Abstract
Background
Transition programmes are designed to prepare adolescent inflammatory bowel disease [IBD] patients for transfer to adult care. It is still unclear which outcome parameters define ‘successful transition’. Therefore, this study aimed to identify outcomes important for success of transition in IBD.
Methods
A multinational Delphi study in patients, IBD nurses, and paediatric and adult gastroenterologists was conducted. In stage 1, panellists commented on an outcome list. In stage 2, the refined list was graded from 1 to 9 [least to very important], by an expert and a patient panel. In stage 3, the expert panel ranked important outcomes from 1 to 10 [least to most important]. Descriptive statistics and Mann–Whitney U-tests were performed.
Results
The final item list developed in stage 1 was tested by the expert [n = 74 participants, 52.7% paediatric] and patient panel [n = 61, aged 16–25 years, 49.2% male]. Respectively, ten and 11 items were found to be important by the expert and patient panel. Both panels agreed on eight of these items, of which six reflected self-management skills. In stage 3, the expert panel formed a top-ten list. The three most important items were: decision-making regarding IBD [mean score 6.7], independent communication [mean score 6.3] and patient satisfaction [mean score 5.8].
Conclusion
This is the first study identifying outcomes that IBD healthcare providers and patients deem important factors for successful transition. Self-management skills were considered more important than IBD-specific items. This is a first step to further define success of transition in IBD and subsequently evaluate the efficacy of different transition models.
Keywords: IBD, transition, transfer, success, outcome
1. Introduction
In up to 25% of patients inflammatory bowel disease (IBD; Crohn’s disease [CD] and ulcerative colitis [UC]) manifests during late childhood or adolescence.1,2 As IBD is a lifelong disease, all of these patients will need to undergo transfer of paediatric to adult care. To optimize this transfer and minimize adverse outcomes, it is advised to have a transition period during which patients [and parents] are prepared for the actual transfer.3,4 Transition is defined as the purposeful planned movement and preparation of adolescents and young adults with chronic medical conditions from child-centred to adult-orientated healthcare systems.5 In the transition process the patient, parent, paediatric gastroenterologist, adult gastroenterologist and IBD nurse have specific tasks.3,6 Patients should acquire [disease] knowledge, autonomy and self-management.7–11 Parents need to allow their adolescent child more independence. Physicians and nurses should support the transition process, be knowledgeable of adolescents’ developmental and health issues, and prepare adolescents for the changes that will be encountered in the adult healthcare system.6,12,13 Transitional programmes are designed to facilitate all these processes12,14,15 and prepare the individual patient for his/her transfer by helping to increase knowledge as well as to reach a higher level of self-management.
As summarized in the UK guideline on transition in patients with chronic digestive diseases, inadequate transition arrangements have been associated with adverse outcomes across several medical conditions, such as diabetes,16 heart disease17 and sickle cell disease.18 In IBD, studies investigating the impact of structured transition are scarce. Studies have shown that the lack of a structured transition service negatively impacted adherence19,20 and attendance,19,20 and was associated with a higher hospitalization and surgery rate.19 On the other hand, structured transition programmes have been shown to result in better disease-related outcomes,21,22 improved self- and disease knowledge and improved quality of life.22,23
Although many different models for transitional care have been proposed in IBD [e.g. 4,12,14,24], there is no evidence that one particular model is more effective than others.3 In addition, a clear definition on success of transition in IBD is lacking.12,19,25 Two recent studies identified general, non-disease-specific indicators for success of transition in adolescent medicine. Outcomes such as quality of life, continuity of care, self-management, therapy knowledge and adherence were recognized as important outcomes for successful transition.26,27 Continuity of care is considered a core issue,27 and this was also emphasized in a systematic review that showed engagement in adult care (attending first [two] visits) and retention in adult care [continuing to attend scheduled clinic appointments] were often used in studies investigating transition in chronically ill adolescents.28
In another recent study, IBD patients, their parents and paediatric healthcare providers were asked to select five of items from the Transition Readiness Assessment Questionnaire [TRAQ], thought to be important for successful transition. All three stakeholders had a different selection of items,29 but all selected items related to adherence, communication with the doctor, calling in case of problems or adverse reactions to medication.29
As emphasized in the European Crohn’s and Colitis Organisation [ECCO] topical review on transitional care in IBD, it is important to identify objective outcome measures that can be used to define successful transition in IBD.3 Therefore, the primary aim of this study was to identify outcomes that healthcare providers working with IBD patients think are important for success of transition in IBD, using a Delphi procedure in three types of healthcare providers working with IBD patients. Our secondary aim was to compare the outcomes identified by healthcare providers to outcomes selected by a patient panel, which was recruited in the second instance.
2. Materials and Methods
To identify healthcare transition outcomes for IBD, we conducted a three-stage Delphi30–33 process, a commonly used method for reaching consensus. The survey consisted of three rounds, which were designed and distributed using an online survey program [SurveyMonkey]. At each stage, all experts were contacted via e-mail explaining the task to be done, and a web link was included to complete the questionnaire. At each round, participants were given 2 weeks to send in their reply. Every 2 weeks a reminder was sent to all participants who had not yet replied. After three reminders, the web link was closed. We decided to give only factual feedback after each round, to avoid influencing panellists’ opinion.34 The study started in July 2016 and ended in March 2018.
