Abstract
Background
Surgery performed to improve or replace the function of the diseased urinary bladder has been carried out for over a century. Main reasons for improving or replacing the function of the urinary bladder are bladder cancer, neurogenic bladder dysfunction, detrusor overactivity and chronic inflammatory diseases of the bladder (such as interstitial cystitis, tuberculosis and schistosomiasis). There is still much uncertainty about the best surgical approach. Options available at the present time include: (1) conduit diversion (the creation of various intestinal conduits to the skin) or continent diversion (which includes either a rectal reservoir or continent cutaneous diversion), (2) bladder reconstruction and (3) replacement of the bladder with various intestinal segments.
Objectives
To determine the best way of improving or replacing the function of the lower urinary tract using intestinal segments when the bladder has to be removed or when it has been rendered useless or dangerous by disease.
Search methods
We searched the Cochrane Incontinence Group Specialised Trials Register (searched 28 October 2011), which contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and CINAHL, and handsearching of journals and conference proceedings, and the reference lists of relevant articles.
Selection criteria
All randomised or quasi‐randomised controlled trials of surgery involving transposition of an intestinal segment into the urinary tract.
Data collection and analysis
Trials were evaluated for appropriateness for inclusion and for risk of bias by the review authors. Three review authors were involved in the data extraction. Data were combined in a meta‐analysis when appropriate.
Main results
Five trials met the inclusion criteria with a total of 355 participants. These trials addressed only five of the 14 comparisons pre‐specified in the protocol. One trial reported no statistically significant differences in the incidence of upper urinary tract infection, uretero‐intestinal stenosis and renal deterioration in the comparison of continent diversion with conduit diversion. The confidence intervals were all wide, however, and did not rule out important clinical differences. In a second trial, there was no reported difference in the incidence of upper urinary tract infection and uretero‐intestinal stenosis when conduit diversions were fashioned from either ileum or colon. A meta‐analysis of two trials showed no statistically significant difference in daytime or nocturnal incontinence amongst participants who were randomised to ileocolonic/ileocaecal segment bladder replacement compared to an ileal bladder replacement. However, one small trial suggested that bladder replacement using an ileal segment compared to using an ileocolonic segment may be better in terms of lower rates of nocturnal incontinence. There were no differences in the incidence of dilatation of upper tract, daytime urinary incontinence or wound infection using different intestinal segments for bladder replacement. However the data were reported for 'renal units', but not in a form that allowed appropriate patient‐based paired analyses. No statistically significant difference was found in the incidence of renal scarring between anti‐refluxing versus freely refluxing uretero‐intestinal anastomotic techniques in conduit diversions and bladder replacement groups. Again, the outcome data were not reported as paired analysis or in form to carry out paired analysis.
Authors' conclusions
The evidence from the included trials was very limited. Only five studies met the inclusion criteria; these were small, of moderate or poor methodological quality, and reported few of the pre‐selected outcome measures. This review did not find any evidence that bladder replacement (orthotopic or continent diversion) was better than conduit diversion following cystectomy for cancer. There was no evidence to suggest that bladder reconstruction was better than conduit diversion for benign disease. The clinical significance of data from one small trial suggesting that bladder replacement using an ileal segment compared to using an ileocolonic segment is better in terms of lower rates of nocturnal incontinence is uncertain. The small amount of usable evidence for this review suggests that collaborative multi centre studies should be organised, using random allocation where possible.
Plain language summary
Urinary diversion and bladder reconstruction/replacement using intestinal segments for intractable incontinence following bladder surgery
The normal urinary bladder is a hollow muscular organ that lies deep in the pelvis. It functions through the balanced activity of many inter‐related nerves and muscles that contain or empty urine as needed. If the bladder has been damaged by disease, surgery can be performed to divert the urine from the bladder (urinary diversion), to reconstruct the bladder or to replace the bladder with intestinal segments. The review did not find enough evidence from trials to show which surgical options are the most effective. One small trial suggested that the ileum bowel segment (small bowel) may be better compared to ileocolonic bowel segment (combination of small and large bowel) for night time incontinence. More research is needed to determine the most effective surgical methods for urinary diversion, reconstruction or replacement of the urinary bladder that has been damaged by disease.
Background
For over a century, urological surgeons have grappled with the problem of how to improve or replace the function of the lower urinary tract when it has been rendered useless or dangerous by disease.
The lower urinary tract consists of the bladder (reservoir), urethra (conduit) and sphincters (continent mechanism). The normal urinary bladder is a hollow muscular organ that lies deep in the pelvis. It functions through the balanced activity of many inter‐related neural and muscular structures. Co‐ordinated reflex activity of the detrusor muscle and sphincter complex results in a low‐pressure reservoir for urine storage that is capable of complete emptying through the urethra, in addition to allowing continence between voids. The ideal bladder replacement would have the following attributes:
(1) good volume with low pressure storage; (2) socially acceptable voluntary and complete efficient emptying either by valsalva or clean intermittent self catheterisation (CISC); (3) allows continence between voids; (4) protection of upper urinary tract (kidney and ureter); (5) avoidance of harmful long term sequelae and optimise quality of life; (6) cost effective.
When the bladder has to be removed or when it has been rendered useless or dangerous by disease, the solutions have ranged from: (a) urinary diversion: (i) conduit diversion (the creation of various intestinal conduits to the skin); (ii) continent diversion (simple drainage by anastomosis (surgical joining) of the ureters to the colon (ureterosigmoidostomy), which include either a rectal reservoir or continent cutaneous diversion); (b) the reconstruction of the bladder; or (c) replacement of the bladder with various intestinal segments.
Terminology
We used the term continent diversion strictly to mean continent cutaneous diversion, uretero‐sigmoidostomy and the newer variants of uretero‐sigmoidostomy. By bladder reconstruction we meant that the native bladder was surgically manipulated to improve its function. Whilst for the purpose of this review we only assessed the surgical procedures that made use of intestinal segments as part of the bladder reconstruction (e.g. augmentation cystoplasty or enterocystoplasty), we acknowledge that the true meaning also includes other procedures like detrusor myectomy or auto‐augmentation. The terms bladder replacement or substitution were used to mean that the native bladder was removed completely and a new reservoir created, positioned where the native bladder used to be and connected to the native urethra, therefore allowing patients to void in a natural way. The term "undiversion" was taken to mean conversion from conduit to bladder reconstruction, bladder replacement or continent diversion.
Principles underlying the various surgical options are outlined below:
a) Urinary diversion
Conduit (incontinent) diversion
The ureters are disconnected from the native bladder and anastomosed to the proximal end of a 15 cm (approximately) isolated bowel segment (Bricker 1950). The distal end of the bowel segment is brought out through the abdominal wall as a stoma to which a bag is attached to collect the draining urine. Whilst traditionally, small intestine is used, large intestine has also been used.
Continent diversion
i) Continent cutaneous diversion
This involves the creation of a low pressure reservoir of good capacity using a detubularised intestinal segment technique pioneered by Kock et al (Kock 1982). The disconnected ureters are anastomosed to the reservoir. Various techniques can be used to maintain continence. In the nipple valve principle, the valve protrudes into the reservoir cavity and as the reservoir fills, the valve is compressed preventing incontinence. The flap valve technique relies on the proximal segment of the continence channel running on the inner wall of the reservoir. As the reservoir fills, the channel is compressed preventing incontinence. An alternative approach is to use a flap valve. The most popular type of flap valve is the appendix implanted into the reservoir (Mitrofanoff principle). The distal end of the continence channel is brought out as a stoma through the abdominal wall for clean intermittent self‐catheterisation, thus avoiding use of a stoma bag. The main difference compared to the conduit diversion is that the reservoir is internal rather than external (stoma bag use).
ii) Rectal reservoir
Classical ureterosigmoidostomy has been replaced with the more modern low‐pressure rectal reservoir. The ureters are anastomosed to the rectum which acts as the reservoir and the anal sphincter employed to maintain continence. In some of these techniques, attempts are made to limit the admixture of urine and faeces and, in some cases, this involves disconnecting the sigmoid colon and either bringing it out as a stoma or, more commonly, through the perineum. By doing the latter, both urinary and bowel control can be maintained. Some techniques use proximal intussusception of the sigmoid colon to confine urine to a smaller surface area hence limiting the metabolic disturbance seen in the classical ureterosigmoidostomy (Kock 1988).
b) Bladder reconstruction
Augmentation cystoplasty/enterocystoplasty
Mikulicz in 1899 (Mikulicz 1899) was the first to describe using a segment of ileum to perform an augmentation onto a coronally bisected human bladder. Clam enterocystoplasty described by Bramble (Bramble 1982; Bramble 1990) was therefore a modified technique and involved the incorporation of a detubularised isolated bowel segment onto a near‐complete sagittally bisected bladder.
c) Bladder replacement or substitution
Orthotopic neobladder In orthotopic (in the normal or usual place) bladder replacement, creation of the neobladder and its anastomosis to the disconnected ureters uses the same principles as in continent cutaneous diversion surgery. For the outlet, the reservoir is anastomosed to the native urethra and therefore patients can maintain continence (if the native sphincter mechanism is still intact) and void via their native urethra. If patients encounter difficulty emptying the reservoir, they can perform clean intermittent self‐catheterisation (CISC). The proportion needing to perform CISC following orthotopic reconstruction varied in different series from 0% to 70%. The remaining patients learnt to recognise when the neo‐bladder was full and strained to void. The technique of CISC is well tolerated (Lapides 1972; Webb 1990).
Regardless of the bowel segment used to augment or create a neo‐bladder, results were relatively satisfactory if the bowel was detubularised and a spherical‐shaped reservoir created. Contractile activity thereafter became discontinuous and disorganised reducing the pressure within the reconstructed bladder hence decreasing the chances of post‐operative incontinence. Critical to the success of any urinary diversion is the creation of a safe uretero‐intestinal anastomosis that is prone neither to leakage nor stricture. As a freely refluxing anastomosis could lead to upper tract dilatation in the presence of phasic intestinal contractions (Neal 1989), the alternative historically, was the use of an anti‐reflux anastomotic technique. However, this carried a higher risk of upper tract obstruction because of stricture formation. More recently, Stüder et al (Studer 1996) reported that the deleterious effect of reflux could be eliminated by implantation of the ureters into an afferent, tubular, iso‐peristaltic 20 cm length of ileum without the use of an anti‐reflux anastomotic technique. There is therefore a dilemma between the use of a refluxing anastomosis with a reportedly lower stricture rate, but with the potential to cause renal damage and the use of an anti‐refluxing anastomosis with a reportedly higher stricture rate, but with less potential to cause renal damage (if not stenotic).
Reasons for urinary diversion or bladder reconstruction /replacement
The main indications for performing a urinary diversion or a bladder reconstruction/replacement using transposed intestinal segments are bladder cancer, neurogenic bladder dysfunction, idiopathic detrusor overactivity and chronic inflammatory conditions (such as interstitial cystitis, tuberculosis, schistosomiasis and post‐radiation bladder contraction).
Bladder cancer
People with muscle invasive bladder cancer require aggressive treatment which usually means either radiotherapy or cystectomy (surgery to remove the bladder) with or without chemotherapy. If the decision is radical cystectomy, the choice of how to replace lower urinary tract function rests between conduit diversion, bladder replacement or continent diversion.
