Abstract
Background
Recurrent dislocation after THA remains a serious complication that carries with it a high risk of revision surgery. Previous studies have shown reduced dislocation rates with the use of lipped polyethylene (PE) liners in modular uncemented acetabular components, but there may be increased wear because of impingement, which may lead to aseptic loosening in the longer term; whether the aggregate benefit of lipped PE liners outweighs the risks associated with their use remains controversial.
Questions/purposes
We used data from the New Zealand Joint Registry to (1) compare Kaplan-Meier survival rates, (2) rates of revisions for dislocation between neutral and lipped PE liners, and (3) revision rates for aseptic loosening for the four most commonly used modular uncemented cups.
Methods
We used data from the New Zealand Joint Registry (NZJR) to identify 31,247 primary THAs using the four most commonly used uncemented modular acetabular implants from January 1, 1999 to December 31, 2018. The lipped liner group comprised 49% males (9924 of 20,240) compared with 42% (4669 of 11,007) in the neutral group (p < 0.001); 96% (19,382 of 20,240) of patients in the liner group had OA versus 95% (10,450 of 11,007) in the neutral group (p < 0.001). There was no difference in other patient characteristics such as age (mean 66.9 years), BMI (mean 29 ± 6 kg/m2) and American Society of Anesthesiologists grade. The mean follow-up was 5.1 years (SD 3.9) and longest follow-up 19.3 years. The NZJR has more than 96% capture rate and data entry is a mandatory requirement of members of the New Zealand Orthopaedic Association. Kaplan-Meier survival rates were compared between 20,240 lipped and 11,007 neutral PE liners. Highly cross-linked polyethylene was used in 99% of lipped liner cups and 85% of neutral liner cups. Associated hazard ratios were calculated using a Cox regression analysis with a Kaplan-Meier revision-free estimates plot.
Results
The Kaplan-Meier survival at 10 years for lipped PE liners was 96% (95% confidence interval 95.4 to 96.2) and for neutral liners 95% (95% CI 94.7 to 95.9). After controlling for age, gender approach, femoral head size, and the use of image guidance, the all-cause revision risk was greater for neutral PE liners than that for lipped PE liners (HR 1.17 [95% CI 1.06 to 1.36]; p = 0.032). There was a higher risk of revision for dislocation in those with neutral PE liners than in those with lipped liners (HR 1.84 [95% CI 1.41 to 2.41]; p < 0.001) but no difference in the revision rate for aseptic acetabular component loosening (HR 0.85 [95% CI 0.52 to 1.38]; p = 0.511).
Conclusions
The use of a lipped PE liner is not associated with a higher rate of aseptic loosening in patients who undergo primary THA compared with a neutral PE liner. Lipped PE liners are associated with lower rates of dislocation and lower all-cause revision rates without any increased association with revision rates for wear and aseptic loosening.
Level of Evidence
Level III, therapeutic study.
Introduction
In general, there are two designs of polyethylene liners in common use for THA, lipped and non-lipped. Neutral or non-lipped liners have the same PE depth around their circumference while lipped PE liners, originally designed to reduce posterior instability, have an augmented rim. This rim increases the travelling distance of the head before dislocation occurs. The surgeon typically places the lip in the position that will reduce dislocation risk [12]. However, when the hip is rotated in the opposite direction, the neck of the stem may come into contact with the lip (impingement), which may potentially increase the risk of instability in the opposite direction or lead to increased wear or risk of a liner fracture. Lipped polyethylene (PE) liners in conjunction with modular uncemented acetabular components have been shown to reduce the medium-term risk of revision for instability [6]. However, lipped PE liners may cause late instability and aseptic loosening as a result of impingement and PE-associated wear [12]. Lipped liners can have lips that vary from 10° to 20° and have differing heights depending on the manufacturer. Face-changing options are also available.
