Abstract
Background:
The maxillary sinus (MS) is described as a pyramid-shaped cavity of the maxilla.
Aim:
The aim of this research is to present a strategy for morphological analysis of the MS using three-dimensional (3D) printing acquired through cone-beam computed tomography images.
Material and Methods:
A cross-sectional exploratory, single-blind study was conducted, including 24 subjects. MSs were reconstructed, and 3D virtual modeling was done bilaterally, obtaining 48 physical models generated on a 3D printer. The statistical analysis used tests of normality and tests using a value of P < 0.05 to establish statistical significance.
Results:
The mean of the MS volume was 15.38 cm3 (±6.83 cm3). The minimum volume was 5.4 cm3 and the maximum was 30.8 cm3. In a bilateral comparison of the right and left volume of the same individual, there were no significant differences (P = 0.353). In relation to the morphology of the MSs, the most prevalent was pyramidal with a square base with a prevalence of 66.7%. Related to gender, significant differences were observed only for the left volume (P = 0.009), with the mean volume being significantly greater in the men (19.69 cm3) than in the women (12.28 cm3).
Conclusion:
3D printing of the MS permitted the more precise observation of anatomical features that cannot be seen on a 2D screen. A classification is presented that allows an analysis of sinus morphology, although it is necessary to conduct studies with larger samples to obtain more conclusive results.
Keywords: Maxillary sinus, sinus morphology, three-dimensional printing
Introduction
The maxillary sinus (MS) is located within the maxillary body. It is the first sinus to develop;[1] it is the paranasal sinus of greatest volume[1,2] and is generally pyramid-shaped.[2,3] Anatomically, it has six thin bone walls: the superior (associated with the orbital floor), inferior (formed by the alveolar process of the maxilla),[4] lateral, medial (side wall of the nasal cavity), anterior, and posterior (pterygomaxillary region).[1]
At birth, the volume of the MS is from 6 to 8 cm3, and then, it grows with age. It has been reported that its development continues until the third decade in men and the second decade in women, and then, its size begins to decrease.[5] Increases in volume are observed after tooth loss.[3] The high variation in both the normal and abnormal anatomy of the MS and how its morphology is preserved among polyethnic groups continues to be studied.[3]
MSs can vary depending on the individual, the age, and even between the right and left side in the same person.[5,6] Studies of MSs have been done using cadavers,[7] X-rays,[8] computed tomography (CT),[9] magnetic resonance imaging,[10] and cone-beam CT (CBCT);[6] however, a gold standard method to characterize the morphology of the MS has not yet been determined.
A large number of the studies that measure the dimensions of the MS do so through linear morphometry[11,12,13,14] or they calculate the volume of the MS through software that automatically calculates the volume,[5,14,15] which does not allow for the specification of all the irregular anatomical details, which can lead to errors.[16] This is why three-dimensional (3D) printing technology can be useful for these assessments.
3D printing was introduced in the 1980s and can produce physical models directly, in a relatively short time from 3D computer-aided design objects. 3D printers use 3D models created by software based on the CBCT images and generate the final physical model.[17]
The aim of this study is to identify the volume and characterize the morphology of the MS using 3D printing in fully dentate adult subjects.
Materials and Methods
A cross-sectional descriptive, analytical study was designed in participants over 20 years of age with all their teeth in the maxilla and mandible that were included (not including third molars), who presented a CBCT image for the diagnosis and treatment at the Dental Clinic (Commission on Dental Accreditation) at the Universidad de La Frontera. Individuals with injuries affecting the MS (tumors, odontogenic lesions, bone injuries, traumas, and inflammatory lesions) or surgeries in the area and individuals with current or past orthodontic treatment and/or endodontic treatment in any tooth associated with the MS were excluded. Also excluded were CBCT studies that showed metallic devices on the image. This study was approved by the Institutional Science Ethics Committee.
