Abstract
We report the transcranial fPA neuroimaging of N-methyl-D-aspartate (NMDA) evoked neural activity in rat hippocampus. Concurrent quantitative EEG (qEEG) and microdialysis recorded real-time circuit dynamics and excitatory neurotransmitter concentrations, respectively. We hypothesized that location-specific fPA VSD contrast would identify neural activity changes in hippocampus which correlate with NMDA-evoked excitatory neurotransmission. Transcranial fPA VSD imaging at the contralateral side of the microdialysis probe provided NMDA-evoked VSD responses with positive correlation to extracellular glutamate concentration changes. Quantitative EEG (qEEG) validated a wide range of glutamatergic excitation, which culminated in focal seizure activity after a high NMDA dose. We conclude that transcranial fPA VSD imaging distinguished focal glutamate loads in rat hippocampus, based on the VSD redistribution mechanism sensitive to electrophysiologic membrane potential. Our results suggest the future utility of this emerging technology in laboratory and clinical sciences as an innovative functional neuroimaging modality.
Keywords: Photoacoustic, neuroimaging, voltage-sensitive dye, microdialysis, quantitative electroencephalogram, N-methyl-D-aspartate, glutamate, hippocampus
Introduction
Whereas electrophysiological and invasive neurochemical techniques have been valuable in assessing activity within specific neuronal circuits in the brain, there is a distinct need for a non-invasive means to image real-time functional activity in deep brain structures in vivo. Previous optical imaging approaches to investigate local cortical circuits of rodents [1–3] applied invasive procedures to overcome superficial imaging depth, but further extension to deeper brain regions such as the hippocampus was prohibitive. The imaging of electrophysiological or neurochemical dynamics within the hippocampus has been accomplished primarily by optical imaging of freshly-sliced brain tissue [4] or magnetic resonance imaging spectroscopy (MRS) for non-invasive quantification of glutamate at high spatial resolution [5,6]. However, optical neuroimaging and MRS suffer from shallow imaging depth and from slow imaging speed, respectively. The application of two-photon microscopy to measure calcium ion dynamics in specific deep brain structures, including hippocampus, has poor temporal resolution [7]. Therefore, non-invasive neuroimaging of electrophysiological activity in deep brain structures, which reflects local excitatory neurotransmission, would be a significant advance.
Photoacoustic (PA) imaging is a hybrid approach combining optics and acoustics where the signal corresponding to neural activity is detected in the form of acoustic transcranial imaging with optical absorbance as an image contrast [8,9]. PA imaging is based on thermo-elastic perturbation of a target evoked by light absorbance from a pulsed laser illumination, which generates radio-frequency (RF) acoustic pressure waves detected by piezoelectric ultrasound transduction or optical interferometry. With this unique imaging technology, several attractive applications have been proposed for preclinical and clinical research with tomographic and microscopic imaging modes, including detection of endogenous contrast of cancer indicators, e.g., melanoma [10], breast microcalcifications [11–13], monitoring of cancer angiogenesis [14], oxygen metabolism [15], and quantification of lipid content [16,17], among others. Recently, we reported that functional PA (fPA) neuroimaging of near-infrared voltage-sensitive dye (VSD) redistribution can detect graded membrane potential changes in a lipid vesicle model and a chemo-convulsant seizure model in rodent brain in vivo [18].
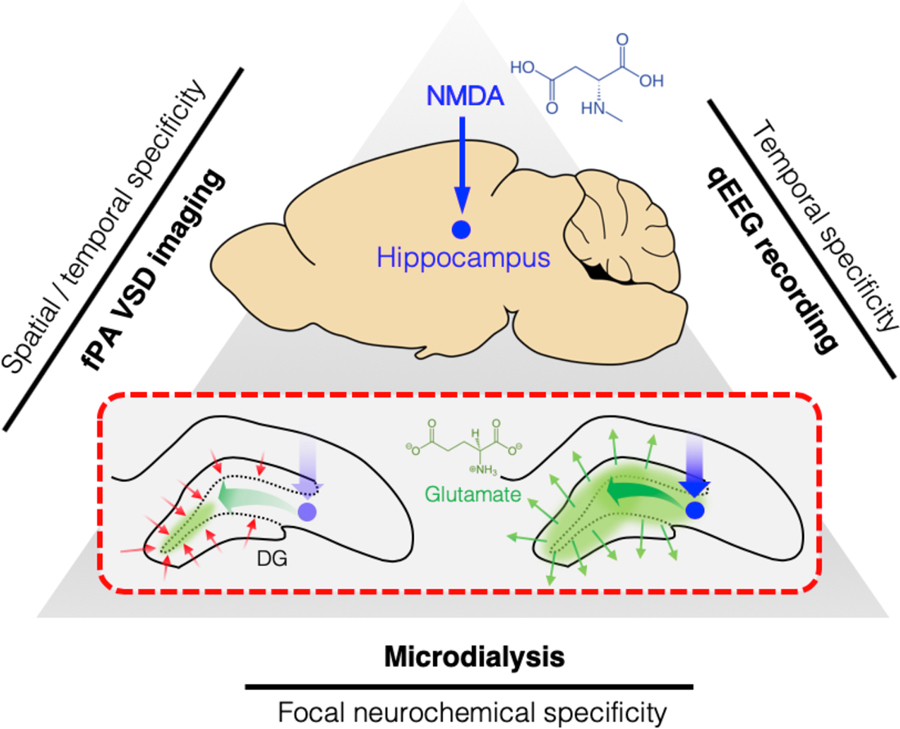
Here, we validated the transcranial fPA neuroimaging of electrophysiological activity in rat hippocampus in vivo through intact scalp, with a direct correlation to focal excitatory neurotransmission. The tri-modal neural sensing approach utilized microdialysis, quantitative electroencephalography (qEEG), and transcranial fPA neuroimaging to simultaneously monitor electrophysiological changes associated with focal glutamatergic excitation (Figure 1). To stimulate the hippocampus, we infused N-methyl-D-aspartate (NMDA) into rat hippocampus by reverse microdialysis to stimulate NMDA receptors. This scheme produces dramatic changes in the extracellular glutamate concentration in hippocampus which can be related to fPA neuroimaging over the widest possible range. Dramatic electrophysiological changes were identified, culminating in seizure activity detected by qEEG, implying a disruption of the dentate gyrus (DG) gatekeeping function. It is known that failure of the DG to gate the propagation of excitatory inputs into the hippocampus will result in overexcitation and seizures [19]. In our experiments, the DG in rat hippocampus was specifically targeted for the NMDA infusion, as its cells hold more hyperpolarized resting membrane potential when compared to other regions. Such baseline hyperpolarization will produce higher contrast in the VSD redistribution mechanism when depolarization occurs. In the presence of NMDA infusion by reverse microdialysis, we quantified the change in extracellular glutamate concentration by forward microdialysis and high-performance liquid chromatography (HPLC). Each of the three modalities thus provided information with different degrees of specificity, including spatiotemporal specificity from fPA imaging, electrophysiologic specificity from qEEG, and neurochemical specificity from microdialysis in rat hippocampus.
