Abstract
Objective:
The purpose of this study was to evaluate the change in periodontal status of the adjacent second molar of the impacted mandibular third molar after surgical extraction and its association with the third molar condition in the presurgical stages, including position, eruption level, and local complications.
Materials and Methods:
The study was based on a 6-month follow-up of 38 patients (19 males and 19 females; Mean age: 21.89 ± 2.74) recruited consecutively after surgical extraction of an impacted lower third molar. The third molar's presurgical position, eruption level, and local complications were examined. Periodontal status, including Plaque Index (PI), Gingival Index (GI), and gingival bleeding on probing (BOP), of the teeth in the adjacent sextant was clinically evaluated. The pocket depth (PD) and the distance between the epithelial attachment and the adjacent second molar's occlusal surface were clinically measured; and the distance between the alveolar bone crest and cementoenamel junction (AC–CEJ) of the adjacent second molar was evaluated by the periapical film. All measures were recorded at the time of surgery and 1, 3, and 6 months after surgery.
Results:
The values of PI, GI, BOP, PD, and EA–OS were significantly reduced after 1, 3, and 6 months compared to baseline data. The AC–CEJ was decreased after 1 month but significantly increased after 3 and 6 months. Presurgical local complications of the impacted third molar mostly were significantly associated with the periodontal status of the adjacent sextant.
Conclusion:
There was a significant improvement of periodontal conditions of the second molar and adjacent sextant after impacted third molar surgery.
Keywords: Adjacent second molar, impacted mandibular third molar, periodontal status, surgical extraction
Introduction
Like other unerupted or impacted teeth, lower wisdom teeth can affect the rest of the teeth of the arch, jaw, or facial soft tissue, causing tooth decay and periodontitis due to cramping; peritonitis and facial infections due to resident bacteria in the mouth or trauma due to upper third molars; root resorption caused by pressure on the adjacent teeth, tumor and cysts, jaw fractures; or temporomandibular joint disorders.[1,2,3,4,5] These problems can lead to symptoms that seriously affect the patient's quality of life.
Mandibular third molars have been found to be the most commonly impacted teeth, and periodontal diseases are related to impacted third molars.[6] The indications of impacted mandibular third molar surgical extraction to solve and prevent the complications are proposed and widely accepted by the most clinicians.[7] The existing literature has shown conflicting data on the effect of surgical removal of the impacted third molar with varying outcomes on the periodontal health of the adjacent sextant or second molar. The previous studies have focused on the effect of impacted mandibular third molar removal on the periodontal status of the adjacent teeth. Some studies suggest that early extraction of impacted mandibular third molars has a positive effect on the health of periodontal tissue distal to the second molars and adjacent sextant teeth.[1,7,8,9,10] In contrast, several other studies conclude that mandibular third molar extraction can cause periodontal tissue defects in the distal root of the adjacent second molar, reduce the alveolar bone height, increase the loss of attachment, and increase the periodontal pocket depth (PD) in the distal aspect of this tooth.[11,12] However, a little research has been conducted to study the effect of factors such as the age of the patient, position, eruption level, and presurgery complications of the third molar on the periodontal condition of the adjacent sextant after surgery.
To better understand, the change in periodontal condition of the second molar and adjacent teeth after mandibular third molar surgical extraction, we conducted this study to evaluate the changes in the periodontal status, including the Plaque Index (PI); Gingival Index (GI); gingival bleeding on probing (BOP) of the teeth of the adjacent sextant; periodontal PD; distance from the junctional epithelium to the occlusal surface (JE–OS); distance from the alveolar bone crest to the cementoenamel junction (AC–CEJ) of the adjacent second molar; effects of the factors of age, position, eruption level of the third molar; and complications before surgery on the periodontal condition of the adjacent sextant teeth 1, 3, and 6 months after surgery.
Materials and Methods
The convenience sample comprised 62 patients, who were indicated for and requested lower third molar extraction surgery at the Department of Oral Surgery, Faculty of Odonto-Stomatology, HCMC University of Medicine and Pharmacy, in 2014. Participants were provided information regarding the risks and benefits of the study and written informed consent was obtained. The protocol of this study was approved by the Ethics Committee of the University of Medicine and Pharmacy, Ho Chi Minh City, Vietnam (Reference number: 40/ĐHYD-HĐ). Inclusion criteria: patients had to be aged 18 years or older, in good health, not using drugs that affect bleeding and wound healing after surgery, and presenting a mesially inclined impacted mandibular third molar characterized by the angle of the lines through occlusal surfaces of the third molar and the adjacent second molar ranging from 30° to 90°. Exclusion criteria: patients who were being treated for periodontal disease during the study period, pregnant or breastfeeding, or not compliant with regularly scheduled follow-up appointments were excluded from the study. Twenty-four of the 62 patients did not complete the treatment procedures; thus, 38 (19 males and 19 females), aged 18–30 years (the average age 21.89 ± 2.74) was the final number of patients in this study.