2.1. Delphi panel
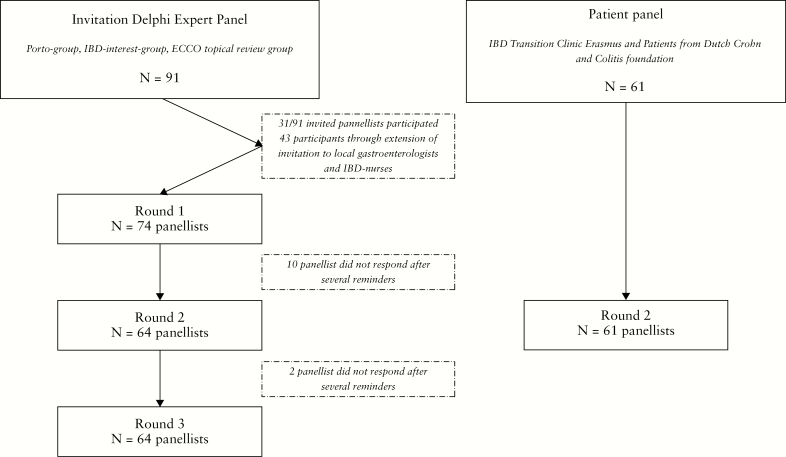
The Delphi panel was composed based on a practical approach. To achieve international consensus, experts in the field of IBD from around the world were invited to participate. Our main aim was to create a balanced panel of all healthcare providers working with IBD patients in the transition process. Therefore, paediatric gastroenterologists, [adult] gastroenterologists, and paediatric and adult IBD nurses were invited. The first step in composing the Delphi Panel was inviting all members of the ‘Paediatric IBD Porto and Interest Groups of European Society for Paediatric Gastroenterology Hepatology and Nutrition [ESPGHAN]’ and the authors of the ECCO Topical Review on transitional care in IBD.3 The ‘Paediatric IBD Porto Group’ is a group of 36 paediatric IBD experts from the ESPGHAN whose goals are to generate collaborative international research and to provide a leadership role concerning current diagnosis and management of IBD in children. The IBD Interest Group is an open, growing group of 48 ESPGHAN members at the time of the study who participate in all activities generated by the Porto group such as collaborative studies and guidelines preparation. The two groups consist mostly of paediatric gastroenterologists from Europe as well as Israel and some from North America. A total of 91 panellists were invited and were asked to participate as well as to invite a paediatric IBD nurse, adult gastroenterologist and adult IBD nurse, from their own hospital. From the 91 invited panellists, 31 [34%] agreed to participate. The 31 panellists invited another 43 physicians or nurses and vouched for their credentials. In addition, the website of the hospital where they worked was also checked to double-check their credentials. This resulted in 74 panellists [hereafter ‘Expert panel or panellists’; Figure 1].
Figure 1.
Flowchart composition Delphi panel.
After completing the Delphi stages in the expert panel, we concluded that also including the perspective of the adolescent and young adult patients would be of great added value. Therefore, we also included adolescent and young adult patients, hereafter defined as ‘patient panel or patients’. The patients were recruited from two sources: [a] an ongoing study into transition at the IBD outpatient transition clinic in the Erasmus Medical Centre in Rotterdam [the study was approved by the Medical Ethics Committee and patients provided informed consent], and [b] young adult IBD patients from the Dutch Crohn and Colitis patient organization. All patients were given 3 weeks to complete the survey and provided information with regard to their sex, age, disease duration and disease type. The patient panel participated in stage 2 only, but were asked after completing stage 2 if they thought an item was missing.
2.1.1. Stage 1
In this first stage, a literature review4,19,20,26–28,35,36 was performed and a list with items related to outcomes of transition was created. This list was sent to the research team, and was discussed in a joint meeting. The 23-item list was sent to all 74 participants of the expert panel [Figure 2A]. In stage 1, participants were asked to comment on the list, for example to state if they thought an item should be removed from the list [for reasons of not being associated with outcome of transition], merged with another item or rephrased. Additionally, participants were invited to add new items to the list. Lastly, all panellists were asked to complete a short form to collect demographic characteristics, such as their name, academic degree[s], department, position and details about the hospital where they work (name, city, country and hospital type [community vs tertiary hospital]).
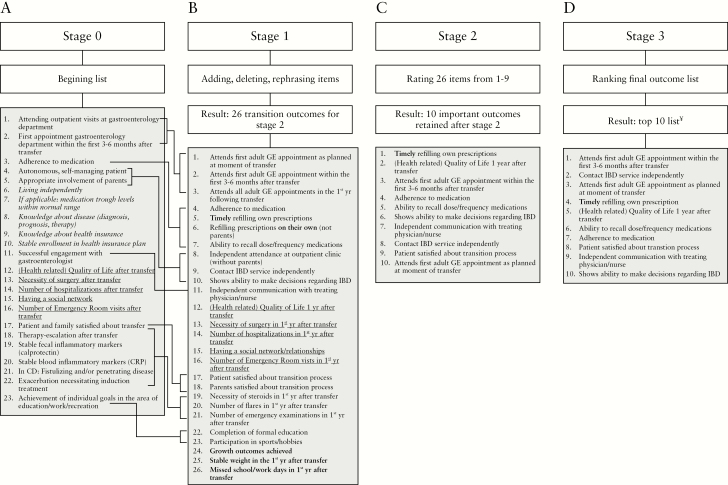
Figure 2.
Summary of stage 3 of the Delphi procedure. Note: panel A: italic, removed items; underlined, items not changed in stage 1. Panel B: bold items are those newly suggested. Panel C: §order of the items is based on the lowest [1] to highest [10] mean score [Table 3]. Panel D: ¥10 reflecting the most important, 1 the least important.
The research team analysed all responses from stage 1; each member first evaluated the responses individually, and in a meeting consensus was reached. Criteria to accept items were [a] suggestions to refine or specify items if it improved clarity or [b] every new suggested item related to outcomes of transition. Items were rejected or deleted if [a] they were not related to outcomes of transition [but to, for example, organization or availability or the IBD transition clinic] or [b] showed high similarity with an item already on the list. Similar outcomes were categorized into themes. Country-specific items were deleted, as our aim was to achieve international consensus.
2.1.2. Stage 2
In the second stage, participants were given a brief summary of the results of stage 1, indicating that some items had been deleted, rephrased or reformulated, and explaining that the new item list with outcomes of transition consisted of 26 items [Figure 2B]. In stage 2, the panellists were asked to rate each item on a scale from 1 [least important outcome of transition] to 9 [very important outcome of transition]. At all times, participants could contact the research team to comment or clarify. Before the start of the study, the research team agreed to use the ‘Rand UCLA criteria for agreement’, often used in Delphi studies,26,37 to categorize the outcomes as important, equivocal or not important. A threshold for retaining transition outcomes was established, based on the overall level of agreement among participants. Outcomes were labelled important when they had a mean of 7–9 without disagreement, outcomes rated 4–6 were considered equivocal, and outcomes rated 1–3 were rated as not important. Disagreement was defined as 30% of ratings being in the lower third [rating 1–3] and 30% in the upper third [7–9].38 Two members of the research team [G.B. and J.C.E.] analysed the responses and calculated means for each outcome and determined whether disagreement was present. This stage was also completed by the adolescent and young adult patient panel, recruited in a second instance.
