Abstract
Total hip arthroplasty (THA) in sickle cell disease (SCD) patients can be a challenging procedure.
This systematic review evaluated the revision rate, functional outcomes and complications of THA in sicklers.
A systematic search was conducted according to the PRISMA guidelines, using four search engines from inception to May 2019.
Fifteen studies with 971 THAs were included. There were 437 cemented and 520 uncemented THAs.
There were 164 revision THAs (16.8%); 52 uncemented and 105 cemented THAs.
Forty-two infections were recorded; 16 infections for cemented and 23 for uncemented THAs.
Fifty-seven cups, 26 stems, eight cup/stem with aseptic loosening that were more frequently cemented were reported. The 28 unspecified aseptic loosening cases were more frequently uncemented THAs.
All studies demonstrated the functional improvement of patients.
There were 109 medical complications (14.3%). Sickle cell crises (SCC) and transfusion reactions were most usually recorded.
Forty-six intraoperative complications (4.7%) were reported; 18 femoral fractures, four acetabular and 18 femoral perforations. Seventeen femoral fractures occurred during uncemented THA.
THA in SCD is still related to a high risk of complications. The outcomes in properly selected sicklers have been improved. Perioperative adequate hydration, warming, oxygen supply and transfusion protocols are mandated to prevent SCC and transfusion reactions. The surgeon must be prepared to deal with a high rate of intraoperative fractures and have different implant options readily available. No definite conclusion can be made regarding the best fixation mode. Cemented implants demonstrated a higher revision rate and uncemented implants a higher risk for intraoperative complications.
Cite this article: EFORT Open Rev 2020;5:180-188. DOI: 10.1302/2058-5241.5.190038
Keywords: avascular necrosis of femoral head, SCD, sickle cell disease, sicklers, THA, total hip arthroplasty, total hip replacement
Introduction
Sickle cell disease (SCD) is a common autosomal recessive disorder, caused by a point mutation in the b-globin chain of haemoglobin1. This hemoglobinopathy affects the shape of red blood cells that, under low oxygen tension, are susceptible to sickling and hence impede the blood supply to the human tissues.1,2 SCD has high mortality rates.3 The prevalence and severity of the disease are higher in some parts of the world such as Africa.4 SCD patients develop a variety of symptoms based on the severity of the disease. Anaemia, vaso-occlusive crises and chronic organ failure are the main features of SCD.2 Skeletal manifestations of SCD are also prevalent, including avascular necrosis (AVN) of the femoral head, osteoporosis, pathological fractures and infections, namely septic arthritis and osteomyelitis.2,5 Bony deformities such as marrow hyperplasia, thinning of trabeculae and cortices, as well as sclerotic areas that obliterate the femoral canal, are frequently encountered.2,5,6
SCD is one of the most common causes of AVN in childhood.7 The incidence of AVN in sicklers ranges from 3–50% based on the specific genotype.2,8 Symptomatic AVN in sicklers has a high probability of progressing to hip osteoarthritis (OA), usually in the third or fourth decade of life;1 bilateral hip involvement reaches 20–30%.2,8 The initial studies of total hip arthroplasty (THA) for the management of end-stage hip OA in SCD patients reported a high level of failure and complications.9–13 Recent diagnostic and therapeutic advances in the treatment of SCD have improved the life expectancy of sicklers1,6 and the evolution of surgical techniques and implant design promise better outcomes.
This comprehensive systematic review aims to evaluate the literature in terms of revision rate, functional outcomes, type of implant fixation and complications of THA in patients suffering from SCD-related AVN.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.14
Search strategy
A systematic search of PubMed, Cochrane library, ScienceDirect and Ovid MEDLINE was conducted from inception to May 2019 to identify studies reporting outcomes of THA for AVN in SCD patients. In addition, reference lists of relevant published articles were manually searched for missing records. Keywords used in electronic search included “hip arthroplasty”, “hip replacement”, “hip reconstruction”, “sickle cell disease”, “sickle cell anaemia”, “sickle cell”, “sickle cell trait”, “haemoglobin SC Disease”, “Hb SC disease” and these were appropriately combined using Boolean operators.
Eligibility criteria
Eligible studies were randomized and non-randomized controlled clinical trials, retrospective and prospective cohort or case-control studies and case series. The search was narrowed to articles that were published in the English language, whereas no restrictions in the year of publication were imposed. We included studies reporting data on implant survival in primary THAs performed for AVN secondary to SCD. We excluded studies reporting short-term postoperative results (< 2 years), studies reporting arthroplasties other than primary THA (bipolar hemiarthroplasties, resurfacing, resection or revision arthroplasties) and reports on THAs for AVN of different aetiology. Studies evaluating outcomes of different treatment options in SCD patients that do not clearly state results for THA were also excluded.
Outcomes
The primary outcome was the rate of revision of THA in sicklers. Secondary outcomes were the functional outcomes, medical, intraoperative and postoperative complications and the influence of implant fixation type.