Before surgery
Clinical examination and history revealed complications of swelling or pain in the third molar, requiring extraction and the third molar eruption condition (”erupted” or “unerupted”) by recording the presence of the third molar in the mouth. Periapical radiographs were taken to evaluate the third molar position according to Pell and Gregory's classification and categorized into Class I, Class II, or Class III (mandibular ramus-related depth), as well as type A, type B, or type C (relative depth to the occlusal surface of the second molar). Classes I, II, and III are determined when the distance between the anterior border of the ramus and the distal aspect of the second molar is adequate for, smaller than, or completely unavailable for the mesiodistal width of the third molar, respectively. Type A means the uppermost aspect of the third molar is at the same level as or higher than the occlusal surface of the second molar. Type B means the uppermost aspect of the third molar is apical to the occlusal surface, but coronal to the cervical line of the second molar. Type C means the uppermost part of the third molar is apical to the cervical line of the second molar.[13] The third molar is scored according to Montero as follows: class I and Type A is scored 0, Class II and Type B is scored 1, and Class III and Type C is scored 2.[7] The score of the third molar is the sum of scores in both relationships, and the position of the third molar is classified as “superficial third molar” with a score ≤1 and “deep third molar” with a score ≥2.
Examination of periodontal status
The periodontal parameters of all patients were examined at baseline, 1, 3, and 6 months after surgery by one dentist who was not the surgeon in the study. The PI, GI, and BOP of the teeth in the adjacent sextant to the third molar needing extraction and the PD, EA–OS, and AC–CEJ of the adjacent second molar to the third molar needing extraction were examined. The PI and GI at distobuccal, distolingual, midbuccal, and midlingual sites of the teeth in the sextant adjacent to the third molar needing extraction were examined.[14] The highest PI and GI values for each tooth in the sextant were recorded. The percentage of the sites with BOP was examined at distobuccal, distolingual, midbuccal, and midlingual sites of the teeth in the sextant adjacent to the third molar and calculated as %BOP = (the number of bleeding sites on probing × 100)/total examined sites. PD of the adjacent second molar was recorded as the measurement of the distance from the gingival margin to the depth of the periodontal pocket at the distobuccal, distolingual, midbuccal, and midlingual sites of the adjacent second molar using a UNC periodontal probe. The distance between the epithelial attachment and the adjacent second molar's occlusal surface (EA–OS) was measured from the upper border of the individual biting lock (with small grooves that have been drilled at the distobuccal, distolingual, midbuccal, and midlingual sites) to the depth of the periodontal pocket on the adjacent second molar. The distance between the AC–CEJ of the adjacent second molar was recorded by parallel periapical radiographic technique, standardized by the utilization of a film-holding device and individual biting lock, combined with a tracing and measurement method on paper, which is specifically used for orthodontics and superimposition of periapical radiographs [Figures 1–3].
Figure 1.
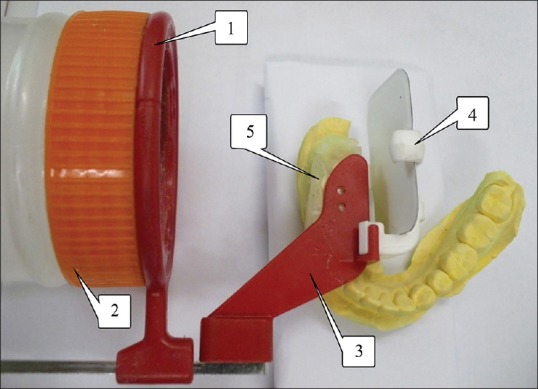
Modified film-holding device. 1: Positioning ring; 2: Additional plastic cylinder; 3: Arm; 4: Film-holding device; 5: Individualized occlusal index
Figure 3.
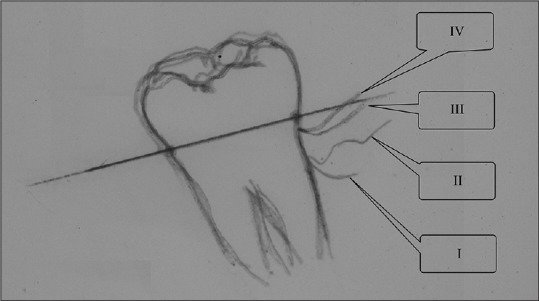
Periapical radiograph superimposition. I: At baseline, II: 1 month, III: 3 months, IV: 6 months after surgery
Figure 2.