Figure 1. Tri-modal sensing of rat hippocampus.
Red dotted rectangular describes dentate gyrus (DG) gating breakdown at hippocampus to a focal NMDA infusion. NMDA, N-methyl-d-aspartate; VSD, voltage-sensitive dye.
Results
Transcranial fPA neuroimaging of rat hippocampus.
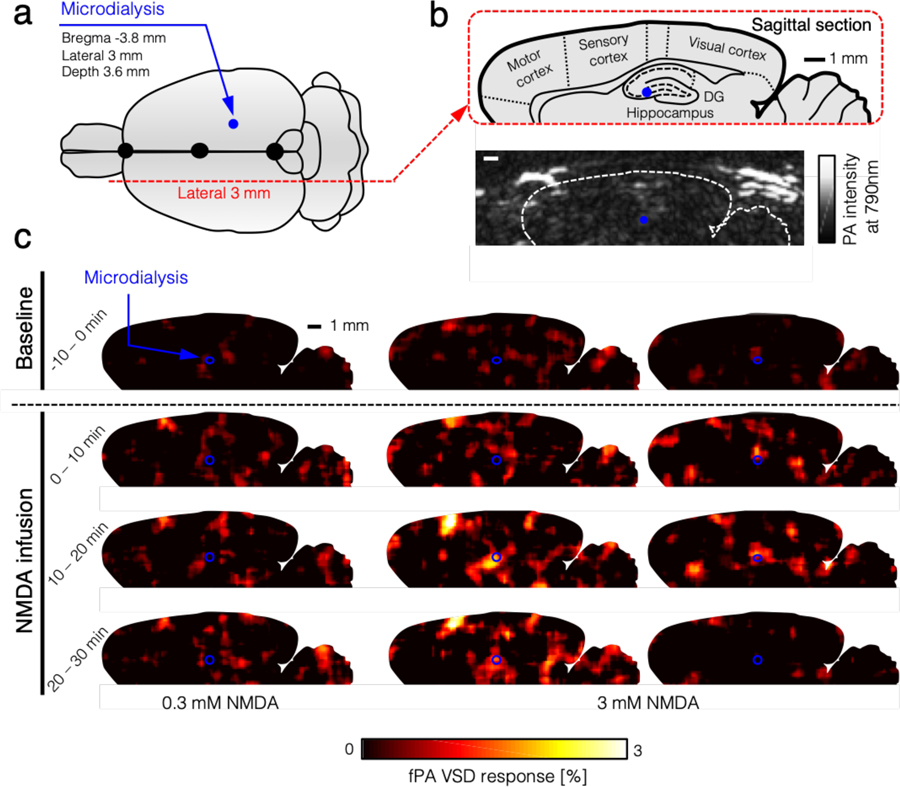
Transcranial fPA imaging of neural circuit dynamics was performed during NMDA infusion into rat hippocampus (Figure 2). The representative fPA sagittal planes obtained at 790 nm presented a sufficient sensitivity at the depths of interest, i.e., 3.6 mm, at a contralateral position to the microdialysis probe (Figure 3a). The sagittal PA imaging plane of hippocampus revealed the cross-sections of transverse sinus and inferior cerebral vein in the superficial depth range (Figure 3b). From the temporal dimension, time-averaged VSD responses were reconstructed pixel-by-pixel for pre-injection phase (−10 – 0 min) followed by the results for time bins in 10 min interval: 0 – 10 min, 10 – 20 min, and 20 – 30 min. The total recording duration (40 min) was limited by internal memory of the fPA neuroimaging system. Figure 3c shows the representative VSD responses in rat hippocampus collected during 0.3 mM and 3.0 mM NMDA infusion. Note that the fPA VSD responses at the regions-of-interest (ROIs, blue rounds in Figure 3c) represent the NMDA-evoked electrophysiological activity within the DG circuit in rat hippocampus before being filtered by the DG gating function. As a result, the VSD responses averaged in each NMDA acquisition phase (−10 – 0 min; 0 – 20 min; 20 – 30 min) demonstrated a positive correlation to the range of extracellular glutamate concentration with distinct doses of focal NMDA infusion, i.e., 0.3 mM (n = 6) and 3 mM (n = 3) (Figure 5). In addition, in the 3.0 mM NMDA infusion group, the averaged VSD responses were consistently maximized within the first 20 min of NMDA infusion, and their intensities corresponded well to the extracellular glutamate concentration measured in the forward microdialysis (Figure S1). Further comprehensive and quantitative analysis will be given in the following ‘Quantitative multi-modal correlation’ subsection.
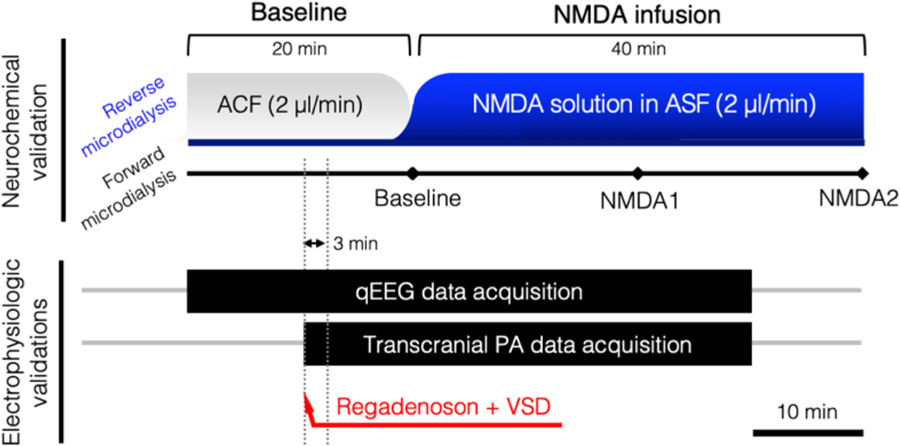
Figure 2. In vivo experimental protocol.
