Abstract
Background
Improved understanding of the mediators of physical activity (PA) interventions could lead to improvements in theory and programs.
Purpose
To examine the 24-month mediating effects of psychosocial variables on PA and cardiorespiratory fitness (CRF) outcomes in 878 initially sedentary adults aged 35–75 participating in the Activity Counseling Trial.
Methods
Participants were assigned to one of three intervention arms: physician advice, assistance, or counseling. MacKinnon’s product of coefficients was used to test for longitudinal and contemporaneous mediation.
Results
Changes in behavioral processes of change from baseline to 24 months significantly mediated the relationship between the active intervention arms and improvements in PA and CRF from baseline to 24 months in both men and women. None of the other psychosocial variables tested met criteria for mediation.
Conclusions
Results indicate that behavioral interventions should incorporate methods to encourage participants to use these behavioral strategies as they attempt to become more active.
Keywords: Behavior change, Exercise, RCT, Intervention, Physician counseling
Introduction
Progress has been made in developing more effective approaches to promoting physical activity (PA) [1]; however, much less is known regarding how behavioral interventions work [2]. As a result, there has been a call for research on mediating mechanisms [2]. A mediator is an intervening variable that provides a possible explanation for the causal relationship between an intervention and an outcome [3]. More specifically, mediators begin to open up the “black box” of behavior change and provide explanations for why or how interventions produce improvements in behavior, or fail to do so [4]. Behavioral interventions are typically designed to change mediators that are implicitly or explicitly identified, but effects on potential mediators are seldom examined. Investigating potential mediators may assist researchers in understanding which variables are most important for increasing PA, potentially leading to more effective and targeted interventions [5].
Although some researchers have criticized the transtheoretical model (TTM) [6–8], it has been successfully used to understand behavior change [9]. A meta-analysis by Marshall and Biddle [10] found support for the application of the TTM in predicting and explaining PA behavior. This model proposes that individuals move through various stages as they attempt to adopt and maintain PA (i.e., precontemplation, contemplation, preparation, action, and maintenance) [11]. Three constructs are hypothesized to mediate the change process: decisional balance, cognitive and behavioral processes of change, and self-efficacy [10]. A number of studies have examined theoretical constructs from the TTM as mediators of PA change, and findings have been mixed [5, 12–17].
Napolitano et al. [14] found that the behavioral processes of change mediated the relationship between two types of tailored interventions (each compared to the control group) and PA change, whereas self-efficacy, decisional balance, and the cognitive processes did not. Calfas et al. [16] also found that the behavioral processes of change were significant mediators of PA change in a primary care intervention, whereas self-efficacy and cognitive processes of change were not. In another primary care intervention, Pinto et al. [15] found that decisional balance and behavioral processes of change significantly mediated changes in PA at 6 weeks but not at 8 months. Self-efficacy and cognitive processes of change were not significant mediators at either time point. Lewis et al. [12] found partial support for self-efficacy and the behavioral processes of change as mediators of an individually tailored PA intervention, but no support for decisional balance and the cognitive processes. Finally, two interventions, one with breast cancer survivors [13] and the other with mothers enrolled in the Women, Infant, and Child (WIC) Program [17], found no support for hypothesized TTM constructs (cognitive and behavioral processes of change, decisional balance, and self-efficacy) as mediators of PA change. Although the findings from these studies make it difficult to make definitive conclusions as to which mediators may be most important for PA change, the behavioral processes of change seem to be the most consistent mediator in the available literature. Additional mediation analyses will allow researchers to compare results with other studies, and help to understand the key factors that might explain why an intervention improves PA. Further research on theoretical mediators of PA behavior change is crucial for moving the PA intervention field forward [1].
Primary care settings are an appealing setting for PA interventions because of the potential broad population reach and the perceived influence of medical practitioner advice on individuals’ health information [18]. The Activity Counseling Trial (ACT) provides an opportunity to conduct comprehensive mediation analyses in a large diverse sample. The ACT was a multicenter randomized controlled trial that evaluated the efficacy of three levels of primary care PA counseling, delivered over 2 years, in increasing and maintaining PA and cardiorespiratory fitness (CRF) in sedentary adults [19, 20]. Because the transtheoretical model (TTM) was used to develop and guide intervention strategies in the ACT, constructs from the TTM were tested as mediators [9]. The purpose of this study was to examine the mediating effects of psychosocial variables on PA and CRF outcomes in the ACT. Consistent with the theoretical model and the design of the interventions themselves, we hypothesized that changes in self-efficacy, decisional balance, and cognitive and behavioral processes of change would mediate changes in PA and CRF.
Methods
A more detailed description of the ACT is provided elsewhere [19–21]. In brief, the ACT compared the effects of three PA counseling interventions on PA and CRF over 24 months in patients recruited from primary care settings. The interventions varied by level of counseling intensity and resource requirements [20, 21]. The interventions were designed and powered to test the research questions for men and women separately [20, 21]; therefore, mediation analyses were conducted separately by gender. Participants were recruited over an 18-month period from ten primary care facilities, involving 51 physicians, four physician assistants, and one nurse practitioner [21]. The primary care facilities were affiliated with three clinical centers: Stanford University, the University of Tennessee, and the Cooper Institute in conjunction with the University of Texas Southwestern Medical Center. The ACT coordinating center was Wake Forest University School of Medicine, and the project office was the National Heart, Lung, and Blood Institute [21]. The ACT study was approved yearly by each of the Institutional Review Boards from the clinical and coordinating centers.
Procedures
After baseline assessments, participants were randomly assigned to one of three treatment arms: physician advice, assistance, and counseling [19]. With the exception of physician advice, the intervention was delivered by ACT health educators [21]. All three arms were given the same PA goals, based on the national recommendations of five or more days of 30 min or more of moderate intensity PA [22] or three or more days of 30 min of vigorous intensity PA [23]. See Table 1 and King et al. [19] for a more detailed description of the intervention components for each of the three intervention arms.
Table 1.
Intervention components for the Activity Counseling Trial arms
| Intervention arm | ||
|---|---|---|
| Advice (“standard care”) | Assistance | Counseling |
| • Brief counseling (2–4 min) from primary care physician on recommended amount of PA | • Everything the Advice group received, plus: | • Everything the Advice and Assistance groups received, plus: |
| • 30–40 min counseling session with HE | ||
| • Educational videotape that modeled targeted PA behavior | • HE-initiated telephone counseling bi-weekly for the first 6 weeks, then monthly for the remainder of year 1. During year 2, the participant and HE decided on the frequency of subsequent calls | |
| • Physician encouragement to select enjoyable activities and ask for PA support | ||
| • HE advice and assistance related to PA goals set by physician, specific benefits of PA, and development of short-term PA plan | ||
| • Provided additional feedback | ||
| • Physician assistance in developing realistic expectations of outcomes that could be achieved with regular PA | • Evaluated and updated PA goals | |
| • One staff-initiated counseling call (5–10 min) one week after initial visit | • Facilitated active problem-solving around barriers | |
| • Discussed future barriers and plans to effectively cope (i.e., relapse prevention) | ||
| • Assessed success in meeting first goal, set subsequent goals, provided social support, and problem-solved any encountered barriers | ||
| • Physician assistance in making personal benefits of being PA more salient | • Provided reinforcement and social support | |
| • Encouraged to call HE throughout intervention if assistance was needed | • Offered additional in-person counseling throughout intervention (content similar to the telephone counseling) | |
| • Written materials on PA guidelines from ACT health educator (HE) | ||
| • Interactive mailed newsletters | ||
| • Invited to call HE with questions | • Intended to increase cognitive and behavioral skills (at all stages of change) | • Weekly behavioral counseling classes by HEs were offered |
| • Newsletters included a postage-paid mail back card used by participants to report their weekly PA, current goals, and barriers | • Focused on building cognitive and behavioral skills needed to adopt and maintain PA | |
| • Addressed adoption and maintenance issues | ||
| • HEs sent feedback sheets addressing the specific barriers reported on the mail back card | • Facilitated group support | |
| • Designed to meet needs of participants in various stages of change | ||
| • Pedometer and calendar to encourage self-monitoring | ||
| • Inexpensive incentives | ||
| • Brief behavioral counseling from HE at subsequent physician visits | ||
Measures
Demographic variables
Participants were asked to report their age, gender, race, current marital status, income, and highest grade of school completed [24].
