Abstract
Aims:
The aim of this systematic review was to compare the effectiveness of temporary anchorage devices (TADs) and conventional segmented arches (CSAs) during incisor intrusion in adult patients with a deep bite and their adverse effects.
Settings and Design:
Four electronic databases were searched. In addition, articles were manually searched for using the reference lists of relevant articles, grey literature, and peer-reviewed orthodontic journals.
Subjects and Methods:
Data from the retrieved articles were selected and evaluated by two independent reviewers using a new systematic review software program, DistillerSR. A meta-analysis of raw mean differences was performed.
Results:
Initially, we retrieved 9600 articles, but the selection process resulted in six articles. The included studies ranged from low to high in quality. Meta-analysis showed that TADs enabled 0.78 mm more upper incisor intrusion than the conventional method (95% confidence interval [CI] = 0.28–1.29). There was no significant anchorage loss difference in the CSA group compared to the TAD group (mean difference [MD] −3.68; 95% CI −7.41–0.05). Furthermore, a significant molar tipping of 1.03° was observed in the CSA group (P = 0.008) compared to the TAD group (MD −1.03; 95% CI −1.79–−0.27).
Conclusions:
The results of this meta-analysis showed that patients receiving TADs had 0.78 mm greater upper incisor intrusion than patients receiving the conventional treatment. This was statistically significant, but not clinically relevant. No clinical difference was found between TADs and the conventional method of anchorage loss.
Keywords: Deep bite, incisor, intrusion, mini-implant
Introduction
Deep bite correction during orthodontic treatment is often tricky, and relapse may occur in some cases.[1] The action of the orthodontic appliance in overbite correction is based on an extrusion of molars, an intrusion of incisors, or by a combination of both.[2] Several studies have attempted to quantify these different approaches.[3] The orthodontic intrusion of the anterior teeth is indicated for the management of a deep overbite. The functional evaluation of the upper gingival line in relation to the upper lip indicates whether the maxillary or mandibular anterior teeth should be intruded.[4]
Orthodontic intrusion techniques for the anterior teeth can be achieved by either conventional segmented arch (CSA)[5] and utility arch or recent method as segmented arch connected by temporary anchorage devices (TADs)[6] which is used as fixed anchorage units.
With a CSA, it was found that it can produce genuine incisor intrusion with little side effects on the molars. The application of this technique, rather than using continuous arch wires, therefore, was indicated if correction of deep bite by intrusion is desired as shown in Figure 1.[7]
Figure 1.

Illustrating using conventional segmented arch in incisor intrusion
Mini-screw implants or TADs are a compliance-free alternative to more traditional forms of incisor intrusion. It has recently been developed. They are smaller than regular dental implants and have the advantages of reducing patient compliance, immediate loading, uncomplicated placement, and minimal expense for patients.[8] Mini-screw implants have also been successfully used for intruding teeth because they make it possible to apply light continuous forces of known magnitudes. Better control of the forces could decrease external apical root resorption, which often associated with intrusive movements as shown in Figure 2.[9] However, several recent studies have demonstrated significant incisor intrusion with TADs, whereas others found that it causes significant tipping of incisors according to its location away from center of resistance (CR),[10] and also others found no difference between these methods.[6] Moreover, last systematic review has been published in 2005 entitled, “True incisor intrusion attained during orthodontic treatment: A systematic review and meta-analysis,” tried to quantify the amount of true incisor intrusion; however, since this review was somehow old, it did not consider mini-implants as a method for the intrusion.[11]
Figure 2.

Illustrating using temporary anchorage devices in incisor intrusion
Objectives
The aim of this systematic review was to compare the effectiveness of TADs and the CSAs during incisor intrusion in the patients with an increased overbite.
Materials and Methods
This systematic review was conducted according to the preferred reporting items for systematic review and meta-analysis protocols (PRISMA) 2015 checklist. This review was registered on the International Prospective Register of Systematic Reviews on July 25, 2016, and the registration number was CRD42016043491.
Eligibility criteria
Study design: randomized controlled trials (RCTs) and controlled clinical trials (CCTs)
Participants: Deep bite patients with permanent dentition
Interventions: Upper incisor intrusion with TADs
Control group: Upper incisor intrusion with CSA
Outcome measures: The primary outcome was the amount of upper incisor intrusion. The secondary outcomes were the amount of upper incisor tipping, the treatment duration, the amount of anchorage loss, and the amount of molar tipping as shown in Table 1.