Neurogenic bladder dysfunction
This may result from congenital or acquired disorders (e.g. neural tube defect or spinal cord injured patients) and can present clinically in a number of ways including frequency, urgency, urinary incontinence, intermittency, urinary retention or urinary tract infections. Dysfunction of the lower urinary tract may result in vesico‐ureteric reflux or impaired drainage of the ureters resulting in hydronephrosis. Before the era of clean intermittent self‐catheterisation (CISC), many patients with neurogenic bladder dysfunction had their urine diverted by means of an ileal conduit when conservative measures failed. Nowadays, however, the options would include either bladder reconstruction, replacement or continent diversion. The main indications for such surgery in this group of patients include intractable incontinence, deteriorating renal function and high bladder pressures.
Detrusor overactivity
Detrusor overactivity is characterised by detrusor (bladder wall muscle) contractions either spontaneously or on provocation during the filling phase while the patient is attempting to inhibit micturition. The urological management of people with detrusor instability (DI) is difficult (Couillard 1995). Patients with severe detrusor instability are distressed by urinary incontinence and often desperate for treatment. The majority of patients with detrusor instability are treated conservatively using drug therapy, transcutaneous electrical nerve stimulation or S3‐neuromodulation. If conservative measures fail however, surgery which may involve transposition of intestinal segments into the urinary tract (e.g. Clam enterocystoplasty) can provide effective treatment for some patients (George 1991; Kockelbergh 1991; Lewis 1990; Sethia 1991).
Chronic inflammatory disorders of the bladder
(a) Interstitial Cystitis Idiopathic interstitial cystitis is a chronic inflammatory bladder disorder of unknown aetiology (Hanno 1990; Thompson 1996). In most patients conservative treatments produce only temporary relief and in some there is progressive deterioration which often culminates in a request for surgical treatment. The options range from ileal conduit diversion to orthotopic bladder replacement, but choosing patients who will benefit from surgery is difficult.
(b) Tuberculosis The World Health Organisation estimates that there are approximately 10 million new cases of all forms of tuberculosis each year predominantly affecting people living in developing countries. It is estimated that between 8 to 20 % of patients with pulmonary tuberculosis have Mycobacterium tuberculosis in their urine. Tuberculosis can affect the entire genito‐urinary tract. When it affects the bladder, it may result in intolerable frequency, pain, urgency and haematuria. The bladder can become small, contracted and incapable of holding more than 100 ml of urine, which may lead to treatment by augmentation cystoplasty.
The purpose of the review was to provide an easily accessible, periodically updated, comprehensive systematic review which would not only help to identify optimal practice, but also highlight gaps in the evidence base.
Objectives
To determine the best way of improving or replacing the function of the lower urinary tract using intestinal segments when the bladder has to be removed or when it had been rendered useless or dangerous by disease.
The following comparisons were pre‐stated:
(1) whether continent diversion is better than conduit diversion;
(2) whether bladder reconstruction is better than conduit diversion;
(3) whether bladder reconstruction is better than continent diversion;
(4) whether bladder reconstruction is better than bladder replacement;
(5) whether bladder replacement is better than conduit diversion;
(6) whether bladder replacement is better than continent diversion;
(7) whether one form of continent diversion is better than another;
(8) whether use of an intestinal segment from one part of the gut for bladder reconstruction is better than a segment from another part;
(9) whether use of an intestinal segment from one part of the gut for bladder replacement is better than a segment from another part;
(10) whether use of an intestinal segment from one part of the gut for continent cutaneous diversion is better than a segment from another part;
(11) whether use of an intestinal segment from one part of the gut for conduit diversion is better than a segment from another part;
(12) whether the use of an anti‐reflux uretero‐intestinal anastomotic technique is better than a freely refluxing anastomosis in bladder replacement;
(13) whether the use of an anti‐reflux uretero‐intestinal anastomotic technique is better than a freely refluxing anastomosis in continent diversion;
(14) whether the use of an anti‐reflux uretero‐intestinal anastomotic technique is better than a freely refluxing anastomosis in conduit diversion.
Whilst we understood that there were important issues of choice within these broad groups, which deserved a review of the evidence in their own right, for instance, choice of continence mechanism in bladder replacement or the choice of outlet in continent cutaneous diversion, these were not considered in this review.
Methods
Criteria for considering studies for this review
Types of studies
All randomised or quasi‐randomised controlled trials of surgery involving transposition of an intestinal segment into the urinary tract.
Types of participants
All patients that underwent surgery involving transposition of an intestinal segment to improve or replace lower urinary tract function. No exclusions were based on age or sex.
Types of interventions
Eligible studies would include one or more of the following:
Conduit diversion
Continent diversion
Bladder reconstruction (only those using intestinal segments)
Bladder replacement / substitution
Types of outcome measures
Quality of life
General measures of health status ‐ Short Form 36 (Ware 1993)
Disease specific measures of quality of life
Other measures of patient satisfaction (including sexual function)
Patient symptoms
Lower urinary tract infection (frequency and hospital admissions)
Upper urinary tract infection (frequency and hospital admissions)
Clean intermittent self catheterisation rates
Mucus
‐ catheter blockage ‐ urostomy pouch blockage ‐ patient complaint
Bowel dysfunction
‐ diarrhoea ‐ faecal urgency ‐ faecal incontinence ‐ flatus leakage ‐ constipation
Urinary incontinence (daytime and night‐time)
Odour
Stoma stenosis / hernia
Clinical end points
Need for re‐operation
Operative complications
Post‐operative morbidity / mortality
Length of operation
Length of hospital stay
Anastomotic leak (bowel or bladder)
Health economic measures
Cost of the alternative managements
Cost consequence of effects of management
Formal cost‐effectiveness analyses
Physiological/radiological measures
Active reflux
Upper tract dilatation
Urinary stones (lower and upper)
Bone disease
Vitamin B12 deficiency
Metabolic acidosis / alkalosis
Bile acid malabsorption
Hepatic encephalopathy
Deterioration of glomerular filtration rate
Renal failure
Renal scarring
Urodynamic measures
Endoscopic assessment
Cancer development
Search methods for identification of studies
We did not impose any language or other restrictions on any of these searches detailed below.
Electronic searches
This review has drawn on the search strategy developed for the Incontinence Review Group. We identified relevant trials from the Group's Specialised Register of controlled trials which is described under the Incontinence Group's module in The Cochrane Library. The register contains trials identified from MEDLINE, CINAHL, The Cochrane Central Register of Controlled Trials (CENTRAL) and handsearching of journals and conference proceedings. The Incontinence Group's register was last searched on 28 October 2011 using the Group's own keyword system, the search terms used were: ({design.cct.*} OR {design.rct.*}) AND topic.urine* AND ({intvent.surg.bladdistension.} OR {intvent.surg.cystoscopy.} OR {intvent.surg.diathermy.} OR {intvent.surg.diversion.*} OR {intvent.surg.neurological.} OR {intvent.surg.self‐dilatation.} OR {intvent.surg.sphincterectomy.} OR {intvent.surg.sphincterotomy.} OR {intvent.surg.urethrotomy.} OR {intvent.surg.cryosurgery.} OR {intvent.surg.gynaecology.}) (All searches were of the keyword field of Reference Manager 12, Thomson Reuters).
The trials in the Incontinence Group's Specialised Register are also partially contained in CENTRAL.
For the previous version of this review extra specific searches were performed. These are detailed in Appendix 1, including the search terms used.
Searching other resources
The reference lists of relevant articles were searched for other possible relevant trials.
Data collection and analysis
Selection of studies
The reports of all possibly eligible studies were evaluated for risk of bias and appropriateness for inclusion by the reviewers without prior consideration of the results. Any disagreements were resolved by discussion. Where these were not resolved, arbitration rested with a third person. Studies were excluded if they were not randomised or quasi‐randomised trials for patients with intractable incontinence or following cystectomy. Excluded studies were listed with reasons for their exclusion.
Data extraction and management
Data extraction were undertaken independently by the reviewers and cross checked. Where data may have been collected but not reported, clarification was sought from the trialists. Included trial data was processed as described in the Cochrane Collaboration Handbook (Higgins 2011). Information on the characteristics of participants and interventions as well as on the pre‐specified outcome measures was extracted for each trial.
Assessment of risk of bias in included studies
Assessment of risk of bias was undertaken by each reviewer using the Cochrane Collaboration's Risk of Bias tool which included quality of random allocation and concealment, description of dropouts and withdrawals, analysis by intention to treat, and 'blinding' during treatment and at outcome assessment.
Measures of treatment effect
For dichotomous outcomes we related the numbers reporting an outcome to the numbers at risk in each group to derive a risk ratio, and for continuous variables we used means and standard deviations to derive a weighted mean difference, both with 95% confidence intervals (CIs). The intention had been to undertake meta‐analysis, when appropriate, using a fixed effects model and exploring differences between trials if significant heterogeneity was found or appeared obvious from visual inspection of the results.
If appropriate, the results of included studies were combined for each outcome in a formal meta‐analysis to produce an overall estimate of treatment effect. were derived using a fixed effects model and for continuous data weighted mean differences (WMD ‐ weighted by the inverse of the variance)
Assessment of heterogeneity
Heterogeneity amongst studies was explored by means of a visual inspection of the graphical plot of the results and formally by the Chi‐squared test and I square test. In case of considerable statistical heterogeneity (e.g. significance level less than 0.10) with no clear explanation, the reviewers adopted the following options:
to exclude the results of studies that contributed most variation and repeat the analysis (recalculating the summary measure of effect and the heterogeneity statistics for the remaining studies) until no heterogeneity is present;
to use both a fixed and a random effects model to see if they give substantially different results.
Data synthesis
If appropriate, the results of included studies were combined for each outcome in a formal meta‐analysis to produce an overall estimate of treatment effect using a fixed effects model
Sensitivity analysis
Although trials with participants of different aetiologies for the purpose of analysis were grouped together, we recognised that the outcomes may have been different. For instance, mortality in patients having surgery because of bladder cancer would have been expected to be different to that for benign disease. We therefore planned to perform sensitivity analysis for such patient groups. However, in the event this was not possible because no data were available on mortality.
Results
Description of studies
Results of the search
For this review 51 records were screened and 35 full text articles were retrieved; of these 25 reports were excluded with reasons given in the Characteristics of excluded studies table. Ten reports of five studies met the eligibility criteria and were included (Chen 2009; Khafagy 2006; Kristjansson 1995; Shaaban 2006; Studer 1996). Please see the PRISMA diagram in Figure 1 for the flow of literature through the assessment process.
1.
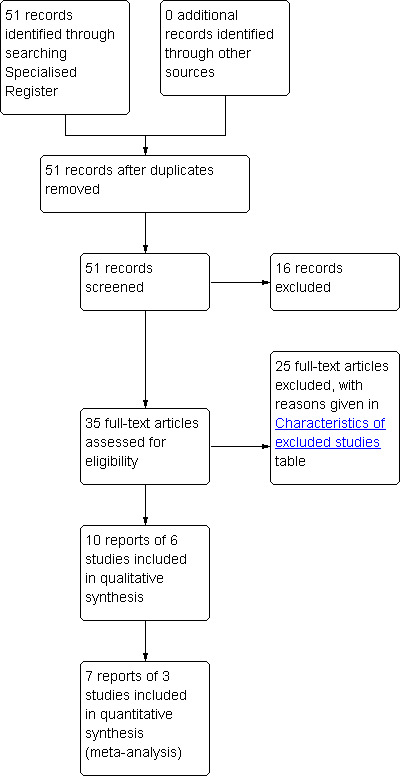
PRISMA study flow diagram.
