Abstract
Bilharziasis (Schistosomiasis) is the third devastating tropical disease globally and is endemic in many countries including Egypt. The pathology of chronic colonic schistosomiasis results from egg‐induced immune response, granuloma formation, and associated fibrotic changes that may manifest as bloody diarrhea, cramping, and, eventually, inflammatory colonic polyposis. Huge polyps complicating schistosomiasis are not frequently reported in the literature. Also, huge polyps as a sole manifestation of intestinal bilharziasis are rather rarely reported. Here, we report an Egyptian male patient who presented with bleeding per rectum with a huge polyp on colonoscopy, with morphological traits that mimicked colon cancer and proved to be of bilharzial etiology after surgical excision.
Keywords: bilharziasis, cancer colon, intestinal schistosomiasis, polyp
Bilharziasis is an endemic helminthic disease in Egypt. Huge colonic polyps may be of bilharzial origin, and it may be the lone pathology of this disease. Furthermore, it may mimic colon cancer.

Introduction
Bilharziasis (Schistosomiasis) is a helminthic disease that has been endemic in Egypt around the river Nile over centuries, and some evidence supports its prevalence in ancient Egypt as well. In Egypt, we have two prevalent species of Schistosoma: Schistosoma haematobium and Schistosoma mansoni, inhabiting the vesical and mesenteric venous plexuses causing urinary and intestinal bilharziasis, respectively.1
Schistosomiasis is not limited to Egypt, and it is the third devastating tropical disease globally and is a major cause of morbidity and mortality in developing countries in Africa, South America, the Caribbean, the Middle East, and Asia, with different species of the parasite prevalent in many regions around the world. The disease is endemic in 74 countries, and it is estimated that 250 million people are infected, and approximately 700 million people are at risk of infection. Regarding the at‐risk population, an estimated 660 million are concentrated in Africa, accounting for 85% of the global at‐risk estimate.2
In case of S. mansoni infection, the adult worms migrate against the blood stream inside the intestinal venous plexus until they finally lay eggs in the bowel wall. The eggs dig their way through the wall and extrude from the mucosa, causing minute ulcers that bleed, and some eggs pass in the stool. Eggs trapped inside the lumen will evoke granuloma formation that ends by fibrosis. With the accumulation of granuloma, a polyp may be finally formed and protrude within the bowel lumen, and it may ulcerate and cause intermittent bleeding. Most of the formed polyps are small in size and are rarely mistaken for malignant polyps.3
Colon cancer is the seventh most common cancer in Egypt, representing 3.47% of cancers in men and 3% of cancers in women. In 2015, the estimated number of colon cancer patients (excluding rectal cancer) was approximately 3 000.4 Huge polyps complicating schistosomiasis are not frequently reported in the literature, and polyps as a sole manifestation of intestinal bilharziasis are rather rarely reported in the literature.
Case report
Here, we report a 48‐year‐old Egyptian male farmer who presented to our outpatient clinic with recurrent episodes of fresh bleeding per rectum. The patient had no local causes for rectal bleeding as confirmed by surgical consultation. The laboratory data were as follows: Hb 10.8 g/dL, serum albumin 4.2 g/dL, serum bilirubin 1 mg/dL, serum creatinine 0.9 mg/dL, and negative for hepatitis C virus antibodies. Pan‐colonoscopy of the cecum showed a huge polypoidal mass of about 5 cm with broad pedicle 20 cm from the anal verge (Fig. 1). Despite the suspicious malignant features of the mass, large size, broad base, eroded surface, and high vasculature, the histopathology showed small bilharzial granulomas (Fig. 2), and the patient received a single dose of praziquantel. Six weeks later, a second colonoscopy was performed as the bleeding persisted. No noticeable change in size was observed. The second biopsy was confusing as it did not detect any bilharzial ova or malignancy and showed hyperplastic mucosa. Computed tomography (CT) examination demonstrated the luminal mass and showed circumferential wall thickening in the colon. On these findings, the probability of malignancy could not be excluded, so the patient was referred for surgical resection and anastomosis (Fig. 3). The postoperative biopsy proved the pure bilharzial nature of the mass with both fresh and calcified ova.
Figure 1.

Colonoscopy showing huge polyp.
Figure 2.