Body mass index
Height to the nearest 1/10 cm and weight to the nearest 1/10 kg were obtained by trained staff. To calculate body mass index (BMI), weight in kilograms (kg) was divided by height in squared meters (m2). Overweight was defined as a BMI of 25.0–29.9 kg/m2, and obese was defined as a BMI of≥30.0 kg/m2.
Physical activity
PA was assessed as average energy expenditure per day (kcal/kg/day) using the 7-day PA recall (PAR) [25, 26]. During a structured interview, participants were asked to recall the amount of time spent in each 24-h period during the past 7 days in four categories of activity intensity: sleep (1.0metabolic equivalent of tasks; METs), moderate (3.0–5.0 METs), hard (5.1–6.9 METs), and very hard (≥7.0 METs) [20, 21]. Hours of light intensity activity (1.1–2.9 METs) were obtained by subtracting the sum of the other activity categories from 24. The interviewers guided participants through the recall process day-by-day (starting with the previous day and working backwards), by asking open-ended questions, and using prompts and cues. The interviewer first asked about the participant’s sleep (e.g., what time did you go to bed last night? What time did you get out of bed this morning?), and then about all other physical activities of at least walking intensity performed. Participants were asked to report the intensity and duration of each activity performed throughout the day. To provide a frame of reference and thus assist with recall, each day was segmented into morning, afternoon, and evening. To improve precision at each time point, the 7-day PAR was administered twice, at least 7 days apart at baseline, 6 months (once in person and once by telephone), and 24 months [20, 21]. The values from the two interviews at each time point were averaged [21]. Interviewers administering the 7-day PAR were trained to use a standardized protocol [21]. Skewness in the PAR data in the present study was corrected with a square root transformation. The 7-day PAR is widely used, and has been shown to be sensitive to change in PA interventions [27–29] and to have good reliability and validity [26, 29–34].
Cardiorespiratory fitness
CRF was assessed by measuring maximal oxygen uptake (VO2 max, ml/kg/min) using a graded maximal exercise test on a treadmill. After participants warmed-up with a brief walk at a 0% grade, the speed was increased until steady-state heart rate of 60% of age-predicted maximum or a rating of 11–13 on the Borg scale [35] of perceived exertion was maintained for 4 min [20, 21]. Then, treadmill grade was elevated 2% in 2-min stages until the RPE reached 17 or above; thereafter, increasing the grade by 1% until the participant reached volitional fatigue or standard stopping criteria [20, 21, 36].
Self-efficacy
Self-efficacy for overcoming barriers to regular PA (i.e., barriers efficacy) was measured using the 14-item Stanford self-efficacy scale [37]. Using an 11-point scale ranging from “I cannot do at all” to “certain that I can do,” participants were asked how confident they were that they could be physically active under a variety of conditions over the next 6 months (e.g., when tired, when feeling depressed, when on vacation, during bad weather). Items were summed to obtain a barriers efficacy score. Performance self-efficacy, which was developed for ACT [24] and was based on the self-efficacy construct [38], was measured with five items. Using the same 11-point scale, participants were asked how confident they were that at the present time they could walk at a fast pace without stopping for different durations of time (e.g., 10, 20 min, etc.). Items were summed to obtain a performance efficacy score. The barriers efficacy scale has been shown to have an internal consistency of 0.92 and to be significantly correlated with PA [39]. The internal consistency for the present study was 0.91 for barriers efficacy and 0.93 for performance self-efficacy.
Decisional balance
Decisional balance was assessed using a 12-item measure by Marcus et al. [40]. Six items assessed pros to PA (e.g., I would feel less stressed if I was regularly PA) and six items assessed cons to PA (e.g., I feel uncomfortable when I engage in PA because I get out of breath and my heart beats very fast). Using a five-point scale ranging from “not at all important” to “extremely important,” participants were asked to rate how important each statement was in their decision concerning whether or not to be physically active. Items were summed separately to obtain an overall “pros” and “cons” score. Decisional balance has been shown to have good internal consistency (0.79 for pros, 0.95 for cons) and has correlated significantly with the stage of change of PA [40]. The internal consistency for the present study was 0.87 for the pros score and 0.73 for the cons score.
Processes of change
Cognitive and behavioral motivational processes of PA change were assessed using the 20-item version of the Marcus et al. scale [41]. Using a five-point scale ranging from “never” to “repeatedly,” participants were asked to rate the frequency of experiences that could affect PA during the past month. Ten items were used to assess the behavioral processes of change (enlisting social support, reward yourself, remind yourself, commit yourself, substitute alternatives) and ten items were used to assess the cognitive processes of change (comprehend the benefits, increase healthy alternatives, increase knowledge, warnings of risk, care about the consequences). Items were summed to obtain a behavioral process of change score and a cognitive process of change score. In addition to overall indices, individual behavioral and cognitive processes were scored by summing the two items used to measure each. The processes of change have been shown to have good internal consistency (0.83) and to be correlated with stage of change (ŋ2=0.06–0.20 for behavioral processes, ŋ2= 0.11–0.45 for cognitive processes, p<.001 for all) [42]. The internal consistency for the present study was 0.77 for the cognitive processes and 0.72 for the behavioral processes. The internal consistencies for the individual cognitive processes ranged from 0.43 to 0.84 and from 0.55 to 0.71 for the individual behavioral processes.
Statistical Analyses
Longitudinal (i.e., changes in mediators from baseline to 6 months and changes in PA and CRF from 6 to 24 months) and contemporaneous (i.e., changes in mediators and changes in PA and CRF from baseline to 24 months) mediation were examined separately. The two active intervention arms, assistance and counseling, were combined and compared to the advice arm because CRF in women at 24 months was significantly higher in both the assistance and counseling groups than in the advice group, with no differences between the counseling and advice groups (for men, all three arms showed increases over time). Mediation analyses were conducted separately for men and women.
To test for mediation, MacKinnon’s product of coefficients test (αβ) as used [43]. This test consists of: (1) estimating the effect of the intervention on changes in each potential mediator (α coefficient) by regressing the hypothesized mediator on intervention arm, controlling for the mediator at baseline, (2) estimating the effect of changes in the mediator on changes in the outcome (β coefficient) by regressing the outcome on the hypothesized mediator, controlling for intervention arm, the outcome at the previous time point, and the mediator at the previous time point(s), (3) calculating the product of coefficients by multiplying the α and β coefficients (αβ), and (4) constructing asymmetric confidence limits base on the distribution of the product using the PRODCLIN program [44]. Confidence intervals that did not include zero were considered statistically significant. All models also controlled for age, race/ethnicity, education level, BMI, and site (dummy coded).