2.1.3. Stage 3
In the third stage, the expert panel was given a brief summary of the results of stage 2, indicating that using the Rand UCLA criteria, the item list with 26 items was reduced to ten. In stage 3, this list with ten important outcomes was sent to the panel with the request to rank the items from 1 to 10, with ‘1’ meaning least important outcome of transition, and ‘10’ reflecting an essential outcome of transition. It was emphasized that each item could receive only one position between 1 and 10. Thus, the expert panel was now instructed to rank the important items from stage 2 in a top ten list, forcing them to re-prioritize the items and state which ones they consider most important.
2.2. Statistical analysis
Descriptive statistics were used to summarize the panellists’ opinions for closed questions at each round. Data were analysed with SPSS 23 [IBM] and analyses were conducted blind to the names of the participants. Open comments were analysed qualitatively and clustered into main themes. For stage 2, according to the ‘Rand UCLA criteria for agreement’, mean scores were calculated per item, and proportions were given to determine disagreement. Because of a non-normal distribution of the data, subgroups [e.g. patients panel vs expert panel or paediatric vs adult providers] were compared using a Mann–Whitney U test. Holms correction for multiple testing was used,39 and a corrected p-value < 0.05 was considered significant.
3. Results
3.1. Delphi panel
A total of 74 participants, from 17 countries, agreed to participate in the Delphi expert panel. Seventy-seven per cent of the experts came from Europe [n = 57; Austria n = 2, Croatia n = 1, Czech Republic n = 2, Denmark n = 3, England n = 18, Finland n = 1, Germany n = 2, Greece n = 2, Hungary n = 2, Italy n = 1, Lithuania n = 1, Scotland n = 7, Spain n = 1, the Netherlands n = 14], while the other participants came from Israel [n = 8], Canada [n = 3] and the United States [n = 6] [Table 1]. Participants belonged to one of the four core groups: paediatric gastroenterologist, paediatric IBD nurse, gastroenterologist or adult IBD nurse. The clinical research fellow was a medical doctor [MD] working in paediatrics [‘paediatric gastroenterologist group’], the transition manager had a Bachelor of Science in adolescent care [‘paediatric nurse group’] and the fellow paediatric gastroenterology was an MD working in paediatrics [‘paediatric gastroenterologist group’]. Of the 74 panellists, 40.5% were male, 91.9% worked in a tertiary hospital, 52.7% worked in the paediatric department and 30% were IBD nurses [Table 1].
Table 1.
Demographic characteristics of the expert panel [n = 74]
| N [%] | ||
|---|---|---|
| Sex | Male, % | 40.5 |
| Hospital type | Community hospital | 6 [8.1] |
| Tertiary hospital | 68 [91.9] | |
| Department | Paediatrics | 39 [52.7] |
| Gastroenterology | 29 [39.2] | |
| Internal Medicine | 6 [8.1] | |
| Position | Paediatric Gastroenterologist | 28 [37.8] |
| Paediatric IBD nurse | 10 [13.6] | |
| Gastroenterologist | 22 [29.7] | |
| Adult IBD nurse | 11 [14.9] | |
| Clinical research fellow | 1 [1.4] | |
| Transition manager | 1 [1.4] | |
| Fellow Paediatric Gastroenterology | 1 [1.4] | |
| Continent of origin | Europe | 57 [77.0] |
| North America | 9 [12.2] | |
| Asia | 8 [10.8] |
3.2. Patient panel [only participating in stage 2]
A total of 61 adolescent and young adult patients were recruited: 67.2% originated from the IBD-transition clinic in the Erasmus Medical Centre, 49.2% were male and mean age was 18.7 years [Table 2].
Table 2.
Demographics of the patient panel [n = 61]
| N [% or median] [IQR] | ||
|---|---|---|
| Recruited from | Dutch Crohn and Ulcerative Colitis Patient organization | 20 [32.8] |
| IBD Transition Clinic Erasmus Medical Centre | 41 [67.2] | |
| Age [years] | Range | 16.5–24.7 |
| Median [IQR] | 18.7 [18.1–20.1] | |
| Sex | Male | 30 [49.2] |
| Disease duration [years] | Range | 1–18 |
| Median [IQR] | 5.0 [3.0–7.0] | |
| Disease type | Crohn’s disease | 34 [55.7] |
| Ulcerative colitis | 23 [37.7] | |
| IBD unclassified | 4 [6.6] |
Abbreviation: IQR: interquartile range
3.2.1. Stage 1
All 74 panellists included in the expert panel responded to stage 1. Many panellists responded with suggestions for rephrasing of items already on the list, such as timely medication refill and refilling their own prescriptions. Using the suggestions from the panellists, several items were rephrased, split into more parts or specified [Figure 2A,B]. Five items were removed from the list [italic items in Figure 2A] for the following reasons: items 7, 9 and 10 were removed because of their country- and patient-specific nature. In addition, items 6 and 9 were removed because they were not considered to reflect outcomes of transition, and other items reflecting autonomy and knowledge were already on the list. Three new items were suggested by the panel and added to the list: growth target achieved, stable weight and missed school/work days [items 24–26, Figure 2B]. The new list thus consisted of 26 items [Figure 2B]. Some panellists also suggested items only reflecting disease-related knowledge and organization of the transition process [e.g. good collaboration of paediatric and adult gastroenterologist], and these were not used to refine the list with outcomes.
3.2.1. Stage 2
Of the 74 panellists in the expert panel, 64 [86.5%] responded to stage 2, rating each item with a number from 1 to 9 [9 = most important outcome for transition]. Of the 64 remaining participants, 14 were IBD nurses [21.8%], 28 [43.8%] paediatric gastroenterologists and 22 [34.4%] gastroenterologists. Nine out of ten non-responders worked in a tertiary hospital [one paediatric gastroenterologist, seven IBD nurses, one research fellow, one transition manager].