Included studies
The five included trials had a total of 355 participants (Chen 2009; Khafagy 2006; Kristjansson 1995; Shaaban 2006; Studer 1996). All were randomised trials. For two trials (Kristjansson 1995; Studer 1996) the report of longer‐term follow‐up was considered as the primary report by the reviewers. The first of these two trials (Studer 1996) was originally carried out in 1991 (Studer 1991) and the second (Kristjansson 1995a) in 1989 (Mansson 1989). This trial (Mansson 1989), had essentially one subsequent follow‐up report with different outcome measures reported in two papers in the same volume of the British Journal of Urology. These two follow‐up papers had the same first author (Kristjansson 1995). The first paper, which had the same outcome measures (renal function, uretero‐intestinal strictures and incidence of urinary tract infections) as the original report (Mansson 1989), was assigned as the primary reference (Kristjansson 1995a) as it had the longest follow‐up on the original group of patients studied. The second paper by Kristjansson et al (Kristjansson 1995b) reported on the incidence of renal scarring (determined by renal scintigraphy) and location of bacteriuria (detected by urine sampling from the conduit and direct renal pelvis percutaneous aspiration). Whilst Studer refers to the afferent ileal tubular segment as a dynamic anti‐reflux device under low pressure conditions (Studer 1996), the anastomosis of the ureters to the ileal segment is that of a freely refluxing anastomosis and for the purposes of this review is classified as such.
Two trials (Khafagy 2006; Chen 2009) compared the outcomes of two different types of bowel segments used for bladder replacement and Shaaban et al (Shaaban 2006) reported outcomes of refluxing and anti‐refluxing techniques of uretero‐enteric anastomosis in bladder replacement surgery.
Excluded studies
Twenty five studies were excluded. Eleven were excluded because they did not fulfil the criteria of the review (Davidsson 1996; Degen 1997; El 2002; Ghoneim 1988; Lampel 1995; Lightfoot 2007; Mansson 2004; Mattei 2008; Morey 2006; Osman 2004; Osman 2009; Shaaban 1992; Shokeir 1995; Thakar 1998; Vakalopoulos 2011). Nine studies were excluded principally because they were not prospective randomised trials (Bassi 1996; Boyd 1987; Brough 1998; De Carli 1997; Kolettis 1996; Mansson 1997; Okada 1989; Speakman 1989; Studer 1997). One further study (Ghoneim 1981) appeared to fulfil the criteria of the review, but was not included as the authors did not report the number of patients in each treatment group. This omission did not allow analysis of the data presented. This trial compared refluxing versus non‐refluxing techniques in a continent diversion (ureterosigmoidostomy) looking at outcome measures of upper tract dilatation and incidence of day / night time incontinence. The reviewers are attempting to contact the authors about providing further data, and will update the review accordingly if successful.
Comparisons on interventions and outcome measures
The first included trial (Studer 1996) compared an anti‐reflux mechanism (anti‐reflux nipple) against a refluxing mechanism (afferent ileal tubular segment). Outcome measures that this trial looked at included number of patients with pyelonephritis (no incidence of hospitalisation mentioned), number with urinary incontinence, number with uretero‐intestinal stenosis and physiological / radiological measures such as the incidence of active reflux, upper tract dilatation, lower urinary stones, vitamin B12 deficiency and increase in kidney size.
Kristjamsson et al (Kristjansson 1995) compared (1) Continent diversion vs Conduit diversion, (2) Anti‐reflux mechanism vs refluxing mechanism for the conduit diversion and (3) One segment (ileal) vs another (colon) for conduit diversion. Outcome measures for the first comparison (continent vs conduit diversion) included the number of patients with upper urinary tract infection (no incidence of hospitalisation mentioned), number with uretero‐intestinal stenosis and physiological / radiological measures such as the glomerular filtration rate and presence of renal scarring as measured by renal scintigraphy. The outcome measures for the second comparison (anti‐reflux vs reflux for conduit diversion) included physiological / radiological measures such as the presence of renal scarring as measured by renal scintigraphy. Finally, the outcome measure for the third comparison (one segment vs another for conduit diversion) included the number of patients with upper urinary tract infection (no hospitalisation mentioned), number with uretero‐intestinal stenosis and physiological / radiological measures such as the glomerular filtration rate and presence of renal scarring as determined by renal scintigraphy.
Khafagy and Chen (Chen 2009; Khafagy 2006) compared the outcomes of two different types of bowel segments used in bladder replacement. Khafagy (Khafagy 2006) compared ileocaecal with an ileal segment (Studer technique) and Chen (Chen 2009) compared ileocolonic (Le Bag technique) with an ileal segment. Le Bag technique used in the Chen (Chen 2009) study used a freely refluxing Bricker anastomosis where as in the Khafagy trial (Khafagy 2006) the ileocaecal procedure was non‐refluxing. Both trials included outcomes measures on early complications (urinary leakage, wound infections etc.) urinary incontinence; serum biochemistry and radiological changes of the upper tract as seen on intravenous urograms.
Shaaban et al (Shaaban 2006) compared outcomes of refluxing and anti‐refluxing techniques of uretero‐enteric anastomosis in patients with bladder replacement. Renal units ( left or right) were randomised to techniques in the same patient. Randomisation was carried out for the technique and not for the patients. Outcomes of interest in this study were: early complications; dilatation of upper tract ( including due to strictures); follow‐up glomerular filtration rates; and requirement of secondary surgical interventions.
Participants and sample characteristics
Studer et al (Studer 1996) had a total number of 70 participants with 35 allocated to the group with the anti‐reflux nipple mechanism and 35 to the remaining group with the refluxing mechanism (afferent ileal tubular segment). All the trial patients were male with a median age of 66.6 years in the anti‐reflux nipple mechanism group and 63.8 years in the afferent ileal tubular segment group. The reported median follow‐up was 57 months for the group with the anti‐reflux nipple mechanism and 45 months for the group with the afferent ileal tubular segment. There was no specific mention of the inclusion criteria of patients into the trial, although it was reported that a proportion of the patients underwent radical cystectomy and subsequent bladder replacement for bladder cancer.
Kristjansson et al (Kristjansson 1995) originally had 94 participants in their trial as reported in 1989, with 38 patients prospectively randomised to have formation of ileal conduit, 30 patients had formation of colonic conduit and the remaining 26 patients had formation of a continent caecal reservoir. The authors reported that only 56 patients were evaluable at the end of the study period with 38 unevaluable patients. No reasons were given as to why these 38 patients were not evaluable. Therefore, the final numbers for the purposes of evaluation were: 18 patients for the ileal conduit group, 20 patients for the colonic conduit group and 18 patients for the continent caecal reservoir group. There were 43 male patients and 13 female patients. The reported mean age was 60 years for both the ileal conduit and colonic conduit group. The reported mean age for the caecal reservoir group was 50 years. The reported mean follow‐up was 121 months for the ileal conduit group, 117 months for the colonic conduit group and 132 months for the continent caecal reservoir group. Of the original 94 patients, 88 patients underwent radical cystectomy and urinary diversion whereas the remaining 6 patients had simple cystectomy and urinary diversion for neurogenic bladder dysfunction. The inclusion criteria included invasive bladder cancer and neurogenic bladder dysfunction.
Shaaban et al (Shaaban 2006) had 60 patients in their study. A mean follow‐up of 23 months was available for 53 patients. They were generally healthy with no major co‐morbidity and all were undergoing ileal bladder replacement.
Khafagy et al (Khafagy 2006) randomised 60 patients into two groups depending on the type of bowel segment used for bladder replacement. Group one patients had ileal neobladder reconstruction and group two patients had ileocaecal neobladder reconstruction following radical cystectomy. All participants had undergone radical cystectomy for muscle invasive bladder cancer.
One trial (Chen 2009) included 71 male patients randomised to ileocolonic segment (Le Bag) or ileal segment (Studer technique). Urodynamic parameters and continence rates were measured at 6 months.
Risk of bias in included studies
Allocation
All the included trials (Chen 2009; Khafagy 2006; Kristjansson 1995; Shaaban 2006; Studer 1996) were stated to be randomised trials. However there were no further details provided about the methods of randomisation or concealment.
Blinding
There were no reports of how the authors in the trials attempted to limit treatment and outcome assessment bias by ensuring that both patients and assessors were blinded to the initial selection, treatment and subsequent assessment of trial results.
Incomplete outcome data
In two trials (Khafagy 2006; Studer 1996), there were no reported drop‐outs or losses to follow‐up. However, Studer et al (Studer 1996) reported 22 patient deaths were reported due to progressive bladder cancer, with no reports of the number of deaths in each study arm. Kristjansson et al (Kristjansson 1995), originally had 94 patients but only reported on 56 patients. The authors failed to state the reasons as to why 38 patients were not evaluable. It was unknown whether these 38 patients had dropped‐out from the trial, were lost to follow‐up or had died. There were no reasons reported for the loss of follow‐up in one trial (Shaaban 2006). There was a differential dropout in the Chen trial (Chen 2009), 90 patients were randomised, 85 accepted their assigned randomisation. In the ileocolonic group 42 patients underwent the operation 33 had complete follow‐up at 6 months. In ileal neobladder 43 underwent operation 38 had complete follow‐up.
Effects of interventions
Data obtained from the included trials (Chen 2009; Studer 1996; Shaaban 2006; Khafagy 2006; Kristjansson 1995) related to five of the comparisons: continent diversion vs conduit diversion, one segment vs another for conduit diversion, one segment vs another for bladder replacement; anti‐reflux uretero‐intestinal anastomotic technique vs freely refluxing for bladder replacement and anti‐reflux uretero‐intestinal anastomotic technique vs freely refluxing for conduit diversion. It was not possible to address the remaining 9 comparisons as listed above (Objectives). One comparison (hypothesis 12) was addressed by two trials (Shaaban 2006; Studer 1996), but the data could not be combined because the reported analysis did not take into account the paired nature of the data (renal units within the patients). When the random allocation was to different sides (renal units) as reported by Shabaan et al (Shaaban 2006), the issue is similar to cross‐over trails, where people are randomised but the analysis is paired on renal units. The issue is like cluster trial of two units per cluster. The other four hypotheses were addressed by only single trial.
Hypothesis 1: Whether continent diversion is better than conduit diversion [see comparison 1].
Only one trial (Kristjansson 1995) provided data for evaluation of this comparison. In this trial, two types of conduit diversions [ileal (n = 18) and colonic (n = 20)] and caecal continent diversion (n = 8) were used for the treatment of patients. For the statistical analysis, the combined outcome measures of the ileal and colonic conduit diversions (n = 38) were compared to the outcome measures of the caecal continent diversion. There were no statistically significant differences in the relative risks of upper urinary tract infection, number with uretero‐intestinal stenosis, incidence of glomerular filtration rate deterioration (of more than 25%) and renal scarring. The confidence intervals were all wide, however, and did not rule out clinically important differences.
Hypothesis 9: Whether use of an intestinal segment from one part of the gut for bladder replacement is better than a segment from another part [see comparison 9].