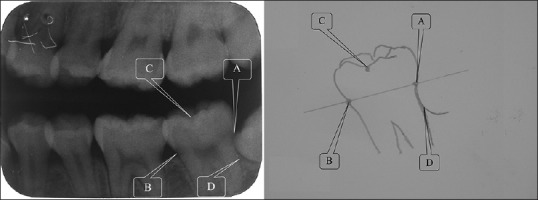
Periapical radiographic tracing. A: Distal cementoenamel junction; B: Mesial cementoenamel junction; C: Buccal groove of the second adjacent molar; D: Intersection of the distal alveolar crest and distal outline of the adjacent second molar
During surgery
All patients in the study received the same standard surgical technique performed by the same surgeon. Patients were under local anesthesia, generally with lidocaine in a 2% solution with adrenaline at 1:100,000 (Lignospan standard, Septodont, France). The surgical field and all surgical materials were sterile. After incision with a no. 15 scalpel blade, the soft tissue was displaced to expose the surgical area. Subsequently, the soft tissue was withdrawn and low-speed osteotomy was conducted with cylinder burs (no. 703, Dentsply) mounted on a handpiece device (20,000 rpm). The osteotomy and odontosection procedures were performed under constant irrigation with sterile sodium chloride solution (0.9%). The extraction was then performed using straight elevators and/or curved elevators, careful curettage, bone regularization, and surgical cleansing, with abundant irrigation. The suture was made using Black Silk 3.0 (CPT Sutures Co. Ltd, Vietnam) and isolated points. The suture was removed after 7 days. After the operation, the patients were given the same prescription, including an antibiotic (amoxicillin 500 mg, 1.5 g/day for 5 days), an anti-inflammatory agent (diclofenac 500 mg, 1.5 g/day for 3 days), and an analgesic (paracetamol 50 mg, 1.5 g/day for 3 days). All postoperative instructions were explained to the patients by one dentist and were also printed on a paper sheet that was given to the patients. All patients were asked to perform their regular oral hygiene care, except in the region of the surgical wound, 1 day after surgery. These instructions for oral hygiene were also repeated in each of the follow-up visits.
After surgery
After 7 days, the suture was removed. The patients were asked to schedule a follow-up visit at 1, 3, and 6 months after surgery. At each follow-up visit, the patients were examined; the PI, GI, BOP, PD, and JE–OS were recorded; and a radiograph of the AC–CEJ was taken by the same dentist.
Statistical analyses
Recorded data were inputted and analyzed by SPSS version 22 software (SPSS Japan, Tokyo, Japan) using repeated-measures ANOVA test, independent t, and Mann–Whitney tests. The tests were statistically significant when P < 0.05.
Results
Subjects and third molar condition at presurgery
The sample comprised 38 patients (19 males and 19 females) aged 18–30 years (Mean: 21.89 ± 2.74). Twenty-four (63.2%) patients had local complications and 14 (36.8%) had no local complications. Among 38 third molars, 22 had erupted (57.9%) and 16 were unerupted (42.1%). The percentage of superficial third molars was 60.5% (23 teeth) and deep third molars 39.5% (15 teeth).
The change in periodontal status of the adjacent sextant
The periodontal status, including the PI, GI, and BOP of the teeth of the adjacent sextant and the PD, EA–OS, and AC–CEJ of the adjacent second molar of the third molar extracted at baseline and 1, 3, and 6 months after surgery, is presented in Table 1.
Table 1.
The periodontal status of the adjacent sextant at baseline and 1, 3, and 6 months after surgery
| Parameters | Baseline | 1 month after surgery | 3 months after surgery | 6 months after surgery | P |
|---|---|---|---|---|---|
| PIa | 1.47±0.69 | 1.05±0.53 | 0.73±0.38 | 0.51±0.21 | <0.001 |
| GIa | 1.43±0.61 | 0.92±0.43 | 0.74±0.36 | 0.47±1.21 | <0.001 |
| BOPb | 28.62 | 14.31 | 5.76 | 2.14 | <0.001 |
| PDb | 3.05±0.70 | 2.72±0.39 | 2.47±0.42 | 2.09±0.35 | <0.001 |
| EA-OSb | 13.26±0.91 | 12.89±0.71 | 12.66±0.69 | 12.15±0.55 | <0.001 |
| AC-CEJb | 3.65±1.15 | 3.92±1.12 | 3.26±0.88 | 2.83±0.82 | <0.001 |
PI, GI, and BOP for the teeth in the sextant adjacent to the third molar needing extraction; PD, EA–OS, and AC–CEJ for the second molar adjacent to the third molar needing extraction; repeated-measures ANOVA test, significance at P<0.05. PI: Plaque Index; GI: Gingival Index; BOP: Bleeding on probing; PD: Pocket depth; AC–CEJ: Alveolar bone crest and cementoenamel junction; EA–OS: Epithelial attachment and the adjacent second molar’s occlusal surface
The PI decreased statistically significantly from baseline (1.47 ± 0.69) to 1 month (1.05 ± 0.53), 3 months (0.73 ± 0.38), and 6 months (0.51 ± 0.21) after surgery. Similarly, the GI decreased statistically significantly from baseline (1.43 ± 0.61) to 1 month (0.92 ± 0.43), 3 months (0.74 ± 0.36), and 6 months (0.47 ± 1.21) after surgery. The BOP decreased statistically significantly from 28.62% (baseline) to 14.31% (1 month), 5.76% (3 months), and 2.14% (6 months).