Tri-modal monitoring of rat hippocampus using reverse/forward microdialysis, transcranial PA imaging, and qEEG. ACF, artificial cerebrospinal fluid.
Figure 3. Transcranial PA neuroimaging of the hippocampal circuit dynamics following focal NMDA infusion.
(a) Illustration of stereotaxic coordinates for the microdialysis probe and sagittal cross-sections for real-time PA recording. (b) The sagittal PA imaging plane was selected in the contralateral side of the microdialysis probe infusing NMDA into the brain (3 mm lateral). (c) Time-averaged VSD response maps during −10 – 0 min (baseline phase); 0 – 10 min, 10 – 20 min, and 20–30 min (NMDA infusion phases). Note that the blue points indicate microdialysis probe in contra-lateral positions. Maximal glutamate concentration increases for representative fPA images were 34.23 % (left), 734.48 % (center) and 493.91 % (right).
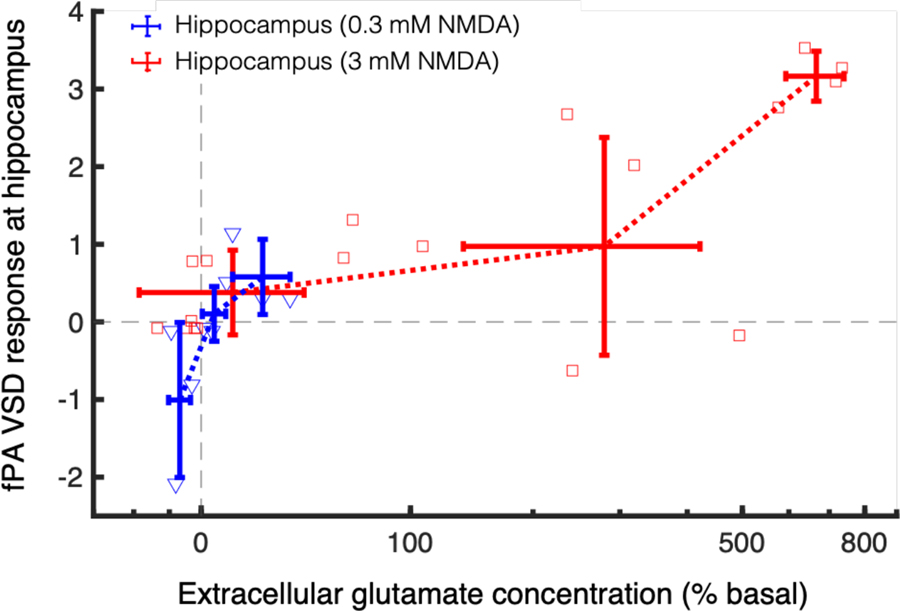
Figure 5. fPA VSD response at hippocampus as a function of extracellular glutamate concentration change.
Grey dotted lines indicate the basal level in fPA VSD response and extracellular glutamate concentration.
NMDA-evoked glutamatergic neurotransmission.
Intrahippocampal infusion of NMDA diluted into artificial cerebrospinal fluid at the required concentrations was delivered through the microdialysis probe. Concentrations of glutamate release in the dialysate were calculated from values of three baseline samples collected at 20 min intervals before NMDA infusion. During infusion into hippocampus (bregma −3.8 mm, lateral 3.0 mm, depth 3.6 mm; Figure 4a), samples continued to be collected every 20 min for the remainder of the study. Glutamate release was calculated as a % of basal values. Figure 4b shows the effect of NMDA infusion on glutamate release in the hippocampus of anesthetized rats. The results demonstrate the dose-related response of NMDA infusion at 0.3 (n = 3), 1.0 (n = 1), and 3.0 mM (n = 6) into the hippocampus, where 0.3 mM NMDA caused a 17.93±19.05 % increase in glutamate levels that remained elevated for the duration of the infusion; the 1.0-mM NMDA infusion caused doubling of the glutamate levels in the hippocampus compared to baseline (i.e., 112.42 %). The increase observed at the 1.0-mM dose remained elevated to the end of the NMDA infusion. At the 3.0-mM dose, the NMDA infusion raised glutamate level up to 392.99±250.54 % above baseline level, which peaked during the second 20-min sampling period.
Figure 4. Extracellular glutamate concentration and concomitant electrophysiology during NMDA-evoked activity in the hippocampus.
(a) Illustrates stereotaxic coordinates for the microdialysis probe and recording leads. Ground electrode was implanted over the rostrum. (b) 0.3 (n = 3), 1.0 (n = 1), and 3.0 mM (n = 6) NMDA infusion into the hippocampus caused maximal glutamate increases of 17.93±19.05%, 112.42%, and 392.99±250.54% respectively as compared to % baseline. Gray dotted line indicates the baseline. (c) Gamma (35–50Hz) power shows a 5-min baseline recording (black trace), followed by two consecutive 5 min traces (blue trace) following focal NMDA infusion in the hippocampus. EEG demonstrated a 261% increase in gamma power, as compared to % baseline, and an onset of epileptiform discharges after focal NMDA infusion (see inset bar graph; asterisk denotes epileptiform activity). (d) Respective theta power after NMDA infusion represents the theta component of the focal seizure. (e) 15-min spectral power heat map demonstrates the spectral power changes associated with NMDA infusion and subsequent epileptiform activity (denoted by black asterisk in e). (f) The representative raw EEG trace during the occurrence of the epileptiform event (solid black line in e) for full (05.−50Hz), gamma (0.5–50Hz), and theta (5.5–8.5Hz) power; respectively. For the expanded time scale of the focal hippocampal seizure see Supplemental 1.
EEG of electrophysiological activity in hippocampus.
Hippocampal infusion of 3.0 mM NMDA induced a significant rise in extracellular glutamate concentration, which correlated with fPA VSD responses, suggesting a potential break in the DG gate and synchronized DG firing that may lead to acute seizure activity. We therefore utilized qEEG during the same hippocampal 3.0 mM NMDA infusion protocol to identify if the maximal VSD response, and extracellular glutamate concentrations were associated with significant electrophysiological activity resulting from the breakdown of the DG gate and synchronous DG firing resulting in seizure onset. The DG is a hippocampal region specifically subjected to a barrage of excitatory inputs. However, the majority of excitatory activity does not propagate through the DG and into the hippocampus as the DG performs a gating function. Otherwise, excessive activation of the DG would disrupt its gating function and induces acute seizures in naïve animals [19].