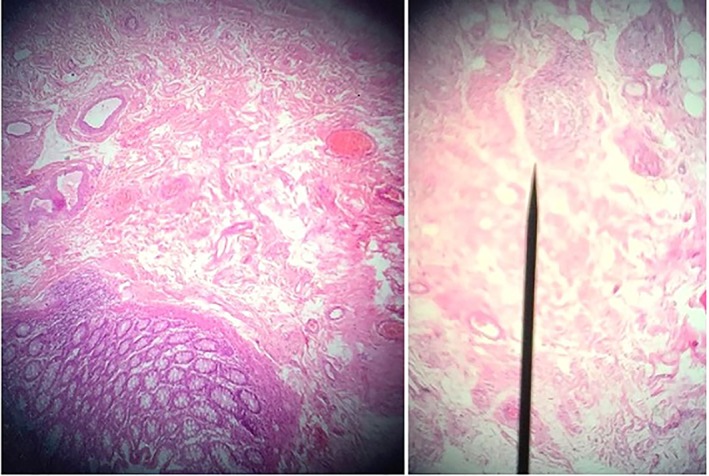
Histopathology showing the bilharzial ova with chronic inflammatory cell infiltrate.
Figure 3.

Resected segment of the colon with the polyp.
Discussion
The development of a bilharzial polyp occurs through different steps. It begins as a small submucosal granuloma, elevating the mucosa overlying it. Then, owing to its weight, proliferation of the mucosa overlying and surrounding it, and pressure of the stools, it acquires a stalk. The stalk is composed of a layer of actively proliferating mucosa, covering a core of connective tissue containing the blood supply. The body of the polyp is composed of a covering of the same sort of epithelium as that which covers a small bilharzial granuloma; it contains an abundance of goblet cells that secrete a great deal of mucous; and it is delicate, very vascular, and bleeds easily with the passage of stools or when touched with the end of the scope. This explains the frequent, mucous, and bloody stools noticed in most of these patients. Although any part of the bowel may be the seat for bilharzial polyps, it is commonly encountered in the rectosigmoid region. However, large polyps were also reported in the ascending colon and the cecum.5
The symptoms associated with colonic schistosomiasis are nonspecific and may mimic other gastrointestinal pathologies, like nonspecific abdominal pain, diarrhea, constipation, alternating bowel habits, or bleeding per rectum.6 Atik et al.6 reported an extremely rare presentation in a 25‐year‐old Brazilian patient who presented colonic perforation and fecal peritonitis due to multiple colonic bilharzial polyps, and thick colonic wall perforating into the abdominal cavity was detected in postlaparotomy histopathology. In addition, Issa et al.5 reported large right‐side colonic bilharzial polyp is a 20‐year‐old Ethiopian woman, who presented with long‐standing abdominal pain. Our patient did not report any symptoms suggestive of bilharziasis. In fact, the bleeding per rectum experienced by our patient was investigated by colonoscopy after exclusion of local causes. In agreement with the nonspecific presentations of our patient, Titi et al.7 reported bilharzial cecal polyp as the cause of nonspecific abdominal pain in a 61‐year‐old male patient, initially diagnosed as Crohn's disease, following single accidental exposure to infected water.
Colonic polyps are markers of the chronic stage of the disease. Hence, diagnosis of colonic polyps is mainly dependent on rigid sigmoidoscopy, colonoscopy, or barium enema. For decades, rectal snips taken in the outpatient department by rigid sigmoidoscopy and freshly examined slides by transparency technique were used not only for diagnosis but also to differentiate living from dead ova.8 In the past, sigmoidoscopy and barium enema were used. However, with the introduction of colonoscopy, lesions beyond the reach of sigmoidoscopy, including the rectal valves, which are known to be heavily infiltrated, can be visualized, biopsied, and excised. In the early stage of the disease, the colonoscopy findings can range from normal mucosa to edematous, congestive mucosa; petechial hemorrhages; or even frank ulcerations. In the late stage, it may show thickened bowel wall, elevated yellow nodules, polyps, and/or bowel stricture.9 In our case, pan‐colonoscopy was unremarkable except for the polyp, and none of the previously described lesions were detected.
In colonic bilharziasis, medical treatment alone will be enough to cure the earliest (infiltration) stage of the disease; it will also cure ulcerating granulomas but will have no great effect on polyps. S. mansoni infection is more resistant than S. hematobium, and the course may need to be repeated after a few weeks. However, some authors reported regression of the polyp size and even disappearance after multiple courses of praziquantel therapy (personal experience). This is logical due to regression of the granuloma size surrounding the dead ova, and that is why we gave the patient praziquantel after the first biopsy, but because we gave only one dose, the polyp did not show any noticeable change in its size.