Whether the aggregate benefit of lipped PE liners outweighs the long-term potential risks remains controversial, especially given the advances in modern highly-crosslinked polyethylene [3]. This is an important question, however, as instability remains one of the most common reasons for early revision after primary THA [12, 13] and is a function of patient factors (such as obesity, underlying diagnosis, increased age, sex, cognitive function, neurologic dysfunction, compliance issues, or previous surgery), operative factors (like approach, implant alignment, restoration, or establishment of hip biomechanics) [16], and surgeon factors (for instance, training and experience) [15]. All-cause revision rate analysis is important because reasons for revision often coexist (for example, aseptic stem loosening and periprosthetic fracture, infection with pain, loosening and fracture). To capture the entirety of any association all-cause revision must therefore be considered. All-cause revision is also the most important to patients. If a stem neck impinges onto a lipped liner it potentiates PE wear, increasing the risk of loosening, and loose implants may be more likely to become infected from the hematogenous spread of bacteria. Also, PE wear leading to increased osteolysis is likely to lead to a higher periprosthetic fracture risk.
We therefore used data from the New Zealand Joint Registry (NZJR) to compare (1) Kaplan-Meier survival rates with the outcomes of (1) all-cause revision (2) revision for dislocation and (3) revisions for aseptic loosening between neutral and lipped PE liners used in the four most common modular uncemented cups.
Patients and Methods
Data Source
The NZJR was established in 1998 and has a greater than 96% data capture rate of all joint arthroplasties [13]. Prospective entry of data into the NZJR is a mandatory requirement of all members of the New Zealand Orthopaedic Association, with all data held securely in Christchurch, New Zealand. Data linkage to the national New Zealand register for marriages, births, and deaths is performed automatically to the NZJR every 6 months. One of the authors (CMAF) accessed the database to acquire data specifically for this study. The de-identified data of all patients undergoing primary THA from the NZJR’s inception to December 31, 2018 was available for analysis. We performed and reported this study in accordance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) and Reporting of studies Conducted using Observational Routinely-collected Data (RECORD) guidelines [2].
Ethical Approval
No formal institutional review board approval was required because this was a review of de-identified data from the NZJR, which already has institutional review board approval for the publication of results stored in its registry.
Patient Demographics and Diagnosis
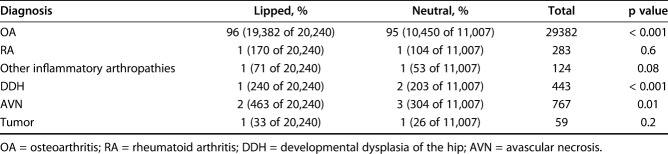
We extracted data on age, sex, BMI, American Society of Anesthesiologists class, and preoperative diagnosis associated with the primary procedure. In all, 20,240 lipped liners and 11,007 neutral liners were identified for analysis. The lipped liner group comprised 49% males (9924 of 20,240) compared with 42% (4669 of 11,007) in the neutral group (p < 0.001); 96% (19,382 of 20,240) had OA versus 95% (10,450 of 11,007) in the neutral group (p < 0.001). (Table 1). There was no difference in other patient characteristics such as age (mean 66.9 years), BMI (mean 29 ± 6 kg/m2) and American Society of Anesthesiologists grade. Highly cross-linked polyethylene (HXLPE) was used in 99% of lipped liner cups and 85% of neutral liner cups. In both groups, the posterior approach was the most common surgical approach; it was used in 81% of patients (16,394 of 20,240) with lipped liners and 65% of patients (7154 of 11,007) with neutral liners. However, lipped PE liners were used in a greater proportion of patients whose THA was performed through the posterior approach (p < 0.001). The lateral approach was used in 17% of lipped liners (3200) and 31% of neutral liners (3131); the direct anterior approach was used in 2% of lipped liners (309) and 4% of neutral liners (694). The mean follow-up was 5.1 years (SD 3.9) and longest follow-up was 19.3 years.
Table 1.
Comparison of diagnoses between the lipped and neutral PE liner groups
Operative Cohort
Through an analysis of all brand information and catalog numbers, we identified all lipped and non-lipped PE liners used in the four most frequently used modular uncemented acetabular systems: the Duraloc® (DePuy, Warsaw, IN, USA; included lipped liners had 10° lips with either HXLPE or ultra-high molecular weight polyethylene [UHMWPE]), Pinnacle® (DePuy); included lipped liners had 10° lips with either HXLPE or UHMWPE), Trident® (Stryker, Mahwah, NJ, USA; included lipped liners had 10° lips; we excluded those with an elevated rim and all eccentric inserts), and Trilogy® (Zimmer, Warsaw, IN, USA; the included lipped liners had 10° and 20° lips, but we excluded constrained, dual mobility and 7-mm offset liners). All constrained, face-changing, lateral offset liners and dual mobility constructs were excluded from the analyses.