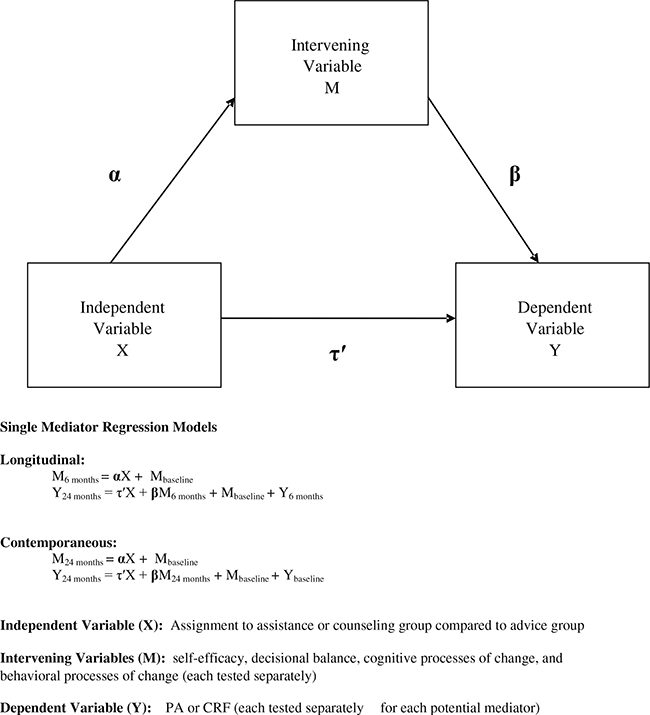
Because multicollinearity may be present in a multiple mediator model, we first tested each mediator separately in a single-mediator model. Next, multiple-mediator models were used to (1) test the independent effects of those variables found to be significant in the single-mediator models, and to (2) test for suppression effects in the single-mediator models (all potential mediators were entered simultaneously to see if particular mediators suppressed the effects of other mediators). Finally, to determine the extent of the mediated effect, the percentage of the total effect mediated was calculated for each significant mediator by the following equation: αβ/(αβ+c), where c is the direct effect of the intervention on the outcome (PA or CRF) [45]. These analyses were conducted for changes in mediating variables from baseline to 6 months and baseline to 24 months, and separately for each outcome variable (PA and CRF from 6 to 24 months and baseline to 24 months) and gender. Figure 1 depicts our hypothesized mediation model. Proc GLM was used to conduct all mediation analyses (SAS version 9.2; SAS Institute, Cary, NC, USA).
Fig. 1.
Activity Counseling Trial hypothesized mediation model
Results
More detailed results of the ACT have been published elsewhere [21]. Briefly, for women at 24 months, CRF was significantly higher in both the assistance and the counseling arms compared to the advice arm. There were no significant differences in CRF between the counseling and assistance arms. There were also no significant between arms differences in reported total PA for women, which generally increased across all three arms. For men, there were no significant between arm differences in CRF or in total PA at 24 months [21]. Men in all three arms generally increased their fitness and PA across the 24-month period [21].
Participants
As has been reported elsewhere [21], participants were 874 community-dwelling adults (395 women and 479 men), 35–75 years of age, without a history or evidence of coronary heart disease who were patients of an ACT primary care provider and physically inactive. The mean age of participants was 51.9±9.7 years for women and 51.4± 9.6 year for men. Nearly one third of the participants belonged to a minority racial/ethnic group, 56% were college graduates, and more than 41% reported annual household incomes of $75,000 or more.
PA Mediation Results for Men
Table 2 shows the α and β coefficients, their standard errors, the αβ estimate, and the asymmetric confidence limits for changes in each potential mediator from baseline to 6 and 24 months for PA outcomes in men in the single and multiple mediator models. Changes in hypothesized mediators from baseline to 6 months did not significantly mediate the relationship between intervention group assignment and change in PA from baseline to 24 months (longitudinal mediation). However, changes in behavioral processes of change from baseline to 24 months mediated the relationship between intervention group and PA at 24 months (contemporaneous mediation). More specifically, committing yourself and substituting alternatives uniquely contributed to the significant relationship. The behavioral processes of change mediated 28% of the total effect of the intervention on PA change. Behavioral processes remained significant in the multiple-mediator model. Table 3 summarizes the significant findings (mediators, α, and β paths) for the baseline to 6 and 24 month mediators for the PA outcome in men in the single- and multiple-mediator models.
Table 2.
Summary of mediation effects for physical activity in men
| Mediator | Longitudinal mediation: Δ in mediators from baseline to 6 months predicting Δ in PA from 6 to 24 months |
Contemporaneous mediation: Δ in mediators from baseline to 24 months predicting Δ in PA from baseline to 24 months |
||||||
|---|---|---|---|---|---|---|---|---|
| α coefficient (SE) | β coefficient (SE) | α β | Asymmetric confidence limit | α coefficient (SE) | β coefficient (SE) | α β | Asymmetric confidence limit | |
| Cons of exercise | ||||||||
| Single-mediator model | −0.034 (0.061) | −0.007 (0.012) | 0.000 | −0.001, 0.002 | −0.014 (0.065) | −0.006 (0.011) | 0.000 | −0.001, 0.001 |
| Multiple-mediator model | 0.007 (0.014) | −0.000 | −0.002, 0.001 | 0.012 (0.012) | −0.000 | −0.002, 0.001 | ||
| Pros of exercise | ||||||||
| Single-mediator model | 0.125 (0.073) | −0.018 (0.010) | −0.002 | −0.007, 0.000 | 0.246 (0.076)** | 0.014 (0.009) | 0.003 | −0.001, 0.009 |
| Multiple-mediator model | −0.032 (0.012)** | −0.004 | −0.010, 0.000 | 0.005 (0.011) | 0.001 | −0.004, 0.007 | ||
| Barriers efficacy | ||||||||
| Single-mediator model | −0.112 (1.592) | 0.001 (0.0004) | −0.000 | −0.003, 0.003 | 0.136 (1.781) | 0.002 (0.000)** | 0.000 | −0.007, 0.007 |
| Multiple-mediator model | 0.001 (0.001) | −0.000 | −0.004, 0.003 | 0.002 (0.000)** | 0.000 | −0.007, 0.007 | ||
| Performance efficacy | ||||||||
| Single-mediator model | 2.851 (2.207) | 0.000 (0.000) | 0.000 | −0.001, 0.002 | 3.733 (2.216) | 0.000 (0.000) | 0.011 | −0.001, 0.004 |
| Multiple-mediator model | −0.000 (0.000) | −0.001 | −0.002, 0.002 | −0.000 (0.000) | −0.001 | −0.004, 0.002 | ||
| Cognitive processes of change | ||||||||
| Single-mediator model | 0.027 (0.052) | 0.027 (0.014)* | 0.001 | −0.002, 0.004 | 0.120 (0.059)* | 0.023 (0.012) | 0.003 | −0.000, 0.007 |
| Multiple-mediator model | 0.050 (0.018)** | 0.001 | −0.004, 0.007 | −0.009 (0.016) | −0.001 | −0.006, 0.003 | ||
| Behavioral processes of change | ||||||||
| Single-mediator model | 0.148 (0.057)** | 0.002 (0.013) | 0.000 | −0.004, 0.004 | 0.196 (0.063)** | 0.035 (0.011)** | 0.007 | 0.002, 0.014a |
| Multiple-mediator model | −0.006 (0.017) | −0.001 | −0.006, 0.004 | 0.030 (0.015) | 0.006 | 0.000, 0.014a | ||
Significant mediator
p<0.05
p<0.01
Table 3.