Table 3 shows the mean ratings for each of the 26 items for both the expert and the patient panel. For the expert panel, ten items had a mean score above 7 without disagreement, indicating important outcomes. The top five outcomes at this stage were [starting with the most important item]: attends first adult GE appointment as planned (mean 7.92, standard deviation [SD] 1.4), patient satisfied about transition process [mean 7.89, SD 1.5], contacting IBD service independently [mean 7.81, SD 1.1], independent communication [mean 7.79, SD 1.2] and shows ability to make decisions regarding IBD [mean 7.59, SD 1.2]. The least important outcomes were ‘necessity surgery’, ‘independent attendance outpatient clinic’, ‘participation sports/hobbies,’ ‘necessity steroids’ and ‘stable weight’. Continent of origin did not influence grading. Female members of the expert panel gave a significantly higher grade to the items ‘patient satisfaction’ (mean males 7.2 [SD 1.6]; mean females 8.4 [SD 1.0]; p = 0.008), ‘parental satisfaction’ (mean males 6.1 [SD 1.9]; mean females 7.6 [SD 1.3]; p = 0.008) and ‘growth outcomes achieved’ (mean males 5.1 [SD 2.3]; mean females 7.0 [SD 2.6]; p = 0.024).
Table 3.
Mean importance ratingsa of all 26 items from stage 2
| Item number | Mean score [SD] expert panel [n = 64] | % with a score 1.2 or 3b | Mean score [SD] patient panel [n = 61] | % with a score 1.2 or 3b | Corrected p-value | |
|---|---|---|---|---|---|---|
| 1. | Attends first adult GE appointment as planned at moment of transfer | 7.92 [1.4] | 1.6 | 6.98 [2.0] | 4.9 | 0.036* |
| 2. | Attends first adult GE appointment within the first 3–6 months after transfer | 7.12 [2.0] | 7.8 | 6.62 [2.1] | 11.5 | 1.000 |
| 3. | Attends all adult GE appointments in the 1st year following transfer | 6.76 [1.9] | 6.3 | 7.23 [2.1] | 6.6 | 0.649 |
| 4. | Adherence to medication | 7.48 [1.8] | 3.1 | 8.08 [1.6] | 3.3 | 0.09 |
| 5. | Timely refilling own prescriptions | 7.02 [1.5] | 1.6 | 7.82 [1.7] | 3.3 | 0.002* |
| 6. | Refilling prescription on their own [not parents] | 6.91 [1.6] | 4.7 | 7.33 [2.0] | 6.6 | 0.390 |
| 7. | Ability to recall dose/frequency medications | 7.56 [1.5] | 3.1 | 7.92 [1.5] | 1.6 | 0.480 |
| 8. | Independent attendance at outpatient clinic [without parents] | 5.94 [2.2] | 17.2 | 5.20 [2.8] | 32.8 | 1.000 |
| 9. | Contact IBD service independently | 7.81 [1.1] | 0 | 7.77 [1.6] | 1.6 | 1.000 |
| 10. | Shows ability to make decisions regarding IBD | 7.59 [1.2] | 1.6 | 8.16 [1.3] | 0 | 0.055 |
| 11. | Independent communication with treating physician/nurse | 7.79 [1.2] | 0 | 8.39 [0.8] | 0 | 0.036* |
| 12. | [Health-related] Quality of life 1 year after transfer | 7.11 [1.5] | 1.6 | 7.39 [1.9] | 6.6 | 1.000 |
| 13. | Necessity of surgery in 1st year after transfer | 5.56 [2.4] | 23.4 | 2.66 [2.1] | 72.1 | < 0.0001* |
| 14. | Number of hospitalizations in 1st year after transfer | 6.36 [2.3] | 12.5 | 3.08 [2.3] | 62.3 | < 0.0001* |
| 15. | Having a social network/relationships | 6.39 [1.9] | 10.9 | 6.46 [2.8] | 19.7 | 1.000 |
| 16. | Number of Emergency Room visits in 1st year after transfer | 6.59 [2.2] | 10.9 | 3.05 [2.5] | 65.6 | < 0.0001* |
| 17. | Patient satisfied about transition process | 7.89 [1.5] | 1.6 | 7.56 [1.9] | 6.6 | 1.000 |
| 18. | Parents satisfied about transition process | 6.92 [1.8] | 6.3 | 7.28 [1.9] | 6.6 | 1.000 |
| 19. | Necessity of steroids in 1st year after transfer | 6.02 [2.5] | 18.8 | 2.64 [2.1] | 68.9 | < 0.0001* |
| 20. | Number of flares in 1st year after transfer | 6.43 [2.3] | 14.1 | 3.15 [2.4] | 63.9 | < 0.0001* |
| 21. | Number of emergency examinations in 1st year after transfer | 6.36 [2.1] | 10.9 | 3.21 [2.2] | 59.0 | < 0.0001* |
| 22. | Completion of formal education | 6.17 [2.2] | 14.1 | 6.70 [2.9] | 19.7 | 0.238 |
| 23. | Participation in sports/hobbies | 5.97 [2.0] | 14.1 | 5.90 [2.8] | 23.0 | 1.000 |
| 24. | Growth outcomes achieved | 6.16 [2.6] | 18.8 | 5.41 [2.8] | 27.9 | 1.000 |
| 25. | Stable weight in the 1st year after transfer | 6.06 [1.9] | 9.4 | 5.72 [2.5] | 23.0 | 1.000 |
| 26. | Missed school/work days in 1st year after transfer | 6.67 [1.8] | 6.3 | 4.10 [2.7] | 47.5 | < 0.0001* |
Abbreviation: GE: gastroenterology.
aParticipants rated each item from 1 to 9.
bNo disagreement was found (30% of ratings in lower third [rating 1–3] and 30% in upper third [7–9]).
Bold represents a mean score of 7–9 without disagreement, which reflect ‘important outcomes’. *Corrected p-value using Holms correction for multiple testing <0.05 .
For the patient panel, 11 of the 26 items had a mean score above 7 without disagreement. The top five outcomes were [starting with the most important item]: independent communication [mean 8.39, SD 0.8], shows ability to make decisions regarding IBD [mean 8.16, SD 1.3], adherence to medication [mean 8.08, SD 1.6], ability to recall dose/frequency medication [mean 7.92, SD 1.5] and timely refilling own prescriptions [mean 7.82, SD 1.7]. The least important outcomes were: ‘necessity of surgery’, ‘necessity of steroids’, number of ‘hospitalizations’, ‘ER visits’ or ‘flares’ [Table 3]. No additional items related to success of transition were suggested by the patient panel. Sex did not influence grading within the patient panel [data not shown].
