Abstract
Quality of life (QOL) has been considered as an important outcome indicator in holistic care for HIV-infected people, especially as HIV/AIDS transforms from a fatal illness to a chronic condition. This study aimed to identify trends and emerging topics among research concerning the QOL of people living with HIV/AIDS (PLWHA). The analyzed data were English papers published from 1996 to 2017, searched and extracted from the Web of Science Core Collection. Collaborations between countries and the correlation between the keywords were visualized by VOSviewer while the abstracts’ content was analyzed using exploratory factor analysis and Jaccard’s’ similarity index. There has been an increase in both the number of publications and citations. The United Nations of America leads in terms of paper volume. The cross-nation collaborations are mainly regional. Despite a rather comprehensive coverage of topics relating to QOL in PLWHA, there has evidently been a lack of studies focusing on socio-cultural factors and their impacts on the QOL of those who are HIV-infected. Further studies should consider investigating the role of socio-cultural factors, especially where long-term treatment is involved. Policy-level decisions are recommended to be made based on the consideration of cultural factors, while collaborations between developed and developing nations, in particular in HIV/AIDS-ridden countries, are strongly recommended.
Keywords: scientometrics, HIV/AIDS, bibliometric, quality of life
1. Introduction
Human immunodeficiency viruses (HIV) is one of the leading causes of disability and mortality worldwide, with more than 76.1 infected people and 35.0 million deaths [1,2,3]. In 2017, there were 1.8 million people newly infected with HIV and Acquired immunodeficiency syndrome (AIDS), 36.9 million people living with HIV and AIDS (PLWHA), and 940,000 deaths related to life-threatening infections and cancers [4]. Hence, ensuring sufficient care and treatment, as well as treatment provision, has become a challenge for global public health systems.
Quality of life (QOL), as noted by the existing literature, has been described as an umbrella term for a variety of human needs, including the position in life, goals, standards, expectations, and concerns in the context of the culture and value systems. It manifests within patients as symptomatic, social functioning, and spirituality [5]. In terms of health promotion, health-related quality of life (HRQOL) is also considered as a priority health indicator. Since 1996, optimizing adherence to Antiretroviral Therapy (ART) has brought the chance to transform HIV—an incurable disease—into a chronic health condition [6], which in turn prolongs the life of PLWHA and improves their QOL [6]. In many settings, poor QOL is associated with a lower immune response, non-adherence, poor mental health, and greater disease severity [7,8,9]. Therefore, QOL attracted great attention from regulatory authorities and health providers as an important outcome to evaluate the effectiveness of HIV treatment [10,11,12,13]. People who were effectively treated with HAART, however, have been found to have a lower QOL compared with other long-term chronic illnesses [14]. Over time, the expansion of HAART coverage not only prolonged the life expectancy of PLWHA, but also boosted the innovation of new QOL instruments to adapt to the complexity of care. The previous literature has reported a high burden of comorbidities suffered by PLWHA, as well as adverse side impacts of long-term treatment on their health [15,16], while a complex combination of psychological and social factors which also influence their physical, mental and social conditions, directly and indirectly, affect their QOL [17,18,19,20,21,22]. On the other hand, in recent years, the availability of early HIV diagnosis, antiretroviral (ARV) treatments and enhanced healthcare services have been found to support the improvement in the QOL of PLWHA [23].
Thus, in order to improve the quality and effectiveness of HIV/AIDS treatment and prevention programs, qualitative as well as quantitative analyses on the QOL of PLWHA are needed. In 2017, Cooper, et al. conducted a systematic review on the finding of existing reviews on QOL of the HIV/AIDS-infected population in various aspects, including the development, validation, and effectiveness of the most commonly used instruments [12]. Though informative, reviews of such kind suffer from the limitation of a narrow focus on specific questions or issues. In order to broaden the scope of research, a new approach is needed that has the ability to cover a large volume of global data on QOL in PWLHA research and allows for complex analysis to identify the research trend [12,18,24,25].
Our study adopts the scientometrics approach that gathers and analyze publications on a global level, coupled with more a technical analysis approach applied to the content of papers’ title and abstract to identify emerging research topics as well as the current level of international collaboration in research on the QOL of PLWHA. This study aims to supplement the current literature while uncovering research gaps, suggest directions for future studies, and act as a reference point for priority settings and strategies initiating in HIV/AIDS management.
2. Materials and Methods
2.1. Study Design
Serving as the best approach to evaluate evidence, the increase in the number of systematic reviews of QOL regarding HIV/AIDS could provide an insightful view of various aspects, including evaluating the effectiveness of instruments, clinical intervention, and HIV/AIDS programs in vulnerable populations. In addition to having a limited scope of research; such reviews also remain lack of the comparison of findings over time and overlap with information. Several researchers use bibliometrics with the expectation that it could fill the gap in the literature and provide the research trend using quantitative analysis. It can be seen that the bibliometric approach sometimes could not draw a full picture because the majority only present the number without a comprehensive reading of the literature [26]. In order to provide a comprehensive view of the current status of the quality of life in terms of the HIV/AIDS literature, we conducted the scientometric approach combined with content analysis.
The current study is a part of a larger project, Global Analysis for Policy in Research (GAPRESEARCH), that aims to set priorities in global health evolution and provide empirical evidence for designing effective interventions and policies [27,28,29,30,31,32]. The findings of this study, therefore, can be used as a reference point for directing investments, allocating resources, and crafting policies.
2.2. Search Strategy
A search for HIV/AIDS publications was performed on the Web of Science (WoS) Core Collection. This database was prioritized because it has covered all scientific publications with full cited reference indexing since 1900 and allowed downloading information with a diversity of research disciplines that far outweigh other databases such as Scopus or MEDLINE [32].
We applied a search query containing the search terms of “HIV” OR “human-immunodeficiency-virus” OR “AIDS” OR “Acquired-Immune-Deficiency-Syndrome”. Data were extracted in a unit of 500 publications from the first publication in the dataset end up in 2017. As the process was conducted in July 2018, we excluded all papers published in 2018 as the partial coverage of publications published in 2018 would not fully reflect the publication trend of the year. The selection criteria for study subjects were English peer-review articles, including original articles and reviews (see Figure A1). Any paper with anonymous or no authors would be excluded. In the next step, we continue refined relevant research by using the research term “quality of life”, articles could be removed if they did not include “quality of life” in titles and abstracts. Any disagreement during the screening process could be discussed with a senior researcher.