Two dentists were calibrated with 10 CBCT images to accurately recognize the anatomy and the limits of the MSs on the three axes (axial, coronal, and sagittal), first using the Ez3D 2009 program (Vatech, México D.F., Mexico) and then the Slicer 4.4 program (Slicer.org, USA, 2014). In all cases, the CBCT images were captured on the Pax Zenith imaging system (Vatech, Korea, 2011), using 90 kV and 120 mA, FOV 24 cm × 19 cm. The images were exported as Digital Imaging and Communications in Medicine (DICOM) files and were processed as virtual models.
Creation of virtual three-dimensional models of maxillary sinuses
The CBCT data were analyzed on a personal computer by importing the files in DICOM format to the Slicer 4.4 program and identifying the 2D images for the manual delimitation of the MS borders. This method was chosen to increase the accuracy in the anatomical limits due to the inherent irregularity of the MS; thus, errors regarding its shape could be avoided. In each 2D section of the MS (coronal, sagittal, and cross-sectional), the image was filled, eliminating the intrasinus septum and septa. Using another tool of the software, a virtual 3D model of each MS was created based on the previously filled 2D sections in stereolithography format.
Creation of the physical three-dimensional prototype of the maxillary sinus
From the 24 subjects included, 48 virtual models of MSs were exported to the 3D ReplicatorG design software (GNU, USA, 2012), where the MSs were positioned spatially and transferred to × 3 g format to be reconstructed physically on the MBot Grid II 3D printer (Magicfirm MBot3D, China, 2014) using polylactic acid material specific to this type of printer. All the printed models were done on a 1:1 scale. The printing was done by ThermoFusion based on horizontal and vertical lines that form the body of the model to be printed; the thickness of the lines or fibers is adjustable.
Analysis of morphology and volume
The MSs printed were randomized and their morphology was analyzed by two masked and previously calibrated observers. The 24 subjects (48 sinuses) were classified according to their shape in pyramidal with quadrangular base and pyramidal with a triangular base and wing-shaped.
Finally, 48 models of MSs were classified by direct observation of the physical models on a flat surface in a uniform color different from the color of the MSs. The medial wall was considered the base of the MS as it is the most stable in the sinus morphology.
To obtain the volume of the MSs, each model was submerged in a 500 ml graduated flask of precipitate, and its volume was measured using the principle of water displacement for irregular objects. The unit of measurement was cm3.
Data analysis
The data were recorded on a Microsoft Excel® spreadsheet. For the data analysis, the statistical program SPSS Statistics for Windows. (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY, IBM Corp.) was used. To assess the fit of the distributions of the variables to a normal distribution, the Shapiro–Wilk test and ANOVA were performed, and then, Mann–Whitney U- and Kruskal–Wallis tests were applied; also, the Wilcoxon signed-rank test was used to determine if there were differences between the volume of the left and right sinuses in the same individual. When there were significant differences, a multiple comparison analysis was performed using Dunnett's test. In addition, Pearson's Chi-squared test was done to associate qualitative variables. P < 0.05 was chosen to establish statistical significance in the tests used.
Results
The sample comprised 24 individuals, with a mean age of 32.38 years (range: 20–51 years) and a standard deviation (SD) of 8.36. About 54.16% of the sample were female and 45.84% were male.
The mean of the MS volume was 15.38 cm3 and the ± SD was ± 6.83 cm3. The minimum volume was 5.4 cm3 and the maximum volume was 30.8 cm3. For the right volume, the mean was 15.09 ± 7.25 cm3, and for the left volume, the mean was slightly higher at 15.67 ± 6.71 cm3 [Table 1]. In a bilateral comparison between the volume of the right and left sides in the same individual, no significant differences were found using the Wilcoxon signed-rank test (P = 0.353).
Table 1.