In patients with focal epilepsy, gamma and theta activity from scalp EEG are indicators of the seizure onset zone and ictal onset [20,21]. Here, the temporal specificity of qEEG recorded circuit responses in real-time, before and after focal NMDA infusion. The 3.0 mM NMDA infusion into the hippocampal circuit induced focal seizure activity recorded by qEEG (Figure 4c black asterisk and S2). When NMDA was delivered to the hippocampal circuit by the microdialysis probe (Figure 4a) [22], a significant change in qEEG spectral power was detected, especially in the gamma range (Figure 4c). In the theta range, spectral power increased during the seizure (Figure 4d) further supporting the identification of focal seizure activity. The seizure trace measured by EEG demonstrated both a gamma and theta component (Figure 4f). The dose-related VSD and extracellular glutamate concentration response, along with the qEEG findings, suggest that the 3.0-mM NMDA infusion resulted in a break in the DG gate associated with focal seizure activity that can propagate to other cortical regions.
However, qEEG lacks spatial resolution, and recordings from deep brain structures cannot be isolated without implantation of invasive depth electrodes. Therefore, in order to maintain the tri-modal experimental paradigm we opted not to place depth electrodes. We made the stimulation focal, according to the previous proof-of-concept results by fPA detection onset of generalized seizures through an intact skull and scalp [18].
Quantitative multi-modal correlation.
The fPA VSD responses at the contralateral side to the microdialysis probe (blue rounds in Figure 3c) were measured and plotted as a function of the corresponding changes in extracellular glutamate concentration (Figure 5). Note that the ROIs to quantify the VSD responses were in 1 x 1 mm2 size in the sagittal cross-sections of rat hippocampus. The reference phase for VSD response quantification was obtained from the baseline phase: 5 – 10 min. In fPA imaging, 3.0 mM NMDA infusion into the hippocampus yielded significant elevation of VSD response: 0.08±0.35, 2.24±1.06, and 1.17±1.56 for baseline (−10 – 0 min), NMDA1 (0 – 20 min), and NMDA2 (20 – 30 min) phases, respectively (Figure S1a). The increase in glutamate concentration was correspondingly elevated from −4.67±4.48 %, 369.75±254.91 %, to 392.99±250.54 %. In addition, when re-analyzing the data for −50 – 100 %, 100 – 500 %, and 500 – 1,000 % bins of fractional glutamate concentration change, a high positive correlation was obtained with VSD responses: 0.38±0.55 (nsample = 9), 0.97±1.40 (nsample = 5), and 3.17±0.32 (nsample = 4) for 11.04±29.60 %, 279.85±141.64 %, to 666.49±73.63 % of glutamate concentration changes (red lines in Figure 5). The goodness of fit (R2) among the mean values was 0.95 with slope and y-intercept at 0.12 and 0.00, respectively. The qEEG revealed increased bursts of gamma power during 3.0 mM NMDA infusion, reaching up to ~261 % increase with a focal seizure, which indicates a breakdown of DG gate with the glutamatergic excitation induced (Figure 4c and S1). By contrast, focal 0.3 mM NMDA infusion into the hippocampus did not produce any statistically significant increase in circuit activity. The VSD responses were −0.11±0.02, −0.15±1.71, and −0.07±0.64 in baseline, NMDA1, and NMDA2 phases, respectively, while the corresponding glutamate concentration changes in hippocampus were −1.65±6.90 %, 3.90±10.41 %, and 17.93±19.05 % (Figure S1b). However, even in this case, the VSD responses presented strong positive correlation with fractional glutamate concentration changes, when re-analyzed in −10 – 0 %, 0 – 10 %, and 10 – 50 % bins (blue lines in Figure 5): −1.00±1.00, 0.10±0.35, and 0.58±0.48 (nsample = 3 for each) with −6.84±3.38 %, 4.43±4.05 %, and 22.59±11.64 % of fractional glutamate concentration changes, respectively. The R2 was 0.88 with slope and y-intercept at 0.05 and −0.46, respectively. Therefore, the fPA VSD neuroimaging revealed positive correlation to focal glutamatergic excitation in rat hippocampus.
Brain histology.
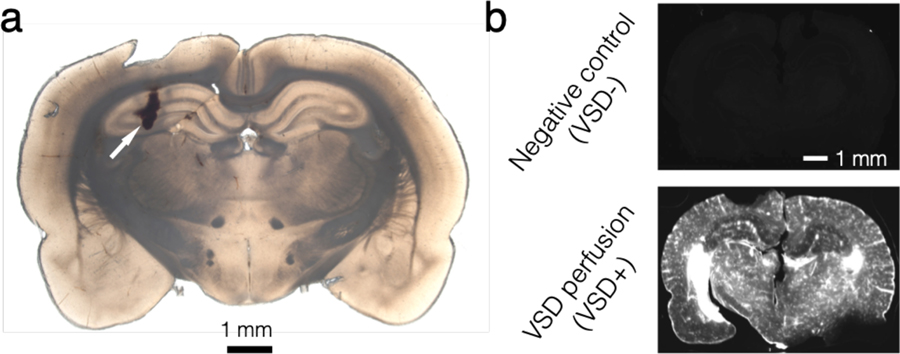
Brains were extracted after all in vivo experimental protocols. The brain was frozen-sectioned into slices of 300-µm thickness and evaluated to confirm probe placement using the scar caused by the microdialysis probe insertion for the NMDA infusion and collections as a marker. Figure 6a shows the bright-field images of the coronal plane of the hippocampus at −3.8 mm from bregma, respectively. White arrows indicate the lesion caused by the microdialysis probe positioned at the following coordinates in hippocampus: bregma −3.8 mm, lateral 3 mm, and depth 3.6 mm. The VSD staining of brain tissue was confirmed with near-infrared fluorescence microscopy. Uniform VSD fluorescence was found in the VSD perfusion animal, while negative control (VSD-) presented negligible fluorescence emission (Figure 6b), which again confirms the results in our previous publication [23].
Figure 6. Histopathological confirmation.
(a) Microdialysis probe at hippocampus. White arrow indicates the wound caused by microdialysis probe installation. (b) Frozen-sectioning histopathological confirmation of systematic VSD delivery throughout brain tissue region.