Study selection and data extraction
In the first review of the literature, two independent authors (EK, KK) screened titles and abstracts for potentially eligible studies based on the inclusion criteria. Conflicts were resolved through discussion and, when needed, a third investigator independently evaluated any study. Two authors (EK, KK) examined independently in full text and duplicated all the potentially eligible studies based on a standardized data extraction form. Data extracted were demographics, study design, type of implants and fixation, revision rate, functional outcomes and complications. Conflicts were resolved through discussion and when necessary, the senior author evaluated each study independently.
Results
Search results
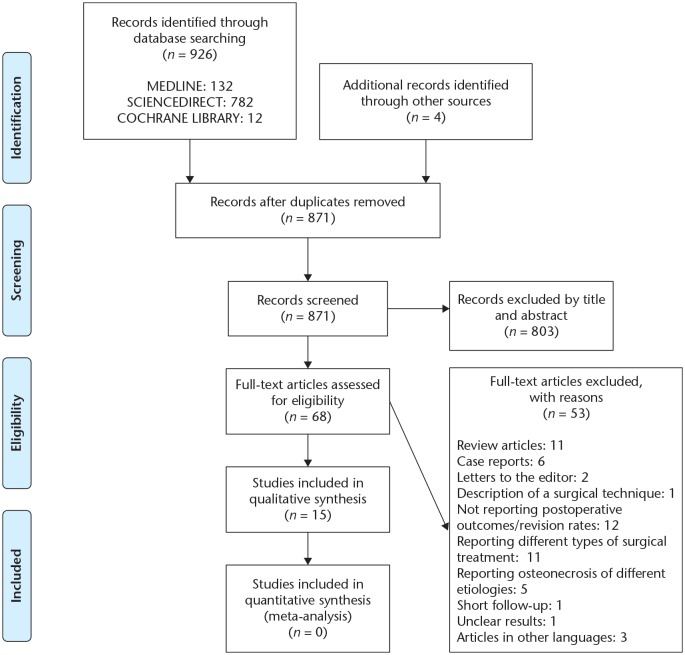
The search of electronic databases revealed a total of 926 relevant studies. Additionally, four related studies were found through a manual search of the reference lists of other studies. After removal of duplicates and assessment of titles and abstracts, 68 studies were considered potentially eligible and were studied in full text. Fifty-three studies were excluded because they did not meet the inclusion criteria. At last, 15 studies were considered eligible and were analysed in this systematic review. Details of the study screening and selection are shown in Fig. 1.
Fig 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines flowchart illustrating the search strategy.
Demographics, patient characteristics, study design
The studies have been published between 1988 and 2019. The vast majority are retrospective case series;7,9–13,15,16,19–23 two of them are retrospective comparative studies.17,18 The number of reported THAs per study ranged from seven to 312. A total of 752 SCD patients undergoing 971 THAs were included; 142 patients received bilateral THAs. Thirteen studies reported on the severity of SCD; 517 homozygous SCD patients were recorded. The mean age of patients at the time of THA ranged from 23.8 to 37 years and the mean follow-up from 3.8 to 14.6 years. Twelve studies reported short-term follow-up (< 10 years)7,9–13,15,17–20,23 and three long-term follow-up results (>10 years).16,21,22 Demographics and other patient and study characteristics are depicted in Table 1.
Table 1.
Demographics, patients’ characteristics and study design of the included studies
| Author | Study type | Patients/ THAs (bilateral) | Severity of SCD | Time of THA | Age at THA*
(years) |
ON stage | Follow up*
(years) |
Sex (men/ women) |
|---|---|---|---|---|---|---|---|---|
| Bishop et al9 | RCS | 11/13 (2) | 6 SS, 2 SC, 3 SThal |
1974–1984 | 31 (16–47) |
N/A | 7.6 (2.8–13.0) |
5/6 |
| Hanker and Amstutz10 | RCS | 5/9 (4) | 2 SS, 1 SThal, 2 AS |
1971–1984 | 32.7 (23–49) |
stage IV: 8 stage III: 1 |
6.25 (2.0–10.4) |
3/2 |
| Acurio and Friedman11 | RCS | N/A/20 | N/A | 1970–1986 | N/A | N/A | N/A | N/A |
| Moran et al12 | RCS | 12/15 (3) | 9 SS, 2 SThal, 4 AS |
1973–1988 | 37 (17–58) |
End-stage ON | 4.8 (2.2–10.4) | N/A |
| Hickman and Lachiewicz13 | RCS | 4/7 (2) | SS, AS and SThal | N/A | N/A | N/A | 6 (2-12) | N/A |
| Al-Mousawi et al15 | RCS | 28/35 (7) | All SS 1 AS |
1984–1995 | 27.5 (19–42) |
N/A | 9.5 (5–15) |
15/13 |
| Hernigou et al16 | RCS | 244/312 (34) | 145 SS,87 SC, 12 SThal |
1980–2000 | 32 (18–51) |
Steinberg IV | 13 (5–25) |
118/126 |
| Al Omran17 | RC | 118/136 (18) | 92 SS, 24 SThal, 18 AS, 2 SC | 1991–2007 | 28–29 (17–38) |
N/A | 7(2–18) C:12/U:5 |
82/54 |
| Issa et al18 | RC | 32/42 | 22 SS, 10 AS | 2001–2007 | 37 (18–58) |
Ficat III:8, IV:34 | 7.5 (5–11) |
10/22 |
| Gulati et al7 | N/A | 39/50 (11) | 19 SS,15 SC, 5 SThal | 2007–2011 | 22 (13–49) |
SteinbergIII:4, IV:9, V:26 | 3.8 (2–6) |
11/28 |
| Jack et al19 | RCS | 40/52 | 31 SS, 8 SC, 1 SThal |
2002–2011 | 36.1 (17–54) |
N/A | 5.2 (2.0–10.1) |
16/24 |
| Azam and Sadat-Ali20 | RCS | 67/84 (17) | 39 SS, 28 AS |
1990–2012 | 24 (17–46) |
Ficat IV | 7.5 (4–12) |
37/30 |
| Ilyas et al21 | RCS | 101/133 (32) | All SS | 2000–2012 | 25 (16–54) |