Distribution of the 24 subjects included according to the observed volume and gender of the subjects
| Gender | n | Right MS volume (cm3) | Left MS volume (cm3) | Total volume (cm3) | |||
|---|---|---|---|---|---|---|---|
| X̅ ±SD | Mann-Whitney U (P) | X̅ ±SD | t-test (P) | X̅ ±SD | t-test (P) | ||
| Men | 13 | 18.73±8.54 | 0.055 | 19.69±7.39 | 0.009 | 19.21±7.76 | 0.016 |
| Women | 11 | 12.01±4.19 | 12.28±3.69 | 12.15±3.81 | |||
| Total | 24 | 15.09±7.25 | - | 15.67±6.71 | - | 15.38±6.83 | - |
MS: Maxillary sinus; SD: Standard deviation
The normality of the distribution of the volumes of the right and left MSs for men and women was determined using the Shapiro–Wilk test; the variable follows a normal distribution for both men and women, and t-test was applied to compare the volumes of the left MSs, with the average of the left volume being significantly greater in the men (19.69 cm3) than in the women (12.28 cm3) (P = 0.009). Since the variable right volume did not have a normal distribution, the Mann–Whitney U-test was used, and no significant differences were noted in these variables (P = 0.055).
For the shape of the MSs [Table 2], the most prevalent was the pyramid with a quadrangular base [Figure 1] at 66.7%, then the pyramid [Figure 2] shape with a triangular base at 20.8%, and the least prevalent shape was the wing shape at 12.5%. No significant association was found between the variables such as gender and shape of the MS (P = 0.328). On the other hand, using the Kruskal–Wallis test, the age of the individuals did not present a statistically significant relationship (P = 0.069) with any specific shape of the MS.
Table 2.
Distribution of the 24 subjects included according to the shape and observed volume
| Shape | n | Right MS volume (cm3) | Left MS volume (cm3) | Total volume (cm3) | |||
|---|---|---|---|---|---|---|---|
| X̅ ±SD | Kruskal-Wallis (P) | X̅ ±SD | ANOVA (P) | X̅ ±SD | ANOVA (P) | ||
| Pyramid quadrangular base | 16 | 16.85±7.51 | 0.036 | 17.82±6.85 | 0.043 | 17.34±6.99 | 0.062 |
| Pyramid triangular base | 5 | 14.16±5.42 | 13.28±3.91 | 13.72±4.65 | |||
| Wing | 3 | 7.26±1.90 | 8.23±0.90 | 7.75±1.22 | |||
MS: Maxillary sinus; SD: Standard deviation
Figure 1.
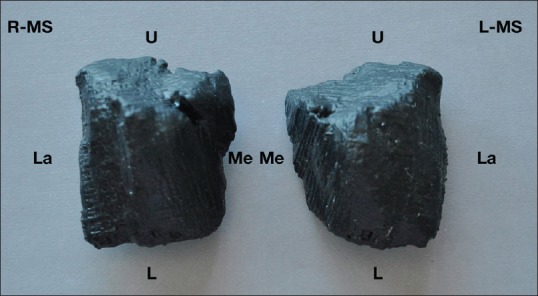
Frontal view of the right and left maxillary sinuses with a quadrangular base. R-MS: Right maxillary sinus, L-MS: Left maxillary sinus, U: Upper area, L: Lower area, La: Lateral area, Me: Medial area
Figure 2.

Frontal view of the right and left maxillary sinuses with a pyramidal base. R-MS: Right maxillary sinus, L-MS: Left maxillary sinus, U: Upper area, L: Lower area, La: Lateral area, Me: Medial area
A comparison of the shape and right volume revealed statistically significant differences (P = 0.036) using the Kruskal–Wallis test. To compare the shape and left volume, an ANOVA was used, with statistically significant differences being observed (P = 0.043). Then, Dunnett's test of multiple comparisons was used, which showed significant differences between the volumes of the pyramid shape with a quadrangular base and the wing shape (P = 0.033).
Discussion
It has been reported that the pattern of MS development shows differences related to individual characteristics such as age and function, even in the same person.[5] It is possible that changes in the sinus morphology appear in life; however, our results show that the age was not related to MS morphology.