Table 1.
Outcome table
| Outcome | Reading | Definition |
|---|---|---|
| 1. Amount of upper incisor intrusion | CR1-PP | Linear distance between CR of upper central incisor and PP |
| 2. Amount of upper incisor tipping | U1/PP | Angle between line connecting incisal edge and root apex of the maxillary central incisor and PP |
| 3. Treatment duration | Calendar | - |
| 4. Amount of anchorage loss | U6-PTV | Linear distance between the mesiobuccal cusp tip of the maxillary first molar and pterygoid vertical |
| 5. Amount of molar tipping | U6/PP | Angle between line connecting mesiobuccal cusp tip and root apex of mesiobuccal root of the maxillary first molar and PP |
CR1-PP: Central incisor-palatal plane; U6-PTV: Upper first molar - Pterygoid vertical; CR: Center of resistance
Exclusion criteria
Cohort studies, cross-sectional studies, case series, case reports, and animal studies
Studies published before 2000
Deep bite cases treated with orthognathic surgery.
Search strategy, study selection, and information sources
The following electronic databases were searched as shown in Table 2: MEDLINE (2000 to November 2017), Central-Cochrane Registers of Controlled Trials (2000 to November 2017), SCOPUS, and LILACS. Unpublished literature was searched electronically using ClinicalTrials.gov (www.clinicaltrials.gov), Google Scholar, and Egyptian University Library Consortium.
Table 2.
Search Strategy showing databases with keywords used
| Database | Key words | Limits |
|---|---|---|
| PubMed | Overbite [Mesh] OR deepbite OR over-bite OR over bite OR deep overbite OR gummy smile | 2000-November 2017 |
| AND implant OR mini implant* OR micro implant* OR microimplant* OR screw* OR mini screw* OR miniscrew* OR micro screw* OR microscrew* OR temporary anchorage device | ||
| OR skeletal anchorage OR tad OR plate OR intrus* OR incisor* OR anterior* | ||
| COCHRANE | Overbite [Mesh] OR deepbite OR over-bite OR over bite OR deep overbite OR gummy smile | 2000-November 2017 |
| AND implant OR mini implant* OR micro implant* OR microimplant* OR screw* OR mini screw* OR miniscrew* OR micro screw* OR microscrew* OR temporary anchorage device | ||
| OR skeletal anchorage OR tad OR plate OR intrus* OR incisor* OR anterior* | ||
| LILACS | Overbite [Mesh] OR deepbite OR over-bite OR over bite OR deep overbite OR gummy smile | 2000-November 2017 |
| AND implant OR mini implant* OR micro implant* OR microimplant* OR screw* OR mini screw* OR miniscrew* OR micro screw* OR microscrew* OR temporary anchorage device | ||
| OR skeletal anchorage OR tad OR plate OR intrus* OR incisor* OR anterior* |
The following journals were manually screened: European Journal of Orthodontics, American Journal of Orthodontics and Dentofacial Orthopedics, and Angle Orthodontist. The literature search, assessment of relevance, risk of bias analysis, and data extraction were performed. Data collection was performed by two investigators (A.A. and M.A.) and exported to DistillerSR (Recent Systematic Review Software, Ottawa, Canada). Both investigators used program for handling of the retrieved article. Disagreements were resolved by discussion and consultation with the third author (F.H.) while the fourth author (M.F.) was consulted for her scientific expertise on orthodontics.
Data extraction
Data extraction sheets were developed, and data were extracted independently by the two investigators (A.A. and M.A.) as shown in Tables 3–5. We contacted authors for further information.
Table 3.