Steinberg ⩾ IV |
14.6 (5–17) |
49/52 |
| Farook et al22 | RCS | 30/34 (4) | 24 SS, 4 SC, 1 Sthal, SS G | 1999–2016 | 36.7 (20-59) |
Steinberg ⩾ IV |
10.5 (1–18) |
12/18 |
| Katchy et al23 | N/A | 21/29 (8) | N/A | 2008–2012 | 23.8 (18–32) |
N/A | 5 (N/A) |
18/3 |
Note. RCS, retrospective case series; RC, retrospective comparative study; N/A, not answered; SCD, sickle cell disease; SS, SCD homozygous for the sickle cell gene; SC, SCD heterozygotes for Hb S and Hb C; Sthal, types of sickle-beta-thalassemia; SS G, G Philadelphia variant; AS, sickle cell trait; ON, osteonecrosis; C, cemented; U, uncemented.
Results are given as mean with the range in parentheses.
Operative and implant data
Twelve studies reported on the type of surgical approach used.7,9,12,13,15,16,18–23 The posterior-based approaches were used in 422 patients, lateral (Hardringe) for 183, anterolateral for 150, Freeman transgluteal for 34 and the transtrochanteric approach in four patients. Fourteen studies7,9,11–13,15–23 reported on the type of implant fixation; there were 437 cemented, 520 cementless and five hybrid THAs; nine cases were unspecified. The majority of studies published before 2010 reported on cemented THAs but afterward this date only uncemented THAs were reported. Six studies gave information about the bearing couple of THA used.7,17–19,21,22 The operative and implant data are depicted in Table 2.
Table 2.
Operative and implant characteristics, and functional scores of SCD patients for the included studies
| Author | Surgical Approach | Type of anaesthesia | Type of fixation | Type of stem | Femoral Head/bearing couple | Type of Cup | Functional Score (preop/postop) |
|---|---|---|---|---|---|---|---|
| Bishop et al9 | Posterior, lateral | N/A | 12 C 1 U |
N/A 1 pc |
N/A | N/A 1 pc |
HHS (72–83) |
| Hanker and Amstutz10 | N/A | N/A | N/A | N/A | N/A | N/A | UCLA |
| Acurio and Friedman11 | N/A | N/A | 16 C, 4 U | N/A | N/A | N/A | HHS |
| Moran et al12 | Posterior 11 Transtrochanteric 4 |
General, epidural | 13 C 2 U |
N/A 1H-G, Zimmer 1Omnifit, Osteonics |
N/A | N/A H-G (Zimmer) |
HHS (47/88) |
| Hickman and Lachiewicz13 | PL | General and spinal | U | 5 H-G, 2 Multilock (Zimmer) | N/A | H-G (Zimmer) |
HSS (36/94) |
| Al-Mousawi et al15 | PL | 24 General, 4 Spinal |
C | N/A | N/A | N/A | HSS (36/ 86) |
| Hernigou et al16 | PL | General | C | Ceraver Osteal (Ceraver) | 32 mm ceramic | Polyethylene cup Ceraver | MAP pain (2.5/5.8) |
| Al Omran17 | N/A | N/A | 46 C 90 U |
Charnley 54 JRI-Furlong (JRI) 36 Bimetric (Biomet) |
22.25mm ceramic CoCr |
UHMWP cup threaded cup Ring Loc cup |
HSS (42/92) HSS (38/84) |
| Issa et al18 | AL 37 Posterior 5 | N/A | U | Accolade (Stryker) |
Ceramic/ CoCr | Trident (Stryker) | HSS (43/87) |
| Gulati et al7 | Lateral (Hardringe) | N/A | U | Accolade (Stryker- Howmedica) | 28/36 mm CoCr | HA-coated (Stryker) |
HSS (42/92) |
| Jack et al19 | Posterior | Spinal or epidural | U | Modular SROM: 48, A Solutions: 3, AML: 1 (DePuy) | CoC (Ceramtec) |
Duraloc: 42 Deltamotion: 1 Pinnacle: 9 (DePuy) |
N/A |
| Azam and Sadat-Ali20 | AL | N/A | U | pc proximal fixation |
N/A | pc | HSS (46/81) |
| Ilyas et al21 | Lateral (Hardringe) | Epidural: 82, General: 51 |
U | Bimetric (Biomet) |
MoP 96 CoP 20 CoC 10 |
Mallory-Head (Biomet) |
MAP Pain: (1,2/5,1) |
| Farook et al22 | Freeman’s transgluteal | Spinal General |
3 C, 5 H, 26 U |
Exeter TM: 8 (Stryker Howmedica) ABG: 3 (Stryker), S-ROM: 4, JRI: 2, Corail: 17 (DePuy) |
CoC 21 MoM 2 MoP 2 CoP 1 |
N/A | N/A |
| Katchy et al23 | AL | General 7 regional 22 | U | Corail (DePuy) | 28 mm | Dulalock (DePuy) | HHS (20.1-88.7) |
Note. N/A, not answered; PL, posterolateral; AL, anterolateral; C, cemented; U, uncemented; H, hybrid; pc, porous-coated; H-G, Harris-Galante; AML, anatomic medullary locking; CoC, ceramic on ceramic; CoP, ceramic on polyethylene; MoM, metal on metal; MoP, metal on polyethylene; UHMWP, ultrahigh molecular weight polyethylene; HHS, Harris Hip Score; MAP, Merle D’Aubigne Postel score.
