Abstract
Background
Hip fractures are associated with 1-year mortality rates as high as 19% to 33%. Nonwhite patients have higher mortality and lower mobility rates at 6 months postoperatively than white patients. Studies have extensively documented racial disparities in hip fracture outcomes, but few have directly assessed racial disparities in the timing of hip fracture care.
Questions/purposes
Our purpose was to assess racial disparities in the care provided to patients with hip fractures. We asked, (1) do racial disparities exist in radiographic timing, surgical timing, length of hospital stay, and 30-day hospital readmission rates? (2) Does the hospital type modify the association between race and the outcomes of interest?
Methods
We retrospectively reviewed the records of 1535 patients aged 60 years or older who were admitted to the emergency department and treated surgically for a hip fracture at one of five hospitals (three community hospitals and two tertiary hospitals) in our health system from 2015 to 2017. Multivariable generalized linear models were used to assess associations between race and the outcomes of interest.
Results
After adjusting for patient characteristics, we found that black patients had a longer mean time to radiographic evaluation (4.2 hours; 95% confidence interval, -0.6 to 9.0 versus 1.2 hours; 95% CI, 0.1-2.3; p = 0.01) and surgical fixation (41 hours; 95% CI, 34-48 versus 34 hours 95% CI, 32-35; p < 0.05) than white patients did. Hospital type only modified the association between race and surgical timing. In community hospitals, black patients experienced a 51% (95% CI, 17%-95%; p < 0.01) longer time to surgery than white patients did; however, there were no differences in surgical timing between black and white patients in tertiary hospitals. No race-based differences were observed in the length of hospital stay and 30-day hospital readmission rates.
Conclusions
After adjusting for patient characteristics, we found that black patients experienced longer wait times to radiographic evaluation and surgical fixation than white patients. Hospitals should consider evaluating racial disparities in the timing of hip fracture care in their health systems. Raising awareness of these disparities and implementing unconscious bias training for healthcare providers may help mitigate these disparities and improve the timing of care for patients who are at a greater risk of delay.
Level of Evidence
Level III, therapeutic study.
Introduction
As the population ages, the annual number of hip fractures in the United States is expected to increase from 340,000 [13] to 840,000 [15] by 2040. Hip fractures are associated with substantial rates of morbidity [4, 18], and mortality rates after hip fracture have been reported to range from 3.5% to 10% at 30 days [6, 9] and from 19% to 33% at 1 year [30, 37]. Hip fractures are also expensive to treat, accounting for approximately 72% of total fracture costs but constituting only 14% of all fractures [5]. A recent study reported that the average direct annual medical cost associated with a hip fracture is more than USD 50,000, costing the United States healthcare system nearly USD 6 billion yearly [2]. Enhancing the delivery of hip fracture care can improve patient outcomes and reduce the economic burden of this condition [21].
Despite studies showing racial disparities in orthopaedic care [24, 27], a recent survey of members of the American Orthopaedic Association found that only 9% of orthopaedic surgeons believe that race or ethnicity influences the orthopaedic care patients receive [1]. One study reported that nonwhite patients with hip fractures have lower mobility rates and higher mortality rates at 6 months postoperatively than white patients do [28]. Dy et al. [12] assessed racial disparities in the care of patients with hip fractures, reporting that black patients were at a greater risk of death within 1 year and were more likely to be re-admitted to the hospital within 90 days and have delayed surgery than white patients were. Their findings were limited because they used administrative data, which are susceptible to inconsistent reporting and coding inaccuracies [19, 33]. To our knowledge, race-based differences in radiographic timing and length of hospital stay for patients with hip fractures have not been reported. Racial disparities in surgical timing and readmission rates have been examined, with conflicting results because of the quality and settings of the studies [12, 26, 32]. We therefore wished to assess racial disparities in the care provided to patients with hip fractures.
Specifically, we asked, (1) do racial disparities exist in radiographic timing, surgical timing, length of hospital stay, and 30-day hospital readmission rates? (2) Does the hospital type modify the association between race and the outcomes of interest?
Patients and Methods
Study Population
After obtaining a waiver of consent from our institutional review board, we performed a retrospective review and extracted patient information from our institution’s electronic medical record. We identified all patients aged 60 years or older who were admitted to the emergency department and treated surgically for a hip fracture at five hospitals in our health system from January 1, 2015 through December 31, 2017. We used the International Classification of Diseases, Tenth Revision, diagnosis codes and Current Procedural Terminology codes (27235, 27236, 27244, and 27245) to identify patients with operatively treated hip fractures.