Data extraction (demographic difference table of included studies)
| Authors | Publication year | Country | Journal | Type of study | Sample size (patients) | Gender | Age (years) | ||
|---|---|---|---|---|---|---|---|---|---|
| Women | Men | CSA | TADs | ||||||
| Senışık and Türkkahraman | 2012 | Turkey | AJODO | RCT | 45 | 26 | 19 | 20.32±3.22 | 20.13±2.48 |
| Polat-Özsoy et al. | 2011 | Turkey | AJODO | CCT | 24 | 14 | 10 | 15.25±3.93 | 20.90±7.12 |
| Krishna et al. | 2011 | India | Journal of Indian Orthodontic Society | CCT | 14 | - | - | - | - |
| Raj et al. | 2015 | India | J Res Adv Dent | CCT | 20 | 8 | 12 | 14-20 | 14-20 |
| El Namarawy et al. | 2014 | Cairo | Master thesis at Cairo University | CCT | 30 | 21 | 9 | 22.6±5.3 | 19.5±2.5 |
| Jain et al. | 2014 | India | Journal of clinical and diagnostic research | RCT | 30 | 19 | 11 | 16-22 | 16-22 |
CSA: Conventional segmented arch; TADs: Temporary anchorage devices
Table 5.
Data extraction (results of included studies)
| Authors | Duration (months) | U1/PP (°) | CR1-PP (mm) | U6-PTV (mm) | U6/PP (°) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| CSA | TAD | CSA | TAD | CSA | TAD | CSA | TAD | CSA | TAD | |
| Senışık and Türkkahraman | 6.88±0.95 | 6.93±1.17 | 4.87±5.64 | 8.10±5.17 | - | - | 9.83±3.53 | 0.00±0.00 | ||
| Polat-Özsoy et al. | 6.61±2.46 | 6.61±2.95 | 13.55±13.45 | 3.85±5.36 | −0.86±2.30 | −1.75±2.66 | -0.98±6.48 | 0.15±3.96 | ||
| Krishna et al. | 6 | 6 | ||||||||
| Raj et al. | 5 | 5 | 10.9±4.61 | 2.7±2.11 | −2.3±1.54 | −3.5±1.51 | −4.2±2.07 | 0.9±0.96 | ||
| El Namarawy et al. | 4.8±1 | 5.3±1 | 7.9±4.7 | 2.3±5.7 | −1.6±0.8 | −2.3±0.8 | −1±1.5 | 0.03±0.1 | ||
| Jain et al. | 4 | 4 | - | - | ||||||
CSA: Conventional segmented arch; TAD: Temporary anchorage device
Table 4.
Data extraction (methodological difference table of included studies)
| Authors | Groups Compared | Leveling and alignment | Screw used | Wire used | Force | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Diameter (mm) | Length (mm) | Type | Location | Loading | Application of force | Diameter | Type | Base Arch | CSA (g) | TAD (g) | |||
| Senışık and Türkkahraman | 3 groups: 2 treatment groups and 1 untreated control group (n=15/each group) | Not performed | Two | 1.3 | 5 | Absoanchor | Between the roots of the lateral incisors and canines | Immediately | NITI closed coil springs | 0.016 × 0.022 Niti | Ortho organizers | 0.016 st.st | 60 | 90 |
| Polat-Özsoy et al. | 2 groups: Group 1 (TAD), (n=13) Group 2 (CSA) (n=11) | Done | Two | 1.2 | 6 | Absoanchor | Distally to the maxillary lateral incisors | 1 week later | NITI closed coil springs | 0.016 × 0.016-in blue Elgiloy | Rocky mountain orthodontics | 0.016 × 0.022 st.st | - | 80 |
| Krishna et al. | Two groups (n=7/each group) | Done (approximately 2 months) | One | 2 | 8 | Leone | Between the maxillary central incisors | 2 weeks later | NITI closed coil springs | 0.016” × 0.022” TMA | - | - | 50 | 50 |
| Raj et al. | 2 groups (n=10/each group) | Done (approximately 3 months) | Two | - | - | - | Between roots of upper laterals, canines | 2 weeks later | NITI closed coil springs | Burstone intrusive arch | - | - | 70 | 70 |
| El namarawy et al. | Two groups (n=15/each group) | Done | Two | 1.4 | 6 | Jeil | Distally to the maxillary lateral incisors | 2 weeks later | NITI closed coil springs | 0.017” × 0.025” TMA | Ormco | 0.016” × 0.022” st.st | 100 | 100 |
| Jain et al. | Three Groups: Group 1 (TAD) (n=10) Group 2 ( J-hook headgear) (n=10) Group 3 (utility arch) (n=10) | Done | Two | 1.4 | 6 | Absoanchor | Between the maxillary central and lateral incisor | Not mentioned | NITI closed coil springs | 19 × 25 blue elgiloy | Not mentioned | 19 × 25 St.st | 1.5 ounces = 42.5 | 1.5 ounces =4 2.5 |
CSA: Conventional segmented arch; TAD: Temporary anchorage device
Risk of bias in individual studies
The Cochrane collaboration tool[12] for assessing the risk of bias in RCTs was applied using the following criteria as shown in Figure 3. An overall assessment of the risk of bias (high, unclear, and low) was made accordingly. Studies with at least one criterion for a high/unclear risk of bias were designated as having an overall high/unclear risk of bias. The quality of nonrandomized clinical trials was assessed using the risk of bias in nonrandomized studies of interventions (ROBINS-I) as shown in Table 6.[13]
Figure 3.