2.3. Summary Measures
The retrieved data consisting mainly of publication indexes were contained the following information: Title; years of publication; the total number of papers; citations up to 2017; usages/number of downloads; keywords (authors’ keywords); authors’ affiliations; most prolific countries and collaborations. In order to describe the change of publication over time, we calculated several fundamental domains including the speed of publication (total number of papers), the level of reader attention (mean cited rate per year), the level of short-term and long-term interest (mean usage rate last 6 months/5 years). We also illustrated the major topic clusters and landscapes of QOL in the field of HIV/AIDS by calculating the frequency of co-occurrence of keywords and synthesized from abstract’s content.
2.4. Data Analysis
The extracted data were sorted by Macro in Microsoft Excel to calculate the indexes. The connection among countries by sharing co-authorships’ data (we applied full counting for papers sharing by more than one country), networks of co-occurrence authors’ keywords, and clusters of topic groups were visualized by VOSviewer (version 1.6.11, Center for Science and Technology, Leiden University, the Netherlands). The cluster topics of QO were then identified from the frequency of keywords and named by expert opinions.
The exploratory factor analysis (EFA) and Jaccard’s similarity index were performed using STATA software version 15.0. This index was defined as the magnitude of the intersection divided by the magnitude of the union of two sets of co-occurring terms; thus, multi-dimensional scaling could be used to adjust a point for a topic category, the distance between items and color presented the partnership of certain key terms. To measure the likelihood of research trends (e.g., emerging research domains and landscapes), we utilized exploratory factor analysis (EFA), which allows us to test the variance in the domains and landscape appearing from the abstract’s contents. The summary of the technique used for analyzing is described in Table A1.
3. Results
Table 1 shows an expansion in the volume of publications on QOL among HIV/AIDS populations. The period between 2007 and 2017 saw the number of papers grow from 114 to 234. In particular, the total citation (from the year published up to 2017) has also risen remarkably in 2005 and 2013.
Table 1.
General indicators of publications
| Year Published | Total Number of Papers | Total Citations | Mean Cite Rate per Year 1 | Total Usage* Last 6 Months | Total Usage* Last 5 Years | Mean Use Rate Last 6 Months 2 | Mean Use Rate Last 5 Years 3 |
|---|---|---|---|---|---|---|---|
| 2017 | 234 | 11,965 | 51.1 | 356 | 1,151 | 1.5 | 1.0 |
| 2016 | 215 | 11,221 | 26.1 | 211 | 1,619 | 1.0 | 1.5 |
| 2015 | 218 | 10,985 | 16.8 | 174 | 1,972 | 0.8 | 1.8 |
| 2014 | 211 | 9,638 | 11.4 | 107 | 1,891 | 0.5 | 1.8 |
| 2013 | 213 | 9,866 | 9.3 | 96 | 2,286 | 0.5 | 2.1 |
| 2012 | 185 | 8,773 | 7.9 | 52 | 1,692 | 0.3 | 1.8 |
| 2011 | 169 | 8,476 | 7.2 | 65 | 1,315 | 0.4 | 1.6 |
| 2010 | 167 | 7,462 | 5.6 | 46 | 1,160 | 0.3 | 1.4 |
| 2009 | 140 | 6,445 | 5.1 | 62 | 908 | 0.4 | 1.3 |
| 2008 | 122 | 5,468 | 4.5 | 53 | 818 | 0.4 | 1.3 |
| 2007 | 114 | 5,639 | 4.5 | 33 | 622 | 0.3 | 1.1 |
| 2006 | 96 | 4,588 | 4.0 | 41 | 606 | 0.4 | 1.3 |
| 2005 | 112 | 5,265 | 3.6 | 61 | 767 | 0.5 | 1.4 |
| 2004 | 80 | 3,746 | 3.3 | 36 | 414 | 0.4 | 1.0 |
| 2003 | 73 | 3,012 | 2.8 | 25 | 374 | 0.3 | 1.0 |
| 2002 | 58 | 2,579 | 2.8 | 10 | 226 | 0.2 | 0.8 |
| 2001 | 51 | 2,163 | 2.5 | 11 | 264 | 0.2 | 1.0 |
| 2000 | 66 | 2,759 | 2.3 | 11 | 309 | 0.2 | 0.9 |
| 1999 | 49 | 2,291 | 2.5 | 13 | 212 | 0.3 | 0.9 |
| 1998 | 56 | 2,385 | 2.1 | 16 | 214 | 0.3 | 0.8 |
| 1997 | 39 | 1,708 | 2.1 | 7 | 128 | 0.2 | 0.7 |
| 1996 | 44 | 1,455 | 1.5 | 11 | 169 | 0.3 | 0.8 |
* Usage: downloaded time; 1 Mean cited rate per year = Total citations/(Total citations × (2018-that year)); 2 Mean usage rate last 6 months = Total usage last 6 months/Total number of papers; 3 Mean use rate last 5 years = total usage last 5 years/(total number of papers × 5).
Table 2 indicates the frequency of countries by counting such study settings in the mentioned abstracts. In the top 10, except countries with the highest HIV prevalence, such as South Africa, the number of studies were mostly produced in upper-middle-income and high-income countries (United States, Brazil, China, Canada, Thailand, England, Australia) [33]. The low and middle-income countries such as Botswana, Zambia, Lesotho, Swaziland had below 10 papers, even though these countries have been reported as having the highest rate of HIV/AIDS [34].
Table 2.
A number of papers by countries as study settings.