Summary of significant physical activity findings for men
| Single-mediator models |
Multiple-mediator models |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Longitudinal mediation |
Contemporaneous mediation |
Longitudinal mediation |
Contemporaneous mediation |
|||||||||
| Mediator | α | β | Med | α | β | Med | α | β | Med | α | β | Med |
| Cons of exercise | ||||||||||||
| Pros of exercise | √ | √ | √ | |||||||||
| Barriers efficacy | √ | √ | ||||||||||
| Performance efficacy | ||||||||||||
| Cognitive processes of change | √ | √ | √ | √ | ||||||||
| Behavioral processes of change | √ | √ | √ | √ | √ | √ | √ | |||||
α the path from the intervention to the proposed mediating variable; β the path from the proposed mediating variable to the outcome variable; Med mediation (αβ)
CRF Mediation Results for Men
Table 4 shows the α and β coefficients, their standard errors, the αβ estimate, and the asymmetric confidence limits for changes in each potential mediator from baseline to 6 and 24 months for CRF outcomes in men in the single and multiple mediator models. Changes in hypothesized mediators from baseline to 6 months did not significantly mediate the relationship between intervention group assignment and change in CRF from baseline to 24 months (longitudinal mediation). However, changes in behavioral processes of change from baseline to 24 months mediated the relationship between intervention group and CRF at 24 months (contemporaneous mediation). More specifically, substituting alternatives uniquely contributed to the significant relationship. The behavioral processes of change mediated 26% of the total effect of the intervention on CRF change. In the multiple mediator model, the effect for behavioral processes of change was no longer significant, likely due to its relationship with the cognitive processes (r=0.70) and pros of exercise (r=0.49) at 24 months. Table 5 summarizes the significant findings (mediators, α, and β paths) for the baseline to 6 and 24 month mediators for the CRF outcome in men in the single and multiple mediator models.
Table 4.
Summary of mediation effects for cardiorespiratory fitness in men
| Mediator | Longitudinal mediation: Δ in mediators from baseline to 6 months predicting Δ in CRF from 6 to 24 months |
Contemporaneous mediation: Δ in mediators from baseline to 24 months predicting Δ in CRF from baseline to 24 months |
||||||
|---|---|---|---|---|---|---|---|---|
| α coefficient (SE) | β coefficient (SE) | α β | Asymmetric confidence limit | α coefficient (SE) | β coefficient (SE) | α β | Asymmetric confidence limit | |
| Cons of exercise | ||||||||
| Single-mediator Model | −0.034 (0.061) | 0.087 (0.335) | −0.002 | −0.032, 0.022 | −0.014 (0.065) | −0.901 (0.340)** | 0.013 | −0.105, 0.137 |
| Multiple-mediator model | 0.044 (0.393) | −0.001 | −0.032, 0.027 | −0.754 (0.377)* | 0.011 | −0.089, 0.118 | ||
| Pros of exercise | ||||||||
| Single-mediator model | 0.125 (0.073) | 0.020 (0.283) | 0.003 | −0.072, 0.079 | 0.246 (0.076)** | 0.316 (0.297) | 0.078 | −0.060, 0.247 |
| Multiple-mediator model | −0.039 (0.347) | −0.005 | −0.100, 0.085 | 0.177 (0.338) | 0.044 | −0.118, 0.223 | ||
| Barriers efficacy | ||||||||
| Single-mediator model | −0.112 (1.592) | 0.002 (0.013) | −0.000 | −0.008, 0.007 | 0.136 (1.781) | 0.038 (0.013)** | 0.005 | −0.132, 0.145 |
| Multiple-mediator model | −0.005 (0.016) | 0.006 | −0.017, 0.019 | 0.019 (0.015) | 0.003 | −0.069, 0.078 | ||
| Performance efficacy | ||||||||
| Single-mediator model | 2.851 (2.207) | 0.017 (0.011) | 0.048 | −0.024, 0.167 | 3.733 (2.216) | 0.044 (0.011)** | 0.164 | −0.021, 0.395 |
| Multiple-mediator model | 0.017 (0.012) | 0.048 | −0.027, 0.172 | 0.038 (0.012)** | 0.142 | −0.016, 0.357 | ||
| Cognitive processes of change | ||||||||
| Single-mediator model | 0.027 (0.052) | 0.214 (0.383) | 0.006 | −0.023, 0.043 | 0.120 (0.059)* | 0.550 (0.378) | 0.066 | −0.018, 0.198 |
| Multiple-mediator model | 0.403 (0.513) | 0.011 | −0.034, 0.073) | −0.128 (0.499) | −0.015 | −0.148, 0.105 | ||
| Behavioral processes of change | ||||||||
| Single-mediator model | 0.148 (0.057)** | −0.130 (0.359) | −0.019 | −0.135, 0.086 | 0.196 (0.063)** | 0.844 (0.351)* | 0.165 | 0.026, 0.362)a |
| Multiple-mediator model | −0.338 (0.477) | 0.008 | −0.213, 0.084 | 0.505 (0.488) | 0.099 | −0.081, 0.322 | ||
Significant mediator
p<0.05
p<0.01
Table 5.
Summary of significant cardiorespiratory findings for men
| Single-mediator models |
Multiple-mediator models |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Longitudinal mediation |
Contemporaneous mediation |
Longitudinal mediation |
Contemporaneous mediation |
|||||||||
| Mediator | α | β | Med | α | β | Med | α | β | Med | α | β | Med |
| Cons of exercise | √ | √ | ||||||||||
| Pros of exercise | √ | √ | ||||||||||
| Barriers efficacy | √ | |||||||||||
| Performance efficacy | √ | √ | ||||||||||
| Cognitive processes of change | √ | √ | ||||||||||
| Behavioral processes of change | √ | √ | √ | √ | √ | √ | ||||||
α represents the path from the intervention to the proposed mediating variable; β the path from the proposed mediating variable to the outcome variable; Med mediation (αβ)
PA Mediation Results for Women
Table 6 shows the α and β coefficients, their standard errors, the αβ estimate, and the asymmetric confidence limits for changes in each potential mediator from baseline to 6 and 24 months for PA outcomes in women in the single and multiple mediator models. Changes in hypothesized mediators from baseline to 6 months did not significantly mediate the relationship between intervention group assignment and change in PA from baseline to 24 months (longitudinal mediation). However, changes in behavioral processes of change from baseline to 24 months mediated the relationship between intervention group and PA at 24 months (contemporaneous mediation). More specifically, substituting alternatives uniquely contributed to the significant relationship. The behavioral processes of change mediated 43% of the total effect of the intervention on PA change. In the multiple mediator model, the effect for behavioral processes of change was no longer significant, likely due to its relationship with the cognitive processes (r=0.66), barriers self-efficacy (r=0.47), pros of exercise (r=0.39), and performance self-efficacy (0.36) at 24 months. Table 7 summarizes the significant findings (mediators, α, and β paths) for the baseline to 6 and 24 month mediators for the PA outcome in women.
Table 6.