Revision rate, infection and aseptic loosening
A total of 164 THAs were revised, demonstrating an overall revision rate of 16.8%. The revision rate ranged from 0% to 55.5% in different studies; it was reduced for studies reported during the last two decades (Table 3). One hundred and five revisions were reported for cemented (24%), 52 for uncemented (10%) and two for hybrid THAs; there were also five revision cases with unspecified type of fixation. Long-term follow-up studies16,21,22 demonstrated 10.5% to 17.6% revision rates. In the longest follow-up studies, 48 out of 312 cemented THAs were revised at a mean of 13 years16 and 14 out of 133 uncemented THAs at a mean of 14.6 years.21
Table 3.
Postoperative complications and revision rate of the SCD patients in the included studies
| Author | Complications | Revisions (rate)** | PJI rate** | Aseptic loosening** | ||
|---|---|---|---|---|---|---|
| Medical | Intraop | Postop | ||||
| Bishop et al9 | 0 | N/A | N/A | 3 (23) | 3 (23) | 0 |
| Hanker and Amstutz10 | SCC: 2, TR: 1, UTI: 1, heart failure: 2 |
FP: 1 | SNP: 1 | 5 (55.5) | 3 (33) | 2 (22.2) |
| Acurio and Friedman11 | N/A* | N/A* | N/A* | 10 THA (50) | N/A | N/A |
| Moran et al12 | UTI: 1, DVT: 1, SCC: 1, TR: 1, heart failure: 2 |
FP: 1, AP: 1 | WD: 3, WH: 2, Dislo: 1 |
5 (33.3) | 1 (6.6) | Cup: 4 (26.6) Stem: 0 |
| Hickman and Lachiewicz13 | SCC: 1, DVT: 1 TR: 1 |
PF: 1 | WH: 1, Dislo: 3 Exc bleeding: 2 |
2 (28.5) | 0 | Ischial: 2 (28.5) |
| Al-Mousawi et al15 | SCC: 6 | FP: 3, FF: 1 Excessive bleeding: 2 |
WD: 4 HO: 4 |
7 (20) | 1 (2.8) | Cup and stem: 4 (11.4) Cup: 2 (5.7) |
| Hernigou et al16 | SCC: 2, ACS: 4, DVT: 1, PE: 1 TR - Minor: 62 - Major: 9 |
FP: 6 Repeat cup fixation:4 |
WH: 4, peroneal nerve palsy 2, HO: 12 Dislo: 6 |
48 (15.3) | 10 (3) | Cup: 21 (7) Femur: 17 (5) |
| Al Omran17 | N/A | N/A | 2 recurrent dislo (C) | Total: 48 (35.2) C: 28 U: 20 |
C: 1 (2.1) U: 1 (1.1) |
C/Cup: 15 (32.6), Stem: 8 (17.3), both: 2 (4.3) U: 19 (21.1) |
| Issa et al18 | N/A | None | None | 5 (11.9) | 2 (4.7) | Cup/stem:2 (4.7) |
| Gulati et al7 | SCC: 6 | FF: 1 | WH: 3, WD: 2 LLD < 1 m: 3 |
0 | 0 | 0 |
| Jack et al19 | SCC: 5, UTI: 1, PS: 1, chickenpox: 1, DHTR: 3, VE: 2 | FF: 5 | Dislo: 2, LLD 1 cm: 2, HO: 34 Brooker I (33) |
1 (1.9) | 0 | 0 |
| Azam and Sadat-Ali20 | ACS: 2 | FF: 5 AP: 3, FP: 4 |
WH: 7 Thigh pain: 2 |
10 (11.9) | 8 (9.5) S: 6 D: 2 |
7 (8.3) |
| Ilyas et al21 | SCC: 12, ACS: 3 | FF: 6 - 4 calcar - 2 shaft |
HO: 60 Brooker I: 36, II: 12, III: 7, IV: 5, Dislo: 1, SNP: 2 |
14 (10.5) | 9 (6.7) S: 4 D: 5 |
Cup: 8 (6) Stem: 1 (0.75) |
| Farook et al22 | PE: 1 | FP: 2 | HO: 8 Brooker I–II |
6 (17.6) C: 4, H: 2 |
U: 2 (5.8) | Cup: 5 (14.7) Stem: 0 |
| Katchy et al23 | Pulmonary: 1, SCC: 1 | (N/A) | PPF: 1 | 0 | 1 (3.4) | 0 |
Note. SCC, sickle cell crisis; TR, transfusion reaction; UTI, urinary tract infection; DVT, deep vein thrombosis; N/A, not answered; ACS, acute chest syndrome; PE, pulmonary embolism; PS, pseudomonas sepsis; DHTR, delayed hemolytic transfusion reactions; VE, vasovagal episodes; FP, femoral perforations; AP, acetabular perforations; FF, femoral fractures; SNP, sciatic nerve palsy; WD, wound drainage; WH, wound hematoma; Dislo, dislocation; Exc, excessive; HO, heterotopic ossification; PFF, periprosthetic fracture; THA, total hip arthroplasty; C, cemented; U, uncemented; H, hybrid; S, superficial; D, deep.