| No. | Country Settings | Frequency | % | No. | Country Settings | Frequency | % |
|---|---|---|---|---|---|---|---|
| 1 | United States | 271 | 21.1% | 31 | Sweden | 8 | 0.6% |
| 2 | South Africa | 108 | 8.4% | 32 | Zambia | 8 | 0.6% |
| 3 | India | 74 | 5.8% | 33 | Cambodia | 7 | 0.5% |
| 4 | Brazil | 60 | 4.7% | 34 | Ghana | 7 | 0.5% |
| 5 | China | 60 | 4.7% | 35 | Lesotho | 7 | 0.5% |
| 6 | Uganda | 52 | 4.0% | 36 | Netherlands | 7 | 0.5% |
| 7 | Canada | 42 | 3.3% | 37 | Swaziland | 7 | 0.5% |
| 8 | Thailand | 32 | 2.5% | 38 | Switzerland | 7 | 0.5% |
| 9 | United Kingdom | 30 | 2.3% | 39 | Hong Kong | 6 | 0.5% |
| 10 | Australia | 29 | 2.3% | 40 | Jamaica | 6 | 0.5% |
| 11 | Ethiopia | 27 | 2.1% | 41 | Japan | 6 | 0.5% |
| 12 | Niger | 25 | 1.9% | 42 | Nepal | 6 | 0.5% |
| 13 | Nigeria | 25 | 1.9% | 43 | Germany | 5 | 0.4% |
| 14 | Malawi | 21 | 1.6% | 44 | Mexico | 5 | 0.4% |
| 15 | Viet Nam | 20 | 1.6% | 45 | Peru | 5 | 0.4% |
| 16 | Ireland | 19 | 1.5% | 46 | Wallis and Futuna | 5 | 0.4% |
| 17 | Taiwan | 18 | 1.4% | 47 | Colombia | 4 | 0.3% |
| 18 | Rwanda | 17 | 1.3% | 48 | Georgia | 4 | 0.3% |
| 19 | Kenya | 15 | 1.2% | 49 | Haiti | 4 | 0.3% |
| 20 | Iran | 14 | 1.1% | 50 | Jersey | 4 | 0.3% |
| 21 | Spain | 14 | 1.1% | 51 | Portugal | 4 | 0.3% |
| 22 | Tanzania | 14 | 1.1% | 52 | Romania | 4 | 0.3% |
| 23 | Zimbabwe | 14 | 1.1% | 53 | Singapore | 4 | 0.3% |
| 24 | Malaysia | 13 | 1.0% | 54 | Burkina Faso | 3 | 0.2% |
| 25 | Cameroon | 12 | 0.9% | 55 | Democratic Republic of the Congo | 3 | 0.2% |
| 26 | Italy | 12 | 0.9% | 56 | Republic of the Congo | 3 | 0.2% |
| 27 | France | 11 | 0.9% | 57 | Finland | 3 | 0.2% |
| 28 | Botswana | 9 | 0.7% | 58 | Guinea | 3 | 0.2% |
| 29 | Indonesia | 9 | 0.7% | 59 | Lebanon | 3 | 0.2% |
| 30 | Puerto Rico | 8 | 0.6% | 60 | Mali | 3 | 0.2% |
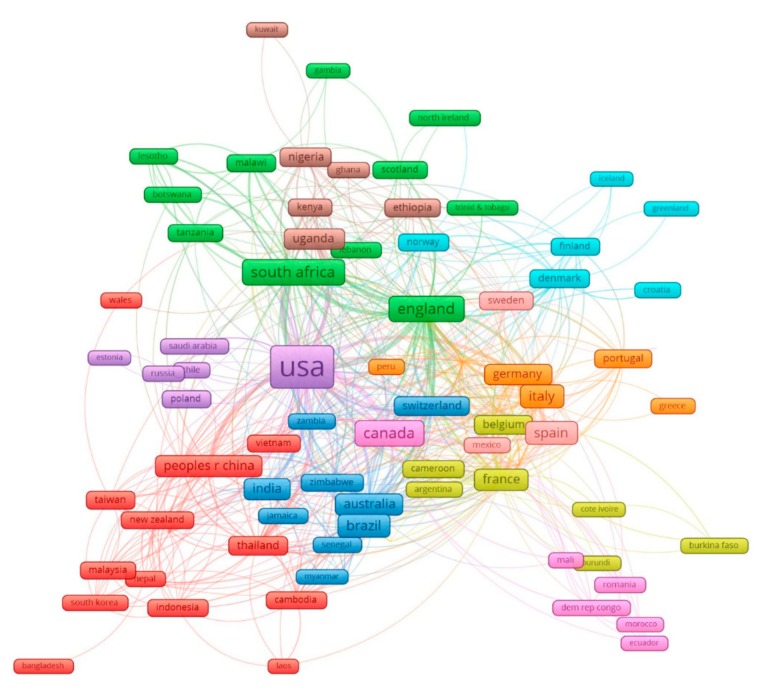
Figure 1 displays the global network between 102 countries having co-authorships of selected papers. These countries have been classified into 10 clusters of at least five countries, depending on their level of international collaboration.
Figure 1.
The network of 102 countries having international co-authorships in quality of life research in HIV/AIDS.
Cluster 1 (red) refers to the network of countries in the two regions: South-East Asia and the Western Pacific. Cluster 2 (purple) indicates the link of the USA with European countries and Saudi Arabia. Cluster 3 (blue) illustrates international collaborations between the Americas, South Africa, and some countries in Asia. Cluster 4 (brown and green) demonstrates the co-authorship between countries within Southeast Africa. In addition, they have an additional link with England. The European countries tend to associate with each other by geographical areas, such as orange, pink, light blue, and yellow (French West Africa).
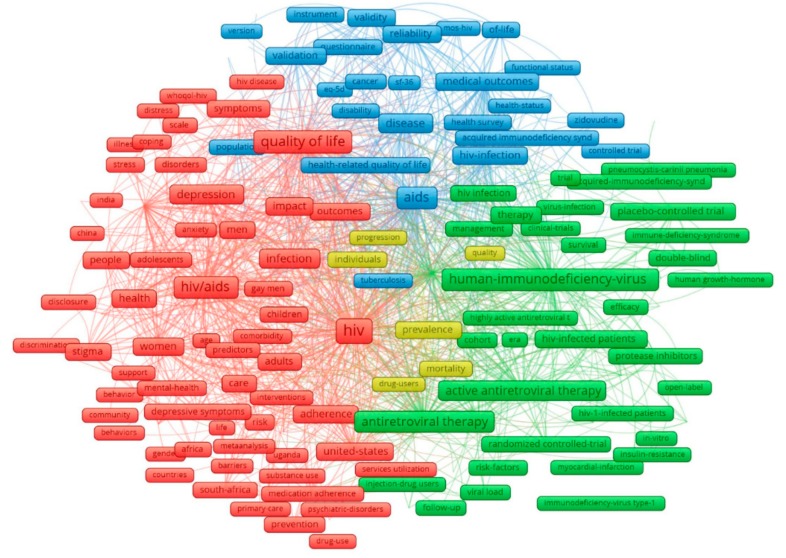
Figure 2 describes the core components of the keywords with the most common groups of terms. There were four major clusters that emerged from 205 most frequent co-occurrence keywords with a minimum frequency of 20 times. Three major clusters (red, blue, and green) indicate three topics of quality of life.
Figure 2.
The most common author keywords. Note: the principal components of the data structure were visualized regarding the colors of the nodes; the node size was identified by the keywords’ occurrences; the closer the nodes are, the stronger the association between two keywords are.
Cluster 1 (red) covers mental health, social, and associated factors. It includes psychological disorders (depression, anxiety, stress); social behavior (stigma, discrimination); specific HIV groups (such as gay, children, women, and men), and regions (India, South Africa, Uganda). Cluster 2 (blue) presents physical health-related aspects: treatment, outcome, mortality, and disability. Cluster 3 (green) indicates ART adherence studies: study design and laboratory results.
