanced and costly therapy is associated with a high incidence of complications, and substantially impacts the lifestyle of patients and their caregivers.4 The decision to implant an LVAD is complex and shared by the medical team, patients and caregivers.5 The medical team is equipped with medical knowledge and various tools and guidelines to allow comprehensive assessment of patient candidacy for an LVAD.6–8 Limited data exist to understand how patients make decisions to proceed with or decline device implantation.9–12 Worsened severity of disease as measured by increased symptom burden, poor HRQOL and reduced self-assessed prognosis have all been associated with patient willingness to receive an LVAD.13,14 Socioeconomic status (SES) is broadly defined as characteristic arising from a combination of sociological and economic influences on an individual’s position in the society, and takes into account various factors such as income, education, cultural background, occupation, as well as home environment. SES has been shown to be an important predictor of outcomes in patients with advanced HF.15 The reasons for the disparities are complex and uncertain. One potential explanation is that disease independent factors such as health literacy, cognitive biases, emotions, cultural and religious influences, and family dynamics may impact decision making.5,12
We therefore examined the association of socioeconomic factors with expressed patient preference for LVAD therapy in a large, multicenter cohort of LVAD eligible subjects.
Methods
Study Design.
We performed a cross-sectional study of ambulatory patients with advanced HF from the REVIVAL (Registry Evaluation of Vital Information for VADs in Ambulatory Life) study at the time of their baseline visit. Patients were enrolled from 21 centers between July 2015 and June 2016. Subjects enrolled were aged 18 to 80 years with New York Heart Association (NYHA) functional class II - IV limitation for at least 45 of the last 60 days, left ventricular ejection fraction ≤35%, and a HF diagnosis >12 months. All patients were under the care of a cardiologist at the study site and receiving appropriate guideline-directed medical and electrical HF therapies for ≥ 3 months prior to enrollment or had a documented contraindication. Enrollment required subjects to have either one high-risk feature (low peak oxygen uptake, reduced 6-minute walk distance, elevated natriuretic peptide level, low serum sodium concentration, decreased Seattle Heart Failure Model [SHFM] one-year predicted survival, or active UNOS status 2 for heart transplantation), one unplanned HF hospitalization in the prior 12 months with a lesser threshold for natriuretic peptide level, or two unplanned HF hospitalizations in the prior 12 months. Supplementary Tables 1 and 2 detail the inclusion and exclusion criteria. An independent Observational Study Monitoring Board oversaw the conduct of the REVIVAL study. The Institutional Review Board at each center approved the study. All subjects provided written informed consent prior to study participation.16
Determination of Preference for LVAD Therapy.
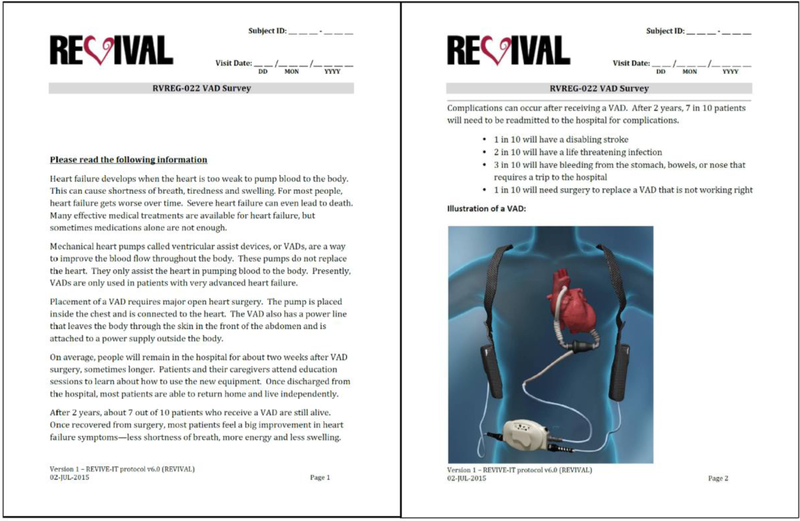
The primary outcome for the present analysis was willingness to accept LVAD therapy. Patients were asked to read a 2-page document containing a basic description and illustration of an LVAD, along with information about indications, benefits and complications of LVAD therapy (Figure 1). The description of LVAD therapy was written at a US 8th grade education level (Flesch-Kincaid readability ease). The probabilities of survival, recurrent hospitalization and adverse events following LVAD included in the instrument were based on event rates of approved devices at the time of survey development in 2015. Subjects were then asked to reply on a Likert-type scale to the question: “Based on how you feel right now, how would you feel about having a VAD placed to treat your heart failure?” Subjects were classified into 3 groups based on their responses: 1 - wanting LVAD (including “definitely want” and “probably want”), 2 – unsure, and 3 – not wanting LVAD (including “probably not want” and “definitely not want”).
Figure 1. Information Materials for VAD Survey.