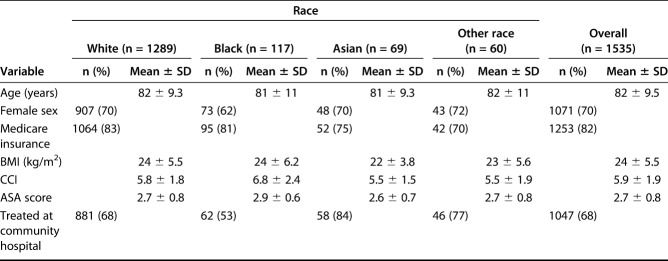
A total of 1535 patients (70% women) met our inclusion criteria (Table 1). Most patients were white (84%), followed by patients who were black (7.6%), Asian (4.5%), and other races (3.9%). Insurance status was categorized as Medicare (82%), private insurance (16%), Medicaid (0.7%), or other (1.9%). The “other” category included worker’s compensation, self-pay, and auto mobile insurance.
Table 1.
Characteristics of 1535 patients treated surgically for hip fractures at five hospitals, 2015 to 2017
Variables
Patient race was classified as white, black, Asian, or other race. Patients who identified as American Indian, Alaska Native, Native Hawaiian, other Pacific Islander, or other were all included in the other race category because of the small sizes of the individual groups. Data on ethnicity were unavailable. Each hospital was categorized as a community hospital (n = 3) or a tertiary hospital (n = 2). Hospitals were classified according to size and location. Community hospitals had fewer than 300 patient beds and were located in suburban areas, whereas tertiary hospitals had more than 300 patient beds and were located in urban areas. Hospital type was explored as an effect modifier between race and the outcomes of interest. We adjusted for the following potential confounders: age, sex, insurance status, BMI, Charlson comorbidity index (CCI) value, and American Society of Anesthesiologists (ASA) score.
Outcomes
The primary outcomes of interest were the time from rooming in the emergency department to the first radiograph of the hip (radiographic timing) and the time from rooming in the emergency department to surgery (surgical timing). Additional outcomes were the length of hospital stay and 30-day readmission rate.
Statistical Analysis
Generalized linear models were used to assess the association between race and the outcomes of interest, with adjustment for patient age, sex, insurance status, BMI, CCI, and ASA score. Insurance status was dichotomized as Medicare or other in the models. Normal distribution with log link and binomial distribution with logit link were used for continuous and binary outcomes, respectively. These models included within-patient robust variance estimates to account for repeated observations for a patient [31].
Potential effect modification by hospital type was explored by incorporating appropriate statistical interaction terms of race and hospital type in the multivariable models. Because of small sample sizes, only white and black patient groups were used in the effect modification analysis.
All tests were two-sided, and statistical significance was considered to be p < 0.05. Analyses were performed using Stata software, version 15 (StataCorp LLC, College Station, TX, USA).
Results
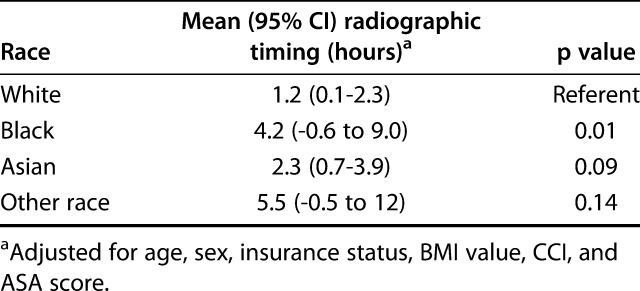
Radiographic Timing
The mean ± standard deviation of radiographic timing was 1.8 hours ± 6.9 hours. After adjusting for age, sex, insurance status, BMI, CCI, and ASA score, black patients waited, on average, 3.0 hours longer than white patients for their first hip radiograph (4.2 hours; 95% confidence interval, -0.6 to 9.0 versus 1.2 hours; 95% CI, 0.1-2.3; p = 0.01) (Table 2). Compared with a radiographic timing of less than 2 hours, a wait time of more than 4 hours was associated with a 57% increase in time to surgery (p < 0.01). Hospital type did not modify the difference in radiographic timing between white and black patients (effect size = 21.3; 95% CI, 0.01-34000; p = 0.42).
Table 2.
