Abstract
Background
Delayed time to surgery of at least 2 days after hospital arrival is well known to be associated with increased complications after standard hip fracture surgery; whether this association is present for pathologic hip fractures, however, is unknown.
Questions/purposes
(1) After controlling for differences in patient characteristics, is delayed time to surgery (at least 2 days) for patients with pathologic hip fractures independently associated with increased complications compared with early surgery (fewer than 2 days)? (2) What preoperative factors are independently associated with major complications and mortality after surgery for pathologic hip fractures?
Methods
A retrospective study was conducted using the American College of Surgeons National Surgical Quality Improvement Program database of pathologic hip fractures (including femoral neck, trochanteric, and subtrochanteric fractures) from 2007 to 2017. This database was chosen over other databases given the high-quality preoperative medical history and postoperative complication (including readmissions, reoperations, and mortality) data collected from patient medical records through the thirtieth postoperative day. Patients were identified using Common Procedural Terminology codes for hip fracture treatment (THA, hemiarthroplasty, proximal femur replacement, intramedullary nail, and plate and screw fixation) with associated operative diagnoses for pathologic fractures as identified with International Classification of Diseases codes. A total of 2627 patients with pathologic hip fractures were included in this study; 65% (1714) had surgery within 2 days and 35% (913) had surgery after that time. Patient demographics, hospitalization information, and 30-day postoperative complications were recorded. Differences in characteristics between patients who underwent surgery in the early and delayed time periods were assessed with chi-square tests for categorical variables and t-tests for continuous variables. Delayed-surgery patients were more medically complex at the time of admission than early-surgery patients, including having higher American Society of Anesthesiologists classification (mean ± SD 3.18 ± 0.61 versus 2.94 ± 0.60; p < 0.001) and prevalence of advanced, “disseminated” cancer (53% versus 39%; p < 0.001). Propensity-adjusted multivariable logistic regression analyses were performed to assess the effect of delayed time to surgery alone on the various outcome measures. Additional independent risk factors for major complications and mortality were identified using backwards stepwise regressions.
Results
After controlling for baseline factors, the only outcome associated with delayed surgery was extended postoperative length of stay (odds ratio 1.94 [95% CI 1.62 to 2.33]; p < 0.001). Delayed surgery was not associated with any postoperative complications, including major complications (OR 1.23 [95% CI 0.94 to 1.6]; p = 0.13), pulmonary complications (OR 1.24 [95% CI 0.83 to 1.86]; p = 0.29), and mortality (OR 1.26 [95% CI 0.91 to 1.76]; p = 0.16). Histories of chronic obstructive pulmonary disease (OR 2.48), congestive heart failure (OR 2.64), and disseminated cancer (OR 1.68) were associated with an increased risk of major complications, while dependent functional status (OR 2.27), advanced American Society of Anesthesiologists class (IV+ versus I-II, OR 4.81), and disseminated cancer were associated with an increased risk of mortality (OR 2.2; p ≤ 0.002 for all).
Conclusions
After controlling for baseline patient factors, delayed time to surgery was not independently associated with increased 30-day complications after surgical treatment of pathologic hip fractures. These results are in contrast to the traditional dogma for standard hip fractures that surgery within 2 days of hospital arrival is associated with reduced complications. Although surgery should not be delayed needlessly, if the surgeon feels that additional time could benefit the patient, the results of this study suggest surgeons should not expedite surgery because of the risk of surgical delay observed for standard hip fractures.
Level of Evidence
Level III, therapeutic study.
Introduction
Metastatic disease remains one of the largest unsolved problems in cancer biology [17], and bone is the third most frequent location of metastases behind the lung and liver [6]. Bone metastases can lead to several complications, including bone pain, hypercalcemia, epidural spinal cord compression, and cancer cachexia [20]. In addition, most bone metastases are osteolytic or mixed, which places patients at a substantial risk of having pathologic fractures [6, 8]. One of the most common locations for pathologic fractures is the hip, where approximately 10% of all cancer patients have metastatic lesions [8]. When pathologic hip fractures occur, they are best treated using a multidisciplinary approach including primary medical doctors, medical oncologists, radiation oncologists, orthopaedic oncologists and/or orthopaedic trauma surgeons, and the patient and his or her family. With an estimated 1-year survival rate of 30% after operative treatment [9, 23], time before surgery must be dedicated to creating a treatment plan in line with a patient’s goals of care. Surgical treatment may be further delayed by the need for medical management, surgical planning, additional imaging to assess for further metastatic burden, potential biopsy, vascular embolization for renal cell carcinoma, or transfer to a tertiary care center with a dedicated orthopaedic oncology team [8, 10].