The top 50 emerging research domains have been discovered from the content analysis of abstracts using exploratory factor analysis (Table 3). Mental health (62.6% of papers containing mental health-related keywords) appears to receive more attention from researchers compared to other health problems (e.g., chronic conditions 23.4%, or cost-effectiveness 37.5%). Other major domains cover coping strategies and social support. Nearly half of the articles have keywords related to the randomized and controlled trial. Meanwhile, the keywords concern comorbidities account for less than 10%.
Table 3.
Top 50 research domains emerged from exploratory factor analysis of all abstracts’ contents.
| Name | Keywords | Eigen Value | FREQ | % Cases |
|---|---|---|---|---|
| Mental health summary | Medical Outcomes Study (MOS); summary; mental; survey; physical; scores; medical; score; health related quality of life (HRQOL); outcomes; short form (SF) | 26.1 | 4123 | 62.60% |
| Criteria; controlled trials | Criteria; trials; objectives; controlled; main; evidence; performed; review; evaluate | 1.9 | 2357 | 48.90% |
| The World Health Organization Quality of Life brief (WHOQOL-BREF); Domain |
WHOQOL; BREF; Domain; domains; world; version; QOL; psychological; social | 3.3 | 2335 | 44.20% |
| Randomized; Controlled trial | Randomized; trial; placebo; controlled; weeks; week; groups; primary; intervention | 7.2 | 2312 | 39.30% |
| Cost-effectiveness; costs | Cost; costs; effectiveness; effective; economic; model; year | 1.9 | 1643 | 37.50% |
| Coping strategies; social support | Coping; strategies; support; social | 1.3 | 1522 | 37.10% |
| Depressive; anxiety and depression | Depressive; depression; symptoms; anxiety; psychiatric; psychological | 2.7 | 1722 | 36.10% |
| Reliability and validity; item scale | Validity; reliability; item; items; instrument; factor; scales; measure; good; scale | 2.2 | 1923 | 36.10% |
| Care access | Access; services; care | 1.3 | 1220 | 33.40% |
| Role functioning | Role; function; cognitive; functioning | 1.5 | 1025 | 27.30% |
| Viral load; count | Load; viral; count; counts; cells | 1.8 | 1384 | 27.00% |
| Literature; review | Literature; review; evidence | 5 | 919 | 24.10% |
| Sex; men and women | Sexual; men; sex; women | 1.8 | 1002 | 23.90% |
| Chronic conditions | Conditions; chronic; diseases | 1.6 | 840 | 23.40% |
| Stigma; disclosure | Stigma; disclosure; perceived; negative | 3.7 | 837 | 23.20% |
| Cross-sectional | Sectional; cross; prevalence | 2.5 | 1128 | 23.00% |
| Side effects | Side; effects | 1.5 | 815 | 22.80% |
| Follow-up period | Period; follow; month; year | 2.3 | 852 | 22.50% |
| Body mass; fat loss | Mass; body; fat; weight; kg; loss; nutritional; exercise; testosterone; index | 3.3 | 1169 | 21.40% |
| Drug users | Users; methadone; drug; substance | 2.3 | 766 | 21.00% |
| Outcome measures | Outcome; measures | 1.3 | 718 | 20.60% |
| Control | Controls; control; intervention | 1.7 | 712 | 20.10% |
| Anti; development | Anti; development; resistance; therapeutic | 1.2 | 712 | 19.70% |
| Palliative; cancer pain | Palliative; cancer; advanced; pain | 1.9 | 620 | 18.20% |
| Adherence to medication | Medication; adherence | 1.6 | 639 | 18.10% |
| Developed countries | Countries; developed; settings | 1.2 | 600 | 18.00% |
| Screening; early | Screening; early; settings | 1.2 | 500 | 15.50% |
| Combination | Combination; response | 1.3 | 416 | 13.50% |
| Demographic | Demographic; characteristics | 1.5 | 456 | 13.40% |
| Children | Children; adoslescents; caregivers; family | 1.7 | 499 | 13.30% |
| EuroQOL (EQ); HRQOL demension | EQ; HRQOL; Dimensions | 1.6 | 445 | 13.30% |
| Reduction | Reduction; improvement | 1.4 | 407 | 13.10% |
| Morbidity and mortality | Mortality; morbidity | 1.7 | 497 | 12.60% |
| Inhibitor; protease inhibitor (PI) regimens | Inhibitor; PI; regimen; regimens | 3.1 | 498 | 12.20% |
| Death | Death; hospital | 1.3 | 357 | 12.00% |
| Emotional | Emotional; functional | 1.3 | 358 | 11.80% |
| Exercise | Exercise; activity; week | 1.3 | 374 | 11.70% |
| Moderate to severe | Severe; moderate; haemophilia | 1.5 | 390 | 11.70% |
| Long-term | Term; long | 2.1 | 522 | 11.20% |
| Adverse effect | Events; adverse | 1.4 | 426 | 11.20% |
| Cytomegalovirus (CMV); Prophylaxis | CMV; prophylaxis; infections | 1.4 | 348 | 10.80% |
| South Africa | South; Africa | 2 | 344 | 8.60% |
| Food | Food; people living with HIV (PLHIV); nutritional | 1.3 | 225 | 6.90% |
| Facial | Facial; satisfaction | 1.3 | 177 | 5.90% |
| Hepatitis | Hepatitis; hepatitis C virus (HCV) | 1.9 | 215 | 5.60% |
| Sleep | Sleep; fatigue | 1.4 | 155 | 4.80% |
| Failure | Failure | 1.4 | 120 | 4.30% |
| Anemia | Anemia | 1.4 | 49 | 1.70% |
| Diarrhea | Diarrhea | 1.5 | 44 | 1.60% |
| Tuberculosis (TB) | TB | 1.4 | 38 | 1.40% |
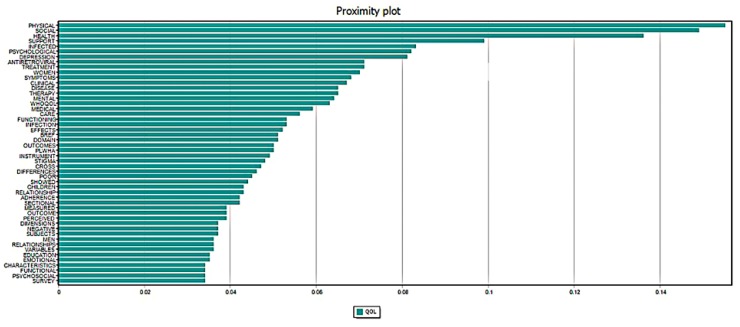
Figure 3 illustrates the similarity between QOL and the top 50 co-occurrence terms. In particular, physical, social, and health were the most common terms that co-occurred with QOL in all abstracts. The term related to women was more common than that of men in the literature. Antiretroviral, treatment, and infection were also co-occurrence terms with a high frequency of appearance.
Figure 3.