Patients were presented with a 2-page document containing a basic description and illustration of an LVAD, and information about indications, benefits and complications of LVAD therapy (based on event rates of approved devices at the time of survey development in 2015).
Predictors of Interest.
This study was designed to evaluate whether SES influenced expressed patient preference for LVAD implantation. SES was characterized by the level of education (≤ 12th grade of high school, attended college/technical school, associate/bachelor’s degree, or post-college graduate degree), annual household income (< $40,000, $40,000–80,000, or > $80,000, in U.S. dollars), type of health insurance (Medicare/Medicaid/Tricare [1], private/commercial/Workers Compensation/other [2], or both [1] and [2]), and immediate availability of social support (marital status) in the household (social support available if married/have a domestic partner, or not available if single/divorced/separated/widowed).
Demographic and clinical characteristics evaluated as potential predictors or confounders included gender, age, race, NYHA class, Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) patient profile, and the number of HF-related hospitalizations within the past 12 months. Participants were specifically asked to estimate how much longer they would live if LVAD or cardiac transplantation were not possible (i.e., patient self-assessment of remaining life). Additionally, the patients were asked to complete the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated instrument for measuring heart failure related quality of life.17
Statistical Analysis.
Demographic and clinical variables were summarized with standard descriptive statistics and presented as mean (with standard deviation, SD) for continuous data, or counts (with percentages, %) for categorical data. Demographic and clinical data were compared among LVAD preference groups by chi-square or Kruskal-Wallis. Univariable and multivariable ordinal logistic regression analyses were performed to assess the impact of SES, clinical and demographic characteristics on preference for LVAD therapy. We used NYHA class, INTERMACS profile and the number of HF hospitalizations as surrogate measures for severity of HF, KCCQ overall summary score as a measure of HRQOL, and patient self-assessment of remaining life as a measure of self-assessed prognosis. Proportional odds ratios (OR) and 95% confidence intervals (CI) were calculated. Variables with p < 0.10 on univariable analysis were included in the backward stepwise multivariable selection model. A p-value of < 0.05 was considered statistically significant in the final multivariable model. No adjustment was done for multiple testing; therefore p-values should be interpreted with caution.
Given the extent of missing data (36%) in two key SES predictors (income and education), we used multiple imputation to create and analyze 36 multiply imputed datasets.18 Summary statistics and inference was based on the pooling method of Rubin that appropriately incorporates additional uncertainty owing to the imputation process.19 As a sensitivity analysis, we also repeated the analyses described above on the subset of complete cases (details provided in Supplementary Appendix). To explore the potential bias and pattern of missingness for education and income data, demographic, other clinical data, and the preference for LVAD were compared between the group with and without available education or income data using t-test or Wilcoxon rank sum test for continuous and ordinal variables, and Fisher exact test or χ2-test for categorical variables. Spearman correlation coefficient was also calculated to determine the degree of correlation between education and income levels. Analyses were performed using SAS software version 9.4.
Results
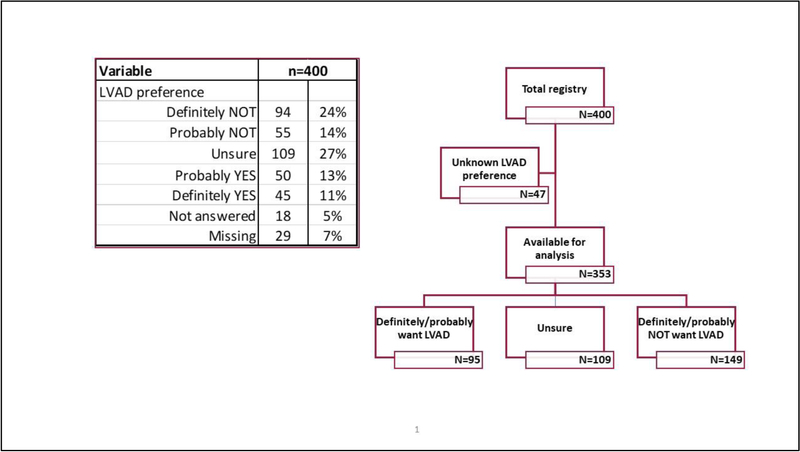
The REVIVAL Registry enrolled 400 subjects, of whom 353 provided their preference for whether to accept or not to accept an LVAD to treat their current level of HF; these subjects were included in the analysis (Figure 2). In this cohort, 263 participants were men (74.5%), 83 were black (23.5%), and the mean age was 60.3 ± 11.2 years. Ischemic etiology of cardiomyopathy was present in 153 subjects (43.3%). Only 53 subjects (15%) had previously undergone LVAD evaluation (8 were approved but not implanted, 34 were deferred due to being too well, and 11 patients were not eligible due to age, medical or psychosocial reasons). Detailed characterization of the cohort is provided in Table 1 and Supplementary Table 3.
Figure 2. Flow Chart of the REVIVAL Participants by LVAD Preference.