Associations between patient race and radiographic timing for 1535 patients treated surgically for hip fractures at five hospitals, 2015 to 2017
Surgical Timing
The mean ± SD surgical timing was 35 hours ± 34 hours. After adjustment for patient characteristics, black patients had a longer time to surgery (mean 41 hours; 95% CI, 34-48) than white patients did (mean 34 hours; 95% CI, 32-35; p = 0.045) (Table 3).
Table 3.
Associations between patient race and surgical timing for 1535 patients treated surgically for hip fractures at five hospitals, 2015 to 2017
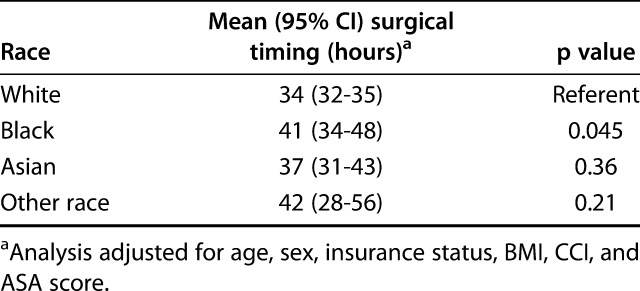
Hospital type modified the difference in surgical timing between white and black patients (95% CI, 1.08-2.41; effect size 1.62; p = 0.02 for interaction). In the adjusted analysis, black patients who were treated at community hospitals had a wait time to surgery that was 51% (95% CI, 17%-95%; p = 0.002) longer than that experienced by white patients. However, in tertiary hospitals, there was no association between race and surgical timing (ratio of means 1.07; 95% CI, 0.80-1.44; p = 0.65).
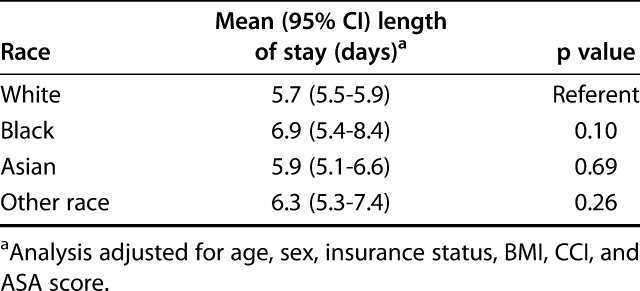
Length of Hospital Stay
The mean ± SD length of hospital stay was 5.9 days ± 4.2 days. No racial disparities in the length of hospital stay were observed (Table 4). Hospital type did not modify the difference in the length of hospital stay between white and black patients (effect size 1.02; 95% CI, 0.65-1.59; p = 0.95). Older age and higher BMI, CCI, and ASA score were associated with longer hospital stays.
Table 4.
Associations between patient race and length of hospital stay for 1535 patients treated surgically for hip fractures at five hospitals, 2015 to 2017
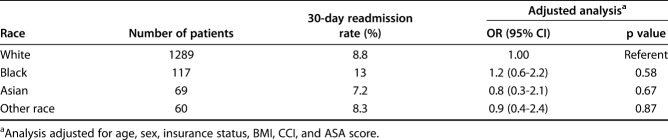
Thirty-day Hospital Readmissions
Overall, the 30-day readmission rate was 9.1%. We found no racial disparities in 30-day readmission rates (Table 5). Hospital type did not modify the association between race and the 30-day readmission rate (effect size 1.29; 95% CI, 0.36-4.63; p = 0.69). Male sex and higher CCI values were associated with a greater risk of 30-day readmission.
Table 5.
Odds and rates of 30-day hospital readmission by patient race for 1535 patients treated surgically for hip fractures at five hospitals, 2015 to 2017
Discussion
Few studies have directly assessed racial disparities in hip fracture care. The studies that have examined these disparities reported inconsistent results because of differences in the quality of data and study setting. We used clinical data from five hospitals in our health system to determine whether patient race is associated with radiographic timing, surgical timing, length of hospital stay, and 30-day hospital readmission rates. We also wanted to determine whether the hospital type modified the association between race and the outcomes of interest.
Limitations
Our study has several limitations in addition those that generally apply to retrospective studies. The results from this study are based on one health system and are not generalizable to other locations. In addition, we were unable to include ethnicity in our analysis. Similarly, we could not conduct analyses of individual racial groups (for example, American Indian or Alaska Native) because of small sample sizes. Additionally, because of the limited sample sizes of racial groups other than black and white, modification of hospital type was not analyzed, and some conclusions are limited for these groups. Although we had small sample sizes for nonwhite racial groups, our study was more representative of the racial diversity of the United States population than previous studies were [12, 26] (the Unites States population is 76.5% white, 13.4% black, and 5.9% Asian) [35]. We made our selection criteria as inclusive as possible and adjusted for various patient factors in our analysis to minimize selection bias. We also used objective outcome measures to limit concerns of assessment bias.