Endoscopic removal of the polyps may be the gold standard, especially for nonsmall polyps that are not expected to regress with multiple courses of praziquantel. This was the rationale used to schedule our patient for a polypectomy in the workshop. Different authors reported successful removal of bilharzial polyps using endoscopy with a low complication rate. In the study by El‐Afifi et al.,10 the authors successfully removed multiple bilharzial polyps without any complications. In another study by Issa et al.,5 the authors successfully excised a large polyp in the right colon.
Surgery is not routinely used for the removal of bilharzial polyps. However, surgery may be required in certain situations: first, for low rectal polyps within the reach of fingers; second, in the past, before the availability of flexible colonoscopy, it was performed for high polyps beyond sigmoidoscopic reach; and third, for massive polyposis of the pelvic colon. All these indications encouraged Bessa et al.11 to perform surgical procedures for 40 patients with colonic schistosomiasis after they failed to control the severe dysenteric symptoms through medical treatment, and they concluded that surgical procedures are safe. In our case, we referred the patient for surgery due to the high possibility of malignancy. In addition, CT scans increased our suspicion.
In our case, we have several points on which to base the ligation. First, the size of the polyp we reported was huge, and this is not frequently seen in bilharziasis. Second, there was a lack of other morphological features suggestive of bilharzial colonic affection, for example, ulcers and the occurrence of this solitary large polyp as the sole manifestation of intestinal bilharziasis. Hence, we can advise endoscopists working in bilharzia‐endemic areas not to ignore bilharziasis as an etiology of colonic polyps, even if they are huge or not associated with other morphological lesions in the colonic mucosa. Third, there was confusion regarding malignancy due to the polyp's high vascular pattern, and in our case, although gross features were in favor of malignancy, the biopsy dilemma made the group favor malignancy. Finally, it seems that a single dose of praziquantel is not effective in treating such cases because our patient showed no noticeable change in polyp size nor complaint.
In conclusion, we believe that, after management of this patient, including surgical excision of this huge polyp, we served our patient in the right way, and we demonstrated to our peer gastroenterologists and endoscopists, not only in our locality but also worldwide, that huge polyps may be of bilharzial origin, and they may be the lone pathology of this disease. Furthermore, they may mimic colon cancer.
Declaration of conflict of interest: None.
References
- 1. Strickland GT. Liver disease in Egypt: hepatitis C superseded schistosomiasis as a result of iatrogenic and biological factors. Hepatology. 2006; 43: 915–22. [DOI] [PubMed] [Google Scholar]
- 2. Olveda DU, Li Y, Olveda RM et al. Bilharzia: pathology, diagnosis, management and control. Trop. Med. Surg. 2013; 1: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mostofi FK. Bilharziasis, 1967. https://www.springer.com/gp/book/9783642494925 [Google Scholar]
- 4. Ibrahim AS, Khaled HM, Mikhail NNH, Baraka H, Kamel H. Cancer incidence in Egypt: results of the national population‐based cancer registry program. J. Cancer Epidemiol. 2014; 2014: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Issa I, Osman M, Aftimos G. Schistosomiasis manifesting as a colon polyp: a case report. J Med Case Reports. 2014; 8: 331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Atik FA, Lopes Filho GJ, Linhares MM, Seda Neto J, Mansur NS. Large intestine obstruction complicated with perforation: a rare manifestation of Schistosoma mansoni infection. Sao Paulo Med. J. 1998; 116: 1781–3. [DOI] [PubMed] [Google Scholar]
- 7. Titi S, Kosik‐Warzyńska R, Sycz K, Chosia M. Intestinal schistosomiasis–a case report. Pol. J. Pathol. 2003; 54: 283–5. [PubMed] [Google Scholar]
- 8. Harries AD, Speare R. Rectal snips in the diagnosis of hepatosplenic schistosomiasis. Trans. R. Soc. Trop. Med. Hyg. 1988; 82: 720. [DOI] [PubMed] [Google Scholar]
- 9. Tarik Zaher MB, Ibrahim A, Ahmady M, Esmat S, Gouda H, El‐Alfy Y. Colorectal polyps in Sharykia, Egypt: clinico‐pathological study of our experience with endoscopy. J. Med. Sci. 2008; 8: 5. [Google Scholar]
- 10. El‐Afifi S. Intestinal bilharziasis. Dis. Colon Rectum. 1964; 7: 1–13. [DOI] [PubMed] [Google Scholar]
- 11. Bessa SM, Helmy I, Mekky F, Hamam SM. Colorectal schistosomiasis: clinicopathologic study and management. Diseases of the Colon & Rectum. 1979; 22: 390–5. [DOI] [PubMed] [Google Scholar]