After reading information materials about LVAD therapy, patients completed a survey to indicate their preference by answering a question: “Based on how you feel right now, how would you feel about having a VAD placed to treat your heart failure?”
Table 1.
Clinical Characteristics.
| Variable | Total, N (%) | Patient Preference for LVAD, n (%) | p-value | ||
|---|---|---|---|---|---|
| N=353 | Want N=95 | Unsure N=109 | Don’t Want N=149 | ||
| Male | 263 (74.5%) | 68 (71.6%) | 83 (76.1%) | 112 (75.2%) | 0.73 |
| Age, years, mean (SD) | 60.3 (11.2) | 60.3 (9.9) | 61.4 (10.5) | 59.5 (12.4) | 0.67 |
| Black | 83 (23.5%) | 22 (23.2%) | 26 (23.9%) | 35 (23.5%) | 0.99 |
| Hispanic or Latino (n=346) | 24 (6.8%) | 7 (7.4%) | 5 (4.6%) | 12 (8.1%) | 0.69 |
| NYHA class | 0.006 | ||||
| I | 6 (1.7%) | 1 (1.1%) | 1 (0.9%) | 4 (2.7%) | |
| II | 96 (27.2%) | 20 (21.1%) | 32 (29.4%) | 44 (29.5%) | |
| III | 212 (60.1%) | 57 (60.0%) | 66 (60.6%) | 89 (59.7%) | |
| IIIb | 30 (8.5%) | 12 (12.6%) | 7 (6.4%) | 11 (7.4%) | |
| IV | 9 (2.5%) | 5 (5.3%) | 3 (2.8%) | 1 (0.7%) | |
| INTERMACS profile | 0.06 | ||||
| 4 | 31 (8.8%) | 11 (11.6%) | 10 (9.2%) | 10 (6.7%) | |
| 5 | 72 (20.4%) | 19 (20.0%) | 27 (24.8%) | 26 (17.4%) | |
| 6 | 136 (38.5%) | 41 (43.2%) | 35 (32.1%) | 60 (40.3%) | |
| 7 | 114 (32.3%) | 24 (25.3%) | 37 (33.9%) | 53 (35.6%) | |
| HF hospitalizations within the last year, mean (SD) | 1.04 (1.4) | 1.25 (1.6) | 0.79 (1.1) | 1.09 (1.4) | 0.055 |
| KCCQ, mean (SD)* | 62.6 (20.5) | 59.9 (22.4) | 61.3 (19.3) | 65.4 (19.9) | 0.12 |
| Patient Self-Assessment of Remaining Life, years (n=290), mean (SD) | 10.3 (9.6) | 9.2 (7.8) | 10.0 (9.6) | 11.2 (10.4) | 0.4 |
Data presented as mean (SD), or counts and percentages.
The observed range for KCCQ was 13–100 (potential range 0–100).
HF, heart failure; INTERMACS, Interagency Registry for Mechanically Assisted Circulatory Support; KCCQ, Kansas City Cardiomyopathy Questionnaire Overall Summary Score; NYHA, New York Heart Association.
Overall, 27% (95/353) of survey responders definitely or probably wanted an LVAD to treat their current level of HF, 31% (109/353) were unsure, and 42% (149/353) definitely or probably did not want an LVAD (Figure 2).
The SES profile of REVIVAL participants was quite diverse (Table 2). Nearly one-third of participants had ≤ 12th grade of high school education, while roughly 30% had attained a college or postgraduate degree. Over one-third of patients had an annual household income < $40,000 (for context, the median household income in U.S. in 2016 was $57,617).20 Government sponsored health insurance plans (Medicare/Medicaid/Tricare) and private health insurance plans (commercial/Workers Compensation/other) were equally represented. Two-thirds were married or had a domestic partner.
Table 2.
Socioeconomic Characteristics.