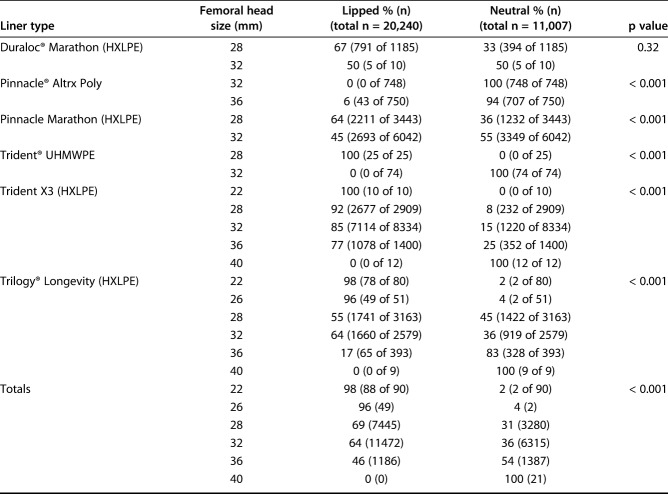
We identified 31,247 primary THAs using the most frequently used uncemented modular acetabular implants, as reported in the NZJR between January 1, 1999 and May 31, 2018, representing approximately 60% of all primary uncemented THAs in the NZJR. There were 20,240 lipped PE liners and 11,007 neutral PE liners. There was an uneven distribution of large-diameter femoral heads between groups, with neutral liners predominating as head sizes approach 36 mm and 40 mm (Table 2).
Table 2.
Distribution of femoral head sizes and PE liner type
Outcome Measures
Survival was calculated using the Kaplan-Meier method with 95% CIs. We first examined the all-cause rates of revision between study groups. We defined a revision as a new operation in a patient who had undergone a previous THA during which one or more of the components was exchanged, removed, manipulated, or added. Revision included excision arthroplasty but not soft tissue-only procedures. The all-cause revision rate provides the most conservative estimate of prosthesis survivorship. Kaplan-Meier estimates are the appropriate method when exploring implant failure [11]. In addition, we examined survival with revision for dislocation and also aseptic acetabular component loosening and compared them between groups using a multivariate analysis that adjusted for surgical approach, whether the procedure was image-guided, and femoral head size. Overall, 86 lipped liners (15.9%) were revised for “other” reasons compared with 64 (19.6%) neutral liners (p = 0.355).
Statistical Analysis
We performed Kaplan-Meier survival analysis. Hazard ratios with 95% CIs were calculated using Cox regression analyses. Age, BMI, and Oxford hip scores were compared between study groups using an ANOVA, and sex, American Society of Anesthesiologists class, surgical approach, and diagnoses were compared using chi-square tests.
Results
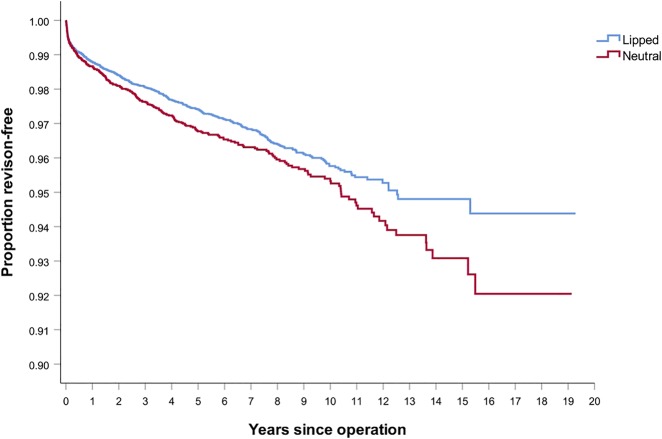
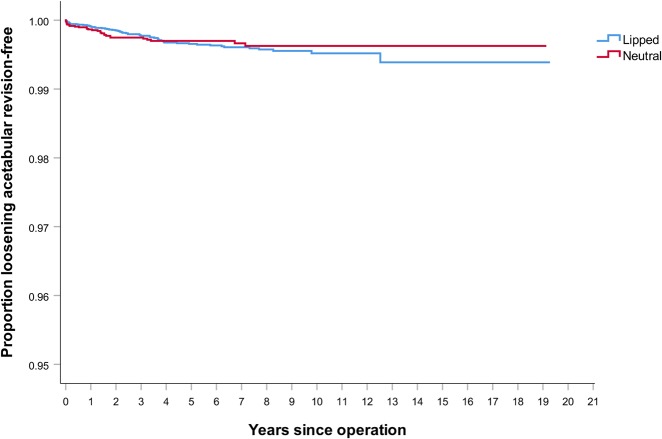
After controlling for age, sex, approach, femoral head size, and the use of image guidance (Table 3), we found the all-cause revision risk to be greater in patients who received neutral PE liners than those who received lipped liners (HR 1.19 [95% CI 1.03 to 1.37]; p = 0.02) (Fig. 1). Controlling for the same confounders, there was no difference in the rate of revision for deep infection between lipped PE liners and neutral PE liners, but there was a higher rate of revision for periprosthetic femoral fracture in the neutral PE liner group than in the lipped PE liner group (adjusted HR 1.56 [95% CI 1.12 to 2.18]; p = 0.008).
