Abstract
The first actions and provisions in a Southern Italy Department of Radiation Oncology are described at the inception of the COVID-19 pandemic.
Introduction
On March 11, 2020, after the global spread of the coronavirus disease 2019 (COVID-19) epidemic, the World Health Organization declared a spreading pandemic.1 As of March 31, 809,608 people globally are registered as confirmed cases and 39,033 have died. Italy has been particularly affected, second only to the United States in confirmed cases and having the most deaths.2 In these days health capacity to assure equal assistance is scarce.3 Some radiation oncologists in the north of Italy have described their experience in an area with a high incidence of the viral disease.4,5
The first COVID-19 patient in the Apulia region (Italy), one of the largest regions of the south, was diagnosed on February 24, 2020. On February 20, the first Italian patient in a hospital ward in Italy was diagnosed in Codogno, a town in the south of Lombardy, the most populous Italian region. Codogno has the highest gross internal product per capita. The first case diagnosed in Apulia was a man who had been some days before in Codogno.
Because many people who live or work in Lombardy are originally from the south, their visits to parents and relatives represented one of the major ways the infection spread from affected areas in the north to the south of Italy. Another way of infectious spread could have been by the transfer of patients, mostly cancer patients, who, despite living in the south of Italy, are treated in health institutions in Lombardy. This phenomenon is called “health migration” and it is caused by a shortage of health care facilities in the south, the reasons for which are beyond the scope of this article. According to the Italian Ministry of Health, almost 40,000 hospital admissions per year are patients from the Apulia region and more than 10,000 patients are from Lombardy.6
On March 28, 2020, total diagnosed cases in Lombardy amounted to 39,415 and to 1458 in Apulia. It should be noted that on the night of March 8, after miscommunications regarding the first government restrictions on mobility from Lombardy and some other northern areas, about 25,000 students and workers came back to the south. A regional act required them to communicate their arrival to regional authorities and to self-quarantine: in the Apulia region about 2000 did so.
This article describes how the COVID-19 pandemic has changed the availability of radiation therapy, patient outcomes, and risk to health care providers.
First COVID-19 Patients in Our Radiation Oncology Department
On March 2, 2020, in our radiation oncology department (ROd), a male patient with mediastinal syndrome was referred from the medical oncology department. He underwent computed tomography simulation and started treatment of 5 daily fractions. On March 5, a woman with brain metastasis underwent computed tomography simulation for whole brain and another patient with bone metastasis started treatment. During the second session of radiation therapy the patient with brain metastasis vomited in the treatment room and treatment was stopped. Three technologists and 1 physician did not use personal protective equipment (PPE) when they made contact with her. On March 13, the head of ROd was informed that the aforementioned patients were COVID-19 positive. Two of them died some days after. The 4 professionals were put in quarantine and COVID-19 tests were required. On March 9, PPE was provided to staff, including surgical masks, filtering face piece (FFP)–2 mask to be used during contact with patients, disposable gowns, and gloves. FFP1 masks filter nontoxic powder with an admitted leakage of 15%, FFP2 masks filter powder fumes and aerosols that are damaging to human health with maximum leakage of 11%, and FFP3 masks are similar to FFP2, but they also filter viruses and bacteria with a maximum leakage of 5%.
On March 19, the health director of the hospital decided all personnel should have COVID-19 tests: 1 out of 27 tested positive. Note that these results were communicated 1 week after the tests were performed. None of the professionals got ill during this period.
After initial, inhomogeneous reactions across different regions, testing for all health care workers (HCWs) was required by professional organizations. Although these protests of the professional associations, quarantine was reserved only for HCWs coming into “strict contact” (less than 1 meter) with COVID-19 positive patients without PPE (at least a surgical mask), and tests were performed on the seventh day after contact. In cases of other types of contact with positive patients, HCWs are required to keep working and to self-monitor their health status (temperature monitoring). It is likely that this policy was decided on because of a regional shortage of tests and personnel. In this department positive nurses were put in quarantine and the remaining HCWs were treated as cases with nonstrict contact because of the use of surgical masks.