Although surgical treatment is employed for most pathologic hip fractures [1, 8, 9], little is known about perioperative factors associated with operative success in this setting. In contrast, for standard hip fractures, it is well known that surgery at least 2 days after hospital arrival is associated with increased risk of complications and death [7, 13, 15, 16]. On the other hand, Bovonratwet et al. [5] and Sellan et al. [14] recently demonstrated that surgery within 2 days of hospital arrival was not associated with reduced complications or death for patients with periprosthetic hip fractures, raising questions about whether the time-to-surgery effect seen in standard hip fractures is generalizable to other complex hip fractures in which surgical delay could theoretically provide benefit. To our knowledge, no study has evaluated the association between time to surgery and complications in patients with pathologic hip fractures.
Therefore, we asked, (1) after controlling for differences in patient characteristics, is delayed time to surgery (at least 2 days) for patients with pathologic hip fractures independently associated with increased complications or mortality compared with early surgery (fewer than 2 days)? (2) What preoperative factors are independently associated with major complications and mortality after surgery for pathologic hip fractures?
Patients and Methods
We conducted a retrospective study using the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database from 2007 to 2017 to identify patients who underwent surgical management of pathologic hip fractures, which included femoral neck, trochanteric, and subtrochanteric fractures from tumors. The benefit of using a database to study surgery for pathologic hip fractures stems from the rarity of this intervention, often making individual hospital or even multicenter studies too small to provide meaningful conclusions. The NSQIP database, a convenience sample containing data from more than 700 hospitals participating in the American College of Surgeon’s NSQIP as of 2017, was chosen for the study of pathologic hip fractures for several reasons. First, it has a large sample size of surgical procedures, each with more than 200 highly granular preoperative, intraoperative, and postoperative variables. The large sample helps capture relatively rare events, while detailed variables allow for accurate risk stratification in analyses that could be subject to confounding, such as this one. The NSQIP database also provides highly accurate Common Procedural Terminology (CPT) coding, which allows for greater specificity than databases that only have International Classification of Diseases (ICD) procedure codes (for example, ICD procedure codes only localize to the femur for open reduction internal fixation and do not specify plate and screw fixation or intramedullary nailing). Next, the database is longitudinally maintained by trained medical reviewers directly from patient charts starting at the time of admission through 30 days postoperatively. The high-quality data collected directly from patient records is a key strength of the NSQIP database compared with other administrative claims databases that rely on billing codes [4, 7]. Moreover, the availability of data on 30-day complications was a strong determinant over other databases because short-term complication rates are particularly important for oncology patients, who may have limited life expectancy. Finally, the NSQIP database has been used successfully in prior studies on time to surgery for patients with standard [7] and periprosthetic [5] hip fractures, as well as for studies on pathologic femur fractures [11, 22].
Carefully adapting the recent protocol of McLynn et al. [11] and Fu et al. [7], we identified pathologic hip fractures using ICD 9th or 10th Edition revision codes for pathologic fractures (733.1X and M84.4X/5X, respectively) that were surgically treated with endoprosthestic reconstruction (CPT codes: THA, 27130; hip hemiarthroplasty, 27125 and 27236; or proximal femur replacement, any of the prior codes), hip fracture fixation with a plate and screw construct (CPT code: 27244), or hip fracture fixation with an intramedullary implant (CPT code: 27245), yielding 2846 patients. Consistent with a previous report examining the time to surgery using the NSQIP database [5], we excluded patients with missing key preoperative or procedural characteristics (n = 179), preoperative sepsis (n = 21), preoperative pneumonia (n = 4), or preoperative acute renal failure (n = 15) for a final sample of 2627 patients. The less than 10% incidence of missing data is unlikely to influence our results [3]. Of the 2627 study patients, 65% (1714) had surgery within 2 days of hospital arrival (early) and 35% (913) had surgery at least 2 days after arrival (delayed).