Comparing the grades from the expert [n = 64] and the patient [n = 57] panel [Table 3] showed that both panels identified the same eight items as important (mean grades for these items were quite similar [<1 point difference between the two groups]). Additionally, the patient panel found ‘attends all GE appointments in first year following transfer’, ‘parents satisfied with transition’ and ‘refilling prescriptions on own’ to be important, and the expert panel considered ‘attend first GE appointment as planned’ and ‘within the first 3–6 months after transfer’ to be important. For some of the ‘non-important’ items [mean < 7] differences between the two panels were large: disease-related outcomes [items 13, 14, 16, 19–21] and ‘school/work absence’ [item 26] received a significantly lower mean score by the patient panel [range 2.6–3.3] compared to the expert panel [range 5.5–6.6].
Comparing the different providers within the expert panel (adult [n = 32] vs paediatric [n = 32] healthcare providers; paediatric [n = 28] vs adult [n = 22] gastroenterologists; nurses [n = 13] vs physicians [n = 50]) did not show significant differences after correction for multiple testing.
3.2.3. Stage 3
Of the 64 experts, 62 responded to stage 3. Table 4 and Figure 2D display the top-ten ranking of the important outcomes from stage 2. For the panel as a whole, ‘ability to make decisions regarding IBD’ [mean 6.7, SD 2.7], ‘independent communication’ [Mean 6.3, SD 2.8] and ‘patient satisfaction’ [mean 5.8, SD 2.4] were the top three outcomes, whereas ‘attends first GE appointment within the first 3–6 months after transfer’ [mean 4.4, SD 3.2], ‘contact IBD service independently’ [mean 5.2, SD 2.4] and ‘attends first GE appointment as planned’ [5.4, SD 3.6] received lower scores [Table 4]. Differences for the three provider types are shown in Table 4. Comparing the different providers within the expert panel (adult [n = 32] vs paediatric [n = 28] healthcare providers [see Supplementary Figure 1]; paediatric [n = 28] vs adult [n = 22] gastroenterologists; nurses [n = 12] vs physicians [n = 50]) did not show significant differences after correction for multiple testing.
Table 4.
Top ten ranking of stage 3 outcomes all 62 participants and per provider type
| Top ten – all 62 participants | Mean [SD] | Top ten – pediatric gastroenterologists [n = 28] | Mean [SD] | Top ten – gastroenterologists [n = 22] | Mean [SD] | Top ten – IBD nurses [n = 12] | Mean [SD] |
|---|---|---|---|---|---|---|---|
| Attends first adult GE appointment within the first 3–6 months after transfer | 4.37 [3.2] | Attends first adult GE appointment within the first 3–6 months after transfer | 4.11 [3.2] | Attends first adult GE appointment within the first 3–6 months after transfer | 4.14 [2.7] | Adherence to medication | 4.17 [3.2] |
| Contact IBD service independently | 5.15 [2.4] | Timely refilling own prescriptions | 5.04 [2.8] | Attends first adult GE appointment as planned at moment of transfer | 4.5 [3.5] | Timely refilling own prescriptions | 4.42 [1.9] |
| Attends first adult GE appointment as planned at moment of transfer | 5.40 [3.6] | Ability to recall dose/ frequency medications | 5.39 [2.6] | Contact IBD service independently | 4.91 [1.9] | Contact IBD service independently | 4.58 [3.0] |
| Timely refilling own prescriptions | 5.42 [2.7] | [Health-related] Quality of life 1 year after transfer | 5.43 [3.1] | Adherence to medication | 5.27 [2.4] | Attends first adult GE appointment within the first 3–6 months after transfer | 5.42 [3.8] |
| [Health-related] Quality of life 1 year after transfer | 5.44 [3.3] | Contact IBD service independently | 5.57 [2.5] | [Health -related] Quality of life 1 year after transfer | 5.32 [3.7] | Ability to recall dose/ frequency medications | 5.50 [1.7] |
| Ability to recall dose/ frequency medications | 5.53 [2.8] | Attends first adult GE appointment as planned at moment of transfer | 5.79 [3.7] | Patient satisfied about transition process | 5.41 [2.7] | [Health-related] Quality of life 1 year after transfer | 5.67 [3.2] |
| Adherence to medication | 5.55 [2.3] | Patient satisfied about transition process | 5.93 [2.4] | Ability to recall dose/ frequency medications | 5.77 [2.3] | Patient satisfied about transition process | 6.00 [2.1] |
| Patient satisfied about transition process | 5.76 [2.4] | Independent communication with treating physician/nurse | 6.00 [2.9] | Independent communication with treating physician/nurse | 6.27 [2.9] | Shows ability to make decisions regarding IBD | 6.00 [2.7] |
| Independent communication with treating physician/nurse | 6.31 [2.8] | Adherence to medication | 6.32 [2.7] | Timely refilling own prescriptions | 6.45 [2.7] | Attends first adult GE appointment as planned at moment of transfer | 6.17 [3.8] |
| Shows ability to make decisions regarding IBD | 6.65 [2.7] | Shows ability to make decisions regarding IBD | 6.68 [2.6] | Shows ability to make decisions regarding IBD | 6.95 [2.7] | Independent communication with treating physician/nurse | 7.08 [2.4] |
Note: the most important outcomes, with highest importance rank, are on the lower part of the list.
Abbreviation: GE: gastroenterology.
4. Discussion
The primary objective of this study was to identify outcomes that three types of healthcare providers responsible for the care of IBD patients [gastroenterologists, paediatric gastroenterologists and IBD nurses] thought were important for success of transition in IBD patients. Our secondary aim was to compare these outcomes to those selected by a patient panel recruited in the second instance, i.e. who only participated in stage 2 of this Delphi study. In stage 2, ten and 11 out of 26 items were identified as important by the expert [n = 64] and the patient panel [n = 61], respectively [Stage 2, Table 3]. Surprisingly, results show that both the expert and the patient panel thought the same items were important for success of transition: eight items were identified as important in both the patient and the expert panel. Of these, six concerned self-management skills and autonomy [e.g. independent communication, medication adherence], while the other two items were more general: health-related quality of life and patient satisfaction about transition process. In addition, both panels thought that attendance at adult gastroenterology appointments was important, but gave slightly different grades [difference < 1 point] to the relevant items [items 1–3, Table 3]. Similarly, ‘satisfaction of parents about transition process’ was considered important in both panels, and almost reached the threshold for importance in the expert panel. Likewise, ‘independent attendance at outpatient clinic’ received a low grade [<6] by both the expert and the patient panel, possibly reflecting that both value or at least do not disapprove the presence of parents.