Sequence of Legislative Provisions and the New Internal Procedures
On March 8, the prime minister7 decreed a lockdown of the areas where the epidemic originated from and of those in which spread was faster; in the following days, other decrees extended the lockdown to the entire nation.8,9 In this latter decree, health professionals were required to adopt all measures provided by World Health Organization for effective prevention of the diffusion of the respiratory infection.10 On March 9, a new decree-law was published by the national government for the empowerment of health service requiring health professionals to start, differently from general population, quarantine only at the onset of symptoms or after a positive test.11 These provisions obviously applied to the entire personnel of this department in the week after the COVID-19 tests, the results of which found that 1 person was positive. As a consequence, the tests were performed again.
Because the health service depends on regional governments, the Apulia government published a general act on March 8 obliging people coming from the regions of onset of the epidemic to declare their name and address. Furthermore, an administrative act declared medical activities should still be performed, including radiation oncology.12
On March 13, another administrative act defined procedures to be taken in case of contact between a health professional and a COVID-19-positive patient.13 In case of contact with a confirmed COVID-19 patient without PPE, the professional must be put in quarantine and tested 7 days after contact.
On March 16, the local authority mandated the use of FFP2 masks when dealing with suspected cases and FFP3 masks in cases of confirmed COVID-19 in aerosol generating procedures. Since then radiation therapy personnel in this hospital have used surgical masks and FFP2 masks when dealing with suspected cases. The local authority also mandated a daily triage of radiation therapy patients. Those with cough or fever are thus to be excluded from radiation therapy treatment and sent to a medical practitioner to start the diagnostic procedures for COVID-19.
On March 17, a hospital directive required physicians to “evaluate, for each patient, the opportunity to perform or delay” radiation therapy, that patients should enter individually into the ROd to avoid simultaneous waiting of too many patients, and that each patient should be given a protective mask. In particular, treatment of breast and prostate postoperative patients and intact prostate cancers in hormone-deprivation patients was postponed. The scheduled delay was 2 weeks.
Conversely, the Italian Health Ministry published a note on March 10 stating that the delivery of radiation therapy treatment in COVID-19 patients should be assured.14 This document declared also that the completion of oncologic treatment for patients who had contact with COVID-19 infected persons should be assured. In our opinion, because the oncologic treatment could worsen immunosuppression and foster virus infection, this measure could lead to additional problems for patients and medical personnel.
On March 19, the Italian Association of Radiation Oncology provided guidelines that were in agreement with the procedures provided by the regional and local health authorities in Apulia.15
Actions
In this department, control visits were delayed unless patients, by telephone, declared active oncologic problems or persistent acute side effects. For a first consultation patients were offered the possibility to send documentation by email and to do a video consultation by means of a dedicated Internet link not requiring any app installation.16 Up to now, we have treated 3 patients from the hospital wards who were subsequently diagnosed as COVID-19-positive, and in 2 cases the start of outpatient radiation therapy treatment was interrupted when they informed us they were under testing after contact with infected relatives.
To avoid having too many patients at the same time in the waiting room we have distributed them into 3 sessions per hour and asked accompanying persons not to enter the department with the patient. This decision has reduced the number of treatments per day. The total number of daily treated patients has been reduced from 65 to 45 (2 LINACs).