The PD of the adjacent tooth decreased statistically significantly from baseline (3.05 ± 0.70 mm) to 1 month (2.72 ± 0.39 mm), 3 months (2.47 ± 0.42 mm), and 6 months (2.09 ± 0.35 mm). The EA–OS of the adjacent tooth decreased statistically significantly from baseline (13.26 ± 0.91 mm) to 1 month (12.89 ± 0.71 mm), 3 months (12.66 ± 0.69 mm), and 6 months (12.15 ± 0.55 mm). These indices decreased statistically significantly from baseline to 1 month after surgery, from 1 month after surgery to 3 months after surgery, and from 3 months after surgery to 6 months after surgery (P < 0.05). However, the AC–CEJ of the adjacent tooth statistically significantly increased from 3.65 ± 1.15 mm (baseline) to 3.92 ± 1.12 mm (1 month after surgery) (P < 0.001). At both 3 and 6 months after surgery, the AC–CEJ statistically significantly decreased to 3.26 ± 0.88 mm and 2.83 ± 0.82 mm, respectively (P < 0.001).
Effects of third molar condition at presurgery on periodontal status of the adjacent sextant
Impacted third molar position
The effects of the position of the third molar needing extraction on periodontal status at baseline and 1, 3, and 6 months after surgery are presented in Table 2. Before surgery, there was no statistically significant difference in the PI, GI, BOP, and PD between the superficial and deep third molar groups, but two groups had a statistically significant difference in the JE–OS at 1 month and 3 months after surgery (P < 0.05). The 1, 3, and 6 months after surgery PI, GI, BOP, and PD between the two groups were different, but without statistical significance. In contrast, superficial third molars had a statistically significantly lower AC–CEJ than deep third molars (P < 0.001).
Table 2.
The effects of the impacted third molar position on the periodontal status of the adjacent sextant at baseline and 1, 3, and 6 months after surgery
| Baseline | 1 month after surgery | 3 months after surgery | 6 months after surgery | |||||
|---|---|---|---|---|---|---|---|---|
| Superficial | Deep | Superficial | Deep | Superficial | Deep | Superficial | Deep | |
| PIa | 1.50±0.65 | 1.43±0.76 | 1.12±0.46 | 0.95±0.63 | 0.78±0.38 | 0.65±0.40 | 0.55±0.21 | 0.43±0.19 |
| GIa | 1.44±0.53 | 1.42±0.72 | 0.98±0.349 | 0.83±0.53 | 0.76±0.35 | 0.70±0.38 | 0.43±0.23 | 0.52±0.39 |
| BOPb | 30.71±23.15 | 25.42±30.57 | 15.22±15.97 | 12.92±21.19 | 5.16±8.35 | 6.67±9.87 | 1.36±3.24 | 3.33±7.03 |
| PDb | 3.01±0.68 | 3.12±0.74 | 2.65±0.40 | 2.83±0.36 | 2.49±0.37 | 2.45±0.50 | 2.07±0.29 | 2.12±0.42 |
| EA-OSb | 13.11±0.77 | 13.50±1.08 | 12.65±0.60 | 13.25±0.73** | 12.47±0.57 | 12.95±0.79*** | 12.09±0.48 | 12.55±0.64 |
| AC-CEJb | 3.08±0.88 | 4.51±1.06* | 3.30±0.81 | 4.87±0.84* | 2.82±0.75 | 3.93±0.59* | 2.45±0.69 | 3.39±0.67* |
PI, GI, and BOP for the teeth in the sextant adjacent to the third molar needing extraction; PD, JE–OS, and AC–CEJ for the second molar adjacent to the third molar needing extraction. at-test, bMann-Whitney test; significance at P<0.05, *P≤0.001, **P≤0.01, and ***P<0.05. PI: Plaque Index; GI: Gingival Index; BOP: Bleeding on probing; PD: Pocket depth; AC–CEJ: Alveolar bone crest and cementoenamel junction; EA–OS: Epithelial attachment and the adjacent second molar’s occlusal surface
Impacted third molar eruption level
The effects of eruption level on periodontal status at baseline and 1, 3, and 6 months after surgery are presented in Table 3. There are no statistically significant differences between the two groups in any of the indices. At the 1-month reexamination, both the erupted and unerupted teeth groups showed virtually no statistically significant changes. However, the BOP index of the erupted group was statistically higher than of the unerupted group; in the erupted third molars group, the AC–CEJ was significantly lower than in the other group (P < 0.01). At both 3 and 6 months after surgery, a significantly greater PI was observed in the erupted third molars group (P < 0.05). In contrast, the AC–CEJ of the erupted group was lower than of the unerupted group (P < 0.05). There were statistically significant changes in the remaining indices of the two groups.
Table 3.
