Abstract
Trauma with an accompanying fracture to the anterior teeth gives an agonizing experience for a young individual due to the physical disfigurement and the psychological impact that is imposed on them. This paper reports a case of complicated crown-root fracture in a young child that was treated by extra-oral fragment reattachment followed by the intentional reimplantation. The tooth was endodontically-treated followed by the placement of fiber-reinforced composite post. The fragments were reattached extra orally following an atraumatic extraction. The tooth was then reimplanted back into the socket followed by splinting. Clinical results were successful after 2 years. This case report demonstrates the importance of modifying a treatment protocol to maintain esthetics up to the completion of the developmental period.
Keywords: Crown-root fracture, esthetics, fiber-reinforced composite post, fragment reattachment, intentional reimplantation
Introduction
Dental trauma is a painful experience that can impair orofacial function, negatively affecting growth, occlusion, and esthetics. At the same time, it has a significant impact, on an emotional and psychological level, distracting from the quality of life of young children and their parents. Any trauma with accompanying fracture to the anterior teeth is an agonizing experience for a young individual, which requires immediate attention, not only because of the physical disfigurement but also because of the psychological impact on the patient.[1] Traumatic dental injuries are common among the boys in the age group of 6–12 years which is particularly true for maxillary central incisors.[2] It has been suggested that the incidence of dental trauma in the near future will overcome the incidence of caries and periodontal disease in children and teenagers.[3] Physical leisure activities at home, in kindergartens, at playgrounds, and in schools continue to account for a significant proportion of traumatic dental injuries in young children and teenagers, on the other hand, are mostly injured during sport activities, traffic accidents, and some forms of violence (e.g., fights, assault).[4] Parents and physical education personnel in institutions have a deficient knowledge toward the management protocol following a traumatic dental injury which can have an effect on the treatment plan.[5,6]
Crown-root fractures account for only 5% of all traumatic injuries and present difficulties for the successful management. The treatment of crown-root fractures in children is compromised by a fracture below the gingival margin and/or bone.[7] When they do occur, they present both endodontic and restorative problems,[8] which are a challenging task.
Some techniques have been developed to restore the fractured crown. Early techniques include jacket crown, orthodontic bands, pin-retained resin, and postcore supported prosthetic restorations such as resin crowns, ceramic crowns, porcelain bonded crown, and composite resin.[7,8] If the fracture extends the biologic width, which is described as the gap between the crestal bone and gingival sulcus, flap surgery combined with osteoplasty/osteotomy procedures is required.[4] In spite of various advances in adhesive material, there is no restorative material that will bring back the perfect esthetics and functionality as much as natural dental structures. Reattachment of the crown fragment to a fractured tooth influences esthetics by retaining natural translucency and surface texture. This is the rationale behind the procedure for being the first choice for crown fractures of the anterior teeth. Once the original fragment is reattached, the natural appearance will be restored instantly.[9] Hence when the tooth's original fragment is used for the reattachment, it is possible to achieve very good esthetics with original tooth contours, texture and radiolucency, and function.[8] Different techniques have been advocated for the fragment reattachment. Some of them are simple reattachment, placement of circumferential bevel at fracture line, placement of external chamfer at fracture line, the use of V-shaped enamel notch, placement of internal groove, and superficial over-contouring of restorative material. To attain isolation for the placement of adhesive resin and to overcome the disadvantages of gingivectomy in esthetic region, intentional replantation has been reported in the literature for managing complicated crown-root fractures.[10,11,12] The prognosis for such treatment may not always be favorable and could vary due to its highly sensitive protocol.[13] It depends on the extra-oral time, handling of the root surface, viability of periodontal ligament cells, and proper maintenance of oral hygiene. Various case reports have been published where a single segment is reattached to the original tooth structure. However, there are no case reports where multiple fragments are reattached in a fragment reattachment procedure with an intentional replantation. In this case report, such an attempt was made to rehabilitate a traumatic dental injury for esthetic reasons with a follow-up period of 2 years.