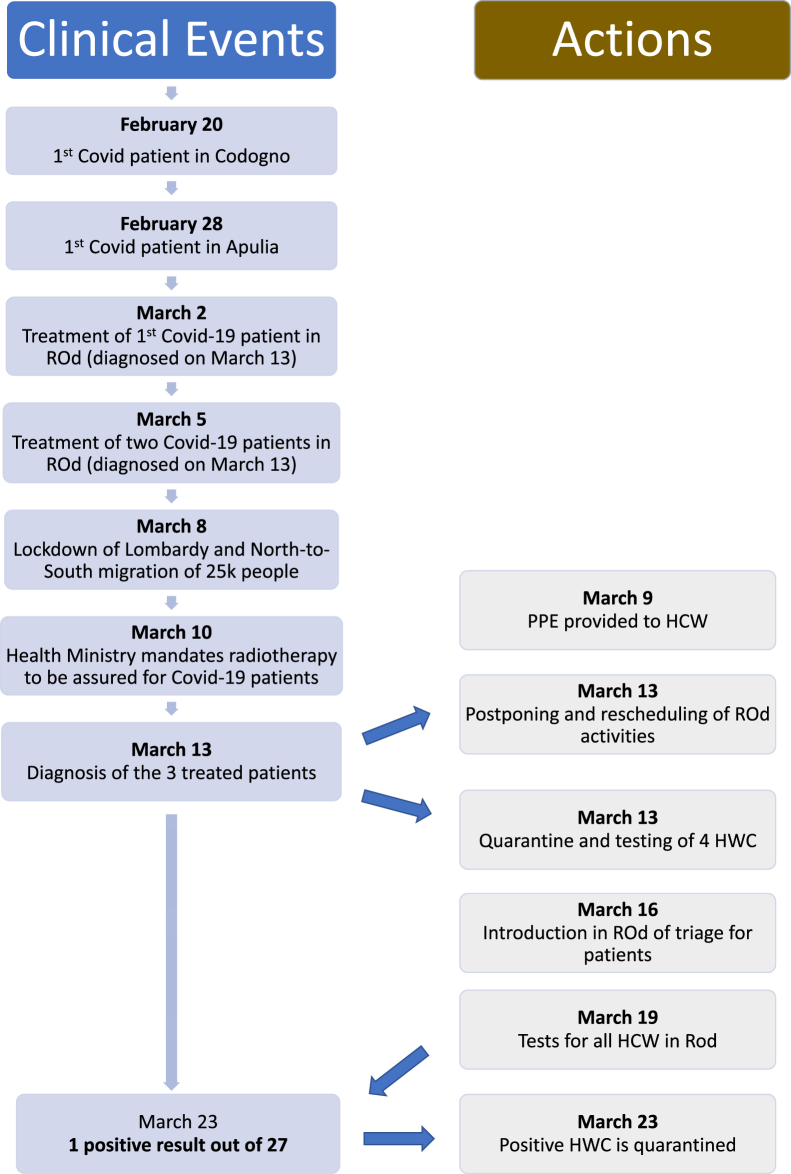
As mentioned, 1 nurse tested positive to COVID-19. According to the previously mentioned rules, there is no forecast of new tests in HCWs without symptoms. Consequently, in our scheduling, postoperative treatments—mostly favorable postoperative breast cancers and prostate cancer under hormone deprivation or with postoperative indication—have been postponed by 2 weeks. We will keep monitoring the effect of COVID-19 on our services (Fig 1).
Figure 1.
Flow chart of clinical events and actions. Abbreviations: HCW = health care worker; ROd = radiation oncology department.
We have registered good compliance with the new rules. Some elderly patients have asked to delay treatment, most likely because mortality for COVID-19 in Italy is higher for people aged 80 and older. We have observed that it is difficult for many patients to complete tumor staging on an outpatient basis because of the restriction of ordinary health procedures. At this time, many wards are being closed and changed into COVID-19 wards, so many surgical operations have been delayed despite the law requiring that they take place.
Concluding Remarks
Although radiation therapy is an activity formally guaranteed by authorities during the pandemic, it is likely that many patients will suffer a real shortage of access to diagnostic and therapeutic procedures, interrupting and postponing their treatment. We expect poorer outcomes for these patients in the near future. We also observed that a delay in providing PPE for medical personnel reduced the available staff, further affecting treatment schedules.
In the controversial debate on whether people are dying with COVID-19 or due to COVID-19, there is probably a forgotten category: patients without COVID-19 who will still die due to COVID-19 and specifically because of the shortage of resources or delays in treatments it is causing.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: none
References
- 1.Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) https://coronavirus.jhu.edu/map.html Available at: Accessed March 20, 2020.
- 2.Ghebreyesus T.A. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020 Available at: Accessed March 20, 2020.