| Variable | Total, n (%) | Patient Preference for LVAD, n (%) | p-value | ||
|---|---|---|---|---|---|
| N=353 | Want N=95 | Unsure N=109 | Don’t Want N=149 | ||
| Education (n=296) | 0.02 | ||||
| <=12th grade | 104 (29.5) | 34 (35.8) | 40 (36.7) | 30 (20.1) | |
| Attended college/tech school | 91 (25.8) | 22 (23.2) | 29 (26.6) | 40 (26.8) | |
| Associate/bachelor’s degree | 71 (20.1) | 19 (20.0) | 16 (14.7) | 36 (24.2) | |
| Post-college graduate degree | 30 (8.5) | 7 (7.4) | 7 (6.4) | 16 (10.7) | |
| Missing data | 57 (16.1) | 13 (13.7) | 17 (15.6) | 27 (18.1) | |
| Annual income, U.S.$ (n=234) | 0.023 | ||||
| <40,000 | 126 (35.7) | 39 (41.1) | 44 (40.4) | 43 (28.9) | |
| 40,000 – 80,000 | 61 (17.3) | 19 (20.0) | 19 (17.4) | 23 (15.4) | |
| >80,000 | 47 (13.3) | 10 (10.5) | 9 (8.3) | 28 (18.8) | |
| Missing data | 119 (33.7) | 27 (28.4) | 37 (33.9) | 55 (36.9) | |
| Insurance (n=349) | 0.65 | ||||
| (1)Medicare/Medicaid/Tricare | 148 (41.9) | 42 (44.2) | 47 (43.1) | 59 (39.6) | |
| (2)Private/Commercial/WC/other | 143 (40.5) | 36 (37.9) | 40 (36.7) | 67 (45.0) | |
| Both from (1) and (2) | 58 (16.4) | 17 (17.9) | 20 (18.3) | 21 (14.1) | |
| Missing data | 4 (1.1) | 0 (0.0) | 2 (1.8) | 2 (1.3) | |
| Social support (n=349) | 0.09 | ||||
| Married/domestic partner | 224 (63.5) | 54 (56.8) | 78 (71.6) | 92 (61.7) | |
| Single/divorced/separated/widowed | 125 (35.4) | 41 (43.2) | 31 (28.4) | 53 (35.6) | |
| Missing data | 4 (1.1) | 0 (0.0) | 0 (0.0) | 4 (2.7) | |
Data presented as counts and percentages.
WC, Workers Compensation.
The extent of missingness was driven by two SES predictors: 16% of education values and 34% of income values were missing. A secondary sensitivity analysis was performed on 227 participants (64% of the 353 total participants) who had complete data sets for both education and income. There was significant correlation between these two variables: r = 0.33 (Supplementary Table 4). When comparing baseline demographic characteristics and LVAD treatment preferences, those with missing education levels were more likely to be black and have private insurance. There were no other statistically or clinically significant differences (Supplementary Tables 5 and 6). However, given the differences related to education data missingness, the more rigorous approach to missingness embodied in the multiple imputation methodology was warranted (Supplementary Methods and Supplementary Table 7).
Univariable Predictors of Wanting an LVAD.
In the univariable model, higher NYHA class, worse HRQOL and low tier income were significant predictors of wanting LVAD compared to unsure or not wanting LVAD groups (Table 3). Every unit increase in NYHA class was associated with 1.47 times higher odds of wanting an LVAD (CI 1.11 – 1.94, p = 0.007). Higher KCCQ overall summary score (indicating better HRQOL) predicted lower likelihood of patients willing to accept an LVAD (OR 0.99 per point, CI 0.98 – 0.999, p = 0.026). The patients in the low income (< $40,000 per year) group were twice as likely to consider an LVAD compared to the higher income (> $80,000) population (OR 2.20, CI 1.24 – 3.91, p = 0.01). The patients’ education level was not a significant predictor of wanting LVAD (p = 0.067) but this effect was entered in the multivariable selection model. Gender, age, race, INTERMACS profile, number of hospitalizations for HF in the preceding year, self-assessed prognosis for remaining life, type of health insurance, and availability of social support were not associated with patient willingness to accept LVAD (all p>0.10).
Table 3.
Univariable Predictors of Patient Preference for LVAD: Multiple Imputation and Complete-Case Models.
| Predictors | Multiple Imputation | Complete-Case | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p-value | Odds Ratio (95% CI) | p-value | |
| NYHA class | 1.47 (1.11 – 1.94) | 0.007 | 1.47 (1.11 – 1.94) | 0.007 |
| KCCQ | 0.99 (0.98 – 0.999) | 0.026 | 0.99 (0.98 – 0.999) | 0.026 |
| Education | 0.067 | 0.047 | ||
| <=12th grade vs PostGrad | 2.16 (1.01 – 4.63) | 0.048 | 2.23 (1.04 – 4.81) | 0.04 |
| Attended college/tech school vs PostGrad | 1.39 (0.64 – 3.02) | 0.41 | 1.32 (0.61 – 2.88) | 0.49 |
| Associate/bachelor’s degree vs PostGrad | 1.16 (0.52 – 2.56) | 0.72 | 1.15 (0.52 – 2.59) | 0.73 |
| <=12th grade vs Associate/bachelor’s degree | 1.87 (1.07 – 3.26) | 0.028 | 1.94 (1.10 – 3.40) | 0.021 |
| Attended college/tech school vs Associate/bachelor’s degree | 1.20 (0.67 – 2.16) | 0.54 | 1.14 (0.64 – 2.04) | 0.65 |
| <=12th grade vs Attended college/tech school | 1.55 (0.94 – 2.56) | 0.088 | 1.69 (1.004 – 2.85) | 0.048 |
| Income, U.S. $ | 0.027 | 0.025 | ||
| <40,000 vs >80,000 | 2.20 (1.24 – 3.91) | 0.01 | 2.42 (1.27 – 4.61) | 0.01 |
| 40,000 – 80,000 vs. >80,000 | 1.79 (0.91 – 3.43) | 0.09 | 2.23 (1.08 – 4.62) | 0.03 |
| <40,000 vs 40,000 – 80,000 | 1.23 (0.74 – 2.05) | 0.43 | 0.93 (0.53 – 1.62) | 0.79 |
| Sex | 0.59 | 0.59 | ||
| Age at baseline, years | 0.44 | 0.44 | ||
| Race | 0.28 | 0.28 | ||
| HF hospitalizations within the last year | 0.65 | 0.65 | ||
| INTERMACS profile | 0.313 | 0.313 | ||
| Ethnicity | 0.66 | 0.64 | ||
| Marital status | 0.46 | 0.49 | ||
| Insurance groups | 0.40 | 0.38 | ||
| BMI (at baseline) | 0.13 | 0.13 | ||
| Patient Self-Assessment of Remaining Life, years | 0.26 | 0.16 | ||
KCCQ, Kansas City Cardiomyopathy Questionnaire Overall Summary Score; LVAD, left ventricular assist device; NYHA, New York Heart Association; PostGrad, post-college graduate degree.