Case Report
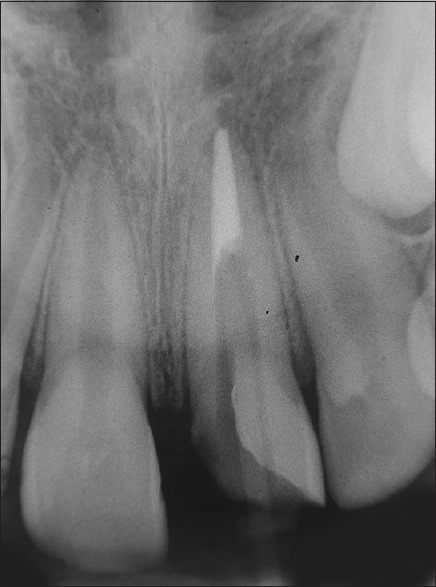
A 12-year-old male patient reported to the Department of Pediatric and Preventive dentistry with a chief complaint of the broken upper front tooth with the broken fragment retrieved by the parent which was stored in the milk until examination. History revealed that the patient had a traumatic fall for1 day before in open ground. On intraoral examination, an oblique complicated crown-root fracture was seen extending into the cementum in the left maxillary central incisor (tooth number: 21) [Figure 1]. The remaining coronal fragment was found to be mobile hanging on to the tooth structure. The patient reported the pain on palpation and percussion. Further examination revealed that there were no injuries to the supporting tissues, lacerations over the lips, or any swelling in and around the region of trauma. Intraoral periapical radiograph revealed two accompanying fracture lines, one extending up to 2 mm into the alveolar crest on the mesial half and the other running from the midline 1 mm into the cementoenamel junction; with a closed apex [Figure 2]. In this case scenario, a regular fragment reattachment procedure would not be possible as there was extensive subgingival involvement. Traditional treatment plan would be extraction, but the patient's parents were not willing for the extraction, and hence, hence, intentional reimplantation with extracoronal fragment reattachment was adviced to the patient and the parent. After obtaining the consent from both the patient and the parents, the treatment was done as follows.
Figure 1.

Preoperative clinical view
Figure 2.

Preoperative radiographic view
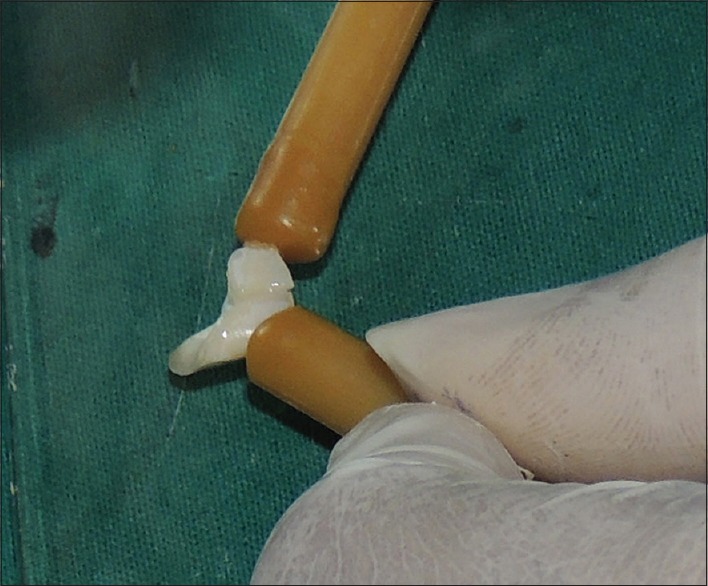
In the first visit, the mobile fragment was removed and stored in isotonic saline solution, till it was reattached. Pulp extirpation was done, and calcium hydroxide closed dressing was given (Calcicur®– VOCO, Germany) followed by the medications. The patient was advised a soft diet and to report after a week. In the second visit, the root canal treatment was done, and the patient was recalled for fiber-reinforced composite post placement after a week. Peeso reamers were used for the post space preparation with up to 6 mm gutta-percha present in the apical region. A fiber-reinforced composite post was placed in the canal space with the help of dual-cure composite resin (Variolink II; Ivoclar Vivadent AG) [Figure 3]. At the same time, the two fractured fragments were cleaned and reattached to form a single segment, and a post space was also prepared using a straight fissure bur number Friction Grip 1157 [Figure 4]. Intraoral reattachment of the united fragments to its tooth structure would be extremely difficult due to the subgingival involvement, and hence, intentional reimplantation was planned, where the tooth segment could be reattached extraorally onto the tooth structure. The tooth was extracted atraumatically under the sterile conditions with very minimal gingival trauma without flap elevation. Care was taken not to handle the root surface to prevent damage to the periodontal ligament fibers. The combined fragment was reattached to the extracted tooth [Figure 5] and then was reimplanted into the socket. Extra-oral dry time was kept as minimal as possible, and the root surface was kept moist by wetting with isotonic saline. A flexible splint using ligature wire and composite was placed for 2 weeks. Postoperative radiograph was taken to verify the correct placement of the tooth in the socket. After removal of the