ABSTRACT
Ulcerative colitis (UC) is a known risk factor for colorectal cancer, but the association between UC and appendiceal adenocarcinoma remains rare. We present a 42-year-old patient with long-standing UC who presented with acute appendicitis shortly after a routine colonoscopy. Histopathological examination revealed moderately differentiated appendiceal adenocarcinoma. The recognition of appendiceal cancer as a complication of long-standing UC warrants increased clinical awareness.
INTRODUCTION
Ulcerative colitis (UC) is a known risk factor for colorectal cancer, especially in patients with long-standing disease, younger age of diagnosis, pancolonic extension, and history of primary sclerosing cholangitis (PSC).1 Although more than half of patients with pancolonic disease have appendiceal involvement, its association with appendiceal adenocarcinoma remains questionable and only a few cases have been reported.2
CASE REPORT
A 42-year-old man with a 10-year history of UC and PSC presented to the emergency department with a 2-day history of progressively worsening right lower quadrant pain. He had been receiving infliximab 10 mg/kg every 8 weeks and azathioprine 2.5 mg/kg daily. The patient had multiple treatment failures in the past including golimumab and 5 mg/kg infliximab therapy. A colonoscopy performed 1 year before showed severe pancolitis, and there was a focus of indeterminate dysplasia on random colon biopsies confirmed by a pathologist with expertise in inflammatory bowel disease (IBD). At that time, the patient was lost to follow up by his previous provider because he had relocated and presented to our clinic 2 weeks before to establish care. A routine colonoscopy was done 3 days before admission to ascertain mucosal healing was compatible with severe UC (Mayo score 3) in the whole colon (Figure 1). Appendiceal orifice appeared congested, and the terminal ileum was normal (Figure 2).
Figure 1.
Spontaneous bleeding and ulceration in the whole colon compatible with severe ulcerative colitis.
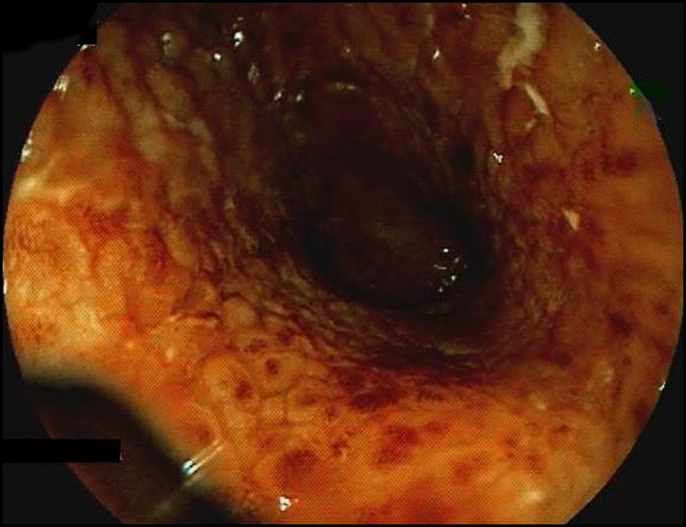
Figure 2.

Inflammation and congestion of the appendiceal orifice.
Physical examination revealed right lower quadrant tenderness and a positive McBurney sign. Laboratory investigation was significant for leukocytosis of 12,570/μL. Abdominal and pelvic computed tomography showed a markedly dilated fluid-filled appendix measuring 2.6 × 2.4 cm consistent with acute appendicitis (Figure 3). Retroperitoneal lymphadenopathy was noted.
Figure 3.
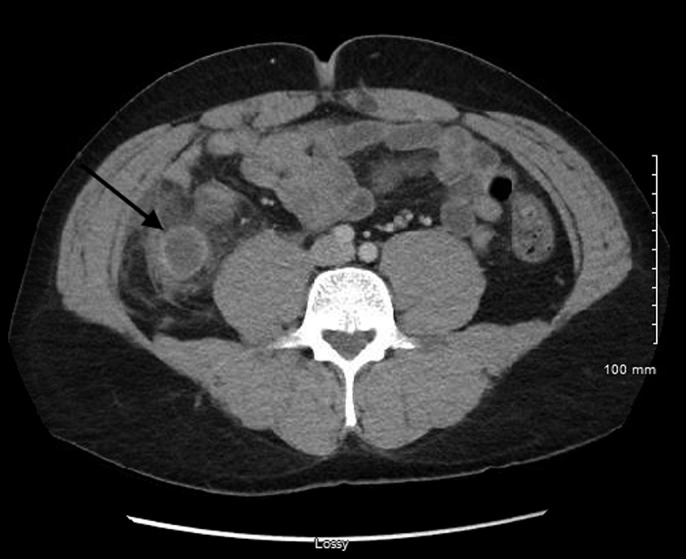
Markedly dilated fluid-filled appendix (arrow) measuring 2.6 × 2.4 cm.