Discussion
The application of fPA neuroimaging has expanded into neuroscience [24–26] as label-free transcranial fPA imaging of neurovascular coupling proposed as a means to quantify hemodynamic changes at cortical / subcortical structures in either anesthetized or freely-moving rodents [27–31]. However, this approach does not yield quantitative neural activities that directly correspond to electrical activity. Hemoglobin provides an effective contrast signal in fPA neuroimaging, but the neurovascular coupling in brain is comparatively slow compared to electrophysiological communication between neurons. Instead, there has been extensive investigation into more effective exogenous contrast agents [32–36]. This strategy has enabled several neuroimaging approaches with functional voltage sensors. Deán-Ben et al. showed real-time PA tomography using a genetically encoded calcium indicator, GCaMP5G, in zebrafish in vivo [37]. Roberts et al. also proposed a new metallochromic calcium sensor for PA imaging (CaSPA) which has a high extinction coefficient, a low quantum yield, and high photo-bleaching resistance for brain and heart imaging [38]. Ruo et al. reported PA imaging of neural activity evoked by electrical stimulation and 4-aminopyridine-induced epileptic seizures using hydrophobic anions such as dipicrylamine (DPA) in mouse brain [39]. However, these voltage sensors require PA imaging at the visible spectral range (488 nm and 530 nm for GCaMP5G; 550 nm for CaSPA; 500 nm and 570 nm for DPA), which is suboptimal when imaging deep brain such as the hippocampus, positioned at a 5–8 mm depth when including intact scalp and cortex in the rat [22,40].
Recently, we proposed transcranial fPA recordings of brain activity in vivo with a near-infrared VSD, delivered through the blood-brain barrier (BBB) via pharmacological modulation, as a promising tool to transcend optical neuroimaging limitations, particularly as it relates to sensing depth [18,23,41]. Our previous studies demonstrated that transcranial fPA neuroimaging distinguishes in vivo seizure activity in stimulated rat brains from that of control groups in real time. However, the results were limited by the use of a global chemo-convulsant, causing perturbation across the entire brain, after intraperitoneal administration of penetylenetetrazole (PTZ). In this paper, we present follow-up advances in fPA VSD neuroimaging by focal neural stimulation of heterogeneous neural circuits, with concomitant validations from qEEG and glutamate quantification using microdialysis. The set of experiments described here yielded key findings as follows: (1) The microdialysis-dependent low-and high-dose NMDA infusion into the central nervous system (CNS) led to a wide range of focal extracellular glutamate increases in the hippocampus up to ~800% above baseline values. (2) The neurochemical response (microdialysis) was well-correlated to the changes in electrophysiological activity as measured by qEEG. The glutamatergic excitation evoked by high-dose NMDA was sufficient to cause a focal seizure in the hippocampal circuit, implying the disruption of DG gating. These results show that a wide range of neural excitation can be obtained from the NMDA infusion scheme. (3) Transcranial fPA neuroimaging data successfully identified hot spots of focal NMDA receptor activation. The hippocampal circuitry provided the proportional excitation of glutamatergic neurotransmission with concomitant NMDA infusion.
Further investigations are required to advance our current perspectives available with tri-modal sensing, including fPA, qEEG, and microdialysis. Glutamate produces fast-rising brief depolarizations in pyramidal neurons. Therefore, the use of fPA neuroimaging will enable us to more precisely assess glutamate and GABA dynamics in order to formulate a more complete profile of circuit activation. Once homeostasis is disrupted, neuronal activity is sensitive to changes both of excitatory and inhibitory mechanisms. Faster neurochemical recording is another approach that may prove useful in assessing the impact of these measures. Although microdialysis successfully provided quantitative, focal neurochemical concentrations, the sampling rate of 1 sample per 20 min was slow. Techniques offering faster temporal resolution may allow more meaningful comparison of the neurochemical changes yielded by microdialysis and the electrophysiological events monitored by qEEG and fPA neuroimaging [42]. One such technique, using custom built hardware and the Amplex Red method, achieved fluorescence-based quantification of glutamate from samples taken every 5 seconds, though reliability appeared to be limited when higher glutamate concentrations were measured [43]. Implantable glutamate biosensors allow sub-second readouts of neurochemical concentrations. However, current limitations include sensitivity, selectivity, and high cost; recent developments in materials, effective modeling, and sensor design may soon alleviate some of these limitations [44,45].
From the results, transcranial fPA neuroimaging was able to differentiate the circuit activity defined with qEEG and microdialysis. However, future developments should serve to further advance the efficacy of the fPA neuroimaging in neuroscience. (1) We expect that improved signal processing for extracting neural activity from background vascular interference will enable better characterization of brain function. The present in vivo experiments confirmed the possibility of background suppression, as also presented in our previous study [18]. Enhanced signal processing and/or use of multi-spectral wavelengths may allow significantly improved spectral differentiation of electrophysiological activities in the brain at higher temporal resolution, leading to development of novel quantitative metrics for brain activity measures. It will also improve the temporal resolution by reducing frame averaging that has been needed to secure signal sensitivity. (2) We are also working on the advancement of the VSD technology. The criteria for the chemical improvement would be better absorbance, faster transmembrane redistribution kinetics, and contrast resolution to membrane potential variation, which will improve both VSD signal sensitivity and temporal resolution [41]. (3) Having isotropic resolution with 2-D PA probes would be another interesting direction to pursue as a follow up to the present work. The use of 2-D PA probe would not only allow real-time volumetric information, but also enable the suppression of off-axis interference. Even though we presented that neural activity can be successfully discerned with our current 1-D PA probe, its sensitivity might be affected by off-axis interferences especially from the elevation direction because of the limited acoustic lens focusing at a fixed depth. The neuroimaging using 2-D PA probe would limit those interferences by the advanced electrical beamforming capability in axial, lateral, and elevation directions. (4) Having an improved PA imaging system would provide a significant breakthrough in terms of spatiotemporal resolution in fPA neuroimaging. Even though our current laser system yields both 4 fps (frame-per-second) of temporal resolution and PA signal sensitivity in rat hippocampus, further optimization of temporal resolution would provide finer spatiotemporal specificity. On the other hand, we consider employing larger animal models for this fPA VSD neuroimaging research. Pigs are an ideal subject to pave the way to human translation of neuroengineering technologies, given their analogous brain structure and physiology, and similarity in scalp and skull thicknesses to those in humans [46]. We already validated the transcranial fPA neuroimaging in the pig model, and will continue to pursue this research direction [47].
In all, the transcranial fPA neuroimaging in hippocampus in in vivo rat brain was successfully correlated with electrophysiologic and neurochemical measurements using qEEG and microdialysis: focal NMDA infusion triggers glutamate release that excites the neural circuit, and at suprathreshold doses it causes runaway excitation in the hippocampus by overcoming DG gating. This is reflected in the lower seizure threshold of the hippocampus. Therefore, the transcranial fPA neuroimaging is a promising technology for the visualization of focal neural events in real time.