Only the expert panel provided a top-ten ranking [=stage 3] of the important items, and this showed that from the ten important items, decision -making, independent communication and patient satisfaction were considered most important for success of transition in IBD patients. Comparing the top ten of different providers did not show significant differences.
Remarkably, none of the IBD/disease-specific items [e.g. surgery, inflammatory markers] were found to be important. The patient panel gave even lower grades than the expert panel. This is in accordance with previous studies discussing successful transition in other chronic diseases such as congenital heart defects,40 rheumatological diseases41,42 and congenital adrenal hyperplasia.43 In all these studies successful transition was not defined by disease-specific items, but by attendance at the first [one or two] visits of the adult healthcare provider. This seems a restricted definition of success. However, continuity of care is seen as a core outcome of transition,27 and is often studied as an outcome of transition.28 Incorporating disease outcomes in the definition of successful transition can be complicated given the heterogeneous course of chronic diseases such as IBD as well as the case mix that occurs when patients with a severe course are seen in [academic] centres.6 Philpott and Kurowski therefore plea for including patient-driven outcomes in the definition of successful transition, such as trust in the adult healthcare system and autonomy.6
In IBD, several studies have investigated outcomes of transition. A study by Bollegala et al. retrospectively compared outcomes 1 year before vs 1 year after transfer [n = 95, no structured transition programme] and report fewer outpatient clinic visits and more non-compliance, but no differences in other aspects of healthcare utilization.20 Furthermore, a survey by Bennett et al. showed no differences in compliance, complications, surgery, hospitalization rate or number of flares between 46 IBD patients who had transferred to adult care [without a structured transition programme] and 36 age-matched patients who received care in an adult setting from the beginning.44 Finally, Cole et al. showed that patients who did not attend a transition service more often needed surgery and hospitalization, and had higher non-attendance and lower treatment adherence than patients who did attend a transition service.19 These studies suggest that clinical outcomes might be different for patients who followed a structured transition programme and those who did not, with possibly better outcomes after structured transition. However, at this point, it is unknown whether absence from the transition programme itself is a risk factor for adverse outcomes or if absence is just a surrogate marker of patients who are not able to attend the transition programme due to a complicated course of IBD.
So far, a definition of successful transition in IBD has not been formulated. Previously, our research group designed a score measure of success of transition in IBD [the Transition Yourself score].45 The score comprised four elements: time to first outpatient visit to adult gastroenterologist, adherence to visits at the gastroenterology outpatient clinic, adherence to medication and qualitative evaluation of transition by the patient. The Transition Yourself score was developed based on a literature review and a focus group review with IBD experts, but has not yet been validated. In addition to validating the score, our research group considered it important to ask the opinion of a larger IBD expert panel in identifying items reflecting success of transition and also ask patients’ opinion.
Two recent studies used a Delphi study to identify general, non-disease-specific indicators for success of transition in adolescent medicine.26,27 First, Fair et al. included 117 experts, mainly from the US [88%], and 70% paediatric professionals. In the final stage, ten important outcomes were found: achieving optimal quality of life, self-managing own condition, understanding characteristics and complications of condition, knowing names and purposes of medication, adherence to medication, attending most medical appointments, having a medical home, avoiding unnecessary hospitalizations, understanding health insurance, and having a social network.26 Second, Suris and Akre included 37 adolescent health workers [mainly physicians] from 15 countries. Items found to be important for success of transition were: patient not lost to follow up, no missed consultations, trusting relationship with provider, attention to self-management, first visit adult care within the first 3–6 months after transfer, number of emergency room visits, patient/family satisfied transfer, maintaining stable disease or improvement.27
The selected items in both studies partly resemble the important items identified in this study. However, some of the items are described in general words, e.g. ‘managing your own condition’, which covers several items from our item list. Due to this lack of specificity, it remains unclear which specific items are valued most by the panellists in the previous studies. Furthermore, only Suris and Akre’s list included a disease-related item: stable disease or disease improvement. In our expert and patient panels, disease-specific parameters received low grades. Moreover, disease knowledge was included in the final outcome list by Fair et al. We chose not to include knowledge of disease in our refined list for stage 1, because items implying disease knowledge were already on the list.
4.1. Strengths and limitations
This study was strengthened by the appropriate use of the Delphi procedure, and the use of a large multinational expert panel, including healthcare providers from 17 countries. Secondly, formation of the Delphi panel was initiated by inviting two pre-existing expert groups with a leadership role and expertise in the care of adolescent IBD patients to form the Delphi panel. Extension of this invitation eventually led to the inclusion of 74 paediatric gastroenterologists, gastroenterologists and IBD nurses from both the paediatric and the adult department. Thirdly, in the second instance a patient panel was composed to provide the patient’s perspective in grading the 26 items in stage 2. Lastly, the expert panel was balanced with 50% of panellists from both the paediatric and the adult department.
The study was limited by a low response rate in the first invitation round [34%], although 31 opinion leaders in IBD with great experience in transition did participate, and the final panel consisted of 74 members. In addition, the majority of experts worked in Europe, which may reflect a Western perspective. Second, 90% of the panellists worked in tertiary hospitals; although this is a limitation, it reflects the fact that most paediatric IBD patients are treated in tertiary hospitals.46 Third, although using the widely accepted RAND UCLA criteria for agreement, items with a mean below 7 were now labelled ‘not important’, which could be judged as too stringent. Fourth, it would have been better if the patient panel was included from the beginning of the study, so that all three Delphi stages would have been completed by all participants at the same time. Fifth, the subgroup analyses performed within the expert panel had a relatively low number of participants. Finally, to ensure clarity of all items on the list, we chose to specify the items as much as possible. As a consequence, sometimes several items concerned the same topic, but had a different emphasis (e.g. three items regarding medication adherence [items 4–6 Figure 2B]).