Summary of mediation effects for physical activity in women
| Mediator | Longitudinal mediation: Δ in mediators from baseline to 6 months predicting Δ in PA from 6 to 24 months |
Contemporaneous mediation: Δ in mediators from baseline to 24 months predicting Δ in PA from baseline to 24 months |
||||||
|---|---|---|---|---|---|---|---|---|
| α coefficient (SE) | β coefficient (SE) | α β | Asymmetric confidence limit | α coefficient (SE) | β coefficient (SE) | α β | Asymmetric confidence limit | |
| Cons of exercise | ||||||||
| Single-mediator model | −0.019 (0.079) | 0.012 (0.010) | −0.000 | −0.002, 0.002 | −0.061 (0.085) | −0.018 (0.009) | 0.001 | −0.002, 0.005 |
| Multiple-mediator model | 0.019 (0.011) | −0.000 | −0.004, 0.003 | −0.005 (0.011) | 0.000 | −0.001, 0.002 | ||
| Pros of exercise | ||||||||
| Single-mediator model | 0.099 (0.091) | 0.003 (0.009) | 0.000 | −0.002, 0.003 | −0.061 (0.104) | 0.012 (0.008) | −0.001 | −0.004, 0.002 |
| Multiple-mediator model | −0.001 (0.011) | −0.000 | −0.003, 0.002 | 0.005 (0.010) | −0.000 | −0.002, 0.001 | ||
| Barriers efficacy | ||||||||
| Single-mediator model | −1.443 (1.995) | 0.000 (0.000) | −0.001 | −0.003, 0.001 | 3.974 (2.438) | 0.002 (0.000) | 0.008 | −0.001, 0.018 |
| Multiple-mediator model | 0.001 (0.001) | −0.001 | −0.008, 0.003 | 0.001 (0.000) | 0.004 | −0.001, 0.011 | ||
| Performance efficacy | ||||||||
| Single-mediator model | 3.325 (3.055) | −0.000 (0.000) | −0.000 | −0.002, 0.002 | 3.816 (3.341) | 0.001 (0.000)** | 0.004 | −0.003, 0.011 |
| Multiple-mediator model | −0.000 (0.000) | −0.000 | −0.003, 0.002 | 0.001 (0.000)* | 0.004 | −0.002, 0.003 | ||
| Cognitive processes of change | ||||||||
| Single-mediator model | 0.036 (0.068) | 0.007 (0.012) | 0.000 | −0.001, 0.002 | 0.051 (0.071) | 0.027 (0.011)* | 0.001 | −0.002, 0.006 |
| Multiple-mediator model | 0.006 (0.015) | 0.000 | −0.001, 0.002 | 0.031 (0.015)* | 0.002 | −0.003, 0.007 | ||
| Behavioral processes of change | ||||||||
| Single-mediator model | 0.274 (0.071)** | 0.007 (0.011) | 0.002 | −0.004, 0.008 | 0.248 (0.080)** | 0.038 (0.010)** | 0.009 | 0.003, 0.018a |
| Multiple-mediator model | 0.009 (0.016) | 0.002 | −0.006, 0.012 | 0.002 (0.016) | 0.000 | −0.007, 0.009 | ||
Significant mediator
p<0.05
p<0.01
Table 7.
Summary of significant physical activity findings for women
| Single-mediator models |
Multiple-mediator models |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Longitudinal mediation |
Contemporaneous mediation |
Longitudinal mediation |
Contemporaneous mediation |
|||||||||
| Mediator | α | β | Med | α | β | Med | α | β | Med | α | β | Med |
| Cons of exercise | ||||||||||||
| Pros of exercise | ||||||||||||
| Barriers efficacy | ||||||||||||
| Performance efficacy | √ | √ | ||||||||||
| Cognitive processes of change | √ | √ | ||||||||||
| Behavioral processes of change | √ | √ | √ | √ | √ | √ | ||||||
α the path from the intervention to the proposed mediating variable; β the path from the proposed mediating variable to the outcome variable; Med represents mediation (αβ)
CRF Mediation Results for Women
Table 8 shows the α and β coefficients, their standard errors, the αβ estimate, and the asymmetric confidence limits for changes in each potential mediator from baseline to 6 and 24 months for CRF outcomes in women in the single and multiple mediator models. Changes in hypothesized mediators from baseline to 6 months did not significantly mediate the relationship between intervention group assignment and change in PA from baseline to 24 months (longitudinal mediation). However, changes in behavioral processes of change from baseline to 24 months mediated the relationship between intervention group and CRF at 24 months (contemporaneous mediation). More specifically, substituting alternatives uniquely contributed to the significant relationship. The behavioral processes of change mediated 22% of the total effect of the intervention on CRF change. In the multiple mediator model, the effect for behavioral processes of change was no longer significant, again, likely due to its relationship with the cognitive processes (r=0.66), barriers self-efficacy (r= 0.47), pros of exercise (r=0.39), and performance self-efficacy (0.36) at 24 months. Table 9 summarizes the significant findings (mediators, α, and β paths) for the baseline to 6 and 24 month mediators for the CRF outcome in women in the single and multiple mediator models.
Table 8.
Summary of mediation effects for cardiorespiratory fitness in women
| Mediator | Longitudinal mediation: Δ in mediators from baseline to 6 months predicting Δ in CRF from 6 to 24 months |
Contemporaneous mediation: Δ in mediators from baseline to 24 months predicting change Δ in CRF from baseline to 24 months |
||||||
|---|---|---|---|---|---|---|---|---|
| α coefficient (SE) | β coefficient (SE) | α β | Asymmetric confidence limit | α coefficient (SE) | β coefficient (SE) | α β | Asymmetric confidence limit | |
| Cons of exercise | ||||||||
| Single-mediator model | −0.019 (0.079) | 0.193 (0.305) | −0.004 | −0.042, 0.029 | −0.061 (0.085) | −0.796 (0.308)* | 0.049 | −0.080, 0.205 |
| Multiple-mediator model | 0.018 (0.344) | −0.000 | −0.015, 0.014 | −0.340 (0.336) | 0.021 | −0.038, 0.109 | ||
| Pros of exercise | ||||||||
| Single-mediator model | 0.099 (0.091) | 0.433 (0.249) | 0.043 | −0.030, 0.155 | −0.061 (0.104) | 0.008 (0.250) | −0.000 | −0.034, 0.033 |
| Multiple-mediator model | 0.386 (0.321) | 0.038 | −0.034, 0.155 | −0.200 (0.287) | 0.012 | −0.036, 0.079 | ||
| Barriers efficacy | ||||||||
| Single-mediator model | −1.443 (1.995) | −0.012 (0.012) | 0.017 | −0.032, 0.091 | 3.974 (2.438) | 0.039 (0.011)** | 0.155 | −0.024, 0.387 |
| Multiple-mediator model | −0.015 (0.015) | 0.022 | −0.040, 0.113 | 0.033 (0.014)* | 0.131 | −0.018, 0.359 | ||
| Performance efficacy | ||||||||
| Single-mediator model | 3.325 (3.055) | −0.000 (0.009) | −0.001 | −0.067, 0.063 | 3.816 (3.341) | 0.018 (0.008)* | 0.069 | −0.041, 0.226 |
| Multiple-mediator model | 0.005 (0.010) | 0.017 | −0.049, 0.105 | 0.012 (0.009) | 0.046 | −0.034, 0.176 | ||
| Cognitive processes of change | ||||||||
| Single-mediator model | 0.036 (0.068) | 0.552 (0.332) | 0.020 | −0.052, 0.112 | 0.051 (0.071) | 0.040 (0.376) | 0.002 | −0.039, 0.046 |
| Multiple-mediator model | 0.858 (0.480) | 0.031 | −0.081, 0.172 | −0.284 (0.460) | −0.014 | −0.091, 0.040 | ||
| Behavioral processes of change | ||||||||
| Single Mediator Model | 0.274 (0.071)** | 0.036 (0.321) | 0.010 | −0.166, 0.189 | 0.248 (0.080)** | 1.046 (0.338)** | 0.259 | 0.066, 0.525a |
| Multiple-mediator model | −0.653 (0.482) | −0.179 | −0.483, 0.071 | 0.403 (0.463) | 0.100 | −0.118, 0.362 | ||
Significant mediator
p<0.05
p<0.01
Table 9.