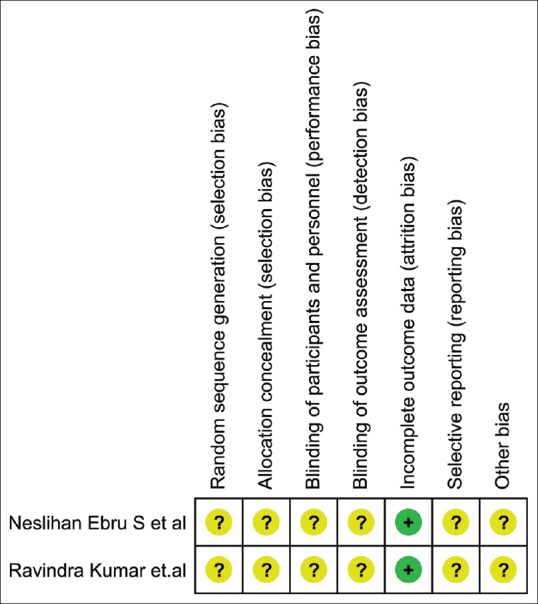
Risk of bias summary
Table 6.
Risk of bias in nonrandomized studies of interventions risk of bias assessment for the controlled clinical trials
| Authors | Confounding | Selection | Measurement of intervention | Missing data | Measurement of outcomes | Reported result | Overall |
|---|---|---|---|---|---|---|---|
| Polat-Özsoy et al. | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Krishna et al. | Serious | Moderate | Moderate | Serious | Serious | Moderate | Serious |
| Raj et al. | Moderate | ? | Moderate | Moderate | Moderate | Moderate | Moderate |
| El Namarawy et al. | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
Low: “Comparable to a well-performed randomized trial,” Moderate: “Sound for a non-randomized study” but not comparable to a rigorous randomized trial, Serious: Presence of “important problems,” Critical: “too problematic . to provide any useful evidence on the effects of intervention,” No information (?): Insufficient information provided to determine risk of bias, Overall risk of bias: Equal to the most severe level of bias found in any domain
Summary measures and approach to synthesis
Random-effect meta-analysis of the mean differences (MDs) was carried out as the principal method to estimate all the pooled estimates.[14] Randomized and controlled clinical studies were statistically evaluated both jointly and separately with subgroup analysis and significance established at P < 0.05. Results of the analyses are presented graphically with forest plots after comparisons of study designs, methods of intrusion, and participants to judge the clinical heterogeneity of the studies. Heterogeneity among studies in every analysis performed was done using the I2 test. The Cochrane rough guide of interpretation of the I2 test was used where values ranging from 0% to 40% represented no heterogeneity, 30% to 60% represented a moderate heterogeneity, 50% to 90% represented a substantial heterogeneity, and finally 75% to 100% represented a considerable heterogeneity. All calculations were carried out using the software: Review Manager (version 5.3; Cochrane Collaboration, Boston, Mass, USA).
Additional analysis
Sensitivity analysis was performed by drawing sensitivity plots to define the influence of specific studies on the total calculated effect (RCTs versus CCTs).
Results
Retrieved studies and data extraction
The PRISMA flowchart depicting the flow of 9600 initially retrieved articles is presented in Figure 4. A total of 9250 titles were screened after duplicates removal using DistillerSR. The number of citations that required title screening was 9250. Of these titles, 9150 studies were excluded on title screening (first level of screening) for reasons of irrelevance for the systematic review, so One hundred studies went to the second level of screening (abstract screening). Of these 100 abstracts, 92 studies were excluded for inclusion and exclusion criteria, so eight studies went to the third level of screening (full-text screening). Of these eight full-text articles, two studies were excluded due to being methodologically irrelevant. Eventually, we obtained two RCTs and four CCTs, giving a total of six studies. A summary of the data extracted from the articles is shown in Tables 3–5.