Table 3.
Multivariate regression analysis for all-cause revisions between lipped and neutral PE groups
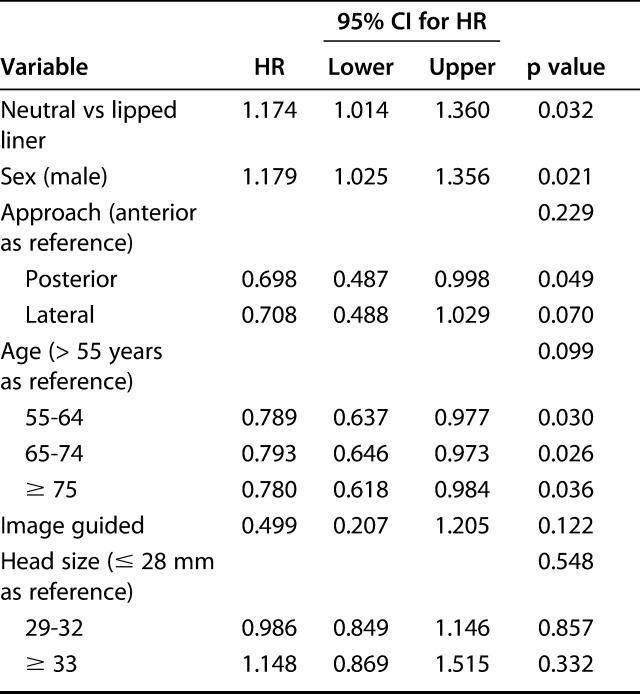
Fig. 1.
These Kaplan-Meier survival curves show the all-cause revision rates in the lipped and neutral PE liner groups.
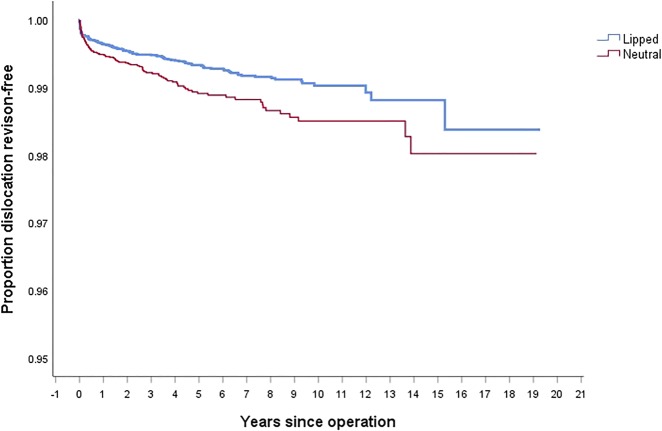
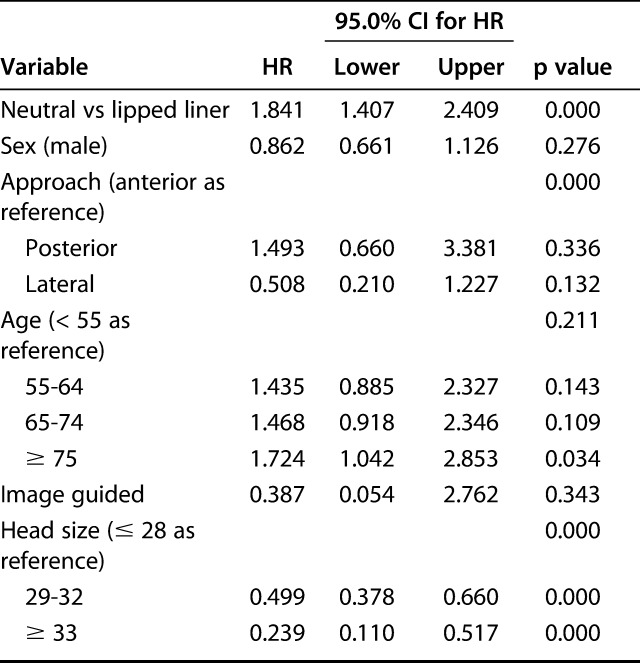
After controlling for age, sex, surgical approach, as well as the use of image-guidance and femoral head sizes, we found that the neutral PE liner group had a higher revision rate for dislocation than the lipped group (HR 1.84 [95% CI 1.40 to 2.41]; p < 0.001) (Fig. 2). Patient age older than 75 years was associated with a HR of 1.7 compared with patients younger than 55 years of age; however, female gender was not associated with a higher rate of revision for dislocation in our study (Table 4).