The effects of eruption level of the impacted third molar on periodontal status of the adjacent sextant at baseline and 1, 3, and 6 months after surgery
| Baseline | 1 month after surgery | 3 months after surgery | 6 months after surgery | |||||
|---|---|---|---|---|---|---|---|---|
| Erupted | Unerupted | Erupted | Unerupted | Erupted | Unerupted | Erupted | Unerupted | |
| PIa | 1.65±0.68 | 1.23±0.65 | 1.19±0.44 | 0.86±0.59 | 0.85±0.38 | 0.56±0.34* | 0.57±0.22 | 0.42±0.18* |
| GIa | 1.56±0.56 | 1.27±0.64 | 1.03±0.34 | 0.77±0.49 | 0.82±0.35 | 0.63±0.35 | 0.47±0.28 | 0.47±0.34 |
| BOPb | 34.38±24.61 | 20.70±26.69 | 17.33±17.14 | 10.16±18.80*** | 5.97±8.51 | 5.47±9.65 | 1.99±4.04 | 2.34±6.40 |
| PDb | 3.17±0.70 | 2.89±0.69 | 2.77±0.34 | 2.66±0.46 | 2.56±0.41 | 2.36±0.43 | 2.14±0.33 | 2.02±0.37 |
| EA-OSb | 13.27±0.94 | 13.25±0.89 | 12.80±0.73 | 13.02±0.68 | 12.57±0.74 | 12.78±0.64 | 12.17±0.63 | 12.13±0.42 |
| AC-CEJb | 3.35±0.89 | 4.06±1.35 | 3.52±0.94 | 4.48±1.14** | 2.95±0.81 | 3.68±0.81** | 2.59±0.77 | 3.15±0.79*** |
PI, GI, and BOP for the teeth in the adjacent sextant to the third molar needing extraction; PD, JE-OS, and AC-CEJ for the second molar adjacent to the third molar needing extraction; at-test, bMann-Whitney test; significance at P<0.05, *P≤0.001, **P≤0.01, and ***P<0.05. PI: Plaque Index; GI: Gingival Index; BOP: Bleeding on probing; PD: Pocket depth; AC-CEJ: Alveolar bone crest and cementoenamel junction; JE-OS: Junctional epithelium to the occlusal surface; EA-OS: Epithelial attachment and the adjacent second molar’s occlusal surface
Complications of the impacted third molar
The effects of complications of third molars needing extraction on periodontal status at baseline and 1, 3, and 6 months after surgery are presented in Table 4. At baseline and 1, 3, and 6 months after surgery, the PI, GI, BOP, PD, and EA–OS indices in the complicated group were statistically significantly higher than in the uncomplicated group (P < 0.05). In comparison to baseline and 1 month after surgery, the AC–CEJ between the two groups were different, but without statistical significance. At both 3 and 6 months after surgery, the AC–CEJ was higher in the complicated group than in the uncomplicated group, with statistical significance.
Table 4.
Effect of complications of the impacted third molar on periodontal status of the adjacent sextant at baseline and 1, 3, and 6 months after surgery
| Baseline | 1 month after surgery | 3 months after surgery | 6 months after surgery | |||||
|---|---|---|---|---|---|---|---|---|
| Complication (+) | Complication (−) | Complication (+) | Complication (−) | Complication (+) | Complication (−) | Complication (+) | Complication (−) | |
| PIa | 1.81±0.64 | 0.89±0.21* | 1.28±0.52 | 0.66±0.27* | 0.86±0.42 | 0.50±0.14* | 0.56±0.24 | 0.41±0.12** |
| GIa | 1.76±0.49 | 0.88±0.31* | 1.09±0.42 | 0.63±0.24* | 0.87±0.37 | 0.50±0.17* | 0.57±0.33 | 0.28±0.13* |
| BOPb | 42.71±22.47 | 4.46±6.68* | 19.27±16.16 | 5.80±18.26*** | 9.75±1.99 | 0.0* | 6.11±1.25 | 0.0** |
| PDb | 3.26±0.74 | 2.70±0.45** | 2.84±0.34 | 2.52±0.40** | 2.67±2.28 | 2.14±0.42* | 2.21±0.31 | 1.88±0.31** |
| EA-OSb | 13.57±0.84 | 12.73±0.79** | 13.06±0.70 | 12.59±0.65*** | 12.88±0.64 | 12.29±0.65** | 12.34±0.49 | 11.82±0.49** |
| AC-CEJb | 3.76±0.89 | 3.44±1.51 | 4.00±0.93 | 3.78±1.42 | 3.51±0.81 | 2.82±0.85*** | 3.08±0.75 | 2.39±0.77*** |
PI, GI, and BOP for the teeth in the adjacent sextant to the third molar needing extraction; PD, EA–OS, and AC-CEJ for the second molar adjacent to the third molar needing extraction. at–test, bMann-Whitney test; significance at P<0.05, *P≤0.001, **P≤0.01, and ***P<0.05. PI: Plaque Index; GI: Gingival Index; BOP: Bleeding on probing; PD: Pocket depth; AC–CEJ: Alveolar bone crest and cementoenamel junction; EA–OS: Epithelial attachment and the adjacent second molar’s occlusal surface
Discussion
In this study, the patients were selected with the criterion of impaction of the lower third molar, 30°–90° mesially inclined. By such selection, we hoped to limit the scope of the survey on patients with lower third molars at high risk for untoward complications. Our research found an improvement in the PI, GI, and BOP of the adjacent sextant from baseline to 1, 3, and 6 months after surgery. Many studies also obtained results similar to ours.[1] Blakey et al. concluded that removal of the lower third molar significantly improves the periodontal status of the distal aspect of the adjacent second molars, and also has a positive impact on the overall periodontal status.[1] Montero and Mazzaglia concluded that there is a gradual improvement of the PI and GI from baseline to 1 year after surgery.[7] Krausz et al. assessed the presence of plaque on the distal surface of the second molar 28 months after extraction of the impacted third molar.[15] They found a significant decrease in the PI when compared with the control group. However, our study differed from Kirtiloǧlu et al.[16] and Stella et al.,[17] who reported an increased PI after extraction. The different assessments of the PI and different follow-up periods were believed to have led to the disparate findings. We assessed the PI of the adjacent sextant for 6 months, whereas Kirtiloǧlu et al.[16] assessed the distal surface of the second molar for 12 months, and Stella et al.[17] assessed all teeth of the entire oral cavity for 6 months.