Figure 4.
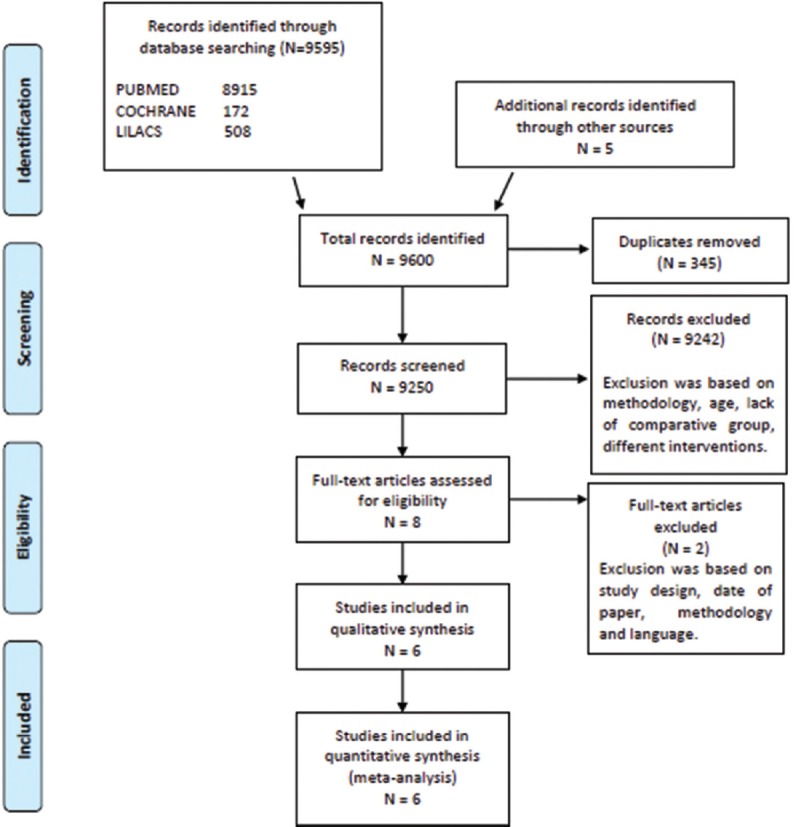
Preferred reporting items for systematic review and meta-analysis diagram of article retrieval
Risk of bias within studies
The assessment of the risk of bias in the RCTs is summarized in Figure 3. Due to lack of information about the randomization process, we assessed the risk of bias as high in the studies by Senışık and Türkkahraman[15] and Jain et al.[3] The quality assessment of the included CCTs is shown in Table 6 using the risk of bias in non-ROBINS-I.[13] Three studies, i.e. Polat-Özsoy et al.,[16] El Namarawy et al.,[17] and Raj et al.,[9] were of moderate quality. One study by Krishna et al.[10] was of serious quality.
Primary outcome measure
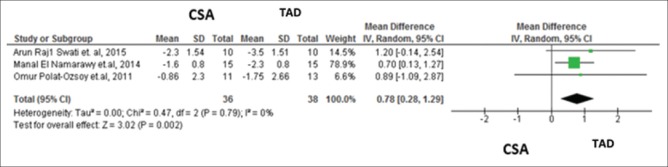
Amount of upper incisor intrusion
The data obtained from three studies, based on the similarity in the intervention, Raj et al., El Namarawy et al., and Polat-Özsoy et al., were pooled to compare the effect of mini-implant group versus control group when measured from CR of maxillary central incisor (CR1) to palatal plane (PP) (CR1-PP). A meta-analysis was undertaken on data from two studies, involving 38 participants who had been treated with the mini-implants and 36 participants who had been treated with conventional intrusion arches. The pooled estimate showed a significant improvement about 0.78 mm of upper incisor intrusion (P = 0.002) in the TAD group compared to control group (MD 0.78; 95% confidence interval [CI] 0.28–1.29) as shown in Figure 5. The test for the heterogeneity showed minimal heterogeneity (I2 = 0%). Subgroup analysis of the RCTs was not possible since there were no RCTs containing this outcome measure.
Figure 5.