Given the severity of his UC, previous focus of indeterminate dysplasia, and nonresponse to multiple therapies, the patient agreed to undergo total proctocolectomy with ileostomy. Histology was consistent with invasive moderately differentiated appendiceal adenocarcinoma involving the visceral peritoneum along with acute appendicitis. Pathologic examination of the colon revealed diffuse moderately active pancolitis with several areas of low-grade dysplasia (Figure 4). The patient's postoperative course was uneventful and was planned for adjuvant chemotherapy after discharge.
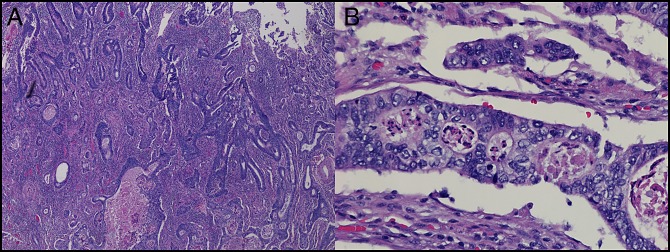
Figure 4.
Hematoxylin and eosin stain of moderately differentiated appendiceal adenocarcinoma at (A) 40× magnification and (B) 400× magnification.
DISCUSSION
Although the appendix is considered by many a vestigial remnant, it has been implicated in the pathogenesis of multiple diseases including UC. In fact, several large population-based studies demonstrated a lower incidence rate ratio of UC after appendectomy compared with controls.3–5 The largest of these studies showed that the risk of UC was significantly reduced only in patients who underwent appendectomy for appendicitis, whereas appendectomy without appendicitis was not associated with a reduced risk.4
More than half of the patients with pancolonic UC are found to have appendiceal involvement.3 Patients with ulcerative appendicitis experience a more aggressive relapsing disease course compared to those without appendiceal involvement.6
Appendiceal carcinomas are exceedingly rare; data from the Surveillance, Epidemiology, and End Results database report an incidence of 0.95 per million people per year with an average age of 63 years at diagnosis.7 In contrast to other appendiceal neoplasms that are usually asymptomatic, adenocarcinoma of the appendix most commonly presents with acute appendicitis.8
In general, they possess a nearly identical phenotype to those of conventional colonic adenocarcinoma.9 However, the natural history and prognosis of appendiceal adenocarcinomas differ from those of adenocarcinomas arising from other large bowel sites and therefore have a separate staging classification. Long-term oncological outcomes are worse in appendiceal cancer compared to colon cancer with a worse 5-year disease-free survival rate, higher rate of peritoneal seeding, and higher risk of perforation.10 In patients with IBD, chronic inflammation is an important risk factor for the development of gastrointestinal malignancies. The pathogenesis of colitis-associated adenocarcinoma is distinct from sporadic colorectal cancer because the underlying inflammation yields a faster and multifocal process of carcinogenesis.11 Because the appendix is affected in half of the patients with pancolitis, the risk of appendiceal cancer is the same as the rest of the colon.
Although only a few cases of UC associated with appendiceal malignancy have been described, the mechanism leading to cancer occurrence is suspected to be the same as colorectal cancer.12 However, dysplasia of the colonic mucosa was not identified in many previously published cases, raising suspicion that the malignancy may have been incidental.13–15 Our patient had multiple risk factors to suggest that the appendiceal adenocarcinoma was a neoplastic complication of his long-standing UC, including prolonged active pancolitis, history of PSC, and multiple areas of low-grade dysplasia of the colon on pathological examination. In addition, significant inflammation and involvement of the appendiceal orifice, as noted in our case, may block excretion from the cavity, leading to increased appendiceal pressure and development of malignancy.16 Patients with pancolonic UC, PSC, and confirmed indeterminate colitis on random colonic biopsies as our patient would benefit from an intensive surveillance strategy for colorectal cancer given their high risk of advanced neoplasia.17
Although adenocarcinoma of the appendix likely precipitated the episode of acute appendicitis, colonoscopy was possibly a contributing factor given the timing of symptoms nearly 24 hours after the endoscopic examination. Basson et al noted an increased risk of appendicitis within 1 week of undergoing a colonoscopy.18
Although the absolute risk of appendiceal neoplasia among patients with IBD remains low, likely pertaining to the small area of mucosa at-risk relative to that of the colorectum, the recognition of appendiceal adenocarcinoma as a complication of long-standing disease warrants increased clinical awareness. Additional studies are needed to further elucidate the nature of this association.