Another potential limitation is the lack of data on the time between injury and presentation to the emergency department. This could have affected the assessment of acuity and consequently the timing of radiographic assessment, but it is unclear what effect this would have on our analysis because, to our knowledge, racial disparities in seeking care for acute injuries have not been described. Moreover, we examined only two patient outcomes: length of hospital stay and the 30-day hospital readmission rate. Ideally, we would have examined outcomes such as postoperative death and complication rates and determined whether disparities in the timing of care were associated with poorer outcomes based on these measures. Finally, we were unable to document readmissions to hospitals outside our system. This may have caused us to underestimate the 30-day readmission rate, but we are unsure about the effect this underestimation may have on our analysis.
Racial Disparities in Key Metrics of Treatment
Racial disparities in emergency department wait times have been reported. Nonwhite [34] and black [3] patients who presented to the emergency department with chest pain waited longer than white patients did to undergo initial electrocardiography. Similarly, black patients with acute ischemic stroke waited longer in the emergency department than white patients did to undergo initial CT [17]. After adjustment for patient characteristics, we found that black patients experienced longer time to radiographic assessment than did white patients. The longer time to radiography experienced by black patients may be attributable to conscious or unconscious biases of healthcare professionals, which may be heightened in the emergency department setting [23, 38]. Addressing this disparity is important because we found that patients who waited more than 4 hours for a radiographic evaluation also waited longer for surgical treatment than did patients who waited less than 2 hours for a radiographic assessment. Extensive research has reported the association between longer surgery delays and worse hip fracture outcomes [11, 14, 22, 29, 36].
Several studies have examined the association between patient race and delayed surgical treatment of hip fractures. Dy et al. [12] used administrative data to retrospectively review nearly 200,000 patients who had hip fracture surgery in New York State between 1998 and 2010. After adjusting for patient characteristics, they reported that black patients had greater odds (odds ratio 1.49; 95% CI, 1.42-1.57) of delayed surgery (defined as more than 48 hours after presentation) than did white patients. Similarly, Ryan et al. [32] analyzed data from more than 2.1 million patients who underwent surgery for hip fractures and found that black patients had greater odds (odds ratio 1.48; 95% CI, 1.39-1.58) of experiencing surgery delays than did white patients. Similarly, our adjusted analysis showed that black patients waited longer for surgery (41 hours) than did white patients (34 hours). In contrast, Okike et al. [26] analyzed data from the Kaiser Permanente Hip Fracture Registry and found no differences in surgery delays between black patients and white patients. The authors attributed the lack of racial disparities to the implementation of standardized protocols by their health system. Although the acceptable waiting time for surgery is debated, a high-quality study found that 24 hours is a threshold above which patients have a higher risk of complications and death [29]. To our knowledge, our study is the first to explore race-based differences in the length of hospital stay for patients with hip fractures. We did not find race-based differences in the length of hospital stay. Surgery within 24 hours has been shown to be associated with a shorter length of stay [36], and none of the racial groups we analyzed had a mean surgery wait time of less than 24 hours. Larger multi-system studies are needed to further explore the presence of racial disparities in the length of hospital stay. Shorter hospital stays not only reduce healthcare costs [20] but are also associated with lower 30-day mortality rates for patients with hip fractures [25].
The 30-day readmission rate is a metric used by the Centers for Medicare & Medicaid Services to assess the quality of care [7]. We found that nonwhite patients had similar rates of 30-day readmission to white patients. Dy et al. [12] and Okike et al. [26] found that black and Asian patients had higher and lower rates, respectively, of 90-day readmission than did white patients. However, 30-day readmissions might be a more accurate measure of quality of hospital care than 90-day readmissions because community- and household-level factors beyond the hospital’s control are associated with higher rates of readmission after the seventh day of discharge [8].