Two trials (Chen 2009; Khafagy 2006) reported on the comparison between two different bowel segments (ileal and ileocolonic Chen 2009 and ileal and ileocaecal Khafagy 2006) in the treatment of patients with bladder replacement. The meta analysis did not show any difference in daytime incontinence but with wide confidence intervals. The meta‐analysis showed heterogeneity for the nocturnal incontinence outcome, hence we used a random effects model. The combined result of the two trials did not show a statistically significant result for nocturnal incontinence (RR 0.62: 95% CI 0.13 to 2.87, Analysis 9.2). However, the Chen trial (Chen 2009) alone did favour the ileal neobladder over the ileocolonic segment using the "Le Bag" technique which used a freely refluxing technique (RR 0.35, 95% CI 0.15 to 0.79. The Khafagy trial (Khafagy 2006) used a non‐refluxing technique with the ileocaecal segment. Chen (Chen 2009) measured continence at 6 months postoperatively and classified continence as unsatisfactory if the patient used more than one pad in the day or night. In the ileocolonic group, one patient developed a fistula from the ileocolonic anastomosis to the skin and one developed urethral stenosis due to infection. In the ileal neobladder group, one patient developed stenosis of the ileoposterior urethral anastomosis and one developed stenosis of the ileoureteral anastomosis. Analysis of complication data could not be carried out in case of double counting participants.
9.2. Analysis.
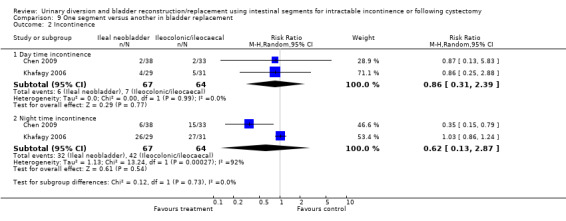
Comparison 9 One segment versus another in bladder replacement, Outcome 2 Incontinence.
In the Khafagy trial (Khafagy 2006) patients who had ileal neobladder (n = 29) were compared with patients who had ileocaecal neobladder (n = 31). Three in each group developed urinary incontinence, three and one wound infection were reported respectively in the two groups. Data for dilatation of the upper urinary tract was reported for 'renal units', but not in a form that allowed appropriate patient‐based analyses (eight units were affected in those allocated to ileal neobladder compared with four in the ileo‐caecal neobladder). The trial reported a similar continence rate between the two procedures. However, there was a higher rate of acidosis, infections and high residual urine in the ileal neobladder group.
Hypothesis 11: Whether use of an intestinal segment from one part of the gut (ileum) for conduit diversion is better than a segment from another part (colon) [see comparison 11].
One trial (Kristjansson 1995) allowed comparison of outcome measures between two different gut segments (ileal and colon) in the treatment of patients with conduit diversion. Patients who had ileal conduit formation (n = 18) were compared with patients who had colonic conduit formation (n = 20). Data were available for only two outcome measures. There were no statistically significant differences in the relative risks of upper urinary tract infection and uretero‐intestinal stenosis. Again, confidence intervals were wide and compatible with large clinical differences.
Hypothesis 12: Whether the use of an anti‐reflux uretero‐intestinal anastomotic technique is better than a freely refluxing anastomosis in bladder replacement [see comparison 12].
The trial by Studer et al (Studer 1996) compared an anti‐reflux mechanism (nipple valve) against a freely refluxing mechanism (afferent ileal tubular segment) in bladder replacement. Data were available for five outcome measures. There were no statistically significant differences in respect of four of these: upper urinary tract infection, daytime incontinence, nighttime incontinence, and uretero‐intestinal anastomotic strictures. Confidence intervals were all wide and clinically important differences were not ruled out. There was a marginally statistically significant difference in the incidence of upper tract dilatation, suggesting a higher rate after nipple value treatment, but this was based on only 11 cases and the confidence interval was wide (RR 0.22; 95% CI 0.05 to 0.96, Analysis 12.4).
12.4. Analysis.
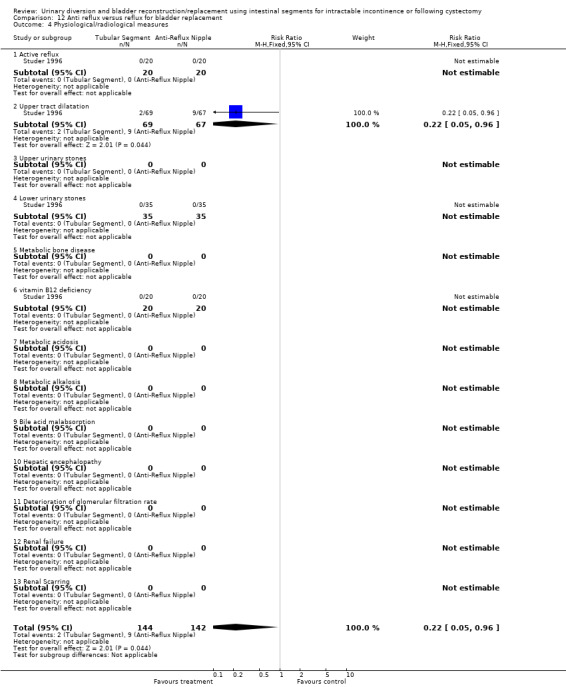
Comparison 12 Anti reflux versus reflux for bladder replacement, Outcome 4 Physiological/radiological measures.
The trial by Shaaban et al (Shaaban 2006) compared refluxing and antirefluxing techniques of uretero‐enteric anastomosis in different renal units for the same patient. Unfortunately they reported neither paired analysis nor data in a form to allow paired analysis. Of the 53 renal units allocated to direct uretero‐ileal anastomosis technique, one was reported to be obstructed compared to be five amongst those with an anti‐refluxive anastomosis. The equivalent figure for reflux were 44 out of 53 versus 6 out of 63; however all five of the obstructed anastomoses had reflux after the obstruction had been corrected, bringing the total of the antireflux group to 11 out of 53. Data on glomerular filtration rates were only reported graphically, but the figure and commentary indicated no statistically significant difference between the two groups of the renal units.
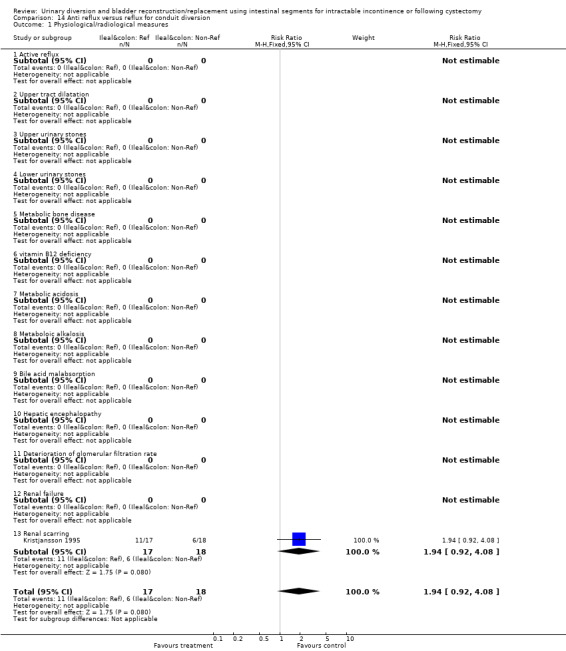
Hypothesis 14: Whether the use of an anti‐reflux uretero‐intestinal anastomotic technique is better than a freely refluxing anastomosis in conduit diversion [see comparison 14].
The trial by Kristjansson et al (Kristjansson 1995b) also compared an anti‐reflux technique and a freely refluxing anastomosis used in the formation of ileal and colonic conduit diversion. Data were only available for one outcome, the incidence of renal scarring. The authors reported renal units affected rather than the number of patients affected. No statistically significant difference was found between the two techniques and the confidence intervals were wide (risk ratio 1.94; 95% CI 0.92 to 4.08); this analysis does not take into account 'clustering' due to the paired renal units.
Discussion
There were few randomised trials that addressed the objectives of the review. From a total of 25 studies that were identified, only five trials were suitable for data analysis. Data from two trials on the outcome of upper tracts (Shaaban 2006; Khafagy 2006) was reported as 'renal units', not in a form to perform paired analysis. No data from eligible trials were available to address 9 of the 14 pre‐stated comparisons and the data from the five eligible trials that were considered were very limited. The outcome measures that were reported did not include a large proportion of the outcome measures that the reviewers felt were important to the review. It was therefore not possible to comment on a significant number of outcome measures. In particular, there was lack of data on outcome measures that looked at patient symptoms and patient quality of life in general. There was lack of data on clinical end points such as the immediate, medium‐term and long‐term problems encountered by patients post‐urinary diversion. Trials did not report on the incidence of cancer development post‐urinary diversion. There was no data regarding health economic measures such as the cost of alternative management, the costs of effects of management and formal cost‐effectiveness analyses. Some data on physiological / radiological measures were found, such as the incidences of active reflux, upper tract dilatation, lower urinary tract stones, vitamin B12 deficiency, deterioration of glomerular filtration rate (more than 25% in the trial reported) and renal scarring. However data on the incidences of physiological / radiological measures such as upper urinary tract stones, metabolic bone disease, metabolic acidosis / alkalosis, bile acid malabsorption and hepatic encephalopathy were not found. The incidence of renal failure was not specifically reported. One trial (Kristjansson 1995) reported on the incidence of glomerular filtration rate deterioration of more than 25%. This is probably important as it suggests significant and progressive impairment that is likely to lead to dialysis in the future. However, it would have been useful to know how many of these patients with deterioration in renal function actually proceeded to dialysis or re‐operation.
Where data were available their usefulness was severely limited by the small sizes of the trials and hence the few participants who experienced any of the outcomes. The confidence intervals around all the estimates were wide and important differences could not be ruled out (or in) with any assurance. One trial (Khafagy 2006) reported a higher rate of post‐void residual urine and biochemical acidosis in patients with bladder replacement using ileal segment of the intestine as compared to the ileocaecal segment. The arterial pH was measured every three monthly in both the groups and was reported significantly higher in the ileal neobladder (mean 7.39 versus 7.41). The clinical significance and long‐term outcome of this biochemical results were not stated. There was no differences in the follow‐up serum creatinine between the two groups. The results from this trial need to be interpreted with caution due to small number of participants and short follow‐up of 2 years.
The data on nocturnal incontinence for two studies (Chen 2009; Khafagy 2006) was conflicting. The small Chen study (Chen 2009) showed a statistically significant result favouring the ileal neobladder over an ileocolonic bladder whereas the data from the similar sized Khafagy trial (Khafagy 2006) showed no statistically significant difference between the ileal neobladder and ileocaecal bladder. Analysis of urodynamic variables suggested that the pressure rise during artificial bladder filling (compliance) was slightly higher on average in those patients with ileocolonic neobladder which may contribute to increased risk of nocturnal incontinence. All other urodynamic variables including capacity and urethral closure pressure were similar between the two types of bladder replacement. The cause and longer term consequences of the increased rate of nocturnal incontinence in patients with ileocolonic neobladder therefore remain uncertain and require exploration in further larger studies with longer follow up.