Fig. 2.
These Kaplan-Meier survival curves show the revision rates for instability in the lipped and neutral PE liner groups.
Table 4.
Multivariate regression analysis of revisions for dislocation between lipped and neutral PE groups
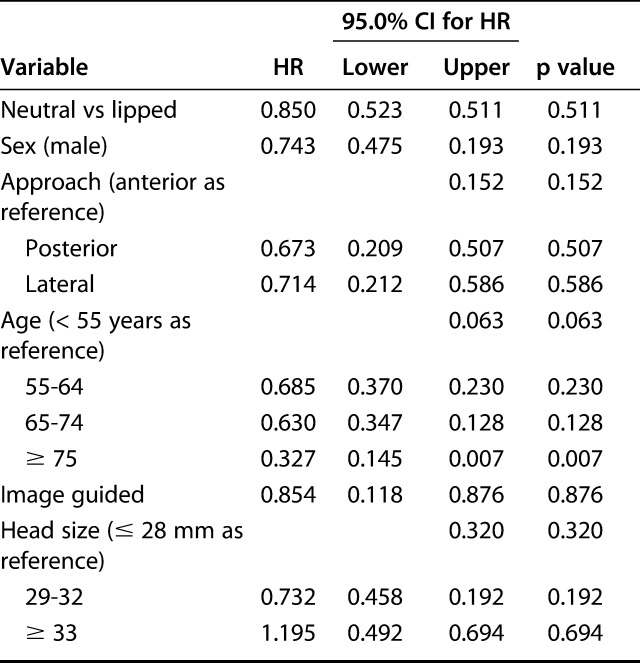
After controlling for age, gender, surgical approach, image guidance, and femoral head size, there was no difference in revision rates for aseptic loosening between groups (Fig. 3). At 10 years, lipped liners had a Kaplan-Meier survival of 99.5% (95% CI 99.3 to 99.7) and neutral liners had a 99.6% survival (95% CI 99.4 to 99.8); for acetabular loosening the HR was 0.85 [95% CI 0.52 to 0.51; p = 0.51) (Table 5).
Fig. 3.
These Kaplan-Meier survival curves show the revision rates for acetabular aseptic loosening in the lipped and neutral PE liner groups.
Table 5.
Multivariate regression analysis of revisions for aseptic acetabular component loosening comparing lipped and neutral PE groups
Discussion
This study was a retrospective analysis of prospectively, systematically, and consecutively collected national registry data with a greater than 96% capture rate. The study represents a wide spectrum of orthopaedic surgeons with varied clinical experience covering an entire nation, leading to generalizability of the findings. National joint registry data can support evidence-based practice, implant surveillance, hospitals, surgeons, and patient-reported outcome measures. They may also be used to identify subtle trends, which would not be logistically feasible through other methods, and with the methods employed here may demonstrate important associations but not causation [5]. We compared the most frequently used modular uncemented acetabular implants using either lipped or neutral polyethylene liners captured in the NZJR. There was no difference in revision rates for aseptic loosening of the acetabular or femoral components. The results of this study therefore suggest that the use of a lipped PE liner in conjunction with these cups is associated with a lower revision risk for all causes and dislocation, without an associated increased revision risk for aseptic loosening.