In this study, we measured the PD and EA–OS of the adjacent second molar with an individual occlusal bit. The improvement of the PD may not be significant in cases of gum recession, especially when the distant site of the adjacent second molar appears. Thus, EA–OS measurement gave more precise results of the position of the epithelial attachment after surgery. Our results showed an improvement in the PD and EA–OS of the adjacent second molars from baseline to 1, 3, and 6 months after surgery. Our results were similar to those found by Stella et al., where a significant reduction in probing depth was recorded for the adjacent second molar 180 days after surgery.[17] Montero and Mazzaglia also showed a gradual but significant improvement of PD from baseline and 1 year after surgery, and this improvement was much higher in adjacent second molars than the mean value recorded in four-posterior sextants.[7] Several authors have reported that food particles in areas that are difficult to clean between the impacted mandibular tooth and adjacent second molar can lead to inflammation and alterations in the gingival tissue around the third molar and sextant.[18,19] This could explain the improvement in the probing depth after extraction of the impacted third molar. However, Wong et al. concluded that there was no change with statistical significance in the PD and the clinical attachment level at three points in the distal aspect (buccodistal, linguobuccal, and mid-distal) on the adjacent second molars before and after extraction of the impacted third molar.[20] The difference in the study results may be due to different sampling methods. The results from our study are opposite those of Peng et al. and Kan et al.[11,21] These authors examined the second molars for more than 6 months after extraction of the impacted third molar, using the contralateral tooth as the control group, while these teeth cannot represent the real change in terms of periodontal PD and clinical attachment level.
Our research shows that the AC–CEJ of the adjacent second molars at 1 month after surgery slightly increased compared to baseline. This could be a result of the drilling operation of the buccal bone of the third molar, as a part of the alveolar bone crest at this location was lost. From 1 month after surgery to 3 and 6 months after surgery, the AC–CEJ gradually decreased. This can be explained by the inflammation caused by the impacted third molar before surgery, which caused mineral loss and made the bone structure more radiolucent, resulting in deficiencies on radiographs. At 3 and 6 months after surgery, the inflammation on the adjacent second molar was eliminated, and there was healing and remineralization of the bone structure; making the bone crest more radiopaque and thus resulting in improved alveolar bone crest height on the radiographs at 3 and 6 months after surgery. Future histologic studies need to be conducted to verify this conclusion. The results of our study agree with Krausz et al., who reported that lower third molar extraction significantly increased the bone height on the distal aspect of the adjacent second molar on the test side, and a mild degree of bone loss was recorded on the control side.[15] Some researchers argued that there are no statistically significant changes of alveolar bone height in the distal aspect of the adjacent second molar after third molar surgical extraction.[20,22,23] Peng et al. suggest that there is a significant alveolar bone loss on the distal aspect of the adjacent second molar on radiographs more than 5 years after surgery.[11] The difference between the results of the studies may be due not only to differences in the sampling and research designs but also to the differences of survey methods and measurement of alveolar bone height.
Many researchers around the world believe that the position of the third molar is one of the main factors affecting the periodontal status before and after surgery.[7,9] However, our study did not find a statistically significant difference between the two groups of superficial and deep third molars in terms of PI, GI, and BOP at baseline and 1, 3, and 6 months after surgery. This difference may be because the majority of the third molars in our study were erupted (Ages: 18–25), so the period of existence of the third molar is too short to affect the chewing habits and oral hygiene of the patient and to have long-term effects on the surrounding periodontal tissues. The AC–CEJ value in the deep third molar group was statistically significantly higher than in the superficial teeth at baseline and 1, 3, and 6 months after surgery. This may be because deeper third molars occupy more space and reduce the amount of bone in the distal aspect of the adjacent second molar more than the superficial third molar. Moreover, during surgery, the surgeon reflected a larger flap for the deep third molar and/or cut more bone so that the alveolar bone and junctional epithelium on the distal aspect of the adjacent second molar were affected more in the deep third molars than in the superficial ones. This can make the AC–CEJ in the deep third molar group statistically significantly higher than in the superficial third molar group at baseline and 1 month and 3 months after surgery. In the study by Stella et al., the findings showed that the PD of the adjacent second molar was also lower when the third molar was Class II or Type A.[17] The authors also explained that the position of the third molar in Class II and Type A could lead to better postoperative healing because it is located just below a gingival layer and in front of the mandibular ramus.