- 3.Rosenbaum L. Facing Covid-19 in Italy — Ethics, logistics, and therapeutics on the epidemic’s front line [epub ahead of print]. N Engl J Med.https://doi.org/10.1056/NEJMp2005492. Accessed March 23, 2020. [DOI] [PubMed]
- 4.Filippi AR, Russi E, Magrini SM, Corvò R. Covid-19 outbreak in northern Italy; first practical indications for radiotherapy departments [epub ahead of print]. Int J Radiat Oncol Biol Phys. 10.1016/j.ijrobp.2020.03.0074. Accessed March 19, 2020. [DOI] [PMC free article] [PubMed]
- 5.Krengli M, Ferrara E, Mastroleo F, Brambilla M, Ricardi U. Running a radiation oncology department at the time of coronavirus: An Italian experience [epub ahead of print]. Adv Radiat Oncol. 10.1016/j.adro.2020.03.003. Accessed March 20, 2020. [DOI] [PMC free article] [PubMed]
- 6.Ministero della Salute Rapporto annual sull’attività di ricovero. Dati SDO 2017. Direzione Generale Programmazione Sanitaria.Gennaio 2019. http://www.salute.gov.it/imgs/C_17_pubblicazioni_2831_allegato.pdf Available at: Accessed March 20, 2020.
- 7.DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 8 marzo 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19. Gazzetta Ufficiale della Repubblica Italiana. N.59 8 marzo 2020. Available at: https://www.gazzettaufficiale.it/eli/id/2020/03/08/20A01522/sg. Accessed March 20, 2020.
- 8.DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 9 marzo 2020 Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell'emergenza epidemiologica da COVID-19, applicabili sull'intero territorio nazionale. Gazzetta Ufficiale n. 62 del 9 marzo 2020. Available at: https://www.gazzettaufficiale.it/eli/id/2020/04/27/20A02352/sg. Accessed March 20, 2020.
- 9.DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 11 marzo 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di con- tenimento e gestione dell’emergenza epidemiologica da COVID-19, applicabili sull’intero territorio nazionale. Gazzetta Ufficiale della Repubblica Italiana. N.64 11 marzo 2020. Available at: https://www.gazzettaufficiale.it/eli/id/2020/03/11/20A01605/sg. Accessed March 20, 2020.
- 10.World Health Organization. Advice on the use of masks in the community, during home care and in healthcare settings in the context of the novel coronavirus (2019-nCoV) outbreak: interim guidance. Available at: https://apps.who.int/iris/handle/10665/330987. Accessed January 29, 2020.
- 11.DECRETO-LEGGE 9 marzo 2020, n. 14 Disposizioni urgenti per il potenziamento del Servizio sanitario nazionale in relazione all'emergenza COVID-19. Gazzetta Ufficiale della Repubblica Italiana. N.62 9 marzo 2020. Available at: https://www.gazzettaufficiale.it/eli/id/2020/03/09/20G00030/sg. Accessed March 20, 2020.
- 12.Regione Puglia Misure per la prevenzione e gestione dell’emergenza epidemiologica da COVID-19 –DISPOSIZIONI. 8 marzo 2020. Available at: https://www.regione.puglia.it/documents/56205/215284/Ordinanza+del+Presidente+della+Regione+Puglia+del+8+marzo+2020.pdf/82a98af0-b9ff-8398-e69f-d66e3e5c8ecd?t=1585818245821. Accessed March 20, 2020.
- 13.Regione Puglia Emergenza sanitaria COVID-19 – Protocolli operativi e flow chart DISPOSIZIONI 13 marzo 2020. Available at: https://fimmg.bari.it/documenti/BQG70_1.pdf. Accessed March 20, 2020.
- 14.Ministero della Salute Raccomandazioni per la gestione dei pazienti oncologici e oncoematologici in corso di emergenza da COVID-19. 0007023-10/03/2020-DGPROGS-MDS-P. http://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2020&codLeg=7363 5&parte=1%20&serie=null Available at: Accessed March 20, 2020.
- 15.Associazione Italiana di Radioterapia Oncologica. Documento di indirizzo per la valutazione e la gestione del rischio dei pazienti e degli operatori nei reparti di radioterapia oncologica in corso di diffusione del COVID-19. Available at: https://www.radioterapiaitalia.it/wp-content/uploads/2020/03/v-2-Documento-AIRO-COVID-19-24-03-2020.pdf. Accessed March 24, 2020.
- 16.L’ospedale Perrino si affida a Plusimple. Available at: https://about.plusimple.com/ospedale-perrino-plusimple/. Accessed April 17, 2020.