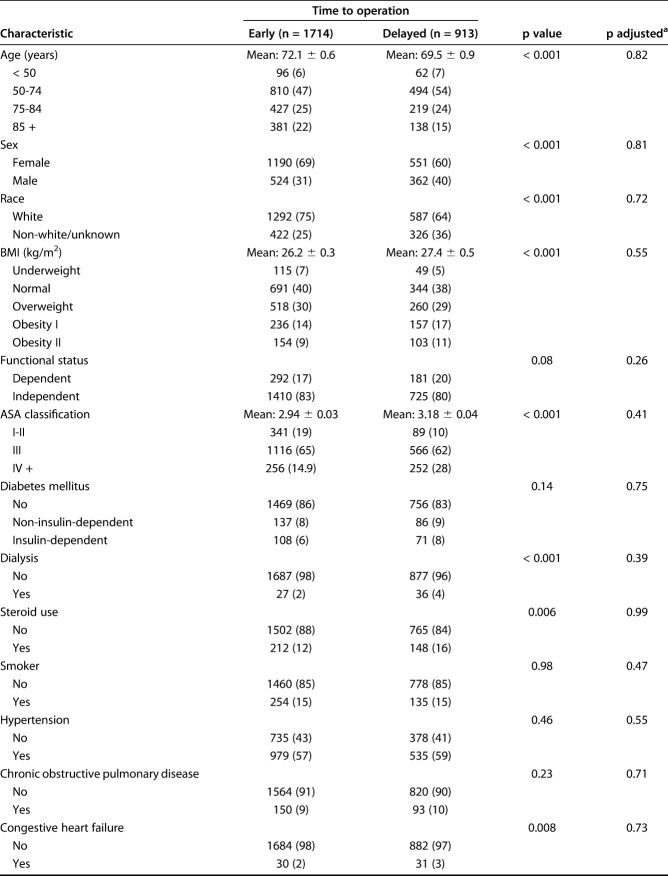
Baseline patient characteristics were sex, age, race (white or other/unknown), BMI (calculated from height and weight), chronic steroid use, smoking status, functional status at the time of surgery (independent or dependent), American Society of Anesthesiologists classification, history of diabetes, dialysis, chronic obstructive pulmonary disease, hypertension, use of anticoagulation or other bleeding disorder, congestive heart failure, and disseminated cancer (major metastatic spread with multi-organ involvement causing physiologic compromise; this variable does not include all cancer patients, and most patients undergoing cancer surgery do not meet this definition) [11, 12, 18, 21]. Operative information included the procedure performed, year of surgery, anesthesia type, operative time, time from hospital arrival to surgery, and postoperative length of stay (Table 1).
Table 1.
Baseline characteristics of patients undergoing early and delayed surgery
Major complications were defined as cardiac complications (cardiac arrest or myocardial infarction), sepsis or septic shock, wound complications (wound dehiscence, superficial surgical site infection, deep surgical site infection, or organ-space surgical site infection), thromboembolic complications (deep vein thrombosis treated with anticoagulation or pulmonary embolism), respiratory complications (pneumonia, on a ventilator for more than 2 days, or unplanned intubation), and renal complications (renal insufficiency or renal failure), similar to prior work [5, 7]. Other measures included 30-day urinary tract infections, transfusions, readmissions (available for patients from 2011 onwards), reoperations, and mortality. Extended postoperative length of stay was defined as the 75th percentile, or 6 days, in this study and another [5]. This study was deemed exempt by our institutional review board.
Statistical Analyses
Differences in baseline patient and procedural characteristics between patients undergoing early (less than 2 days after hospital arrival) and delayed (at least 2 days after admission) surgery were assessed with chi-square tests for categorical variables and t-tests for continuous variables. Delayed-surgery patients were more medically complex at the time of admission than early-surgery patients, including having higher American Society of Anesthesiologists classification (mean ± standard deviation 3.18 ± 0.61 versus 2.94 ± 0.60; p < 0.001) and prevalence of advanced, “disseminated” cancer (53% versus 39%; p < 0.001), among other factors (Table 1). To account for these baseline confounders, propensity adjustment was implemented, controlling for all covariates that were significant to p < 0.05 in the bivariate analysis of baseline characteristics. Propensity scores were defined as the patient’s conditional probability of being in the early or delayed surgery group given the patient’s other covariates [2]. After this procedure, propensity-adjusted p values were calculated, revealing no difference in any of these critical factors between groups.