splint, no mobility was noticed. The patient was recalled for monthly follow-ups up to 5 months and every 3 months thereafter. During the 1st-year review, external root resorption was noticed along the coronal third of the root surface, but the tooth was asymptomatic and did not show any signs of mobility [Figures 6 and 7]. During the 2nd-year review, there was no evident difference in the resorption rate compared to the radiograph taken during the 1st-year review, which could suggest to transient resorption that could have been arrested by the 2nd year. The patient was asymptomatic until the end of 2 years [Figures 8 and 9].
Figure 3.
Radiograph to check postplacement
Figure 4.
First fragment reattachment forming a single segment
Figure 5.

Completely reattached tooth after second fragment reattachment
Figure 6.

1st-year postoperative clinical view
Figure 7.

1st-year postoperative radiographic view
Figure 8.

2nd-year postoperative clinical view
Figure 9.

2nd year postoperative radiographic view
Discussion
Various treatment strategies such as removal of the fragment and restoring the tooth with resin composites or full-crown restorations, orthodontic or surgical extrusion of the fragment, and restoration of the tooth were described in the literature including intentional replantation of the crown-root fractured tooth which was preferred for this case.[14] Intentional replantation should be considered as the last-treatment option as there are more chances of periodontal ligament cell loss, but proper care should be taken such that the extra-oral dry time would be kept at the minimum, and preservation of fragments and handling methods of the tooth are probably of crucial importance for maintaining the vitality of periodontal ligament.[15] Intentional replantation with 180° rotation has been used to treat the localized periodontally compromised teeth, such that remaining healthy periodontal ligament contacts the localized lesion area of the socket while the denuded root surface contacts the previously healthy socket areas.[16] In the treatment of crown-root fractures, the rotation was used to expose the fracture line toward the facial side of the tooth for biological space maintenance. In our case report, the tooth was not rotated as it was not periodontally compromised, and there would be intact periodontal ligament fibers and cementum on root surface as the extra-oral dry time was kept to the minimum of 13 min.[17]
Reis et al. have shown that a simple reattachment with no further preparation of the tooth or fragment was able to restore only 37.1% of the intact tooth fracture resistance. Early retrospective studies indicate that the clinical performance of fiber post is promising, and the failure rate is 3.2% over a period of up to 4 years. Use of fiber post in cases of reattachment is that it serves as a splint between the fractured tooth segment and intact tooth, further reinforcing the fractured segment. It helps not only in conservation of tooth structure, good esthetics, and better adhesion but also the stress distribution is better, as the modulus of elasticity is similar to that of dentin.[18] Thus, we planned to place fiber-reinforced post before the fragment reattachment technique. Yilmaz et al.[19] in a clinical follow-up study, reported success for 2 years by using flowable resin composite for the reattachment with a V-shaped external double chamfer on both the fragments. In the present case, a flowable resin composite (Variolink II; Ivoclar Vivadent AG) was used for the reattachment technique.