We found that the PI, GI, BOP, PD, and EA–OS in the erupted third molar group were higher than in the unerupted-third molar group at baseline and 1, 3, and 6 months after surgery. However, the differences are not statistically significant. The results also showed a somewhat negative effect of the presence of the third molar on periodontal health. Our results also agree with the several other authors. Kaveri and Prakash suggested that just the presence of third molars has shown a negative impact on periodontal health.[24] White et al. reported that people with an erupted third molar more likely to have a greater periodontal probing depth in general, particularly in the second molar, and a level of clinical attachment loss greater than in those whose third molar has not erupted.[25] Our research results showed that all periodontal parameters improved after surgery in both the complicated and uncomplicated groups. The improvement in periodontal status in the uncomplicated group is statistically significantly higher than in the complicated group at baseline and 1, 3, and 6 months after surgery. Similar results were reported by Gröndahl and Lekholm.[23] Furthermore, Kugelberg suggests that when the need for third molar extraction arises, early extractions when there are no complications will have beneficial effects on the periodontal status of the adjacent second molar.[22] However, the results of our study differ from those of some other studies. Some researchers suggested that the periodontal status of the adjacent second molars neither improved nor worsened after third molar extraction, even in patients without complications before the surgery.[12,26,27]
This study has some limitations. We investigated the 6-month follow-up of changes in periodontal status of the adjacent sextant after impacted mandibular third molar surgical extraction in a group of students. Different types of impacted mandibular third molars and/or different populations may have different outcomes. Future research involving longer-term evaluation of periodontal outcomes, different types of tooth impaction, and different populations is needed. A small sample size and the absence of a control group for the comparison of results are also other limitations of this research.
This study found that there is improvement in the periodontal status of the adjacent second molars and sextant after third molar extraction surgery. Presurgical local complications of the impacted third molar mostly were significantly associated with the periodontal status of the adjacent sextant. This research suggests that patients should undergo third molar extraction before complications appear. Radiographs of the third molars should be obtained to verify the level of the third molar in relation to the second molar because some angulation positions are more unfavorable for the maintenance of dental and periodontal health, which is necessary to prevent dental caries and periodontal diseases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Blakey GH, Parker DW, Hull DJ, White RP, Jr, Offenbacher S, Phillips C, et al. Impact of removal of asymptomatic third molars on periodontal pathology. J Oral Maxillofac Surg. 2009;67:245–50. doi: 10.1016/j.joms.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 2.Hazza'a AM, Batained AB, Odat AA. Angulation of mandibular third molars as a predictive factor of Pericoronitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;10:51–8. [PubMed] [Google Scholar]
- 3.Miloro M, DaBell J. Radiographic proximity of the mandibular third molar to the inferior alveolar canal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:545–9. doi: 10.1016/j.tripleo.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 4.Ozeç I, Hergüner Siso S, Taşdemir U, Ezirganli S, Göktolga G. Prevalence and factors affecting the formation of second molar distal caries in a Turkish population. Int J Oral Maxillofac Surg. 2009;38:1279–82. doi: 10.1016/j.ijom.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Yamalik K, Bozkaya S. The predictivity of mandibular third molar position as a risk indicator for pericoronitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;12:9–14. doi: 10.1007/s00784-007-0131-2. [DOI] [PubMed] [Google Scholar]
- 6.Chu FC, Li TK, Lui VK, Newsome PR, Chow RL, Cheung LK. Prevalence of impacted teeth and associated pathologies – A radiographic study of the Hong Kong Chinese population. Hong Kong Med J. 2003;9:158–63. [PubMed] [Google Scholar]
- 7.Montero J, Mazzaglia G. Effect of removing an impacted mandibular third molar on the periodontal status of the mandibular second molar. J Oral Maxillofac Surg. 2011;69:2691–7. doi: 10.1016/j.joms.2011.06.205. [DOI] [PubMed] [Google Scholar]
- 8.Kugelberg CF, Ahlström U, Ericson S, Hugoson A. Periodontal healing after impacted lower third molar surgery. A retrospective study. Int J Oral Surg. 1985;14:29–40. doi: 10.1016/s0300-9785(85)80007-7. [DOI] [PubMed] [Google Scholar]