The study reports on complications but it does not give information for those patients who have undergone THA.
The values are given as raw numbers with the percentages in parentheses.
Forty-two cases of infection (superficial and deep) were recorded. Sixteen infections were reported for cemented (3.6%) and 23 for uncemented THAs (4.4%); there were also three infection cases with unspecified type of fixation. The infection rate of studies varied between 0% and 33%. Long-term follow-up studies reported infection rate between 3% and 6.7%.16,21,22
Fifty-seven THAs were failed due to cup aseptic loosening, 26 due to stem loosening and eight due to combined cup and stem loosening; there were also 28 cases of aseptic loosening that cup or stem was not specified. Forty-three cemented cups, 25 cemented stems and six combined cups and stems demonstrated aseptic loosening. Twelve uncemented cups, one uncemented stem and two combined cups and stems were also recorded; however, another 26 unspecified cases of aseptic loosening were reported for uncemented THAs (Table 3). Studies showed higher aseptic loosening rates for cups than for stems. In the only comparative study cemented THAs failed more frequently than uncemented; however, the follow-up was longer for cemented THAs.17
Functional outcomes
Eleven studies reported on the functional outcomes of SCD patients after THA. The Harris Hip Score (HHS) was used in nine7,9,12,13,15,17,18,20,23 and Merle d’Aubigne and Postel score in two reports.16,21 All studies showed a significant increase in functional scores at the last follow-up (Table 2). The mean HHS was comparable at the last follow-up between two cohorts undergoing THA for SCD or other reason related to AVN.18 In another comparative study, the HHS was significantly improved both in cemented and uncemented THAs, but no comparison between them was provided.17
Complications
Thirteen studies reported the medical, intraoperative and late postoperative complications of sicklers undergoing THA.7,9,10,12,13,15,16,18-23
Medical
A total of 139 medical complications, with an overall complication rate of 14.3% have been reported (Table 3). Sickle cell crises (36) and transfusion reactions (77) were the most frequent medical complications. Nine cases of acute chest syndrome (ACS) have also been recorded. The overall medical complication rate of studies varied significantly from 0% to 43%. During the last two decades the rate has diminished but is still high (Table 3).
Intraoperative
A total of 46 intraoperative surgical complications, with an overall rate of 4.7% have been reported (Table 3). Eighteen femoral fractures, four acetabular and 18 femoral perforations during bone preparation have been recorded. The vast majority of femoral fractures (17/18) occurred during uncemented THA. The overall intraoperative rate of complications ranged from 0% to 17.1%. There are still reports with high complication rates in recent studies (Table 3).
Postoperative
A total of 174 postoperative complications, excluding aseptic loosening and infection, with a limited number of dislocations (15) have been recorded. Recent studies reported on a high percentage of heterotopic ossification reaching as high as 45%;21,22 however, the majority were Brooker type I and II.
Discussion
This systematic review evaluated the outcomes of primary THA in patients suffering from SCD-related AVN. THA performed in sicklers still demonstrates a high percentage of medical, intraoperative and postoperative complications as well as implant failure rate. However, recent advances in the management of SCD patients and improvement of implant design and coating have substantially improved outcomes. Aseptic loosening and infection are the most frequent reasons for revision. Cup aseptic loosening was more commonly reported than stem aseptic loosening. Sickle cell crises and transfusion reactions were the usual medical complications. No definite conclusion can be made regarding the best fixation mode. Cemented implants demonstrated a higher revision rate, and uncemented implants a higher risk of intraoperative complications.
The main limitation of this review is the low level of evidence of the published studies; the majority are non-randomized retrospective case series reporting outcomes over the last 40 years.7,9–13,15,16,19–23 The tremendous changes that have been made during this period in the management of SCD patients affected the uniformity of the studies. The great heterogeneity of the studies raises concerns regarding the validity of the results making it unclear as to whether reasons such as the surgeon’s level of experience, new designs or medical preparation are responsible for better outcomes. On the one hand, there is a lack of comparative studies that could generate more critical outcomes. On the other hand, many reports have published medium to long-term follow-up data strengthening the results. Another limitation is that our study was not registered in a database of systematic review protocols.