Multivariable Predictors of Wanting an LVAD.
The stepwise selection of the initial model began with SES characteristics education and income, in addition to NYHA and KCCQ. In the final model, only higher NYHA class and low income remained significant independent predictors of wanting LVAD compared to unsure or not wanting LVAD groups (Table 4). Every unit increase in NYHA class was associated with 1.43 times higher odds of wanting an LVAD (CI 1.08 – 1.90, p = 0.013). Low income patients were twice as likely to want an LVAD compared to those with income > $80,000 per year (OR 2.10, CI 1.18 – 3.76, p = 0.012).
Table 4.
Multivariable Predictors of Patient Preference for LVAD: Multiple Imputation and Complete-Case Models.
| Predictors | Multiple Imputation | Complete-Case | ||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p-value | Odds Ratio (95% CI) | p-value | |
| NYHA class | 1.43 (1.08 – 1.90) | 0.013 | 1.58 (1.14 – 2.19) | 0.006 |
| Education | 0.04 | |||
| <=12th grade vs PostGrad | 2.17 (1.004 – 4.69) | 0.049 | ||
| Attended college/tech school vs PostGrad | 1.19 (0.54 – 2.60) | 0.67 | ||
| Associate/bachelor’s degree vs PostGrad | 1.12 (0.50 – 2.52) | 0.78 | ||
| Attended college/tech school vs Associate/bachelor’s degree | 1.06 (0.59 – 1.92) | 0.85 | ||
| <=12th grade vs Attended college/tech school | 1.83 (1.08 – 3.09) | 0.025 | ||
| <=12th grade vs Associate/bachelor’s degree | 1.93 (1.10 – 3.41) | 0.023 | ||
| Income, U.S. $ | 0.041 | |||
| <40,000 vs >80,000 | 2.10 (1.18 – 3.76) | 0.012 | ||
| 40,000 – 80,000 vs. >80,000 | 1.73 (0.88 – 3.41) | 0.11 | ||
| <40,000 vs. 40,000 – 80,000 | 1.21 (0.72 – 2.04) | 0.47 | ||
See abbreviations in Table 3.
Complete-Case Analysis.
Univariable analysis of the complete-case subjects indicated that NYHA (OR 1.47, CI 1.11 – 1.94, p = 0.01), KCCQ (OR 0.99, CI 0.98 – 0.999, p = 0.03), education (p = 0.047) and income (p = 0.03) were significant predictors of LVAD preference (Table 3). Specifically, participants with 12th grade education or less were more likely to want LVAD compared to those with a postgraduate degree (OR 2.23, CI 1.04 – 4.81; p = 0.04), associate/bachelor’s degree (OR 1.94, CI 1.10 – 3.40; p = 0.021), or those who attended college/technical school (OR 1.69, CI 1.004 – 2.85; p = 0.048). Likewise, participants with lower income were more likely to express a willingness to consider LVAD (<$40,000 vs >$80,000, OR 2.42, CI 1.27 – 4.61; p = 0.01). However, only NYHA and education level remained significant independent predictors in the final multivariable model in the complete-case analysis (Table 4).
Discussion
REVIVAL is the largest multicenter registry of ambulatory patients with advanced systolic HF to provide insight into how symptom burden, HRQOL and socioeconomic factors impact patient desire for LVAD therapy. The patients in the registry were not inotrope dependent but had high-risk features for increased mortality and hospitalization. Overall, 27% of responders indicated that they would definitely or probably want an LVAD to treat their current level of HF. We found that SES impacted ambulatory patient preference for LVAD independent of symptom burden and HRQOL. In univariable analysis, we found greater preference for LVAD among the patients with high school education or less, and those with annual income < $40,000, whereas patients with higher education levels and higher income were more reluctant to accept an LVAD. In the multivariable model (using the multiply imputed datasets), only higher NYHA functional class and lower income level remained significantly associated with increased willingness to accept an LVAD. In a sensitivity analysis using only the complete cases, higher NYHA functional class and lower education level were multivariable predictors of greater willingness to accept an LVAD.