Proximity Plots of “quality of life” with the top 50 most frequent concurrence terms in abstracts.
4. Discussion
By analyzing the volume and abstract contents of global publications on the QOL of PLWHA during 1996–2017, our research captured and visualized the level of attention, current research trends, and the global networking of researches. The results show rather extensive coverage of topics in the existing literature, ranging from physical-related aspects to mental health, from issues concerning clinical trials to social support. Nonetheless, the current bibliography shows the lack of socio-cultural factors involved in the development and measurement of QOL.
Our study reports an increase in the number of papers using QOL as an important instrument for evaluating HIV/AIDS interventions since 1996, when highly active antiretroviral therapy (HAART) was first introduced [6]. This result is in line with a study conducted by Eltony et al., which confirmed an increasing trend in the volume of publications on QOL of PLWHA [35]. On the other hand, our findings draw a troubling picture regarding the degree of inequality in contributions and collaborative partnerships across settings. While most HIV incidence is located in LMICs, for instance, nearly 70% of individuals infected with HIV live in Sub-Saharan Africa [36], the highest amount of relevant studies belonged to high-income countries. It is widely acknowledged that the combination of low socioeconomic conditions and limited access to health services result in increasing HIV prevalence in sub-Saharan Africa, the Caribbean, and Central Asia [37]. Therefore, these countries may be more focused on the prevention of HIV transmission rather than investing interventions to improve mental health or social situation, for instance, to reduce stigma against HIV patients when accessing general health facilities. The reduction in global funds for HIV—the major source of financing for HIV/AIDS management in LMICs—would also lead to a lack of funding for the crucial activities of collecting empirical data, planning essential investigations, and HIV/AIDS management strategies [38]. Meanwhile, cross-regional collaborations, and especially research partnerships between high-income countries and their low-middle-income counterparts, have been found to still be rather limited (Figure 1). These findings call for more collaboration efforts between developed and developing nations, in which support both in terms of finance and knowledge/ technology should be transferred from advanced to disadvantaged regions. In addition, further research in favor of economic evaluation should be conducted to identify the appropriate interventions in the context of limited funding for HIV/AIDS management.
Knowing the association between the QOL of PLWHA and the effectiveness of HIV programs, QOL has been used as a criteria in assessing HIV/AIDS prevention programs, clinical treatment, and harm reduction strategies [39,40,41]. This is reflected in the finding of our study, as terms relating to QOL measurements like MOS-HIV, EQ-5D, SF-36, and WHOQOL-HIV are found to frequently co-occur with QOL in analyzed publications (Figure 2), while the EFA of abstract content identifies QOL measurements to be an emerging research domain (Table 3). EQ-5D and SF-36 have been broadly used thanks to their ability to be adopted for economic analyses. Meanwhile, MOS-HIV and WHOQOL-HIV have been developed and validated as QOL measurements specifically for the HIV/AIDS-infected population [42,43,44,45,46].
Even with the advancement of health services as well as the high ART coverage, the HIV/AIDS programs remain complex, contextual, and are often referred to as complicated because appropriate recommendations vary according to subpopulation and epidemiological context [23]. Previous studies have reported that in LMIC, a combination of factors, instead only one or two major ones, have major impacts on optimal adherence and rates of virological suppression when a patient is lost to follow-up [23]. The combined language and ethnicity profile of a country has been found to significantly influence culturally sensitive healthcare services—those at risk of HIV infection may face delayed treatment initiation and access to prevention services in regions where stigma against infectious diseases is common, for instance [47]. Some of the most HIV/AIDS-ridden nations in North-Central Africa, such as Cameroon, Nigeria, and the Democratic Republic of the Congo, have been found to also be the most culturally diverse countries [48]. The absence of culture-related terms like language, belief and religion in the keywords and abstract content of our analyzed publications suggest a gap in the research concerning the QoL of PLWHA. Further studies thus may consider assessing the role of cultural factors on QoL of PLWHA, as well as the impacts of diverse beliefs, for instance, on the effectiveness of the programs initiated to improve the QoL of those infected with HIV. Similarly, those involved in developing HIV/AIDS management programs, including policy-makers and non-governmental organizations, should take into account the impact of cultural factors.
The analysis of a principal component of terms in titles and abstracts reveals that QOL tends to co-occur with terms relating to mental disorders and high-risk populations, including adolescents, children, women, and gay. Disclosure, discrimination, and stigma have also been found to appear together with the aforementioned terms, along with keywords like barriers and primary care (Figure 2). This finding suggests that topics on the mental health consequences of HIV infection and its treatments, barriers to treatment due to stigmatization and social-related issues like reluctance to disclosure have been covered in the existing literature. The focus on single domains of QOL, such as physical [14,49,50], psychological [49,51,52,53], social [50,52,53,54], and environmental [55,56] can be said to be common in research concerning QOL among PLWHA. However, given the complex, multi-dimensional nature of the QOL construct, the lack of contextualized factors (sociological perspective, culture, religion for instance) in the titles and abstracts of published papers, as our results reveal, can undermine the power and scope of impact of QOL on PLWHA and the effectiveness of treatments. Therefore, further studies are encouraged to address more contextualized factors and consider adopting multiple QOL measures when attempting to evaluate the association and influence of QOL on PLWHA.
Despite the positive findings of the study, several limitations should be mentioned. As our search strategy was conducted via Web of Science Core Collection solely and only English reviews and articles were included, despite the extensive coverage of WoS and the dominance of English publications, there is a chance that relevant publications not recorded in such a database and/or in other languages would be missed. Our decision to use only the term “quality of life” when conducting a publication search would also filter out possibly related papers where variations of the construct such as “satisfaction with life”, “well-being”; “satisfaction” or “value of life” were used instead. Thus, further researches are strongly encouraged to consider investigating deviations of “quality of life” both as a term and a concept, especially research with a sociological focus. In addition, future studies may also be conducted in the form of systematic reviews and meta-analyses, for instance, on how QOL can or has been used as a measurement for assessing the effectiveness of HIV/AIDS treatments or interventions.
5. Conclusions
Using bibliometrics analysis, we illustrate the development and current global trends of research on the QOL of PLWHA. Meanwhile, the results of the text mining techniques adopted provide a picture of current emerging research trends and topics and highlight research gaps. Despite a rather comprehensive coverage of topics relating to QOL in PLWHA, there has evidently been a lack of studies focusing on socio-cultural factors and their impacts on the QOL of those that are HIV-infected. Further studies should consider investigating the role of socio-cultural factors, especially where long-term treatment is involved. Policy-level decisions are recommended to be made based on the consideration of cultural factors, while collaborations between developed and developing nations, in particular with HIV/AIDS-ridden countries, are strongly recommended.