Materials and Methods
Animal preparation.
For the proposed in vivo experiments, 8–9-week-old male Sprague Dawley rats (Charles Rivers Laboratories, Wilmington, MA, USA) weighing 275–390g were used. The use of animals for the proposed experimental protocol was approved by the Institutional Animal Care and Use Committee of Johns Hopkins Medical Institute (RA16M225). Rats were housed in groups of 3 per cage with free access to food and water, and maintained on a 12hr light / 12hr dark cycle.
On the day of the study, rats were weighed and anesthetized with urethane (1.2mg/kg,). Urethane was given incrementally with alternating intra-peritoneal (ip) and subcutaneous (sc) dosing. Three (3) ml of isotonic saline was given sc on each side of the body to keep the animal hydrated during the experimental procedure. Body temperature was maintained until animal was fully anesthetized and ready for surgery. For fPA and qEEG studies, an iv catheter was inserted into a tail vein prior to dye administration during the studies. Once a stable plane of anesthesia was established, hair was shaved from the scalp of each rat to have acoustic coupling for transcranial fPA recording. The rat was placed into a stereotaxic device (Stoeling Co. Wood Dale, IL, USA). This fixation procedure was required for determining coordinates of microdialysis probe implantation and for preventing any unpredictable movements during fPA or EEG recording of neural activities. A CMA12 microdialysis probe (Harvard Apparatus, Holliston, MA, USA) was implanted into the CA3 region of the right hippocampus (stereotaxic coordinates: 3 mm lateral and 3.8 mm posterior to bregma, and 3.6 mm below the surface of the dura, Figure 3a) [22]. The probe active exchange surface was 2 × 0.5 mm. The probe was secured to the skull using dental acrylic cement. The fPA and qEEG probes were placed on the contralateral side of the microdialysis probe.
Fluorescence quenching-based near-infrared voltage-sensitive dye.
In the present in vivo study, we used the fluorescence quenching-based near-infrared cyanine VSD, IR780 perchlorate (576409, Sigma-Aldrich Chemicals, St. Louis, MO, USA) as used in our previous in vivo study investigating chemo-convulsant seizure activity [18], and it has the analogous chemical structure of PAVSD800–2, our new VSD validated in our previous in vitro study [41]. This VSD yields fluorescence quenching and de-quenching depending on membrane polarization and subsequent change in the local VSD molecule density, leading to a reciprocal change of PA contrast with non-radiative relaxation of absorbed energy.
Functional fPA neuroimaging.
We used real-time PA data acquisition to record electrophysiological neural activities in vivo as in our previous study [18]: an ultrasound research system consisted of an ultrasound linear array transducer connected to a real-time data acquisition system (SonixDAQ, Ultrasonix Medical Corp., Canada). To induce the PA signals, pulsed laser light generated by a second-harmonic (532 nm) Nd:YAG laser pumping an optical parametric oscillator (OPO) system (Phocus Inline, Opotek Inc., USA) provided 690–900 nm of tunable wavelength range and 20 Hz of the maximum pulse repetition frequency. A bifurcated fiber optic bundle, each 40 mm long and 0.88 mm wide, was used for laser pulse delivery. The PA probe was situated between the outlets of the bifurcated fiber optic bundles using a customized, 3-D printed shell for evenly distributing laser energy density in the imaging field-of-view. The alignment of outlets was focused specifically at 20 mm depth. The PA probe was positioned in the sagittal plane contralateral to the microdialysis probe (3 mm) to cover the hippocampal cross-section. The distance between the PA probe and the rat skin surface was 20 mm filled with acoustic gel, and the resultant energy density was at ~3.5 mJ/cm2, which is far below the maximum permissible exposure (MPE) of skin to laser radiation by the ANSI safety standards [48]. A wavelength of 790 nm was used, at which sufficient absorbance can be obtained by the near-infrared VSD, i.e., IR780 perchlorate. Also, excitation at that wavelength prevented the undesired time-variant change of blood oxygen saturation, since the wavelength corresponds to the isosbestic point of Hb and HbO2 absorption spectra. Detailed information of neural activity reconstruction using normalized time-frequency analysis can be found in our previous publication [18].
In vivo microdialysis.
In vivo microdialysis sampling was carried out as previously described [49,50]. For infusion experiments, NMDA (Sigma-Aldrich Chemicals) was weighed, solubilized, and diluted to the desired concentration in artificial cerebrospinal fluid (NaCl, 147 mmol/L; KCl, 2.7 mmol/L; CaCl2, 1.2 mmol/L; MgCl2, 0.85 mmol/L) (Harvard Apparatus) on the study day. Once the probe was inserted and secured, it was perfused with artificial cerebrospinal fluid pumped at a flow rate of 2 µl/min. Samples were collected at 20 min intervals, and immediately transferred to a −80°C freezer until assayed. To allow sufficient time for the glutamate levels to equilibrate, three baseline samples were collected an hour following initiation of infusion. Following collection of these samples, NMDA was infused into the brain directly through the dialysis probe with the same pump parameters as used for the baseline samples. Dialysate samples were assayed for glutamate by a two-step process using HPLC-ECD on an Eicom HTEC-500 system (EICOM, San Diego, CA, USA). After passing the samples through a separation column, they were processed via a column containing immobilized L-glutamate oxidase enzyme, resulting in the release of hydrogen peroxide. The hydrogen peroxide concentration was then determined using a platinum working electrode. Chromatographic data were acquired online and exported to an Envision software system (EICOM) for peak amplification, integration, and analysis.
Our method of reverse microdialysis exerts effects that are largely mediated via the DG circuit in rat hippocampus, since our results agree with those of Ludvig et al. [51] who used similar methods to evoke hippocampal seizures. Our microdialysis probes have an active surface of 2.0 × 0.5 mm, and most evidence suggests a 1 mm cylinder of influence around the probe for substances that are reverse dialyzed into the neuropil [52]. It is important to note that the 3 mM concentration of NMDA in the dialysis perfusion solution is not the concentration of NMDA reaching brain tissue. Perfusion flowrate, probe membrane characteristics, and tissue properties serve to limit the penetrance of reverse dialyzed substances into the brain [53]. Ludvig et al. addressed this issue previously and showed that the biophase concentration of reverse dialyzed NMDA is about 15% of the source concentration. Thus, NMDA concentrations reaching the brain tissue in our experiments probably ranged from 0.045 – 0.45 mM. Another possibility to consider is that infused NMDA is taken up into cells surrounding the probe, thereby keeping biophase concentrations low. Bruhn et al. demonstrated that radiolabeled D-aspartate reverse dialyzed into rat brain is rapidly and effectively extracted from the extracellular fluid by glutamate transport mechanisms [54]. Collectively, this information suggests that neurochemical, EEG, and fPA endpoints that we measured in response to reverse dialyzed NMDA reflect changes localized to the hippocampus.