One marginally statistically significant result was found (Studer 1996). This should be interpreted cautiously for the reasons outlined above and also because the authors used renal units (Khafagy 2006; Kristjansson 1995; Shaaban 2006; Studer 1996) and not actual patient numbers when reporting on the outcome measures of upper tract dilatation and renal scarring respectively. Because the kidneys in an individual participant cannot be considered independent (if one side is affected, it is more likely that the other side will be affected too), the level of statistical significance is likely to be spuriously high. Studer et al (Studer 1996) reported that patients treated with formation of afferent tubular ileal segment for bladder replacement had significantly less upper tract dilatation when compared to those treated with anti‐reflux nipples. The afferent ileal tubular segment is said to be a dynamic anti‐reflux device under low‐pressure conditions. An afferent limb has an inherently higher pressure, per square centimetre, when compared to a larger volume bladder replacement and it is by this intrinsic property that afferent limbs are thought to work, preventing reflux into the ureters that are anastomosed proximally to the afferent limb. It is thought that the longer the afferent limb, the greater the resistance to reverse flow. It was noted that the authors in this trial used the terms of upper tract dilatation and obstruction interchangeably when describing their results. It cannot be assumed that all patients with upper tract dilatation will have clinically significant obstruction, or vice versa. It would have been more meaningful for the authors to have perhaps measured the renal function of these patients with upper tract dilatation and to have reported on the incidence of such patients progressing on to re‐operation or dialysis. Again, it is unclear as to how clinically significant the results may be, as a patient with unilateral upper tract dilatation or renal scarring may conceivably have normal renal function. This underlines the need for caution when interpreting these results.
It is important to note that broader evidence on the topics of this review come from non‐comparative or non‐randomised studies. These were not considered in this review because of the likelihood of bias distorting their interpretation. However, in a separate systematic review (Nabi 2005) of non‐randomised studies, the authors concluded that the level and quality of evidence was poor and added little to the randomised trials. There is clearly a need for more randomised trials. The commonest condition resulting in the need for cystectomy and transposing intestinal segments into the urinary tract in the Western world is advanced bladder cancer. There were 10,335 new cases of bladder cancer diagnosed in the UK in 2008 (Office for National Statistics 2002) The condition and procedures are common enough for a prospective randomised trial to be possible in addition to having considerable cost implications to the National Health Service every year. Where randomisation of a patient population is not possible or inappropriate, then an alternative robust method of determining outcome of 'competing' surgical procedures should be used, for example, a partially randomised patient preference study or a comprehensive cohort design.
Authors' conclusions
Implications for practice.
One small study found higher rates of nocturnal incontinence amongst patients having an ileocolonic bladder replacement compared with an ileal bladder replacement. This study was small and reported few methodological details, longer term outcome was not assessed. This review did not find any evidence that either bladder replacement or continent diversion was better than conduit diversion, or vice versa. There is clearly an absence of good quality data in the literature despite the fact that such surgery is commonplace and has been so for many decades. In conduit diversion, the review did not find any evidence that using a segment of ileum was any more advantageous than using a segment of colon, or vice versa in either bladder replacement or continent diversion. Similarly, no difference was found in using either freely refluxing or anti‐refluxing techniques for conduit diversion from the available evidence. The data reviewed would appear to suggest that afferent ileal tubular segment is less likely to cause upper tract dilatation compared to the anti‐reflux nipples, but even this finding should be interpreted cautiously. Until better evidence becomes available (see below), practice will continue to be dictated by local patient, surgeon and cost factors, together with poorly evaluated advances in surgical technology.
Implications for research.
There is a need for more randomised trials comparing different surgical techniques. Investigators need to look at more comprehensive outcome measures particularly emphasising relevant clinical end points as detailed in this review, quality of life issues and health economic measures. Because relatively small number of patients are treated in individual centres, this will require multi centre collaboration. Where randomisation is difficult or inappropriate other approaches, such as partially randomised patient preference designs or comprehensive cohort studies, should be used. Given the wide scope of treatment options and the paucity of high level evidence it would be important to gain consensus amongst patients, clinicians and health care managers concerning the key research questions and their relative priority.
What's new
| Date | Event | Description |
|---|---|---|
| 22 November 2011 | New search has been performed | one study added, one ongoing trial |
| 22 November 2011 | New citation required but conclusions have not changed | one study added, one ongoing trial |
History
Protocol first published: Issue 4, 2001 Review first published: Issue 1, 2003
| Date | Event | Description |
|---|---|---|
| 13 October 2008 | Amended | Converted to new review format. |
| 19 May 2005 | New search has been performed | For this update of the review N Ghulam and S McClinton assessed the list of 33 potentially relevant trials and added one extra trial to the list of excluded studies. |
| 19 November 2002 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The reviewers are grateful to staff at the editorial base of the Cochrane Incontinence Review Group for the help they provided. The review authors would also like to thank the external reviewers for the very helpful comments they provided on the protocol and on the completed review.
Appendices
Appendix 1. Search methods and terms used for the extra specific searches for this review
For the previous version of this review extra specific searches were performed. These are detailed below, including the search terms used.
MEDLINE (on Ovid) (years searched: 1966 to Week 3 January 2005) and MEDLINE In Process (on Ovid) (search covered: 31 January 2005) were both searched on 2 February 2005
CENTRAL was searched on 17 May 2001 (in The Cochrane Library, Issue 2, 2001 on CD‐ROM)
Dissertation Abstracts (on UMI ProQuest Digital Dissertations) was searched on 18 June 2001
MEDLINE (on Ovid) (years searched: 1966 to Week 3 January 2005), MEDLINE In Process (on Ovid)(search covered: 31 January 2005) were both searched on 2 February 2005 using the following search terms combined together using the Boolean operator 'OR' and then combined using the Boolean operator 'AND' with the first two parts of the Cochrane 'Highly Sensitive Search Strategy' (Dickersin 2002):
urinary diversion/ Cystectomy/ Urinary Reservoirs, Continent/ cystectom$.tw. (conduit$ adj5 (ile$ or urin$ or contine$ or colon$)).tw. (reservoir$ adj5 (ile$ or urin$ or continen$ or colon$)).tw. (urin$ adj2 diversion$).tw. (continen$ adj2 diversion$).tw. (bladder$ adj2 substitut$).tw. neobladder$.tw. cystoplast$.tw. enterocystoplast$.tw. (bladder$ adj2 (reconstruct$ or artificial or replac$ or rectal)).tw. (continen$ adj2 outlet$).tw. (conduit$ adj2 diversion$).tw.
CENTRAL was searched on 17 May 2001 (in The Cochrane Library, Issue 2, 2001 on CD‐ROM) using the following search terms, combined together using the Boolean operator 'OR':
URINARY‐DIVERSION:ME CYSTECTOMY*:ME URINARY‐RESERVOIRS‐CONTINENT*:ME CYSTECTOM* (CONDUIT* near ILE*) (CONDUIT* near URIN*) (CONDUIT* near CONTINEN*) (CONDUIT* near COLON*) (RESERVOIR* near ILE*) (RESERVOIR* near URIN*) (RESERVOIR* near CONTINEN*) (RESERVOIR* near COLON*) (URIN* near DIVERSION*) (CONTINEN* near DIVERSION*) (BLADDER* near SUBSTITUT*) NEOBLADDER* CYSTOPLAST* ENTEROCYSTOPLAST* (BLADDER* near RECONSTRUCT*) (ARTIFICIAL near BLADDER*) (REPLAC* near BLADDER*) (RECTAL next BLADDER*) (CONTINEN* near OUTLET*) (CONDUIT* near DIVERSION*)
Dissertation Abstracts (on UMI ProQuest Digital Dissertations) was searched on 18 June 2001 using the search term: urinary diversion*.
The reference lists of relevant articles were searched for other possible relevant trials.
We did not impose any language or other restrictions on any of these searches.
Data and analyses
Comparison 1. Continent diversion versus conduit.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Quality of life | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number of patients with lower urinary tract infection | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 not requiring hospitalisation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 requiring hospitalisation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 more than 3 infection per year | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number of patients with upper urinary tract infection | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.66 [0.38, 7.20] |
| 3.1 not requiring hospitalisation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 requiring hospitalisation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 more than 3 infection per year | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.4 Number of patients with pyelonephritis (No hospitalisation mentioned) | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.66 [0.38, 7.20] |
| 4 Number requiring CISC | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number with excess mucus production | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 catheter blockage | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 urostomy pouch blockage | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 Number of patients complaining | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number of patients with bowel dysfunction | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 diarrhoea | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 faecal urgency | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 faecal incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.4 flatus leakage | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.5 constipation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number with urinary incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Daytime incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Nightime incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Number complaining of odour | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Number with uretero‐intestinal stenosis | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.24, 1.80] |
| 10 Number with stoma stenosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Number with parastomal hernia | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Number needing re‐operation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Number with operative complications | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Number with post operative morbidity | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Number of post operative mortality | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Length of operation | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Length of hospital stay | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Number with bladder anastomotic leak | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Number with bowel anastomotic leak | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Cost of alternative management | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Cost consequence of effects of management | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Formal cost effectiveness analyses | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Physiological/radiological measures | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 23.1 Active reflux | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.2 upper tract dilatation | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.3 Upper urinary stones | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.4 Lower urinary stones | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.5 Metabolic bone disease | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.6 vitamin B12 deficiency | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.7 Metaboloic acidosis | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.8 Metaboloic alkalosis | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.9 Bile acid malabsorption | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.10 Hepatic encephalopathy | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.11 Deterioration of glomerular filtration rate | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.12 Renal failure | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 23.13 Renal scarring | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 Number with urodynamic measures | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 24.1 bladder capacity | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 25 Number developing cancer | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.3. Analysis.
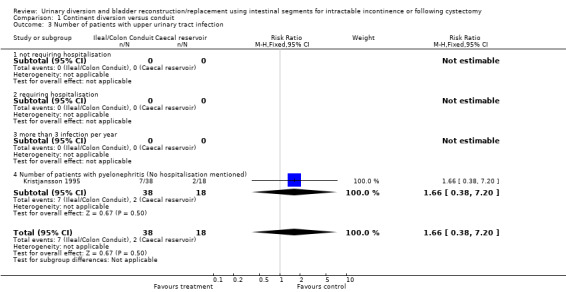
Comparison 1 Continent diversion versus conduit, Outcome 3 Number of patients with upper urinary tract infection.
1.9. Analysis.
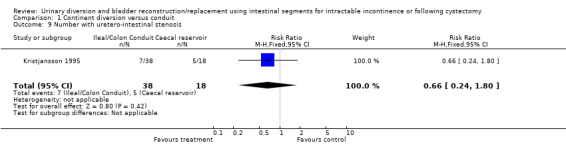
Comparison 1 Continent diversion versus conduit, Outcome 9 Number with uretero‐intestinal stenosis.
1.23. Analysis.
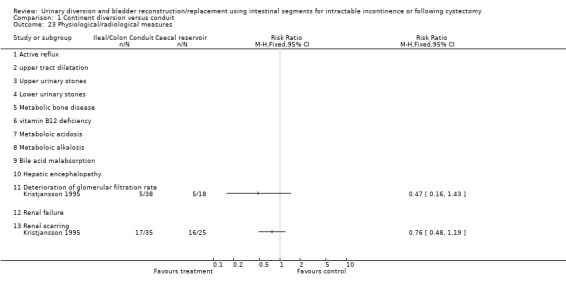
Comparison 1 Continent diversion versus conduit, Outcome 23 Physiological/radiological measures.
Comparison 9. One segment versus another in bladder replacement.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Urinary leakage | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.16, 7.10] |
| 2 Incontinence | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Day time incontinence | 2 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.31, 2.39] |
| 2.2 Night time incontinence | 2 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.13, 2.87] |
| 3 Wound infection | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.21 [0.35, 29.11] |
9.1. Analysis.
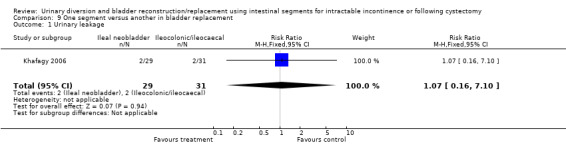
Comparison 9 One segment versus another in bladder replacement, Outcome 1 Urinary leakage.