Acknowledgments
Not applicable.
Appendix A
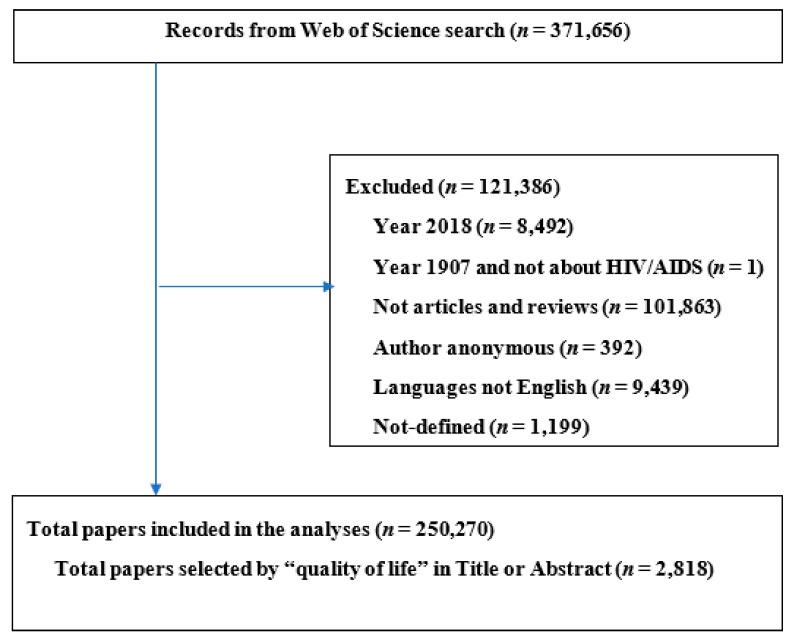
Figure A1.
Selection of papers. The searching and paper selection process identified 250,270 related to HIV/AIDS. Among those, 2818 papers included the terms “quality of life”.
Table A1.
Summary of the techniques and methods.
| Type of Data | Unit of Analysis | Analytical Methods | Presentations of Results |
|---|---|---|---|
| Abstracts Keywords |
Words | Frequency of co-occurrence | 1. The number of articles by countries mentioned in the abstract 2. Networks of co-occurrence authors’ keywords 3. Networks of countries by sharing co-authorships data |
| Abstracts | WoS research domains | Exploratory factor analysis | 1. Top 50 research domains |
| Abstracts | Words | Jaccard’s similarity index | 1. Top 50 most frequent co-occurrence terms |
Author Contributions
Conceptualization, G.T.V., C.L.H., H.T.P., G.H.H. and R.C.M.H.; Data curation, B.J.H., H.T.P. and C.A.L.; Formal analysis, B.X.T., C.L.H., B.J.H. and H.T.P.; Funding acquisition, C.S.H.H. and G.H.H.; Investigation, B.X.T., B.J.H. and C.A.L.; Methodology, B.X.T., C.L.H., C.S.H.H. and G.H.H.; Project administration, G.T.V. and R.C.M.H.; Software, C.A.L. and G.H.H.; Supervision, G.T.V. and R.C.M.H.; Validation, C.S.H.H. and R.C.M.H.; Visualization, C.S.H.H.; Writing—original draft, G.T.V.; Writing—review and editing, G.T.V., B.X.T., C.L.H., B.J.H., H.T.P., C.A.L., C.S.H.H., G.H.H. and R.C.M.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Fauci A.S. The AIDS epidemic--considerations for the 21st century. N. Engl. J. Med. 1999;341:1046–1050. doi: 10.1056/NEJM199909303411406. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Data on the size of the HIV/AIDS epidemic. [(accessed on 26 January 2019)]; Available online: http://apps.who.int/gho/data/view.main.22100WHO?lang=en.
- 3.GBD 2015 HIV Collaborators Estimates of Global, Regional, and National Incidence, Prevalence, and Mortality of HIV, 1980–2015: The Global Burden of Disease Study 2015. Lancet HIV. 2016;3:e361–e387. doi: 10.1016/S2352-3018(16)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNAIDS Global HIV & AIDS statistics—2018 fact sheet. [(accessed on 12 December 2019)]; Available online: Aidsinfo.unaids.org.
- 5.Dennison C.R. The role of patient-reported outcomes in evaluating the quality of oncology care. Am. J. Manag. Care. 2002;8:S580–S586. [PubMed] [Google Scholar]
- 6.Hudelson C., Cluver L. Factors associated with adherence to antiretroviral therapy among adolescents living with HIV/AIDS in low- and middle-income countries: A systematic review. AIDS Care. 2015;27:805–816. doi: 10.1080/09540121.2015.1011073. [DOI] [PubMed] [Google Scholar]
- 7.Safren S.A., Hendriksen E.S., Smeaton L., Celentano D.D., Hosseinipour M.C., Barnett R., Guanira J., Flanigan T., Kumarasamy N., Klingman K., et al. Quality of life among individuals with HIV starting antiretroviral therapy in diverse resource-limited areas of the world. AIDS Behav. 2012;16:266–277. doi: 10.1007/s10461-011-9947-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nojomi M., Anbary K., Ranjbar M. Health-related quality of life in patients with HIV/AIDS. Arch. Iran. Med. 2008;11:608–612. [PubMed] [Google Scholar]
- 9.Pereira M., Canavarro M.C. Gender and age differences in quality of life and the impact of psychopathological symptoms among HIV-infected patients. AIDS Behav. 2011;15:1857–1869. doi: 10.1007/s10461-011-9928-8. [DOI] [PubMed] [Google Scholar]
- 10.Wu A.W., Mathews W.C., Brysk L.T., Atkinson J.H., Grant I., Abramson I., Kennedy C.J., McCutchan J.A., Spector S.A., Richman D.D. Quality of life in a placebo-controlled trial of zidovudine in patients with AIDS and AIDS-related complex. J. Acquir. Immune Defic. Syndr. 1990;3:683–690. [PubMed] [Google Scholar]
- 11.Freedberg K.A., Losina E., Weinstein M.C., Paltiel A.D., Cohen C.J., Seage G.R., Craven D.E., Zhang H., Kimmel A.D., Goldie S.J. The cost effectiveness of combination antiretroviral therapy for HIV disease. N. Engl. J. Med. 2001;344:824–831. doi: 10.1056/NEJM200103153441108. [DOI] [PubMed] [Google Scholar]
- 12.Cooper V., Clatworthy J., Harding R., Whetham J., Emerge C. Measuring quality of life among people living with HIV: A systematic review of reviews. Health Qual. Life Outcomes. 2017;15:220. doi: 10.1186/s12955-017-0778-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ragsdale D., Morrow J.R.J.N.R. Quality of life as a function of HIV classification. Nurs. Res. 1990;39:355–359. doi: 10.1097/00006199-199011000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Miners A., Phillips A., Kreif N., Rodger A., Speakman A., Fisher M., Anderson J., Collins S., Hart G., Sherr L.J.T.l.H. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: A cross-sectional comparison with the general population. Lancet HIV. 2014;1:e32–e40. doi: 10.1016/S2352-3018(14)70018-9. [DOI] [PubMed] [Google Scholar]