Amount of incisors intrusion meta-analysis
Secondary outcome measures
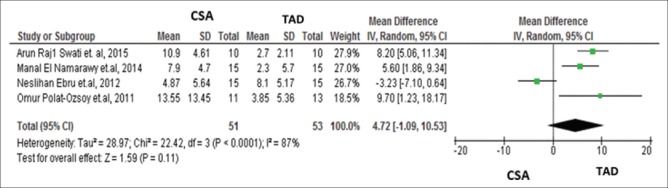
Amount of upper incisor tipping
Data obtained from four studies evaluating similar interventions (Senışık and Türkkahraman, Raj et al., Polat-Özsoy et al., and El Namarawy et al.) and involving 53 participants who had treated with the mini-implants were compared with 51 who acted as a control were pooled to compare the effect of mini-implants versus the control group On U1/PP (°). The overall effect showed no statistically significant difference (MD 4.72; 95% CI −1.09–10.53) as shown in Figure 6. The test for heterogeneity showed a high level of heterogeneity (I2 = 87%). Subgroup analysis of the RCTs was not possible since there was only one RCT containing this outcome measure, and the result showed 3.23° more incisors tipping in the CSA group.
Figure 6.
Amount of incisors tipping meta-analysis
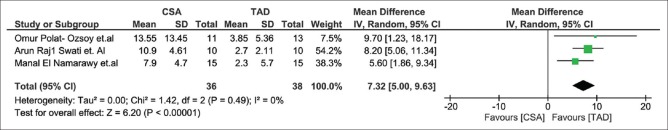
The sensitivity analysis after exclusion of the study by Senışık and Türkkahraman from this meta-analysis showed that a significant improvement about 7.32° of upper incisor tipping (P < 0.00001) in the TAD group compared to control group (MD 7.32; 95% CI 5.00–9.63) as shown in Figure 7. The test for heterogeneity showed minimal heterogeneity (I2 = 0%).
Figure 7.
Amount of incisors tipping meta-analysis (sensitivity analysis)
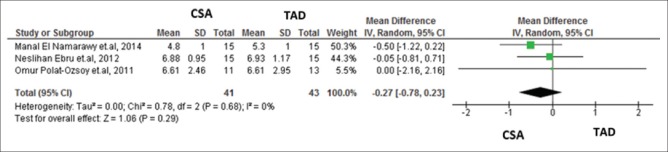
Treatment duration
Data obtained from three studies assessing similar interventions (El Namarawy et al., Senışık and Türkkahraman, and Polat-Özsoy et al.) and involving 43 participants who had been treated with the mini-implants were compared with 41 participants who acted as a control were pooled to compare the effect of mini-implant group versus the control group on the treatment duration. The overall effect showed no statistical differences between TAD and CSA groups (MD −0.27; 95% CI −0.78–0.23) as shown in Figure 8. The test for heterogeneity showed minimal heterogeneity (I2 = 0%). Subgroup analysis of the RCTs was not possible since there was only one RCT containing this outcome measure.
Figure 8.
Amount of treatment duration meta-analysis
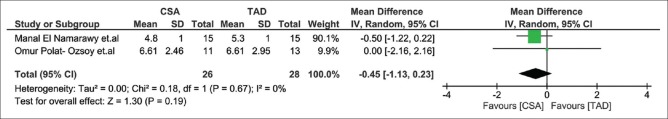
The sensitivity analysis after exclusion of the study by Senışık and Türkkahraman from this meta-analysis showed that no statistically significant difference (MD −0.45; 95% CI −1.13–0.23) as shown in Figure 9. The test for heterogeneity showed minimal heterogeneity (I2 = 0%).
Figure 9.
Amount of treatment duration meta-analysis (sensitivity analysis)
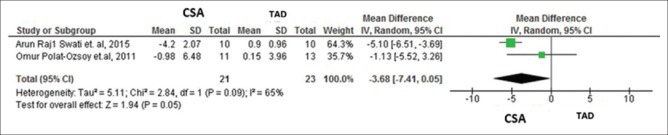
Amount of anchorage loss
Data obtained from two studies assessing similar interventions (Raj et al. and Polat-Özsoy et al.) and involving 23 participants who had been treated with the mini-implants was compared with 21 participants who acted as a control were pooled to compare the effect of mini-implant group versus the control group on U6-PTV. The overall effect showed no statistically significant difference (MD −3.68; 95% CI − 7.41–0.05) as shown in Figure 10. The test for the heterogeneity showed substantial heterogeneity (I2 = 65%). Subgroup analysis of the RCTs was not possible since there were no RCTs containing this outcome measure.