5. Conclusion
This is the first study investigating outcomes reflecting successful transition in IBD patients using a multinational expert panel and comparing the results to a patient panel. Experts and patients agreed to a great extent: eight out of 26 items were found to be important for success of transition, six of which concerned self-management skills/autonomy. Remarkably, no IBD-specific item was found to be important. The three most important outcomes in the top-ten list from the expert panel were independent decision-making, independent communication and patient satisfaction, and these did not differ between paediatric gastroenterologists, gastroenterologists and IBD nurses. Identifying these outcomes can facilitate the definition of successful transition and subsequently the construction of an objective score measuring success of transition. After validation, this score could be used to test the efficacy of the different transition programmes, in order to improve transitional care worldwide.
Funding
None.
Conflict of Interest
The authors report no conflicts of interest.
Author Contributions
G.B. and J.C.E. designed the study. G.B. collected the data and drafted the paper, which was revised for important intellectual content by J.C.E., L.R., J.W. and M.G. All authors read and approved the final manuscript.
Supplementary Material
Acknowledgments
We thank all the panellists for their contribution: Angelika Kindermann, Christine Spray, Vaidotas Urbonas, Almuthe Christina Hauer, Kaija-Leena Kolho, Batia Weiss, Annemone van den Berg, Katrine Carlsen, Lissy de Ridder, Vibeke Wewer, Roma Eleftheria, Johanna Escher, Sanja Kolaček, Ida Vind, Birgit Terjung, Fabiana Castiglione, Patricia Sarlos, Janneke van der Woude, Marijn Visschedijk, Ariella Bar-Gil Shitrit, Rachel Cooney, Krisztine Gecse, Natasha Burgess, Joyce van der Burg, Betty Mazuz, Melanie Love, Rachel Russell, Anneke Kaptein-Schumacher, Lisa Whitley, Revital Barkan, Anita Gaggl, Karen O’Hara-Banack, Greetje Sekema, Anneke de Bruin, Rachel Leshem Namedar, Pamela Rogers, Vikki Garrick, Aileen Fraser, Kay Crook, Elena Gil-Zaragozano, Sibongile Chadokufa, Maria de Jong, Martha van Gaalen, Victoria Merrick, Harland Winter, Javier Martin, Athos Bousvaros, Neil Shah, Gabor Veres, Eytan Wine, Stephan Buderus, Dan Turner, Rafeeq Muhammed, Jiri Bronsky, Patrick van Rheenen, Richard Russell, Jess Kaplan, Christopher Moran, Nick Croft, Christos Tzivinikos, Paul Collins, Pavel Kolhout, James Lindsay, Ian Arnott, Karen Kroeker, Irit Avni-Biron, Marcus Harbord, Gerassimos Mantzaris, Ashwin Ananthakrishnan, Daniel Gaya, Amit Assa, Paul Henderson, Tom Creed and Nigel Mills. In addition, we thank Tineke Markus from the Dutch Crohn and Colitis patient organization for helping us compose the patient panel and thank all the patients who gave their opinion.
References
- 1. Griffiths AM. Specificities of inflammatory bowel disease in childhood. Best Pract Res Clin Gastroenterol 2004;18:509–23. [DOI] [PubMed] [Google Scholar]
- 2. Adamiak T, Walkiewicz-Jedrzejczak D, Fish D, et al.. Incidence, clinical characteristics, and natural history of pediatric IBD in Wisconsin: a population-based epidemiological study. Inflamm Bowel Dis 2013;19:1218–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. van Rheenen PF, Aloi M, Biron IA, et al.. European Crohn’s and Colitis Organisation topical review on transitional care in inflammatory bowel disease. J Crohns Colitis 2017;11:1032–8. [DOI] [PubMed] [Google Scholar]
- 4. Brooks AJ, Smith PJ, Cohen R, et al.. UK guideline on transition of adolescent and young persons with chronic digestive diseases from paediatric to adult care. Gut 2017;66:988–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Blum RW, Garell D, Hodgman CH, et al.. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health 1993;14:570–6. [DOI] [PubMed] [Google Scholar]
- 6. Philpott JR, Kurowski JA. Challenges in transitional care in inflammatory bowel disease: a review of the current literature in transition readiness and outcomes. Inflamm Bowel Dis 2019;25:45–55. [DOI] [PubMed] [Google Scholar]
- 7. van Groningen J, Ziniel S, Arnold J, Fishman LN. When independent healthcare behaviors develop in adolescents with inflammatory bowel disease. Inflamm Bowel Dis 2012;18:2310–4. [DOI] [PubMed] [Google Scholar]
- 8. Fishman LN, Ziniel SI, Adrichem ME, Fernandes SM, Arnold J. Provider awareness alone does not improve transition readiness skills in adolescent patients with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2014;59:221–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Trivedi I, Keefer L. The emerging adult with inflammatory bowel disease: challenges and recommendations for the adult gastroenterologist. Gastroenterol Res Pract 2015;2015:260807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fishman LN, Barendse RM, Hait E, Burdick C, Arnold J. Self-management of older adolescents with inflammatory bowel disease: a pilot study of behavior and knowledge as prelude to transition. Clin Pediatr 2010;49:1129–33. [DOI] [PubMed] [Google Scholar]
- 11. Wright EK, Williams J, Andrews JM, et al.. Perspectives of paediatric and adult gastroenterologists on transfer and transition care of adolescents with inflammatory bowel disease. Intern Med J 2014;44:490–6. [DOI] [PubMed] [Google Scholar]
- 12. Goodhand J, Hedin CR, Croft NM, Lindsay JO. Adolescents with IBD: the importance of structured transition care. J Crohns Colitis 2011;5:509–19. [DOI] [PubMed] [Google Scholar]
- 13. Brooks AJ, Smith PJ, Lindsay JO. Monitoring adolescents and young people with inflammatory bowel disease during transition to adult healthcare. Frontline Gastroenterol 2018;9:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Escher JC. Transition from pediatric to adult health care in inflammatory bowel disease. Dig Dis 2009;27:382–6. [DOI] [PubMed] [Google Scholar]
- 15. Dabadie A, Troadec F, Heresbach D, Siproudhis L, Pagenault M, Bretagne JF. Transition of patients with inflammatory bowel disease from pediatric to adult care. Gastroenterol Clin Biol 2008;32:451–9. [DOI] [PubMed] [Google Scholar]
- 16. Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics 2009;124:e1134–41. [DOI] [PubMed] [Google Scholar]