Studies have analyzed the morphological characteristics of MSs;[5,6,11,12,13,14] however, the morphology and volume of the MS have not been fully analyzed. The present study produced the 3D model with the Slicer 4.4 software and its subsequent 3D printing, observing the anatomical characteristics directly and overcoming some limitations of the 2D visualizations, which we can only analyze on a flat screen.[17]
Although there are methods to measure the volume virtually with computer programs,[6] the analysis of the volume with a previously developed simple method, similar to the one established in this study, fulfilled the role of relating the morphological aspects of the MS with its volume.
With respect to the volume, Jun et al.[5] reported a mean volume of 24.043 cm3 in men and 15.859 cm3 in women, with these values being higher than those noted in our study (19.21 ± 7.76 cm3 for male and 12.15 ± 3.81 cm3 for female). Furthermore, Kirmeier et al.[15] obtained a mean volume of 21.99 cm3 in a sample comprised only of men between 20 and 30 years, using a semi-automatic volume calculation and also using the software. Differences in the composition characteristics of the sample may justify discrepancies in the volumes observed.
No significant differences were found between the left and right volume of the MSs in the same individual, as in other previous studies;[2,6,9] there were significant differences in the volume of the MSs related to gender, being the male volume (19.69 ± 7.39 cm3) significantly greater than the female volume (12.28 ± 3.69 cm3), but only in the left MSs, in agreement with the results of other studies.[5,9] Amin and Hassan[12] also found significant differences between men and women in the cephalocaudal measurement; however, in other studies, the differences by gender were not significant.[6]
Uthman et al.[11] found that MS height was the best parameter to analyze sexual dimorphism, using only linear morphometry and no volume calculation. They only used 2D measurements for their study, which does not adequately represent the complex anatomy of the MS. Discrepancies in height between men and women may explain the volumetric differences between them.
Although the volume in men was greater than in women, in the right MS, the difference between men and women was not statistically significant. This may be due to the nonparametric statistical tests tending to be less powerful than the parametric tests, which, added to the reduced sample size, increases the likelihood of not detecting statistically significant differences although they exist, increasing the Type II error rate. For example, when the Mann–Whitney U-test was used, P = 0.055 was very close to the established significance value (P = 0.05). With these data, it would be expected that with a larger sample size, with greater power, statistically significant results would be obtained.
Related to morphology, our proposal for classification was based on the direct visual observation of the printed MSs according to their similarity with known figures, being classified into three shapes; the most common was the pyramidal shape, consistent with the literature, noting that some presented a triangular base (20.8%) and others a quadrangular base (66.7%). In addition, MSs were found with physical characteristics consistent with the wing shape (12.5%). As they are irregular spaces, MSs are difficult to classify in regular geometric shapes. Most of the studies reviewed used linear morphometry for their analyses,[11,12,13,14] but this does not represent the real shape of the MS with all its sides, variations, and anatomical details.
This qualitative classification of MSs could be used to orient approaches to the MS, in addition to relating them to their associated volume. Scientific information is limited in these descriptions, developing classifications based on linear morphometry; in our analysis, only one study was obtained that reviewed the morphology of the MS and its relation to age, found through linear measures, which reported an inverted pyramid shape and another hexahedral shape.[5]
In recent decades, 3D printing has been used in a variety of medical applications, including patient care, education, or surgical training;[17] it can also improve and facilitate diagnosis and aid in surgical planning. Its application and benefit in craniofacial and maxillofacial surgery have already been proven.[17,18,19]
3D printing, also known as prototyping, has also been used in medical prostheses and implant design. The potential of this technique lies in the possibility of the design and construction of customized prostheses and the optimization of surgical outcomes because individual adjustment with customized anatomical characteristics would be achieved.[17] Knowing the bone characteristics ahead of time enables improved surgical planning and helps to calculate material and supply requirements, the anesthetic technique to use, and the approximate surgical time.[20]
A big effort has been realized to understand the MS morphology in the past; using this technology, there is a new strategy for new analysis.[20] Clinically, it is important because sinus morphology has been related to complications in procedures such as MS lift in dental implant treatment. Some authors observed a bigger wide in the posterior area of the MS than in the anterior area[21] and other proposed a new classification of the MSs based on morphology, contours and measurements,[22] and finally, other authors[23] showed the anatomy of the MSs as an important matter related to surgical treatment.