This study had several limitations. First, the indications for the surgical decision-making in selecting or inserting a neutral or lipped liner are unknown. Surgeons may routinely use a lipped liner, or they may choose it only in circumstances where adequate stability is not obtained using a neutral liner, leading to selection bias. Second, we did not survey surgeon volume/experience and preferences; more experienced surgeons may prefer for a specific liner type in different circumstances. Furthermore, whether a surgeon repaired the capsule and short external rotators when performing a posterior approach was not captured in this study, yet these are important factors that contribute to stability [8, 14]. However, we feel these factors are likely distributed throughout New Zealand and are offset by the large numbers of THA studied. Third, there was also a greater proportion of HXLPE used in the lipped liner group compared with the neutral liner group, and HXLPE is known to contribute to reduced polyethylene wear [3]. However, in both groups HXLPE was used in more than 85% of cases so we do not feel that this contributed substantially to the findings of our study. The differences in revision rates for periprosthetic fractures is likely related to other unexamined confounding factors such as the type of femoral component, and we did not include this in the multivariate analysis; however, there is no plausible reason why this finding would be related to whether the liner was lipped or not. The study methodology precludes analysis of more subtle design-related factors of these PE liners.
Finally, to investigate causation, randomized clinical trial designs are typically used [5]. We were unable to account for other possible confounders such as the severity of joint disease, surgical technique in positioning of the lipped liners, or the increasing complexity of patient comorbidities and medications. We used age and American Society of Anesthesiologists class as proxy indicators for comorbidities with the rationale that these are the best indices in recent research [10]. Additionally, more complex models have not been shown to result in better discrimination in other settings [7]. Revision rates may not capture all failures because some patients with failed or recurrently dislocating implants may undergo nonoperative management or may not be fit for surgery. The decision to perform revision THA depends on patient factors such as comorbidity and choice, surgical factors such as a perceived risk and benefit analysis, surgical skills, and departmental resources. Furthermore, the NZJR does not capture purely soft-tissue procedures. It was not possible in the studied dataset to perform a radiologic analysis of the included procedures; therefore, we were unable to assess factors such as fixation or implant alignment.
Similar to Insull et al. [6] (lipped PE liner revision rate 0.62 per 100 component years), the all-cause revision rate in our medium-term follow-up study was lower with lipped PE liners than for neutral PE liners (lipped PE all-cause revision rate 0.51 per 100 component years). Although our study includes the data from Insull et al. [6], the longer-term follow-up of our study permits the association with long-term impingement, wear, and associated instability to be captured and hence the aggregate longer-term benefit of a lipped PE liner.
We found there was a much lower risk of all-cause revision and revision for dislocation for lipped PE liners than for neutral liners with these four specific uncemented cup designs. This was despite neutral liners being implanted more often with the lateral approach. Lipped liners were inserted more often in male patients, yet on regression analysis gender was not associated with revision for dislocation in this study. In a previous study using data from the NZJR, Insull et al. [6] examined 8023 uncemented cups with lipped PE liners and 4088 with neutral PE liners. After controlling for femoral head size, approach, age, and sex, they found that patients with neutral PE liners were 2.4 times more likely to undergo revision for instability (p < 0.001). This finding concurs with our study of 20,240 lipped PE liners and 11,007 neutral PE liners. In a recent systematic review and meta-analysis, the use of a lipped liner was associated with a reduced instability rate after THA [8]. In this study, patient risk factors for instability were age older than 70 years (RR 1.27 [95% CI 1.02 to 1.57]) compared with patient age younger than 70 years, but not female gender (RR 0.97 [95% CI 1.02 to 1.57]), drug use disorder, social deprivation, BMI > 30 kg/m2 (RR 1.38 [95% CI 1.03 to 1.85] compared with patients with BMI < 30 kg/m2), neurological disorders, psychiatric disease, comorbidity indices, previous surgery including spinal fusion, underlying diagnoses of avascular necrosis, rheumatoid, and other inflammatory arthritis.