Quantitative EEG.
All EEG recordings utilized a three-electrode paradigm: 1 recording, 1 reference (aligned to the site of activation) and 1 ground over the rostrum. The electrodes (IVES EEG; Model # SWE-L25 – IVES EEG solutions, MA, USA) were fixed with minimal cyanoacrylate adhesive (KrazyGlue), similar to previous protocols [55]. Data acquisition was performed using Sirenia software (Pinnacle Technologies Inc., Kansas, USA) with synchronous video capture. Data acquisition had a 14-bit resolution, 400 Hz sampling rate, and a band pass filter between 0.5 Hz and 50 Hz. The acquisition files were stored in an .EDF format and scored manually, using real-time annotations from the experiments. EEG power for 2-second epochs was done using an automated fast Fourier transformation module in Sirenia software [56].
In vivo experimental protocol.
The in vivo protocols were designed for simultaneous multi-modal sensing of the neural activity in the hippocampus: microdialysis-qEEG and microdialysis-fPA neuroimaging. Figure 2 shows a detailed schematic protocol for each group representing the response to the administration of NMDA, Lexiscan, and VSD (i.e., IR780 perchlorate). fPA and qEEG data acquisition were performed for 40 min to correlate with three microdialysis samples collected at 20-min intervals. Graded NMDA infusion concentrations were applied to identify the dose-dependent glutamatergic excitation of hippocampal circuit: 0.3 mM (n = 3) and 3.0 mM (n = 6). VSD and Lexiscan followed the data acquisition sequence with a 3-min delay, thereby 5 min of baseline phase was guaranteed for the VSD response reconstruction in fPA neuroimaging before starting NMDA infusion. The dosing protocol for Lexiscan and VSD administration was as follows: through an iv tail vein catheter, 150 µl of Lexiscan (0.4mg/5ml) was injected, followed by 200 µl of VSD at 2 mg/ml concentration, flushed immediately with 150 µl of 0.9% isotonic saline. The EEG signal was recorded separately in an identical preparation procedure as the fPA neuroimaging, including animal preparation and administration of IR780, Lexiscan and experimental duration time for all recordings.
Brain histology.
Rats used for the above protocol were euthanized, and whole brains immediately harvested and placed in 10 % formalin. All brains were allowed to fix in fresh 10 % formalin for at least 48 hours with gentle agitation on a conical rotator. Subsequently, the brains were processed through a series of sucrose gradients (15 %, 20 %, 30 % for 12–24 hours each) for cryoprotection. Brains were sectioned frozen at 300 µm thickness. Tissue sections were mounted on slides in ProLong Diamond Anti-face mountant. Slides with sections were imaged using an Olympus OM-D E-M5 Mark II for bright field image and using LI-COR Odyssey for fluorescence visualization.
Supplementary Material
Acknowledgements
This work was supported by the NIH BRAIN Initiative under Grant No. R24MH106083-03 (DFW, AR, AAG, EMB, HV, JE) and the NIH National Institute of Biomedical Imaging and Bioengineering (NIBIB) under Grant No. R01EB01963 (LML); NIH National Institute of Child Health and Human Development (NICHD) for R01HD090884 (SDK); NIH National Institute on Drug Abuse (NIDA) Intramural Research Program (IRP) under grant number DA00522 (MHB); NIH National Institute of Heart, Lung and Blood (NHLBI) under grant number R01HL139543 (Jeeun K, APM, EMB); National Cancer Institute (NCI) under grant number R21CA202199 and its equipment supplement (EMB). Funding of the PA equipment was provided via resources of Jin K and EMB NSF Career award #1653322. Jeeun K was partially supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education #2018R1A6A3A03011551.
Footnotes
Publisher's Disclaimer: Accepted Manuscript is “the version of the article accepted for publication including all changes made as a result of the peer review process, and which may also include the addition to the article by IOP Publishing of a header, an article ID, a cover sheet and/or an ‘Accepted Manuscript’ watermark, but excluding any other editing, typesetting or other changes made by IOP Publishing and/or its licensors”
Conflict of Interests
The subject matter described in this article is included in patent applications filed by the University of Connecticut and Johns Hopkins University. LML is a founder and owner of Potentiometric Probes LLC, which sells voltage sensitive dyes.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- [1].Derdikman D, Hildesheim R, Ahissar E, Arieli A and Grinvald A 2003. Imaging spatiotemporal dynamics of surround inhibition in the barrels somatosensory cortex. J Neurosci 23 3100–3105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Petersen CC, Grinvald A and Sakmann B 2003. Spatiotemporal Dynamics of Sensory Responses in Layer 2/3 of Rat Barrel Cortex Measured In Vivo by Voltage-Sensitive Dye Imaging Combined with Whole-Cell Voltage Recordings and Neuron Reconstructions Journal of Neuroscience 23 1298–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Petersen C and Sakmann B 2001. Functionally independent columns of rat somatosensory barrel cortex revealed with voltage-sensitive dye imaging. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience 21 8435–8446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Okubo Y, Sekiya H, Namiki S, Sakamoto H, Iinuma S, Yamasaki M, Watanabe M, Hirose K and Iino M 2010. Imaging extrasynaptic glutamate dynamics in the brain. Proceedings of the National Academy of Sciences 107 6526–6531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Crescenzi R, DeBrosse C, Nanga RP, Byrne MD, Krishnamoorthy G, D’Aquilla K, Nath H, Morales KH, Iba M, Hariharan H, Lee VM, Detre JA and Reddy R 2017. Longitudinal imaging reveals subhippocampal dynamics in glutamate levels associated with histopathologic events in a mouse model of tauopathy and healthy mice Hippocampus 27 285–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Voets NL, Hodgetts CJ, Sen A, Adcock JE and Emir U 2017. Hippocampal MRS and subfield volumetry at 7T detects dysfunction not specific to seizure focus Sci Rep-uk 7 16138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kondo M, Kobayashi K, Ohkura M, Nakai J and Matsuzaki M 2017. Two-photon calcium imaging of the medial prefrontal cortex and hippocampus without cortical invasion. eLife 6 592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Wang LV and Hu S 2012. Photoacoustic tomography: in vivo imaging from organelles to organs. Science 335 1458–1462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wang X, Pang Y, Ku G, Xie X, Stoica G and Wang LV 2003. Noninvasive laser-induced photoacoustic tomography for structural and functional in vivo imaging of the brain Nature Biotechnology 21 803–806 [DOI] [PubMed] [Google Scholar]