Figure 10.
Amount of Anchorage loss meta-analysis
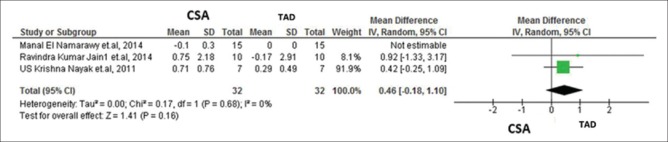
Amount of molar tipping
Data obtained from two studies assessing similar interventions (Senışık and Türkkahraman and El Namarawy et al.) and involving 30 participants who had been treated with the mini-implants was compared with 30 participants who acted as a control were pooled to compare the effect of mini-implant group versus the control group on U6-PP (°). The pooled estimate showed a significant 1.03° molar tipping (P = 0.008) in the control group compared to TAD group (MD − 1.03; 95% CI −1.79–−0.27) as shown in Figure 11. The test for the heterogeneity showed not applicable. Subgroup analysis of the RCTs was not possible since there were no RCTs containing this outcome measure.
Figure 11.
Amount of molar tipping meta-analysis
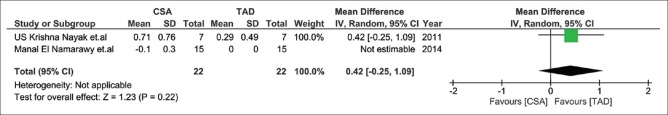
The sensitivity analysis after exclusion of the study by Senışık and Türkkahraman from this meta-analysis showed that no statistically significant difference (MD 0.42; 95% CI −0.25–1.09) as shown in Figure 12. The test for the heterogeneity showed not applicable.
Figure 12.
Amount of molar tipping meta-analysis (sensitivity analysis)
Discussion
Deep bite is a complex orthodontic problem that needs to be corrected at the beginning of the treatment. The maxillary incisor position, especially with the upper lip, is a key factor in determining the type of treatment, since correction of deep bite with maxillary incisor intrusion in patients with insufficient incisor display leads to flattening of the smile arc and reduces smile attractiveness.[16]
The data obtained from meta-analyses showed significant upper incisors intrusion about 0.78 mm in the TAD group compared to control group when measured from CR of maxillary central incisor to PP. The amount of upper incisors intrusion can be assessed by two linear measurements (U1-PP, CR1-PP). Caution is also advised during the implementation of U1-PP finding due to using the incisal edge of upper central as a reference point was unreliable. The CR of the maxillary central incisor was more reliable and determined for each patient rather than the CR of the anterior segment because of its ease of location and high reproducibility.[18] The CR of the maxillary central incisor was taken as the point located at one-third of the distance of the root length apical to the alveolar crest.[16]
As for amount of upper incisor tipping, the data obtained from meta-analyses showed no significant differences in the amount of incisors tipping between groups. Caution is also advised due to Krishna et al. and Jain et al., using TAD away from CR of the anterior segment which may increase incisors tipping and Senışık and Türkkahraman et al., did not do leveling and alignment before the intrusion.
The data obtained from meta-analyses showed no significant differences in the treatment duration between two groups. Caution is also advised during the implementation of these findings due to different forces used for intrusion between the included studies.
The data obtained from meta-analyses showed that no significant anchorage loss between both groups when measured from (U6-PTV). Caution is also advised during the implementation of these findings due to El Namarawy et al. using posterior anchor unit (transpalatal arch) cemented to the first maxillary molars.
The data obtained from meta-analyses showed that significant molar tipping about 1.03° in the control group compared to TAD group when measured from U6/PP.
The overall quality of the included studies was found to be high, moderate, and low; thus, future research, with a well-conducted methodology, may alter the evidence in hand. For this reason, clinicians should be cautious when interpreting these results.
Conclusions
On the basis of this systematic review and meta-analysis, we concluded the following:
The average difference of 0.78 mm regarding the amount of incisors intrusion in TADs group which seems statistically significant, but clinically insignificant
No significant difference was found regarding the amount of incisors tipping and the anchorage loss between the two groups
A significant distal molar tipping of 1.03° in control group greater than TAD group
Clinicians need to interpret these results with caution since they are based on studies with low, moderate, and high qualities which imply that a future well-conducted research may change the available evidence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
I would also like to thank Dr. Ahmed El Khadem for his assistance during the study and having the role of methodological expert.