Fragment reattachment may offer several advantages over the conventional acid etch composite restoration. Improved esthetics is obtained because enamel's original shape, color, brightness, and surface texture are maintained. In addition, the incisal edge will wear at a similar rate to that of the adjacent teeth, whereas composite restoration will likely wear more rapidly. Furthermore, this technique can be less time-consuming and provide more predictable long-term appearance.[20] Although various techniques are available for fragment reattachment, a simple reattachment technique was used in this case report, as it was a less time-consuming and simple procedure, thereby reducing the extra-oral dry time. Keeping the fragments in a moist environment ensured that there is no or minimal collapse of the collagen fibers in the dentin leading to better bond strength. Moreover, it prevents the whitening of the fragment leading to a better esthetic result.[21] Hence, in the present case report, the retrieved tooth fragments were placed in saline until the reattachment procedure was done. Becker and Goultschin reported that slightly elastic properties of the flexible splint material allow the physiological movement of the tooth, and is also noninvasive and reversible in nature.[22] Hence, the splint material of a 0.009 inch was preferred. Trauma could be one of the predisposing factors for cervical resorption of the root surface. According to Heithersay, 15.1% of teeth have trauma as a major predisposing factor, and when the other contributing factors are associated this increases up to 25.7%.[23] The evidence of resorption could be due to traumatic injury which is transient in nature and is not the replacement type.
Treatment plan, in this case, was aimed to maintain the height and thickness of the alveolar ridge until the patient's growth and development ceases and also to provide an immediate esthetic result. Later, alternative replacement techniques such as an implant or bridge can be planned for a better well-functioning and esthetic result.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Arhakis A, Athanasiadou E, Vlachou C. Social and psychological aspects of dental trauma, behavior management of young patients who have suffered dental trauma. Open Dent J. 2017;11:41–7. doi: 10.2174/1874210601711010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schott TC, Engel E, Göz G. Spontaneous re-eruption of a permanent maxillary central incisor after 15 years of ankylosis – A case report. Dent Traumatol. 2012;28:243–6. doi: 10.1111/j.1600-9657.2011.01041.x. [DOI] [PubMed] [Google Scholar]
- 3.Demarco FF, Fay RM, Pinzon LM, Powers JM. Fracture resistance of re-attached coronal fragments-influence of different adhesive materials and bevel preparation. Dent Traumatol. 2004;20:157–63. doi: 10.1111/j.1600-4469.2004.00221.x. [DOI] [PubMed] [Google Scholar]
- 4.Glendor U. Aetiology and risk factors related to traumatic dental injuries – A review of the literature. Dent Traumatol. 2009;25:19–31. doi: 10.1111/j.1600-9657.2008.00694.x. [DOI] [PubMed] [Google Scholar]
- 5.Nikam AP, Kathariya MD, Chopra K, Gupta A, Kathariya R. Knowledge and attitude of parents/caretakers toward management of avulsed tooth in Maharashtrian population: A questionnaire method. J Int Oral Health. 2014;6:1–4. [PMC free article] [PubMed] [Google Scholar]
- 6.Pujita C, Nuvvula S, Shilpa G, Nirmala S, Yamini V. Informative promotional outcome on school teachers' knowledge about emergency management of dental trauma. J Conserv Dent. 2013;16:21–7. doi: 10.4103/0972-0707.105293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma D, Garg S, Sheoran N, Swami S, Singh G. Multidisciplinary approach to the rehabilitation of a tooth with two trauma episodes: Systematic review and report of a case. Dent Traumatol. 2011;27:321–6. doi: 10.1111/j.1600-9657.2011.01006.x. [DOI] [PubMed] [Google Scholar]