Conclusion
In this hand, the measurement of the MS and the study of their anatomy are relevant for surgical approach in clinical dentistry. 3D printing of the MSs through CBCT permits an accurate analysis of the MS anatomy, observing anatomical details that visualization on a 2D screen does not allow. A classification was presented that allows an analysis of sinus morphology, although it is necessary to conduct studies with larger samples to obtain more conclusive results.
Financial support and sponsorship
This work was supported by grant: DI16-0003, Dirección de Investigación Universidad de La Frontera.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This work was supported by grant: DIE18-0006.
References
- 1.Misch CE, Resnik RR, Misch-Dietsh F. Contemporary Implant Dentistry. 38. Barcelona, España: Elsevier Mosby Inc; 2008. Maxillary sinus anatomy, pathology, and graft surgery; pp. 905–74. [Google Scholar]
- 2.Ryu J, Choi SH, Cha JY, Lee KJ, Hwang CJ. Retrospective study of maxillary sinus dimensions and pneumatization in adult patients with an anterior open bite. Am J Orthod Dentofacial Orthop. 2016;150:796–801. doi: 10.1016/j.ajodo.2016.03.032. [DOI] [PubMed] [Google Scholar]
- 3.Lawson W, Patel ZM, Lin FY. The development and pathologic processes that influence maxillary sinus pneumatization. Anat Rec (Hoboken) 2008;291:1554–63. doi: 10.1002/ar.20774. [DOI] [PubMed] [Google Scholar]
- 4.Nimigean V, Nimigean VR, Măru N, Sălăvăstru DI, Bădiţă D, Tuculină MJ, et al. The maxillary sinus floor in the oral implantology. Rom J Morphol Embryol. 2008;49:485–9. [PubMed] [Google Scholar]
- 5.Jun BC, Song SW, Park CS, Lee DH, Cho KJ, Cho JH. The analysis of maxillary sinus aeration according to aging process; volume assessment by 3-dimensional reconstruction by high-resolutional CT scanning. Otolaryngol Head Neck Surg. 2005;132:429–34. doi: 10.1016/j.otohns.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Saccucci M, Cipriani F, Carderi S, Di Carlo G, D’Attilio M, Rodolfino D, et al. Gender assessment through three-dimensional analysis of maxillary sinuses by means of cone beam computed tomography. Eur Rev Med Pharmacol Sci. 2015;19:185–93. [PubMed] [Google Scholar]
- 7.Gosau M, Rink D, Driemel O, Draenert FG. Maxillary sinus anatomy: A cadaveric study with clinical implications. Anat Rec (Hoboken) 2009;292:352–4. doi: 10.1002/ar.20859. [DOI] [PubMed] [Google Scholar]
- 8.Leao de Queiroz C, Terada AS, Dezem TU, Gomes de Araújo L, Galo R, Oliveira-Santos C, et al. Sex determination of adult human maxillary sinuses on panoramic radiographs. Acta Stomatol Croat. 2016;50:215–21. doi: 10.15644/asc50/3/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Emirzeoglu M, Sahin B, Bilgic S, Celebi M, Uzun A. Volumetric evaluation of the paranasal sinuses in normal subjects using computer tomography images: A stereological study. Auris Nasus Larynx. 2007;34:191–5. doi: 10.1016/j.anl.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Rani SU, Rao GV, Kumar DR, Sravya T, Sivaranjani Y, Kumar MP. Age and gender assessment through three-dimensional morphometric analysis of maxillary sinus using magnetic resonance imaging. J Forensic Dent Sci. 2017;9:46. doi: 10.4103/0975-1475.206481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uthman AT, Al-Rawi NH, Al-Naaimi AS, Al-Timimi JF. Evaluation of maxillary sinus dimensions in gender determination using helical CT scanning. J Forensic Sci. 2011;56:403–8. doi: 10.1111/j.1556-4029.2010.01642.x. [DOI] [PubMed] [Google Scholar]