9.3. Analysis.
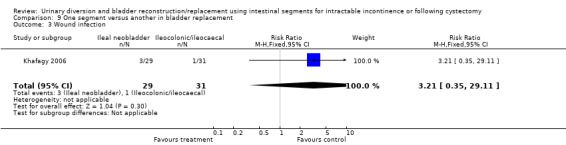
Comparison 9 One segment versus another in bladder replacement, Outcome 3 Wound infection.
Comparison 11. One segment versus another for conduit diversion.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of patients with upper urinary tract infection | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.38, 5.74] |
| 1.1 not requiring hospitalisation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 requiring hospitalisation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 more than 3 infection per year | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 Number of patients with pyelonephritis (No hospitalisation mentioned) | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.38, 5.74] |
| 2 Number with uretero‐intestinal stenosis | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.22, 3.23] |
11.1. Analysis.
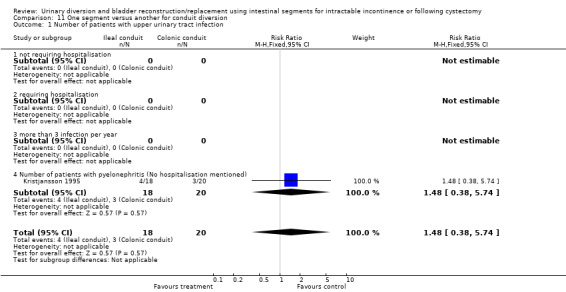
Comparison 11 One segment versus another for conduit diversion, Outcome 1 Number of patients with upper urinary tract infection.
11.2. Analysis.

Comparison 11 One segment versus another for conduit diversion, Outcome 2 Number with uretero‐intestinal stenosis.
Comparison 12. Anti reflux versus reflux for bladder replacement.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of patients with upper urinary tract infection | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.10, 1.13] |
| 1.1 not requiring hospitalisation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 requiring hospitalisation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 more than 3 infection per year | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 Number of patients with pyelonephritis (No hospitalisation mentioned) | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.10, 1.13] |
| 2 Number with urinary incontinence | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.47, 2.14] |
| 2.1 Daytime incontinence | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.27, 3.69] |
| 2.2 Nightime incontinence | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.39, 2.55] |
| 3 Number with uretero‐intestinal stenosis | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 21.06] |
| 4 Physiological/radiological measures | 1 | 286 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 0.96] |
| 4.1 Active reflux | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Upper tract dilatation | 1 | 136 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 0.96] |
| 4.3 Upper urinary stones | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.4 Lower urinary stones | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.5 Metabolic bone disease | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.6 vitamin B12 deficiency | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.7 Metabolic acidosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.8 Metabolic alkalosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.9 Bile acid malabsorption | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.10 Hepatic encephalopathy | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.11 Deterioration of glomerular filtration rate | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.12 Renal failure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.13 Renal Scarring | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
12.1. Analysis.
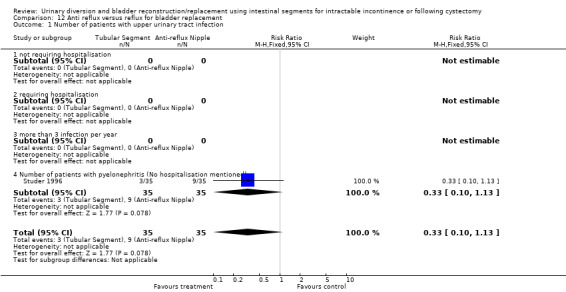
Comparison 12 Anti reflux versus reflux for bladder replacement, Outcome 1 Number of patients with upper urinary tract infection.
12.2. Analysis.
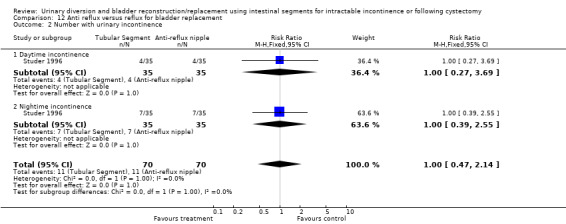
Comparison 12 Anti reflux versus reflux for bladder replacement, Outcome 2 Number with urinary incontinence.
12.3. Analysis.
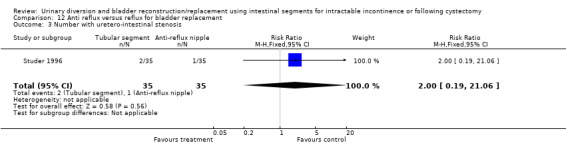
Comparison 12 Anti reflux versus reflux for bladder replacement, Outcome 3 Number with uretero‐intestinal stenosis.
Comparison 14. Anti reflux versus reflux for conduit diversion.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Physiological/radiological measures | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.94 [0.92, 4.08] |
| 1.1 Active reflux | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Upper tract dilatation | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 Upper urinary stones | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 Lower urinary stones | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.5 Metabolic bone disease | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.6 vitamin B12 deficiency | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.7 Metabolic acidosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.8 Metaboloic alkalosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.9 Bile acid malabsorption | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.10 Hepatic encephalopathy | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.11 Deterioration of glomerular filtration rate | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.12 Renal failure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.13 Renal scarring | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.94 [0.92, 4.08] |
14.1. Analysis.
Comparison 14 Anti reflux versus reflux for conduit diversion, Outcome 1 Physiological/radiological measures.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chen 2009.
| Methods | Randomised controlled trial single centre |
|
| Participants | Inclusion: bladder cancer (stage T1G3, T2‐3NO‐NxMo), male sex, no history of urethral trauma or urethral stricture, normal renal function, desire to obtain an orthotopic neobladder Exclusion: more than 80 years old, enteritis 101 men enrolled, 11 patients excluded as did not meet inclusion criteria 90 patients randomised, 85 accepted their assigned randomisation. Ileal neocolonic group 42 patients underwent the operation 33 had complete follow‐up at 6 months. In ileal neobladder 43 underwent operation 38 had complete follow‐up. Remaining patients were not included in the investigation |
|
| Interventions | orthotopic ileocolonic versus ileal neobladder | |
| Outcomes | Continence evaluations assessed at 6 months post operatively, classified as unsatisfactory if patient used more than one pad in the day or night. Serum creatinine, urea nitrogen, serum electrolyte, midstream urine culture, and ultasonography or intravenous urography every 3 months for the first year. Urodynamic studies performed at 6 months postoperatively. Primary end point was continence and urodynamic parameters. Secondary endpoint rate of complications, renal function, serum electrolyte levels and urine culture 6 months postoperatively | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not stated |
| Allocation concealment (selection bias) | Unclear risk | not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | All 90 patients randomised, 85 accepted their assigned randomisation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Micturation/continence questionnaire was administered by a urologist who was independent of all the surgical work |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | In ileocolonic group 42 patients underwent the operation and 33 had complete follow up at 6 months. In the ileal group 43 underwent the operation and 38 had complete follow up at 6 months. The remaining patients were not included in the analyses because they were lost to, or refused, follow up |
Khafagy 2006.
| Methods | Randomised prospective study comparing various outcomes between Ileal and ileocaecal bladder replacement surgery Single centre study Ileal neobladder (studer type reconstruction) All patients had perineal exercises following surgery 3 monthly follow‐up | |
| Participants | Inclusion: All patients with muscle invasive disease undergoing radical cystectomy Excl: Patients with memebranous urethral involvement. | |
| Interventions | Group 1: Ileal neobladder (29) Group 2: Ileocaecal neobladder (31) | |
| Outcomes | Urinary leakage Wound infection Deep vein thrombosis Jaundice Anuria Urinary incontinence Serum biochemistry Upper tract dilatation Cancer outcomes | |
| Notes | No mention of methods of randomisation Urodynamics studies done on follow‐up only in 13 patients (5 in group 1 and 8 in group 2) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | were randomised into two groups |
| Allocation concealment (selection bias) | Unclear risk | not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 29 patients Group A, 31 patients Group B four patients died after surgery, two in each group |
Kristjansson 1995.
| Methods | Randomised prospective study, initially by Mansson, 1989 with 2 subsequent papers published with longer follow‐up: Kristjansson, 1995a (primary reference) and 1995b. Mansson 1989 Mean follow‐up: Ileal conduit 67 months, colonic conduit 66 months and caecal reservoir 62 months Drop‐outs: none Kristjansson 1995a (primary reference) Mean follow‐up: Ileal conduit 121 months, colonic conduit 117 months and caecal reservoir 132 months Drop‐outs: Only 56 patients of previous total 94 patients presented, no reason given. 38 drop‐outs Kristjansson 1995b Mean follow‐up: 150 months Drop‐outs: 5 patients for renal scarring study, 4 patients in bacteriuria study (patients declined to participate) |
|
| Participants | Incl: invasive bladder carcinoma, radical cystectomy and neurogenic bladder dysfunction Mansson 1989 n = 94 Sex: 71 male, 23 female Mean age: Ileal conduit 60 years, colonic conduit 60 years and caecal reservoir 51 years Kristjansson 1995a (primary reference) n = 56 Sex: 43 male, 13 female Mean age: Ileal conduit 60 years, colonic conduit 60 years, caecal reservoir 50 years Kristjansson 1995b n (renal scarring) = 32 n (bacteriuria) = 5 n (GFR in renal units with scarring) = 60 Sex: (no mention) Mean age: (no mention) |
|
| Interventions | I: Ileal conduit diversion ‐ refluxing II: Ileal conduit diversion ‐ non ‐ refluxing III: Colonic conduit diversion ‐ refluxing IV: Colonic conduit diversion ‐ non ‐ refluxing V: Caecal continent diversion ‐ non ‐ refluxing | |
| Outcomes | Mansson 1989
I: Renal function ‐ glomerular filtration rate
II: Ureterointestinal anastomotic strictures
III: Urinary tract infections Kristjansson 1995a (primary reference) I: Renal function: glomerular filtration rate II: Ureterointestinal anastomotic strictures III: Urinary tract infections Kristjansson 1995b I: Renal scarring: Presence and grade (1‐3) II: Bacteriuria: Presence and location III: GFR in renal units with scarring |
|
| Notes | Further follow‐up presented by Kristjansson in 1995 Kristjansson 1995a was used as the primary study as this had a longer follow‐up compared to Mansson 1989 The outcomes in Kristjansson 1995b of the presence and location of bacteriuria were not included as the numbers who participated were very small: 3 with ileal conduit and 2 with colonic conduit. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not stated |
| Allocation concealment (selection bias) | Unclear risk | not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In 10 patients the initial allocation to colonic conduit was changed to ileal because of colonic anomalies. To minimize imbalance between the two conduit groups, each case following an unplanned ileal diversion received a colonic conduit |
Shaaban 2006.
| Methods | Prospective randomised controlled trial comparing reflux vs. anti‐reflux techniques of uretero‐enteric anastomisis during ileal bladder replacement in the same patient. 60 patients ( 53 male and 7 females) | |
| Participants | Incl: Generally healthy patients with no co‐morbid conditions were included Normal upper tract Similar GFR in both the renal units. Organ confined disease Excl: Positive urethral margins for malignancy | |
| Interventions | Refluxing group (Group 1)‐ 60 renal units Anti‐refluxing group (Group 2)‐ 60 renal units | |
| Outcomes | Peri‐operative complications such as urinary leakage Upper tract dilatation (Including strictures) Reflux Glomerular filtration rate Pyelonephreritis Surgical interventions | |
| Notes | Data of outcomes such as GFR presented in a graph with no tabulation, hence difficult to analyse. No mention of method of randomisation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not stated |
| Allocation concealment (selection bias) | Unclear risk | not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | everyone accounted for |
Studer 1996.