SCD is a severe medical condition with a high risk of mortality3 and different prevalence around the world.4 THA remains the gold standard of treatment for end-stage hip OA in SCD patients. In the largest series of cemented16 and uncemented21 THAs significant improvements in pain, hip function and range of motion of patients were reported. All studies reported significant improvement in the quality of life of patients; both cemented and uncemented THAs provided satisfactory functional results.
Although the outcomes of THA in SCD patients have improved during recent decades, the revision rates remain high. In a recent meta-analysis, SCD was recognized as the leading risk factor of higher revision rate in patients undergoing THA for AVN.24 Our study demonstrated an overall revision rate of 16.8%.
Infection and aseptic loosening are the main reasons for revision in SCD. The compromised health status and immunodeficiency secondary to functional asplenia of sicklers increase the vulnerability to bacteremia and hematogenous seeding of the microbes to the bones.1,2 A thorough preoperative evaluation of SCD patients to find all possible sites of bacterial dissemination is necessary; preoperative cholecystectomy has also been proposed in all sicklers with gall stones.16 Quick surgery, proper handling of soft tissues and the use of antibiotic-impregnated cement in cemented THA are essential to reduce the risk of infection.15,16 Salmonella typhi is the most typical microbe found in infected bone of SCD patients. However, as it is more frequently encountered in younger patients and has not been reported as a pathogen in infected THA, the preoperative prophylaxis for salmonella is not recommended.2 Staphylococcus aureus is the most common microorganism isolated in infected THA;16,21 gram-negative microorganisms such as Acinetobacter, Proteus, and Pseudomonas have also been found, and chemoprophylaxis should be adjusted accordingly.16,21 First and second-generation cephalosporins16,18 and combination of cephalosporins with semisynthetic glycopeptide antibiotics19 or aminoglycosides21 for no more than 36 postoperative hours have been used. The routine use of intraoperative cultures and histopathological analyses from skeletal sites before the final implantation and continuation of antibiotics until the results of the cultures has been proposed.25 In the case of positive cultures, the antibiotic therapy is further continued based on the sensitivity profile of the isolated microorganism.25 A perioperative infection rate of 7% to 15% was confirmed in three studies7,16,21 that followed this protocol.
Aseptic loosening is another cause for concern in the young group of SCD patients. The rate of aseptic loosening of the cup was higher than that of the stem. The best implant fixation option for sicklers is still debated. During the last decade, however, all published studies used uncemented implants showing improved results in terms of aseptic loosening.18–23 Unfortunately, there are no high-quality comparative studies between cemented and uncemented implants. The reports of THAs performed before 2000 using cemented implants demonstrated high complication rates;9–13,15 however, the inappropriate management of patients and cement technique probably affected the results. Hernigou et al reported the largest series of fully cemented THAs that were performed before 2000.16 Twenty-one cups (7%) and 17 femoral stems (5%) were revised due to aseptic loosening at a mean follow-up time of 14 years. In the largest series of uncemented THAs performed between 2000 and 2012, Ilyas et al reported two cases of aseptic loosening at a mean follow-up of 15 years; however, osteolysis around the cup was evident in seven other cases where only the liner or both liner and cup were revised.21 In the only comparative study between cemented and cementless fixation in SCD patients, the failure rate of cemented THAs was higher;17 however, cemented THAs had a significantly higher follow-up, were performed in previous decades and had better functional scores than uncemented THAs.17 Advocates of cemented THA contend that cement may tamponade the intramedullary canal reducing blood loss, decrease the rate of bone perforations and fractures following the more conservative bone preparation, and also provide immediate rigid fixation in compromised bone.13,16 The opponents of cementation, however, contend that the additional thermal necrosis further increases the risk of infection and loosening and question the ability of the cement to achieve biologic fixation in cases of avascular and suboptimal bone quality.21,22 The difficulties of femoral preparation may affect the cement mantle in sicklers and the so-called ‘French paradox’ is frequently used.15,16 In this cementing technique, the largest possible rectangular canal filling titanium alloy stem is used without obtaining a continuous cement mantle. It is supported that the close cortical contact and direct load transfer through the implant provide inherent stability and protection to the cement mantle.15,16