References
- 1.Parker CD, Nanda RS, Currier GF. Skeletal and dental changes associated with the treatment of deep bite malocclusion. Am J Orthod Dentofacial Orthop. 1995;107:382–93. doi: 10.1016/s0889-5406(95)70091-9. [DOI] [PubMed] [Google Scholar]
- 2.Björk A. Variability and age changes in overjet and overbite. Am J Orthod. 1953;39:779–801. [Google Scholar]
- 3.Jain RK, Kumar SP, Manjula WS. Comparison of intrusion effects on maxillary incisors among mini implant anchorage, j-hook headgear and utility arch. J Clin Diagn Res. 2014;8:ZC21–4. doi: 10.7860/JCDR/2014/8339.4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zachrisson BU. Esthetic factors involved in anterior tooth display and the smile: Vertical dimension. J Clin Orthod. 1988;32:432–45. [Google Scholar]
- 5.Burstone CJ. The mechanics of the segmented arch techniques. Angle Orthod. 1966;36:99–120. doi: 10.1043/0003-3219(1966)036<0099:TMOTSA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Aydoǧdu E, Özsoy ÖP. Effects of mandibular incisor intrusion obtained using a conventional utility arch vs. bone anchorage. Angle Orthod. 2011;81:767–75. doi: 10.2319/120610-703.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiland FJ, Bantleon HP, Droschl H. Evaluation of continuous arch and segmented arch leveling techniques in adult patients – A clinical study. Am J Orthod Dentofacial Orthop. 1996;110:647–52. doi: 10.1016/s0889-5406(96)80042-4. [DOI] [PubMed] [Google Scholar]
- 8.Veltri M, Balleri B, Goracci C, Giorgetti R, Balleri P, Ferrari M, et al. Soft bone primary stability of 3 different miniscrews for orthodontic anchorage: A resonance frequency investigation. Am J Orthod Dentofacial Orthop. 2009;135:642–8. doi: 10.1016/j.ajodo.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 9.Raj A, Acharya SS, Mohanty P, Prabhakar R, Karthikeyan MK, Saravanan R, et al. Comparison of intrusive effects of mini screws and burstone intrusive Arch: A radiographic study. Adv Hum Biol. 2015;5:49–55. [Google Scholar]
- 10.Krishna NU, Varun G, Farhat G, Rahul S. Comparison of skeletodental changes occurring during deep overbite correction with mini-implant anchorage system and the utility arches reinforced by a transpalatal arch. J Indian Orthod Soc. 2011;45:9–14. [Google Scholar]
- 11.Ng J, Major PW, Heo G, Flores-Mir C. True incisor intrusion attained during orthodontic treatment: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2005;128:212–9. doi: 10.1016/j.ajodo.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 12.Cochrane. Cochrane Risk Of Bias Tool (Modified) For Quality Assessment of Randomized Controlled Trials Study. [Last accessed on Aug 2018]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK132434/bin/appd-fm3.pdf .
- 13.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 15.Senışık NE, Türkkahraman H. Treatment effects of intrusion arches and mini-implant systems in deepbite patients. Am J Orthod Dentofacial Orthop. 2012;141:723–33. doi: 10.1016/j.ajodo.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 16.Polat-Özsoy Ö, Arman-Özçırpıcı A, Veziroǧlu F, Çetinşahin A. Comparison of the intrusive effects of miniscrews and utility arches. Am J Orthod Dentofacial Orthop. 2011;139:526–32. doi: 10.1016/j.ajodo.2009.05.040. [DOI] [PubMed] [Google Scholar]
- 17.El Namarawy M, El Sharaby F, Bushnak M. Incisor Intrusion Thesis. Cairo University; 2014. Evaluation of two Modalities for Deep Bite Correction by Maxillary. [Google Scholar]
- 18.van Steenbergen E, Burstone CJ, Prahl-Andersen B, Aartman IH. The influence of force magnitude on intrusion of the maxillary segment. Angle Orthod. 2005;75:723–9. doi: 10.1043/0003-3219(2005)75[723:TIOFMO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]