- 12.Amin MF, Hassan EI. Sex identification in Egyptian population using multidetector computed tomography of the maxillary sinus. J Forensic Leg Med. 2012;19:65–9. doi: 10.1016/j.jflm.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Holton N, Yokley T, Butaric L. The morphological interaction between the nasal cavity and maxillary sinuses in living humans. Anat Rec (Hoboken) 2013;296:414–26. doi: 10.1002/ar.22655. [DOI] [PubMed] [Google Scholar]
- 14.Hamdy RM, Abdel-Wahed N. Three-dimensional linear and volumetric analysis of maxillary sinus pneumatization. J Adv Res. 2014;5:387–95. doi: 10.1016/j.jare.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kirmeier R, Arnetzl C, Robl T, Payer M, Lorenzoni M, Jakse N. Reproducibility of volumetric measurements on maxillary sinuses. Int J Oral Maxillofac Surg. 2011;40:195–9. doi: 10.1016/j.ijom.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Alves M, Jr, Baratieri C, Mattos CT, Brunetto D, Fontes Rda C, Santos JR. Is the airway volume being correctly analyzed? Am J Orthod Dentofacial Orthop. 2012;141:657–61. doi: 10.1016/j.ajodo.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Rengier F, Mehndiratta A, von Tengg-Kobligk H, Zechmann CM, Unterhinninghofen R, Kauczor HU, et al. 3D printing based on imaging data: Review of medical applications. Int J Comput Assist Radiol Surg. 2010;5:335–41. doi: 10.1007/s11548-010-0476-x. [DOI] [PubMed] [Google Scholar]
- 18.D’Urso PS, Barker TM, Earwaker WJ, Bruce LJ, Atkinson RL, Lanigan MW, et al. Stereolithographic biomodelling in cranio-maxillofacial surgery: A prospective trial. J Craniomaxillofac Surg. 1999;27:30–7. doi: 10.1016/s1010-5182(99)80007-9. [DOI] [PubMed] [Google Scholar]
- 19.Faber J, Berto PM, Quaresma M. Rapid prototyping as a tool for diagnosis and treatment planning for maxillary canine impaction. Am J Orthod Dentofacial Orthop. 2006;129:583–9. doi: 10.1016/j.ajodo.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 20.De Moraes PH, Costa VO, Olate S, Caria PH, Barbosa JR. Estudio morfométrico del seno maxilar mediante tomografías computadorizadas: Evaluación de la reconstrucción total de piso sinusal. Int J Morphol. 2012;30:592–8. [Google Scholar]
- 21.Chan HL, Suarez F, Monje A, Benavides E, Wang HL. Evaluation of maxillary sinus width on cone-beam computed tomography for sinus augmentation and new sinus classification based on sinus width. Clin Oral Implants Res. 2014;25:647–52. doi: 10.1111/clr.12055. [DOI] [PubMed] [Google Scholar]
- 22.Niu L, Wang J, Yu H, Qiu L. New classification of maxillary sinus contours and its relation to sinus floor elevation surgery. Clin Implant Dent Relat Res. 2018;20:493–500. doi: 10.1111/cid.12606. [DOI] [PubMed] [Google Scholar]
- 23.Keceli HG, Dursun E, Dolgun A, Velasco-Torres M, Karaoglulari S, Ghoreishi R, et al. Evaluation of single tooth loss to maxillary sinus and surrounding bone anatomy with cone-beam computed tomography: A Multicenter study. Implant Dent. 2017;26:690–9. doi: 10.1097/ID.0000000000000652. [DOI] [PubMed] [Google Scholar]