| Methods | Randomised prospective study, with 1 subsequent paper published with longer follow‐up data: Studer 1996 (primary reference) Studer 1991 Median follow‐up: Anti‐reflux nipple 36 months, afferent tubular segment 30 months Drop‐outs: Total 60 patients operated on, but data on 40 presented as follow‐up was more than a year in this subgroup. Total 20 drop‐outs. Studer 1996 (primary reference) Median follow‐up: Anti‐reflux nipples 57 months, afferent tubular segment 45 months Drop‐outs: None |
|
| Participants | Incl: radical cystectomy, bladder substitution with ileal segment and male patients only Excl: Patient follow‐up less than a year, female patients Studer 1991 n (anti‐reflux nipple) = 20 n (afferent tubular segment) = 20 Sex: All males Mean age: 63.7 years Studer 1996 (primary reference) n (anti‐reflux nipple) = 35 n (afferent tubular segment) = 35 Sex: All males Median age: anti‐reflux nipple 66.6 years and afferent tubular segment 63.8 years |
|
| Interventions | I: Anti‐reflux nipple II: Afferent ileal tubular segment | |
| Outcomes | Studer 1991
I: Reflux vs No reflux
II: Urinary continence (day and night)
III: Bacteriuria presence
IV: Serum acidosis
V: Serum B12
VI: Kidney size Studer 1996 (primary reference) I: Urinary continence (day and night) II: Bacteriuria presence III: Pyelonephritis IV: Uretero‐intestinal strictures requiring re‐operation V: Upper tract dilatation VI: Functional reserve VII: Renal function VIII: Voiding habits IX: Urinary stones |
|
| Notes | No mention of disease type in the inclusion criteria of the study. Studer 1996 was used as the primary study as this had the longest follow‐up. Studer 1991 Unclear causes of deaths. 18 deaths from "progressive" disease and 3 deaths from "other" causes. In 3 patients with metabolic acidosis requiring correction, no mention was made of which treatment group these patients originated from. Studer 1996 (primary reference) Note 22 deaths from progressive bladder cancer. Conflicting numbers of pyelonephritis in patients compared to Studer 1991. For the purposes of analysis, the numbers from the later report; Studer 1996 were included in the tables. It was not possible to extract data from Fig. 2 of Studer 1996 paper for the purposes of analysing the incidence of bacteriuria / positive culture. In upper tract dilatation, the numbers used in the final analysis were from Studer 1996. It should be noted that renal units were used rather than patient numbers. It was not possible to analyse the outcomes of metabolic acidosis, functional reserve, renal function and voiding habits in both reports as no actual figures were presented. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not stated |
| Allocation concealment (selection bias) | Unclear risk | not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Total 60 patients operated on, but data on 40 presented as follow‐up more than a year in this subgroup. Total 20 drop‐outs. |
Incl. = inclusion criteria Excl. = exclusion criteria GFR = Glomerular filtration rate (mls/min)
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bassi 1996 | This was a non‐randomised study comparing patients with ileal conduits and ileal continent diversions. |
| Boyd 1987 | This was a non‐randomised study looking at quality of life issues in patients with either ileal conduits or ileal continent diversions. |
| Brough 1998 | This was a study looking at the incidence of stone formation in paediatric patients who underwent either enterocystoplasty with continent diversion or augmentation cystoplasty alone. The study was excluded because the patients were in a prospective cohort without randomisation. |
| Davidsson 1996 | This was a randomised prospective trial that looked at outcomes in patients who underwent two different types of outlet surgery for neo‐bladder. Comparisons of outlet surgery outcomes was not a subject of the review. |
| De Carli 1997 | This was a non‐randomised study that compared two different types of uretero‐ileal anastomoses. |
| Degen 1997 | This was a prospective non‐randomised study of ileocaecal transposition in rectal carcinoma which was not relevant for the purposes of this review. |
| El 2002 | The study has only reported as an abstract. We are waiting to see full publication of the results |
| Ghoneim 1981 | Randomised trial compared refluxing versus non‐refluxing techniques in a continent diversion (ureterosigmoidostomy) Results were not reported separately for both groups. Written to authors. |
| Ghoneim 1988 | This was a randomised prospective clinical trial that assessed survival in patients with bladder cancer who had pre‐operative radiotherapy vs no pre‐operative radiotherapy, which was not the objective of the review. |
| Kolettis 1996 | This was a study on a prospective cohort of patients who underwent a particular type of bladder replacement. |
| Lampel 1995 | This was a randomised prospective trial that looked at outcomes in patients who underwent two different types of outlet surgery for neo‐bladder. Comparisons of outlet surgery outcomes was not a subject of the review. |
| Lightfoot 2007 | A randomised controlled trial. This study reported impact of post‐operative intravenous low dose erythromycin on the postoperative ileus. This was no the subject of review. |
| Mansson 1997 | This study looked at the effect of psychosocial intervention on the outcome of 3 different types of urinary diversion. It was excluded because the groups receiving the different types of surgery was non‐randomised. |
| Mansson 2004 | This study compared the health related Quality of life assessment using questionnaires between neutral third party and treating institution personnel. This was not the primary subject of this review. |
| Mattei 2008 | Randomised to stenting |
| Morey 2006 | A randomised controlled trial. This study reports the outcomes of various methods of bowel preparation prior to cystectomy, which was not the subject of the review |
| Okada 1989 | This study was non‐randomised and followed‐up three successive groups of patients who underwent modifications of the nipple valves of their ileal continent diversion. |
| Osman 2004 | This trial was prospectively randomised. However the trial looked at outcomes from 2 different types of anti‐reflux techniques, this was not the subject of this review. |
| Osman 2009 | Comparison of two different anti reflux techniques |
| Shaaban 1992 | This study was prospectively randomised. However the study looked at outcomes from 2 different types of anti‐reflux valves that were not the subject of the review. |
| Shokeir 1995 | not urinary diversion or bladder reconstruction comparing two types of ileal ureter |
| Speakman 1989 | This study was excluded as it was unclear if the treatment arms underwent randomisation prior to selection. |
| Studer 1997 | This was a long‐term report on a prospective cohort of patients who underwent ileal bladder replacement/substitute. |
| Thakar 1998 | This study looked at the effect of hysterectomy on bladder and bowel. Although prospectively randomised, this study was excluded because it was not relevant for the purposes of this review. |
| Vakalopoulos 2011 | No intestinal segment used for uretero‐ureterocutaneostomy |
Characteristics of ongoing studies [ordered by study ID]
Skinner 2009.
| Trial name or title | Skinner 2009 |
| Methods | Randomised controlled trial |
| Participants | Patients with primary bladder cancer. Male and female |
| Interventions | Two types of ileal neo bladder: the studer pouch and the T‐pouch anti refluxing versus freely refluxing |
| Outcomes | Primary end point renal function |
| Starting date | late 2002 |
| Contact information | E.C. Skinner, Dept of Urology, Keck USC School of Medicine, Los Angeles |
| Notes |
Contributions of authors
For this update: N Ghulam and S McClinton assessed the list of 33 potentially relevant trials and added one extra trial to the list of excluded studies.
Original review: J N'Dow and N Dublin wrote the review protocol. S Yong, J N'Dow and J Cody assessed the studies, extracted the data, analysed the data and wrote the review. R Pickard and D Neal provided critical analysis of the review.
Sources of support
Internal sources
University of Aberdeen, UK.
External sources
No sources of support supplied
Declarations of interest
None known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Chen 2009 {published data only}
- Chen Z, Lu G, Li X, Li X, Fang Q, Ji H, et al. Better compliance contributes to better nocturnal continence with orthotopic ileal neobladder than ileocolonic neobladder after radical cystectomy for bladder cancer. Urology 2009;73(4):838‐43; discussion 843‐4. [DOI] [PubMed] [Google Scholar]
Khafagy 2006 {published data only}
- Khafagy M, Shaheed FA, Moneim TA. Ileocaecal vs ileal neobladder after radical cystectomy in patients with bladder cancer: a comparative study. BJU International 2006;97(4):799‐804. [21954] [DOI] [PubMed] [Google Scholar]
Kristjansson 1995 {published data only}
- Kristjansson A, Bajc M, Wallin L, Willner J, Mansson W. Renal function up to 16 years after conduit (refluxing or anti‐reflux anastomosis) or continent urinary diversion. 2. Renal scarring and location of bacteriuria. British Journal of Urology 1995;76:546‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Kristjansson A, Wallin L, Mansson W. Renal Function up to 16 years after conduit (refluxing or anti‐reflux anastomosis) or continent diversion. 1. Glomerular filtration rate and patency of uretero‐intestinal anastomosis. British Journal of Urology 1995;76:539‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Mansson W, Ahlgren G, White T. Glomerular filtration rate up to 10 years after urinary diversion of different types. Scandinavian Journal of Urology and Nephrology 1989;23:195‐200. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Shaaban 2006 {published data only}
- Shaaban AA, Abdel‐Latif M, Mosbah A, Gad H, Eraky I, Ali‐El‐Dein B, et al. A randomized study comparing an antireflux system with a direct ureteric anastomosis in patients with orthotopic ileal neobladders. BJU International 2006;97(5):1057‐62. [21881] [DOI] [PubMed] [Google Scholar]
Studer 1996 {published data only}
- Hugonnet CL, Danuser H, Thalmann GN, Studer UE. [Long‐term urodynamic and clinical follow‐up in 70 patients with ileal bladder replacement combined with an antireflux mechanism or an afferent tubular segment] [French] [Resultats urodynamiques et cliniques a long terme chez 70 patients ayant une vessie ileale de substitution combinee a un mecanisme anti‐reflux ou un segment tubulaire afferent]. Progres en Urologie 1997;7:960‐6. [MEDLINE: ] [PubMed] [Google Scholar]
- Studer U, Danuser H, Thalmann G, Springer J, Turner W. Antireflux nipples or afferent tubular segments in 70 patients with ileal low pressure bladder substitutes: Long term results of a prospective randomized trial. Journal of Urology 1996;156:1913‐7. [MEDLINE: ] [PubMed] [Google Scholar]
- Studer U, Spiegel T, Casanova G, Springer J, Gerber E, Ackermann D, et al. Ileal bladder substitute: Antireflux nipple or afferent tubular segment. European Urology 1991;20:315‐26. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bassi 1996 {published data only}
- Bassi E, Valerio S, Antoniazzi G, Fornasiero GF, Petterle YV. Comparison between results of ileal conduit and continent ileal bladder (VIP), after radical cystectomy. Archivos Espanoles de Urologia 1996;49(9):1003‐6. [MEDLINE: ] [PubMed] [Google Scholar]
Boyd 1987 {published data only}
- Boyd SD, Feinberg SM, Skinner DG, Lieskovsky G, Baron D, Richardson J. Quality of life survey of urinary diversion patients: Comparison of ileal conduits versus continent Kock ileal reservoirs. Journal of Urology 1987;138:1386‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Brough 1998 {published data only}