- 17. Wray J, Frigiola A, Bull C; Adult Congenital Heart disease Research Network (ACoRN) Loss to specialist follow-up in congenital heart disease; out of sight, out of mind. Heart 2013;99:485–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Andemariam B, Owarish-Gross J, Grady J, Boruchov D, Thrall RS, Hagstrom JN. Identification of risk factors for an unsuccessful transition from pediatric to adult sickle cell disease care. Pediatr Blood Cancer 2014;61:697–701. [DOI] [PubMed] [Google Scholar]
- 19. Cole R, Ashok D, Razack A, Azaz A, Sebastian S. Evaluation of outcomes in adolescent inflammatory bowel disease patients following transfer from pediatric to adult health care services: case for transition. J Adolesc Health 2015;57:212–7. [DOI] [PubMed] [Google Scholar]
- 20. Bollegala N, Brill H, Marshall JK. Resource utilization during pediatric to adult transfer of care in IBD. J Crohns Colitis 2013;7:e55–60. [DOI] [PubMed] [Google Scholar]
- 21. Crowley R, Wolfe I, Lock K, McKee M. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child 2011;96:548–53. [DOI] [PubMed] [Google Scholar]
- 22. Mackie AS, Islam S, Magill-Evans J, et al.. Healthcare transition for youth with heart disease: a clinical trial. Heart 2014;100:1113–8. [DOI] [PubMed] [Google Scholar]
- 23. McDonagh JE, Southwood TR, Shaw KL; British Society of Paediatric and Adolescent Rheumatology The impact of a coordinated transitional care programme on adolescents with juvenile idiopathic arthritis. Rheumatology 2007;46:161–8. [DOI] [PubMed] [Google Scholar]
- 24. de Silva PS, Fishman LN. Transition of the patient with IBD from pediatric to adult care – an assessment of current evidence. Inflamm Bowel Dis 2014;20:1458–64. [DOI] [PubMed] [Google Scholar]
- 25. Leung Y, Heyman MB, Mahadevan U. Transitioning the adolescent inflammatory bowel disease patient: guidelines for the adult and pediatric gastroenterologist. Inflamm Bowel Dis 2011;17:2169–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fair C, Cuttance J, Sharma N, et al.; International and Interdisciplinary Health Care Transition Research Consortium International and interdisciplinary identification of health care transition outcomes. JAMA Pediatr 2016;170:205–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Suris JC, Akre C. Key elements for, and indicators of, a successful transition: an international Delphi study. J Adolesc Health 2015;56:612–8. [DOI] [PubMed] [Google Scholar]
- 28. Rachas A, Lefeuvre D, Meyer L, et al. . Evaluating continuity during transfer to adult care: a systematic review. Pediatrics 2016;138:e20160256. [DOI] [PubMed] [Google Scholar]
- 29. Gray WN, Reed-Knight B, Morgan PJ, et al.. Multi-site comparison of patient, parent, and pediatric provider perspectives on transition to adult care in IBD. J Pediatr Nurs 2018;39:49–54. [DOI] [PubMed] [Google Scholar]
- 30. Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Practical Assessment Research and Education 2007:12:1–8. [Google Scholar]
- 31. Dewa LH, Murray K, Thibaut B, et al.. Identifying research priorities for patient safety in mental health: an international expert Delphi study. BMJ Open 2018;8:e021361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Russell D, Atkin L, Betts A, et al.. Using a modified Delphi methodology to gain consensus on the use of dressings in chronic wounds management. J Wound Care 2018;27:156–65. [DOI] [PubMed] [Google Scholar]
- 33. Snelson E, Ramlakhan S. Which observed behaviours may reassure physicians that a child is not septic? An international Delphi study. Arch Dis Child 2018;103:864–7. [DOI] [PubMed] [Google Scholar]
- 34. Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs 2000;32:1008–15. [PubMed] [Google Scholar]
- 35. Oswald DP, Gilles DL, Cannady MS, Wenzel DB, Willis JH, Bodurtha JN. Youth with special health care needs: transition to adult health care services. Matern Child Health J 2013;17:1744–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sattoe JNT, Hilberink SR, van Staa A. How to define successful transition? An exploration of consensus indicators and outcomes in young adults with chronic conditions. Child Care Health Dev 2017;43:768–73. [DOI] [PubMed] [Google Scholar]
- 37. Elwyn G, O’Connor A, Stacey D, et al.; International Patient Decision Aids Standards (IPDAS) Collaboration Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ 2006;333:417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fitch K, Bernstein S, Aguilar MD, et al. . The RAND/UCLA appropriateness method user’s manual. Santa Monica: Rand; 2001. https://www.rand.org/pubs/monograph_reports/MR1269.html. Accessed February 2019. [Google Scholar]
- 39. Holms S. A simple sequential rejective method procedure. Scand J Stat 1979;6:65–70. [Google Scholar]
- 40. Reid GJ, Irvine MJ, McCrindle BW, et al.. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics 2004;113:e197–205. [DOI] [PubMed] [Google Scholar]
- 41. Hazel E, Zhang X, Duffy CM, Campillo S. High rates of unsuccessful transfer to adult care among young adults with juvenile idiopathic arthritis. Pediatr Rheumatol Online J 2010;8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Jensen PT, Karnes J, Jones K, et al.. Quantitative evaluation of a pediatric rheumatology transition program. Pediatr Rheumatol Online J 2015;13:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gleeson H, Davis J, Jones J, O’Shea E, Clayton PE. The challenge of delivering endocrine care and successful transition to adult services in adolescents with congenital adrenal hyperplasia: experience in a single centre over 18 years. Clin Endocrinol (Oxf) 2013;78:23–8. [DOI] [PubMed] [Google Scholar]
- 44. Bennett AL, Moore D, Bampton PA, Bryant RV, Andrews JM. Outcomes and patients’ perspectives of transition from paediatric to adult care in inflammatory bowel disease. World J Gastroenterol 2016;22:2611–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. van den Brink G, van Gaalen MAC, Zijlstra M, de Ridder L, van der Woude CJ, Escher JC. Self-efficacy did not predict the outcome of the transition to adult care in adolescents with inflammatory bowel disease. Acta Paediatr 2019;108:333–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. de Bie CI, Buderus S, Sandhu BK, et al.; EUROKIDS Porto IBD Working Group of ESPGHAN Diagnostic workup of paediatric patients with inflammatory bowel disease in Europe: results of a 5-year audit of the EUROKIDS registry. J Pediatr Gastroenterol Nutr 2012;54:374–80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.