The use of a lipped PE liner was not associated with an increased risk for revision of the acetabular component because of aseptic loosening in our study. This suggests that the aggregate benefit of using PE liners to provide stability is not countered by impingement-related PE wear in the time frame studied. The use of HXLPE in most of the cups in our study is very likely a key factor [3]. The use of lipped PE liners may convey advantages, therefore, in reducing the lifetime risk of revision THA [1, 4, 9].
Conclusions
The use of lipped PE liners is associated with a lower mid-term risk of revision for all causes and for dislocation, without compromising the associated risk for revision for aseptic loosening. We recommend the continued use of lipped liners to reduce the risk of dislocation and all-cause revision.
Acknowledgments
We thank Toni Hobbs for her expertise in retrieving data from the NZJR.
Footnotes
The institution of one or more of the authors (MRW) has received, during the study period, funding from the National Institute of Health Research. The institution of one or more of the authors (GH) has received, during the study period, research stipends from Mathys and Stryker.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution waived approval for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Department of Orthopaedic Surgery and Musculoskeletal Medicine, University of Otago, Christchurch, New Zealand.
References
- 1.Bayliss LE, Culliford D, Monk AP, Glyn-Jones S, Prieto-Alhambra D, Judge A, Cooper C, Carr AJ, Arden NK, Beard DJ, Price AJ. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017;389:1424-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sorensen HT, von Elm E, Langan SM; RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLOS Med. 2015;12:e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Devane P, Horne J, Ashmore A, Mutimer J, Kim W, Stanley J. Highly cross-linked polyethylene reduces wear and revision rates in total hip arthroplasty: A 10-year double-blinded randomized controlled trial. J Bone Joint Surg Am. 2017;99:1703-1714 [DOI] [PubMed] [Google Scholar]
- 4.Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393:647-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Graves S. The value of arthroplasty registry data. Acta Orthopaedica . 2010;81:8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Insull PJ, Cobbett H, Frampton CM, Munro JT. The use of a lipped acetabular liner decreases the rate of revision for instability after total hip replacement. A study using data from the New Zealand Joint Registry. Bone Joint J . 2014;96:884-888. [DOI] [PubMed] [Google Scholar]
- 7.Karres J, Heesakkers NA, Ultee JM, Vrouenraets BC. Predicting 30-day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury. 2015;46:371-377. [DOI] [PubMed] [Google Scholar]
- 8.Kunutsor S, Barrett M, Beswick A, Judge A, Blom A, WyldeWyle V, Whitehouse M. Risk factors for dislocation after primary total hip replacement: a systematic review and meta-analysis of 125 studies involving five million hip replacements. Lancet Rheumatology. 2019;1:PE111-E121. [DOI] [PubMed] [Google Scholar]
- 9.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606-2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ondeck NT, Bohl DD, Bovonratwet P, McLynn RP, Cui JJ, Shultz BN, Lukasiewicz AM, Grauer JN. Discriminative ability of commonly used indices to predict adverse outcomes after poster lumbar fusion: a comparison of demographics, ASA, the modified Charlson Comorbidity Index, and the modified Frailty Index. Spine J. 2018;18:44-52. [DOI] [PubMed] [Google Scholar]
- 11.Sayers A, Evans JT, Whitehouse MR, Blom AW. Are competing risks models appropriate to describe implant failure? Acta Orthop. 2018;89:256-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sultan PG, Tan V, Lai M, Garino JP. Independent contribution of elevated rim acetabular liner and femoral head size to the stability of total hip implants. J Arthroplasty . 2002;17:289-292. [DOI] [PubMed] [Google Scholar]
- 13.The New Zealand Joint Registry. The New Zealand Joint Registry . Nineteen year report January 1999 to December 2017. Available at: https://nzoa.org.nz/system/files/DH8152_NZJR_2018_Report_v6_4Decv18.pdf. Accessed December 10, 2018. [Google Scholar]
- 14.Werner BC, Brown TE. Instability after total hip arthroplasty. World J Orthop . 2012;3:122-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wyatt MC, Hooper G, Frampton C, Rothwell A. Survival outcomes of cemented compared to uncemented stems in primary total hip replacement. World J Orthop. 2014;18:5:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wyatt MC, Kieser DC, Kemp MA, McHugh G, Frampton CM, Hooper GJ. Does the femoral offset affect replacements? The results from a national joint registry. Hip Int. 2019;29:289-298. [DOI] [PubMed] [Google Scholar]