- 8.Eden E, Yanar SC, Sönmez S. Reattachment of subgingivally fractured central incisor with an open apex. Dent Traumatol. 2007;23:184–9. doi: 10.1111/j.1600-9657.2005.00408.x. [DOI] [PubMed] [Google Scholar]
- 9.Choudhary A, Garg R, Bhalla A, Khatri RK. Tooth fragment reattachment: An esthetic, biological restoration. J Nat Sci Biol Med. 2015;6:205–7. doi: 10.4103/0976-9668.149123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faghihian R, Eshghi A, Mosleh H, Akhlaghi N. Management of complicated crown-root fracture in central incisors using intentional replantation with 180 rotation: A case report. Dent Hypotheses. 2017;8:113–6. [Google Scholar]
- 11.Kim DS, Shin DR, Choi GW, Park SH, Lee JW, Kim SY, et al. Management of complicated crown-root fractures using intentional replantation: Two case reports. Dent Traumatol. 2013;29:334–7. doi: 10.1111/j.1600-9657.2011.01075.x. [DOI] [PubMed] [Google Scholar]
- 12.Yuan LT, Duan DM, Tan L, Wang XJ, Wu LA. Treatment for a complicated crown-root fracture with intentional replantation: A case report with a 3.5-year follow up. Dent Traumatol. 2013;29:474–8. doi: 10.1111/j.1600-9657.2012.01130.x. [DOI] [PubMed] [Google Scholar]
- 13.Nuvvula S, Mohapatra A, Kiranmayi M, Rekhalakshmi K. Anterior fixed interim prosthesis with natural tooth crown as pontic subsequent to replantation failure. J Conserv Dent. 2011;14:432–5. doi: 10.4103/0972-0707.87220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dogan MC, Akgun EO, Yoldas HO. Adhesive tooth fragment reattachment with intentional replantation: 36-month follow-up. Dent Traumatol. 2013;29:238–42. doi: 10.1111/j.1600-9657.2012.01144.x. [DOI] [PubMed] [Google Scholar]
- 15.DePasquale S, Gatt G, Azzopardi A. Tooth fragment reattachment following crown root fracture: A case report. Dent Update. 2008;35:696–9. doi: 10.12968/denu.2008.35.10.696. [DOI] [PubMed] [Google Scholar]
- 16.Wang J, Li M. Multidisciplinary treatment of a complicated crown-root fracture. Pediatr Dent. 2010;32:250–4. [PubMed] [Google Scholar]
- 17.Cvek M, Granath LE, Hollender L. Treatment of non-vital permanent incisors with calcium hydroxide 3. Variation of occurrence of ankylosis of reimplanted teeth with duration of extra-alveolar period and storage environment. Odontol Revy. 1974;25:43–56. [PubMed] [Google Scholar]
- 18.Geeta IB, Preethi S. Managment of complex crown root fracture using fibre post – A case report. Endodontology. 2014;26:211–6. [Google Scholar]
- 19.Yilmaz Y, Zehir C, Eyuboglu O, Belduz N. Evaluation of success in the reattachment of coronal fractures. Dent Traumatol. 2008;24:151–8. doi: 10.1111/j.1600-9657.2007.00532.x. [DOI] [PubMed] [Google Scholar]
- 20.Reis A, Francci C, Loguercio AD, Carrilho MR, Rodriques Filho LE. Re-attachment of anterior fractured teeth: Fracture strength using different techniques. Oper Dent. 2001;26:287–94. [PubMed] [Google Scholar]
- 21.Sharmin DD, Thomas E. Evaluation of the effect of storage medium on fragment reattachment. Dent Traumatol. 2013;29:99–102. doi: 10.1111/j.1600-9657.2012.01143.x. [DOI] [PubMed] [Google Scholar]
- 22.Becker A, Goultschin J. The multistrand retainer and splint. Am J Orthod. 1984;85:470–4. doi: 10.1016/0002-9416(84)90086-1. [DOI] [PubMed] [Google Scholar]
- 23.Kandalgaonkar SD, Gharat LA, Tupsakhare SD, Gabhane MH. Invasive cervical resorption: A review. J Int Oral Health. 2013;5:124–30. [PMC free article] [PubMed] [Google Scholar]


