The coronavirus pandemic is mediated by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and has been responsible for more than 900,000 infections and 45,000 deaths worldwide as of April 1, 2020 [1, 2]. The molecular mechanisms leading to SARS-CoV‑2 infection were identified at an incredible pace: Similar to SARS-CoV‑1, the virus which led to the SARS epidemic during 2002–2004, SARS-CoV‑2 infects cells via binding to angiotensin-converting enzyme 2 (ACE2; [3]). Therefore, concerns were raised that higher expression of ACE2 in the respiratory tract may expedite the infection. However, ACE2 also plays beneficial roles in the renin–angiotensin–aldosterone system (RAAS) where it metabolizes angiotensin II (Ang-2), a vasoconstrictor, to angiotensin-(1–7) (Ang-(1–7)), a vasodilator with antihypertrophic properties. Thus, consumption of ACE2 by the virus may result in an overshooting activation of the RAAS. Importantly, inhibitors of angiotensin-converting enzyme inhibitors (ACEI) as well as AT1-receptor blockers (ARB) have been shown in experimental studies to upregulate ACE2 and ACE levels in various tissues [4, 5]. Both ACEI and ARB are widely used for the treatment of heart failure and hypertension, especially in patients with diabetes. The observation that patients suffering from these conditions are at increased risk of dying from SARS-CoV‑2 infection [S1] raised reasonable concerns about whether these drugs might increase the risk of both SARS-CoV‑2 infection and an unfavorable course of the disease. However, several important issues regarding the involvement of ACE2 in the disease and the interaction of its expression and activity with the administration of RAAS-modulating drugs are not fully understood yet:
1. The role of ACE2 in lung injury.
It is accepted that ACE2—together with the protease TMPR22—is crucial for the infection of cells with SARS-CoV‑2 [3, S2]. However, data on the expression of ACE2 in lung tissue are scarce. In contrast to the intestine, heart, and kidney, ACE2 expression levels in the lung are rather modest [S3]. In addition, experimental research revealed that ACE2 might have a protective role in lung injury. In a mouse model of acute acid-induced lung injury, the knockout of Ace2 resulted in detrimental effects, e.g., reduced lung elastance, reduced blood oxygen levels, and more interstitial edema compared with wildtype mice. Importantly, the effects of a lack of Ace2 might be mediated by reduced inactivation of Ang-2: (a) a double knockout of Ace2 and Ace was able to partially revert the effects; (b) pharmacological blockage or a genetic knockout of the AT1 receptor resulted in curtailing of the consequences of acid-induced lung injury [S4].
2. The role of ACE2 in the heart.
Patients suffering from COVID-19 frequently present with elevated cardiac markers, and case reports of acute myopericarditis by SARS-CoV‑2 have recently been published [S5]. There is also genetic evidence that single-nucleotide polymorphisms at the ACE2 locus are associated with left ventricular parameters in men [S6]. As already mentioned, ACE2 is expressed in the heart and inhibitors of the RAAS system have been described to modulate the system in animal models [4, 5]. While cardiotropism via ACE2 seems plausible, ACE2 might also have protective effects: Mice lacking Ace2 displayed reduced myocardial contractility; of note, similar to what has been observed in lung injury, an additional lack of Ace was able to obvert the cardiac phenotype. This again highlights the important role of ACE2 in counteracting Ang‑2 [S7].
3. The effects of ACEI and ARB on ACE2 activity and expression.
The influence of ACEI/ARB on ACE2 activity and expression is not well defined. Some data from animal models [4] but also cell culture experiments [S8] point to an increase of ACE2 expression under ACEI/ARB treatment. However, in humans, for example, in patients with heart failure, such treatment did not translate into altered ACE2 plasma levels [S9]. Expression changes in lung tissue remain unknown, making it impossible to predict exactly the ultimate consequences of RAAS inhibition on ACE2 levels and activity.
4. The role of ACEI and ARB in SARS-CoV-2 infection.
With two intuitively counteracting mechanisms linking SARS-CoV‑2 with ACEI and ARB—i.e., the drugs may potentially enhance virus uptake but also protect the lungs from RAAS overactivation—the net result of such medication is unpredictable. This is also reflected by a statement from the European Society of Cardiology published on March 13, 2020 as well as recent review papers on this topic [S10, S11], with the consequence of the medication being kept for hypertensive patients without any change in the current treatment protocol.
Taken together, ACE2 seems to have protective cardiac and pulmonary effects by counteracting RAAS, i.e., Ang‑2 (Fig. 1). However, given that an influence of ACEI and ARB on ACE2 in the pathophysiology of COVID-19 cannot be neglected, data on such treatment in COVID-19 patients and investigation of outcomes are urgently needed. In particular, one could speculate that ARB in particular, which limit the detrimental effects of Ang‑2 without altering the beneficial effects of Ang-(1–7), might not increase risk or may even improve outcomes.
Fig. 1.
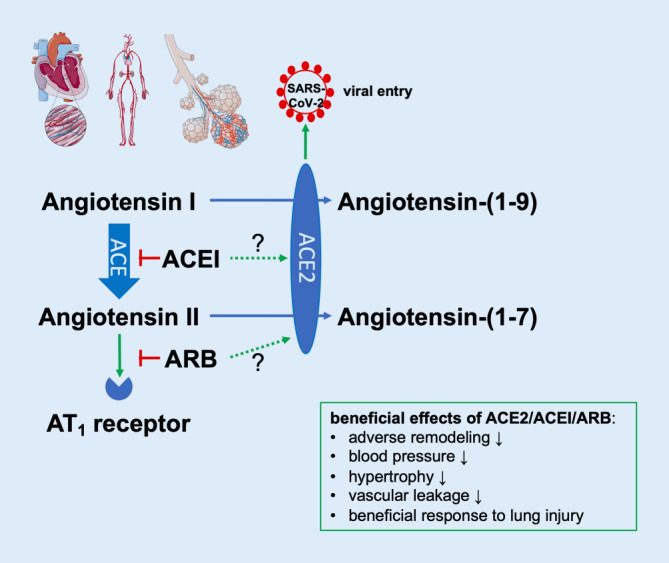
Overview of the possible interaction between the renin–angiotensin–aldosterone system, antihypertensive medication, and COVID-19. For details, see text. ACE2 angiotensin-converting enzyme 2, ACEI angiotensin-converting enzyme inhibitors, ARB AT1-receptor blockers. (Contains modified image material available at Servier Medical Art under a Creative Commons Attribution 3.0 Unported License)
Caption Electronic Supplementary Material
Conflict of interest
T. Kessler and H. Schunkert declare that they have no competing interests.
References
- 1.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus COVID-19 (ed) (2020) Global cases by the center for systems science and engineering at johns Hopkins university. https://coronavirus.jhu.edu/map.html. Accessed 2 Apr 2020
- 3.Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-coV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020 doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferrario CM, Jessup J, Chappell MC, et al. Effect of Angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111:2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 5.Schunkert H, Ingelfinger JR, Hirsch AT, et al. Feedback regulation of angiotensin converting enzyme activity and mRNA levels by angiotensin II. Circ Res. 1993;72:312–318. doi: 10.1161/01.res.72.2.312. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