Summary of significant cardiorespiratory fitness findings for women
| Single-mediator models |
Multiple-mediator models |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Longitudinal mediation |
Contemporaneous mediation |
Longitudinal mediation |
Contemporaneous mediation |
|||||||||
| Mediator | α | β | Med | α | β | Med | α | β | Med | α | β | Med |
| Cons of exercise | √ | |||||||||||
| Pros of exercise | ||||||||||||
| Barriers efficacy | √ | √ | ||||||||||
| Performance efficacy | √ | |||||||||||
| Cognitive processes of change | ||||||||||||
| Behavioral processes of change | √ | √ | √ | √ | √ | √ | ||||||
α the path from the intervention to the proposed mediating variable; β the path from the proposed mediating variable to the outcome variable; Med represents mediation (α * β)
Multiple-mediator Models
The multiple-mediator models were conducted to examine suppression effects and multicollinearity among the hypothesized mediators. Results from these models found no evidence of significant suppression. However, there was multicollinearity among hypothesized mediators in the contemporaneous mediator models, in both men and women and for both outcomes. As mentioned above, some of the mediators at the 24 month time point were highly correlated. Because of this, particularly for the behavioral processes of change, variables found to be significant in the single-mediator models were no longer significant when entered into a model simultaneously. These findings support our reasoning for testing mediation in both singleand multiple-mediator models.
Discussion
Theory-based interventions that assess specific mediating mechanisms have been recommended because they can significantly advance our understanding of PA behavior change [1–3]. Yet, relatively little is known regarding whether these interventions operate in the way specified by the underlying theory or conceptual schema. Mediator analyses may help to identify which variables and which theories are most effective for changing PA-related behaviors. The present study examined the 6 and 24 month psychosocial mediators of a 24-month primary care intervention aimed at increasing PA and CRF in men and women. We found that changes in the hypothesized mediators from baseline to 6 months did not significantly mediate the relationship between intervention group and PA or CRF change from 6 to 24 months (i.e., longitudinal models). Changes in behavioral processes of change from baseline to 24 months were found to be significant mediators of the relationship between intervention group and changes in PA and CRF from baseline to 24 months in both men and women (i.e., contemporaneous models).
We recognize that the lack of significant mediation found with the longitudinal models prevents us from establishing causality [46]. Caution is needed when interpreting the results from the contemporaneous models, as we cannot be certain that the intervention changed the behavioral processes of change first, which in turn increased PA and CRF. However, we feel that temporal precedence in our contemporaneous models can be justified empirically and theoretically, as decisions about the relationship between the mediators and outcomes were based on conceptual theory and prior empirical evidence [45]. Although longitudinal mediation can provide causal information, it may not capture all mediational relationships. The timing of measurements in mediation analyses is very important, as it is possible to miss relationships if the timing of the measures differs from the timing of the mediated effects [45, 47]. For example, it is possible that most of the change in mediators occurred between baseline and 3 months, which led to increases in PA and CRF from 3 to 24 months. In this case, contemporaneous mediational relationships may match the true temporal relationship more closely, and thus be more accurate than the longitudinal mediation models [45]. The lag between measures, particularly at time2 and time3 is quite lengthy (18 months); it is possible that changes in mediating and outcome variables occurred during this time period, but we were unable to capture them.
Mediation analyses allowed us to examine both the action theory (how the intervention changes the mediator, α path) and the conceptual theory (how the mediating variable affects the outcome variable, β path) aspects of the ACT intervention [48]. In cases where there is nonsignificant mediation, these types of analyses help identify which aspect failed, which may help improve future interventions. In examining the action theory aspect of the ACT, the intervention successfully changed three of the targeted mediators in a manner consistent with the TTM: pros of exercise (men only) and the cognitive (men only) and behavioral processes of change. A consistent finding for both men and women was the significant increase in the use of the behavioral processes of change, as measured at both 6 and 24 months. The consistent change in the behavioral processes of change across genders speaks to the robustness of the intervention, which included one-onone counseling, interactive mail, and for the counseling arm, telephone-based advice, in its ability to effectively teach participants how to use these processes in a manner that could produce meaningful changes. The lack of intervention effects for the other targeted TTM constructs could be due to a number of factors. For example, it is possible that the intervention components targeting these constructs were not intensive enough or were not functioning as anticipated. It is also possible that the intervention did change these constructs, but the measures used were not reliable or valid enough to detect change for the targeted population [49]. Our findings are consistent with other studies in that the intervention was able to successfully change certain TTM constructs, but not others [12, 15, 16].
In examining the conceptual theory aspect of the ACT, changes in many of the hypothesized mediators from baseline to 24 months were associated with changes in PA and CRF from baseline to 24 months in both men and women. The TTM posits that individuals will progress through the stages (and thus increase PA) when the pros of exercise increase and the cons decrease (i.e., a positive decisional balance), there is greater use of the cognitive (e.g., seeking out information about PA) and behavioral processes of change (e.g., rewarding oneself for being physically active), and self-efficacy increases [9, 50]. Our findings support the theoretical predictions of the TTM. Changes in the behavioral processes of change seemed especially important again, as changes were consistently related to increases in both outcomes for men and women. Changes in behavioral processes of change have been associated with changes in physical activity in other mediation studies based on the TTM [12, 14–16].
Despite significant α paths and β paths consistent with these theoretical models, mediation was established only for behavioral processes of change (e.g., commit yourself, substitute alternatives), and only in the less rigorous contemporaneous models. In the contemporaneous models, behavioral processes of change emerged as a mediator for men and women for both PA and CRF. This consistency across genders and outcomes points to the importance and strength of this variable in its potential ability to successfully change PA-related behaviors. The behavioral processes of change mediated 22–43% of the total effect of the intervention on changes in PA in CRF. Although these effects may be meaningful in a public health perspective (i.e., small changes can have large effects across a population), caution should be used when interpreting these findings, as the effect of the intervention was small and not statistically significant, with the exception of fitness in women.
The important role of the behavioral processes of change has been shown in several other studies [12, 14–16], including two conducted in primary care settings. Calfas and colleagues [16] examined whether a brief primary care PA intervention involving one behavioral counseling session by physicians was successful in changing hypothesized mediators, and whether changes in these mediators were associated with changes in PA at 6 weeks. Although they did not conduct mediation analyses per se, they also found that the intervention significantly increased behavioral processes of change, and changes in the behavioral processes were associated with significant changes in various PA-related outcomes [16]. Pinto et al. [15] examined similar relationships in a primary care PA intervention of physician counseling. They found that the intervention had a significant effect on behavioral processes of change at 6 weeks, and changes in behavioral processes were related to motivational readiness for PA at 6 weeks. Interestingly, this relationship held at 6 weeks, but at 8 months it was non-significant, perhaps suggesting the early impacts of changes in intervention-based mediators on PA behavior.
Lewis and colleagues reported in their review of PA interventions that behavioral processes of change were the most consistently reported mediator of PA behavior change in theoretically based PA interventions [5]. A recent study by Napolitano et al. found that behavioral processes of change were the only significant mediator for two different types of intervention arms (print and telephone separately compared to control) and PA at 6 months [14]. Consistent with our findings, these intervention arms were able to change other theoretical constructs (i.e., self-efficacy, decisional balance, and cognitive processes). However, because changes in these variables did not result in changes in PA [14], criteria for mediation were not met. Compared to Napolitano et al. [14], the missing links in the mediation chain for the present study were in opposite paths, as we had many significant β paths (strong conceptual theory), but fewer significant α paths (weaker action theory). It should be mentioned that Napolitano et al. [14] used a multiple mediator model; thus, it is possible that the lack of significant β paths were influenced by multicollinearity. Multicollinearity was an issue in our study, as significant β paths in the single-mediator models were sometimes no longer significant in a multiple-mediator model. This was particularly a problem for the behavioral processes of change, which were highly correlated with other tested mediators. The discrepancies discussed here illustrate the inconsistencies in mediator findings across PA intervention studies as described in the Lewis et al. [5] review.