On the other hand, biologic fixation with uncemented implants demonstrated favourable outcomes in SCD patients.17–23 Although the data are limited, and the best type of uncemented implants is unknown, the use of fully porous-coated implants is supported. Al Omran showed that proximally coated stems had a higher failure rate than fully hydroxyapatite-coated stems in sicklers.17 The extensive porous coating of implants and the young age of patients with compromised but still metabolically active femoral canals may explain the better results of uncemented implants.18,19,21 Delayed full weight-bearing is supported for uncemented THA in SCD patients to reduce the risk of early loosening due to the compromised bone quality.7,21
The rate of medical complications following THA in SCD patients has been reduced but remains high. SCD patients have a significantly higher risk of complications, longer hospitalization and higher hospital charges than matched controls.26 Sickle cell crises and transfusion reactions are the most common medical complications following THA. ACS is the most severe but relatively rare complication; it is a form of acute lung injury clinically diagnosed and managed symptomatically with transfusions, oxygen saturation and hospitalization.16
Only medically fit SCD patients may undergo THA. Preoperatively SCD patients need adequate oxygenation, careful hydration as well as analgesia to avoid SC crises.20 Desensitization to decrease the rate of alloimmunization, leukocyte-depleted blood or preoperative autologous donation are measures to prevent transfusion reactions.16 Preoperative transfusion, plasmapheresis or exchange transfusion are used to reduce the levels of Hb S and increase oxygen transfer capacity. In the majority of studies, the standard of care involves conservative transfusion to keep the preoperative and postoperative Hb between 8–10 g/dl, during the first two postoperative days.7,16,18–22 Exchange transfusion is usually performed to decrease Hb S < 30% in patients with a history of ACS or severe anaemia.16,20,21
The orthopaedic surgeon must be prepared to deal with the high rate of intraoperative complications still encountered. Intraoperative complications are more frequent for uncemented than cemented THA.16,21 Almost all the intraoperative femoral fractures were reported using uncemented THA. The metaphyseal femoral morphology is typically distorted in SCD patients, characterized by thin trabeculae and cortices, medullary hyperplasia, low bone density but also patchy areas of bone sclerosis that can obliterate the femoral canal.15 The canal may be either occluded or hyperplastic, and the so-called ‘femur within femur’ that is frequently encountered is characterized by a thin femoral cortical lining inside the outer cortex.19 To facilitate the femoral reaming many surgeons introduce a 4.5 mm drill bit or a high-speed burr under image intensifier, preparing the femoral bone to accommodate flexible intramedullary guidewires and through them cannulated intramedullary reaming is performed.7,20 In case of fracture or femoral perforation, a longer stem17 and in extreme cases with narrowing of the femoral canal small-sized or even developmental dysplasia of the hip (DDH) short stems may be needed.7,15,20 A cylindrical distal geometry stem is reported to work well in the femora of SCD patients19 and the tapered stems to minimize the risk of femoral fracture.21
Fractures and perforations in the acetabulum are less reported; however, bone sclerosis may be a reason for eccentric acetabular reaming19 and higher position of the cup.19 The high incidence of protrusio acetabuli in SCD patients often requires medial bone grafting, an acetabular reinforcement ring or other structural support.16 Protrusio also challenges dislocation; an in situ femoral neck osteotomy may be needed to avoid complications during dislocation.7,13 The hip dislocation is also facilitated by the removal of osteophytes, extensile capsulotomy, adductor tenotomy and removal of adhesions between the head and acetabulum.15
Conclusion
THA for AVN in SCD is a complex primary THA carrying a high risk of medical, intraoperative and postoperative complications. However, recent diagnostic and therapeutic advances have optimized the medical care of SCD patients in addition to the improvement of surgical techniques and implants improving the outcomes in properly selected SCD patients. A multidisciplinary preoperative and intraoperative approach increases the likelihood of favourable results. Sickle cell crises and transfusion reactions are the most common postoperative medical complications. Perioperative adequate hydration, warming, oxygen supply, exclusion of infection sites and conservative transfusion protocols to keep the appropriate level of Hb are needed. The surgeon must be prepared to deal with a high rate of intraoperative complications. Femoral fractures and perforations are more frequently reported. The risk of intraoperative femoral fracture is higher for uncemented THA. Specialized care in the handling of compromised acetabular and femoral bone stock and quality can prevent complications. Different implant options such as short or long stems, revision options and plates for periprosthetic fractures must be present to deal with intraoperative complications. Infection and aseptic loosening are the principal reasons for the failure of THA in SCD. Aseptic loosening of the cup is more frequently recorded than that of the stem. Although cemented THAs have demonstrated a higher revision rate than uncemented implants, no definite conclusion can be made regarding the best fixation mode. This is mainly attributed to methodological issues of the studies and different follow-up times. Fully porous-coated implants are attractive options for this young group of patients; however, modern cemented implants may be equally effective. Further high-quality comparative studies are needed to evaluate the superiority of uncemented implants in this clinical setting. SCD patients must be adequately counselled preoperatively.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Osunkwo I. An update on the recent literature on sickle cell bone disease. Curr Opin Endocrinol Diabetes Obes 2013;20:539–546. [DOI] [PubMed] [Google Scholar]