- 9.Kugelberg CF, Ahlström U, Ericson S, Hugoson A, Kvint S. Periodontal healing after impacted lower third molar surgery in adolescents and adults. A prospective study. Int J Oral Maxillofac Surg. 1991;20:18–24. doi: 10.1016/s0901-5027(05)80689-7. [DOI] [PubMed] [Google Scholar]
- 10.Leung WK, Corbet EF, Kan KW, Lo EC, Liu JK. A regimen of systematic periodontal care after removal of impacted mandibular third molars manages periodontal pockets associated with the mandibular second molars. J Clin Periodontol. 2005;32:725–31. doi: 10.1111/j.1600-051X.2005.00773.x. [DOI] [PubMed] [Google Scholar]
- 11.Peng KY, Tseng YC, Shen EC, Chiu SC, Fu E, Huang YW. Mandibular second molar periodontal status after third molar extraction. J Periodontol. 2001;72:1647–51. doi: 10.1902/jop.2001.72.12.1647. [DOI] [PubMed] [Google Scholar]
- 12.Richardson DT, Dodson TB. Risk of periodontal defects after third molar surgery: An exercise in evidence-based clinical decision-making. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:133–7. doi: 10.1016/j.tripleo.2005.02.063. [DOI] [PubMed] [Google Scholar]
- 13.Pell GJ, Gregory BT. Impacted mandibular third molars: Classification and modified techniques for removal. Dent Dig. 1933;39:330–8. [Google Scholar]
- 14.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(Suppl 6):610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 15.Krausz AA, Machtei EE, Peled M. Effects of lower third molar extraction on attachment level and alveolar bone height of the adjacent second molar. Int J Oral Maxillofac Surg. 2005;34:756–60. doi: 10.1016/j.ijom.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Kirtiloǧlu T, Bulut E, Sümer M, Cengiz I. Comparison of 2 flap designs in the periodontal healing of second molars after fully impacted mandibular third molar extractions. J Oral Maxillofac Surg. 2007;65:2206–10. doi: 10.1016/j.joms.2006.11.029. [DOI] [PubMed] [Google Scholar]
- 17.Stella PE, Falci SG, Oliveira de Medeiros LE, Douglas-de-Oliveira DW, Gonçalves PF, Flecha OD, et al. Impact of mandibular third molar extraction in the second molar periodontal status: A prospective study. J Indian Soc Periodontol. 2017;21:285–90. doi: 10.4103/jisp.jisp_79_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blakey GH, Jacks MT, Offenbacher S, Nance PE, Phillips C, Haug RH, et al. Progression of periodontal disease in the second/third molar region in subjects with asymptomatic third molars. J Oral Maxillofac Surg. 2006;64:189–93. doi: 10.1016/j.joms.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 19.White RP, Jr, Offenbacher S, Blakey GH, Haug RH, Jacks MT, Nance PE, et al. Chronic oral inflammation and the progression of periodontal pathology in the third molar region. J Oral Maxillofac Surg. 2006;64:880–5. doi: 10.1016/j.joms.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 20.Wong SY, Roselinda AR, Haslina T. Effects of lower third molar removal on attachment level and alveolar bone height of the adjacent second molar. Arch Orofac Sci. 2009;4:36–40. [Google Scholar]
- 21.Kan KW, Liu JK, Lo EC, Corbet EF, Leung WK. Residual periodontal defects distal to the mandibular second molar 6-36 months after impacted third molar extraction. J Clin Periodontol. 2002;29:1004–11. doi: 10.1034/j.1600-051x.2002.291105.x. [DOI] [PubMed] [Google Scholar]
- 22.Kugelberg CF. Periodontal healing two and four years after impacted lower third molar surgery. A comparative retrospective study. Int J Oral Maxillofac Surg. 1990;19:341–5. doi: 10.1016/s0901-5027(05)80077-3. [DOI] [PubMed] [Google Scholar]
- 23.Gröndahl HG, Lekholm U. Influence of mandibular third molars on related supporting tissues. Int J Oral Surg. 1973;2:137–42. doi: 10.1016/s0300-9785(73)80030-4. [DOI] [PubMed] [Google Scholar]
- 24.Kaveri GS, Prakash S. Third molars: A threat to periodontal health? J Maxillofac Oral Surg. 2012;11:220–3. doi: 10.1007/s12663-011-0286-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.White RP, Jr, Fisher EL, Phillips C, Tucker M, Moss KL, Offenbacher S, et al. Visible third molars as risk indicator for increased periodontal probing depth. J Oral Maxillofac Surg. 2011;69:92–103. doi: 10.1016/j.joms.2010.07.076. [DOI] [PubMed] [Google Scholar]
- 26.Osborne WH, Snyder AJ, Tempel TR. Attachment levels and crevicular depths at the distal of mandibular second molars following removal of adjacent third molars. J Periodontol. 1982;53:93–5. doi: 10.1902/jop.1982.53.2.93. [DOI] [PubMed] [Google Scholar]
- 27.Quee TA, Gosselin D, Millar EP, Stamm JW. Surgical removal of the fully impacted mandibular third molar. The influence of flap design and alveolar bone height on the periodontal status of the second molar. J Periodontol. 1985;56:625–30. doi: 10.1902/jop.1985.56.10.625. [DOI] [PubMed] [Google Scholar]