The present findings, along with those reported in these other studies, suggest that interventions should incorporate strategies that specifically aim to increase participants’ use of behavioral processes of change such as encouraging participants to enlist social support, reward themselves for being active, or substitute alternatives for being active instead of sedentary. Although one may have expected the cognitive processes of change to act as mediators of PA change given participants enrolled in the ACT were currently inactive, research has shown that people use all ten processes when attempting to change PA behavior [10]. It has also been hypothesized that cognitive processes may change when a person decides to enroll in a PA intervention, which in theory would be before the actual start of the intervention [5]. Both of these are plausible explanations for our findings.
The lack of other significant mediators is a bit perplexing. There are several possible interpretations for these null findings. The “active” intervention arms (i.e., assistance and counseling) did seem effective in changing the targeted constructs, but it also appears that participants in the optimal standard care arm (i.e., physician advice) made changes in both the targeted mediators and PA behaviors. The TTM was developed by observing how people naturally and intentionally make behavioral changes (i.e., “self-help”) [9]. Therefore, it is possible that certain constructs/mediators were changed by participants regardless of intervention arm assignment. Brief structured advice by a physician might have yielded changes in some of these constructs, particularly the cognitive variables. Although changes in many of the targeted constructs (mediators) predicted changes in the PA/CRF outcomes, mediation as evaluated in the current study (i.e., intervention group significantly affects mediator which significantly affects outcome) was not shown for many of the constructs. This may reflect the greater intervention intensity needed to produce improvements in processes sufficient to be linked to behavior changes. Alternatively, these results may reflect shortcomings inherent in the specific methods we used in defining mediation, insufficient statistical power for discerning such mediational effects, or other methodological constraints. Furthermore, it is possible that some unmeasured variable (e.g., exercise enjoyment) was changed by the intervention and subsequently produced changes in PA and CRF.
This study had a number of strengths. CRF was assessed objectively for each participant using a maximal treadmill test, while PA was assessed with a valid self-report measure that was administered via a trained interviewer twice at each time point. All self-report measures used to assess mediators were shown to be reliable, valid measures in other studies. However, we do recognize the potential biases that accompany using any self-report measure. Second, this study had a large enough sample size to conduct gender-specific analyses. Third, the length of the intervention allowed us to examine changes across mediators and outcome variables at multiple time periods (i.e., 6 and 24 months). A limitation to our study was the sample, as they were predominantly White, generally highly educated, and had fairly high income levels. Our study findings may not generalize to other populations.
The present study contributes to the growing literature examining mediators of change in PA interventions. Mediation analyses improve understanding of how effective the intervention was in changing the targeted theoretical constructs and give insight into which constructs are associated with the desired PA-related outcomes. The present findings support the importance of targeting the behavioral processes of change, in both men and women, in PA interventions. Although no other variables were found to be significant mediators, we are not suggesting that behavioral processes should be the only variables targeted by PA interventions. The current relatively small literature of PA mediators is inconclusive, and is limited by sample sizes, analytic approaches, study duration, and inclusiveness of mediating constructs. More research examining a variety of potential mediating theoretical constructs, using appropriate statistical analyses, will assist in understanding which mediators are most important for achieving desired outcomes and how mediators may vary by subpopulation. A better understanding of the most important mediators will allow for more parsimonious interventions, as researchers can eliminate components that target theoretical constructs that are not as important for behavior change, and further emphasize those that do. Such streamlined interventions may be easier to develop, implement, and disseminate.
Acknowledgments
The Activity Counseling Trial was supported by the National Heart, Lung, and Blood Institute through contracts: N01-HC-45135, N01-HC-45136, N01-HC-45137, and N01-HC-45138.
This study was approved by the appropriate ethics committee, therefore being conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki, and all participants gave their informed consent prior to enrolling in the ACT.
We have no financial relationship with the organization sponsoring the ACT. We have full control over all primary data and we agree to allow the Annals of Behavioral Medicine to review our data if they request to.
The investigators express their appreciation to Activity Counseling Trial (ACT) participating physicians and other health professionals, participating patients, and the Data and Safety Monitoring Board, whose members were Albert Oberman (Chair), Rod Dishman, Patricia Dubbert, Elisa Lee, I-Min Lee, and Russell Pate. The following were ACT investigators at the Institutions designated at the time of completion of the trial. Clinical Centers: Cooper Institute for Aerobics Research/University of Texas Southwestern Medical Center, Steven Blair (Principal Investigator), Andrea Dunn, Larry Gibbons, Benjamin Levine (Co-Principal Investigator), Bess Marcus (Brown University), James Sallis (San Diego State University), and Peter Snell (UT SW Medical Center); The Stanford University School of Medicine, Abby King (Principal Investigator), Cheryl Albright, William Haskell, Lisa Palmer, Leslie Pruitt, and Wayne Phillips; University of Tennessee, Memphis, Mary O’Toole (Principal Investigator), William B. Applegate Consultant), Joyce Banton, Mace Coday, Karen C. Johnson, Robert C. Klesges (University of Memphis), Stephen T. Miller, and J. Lee Taylor. Coordinating Center: Wake Forest University School of Medicine, Timothy Morgan (Principal Investigator), Roger Anderson, Stuart Cohen, Mark Espeland, Walter Ettinger, Elizabeth Mayer-Davis, Michael Miller, Jack Rejeski (Wake Forest University), Paul Ribisl (Wake Forest University), Mary Ann Sevick, and Mara Vitolins. Central Laboratory: Penn Medical Laboratories, David Robbins. Project Office: National Heart, Lung, and Blood Institute, Denise Simons-Morton (Project Officer), P. Scott Allender, Eva Obarzanek, Joanna Shih, and Carolyn Voorhees.
Contributor Information
Meghan Baruth, Department of Exercise Science, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA
Sara Wilcox, Department of Exercise Science, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA
Andrea L. Dunn, Klein-Buendel, Inc., Golden, CO, USA
Abby C. King, Department of Health Research and Policy and the Stanford Prevention Research Center, Department of Medicine, Stanford University School of Medicine, Stanford, CA, USA
Bess H. Marcus, Behavioral and Social Sciences Section, Brown University Program in Public Health, Providence, RI, USA
W. Jack Rejeski, Department of Health and Exercise Science, Wake Forest University, Winston-Salem, NC, USA
James F. Sallis, Department of Psychology, San Diego State University, San Diego, CA, USA
Steven N. Blair, Department of Exercise Science, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA; Arnold School of Public Health, University of South Carolina, Columbia, SC, USA; Department of Epidemiology and Biostatistics, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA.