A potential reason for SES influencing inclination for elective device therapy to treat ambulatory HF may lie in how patients arrive at their decisions. A study of semi-structured, in-depth interviews of 22 patients who were offered or had received destination LVAD showed that people use mainly either automatic or reflective type of decision making when considering LVAD options.9 Automatic decision process was primarily focused on intuitive choice between dying or surviving, largely driven by fear of death, when patients perceived that they had “no choice”. All patients exercising automatic approach had less than 4-year college education and accepted the device. Reflective decision makers examined how they valued quality against quantity of life and were able to see death as an alternative to other possible outcomes. The patients in this group tended to be more educated, and 7 out of 10 patients declined the LVAD. Among those who accepted LVAD therapy, 87% had less than a 4-year college education, while 43% of those who declined LVAD achieved at least a college degree.12 Nonetheless, factors that lead to willingness to accept LVAD therapy while still ambulatory are manifold and go beyond the level of education. In a study of 21 patients who declined LVAD therapy, half of the patients did so based on limited knowledge (10/21 subjects made their choice before receiving adequate information about the LVAD therapy), misconceptions about how the device would affect their mobility (13/21 thought they would be tied to energy source unable to leave the room) or underestimating severity of their illness (10/21 patients, mean INTERMACS profile 3.5 in the study cohort).11 The authors found that refusal of LVAD therapy could change with iterative counseling, and half of those who initially declined LVAD therapy ultimately opted for the device as the disease progressed.11 Irrespective of how patients arrived at their decisions to accept an LVAD, regret scores after device implantation were low.10
Low SES is a known risk for increased HF prevalence, mortality and morbidity.15 However, overall mortality of low income patients after LVAD implantation was comparable to that of patients in higher economic strata, although risk of readmissions was higher and time to first event (death or readmission) was shorter in the disadvantaged group.21 Likewise, an analysis of the UNOS database (3361 patients) revealed that SES was not associated with death while on a bridging device, removal from the transplant waitlist or complications requiring UNOS status upgrade. However, post-transplant mortality was higher in the lowest quartile for SES compared to other quartiles.22 This phenomenon supports optimism for favorable outcomes in LVAD recipients despite disadvantaged SES, yet emphasizes the need for enhanced counseling and intensive longitudinal follow-up after device implantation.
Improved understanding of the impact of socioeconomic factors on patient preference for LVAD may further the development of techniques to address gaps in knowledge and minimize misconceptions about LVAD therapy, and thus help patients make more informed LVAD treatment decisions in alignment with their care preferences. In 2012, the American Heart Association issued a Scientific Statement highlighting the importance of shared decision making in advanced HF and outlined a roadmap to guide conversations about the goals of care and patient-specific treatment preferences.5 Differences in literacy may necessitate that communication strategies are tailored to appropriate income and/or education levels to accommodate patients’ needs and facilitate transfer of information. Investigators have proposed various decision aid tools that were tested in two randomized clinical trials and helped improve patient knowledge about the device therapy, but had no significant effect on the rates of device acceptance.23,24 The impact of socioeconomic factors on patients’ desire for LVAD therapy at centers that utilize either of these two decision aids remains to be determined.
These results should be interpreted in light of several limitations. Not all patients in the REVIVAL Registry completed the LVAD survey to indicate their preference for the device. We compared demographic variables, indices of HF severity, HRQOL and SES characteristics between those who completed the LVAD survey (n=353) and those who did not complete the survey (n=47) and found no difference in any of the characteristics between the survey completers and non-completers (data not shown). Our study population was generally reflective of non-inotrope dependent ambulatory patients with systolic HF, but women were underrepresented. Complete data on all study participants were not available, particularly for education level (missing in 16% of study participants) and income (missing in 34%), with only 64% of study subjects having both education and income data, which could certainly result in bias. Thus, our primary analytic approach used a multiple imputation approach which is valid under a missing at random assumption. No significant difference was seen between those with and without income data, and modest differences in race and health insurance status were noted for those with and without data for education level. Differences between the multiple imputation and complete-case approaches with respect to which SES factor is associated with LVAD preference may reflect assumptions about why data are missing. Given the degree of correlation between income and education, we believe that the results support our conclusion that SES influences LVAD treatment preference. This conclusion applies to patients similar to those studied in REVIVAL (i.e., ambulatory patients on oral HF therapies) and may not apply to those with a greater burden of HF, such as patients dependent on intravenous inotropes or receiving temporary mechanical circulatory support. Although the survey instrument has not been independently validated, it has been used in two previous studies, was designed at an 8th grade reading level and has been shown to be responsive to HF burden.13,25 We recognize that a given patient may respond differently to alternative modes of information delivery (i.e. written, verbal, audio, video), which in turn may be impacted by socioeconomic status.26 We could not adjust for baseline knowledge about LVADs. For example, 53 patients (15%) had previously undergone LVAD evaluation and likely had greater understanding about the device therapy compared to the rest of the cohort. We did not explore the specific reasons why patients would or would not be inclined to have an LVAD.