Propensity-adjusted logistic regressions were then performed to assess the independent association between time to surgery and the various outcome measures in this study. Per the Bonferroni correction for multiple hypothesis testing, significance was set at p < 0.004. For measures in which delayed time to surgery was independently associated with greater complications, we performed a backwards stepwise multivariable logistic regression analysis to identify other independent risk factors (significance threshold of retention set at p < 0.004). This analysis allowed for a comparison of the relative effect size of delayed surgery on poorer outcomes compared with other independent risk factors [5, 7]. Finally, we repeated this procedure to determine baseline factors independently associated with major complications and mortality.
To ensure the robustness of our results, we performed a variety of sensitivity analyses. First, to assess the reliability of our time threshold, we repeated all analyses, with early surgery defined as less than 1 day and less than 3 days, instead of less than 2 days, as well as with time to surgery presented as a continuous variable (see Supplemental Digital Content 1, http://links.lww.com/CORR/A257). Next, given three highly-cited meta-analyses finding that delayed surgery was associated specifically with increased mortality for patients with standard hip fractures [13, 15, 16], the propensity-adjusted regression analyses for mortality were repeated while only controlling for the three covariates most strongly associated with mortality (see Supplemental Digital Content 2, http://links.lww.com/CORR/A258). Third, given that delayed time to surgery was associated with increased pulmonary complications in the NSQIP database for standard hip fractures [7], a propensity-adjusted regression analysis for pulmonary complications was performed, controlling for the same factors as in the previous study (see Supplemental Digital Content 3, http://links.lww.com/CORR/A259). Finally, we performed a post-hoc sensitivity analysis of septic complications, excluding patients who met the criteria for systemic inflammatory response syndrome preoperatively (patients with preoperative sepsis were already excluded) (see Supplemental Digital Content 4, http://links.lww.com/CORR/A260). All analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Association Between Time to Surgery and Complications
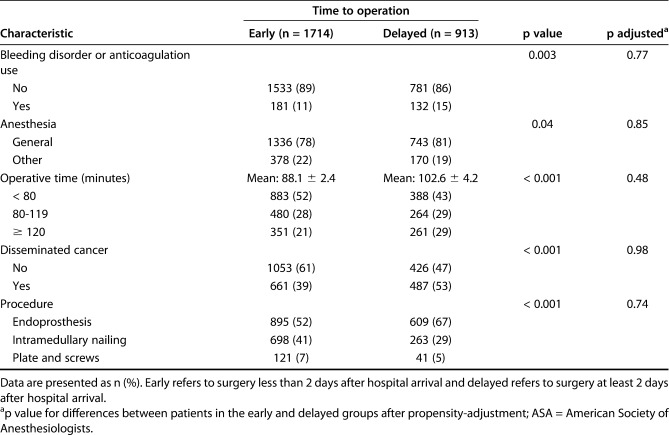
After controlling for differences in patient demographics and comorbidities between the early and delayed patients, we found that extended postoperative length of stay (odds ratio 1.94; 95% CI, 1.62-2.33; p < 0.001) was the only metric evaluated to be associated with delayed surgery (Table 2). There was no association between delayed time to surgery and any postoperative complications, including major complications (OR 1.23; 95% CI, 0.94-1.6; p = 0.13), pulmonary complications (OR 1.24; 95% CI, 0.83-1.86; p = 0.29), and mortality (OR 1.26; 95% CI, 0.91-1.76; p = 0.16). Similar results were observed when early surgery was defined as less than 1 day (see Supplemental Digital Content 1, http://links.lww.com/CORR/A257) or less than 3 days (see Supplemental Digital Content 5, http://links.lww.com/CORR/A261) as well as when time to surgery was evaluated as a continuous variable (see Supplemental Digital Content 6, http://links.lww.com/CORR/A262). Additional sensitivity analyses assessing mortality (see Supplemental Digital Content 2, http://links.lww.com/CORR/A258), pulmonary complications (see Supplemental Digital Content 3, http://links.lww.com/CORR/A259), and septic complications (see Supplemental Digital Content 4, http://links.lww.com/CORR/A260) also demonstrated similar results to the primary analysis, with no association between delayed time to surgery and the respective complications.