References
- 1.Marcus BH, Williams DM, Dubbert PM, et al. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation. 2006; 114: 2739–2752. [DOI] [PubMed] [Google Scholar]
- 2.Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? Am J Prev Med. 1998; 15:266–297. [DOI] [PubMed] [Google Scholar]
- 3.Bauman AE, Sallis JF, Dzewaltowski DA, Owen N. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med. 2002; 23: 5–14. [DOI] [PubMed] [Google Scholar]
- 4.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51: 1173–1182. [DOI] [PubMed] [Google Scholar]
- 5.Lewis BA, Marcus BH, Pate RR, Dunn AL. Psychosocial mediators of physical activity behavior among adults and children. Am J Prev Med. 2002; 23: 26–35. [DOI] [PubMed] [Google Scholar]
- 6.Riemsma RP, Pattenden J, Bridle C, et al. A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change. Health Technol Assess. 2002; 6: 1–231. [DOI] [PubMed] [Google Scholar]
- 7.Adams J, White M. Are activity promotion interventions based on the transtheoretical model effective? A critical review. Br J Sports Med. 2003; 37: 106–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adams J, White M. Why don’t stage-based activity promotion interventions work? Health Educ Res. 2005; 20: 237–243. [DOI] [PubMed] [Google Scholar]
- 9.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992; 47: 1102–1114. [DOI] [PubMed] [Google Scholar]
- 10.Marshall SJ, Biddle SJ. The transtheoretical model of behaviour change: a meta-analysis of applications to physical activity and exercise. Ann Behav Med. 2001; 23: 229–246. [DOI] [PubMed] [Google Scholar]
- 11.Marcus BH, Simkin LR. The stages of exercise behavior. J Sports Med Phys Fitness. 1993; 33: 83–88. [PubMed] [Google Scholar]
- 12.Lewis BA, Forsyth LH, Pinto BM, Bock BC, Roberts M, Marcus BH. Psychosocial mediators of physical activity in a randomized controlled intervention trial. J Sport Exerc Psychol. 2006; 28: 193–204. [Google Scholar]
- 13.Rabin C, Pinto BM, Frierson GM. Mediators of a randomized controlled physical activity intervention for breast cancer survivors. J Sport Exerc Psychol. 2006; 28: 269–284. [Google Scholar]
- 14.Napolitano MA, Papandonatos GD, Lewis BA, et al. Mediators of physical activity behavior change: a multivariate approach. Health Psychol. 2008; 27: 409–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pinto BM, Lynn H, Marcus BH, DePue J, Goldstein MG. Physician-based activity counseling: intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med. 2001; 23: 2–10. [DOI] [PubMed] [Google Scholar]
- 16.Calfas KJ, Sallis JF, Oldenburg B, Ffrench M. Mediators of change in physical activity following an intervention in primary care: PACE. Prev Med. 1997; 26: 297–304. [DOI] [PubMed] [Google Scholar]
- 17.Fahrenwald NL, Atwood JR, Johnson DR. Mediator analysis of moms on the move. West J Nurs Res. 2005; 27: 271–291. [DOI] [PubMed] [Google Scholar]
- 18.Smith BJ. Promotion of physical activity in primary health care: update of the evidence on interventions. J Sci Med Sport. 2004; 7: 67–73. [DOI] [PubMed] [Google Scholar]
- 19.King AC, Sallis JF, Dunn AL, et al. Overview of the Activity Counseling Trial (ACT) intervention for promoting physical activity in primary health care settings. Activity Counseling Trial Research Group. Med Sci Sports Exerc. 1998; 30: 1086–1096. [DOI] [PubMed] [Google Scholar]
- 20.Blair SN, Applegate WB, Dunn AL, et al. Activity Counseling Trial (ACT): rationale, design, and methods. Activity Counseling Trial Research Group. Med Sci Sports Exerc. 1998; 30: 1097–1106. [DOI] [PubMed] [Google Scholar]
- 21.The Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care: the Activity Counseling Trial: a randomized controlled trial. JAMA. 2001; 286: 677–687. [DOI] [PubMed] [Google Scholar]
- 22.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995; 273: 402–407. [DOI] [PubMed] [Google Scholar]
- 23.American College of Sports Medicine position stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness in healthy adults. Med Sci Sports Exerc. 1990; 22: 265–274. [PubMed] [Google Scholar]
- 24.Simons-Morton DG, Hogan P, Dunn AL, et al. Characteristics of inactive primary care patients: baseline data from the activity counseling trial. For the Activity Counseling Trial Research Group. Prev Med. 2000; 31: 513–521. [DOI] [PubMed] [Google Scholar]
- 25.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985; 121: 91–106. [DOI] [PubMed] [Google Scholar]
- 26.Blair SN, Haskell WL, Ho P, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985; 122: 794–804. [DOI] [PubMed] [Google Scholar]
- 27.Dunn AL, Marcus BH, Kampert JB, et al. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999; 281: 327–334. [DOI] [PubMed] [Google Scholar]
- 28.King AC, Castro C, Friedman R, et al. Ongoing physical activity advice by humans versus computers: the Community Health Advice by Telephone (CHAT) trial. Health Psychol. 2007; 26: 718–727. [DOI] [PubMed] [Google Scholar]
- 29.Dubbert PM, Vander Weg MW, Kirchner KA, Shaw B. Evaluation of the 7-day physical activity recall in urban and rural men. Med Sci Sports Exerc. 2004; 36: 1646–1654. [DOI] [PubMed] [Google Scholar]
- 30.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000; 71: S1–14. [PubMed] [Google Scholar]
- 31.Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-day PAR. Med Sci Sports Exerc. 2003; 35: 801–809. [DOI] [PubMed] [Google Scholar]
- 32.Gross LD, Sallis JF, Buono MJ, Roby JJ, Nelson JA. Reliability of interviewers using the Seven-Day Physical Activity Recall. Res Q Exerc Sport. 1990; 61: 321–325. [DOI] [PubMed] [Google Scholar]
- 33.Jacobs DR Jr, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993; 25: 81–91. [DOI] [PubMed] [Google Scholar]
- 34.Washburn RA, Jacobsen DJ, Sonko BJ, Hill JO, Donnelly JE. The validity of the Stanford Seven-Day Physical Activity Recall in young adults. Med Sci Sports Exerc. 2003; 35: 1374–1380. [DOI] [PubMed] [Google Scholar]
- 35.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982; 14: 377–381. [PubMed] [Google Scholar]
- 36.American College of Sport Medicine. Guidelines for exercise testing and prescription. 5th ed. Baltimore: Williams and Wilkins; 1995. [Google Scholar]
- 37.Garcia AW, King AC. Predicting long-term adherence to aerobic exercise: a comparison of two models. J Sport Exerc Psychol. 1991; 13: 394–410. [Google Scholar]
- 38.Bandura A Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice Hall; 1986. [Google Scholar]
- 39.Wilcox S, Sharpe PA, Hutto B, Granner ML. Psychometric properties of the self-efficacy for exercise questionnaire in a diverse sample of men and women. J Phys Act Health. 2005; 3: 285–297. [Google Scholar]
- 40.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992; 11: 257–261. [DOI] [PubMed] [Google Scholar]
- 41.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992; 63: 60–66. [DOI] [PubMed] [Google Scholar]
- 42.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992; 11: 386–395. [DOI] [PubMed] [Google Scholar]
- 43.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V.A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002; 7: 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: program PRODCLIN. Behav Res Methods. 2007; 39: 384–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.MacKinnon DP. Introduction to statistical mediation analysis. New York: Taylor and Francis Group, LLC; 2008. [Google Scholar]
- 46.Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001; 158: 848–856. [DOI] [PubMed] [Google Scholar]
- 47.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002; 59: 877–883. [DOI] [PubMed] [Google Scholar]
- 48.Cerin E, Mackinnon DP. A commentary on current practice in mediating variable analyses in behavioural nutrition and physical activity. Public Health Nutr. 2008; 12: 1182–1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.MacKinnon DP. Analysis of mediating variables in prevention and intervention research. NIDA Research Monograph Series. 1994; 139: 127–153. [PubMed] [Google Scholar]
- 50.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997; 12: 38–48. [DOI] [PubMed] [Google Scholar]