Conclusions
In a population of ambulatory non-inotrope dependent patients with symptomatic chronic systolic HF, patient willingness to consider LVAD therapy was influenced by socioeconomic factors independent of HF severity. Understanding the impact of socioeconomic factors on patient desire for LVAD therapy may help tailor counseling towards individual needs.
Supplementary Material
Highlights.
Only 27% of patients with advanced systolic heart failure would want LVAD therapy.
42% of patients would decline the device, 31% were unsure about their preferences.
Socioeconomic factors impact patient preference for LVAD independent of NYHA class.
Lower income and perhaps lower education level predict greater acceptance of LVAD.
Sources of Funding
The Registry and this study were supported by funding from the National Institutes of Health, National Heart, Lung, and Blood Institute (NHLBI Contract Number:HHSN268201100026C) and the National Center for Advancing Translational Sciences (NCATS Grant Number: UL1TR002240). The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
Abbreviations List
- BNP
B-type natriuretic peptide
- CRT-D
cardiac resynchronization therapy defibrillator
- HF
heart failure
- HRQOL
health-related quality of life
- ICD
implantable cardioverter defibrillator
- INTERMACS
Interagency Registry for Mechanically Assisted Circulatory Support
- KCCQ
Kansas City Cardiomyopathy Questionnaire
- LV
left ventricle
- LVAD
left ventricular assist device
- MedaMACS
Medical Arm of Mechanically Assisted Circulatory Support
- NT-proBNP
N-terminal pro B-type natriuretic peptide
- NYHA
New York Heart Association
- RER
respiratory exchange ratio
- REVIVAL
Registry Evaluation of Vital Information for VADs in Ambulatory Life
- SD
standard deviation
- SES
socioeconomic status
- UNOS
United Network for Organ Sharing
- VE/VC02 slope
minute ventilation / carbon dioxide production (ventilatory efficiency)
- VO2
oxygen consumption
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
K.B.S. serves as a consultant for Medtronic; J.D.E serves as a medical advisor for Medtronic and as a consultant for Abbott; U.P.J. is a consultant for Abbott; and K.D.A. receives consultant and research support from Medtronic, research support from Abbott, consultant support NuPulseCV and is an advisor to Procyrion. No company had any role in the funding of this study or writing of this article. The other authors report no conflicts.
References
- 1. WRITING COMMITTEE MEMBERS, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013. October 15;128(16):e240–327. [DOI] [PubMed] [Google Scholar]
- 2. Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001. November 15;345(20):1435–43. [DOI] [PubMed] [Google Scholar]
- 3. Park SJ, Milano CA, Tatooles AJ, Rogers JG, Adamson RM, Steidley DE, et al. Outcomes in advanced heart failure patients with left ventricular assist devices for destination therapy. Circ Heart Fail. 2012. March 1;5(2):241–8. [DOI] [PubMed] [Google Scholar]
- 4. Kirklin JK, Pagani FD, Kormos RL, Stevenson LW, Blume ED, Myers SL, et al. Eighth annual INTERMACS report: Special focus on framing the impact of adverse events. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2017. October;36(10):1080–6. [DOI] [PubMed] [Google Scholar]
- 5. Allen LA, Stevenson LW, Grady KL, Goldstein NE, Matlock DD, Arnold RM, et al. Decision making in advanced heart failure: a scientific statement from the American Heart Association. Circulation. 2012. April 17;125(15):1928–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Levy WC, Mozaffarian D, Linker DT, Farrar DJ, Miller LW, REMATCH Investigators. Can the Seattle heart failure model be used to risk-stratify heart failure patients for potential left ventricular assist device therapy? J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2009. March;28(3):231–6. [DOI] [PubMed] [Google Scholar]
- 7. Aaronson KD, Schwartz JS, Chen TM, Wong KL, Goin JE, Mancini DM. Development and prospective validation of a clinical index to predict survival in ambulatory patients referred for cardiac transplant evaluation. Circulation. 1997. June 17;95(12):2660–7. [DOI] [PubMed] [Google Scholar]
- 8. Feldman D, Pamboukian SV, Teuteberg JJ, Birks E, Lietz K, Moore SA, et al. The 2013 International Society for Heart and Lung Transplantation Guidelines for mechanical circulatory support: executive summary. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2013. February;32(2):157–87. [DOI] [PubMed] [Google Scholar]