Table 2.
Propensity-adjusted multivariable logistic regression analysis for complications in patients undergoing delayed versus early surgery
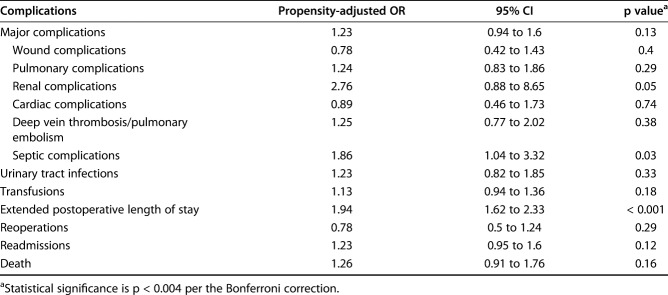
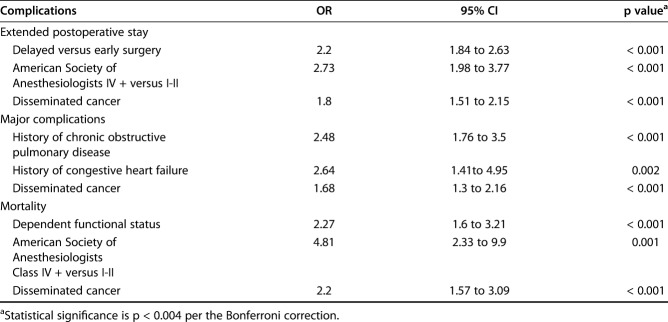
Independent Risk Factors of Complications and Mortality
Independent factors associated with an extended postoperative length of stay were delayed time to surgery (OR 2.20 [95% CI 1.84 to 2.63]; p < 0.001), American Society of Anesthesiologists Class IV + compared with Classes I and II (OR 2.73 [95% CI 1.98 to 3.77]; p < 0.001), and disseminated cancer (OR 1.80 [95% CI 1.51 to 2.15]; p < 0.001) (Table 3). Independent factors associated with major complications were a history of chronic obstruction pulmonary disease (OR 2.48 [95% CI 1.76 to 3.50]; p < 0.001), history of congestive heart failure (OR 2.64 [95% CI 1.41 to 4.95]; p = 0.002), and disseminated cancer (OR 1.68 [95% CI 1.30 to 2.16]; p < 0.001). Finally, dependent functional status (OR 2.27 [95% CI 1.60 to 3.21]; p < 0.001), American Society of Anesthesiologists Class IV + compared with Classes I and II (OR 4.81 [95% CI 2.33 to 9.90]; p = 0.001), and the presence of disseminated cancer (OR 2.20 [95% CI 1.57 to 3.09]; p < 0.001) were independently associated with an increased risk of 30-day mortality.
Table 3.
Factors independently associated with selected outcomes
Discussion
Many studies have explored the association between time to surgery and the outcomes of surgical treatment of standard hip fractures, generally finding that surgery within 2 days of hospital arrival is associated with reduced short-term and long-term complications [7, 13, 15, 16]. However, to our knowledge, these findings have never been explored in patients with pathologic hip fractures. In this large study of 2627 patients with pathologic hip fractures, we found that surgery performed within 2 days of hospital arrival was not associated with a reduction in any postoperative complication. The only difference between early and delayed surgery in this study was an increased risk of extended postoperative length of stay for patients with delayed surgery. Given the complex and interdisciplinary decision making that is often necessary for patients with pathologic hip fractures, these results have an important implication for the management of these fractures.