- 15.Hasan S.S., Keong S.C., Choong C.L., Ahmed S.I., Ching T.W., Anwar M., Ahmadi K., Babar M.G. Patient-reported adverse drug reactions and drug-drug interactions: A cross-sectional study on Malaysian HIV/AIDS patients. Med. Princ. Pract. 2011;20:265–270. doi: 10.1159/000321274. [DOI] [PubMed] [Google Scholar]
- 16.Boyer S., Protopopescu C., Marcellin F., Carrieri M.P., Koulla-Shiro S., Moatti J.P., Spire B., Group E.S. Performance of HIV care decentralization from the patient's perspective: Health-related quality of life and perceived quality of services in Cameroon. Health Policy Plan. 2012;27:301–315. doi: 10.1093/heapol/czr039. [DOI] [PubMed] [Google Scholar]
- 17.Liu C., Johnson L., Ostrow D., Silvestre A., Visscher B., Jacobson L.P. Predictors for lower quality of life in the HAART era among HIV-infected men. J. Acquir. Immune Defic. Syndr. 2006;42:470–477. doi: 10.1097/01.qai.0000225730.79610.61. [DOI] [PubMed] [Google Scholar]
- 18.Drewes J., Gusy B., Ruden U. More than 20 years of research into the quality of life of people with HIV and AIDS--a descriptive review of study characteristics and methodological approaches of published empirical studies. J. Int. Assoc. Provid. AIDS Care. 2013;12:18–22. doi: 10.1177/1545109712456429. [DOI] [PubMed] [Google Scholar]
- 19.Mafirakureva N., Dzingirai B., Postma M.J., van Hulst M., Khoza S. Health-related quality of life in HIV/AIDS patients on antiretroviral therapy at a tertiary care facility in Zimbabwe. AIDS Care. 2016;28:904–912. doi: 10.1080/09540121.2016.1173639. [DOI] [PubMed] [Google Scholar]
- 20.Aranda-Naranjo B. Quality of life in the HIV-positive patient: Implications and consequences. J. Assoc. Nurses AIDS Care. 2004;15:20S–27S. doi: 10.1177/1055329004269183. [DOI] [PubMed] [Google Scholar]
- 21.Davis S. Clinical sequelae affecting quality of life in the HIV-infected patient. J. Assoc. Nurses AIDS Care. 2004;15:28S–33S. doi: 10.1177/1055329004269478. [DOI] [PubMed] [Google Scholar]
- 22.Tran B.X., Hwang J., Nguyen L.H., Nguyen A.T., Latkin N.R., Tran N.K., Minh Thuc V.T., Nguyen H.L., Phan H.T., Le H.T., et al. Impact of Socioeconomic Inequality on Access, Adherence, and Outcomes of Antiretroviral Treatment Services for People Living with HIV/AIDS in Vietnam. PLoS ONE. 2016;11:e0168687. doi: 10.1371/journal.pone.0168687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jin Y., Liu Z., Wang X., Liu H., Ding G., Su Y., Zhu L., Wang N. A systematic review of cohort studies of the quality of life in HIV/AIDS patients after antiretroviral therapy. Int. J. STD AIDS. 2014;25:771–777. doi: 10.1177/0956462414525769. [DOI] [PubMed] [Google Scholar]
- 24.Gakhar H., Kamali A., Holodniy M. Health-related quality of life assessment after antiretroviral therapy: A review of the literature. Drugs. 2013;73:651–672. doi: 10.1007/s40265-013-0040-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu A.W., Hanson K.A., Harding G., Haider S., Tawadrous M., Khachatryan A., Pashos C.L., Simpson K.N. Responsiveness of the MOS-HIV and EQ-5D in HIV-infected adults receiving antiretroviral therapies. Health Qual. Life Outcomes. 2013;11:42. doi: 10.1186/1477-7525-11-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jeavons S., Greenwood K.M., Horne D.J. Accident cognitions and subsequent psychological trauma. J. Trauma. Stress. 2000;13:359–365. doi: 10.1023/A:1007797904536. [DOI] [PubMed] [Google Scholar]
- 27.Tran B.X., Vu G.T., Ha G.H., Vuong Q.H., Ho M.T., Vuong T.T., La V.P., Ho M.T., Nghiem K.P., Nguyen H.L.T., et al. Global Evolution of Research in Artificial Intelligence in Health and Medicine: A Bibliometric Study. J. Clin. Med. 2019;8:360. doi: 10.3390/jcm8030360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tran B.X., Moir M., Latkin C.A., Hall B.J., Nguyen C.T., Ha G.H., Nguyen N.B., Ho C.S.H., Ho R.C.M. Global research mapping of substance use disorder and treatment 1971–2017: Implications for priority setting. Subst. Abus. Treat. Prev. Policy. 2019;14:21. doi: 10.1186/s13011-019-0204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tran B.X., Ho R.C.M., Ho C.S.H., Latkin C.A., Phan H.T., Ha G.H., Vu G.T., Ying J., Zhang M.W.B. Depression among Patients with HIV/AIDS: Research Development and Effective Interventions (GAPRESEARCH) Int. J. Environ. Res. Public Health. 2019;16:1772. doi: 10.3390/ijerph16101772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tran B.X., Dang K.A., Le H.T., Ha G.H., Nguyen L.H., Nguyen T.H., Tran T.H., Latkin C.A., Ho C.S.H., Ho R.C.M. Global Evolution of Obesity Research in Children and Youths: Setting Priorities for Interventions and Policies. Obes. Facts. 2019;12:137–149. doi: 10.1159/000497121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoang C.L., Ha G.H., Kiet P.H.T., Tran B.X., Latkin C.A., Ho C.S.H., Ho R.C.M. Global Mapping of Interventions to Improve Quality of Life of Patients with Alzheimer’s Disease during 1990–2018. Dement. Geriatr. Cogn. Disord. 2020:1–3. doi: 10.1159/000505741. [DOI] [PubMed] [Google Scholar]
- 32.Analytics, C. Web of Science platform: Web of Science: Summary of Coverage. [(accessed on 18 March 2020)]; Available online: https://clarivate.libguides.com/webofscienceplatform/coverage.