- 2. Kenanidis E, Kakoulidis P, Lepetsos P, Potoupnis M, Tsiridis E. Sickle cell disease. In: Tsiridis E, ed. The adult hip: master case series and techniques. Springer, Cham, 2018:339–350. [Google Scholar]
- 3. Platt OS, Brambilla DJ, Rosse WF, et al. Mortality in sickle cell disease: life expectancy and risk factors for early death. N Engl J Med 1994;330:1639–1644. [DOI] [PubMed] [Google Scholar]
- 4. Rees DC, Williams TN, Gladwin MT. Sickle cell disease. Lancet 2010;376:2018–2031. [DOI] [PubMed] [Google Scholar]
- 5. Vanderhave KL, Perkins CA, Scannell B, Brighton BK. Orthopaedic manifestations of sickle cell disease. J Am Acad Orthop Surg 2018;26:94–101. [DOI] [PubMed] [Google Scholar]
- 6. Thomas R, Dulman R, Lewis A, Notarangelo B, Yang E. Prospective longitudinal follow-up of children with sickle cell disease treated with hydroxyurea since infancy. Pediatr Blood Cancer 2019;66:e27816. [DOI] [PubMed] [Google Scholar]
- 7. Gulati Y, Sharma M, Bharti B, Bahl V, Bohra I, Goswani A. Short term results of cementless total hip arthroplasty in sicklers. Indian J Orthop 2015;49:447–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kenanidis E, Kakoulidis P, Leonidou A, Tsiridis E. Osteonecrosis. In: Tsiridis E, ed. The adult hip: master case series and techniques. Springer, Cham, 2018:303–326. [Google Scholar]
- 9. Bishop AR, Roberson JR, Eckman JR, Fleming LL. Total hip arthroplasty in patients who have sickle-cell hemoglobinopathy. J Bone Joint Surg Am 1988;70:853–855. [PubMed] [Google Scholar]
- 10. Hanker GJ, Amstutz HC. Osteonecrosis of the hip in the sickle-cell diseases: treatment and complications. J Bone Joint Surg Am 1988;70:499–506. [PubMed] [Google Scholar]
- 11. Acurio MT, Friedman RJ. Hip arthroplasty in patients with sickle-cell haemoglobinopathy. J Bone Joint Surg Br 1992;74:367–371. [DOI] [PubMed] [Google Scholar]
- 12. Moran MC, Huo MH, Garvin KL, Pellicci PM, Salvati EA. Total hip arthroplasty in sickle cell hemoglobinopathy. Clin Orthop Relat Res 1993;294:140–148. [PubMed] [Google Scholar]
- 13. Hickman JM, Lachiewicz PF. Results and complications of total hip arthroplasties in patients with sickle-cell hemoglobinopathies: role of cementless components. J Arthroplasty 1997;12:420–425. [DOI] [PubMed] [Google Scholar]
- 14. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Al-Mousawi F, Malki A, Al-Aradi A, Al-Bagali M, Al-Sadadi A, Booz MM. Total hip replacement in sickle cell disease. Int Orthop 2002;26:157–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hernigou P, Zilber S, Filippini P, Mathieu G, Poignard A, Galacteros F. Total THA in adult osteonecrosis related to sickle cell disease. Clin Orthop Relat Res 2008; 466:300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Al Omran AS. Choice of implant in total hip arthroplasty for sickle cell disease patients. Eur Orthop Traumatol 2010;1:25–29. [Google Scholar]
- 18. Issa K, Naziri Q, Maheshwari AV, Rasquinha VJ, Delanois RE, Mont MA. Excellent results and minimal complications of total hip arthroplasty in sickle cell hemoglobinopathy at mid-term follow-up using cementless prosthetic components. J Arthroplasty 2013;28:1693–1698. [DOI] [PubMed] [Google Scholar]
- 19. Jack CM, Howard J, Aziz ES, Kesse-Adu R, Bankes MJ. Cementless total hip replacements in sickle cell disease. Hip Int 2016;26:186–192. [DOI] [PubMed] [Google Scholar]
- 20. Azam MQ, Sadat-Ali M. Quality of life in sickle cell patients after cementless total hip arthroplasty. J Arthroplasty 2016;31:2536–2541. [DOI] [PubMed] [Google Scholar]
- 21. Ilyas I, Alrumaih HA, Rabbani S. Non-cemented total hip arthroplasty in sickle-cell disease: long-term results. J Arthroplasty 2018;33:477–481. [DOI] [PubMed] [Google Scholar]
- 22. Farook MZ, Awogbade M, Somasundaram K, Reichert ILH, Li PLS. Total hip arthroplasty in osteonecrosis secondary to sickle cell disease. Int Orthop 2019; 43:293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Katchy AU, Anyaehie UE, Nwadinigwe CU, Eyichukwu GO. Total hip replacement in sickle cell disorder: a preliminary report of challenges and early outcome of 21 consecutive patients. Niger J Clin Pract 2018;21:492–495. [DOI] [PubMed] [Google Scholar]
- 24. Johannson HR, Zywiel MG, Marker DR, Jones LC, McGrath MS, Mont MA. Osteonecrosis is not a predictor of poor outcomes in primary total hip arthroplasty: a systematic literature review. Int Orthop 2011;35:465–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ilyas I, Moreau P. Simultaneous bilateral total hip arthroplasty in sickle cell disease. J Arthroplasty 2002;17:441–445. [DOI] [PubMed] [Google Scholar]
- 26. Perfetti DC, Boylan MR, Naziri Q, Khanuja HS, Urban WP. Does sickle cell disease increase risk of adverse outcomes following total hip and knee arthroplasty? A nationwide database study. J Arthroplasty 2015;30:547–551. [DOI] [PubMed] [Google Scholar]