This study has several limitations. First, information on the type of surgery and fracture type was limited to information available in ICD and CPT codes. This study focused on the surgical treatment of acute pathologic hip fractures that may have been treated with earlier operative intervention; thus, CPT codes for prophylactic treatment of impending pathologic fractures were intentionally excluded. Similarly, ICD diagnosis codes for neoplasms were excluded, which are the indicated diagnosis codes in patients undergoing prophylactic treatment. Second, the reason for surgical delay could not be assessed from the NSQIP database; therefore, we could not quantify if (or how) surgical delay was beneficial for certain patients with delayed surgery (for example, offsetting some of the risk of delay seen for patients with standard hip fractures). Alternatively, the lack of an adverse effect associated with surgical delay could be because patients with pathologic fractures were younger on average than those with standard hip fractures. Hospitals are anonymized in the NSQIP database; thus, hospital-specific reasons for delay could not be assessed. Next, no information on the time from fracture diagnosis to hospital arrival, the type of primary malignancy, or long-term cancer-specific outcomes was available in the NSQIP database. The definition of “disseminated cancer” in the NSQIP database is not necessarily linked to any known clinical outcomes (for example, tumor grade and stage); therefore, it is difficult to ascertain its clinical importance [11, 21]. Although we did not identify any complications that were independently associated with delayed surgery, it is possible that with a larger sample such associations could have been identified. This study had a very large sample size, however, which suggests any undetected effects would be due to a very low effect size or extremely rare events. Additionally, not only were there a large number of events in both groups for the complications most strongly associated with delayed time to surgery for standard hip fractures (for example, 30-day mortality [13, 15, 16] and pulmonary complications [7]), but also specific sensitivity analyses further increased the robustness of these results. For valid statistical analyses with sufficient numbers of events, similar complications (for example, pulmonary embolism and deep vein thrombosis leading to anticoagulation) were grouped together [5, 7]. However, even with grouping, renal complications were extremely rare (13 total) making accurate propensity adjustment invalid; these results should be interpreted with caution. These limitations were offset to some degree by our use of the NSQIP database, which is an excellent source to use in the study of complications after surgery for pathologic hip fractures given its large sample size and its provision of outcome measures through the first 30 days, which may be especially important for oncology patients, whose life expectancy could be limited.
Our finding that delayed time to surgery is not independently associated with an increased risk of 30-day postoperative complications among patients with pathologic fractures parallels findings in other studies on periprosthetic hip fractures [5, 14]. In a retrospective analysis of the NSQIP database [5], time to surgery for periprosthetic hip fractures was not associated with 30-day postoperative complications other than longer postoperative hospital length of stay, which was also the only significant result in this study. As previously mentioned, this is in contrast to similar retrospective studies about standard hip fractures, which demonstrated that an earlier time to surgery was associated with reduced short-term postoperative complications [7, 13, 15, 16]. For example, in a recent retrospective analysis of NSQIP data, Fu et al. [7] demonstrated that time to surgery within 1 day for standard hip fractures was associated with an lower odds of pulmonary complications—including pneumonia, failure to extubate, or reintubation—and extended hospital length of stay. A meta-analysis of more than 250,000 patients [15] demonstrated that surgical delay for at least 2 days was associated with increased 30-day and 1-year all-cause mortality. Other meta-analyses have shown similar increases in mortality and postoperative complications [13, 16].
Although the time to surgery was not independently associated with complications in this study, we found several factors that were. Namely, a history of chronic obstructive pulmonary disease, congestive heart failure, and disseminated cancer were independent risk factors for major complications, while advanced American Society of Anesthesiologists classification, dependent functional status, and disseminated cancer were associated with increased rates of 30-day mortality. These results were similar to the risk factors independently associated with serious adverse events (defined as major complications plus reoperations and death) observed in patients with periprosthetic fractures (that is, a history of congestive heart failure, dependent functional status, and advanced age [5]). Although a dependent functional status and history of congestive heart failure continue to be major risk factors of postoperative complications, the addition of chronic obstruction pulmonary disease in patients with pathologic fractures may further underscore the large effect metastatic cancer may have on pulmonary function. Tsuda et al. [19] reported that pulmonary complications were the most common complications after surgical treatment of pathologic hip fractures, which was also observed in this cohort.
Delayed surgery has been shown to be associated with extended postoperative length of stay in pathologic and periprosthetic settings [5], as well as with extended total hospital length of stay in patients with standard hip fractures [7]. One possible explanation for the postoperative length of stay findings is that a longer hospital time before surgery may result in deterioration in functional status, which may take additional time to restore postoperatively before the patient is ready for discharge. Alternatively, there is always the possibility of an uncontrolled confounder in any non-randomized study, although it did not manifest in any other outcome measures. With respect to mortality, we determined that advanced American Society of Anesthesiologists classification, dependent functional status, and the presence of disseminated cancer were strongly associated with 30-day mortality. These findings are likely because patients with more advanced disease had an increased perioperative risk of death. Nonetheless, these results provide some validation to surgeons and anesthesiologists that these intuitive risk factors are important risk factors for 30-day mortality among patients with pathologic hip fractures.