- 33.Katz D.I., Cohen S.I., Alexander M.P. Mild traumatic brain injury. Handb. Clin. Neurol. 2015;127:131–156. doi: 10.1016/B978-0-444-52892-6.00009-X. [DOI] [PubMed] [Google Scholar]
- 34.Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., Howes M.J., Normand S.L., Manderscheid R.W., Walters E.E., et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 35.Diwakar P. O16. 1 Quality of Life and HIV—A Bibliometric Analysis of Publication Trends between 1995 to 2013. BMJ Publishing Group Ltd.; London, UK: 2017. [Google Scholar]
- 36.Kharsany A.B., Karim Q.A. HIV Infection and AIDS in Sub-Saharan Africa: Current Status, Challenges and Opportunities. Open AIDS J. 2016;10:34–48. doi: 10.2174/1874613601610010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shao Y., Williamson C. The HIV-1 epidemic: Low- to middle-income countries. Cold Spring Harb. Perspect. Med. 2012;2:a007187. doi: 10.1101/cshperspect.a007187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.UNAIDS . The Collapse of Global AIDS Funding. UNAIDS; Geneva, Switzerland: 2016. [Google Scholar]
- 39.Rueda S., Mitra S., Chen S., Gogolishvili D., Globerman J., Chambers L., Wilson M., Logie C.H., Shi Q., Morassaei S., et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: A series of meta-analyses. BMJ Open. 2016;6:e011453. doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Swindells S., Mohr J., Justis J.C., Berman S., Squier C., Wagener M.M., Singh N. Quality of life in patients with human immunodeficiency virus infection: Impact of social support, coping style and hopelessness. Int. J. STD AIDS. 1999;10:383–391. doi: 10.1177/095646249901000606. [DOI] [PubMed] [Google Scholar]
- 41.Pozniak A. Quality of life in chronic HIV infection. Lancet HIV. 2014;1:e6–e7. doi: 10.1016/S2352-3018(14)70003-7. [DOI] [PubMed] [Google Scholar]
- 42.Canavarro M.C., Pereira M. Factor structure and psychometric properties of the European Portuguese version of a questionnaire to assess quality of life in HIV-infected adults: The WHOQOL-HIV-Bref. AIDS Care. 2012;24:799–807. doi: 10.1080/09540121.2011.630362. [DOI] [PubMed] [Google Scholar]
- 43.Pereira M., Martins A., Alves S., Canavarro M.C. Assessing quality of life in middle-aged and older adults with HIV: Psychometric testing of the WHOQOL-HIV-Bref. Qual. Life Res. 2014;23:2473–2479. doi: 10.1007/s11136-014-0707-7. [DOI] [PubMed] [Google Scholar]
- 44.Hsiung P.C., Fang C.T., Wu C.H., Sheng W.H., Chen S.C., Wang J.D., Yao G. Validation of the WHOQOL-HIV BREF among HIV-infected patients in Taiwan. AIDS Care. 2011;23:1035–1042. doi: 10.1080/09540121.2010.543881. [DOI] [PubMed] [Google Scholar]
- 45.Saddki N., Noor M.M., Norbanee T.H., Rusli M.A., Norzila Z., Zaharah S., Sarimah A., Norsarwany M., Asrenee A.R., Zarina Z.A. Validity and reliability of the Malay version of WHOQOL-HIV BREF in patients with HIV infection. AIDS Care. 2009;21:1271–1278. doi: 10.1080/09540120902803216. [DOI] [PubMed] [Google Scholar]
- 46.Tran B.X. Quality of life outcomes of antiretroviral treatment for HIV/AIDS patients in Vietnam. PLoS ONE. 2012;7:e41062. doi: 10.1371/journal.pone.0041062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tucker C.M., Marsiske M., Rice K.G., Nielson J.J., Herman K. Patient-centered culturally sensitive health care: Model testing and refinement. Health Psychol. 2011;30:342–350. doi: 10.1037/a0022967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nota S.P., Bot A.G., Ring D., Kloen P.J.I. Disability and depression after orthopaedic trauma. Injury. 2015;46:207–212. doi: 10.1016/j.injury.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 49.Larios S.E., Davis J.N., Gallo L.C., Heinrich J., Talavera G. Concerns about stigma, social support and quality of life in low-income HIV-positive Hispanics. Ethn. Dis. 2009;19:65–70. [PubMed] [Google Scholar]
- 50.Medeiros R., Medeiros J.A., Silva T., Andrade R.D., Medeiros D.C., Araujo J.S., Oliveira A.M.G., Costa M.A.A., Dantas P.M.S. Quality of life, socioeconomic and clinical factors, and physical exercise in persons living with HIV/AIDS. Rev. Saude Publica. 2017;51:66. doi: 10.1590/s1518-8787.2017051006266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Calvetti P.Ü., Giovelli G.R.M., Gauer G.J.C., Moraes J.F.D.d. Psychosocial factors associated with adherence to treatment and quality of life in people living with HIV/AIDS in Brazil %J Jornal Brasileiro de Psiquiatria. J. Brasileiro De Psiquiatria. 2014;63:8–15. doi: 10.1590/0047-2085000000002. [DOI] [Google Scholar]
- 52.Ruiz Perez I., Rodriguez Bano J., Lopez Ruz M.A., del Arco Jimenez A., Causse Prados M., Pasquau Liano J., Martin Rico P., de la Torre Lima J., Prada Pardal J.L., Lopez Gomez M., et al. Health-related quality of life of patients with HIV: Impact of sociodemographic, clinical and psychosocial factors. Qual. Life Res. 2005;14:1301–1310. doi: 10.1007/s11136-004-4715-x. [DOI] [PubMed] [Google Scholar]
- 53.Lutgendorf S., Antoni M.H., Schneiderman N., Fletcher M.A. Psychosocial counseling to improve quality of life in HIV infection. Patient Educ. Couns. 1994;24:217–235. doi: 10.1016/0738-3991(94)90066-3. [DOI] [PubMed] [Google Scholar]
- 54.Bastardo Y.M., Kimberlin C.L. Relationship between quality of life, social support and disease-related factors in HIV-infected persons in Venezuela. AIDS Care. 2000;12:673–684. doi: 10.1080/095401200750003842. [DOI] [PubMed] [Google Scholar]
- 55.Sowell R.L., Seals B.F., Moneyham L., Demi A., Cohen L., Brake S. Quality of life in HIV-infected women in the south-eastern United States. AIDS Care. 1997;9:501–512. doi: 10.1080/713613191. [DOI] [PubMed] [Google Scholar]
- 56.Bachmann M.O., Louwagie G., Fairall L.R. Quality of life and financial measures in HIV/AIDS in Southern Africa. Springer; New York, NY, USA: 2010. pp. 3223–3243. [Google Scholar]