- 9. McIlvennan CK, Allen LA, Nowels C, Brieke A, Cleveland JC, Matlock DD. Decision making for destination therapy left ventricular assist devices: “there was no choice” versus “I thought about it an awful lot”. Circ Cardiovasc Qual Outcomes. 2014. May;7(3):374–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Blumenthal-Barby JS, Kostick KM, Delgado ED, Volk RJ, Kaplan HM, Wilhelms LA, et al. Assessment of patients’ and caregivers’ informational and decisional needs for left ventricular assist device placement: Implications for informed consent and shared decision-making. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2015. September;34(9):1182–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bruce CR, Kostick KM, Delgado ED, Wilhelms LA, Volk RJ, Smith ML, et al. Reasons Why Eligible Candidates Decline Left Ventricular Assist Device Placement. J Card Fail. 2015. October;21(10):835–9. [DOI] [PubMed] [Google Scholar]
- 12. Magid M, McIlvennan CK, Jones J, Nowels CT, Allen LA, Thompson JS, et al. Exploring cognitive bias in destination therapy left ventricular assist device decision making: A retrospective qualitative framework analysis. Am Heart J. 2016;180:64–73. [DOI] [PubMed] [Google Scholar]
- 13. Stewart GC, Kittleson MM, Cowger JA, Johnson FL, Patel CB, Mountis MM, et al. Who wants a left ventricular assist device for ambulatory heart failure? Early insights from the MEDAMACS screening pilot. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2015. December;34(12):1630–3. [DOI] [PubMed] [Google Scholar]
- 14. Estep JD, Starling RC, Horstmanshof DA, Milano CA, Selzman CH, Shah KB, et al. Risk Assessment and Comparative Effectiveness of Left Ventricular Assist Device and Medical Management in Ambulatory Heart Failure Patients: Results From the ROADMAP Study. J Am Coll Cardiol. 2015. October 20;66(16):1747–61. [DOI] [PubMed] [Google Scholar]
- 15. Hawkins NM, Jhund PS, McMurray JJV, Capewell S. Heart failure and socioeconomic status: accumulating evidence of inequality. Eur J Heart Fail. 2012. February;14(2):138–46. [DOI] [PubMed] [Google Scholar]
- 16. REGISTRY EVALUATION OF VITAL INFORMATION FOR VADs IN AMBULATORY LIFE - Full Text View - ClinicalTrials.gov [Internet]. [cited 2018 Mar 10]. Available from: https://clinicaltrials.gov/ct2/show/NCT01369407
- 17. Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000. April;35(5):1245–55. [DOI] [PubMed] [Google Scholar]
- 18. White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–99. [DOI] [PubMed] [Google Scholar]
- 19. Rubin DB. Multiple Imputation After 18+ Years. J Am Stat Assoc Alex. 1996. June;91(434):473–89. [Google Scholar]
- 20. Household Income: 2016 [Internet]. [cited 2019 Jul 7]. Available from: https://www.census.gov/library/publications/2017/acs/acsbr16-02.html
- 21. Smith SA, Hasan AK, Binkley PF, Foraker RE. The impact of insurance and socioeconomic status on outcomes for patients with left ventricular assist devices. J Surg Res. 2014. October;191(2):302–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clerkin KJ, Garan AR, Wayda B, Givens RC, Yuzefpolskaya M, Nakagawa S, et al. Impact of Socioeconomic Status on Patients Supported With a Left Ventricular Assist Device: An Analysis of the UNOS Database (United Network for Organ Sharing). Circ Heart Fail. 2016. October;9(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Allen LA, McIlvennan CK, Thompson JS, Dunlay SM, LaRue SJ, Lewis EF, et al. Effectiveness of an Intervention Supporting Shared Decision Making for Destination Therapy Left Ventricular Assist Device: The DECIDE-LVAD Randomized Clinical Trial. JAMA Intern Med. 2018. April 1;178(4):520–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kostick KM, Bruce CR, Minard CG, Volk RJ, Civitello A, Krim SR, et al. A Multisite Randomized Controlled Trial of a Patient-Centered Ventricular Assist Device Decision Aid (VADDA Trial). J Card Fail. 2018. October 1;24(10):661–71. [DOI] [PubMed] [Google Scholar]
- 25. Ambardekar AV, Thibodeau JT, DeVore AD, Kittleson MM, Forde-McLean RC, Palardy M, et al. Discordant Perceptions of Prognosis and Treatment Options Between Physicians and Patients With Advanced Heart Failure. JACC Heart Fail. 2017. September 1;5(9):663–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McIlvennan CK, Thompson JS, Matlock DD, Cleveland JC, Dunlay SM, LaRue SJ, et al. A Multicenter Trial of a Shared Decision Support Intervention for Patients and Their Caregivers Offered Destination Therapy for Advanced Heart Failure: DECIDE-LVAD: Rationale, Design, and Pilot Data. J Cardiovasc Nurs. 2016. December;31(6):E8–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.