This study has important implications for guiding future clinical decision making for patients with pathologic hip fractures for whom surgery is indicated. Developing a treatment plan for these patients is complex and involves many key individuals, which may take time to coordinate. Furthermore, additional time may be needed for medical management, such as correction of international normalized ratios, platelet counts, and volume status. If the pathologic fracture leads to the discovery of cancer in a patient, additional biopsy or staging procedures may be indicated before surgical treatment. If a patient presents to a hospital without a dedicated orthopaedic traumatologist or oncologist who is comfortable treating pathologic fractures, this patient may need to be transferred to a tertiary care center. These, among other factors, may lead to the need to delay surgery more often than is seen for patients with standard hip fractures. Despite the many reasons surgery may need to be delayed, current knowledge extrapolated from studies on primary hip fractures suggests that taking time for tasks that could delay surgery may pose an unacceptable risk to the patient [7, 13, 15, 16]. In contrast to our expectations and current thinking, this study demonstrates that surgeons may be able to take this time when necessary. Surgical delay beyond the 2-day time period was not associated with increased complications, including 30-day mortality or pulmonary complications, as has been seen for patients with standard hip fractures.
This study demonstrated that delayed time to surgery was not independently associated with increased 30-day complications after surgical treatment of pathologic hip fractures. Delay to surgery was only associated with an increased risk of extended postoperative length of stay. These results are in contrast to the traditional dogma for standard hip fractures that surgery within 2 days of hospital arrival is associated with reduced complications [7, 13, 15, 16], which, in our experience, is sometimes extrapolated to pathologic hip fractures. However, this study offers the strongest evidence to date, and perhaps the strongest evidence possible given the low frequency of these diagnoses, that the association between delayed surgery and complications seen for patients with standard hip fractures may not exist in the pathologic setting. Although surgery should not be needlessly delayed, if the surgeon feels additional time could provide benefit to the patient, he or she should not feel the need to expedite surgery because of the risk of surgical delay observed for patients with standard hip fractures.
Footnotes
Two authors (NHV, BTA) certify that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. One of the authors certifies that she (AFC) has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from SLACK (Thorofare, NJ, USA); in an amount of less than USD 10,000 from Joint Purification Systems (Solana Beach, CA, USA); in an amount of less than USD 10,000 from ACI (Bala Cynwyd, PA, USA); in an amount of less than USD 10,000 from DePuy (Warsaw, IN, USA); in an amount of less than USD 10,000 from Sonoran Biosciences (Scottsdale, AZ, USA); in an amount of less than USD 10,000 from Graftworx (San Francisco, CA, USA); in an amount of less than USD 10,000 from Pfizer (New York, NY, USA); in an amount of less than USD 10,000 from Avanos (Alpharetta, GA, USA); in an amount of less than USD 10,000 from Irrimax (Gainesville, FL, USA); in an amount of less than USD 10,000 from Convatec (Deeside, UK); in an amount of less than USD 10,000 from 3M (Maplewood, MN, USA); in an amount of less than USD 10,000 from Recro (Malvern, PA, USA); in an amount of less than USD 10,000 from Heraeus (Hanau, Germany). One of the authors certifies that she (AFC) has received payments or benefits in an amount USD 10,000 to USD 100,000 from Stryker (Mahwah, NJ, USA); and in an amount USD 10,000 to USD 100,000 from bOne (Beijing, China).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution waived approval for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Angelini A, Trovarelli G, Berizzi A, Pala E, Breda A, Maraldi M, Ruggieri P. Treatment of pathologic fractures of the proximal femur. Injury. 2018;49:S77–S83. [DOI] [PubMed] [Google Scholar]