- Brough RJ, O'Flynn KJ, Fishwick J, Gough DCS. Bladder washout and stone formation in paediatric enterocystoplasty. Pediatric Urology 1998;33:500‐2. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Davidsson 1996 {published data only}
- Davidsson T, Hedlund H, Mansson W. Detubularized right colonic reservoir with intussuscepted ileal nipple valve or stapled ileal ("Lundiana") outlet. World Journal of Urology 1996;14:78‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
De Carli 1997 {published data only}
- Carli P, Micali S, O'Sullivan D, Mainiero G, Cusumano G, Fattahi H, et al. Ureteral Anastomosis in the Orthotopic Ileal Neobladder: Comparison of 2 techniques. The Journal of Urology 1997;157(2):469‐71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Degen 1997 {published data only}
- Degen LP, Flue MO, Collet A, Hamel C, Beglinger C, Harder F. Ileocecal segment transposition does not alter whole gut transit in humans. Annals of Surgery 1997;226(6):746‐52. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
El 2002 {published data only}
- Bahnasawy MS, Shaaban HS, Gomha MA, Nabeeh A. Management of nocturnal incontinence in orthotopic ileal reservoirs using oxybutinin versus verapamil: A prospective randomized cross‐over study (Abstract). Journal of Urology 2002;167(4 Suppl):86. [17608] [Google Scholar]
Ghoneim 1981 {published data only}
- Ghoneim M, Shehab‐El‐Din A, Ashamallah A, Gaballah M. Evolution of rectal bladder as a method for urinary diversion. Journal of Urology 1981;126:737‐40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ghoneim 1988 {published data only}
- Ghoneim MA, Adhmallah AK, Awaad HK, Shebab El‐Din AB, Kock NG, Whitmore Jr WF. Cystectomy and diversion for carcinoma of the bilharzial bladder. Management of advanced cancer of prostate and bladder. New York: Alan R Liss, Inc, 1988:315‐9. [MEDLINE: ] [PubMed] [Google Scholar]
Kolettis 1996 {published data only}
- Kolettis PN, Klein EA, Novick AC, Winters JC, Appell RA. The Le Bag orthotopic urinary diversion. Journal of Urology 1996;156(3):926‐30. [MEDLINE: ] [PubMed] [Google Scholar]
Lampel 1995 {published data only}
- Lampel A, Hohenfellner M, Schultz‐Lampel D, Thuroff JW. In situ tunneled bowel flap tubes: 2 new techniques of a continent outlet for Mainz pouch cutaneous diversion. Journal of Urology 1995;153:308‐15. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lightfoot 2007 {published data only}
- Lightfoot AJ, Eno M, Kreder KJ, O'Donnell MA, Rao SS, Williams RD. Treatment of postoperative ileus after bowel surgery with low‐dose intravenous erythromycin. Urology 2007;69(4):611‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mansson 1997 {published data only}
- Mansson A, Colleen S, Hermeren G, Johnson G. Which patient will benefit from psychosocial intervention after cystectomy for bladder cancer. British Journal of Urology 1997;80:50‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mansson 2004 {published data only}
- Mansson A, Henningsohn L, Steineck G, Mansson W. Neutral third party versus treating institution for evaluating quality of life after radical cystectomy. European Urology 2004;46(2):195‐9. [19501] [DOI] [PubMed] [Google Scholar]
Mattei 2008 {published data only}
- Mattei A, Birkhaeuser FD, Baermann C, Warncke SH, Studer UE. To stent or not to stent perioperatively the ureteroileal anastomosis of ileal orthotopic bladder substitutes and ileal conduits? Results of a prospective randomized trial. Journal of Urology 2008;179(2):582‐6. [DOI] [PubMed] [Google Scholar]
Morey 2006 {published data only}
- Morey AF, Evans LA, McDonough RC, III, Park AM, Sexton WJ, Basler JW, et al. Evaluation of mechanical bowel preparation methods in urinary diversion surgery. Canadian Journal of Urology 2006;13(5):3250‐4. [23037] [PubMed] [Google Scholar]
Okada 1989 {published data only}
- Okada Y, Arai Y, Oishi K, Takeuchi H, Yoshida O. Stable formation of the nipple valve in Kock Pouch for diversion of the urinary tract. Surgery, Gynecology and Obstetrics 1989;169:315‐8. [PubMed] [Google Scholar]
Osman 2004 {published data only}
- Osman Y, Abol‐Enein H, Nabeeh A, Gaballah M, Bazeed M. Long‐term results of a prospective randomized study comparing two different antireflux techniques in orthotopic bladder substitution. European Urology 2004;45(1):82‐6. [DOI] [PubMed] [Google Scholar]
Osman 2009 {published data only}
- Osman Y, Abol‐Enein H, El‐Mekresh M, Gad H, Elhefnawy A, Ghoneim M. Comparison between a serous‐lined extramural tunnel and T‐limb ileal procedure as an antireflux technique in orthotopic ileal substitutes: a prospective randomized trial. BJU International 2009;104(10):1518‐21. [DOI] [PubMed] [Google Scholar]
Shaaban 1992 {published data only}
- Shaaban AA, Gaballah MA, El‐Diasty TA, Ghoneim MA. Urethral controlled bladder substitution: A comparison between the intussuscepted nipple valve and the technique of Le Duc as antireflux procedures. Journal of Urology 1992;148:1156‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Shokeir 1995 {published data only}
- Shokeir AA, Ghoneim MA. Further experience with the modified ileal ureter. Journal of Urology 1995;154(1):45‐8. [PubMed] [Google Scholar]
Speakman 1989 {published data only}
- Speakman MJ, Bramwell SP, Deane RF. A prospective comparison of ileocystoplasty and human dura mater cystoplasty in the treatment of detrusor instability (Abstract number 134). Proceedings of the 19th Annual Meeting of the International Continence Society; 1989 Sept 7‐9; Ljubljana, Slovenia. 1989:266‐7.
Studer 1997 {published data only}
- Studer UE, Zingg EJ. Ileal orthotopic bladder substitutes. Urologic Clinics of North America 1997;24(4):781‐93. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Thakar 1998 {published data only}
- Thakar BR, Stanton SL, Robinson G, Clarkson P, Shah K, Manyonda IT. Does hysterectomy affect bladder and bowel function (Abstract number 166). Neurourology and Urodynamics 1998;17:83‐4. [Google Scholar]
Vakalopoulos 2011 {published data only}
- Vakalopoulos I, Dimitriadis G, Anastasiadis A, Gkotsos G, Radopoulos D. Does intubated uretero‐ureterocutaneostomy provide better health‐related quality of life than orthotopic neobladder in patients after radical cystectomy for invasive bladder cancer?. International Urology & Nephrology 2011;43(3):743‐8. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Skinner 2009 {published data only}
- Skinner EC, Skinner DG. Does reflux in orthotopic diversion matter? A randomized prospective comparison of the Studer and T‐pouch ileal neobladders. World Journal of Urology 2009;27(1):51‐5. [DOI] [PubMed] [Google Scholar]
Additional references
Bramble 1982
- Bramble FJ. The treatment of adult enuresis and urge incontinence by enterocystoplasty. British Journal of Urology 1982;54(6):693‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bramble 1990
- Bramble FJ. The clam cystoplasty. British Journal of Urology 1982;66(4):337‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bricker 1950
- Bricker EM. Bladder substitution after pelvic evisceration. Surgical Clinics of North America 1950;30:1511‐21. [DOI] [PubMed] [Google Scholar]
Couillard 1995
- Couillard DR, Webster GD. Detrusor instability. Urologic Clinics of North America 1995;22(3):593‐612. [MEDLINE: ] [PubMed] [Google Scholar]
George 1991
- George VK, Russell GL, Shutt A, Gaches CG, Ashken MH. Clam ileocystoplasty. British Journal of Urology 1991;68(5):487‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hanno 1990
- Hanno P, Levin RM, Monson FC, Teuscher C, Zhou ZZ, Ruggieri M, et al. Diagnosis of interstitial cystitis. Journal of Urology 1990;143(2):278‐81. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kock 1982
- Kock NG, Nilson AE, Nilsson LO, Norlen LJ, Philipson BM. Urinary diversion via a continent ileal reservoir: clinical results in 12 patients. Journal of Urology 1982;128(3):469‐75. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kock 1988
- Kock NG, Ghoneim MA, Lycke KG, Mahran MR. Urinary diversion to the augmented and valved rectum: preliminary results with a novel surgical procedure. Journal of Urology 1988;140(6):1375‐79. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kockelbergh 1991
- Kockelbergh RC, Tan JB, Bates CP, Bishop MC, Dunn M, Lemberger RJ. Clam enterocystoplasty in general urological practice. British Journal of Urology 1991;68(1):38‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kristjansson 1995a
- Kristjansson A, Wallin L, Mansson W. Renal Function up to 16 years after conduit (refluxing or anti‐reflux anastomosis) or continent diversion. 1. Glomerular filtration rate and patency of uretero‐intestinal anastomosis. British Journal of Urology 1995;76:539‐45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kristjansson 1995b
- Kristjansson A, Bajc M, Wallin L, Willner J, Mansson W. Renal function up to 16 years after conduit (refluxing or anti‐reflux anastomosis) or continent urinary diversion. 2. Renal scarring and location of bacteriuria. British Journal of Urology 1995;76:546‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lapides 1972
- Lapides J, Diokno AC, Silber SJ, Lowe BS. Clean, intermittent self‐catheterization in the treatment of urinary tract disease. Journal of Urology 1972;107(3):458‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lewis 1990
- Lewis DK, Morgan JR, Weston PM, Stephenson TP. The "clam": indications and complications. British Journal of Urology 1990;65(5):488‐91. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mansson 1989
- Mansson W, Ahlgren G, White T. Glomerular filtration rate up to 10 years after urinary diversion of different types. Scandinavian Journal of Urology and Nephrology 1989;23:195‐200. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mikulicz 1899
- Mikulicz J. [Zur operation der augeborenen blasenspalte]. Zentralblatt für Chirurgie 1899;26:641. [Google Scholar]
Nabi 2005
- Nabi G, Yong SM, Ong E, McPherson G, Grant A, N'Dow J. Is orthotopic bladder replacement the new gold standard? Evidence from a systematic review. Journal of Urology 2005;174(1):21‐8. [DOI] [PubMed] [Google Scholar]
Neal 1989
- Neal DE. Urodynamic investigation of the ileal conduit: upper tract dilatation and the effects of revision of the conduit. Journal of Urology 1989;142(1):97‐100. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Office for National Statistics 2002
- http://info.cancerresearchuk.org/cancerstats/types/bladder/. website Cancer Research UK. [Google Scholar]
Sethia 1991
- Sethia KK, Webb RJ, Neal DE. Urodynamic study of ileocystoplasty in the treatment of idiopathic detrusor instability. British Journal of Urology 1991;67(3):286‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Studer 1991
- Studer UE, Spiegel T, Casanova GA, Springer J, Gerber E, Ackermann DK, et al. Ileal bladder substitute: antireflux nipple or afferent tubular segment?. European Urology 1991;20(4):315‐26. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Thompson 1996
- Thompson AC, Christmas TJ. Interstitial cystitis‐‐an update. British Journal of Urology 1996;78(6):813‐20. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ware 1993
- Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36 Health Survey Manual and Interpretation Guide. Boston, Massachusetts: The Health Institute, New England Medical Centre, 1993. [Google Scholar]
Webb 1990
- Webb RJ, Lawson AL, Neal DE. Clean intermittent self‐catheterisation in 172 adults. British Journal of Urology 1990;65(1):20‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