Association Between Hospital Type and Surgical Timing
The hospital types we studied differed in terms of racial disparities in surgical timing. At our three community hospitals, black patients experienced longer wait times for surgery than did white patients. At our two tertiary hospitals, black and white patients experienced similar wait times for surgical fixation of their hip fracture. This difference based on hospital type may be attributable to residential racial segregation, which has resulted in a differential race composition of the patient population treated at tertiary and community hospitals [39]. We found that black patients comprised 11.3% of patients treated at tertiary hospitals but only 5.9% of patients treated at community hospitals. In a previous study, black people living in predominantly white residential areas reported facing higher levels of discrimination than did black people living in predominantly black residential areas [16]. Our three community hospitals are located in suburban areas where black residents constitute only 5% [10], 20%, and 20% [35] of the population. In contrast, our two tertiary hospitals are located in a city where black residents constitute 63% of the population [35].
Conclusions
After adjusting for patient characteristics, we found that black patients experienced longer wait times to radiographic evaluation and surgical fixation of hip fractures than white patients. Although these disparities in care did not translate to poorer outcomes in terms of length of hospital stay or 30-day hospital readmission rates, it is crucial to address disparities in the timing of care and ensure equitable treatment, regardless of race. Raising awareness of these disparities in the care of hip fractures, especially among orthopaedic surgeons, is imperative because only a small percentage of orthopaedic surgeons perceive that patient race influences orthopaedic care [1]. Furthermore, hospitals should consider evaluating their own time to radiographic assessment and surgical fixation to determine whether racial disparities exist in their health systems. Healthcare institutions can play an active role in mitigating healthcare disparities by facilitating discussions and training sessions for clinicians to promote bias literacy and by considering the implementation of standard pathways.
Acknowledgements
We thank the Johns Hopkins Institute for Clinical and Translational Research for providing statistical support to the study. The Institute for Clinical and Translational Research is funded in part by Grant Number UL1TR001079 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health, and National Institutes of Health Roadmap for Medical Research. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official view of the Institute for Clinical and Translational Research, National Center for Advancing Translational Sciences, or National Institutes of Health.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Johns Hopkins University, Baltimore, MD, USA.
References
- 1.Adelani MA, O'Connor MI. Perspectives of orthopedic surgeons on racial/ethnic disparities in care. J Racial Ethn Health Disparities. 2017;4:758-762. [DOI] [PubMed] [Google Scholar]
- 2.Adeyemi A, Delhougne G. Incidence and economic burden of intertrochanteric fracture: a Medicare claims database analysis. JB JS Open Access. 2019;4:e0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bell PD, Hudson S. Equity in the diagnosis of chest pain: race and gender. Am J Health Behav. 2001;25:60-71. [DOI] [PubMed] [Google Scholar]
- 4.Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51:364-370. [DOI] [PubMed] [Google Scholar]
- 5.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475. [DOI] [PubMed] [Google Scholar]
- 6.Carretta E, Bochicchio V, Rucci P, Fabbri G, Laus M, Fantini MP. Hip fracture: effectiveness of early surgery to prevent 30-day mortality. Int Orthop. 2011;35:419-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Medicare and Medicaid Services. Hospital Readmissions Reduction Program (HRPP). Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed August 4, 2014.
- 8.Chin DL, Bang H, Manickam RN, Romano PS. Rethinking thirty-day hospital readmissions: shorter intervals might be better indicators of quality of care. Health Aff (Millwood). 2016;35:1867-1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daugaard CL, Jorgensen HL, Riis T, Lauritzen JB, Duus BR, van der Mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012;83:609-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.District of Columbia Office of Planning. Population. Available at: https://planning.dc.gov/page/population. Accessed April 22, 2019.
- 11.Doruk H, Mas MR, Yildiz C, Sonmez A, Kyrdemir V. The effect of the timing of hip fracture surgery on the activity of daily living and mortality in elderly. Arch Gerontol Geriatr. 2004;39:179-185. [DOI] [PubMed] [Google Scholar]
- 12.Dy CJ, Lane JM, Pan TJ, Parks ML, Lyman S. Racial and socioeconomic disparities in hip fracture care. J Bone Joint Surg Am. 2016;98:858-865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friedman SM, Mendelson DA. Epidemiology of fragility fractures. Clin Geriatr Med. 2014;30:175-181. [DOI] [PubMed] [Google Scholar]
- 14.Fu MC, Boddapati V, Gausden EB, Samuel AM, Russell LA, Lane JM. Surgery for a fracture of the hip within 24 hours of admission is independently associated with reduced short-term post-operative complications. Bone Joint J. 2017;99:1216-1222. [DOI] [PubMed] [Google Scholar]
- 15.Graves EJ, Owings MF. 1996 summary: National Hospital Discharge Survey. Adv Data. 1998;1-12. [PubMed] [Google Scholar]
- 16.Harvard T. H. Chan School of Public Health. Discrimination in America: experiences and views of African Americans (October 2017). Available at: https://www.npr.org/assets/img/2017/10/23/discriminationpoll-african-americans.pdf. Accessed May 23, 2019.