DISCLOSURES
Author contributions: F. Nehme wrote the manuscript and is the article guarantor. A. Schneider and F. Hamid revised the manuscript.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
REFERENCES
- 1.Keller DS, Windsor A, Cohen R, et al. Colorectal cancer in inflammatory bowel disease: Review of the evidence. Tech Coloproctol. 2019;23(1):3–13. [DOI] [PubMed] [Google Scholar]
- 2.Goldblum JR, Appelman HD. Appendiceal involvement in ulcerative colitis. Mod Pathol. 1992;5(6):607–10. [PubMed] [Google Scholar]
- 3.Hallas J, Gaist D, Vach W, et al. Appendicectomy has no beneficial effect on admission rates in patients with ulcerative colitis. Gut. 2004;53(3):351–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frisch M, Pedersen BV, Andersson RE. Appendicitis, mesenteric lymphadenitis, and subsequent risk of ulcerative colitis: Cohort studies in Sweden and Denmark. BMJ. 2009;338:b716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurina LM, Goldacre MJ, Yeates D, et al. Appendicectomy, tonsillectomy, and inflammatory bowel disease: A case-control record linkage study. J Epidemiol Community Health. 2002;56(7):551–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dendrinos K, Cerda S, Farraye FA. The “cecal patch” in patients with ulcerative colitis. Gastrointest Endosc. 2008;68(5):1006–7. [DOI] [PubMed] [Google Scholar]
- 7.McGory ML, Maggard MA, Kang H, et al. Malignancies of the appendix: Beyond case series reports. Dis Colon Rectum. 2005;48(12):2264–71. [DOI] [PubMed] [Google Scholar]
- 8.Ito H, Osteen RT, Bleday R, et al. Appendiceal adenocarcinoma: Long-term outcomes after surgical therapy. Dis Colon Rectum. 2004;47(4):474–80. [DOI] [PubMed] [Google Scholar]
- 9.Carr NJ, Emory TS, Sobin LH. Epithelial neoplasms of the appendix and colorectum: An analysis of cell proliferation, apoptosis, and expression of p53, CD44, bcl-2. Arch Pathol Lab Med. 2002;126(7):837–41. [DOI] [PubMed] [Google Scholar]
- 10.Son IT, Ahn S, Park KJ, et al. Comparison of long-term oncological outcomes of appendiceal cancer and colon cancer: A multicenter retrospective study. Surg Oncol. 2016;25(1):37–43. [DOI] [PubMed] [Google Scholar]
- 11.Axelrad JE, Lichtiger S, Yajnik V. Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment. World J Gastroenterol. 2016;22(20):4794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyda MH, Noffsinger A, Belli J, et al. Multifocal neoplasia involving the colon and appendix in ulcerative colitis: Pathological and molecular features. Gastroenterology. 1998;115(6):1566–73. [DOI] [PubMed] [Google Scholar]
- 13.Villanueva Saenz E, Pérez-Aguirre J, Belmonte MC, et al. Appendix adenocarcinoma associated with ulcerative colitis: A case report and literature review. Tech Coloproctol. 2006;10(1):54–6. [DOI] [PubMed] [Google Scholar]
- 14.Odze RD, Medline P, Cohen Z. Adenocarcinoma arising in an appendix involved with chronic ulcerative colitis. Am J Gastroenterol. 1994;89(10):1905–7. [PubMed] [Google Scholar]
- 15.Zannoni U, Masci C, Bazzocchi R, et al. Cancer of the appendix in long-standing ulcerative colitis: A case report. Tumori. 1997;83(6):958–9. [DOI] [PubMed] [Google Scholar]
- 16.Takeda Y, Nakase H, Mikami S, et al. Possible link between ulcerative colitis and in situ adenocarcinoma of an appendiceal mucocele: Importance of inflammation in the appendiceal orifice related to UC. Inflamm Bowel Dis. 2008;14(6):873–4. [DOI] [PubMed] [Google Scholar]
- 17.Mahmoud R, Shah SC, Torres J, et al. Association between indefinite dysplasia and advanced neoplasia in patients with inflammatory bowel diseases undergoing surveillance. Clin Gastroenterol Hepatol. 2019. [Epub ahead of print August 22, 2019.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basson MD, Persinger D, Newman WP. Association of colonoscopy with risk of appendicitis. JAMA Surg. 2018;153(1):90–1. [DOI] [PMC free article] [PubMed] [Google Scholar]