- 2.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basques BA, McLynn RP, Fice MP, Samuel AM, Lukasiewicz AM, Bohl DD, Ahn J, Singh K, Grauer JN. Results of database studies in spine surgery can be influenced by missing data. Clin Orthop Relat Res. 2017;475:2893–2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bohl DD, Singh K, Grauer JN. Nationwide databases in orthopaedic surgery research. J Am Acad Orthop Surg. 2016;24:673–682. [DOI] [PubMed] [Google Scholar]
- 5.Bovonratwet P, Fu MC, Adrados M, Ondeck NT, Su EP, Grauer JN. Unlike native hip fractures, delay to periprosthetic hip fracture stabilization does not significantly affect most short-term perioperative outcomes. J Arthroplasty. 2019;34:564–569. [DOI] [PubMed] [Google Scholar]
- 6.Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001;27:165–176. [DOI] [PubMed] [Google Scholar]
- 7.Fu MC, Boddapati V, Gausden EB, Samuel AM, Russell LA, Lane JM. Surgery for a fracture of the hip within 24 hours of admission is independently associated with reduced short-term post-operative complications. Bone Joint J. 2017;99B:1216–1222. [DOI] [PubMed] [Google Scholar]
- 8.Guzik G. Oncological and functional results after surgical treatment of bone metastases at the proximal femur. BMC Surg. 2018;18:2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khattak MJ, Ashraf U, Nawaz Z, Noordin S, Umer M. Surgical management of metastatic lesions of proximal femur and the hip. Ann Med Surg. 2018;36:90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marshall RA, Mandell JC, Weaver MJ, Ferrone M, Sodickson A, Khurana B. Imaging features and management of stress, atypical, and pathologic fractures. Radiographics. 2018;38:2173–2192. [DOI] [PubMed] [Google Scholar]
- 11.McLynn RP, Ondeck NT, Grauer JN, Lindskog DM. What is the adverse event profile after prophylactic treatment of femoral shaft or distal femur metastases? Clin Orthop Relat Res. 2018;476:2381–2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moghadamyeghaneh Z, Hanna MH, Hwang G, Mills S, Pigazzi A, Stamos MJ, Carmichael JC. Outcomes of colon resection in patients with metastatic colon cancer. Am J Surg. 2016;212:264–271. [DOI] [PubMed] [Google Scholar]
- 13.Moja L, Piatti A, Pecoraro V, Ricci C, Virgili G, Salanti G, Germagnoli L, Liberati A, Banfi G. Timing matters in hip fracture surgery: Patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One. 2012;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sellan ME, Lanting BA, Schemitsch EH, MacDonald SJ, Vasarhelyi EM, Howard JL. Does time to surgery affect outcomes for periprosthetic femur fractures? J Arthroplasty. 2018;33:878–881. [DOI] [PubMed] [Google Scholar]
- 15.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–54. [DOI] [PubMed] [Google Scholar]
- 16.Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, DeBeer J, Bhandari M. Effect of early surgery after hip fracture on mortality and complications: Systematic review and meta-analysis. Cmaj. 2010;182:1609–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steeg PS. Targeting metastasis. Nat Rev Cancer. 2016;16:201–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Szender JB, Frederick PJ, Eng KH, Akers SN, Lele SB, Odunsi K. Evaluation of the national surgical quality improvement program universal surgical risk calculator for a gynecologic oncology service. Int J Gynecol Cancer. 2015;25:512–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsuda Y, Yasunaga H, Horiguchi H, Fushimi K, Kawano H, Tanaka S. Complications and postoperative mortality rate after surgery for pathological femur fracture related to bone metastasis: Analysis of a nationwide database. Ann Surg Oncol. 2016;23:801–810. [DOI] [PubMed] [Google Scholar]
- 20.Tsuzuki S, Park SH, Eber MR, Peters CM, Shiozawa Y. Skeletal complications in cancer patients with bone metastases. Int J Urol. 2016;23:825–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Varady NH, Ameen BT, Hayden BL, Yeung CM, Schwab P-E, Chen AF. Short-term morbidity and mortality after hemiarthroplasty and total hip arthroplasty for pathologic proximal femur fractures. J Arthroplasty. 2019;34:2698–2703. [DOI] [PubMed] [Google Scholar]
- 22.Varady NH, Ameen BT, Schwab P, Yeung CM, Chen AF. Trends in the surgical treatment of pathological proximal femur fractures in the United States. J Surg Oncol. 2019;120:994–1007. [DOI] [PubMed] [Google Scholar]
- 23.Wedin R. Surgical treatment for pathologic fracture. Acta Orthop Scand. 2001;72:1–29. [PubMed] [Google Scholar]