- 17.Jacobs BS, Birbeck G, Mullard AJ, Hickenbottom S, Kothari R, Roberts S, Reeves MJ. Quality of hospital care in African American and white patients with ischemic stroke and TIA. Neurology. 2006;66:809-814. [DOI] [PubMed] [Google Scholar]
- 18.Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15:897-902. [DOI] [PubMed] [Google Scholar]
- 19.Khwaja HA, Syed H, Cranston DW. Coding errors: a comparative analysis of hospital and prospectively collected departmental data. BJU Int. 2002;89:178-180. [DOI] [PubMed] [Google Scholar]
- 20.Lott A, Haglin J, Belayneh R, Konda SR, Egol KA. Admitting service affects cost and length of stay of hip fracture patients. Geriatr Orthop Surg Rehabil. 2018;9:2151459318808845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Middleton M, Wan B, da Assuncao R. Improving hip fracture outcomes with integrated orthogeriatric care: a comparison between two accepted orthogeriatric models. Age Ageing. 2017;46:465-470. [DOI] [PubMed] [Google Scholar]
- 22.Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87:483-489. [DOI] [PubMed] [Google Scholar]
- 23.Muroff JR, Jackson JS, Mowbray CT, Himle JA. The influence of gender, patient volume and time on clinical diagnostic decision making in psychiatric emergency services. Gen Hosp Psychiatry. 2007;29:481-488. [DOI] [PubMed] [Google Scholar]
- 24.Nelson CL. Disparities in orthopaedic surgical intervention. J Am Acad Orthop Surg. 2007;15:S13-S17. [DOI] [PubMed] [Google Scholar]
- 25.Nikkel LE, Kates SL, Schreck M, Maceroli M, Mahmood B, Elfar JC. Length of hospital stay after hip fracture and risk of early mortality after discharge in New York state: retrospective cohort study. BMJ. 2015;351:h6246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Okike K, Chan PH, Prentice HA, Paxton EW, Navarro RA. Association between race and ethnicity and hip fracture outcomes in a universally insured population. J Bone Joint Surg Am. 2018;100:1126-1131. [DOI] [PubMed] [Google Scholar]
- 27.Pandya NK, Wustrack R, Metz L, Ward D. Current concepts in orthopaedic care disparities. J Am Acad Orthop Surg. 2018;26:823-832. [DOI] [PubMed] [Google Scholar]
- 28.Penrod JD, Litke A, Hawkes WG, Magaziner J, Doucette JT, Koval KJ, Silberzweig SB, Egol KA, Siu AL. The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci. 2008;63:867-872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens AB, Kreder HJ, Jenkinson RJ, Wodchis WP. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318:1994-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rogers W. Regression standard errors in clustered samples. Stata Technical Bulletin. 1994;3:19-23. [Google Scholar]
- 32.Ryan DJ, Yoshihara H, Yoneoka D, Egol KA, Zuckerman JD. Delay in hip fracture surgery: an analysis of patient-specific and hospital-specific risk factors. J Orthop Trauma. 2015;29:343-348. [DOI] [PubMed] [Google Scholar]
- 33.Southern DA, Roberts B, Edwards A, Dean S, Norton P, Svenson LW, Larsen E, Sargious P, Lau DC, Ghali WA. Validity of administrative data claim-based methods for identifying individuals with diabetes at a population level. Can J Public Health. 2010;101:61-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takakuwa KM, Shofer FS, Hollander JE. The influence of race and gender on time to initial electrocardiogram for patients with chest pain. Acad Emerg Med. 2006;13:867-872. [DOI] [PubMed] [Google Scholar]
- 35.United States Census Bureau. QuickFacts: United States. Available at: https://www.census.gov/quickfacts/fact/table/US/PST045218. Accessed April 22, 2019.
- 36.Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44:726-729. [DOI] [PubMed] [Google Scholar]
- 37.Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53:1476-1482. [DOI] [PubMed] [Google Scholar]
- 38.Wigboldus DH, Sherman JW, Franzese HL, van Knippenberg A. Capacity and comprehension: spontaneous stereotyping under cognitive load. Soc Cogn. 2004;22:292-309. [Google Scholar]
- 39.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404-416. [DOI] [PMC free article] [PubMed] [Google Scholar]