- [10].Zhang HF, Maslov K, Stoica G and Wang LV 2006. Functional photoacoustic microscopy for high-resolution and noninvasive in vivo imaging. Nature Biotechnology 24 848–851 [DOI] [PubMed] [Google Scholar]
- [11].Kang J, Kim E-K, Kim G, Yoon C, Song T-K and Chang J 2015. Photoacoustic imaging of breast microcalcifications: a validation study with 3-dimensional ex vivo data and spectrophotometric measurement. J Biophotonics 8 71–80 [DOI] [PubMed] [Google Scholar]
- [12].Kim G, Kang J, Kwak J, Chang J, Kim S, Youk J, Moon H, Kim M and Kim E-K 2014. Photoacoustic Imaging of Breast Microcalcifications: A Preliminary Study with 8-Gauge Core-Biopsied Breast Specimens Plos One 9 e105878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kang J, Kim E-K, Kwak J, Yoo Y, Song T-K and Chang J 2011. Optimal laser wavelength for photoacoustic imaging of breast microcalcifications Appl Phys Lett 99 153702 [Google Scholar]
- [14].Yao J, Maslov KI and Wang LV 2011. In vivo Photoacoustic Tomography of Total Blood Flow and Potential Imaging of Cancer Angiogenesis and Hypermetabolism Technol Cancer Res T 11 301–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hu S 2016. Listening to the Brain With Photoacoustics IEEE Journal of Selected Topics in Quantum Electronics 22 117–126 [Google Scholar]
- [16].Hui J, Cao Y, Zhang Y, Kole A, Wang P, Yu G, Eakins G, Sturek M, Chen W and Cheng J-X 2017. Real-time intravascular photoacoustic-ultrasound imaging of lipid-laden plaque in human coronary artery at 16 frames per second. Scientific Reports 7 1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wu M, Springeling G, Lovrak M, Mastik F, Iskander-Rizk S, Wang T, van Beusekom HM, van der Steen A and Soest G 2017. Real-time volumetric lipid imaging in vivo by intravascular photoacoustics at 20 frames per second. Biomed Opt Express 8 943–953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kang J, Zhang HK, Kadam SD, Fedorko J, Valentine H, Malla AP, Yan P, Harraz MM, Kang JU, Rahmim A, Gjedde A, Loew LM, Wong DF and Boctor EM 2019. Transcranial Recording of Electrophysiological Neural Activity in the Rodent Brain in vivo Using Functional Photoacoustic Imaging of Near-Infrared Voltage-Sensitive Dye Front Neurosci-switz 13 579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Krook-Magnuson E, Armstrong C, Bui A, Lew S, Oijala M and Soltesz I 2015. In vivo evaluation of the dentate gate theory in epilepsy J Physiology 593 2379–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Andrade-Valenca L, Dubeau F, Mari F, Zelmann R and Gotman J 2011. Interictal scalp fast oscillations as a marker of the seizure onset zone. Neurology 77 524–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Foldvary N, Klem G, Hammel J, Bingaman W, Najm I and Luders H 2001. The localizing value of ictal EEG in focal epilepsy Neurology 57 2022–8 [DOI] [PubMed] [Google Scholar]
- [22].Paxinos G and Watson C 2014. The Rat Brain in Stereotaxic Coordinates Elsevier Academic Press [Google Scholar]
- [23].Pak RW, Kang J, Valentine H, Loew LM, Thorek DL, Boctor EM, Wong DF and Kang JU 2018. Voltage-sensitive dye delivery through the blood brain barrier using adenosine receptor agonist Regadenoson Biomed Opt Express 9 3915–3922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Nie L, Cai X, Maslov K, Garcia-Uribe A, Anastasio MA and Wang LV 2012. Photoacoustic tomography through a whole adult human skull with a photon recycler Journal of Biomedical Optics 17 110506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Li W, Chen R, Lv J, Wang H, Liu Y, Peng Y, Qian Z, Fu G and Nie L 2018. In Vivo Photoacoustic Imaging of Brain Injury and Rehabilitation by High-Efficient Near-Infrared Dye Labeled Mesenchymal Stem Cells with Enhanced Brain Barrier Permeability Adv Sci 5 1700277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Liu Y, Yang Y, Sun M, Cui M, Fu Y, Lin Y, Li Z and Nie L 2017. Highly specific noninvasive photoacoustic and positron emission tomography of brain plaque with functionalized croconium dye labeled by a radiotracer Chem Sci 8 2710–2716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hu S and Wang LV 2010. Neurovascular photoacoustic tomography. Frontiers in neuroenergetics 2 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Zhang P, Li L, Lin L, Hu P, Shi J, He Y, Zhu L, Zhou Y and Wang LV 2018. High-resolution deep functional imaging of the whole mouse brain by photoacoustic computed tomography in vivo. J Biophotonics 11 e201700024 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Tsytsarev V, Rao B, Maslov KI, Li L and Wang LV 2013. Photoacoustic and optical coherence tomography of epilepsy with high temporal and spatial resolution and dual optical contrasts. J Neurosci Meth 216 142–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gottschalk S, Fehm T, Deán-Ben X, Tsytsarev V and Razansky D 2017. Correlation between volumetric oxygenation responses and electrophysiology identifies deep thalamocortical activity during epileptic seizures Neurophotonics 4 011007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Xi L, Jin T, Zhou J, Carney P and Jiang H 2017. Hybrid photoacoustic and electrophysiological recording of neurovascular communications in freely-moving rats Neuroimage 161 232–40 [DOI] [PubMed] [Google Scholar]
- [32].Luke GP, Yeager D and Emelianov SY 2011. Biomedical Applications of Photoacoustic Imaging with Exogenous Contrast Agents Annals of Biomedical Engineering 40 422–437 [DOI] [PubMed] [Google Scholar]
- [33].Weber J, Beard PC and Bohndiek SE 2016. Contrast agents for molecular photoacoustic imaging. Nature Methods 13 639–650 [DOI] [PubMed] [Google Scholar]
- [34].Huynh E, Jin CS, Wilson BC and Zheng G 2014. Aggregate enhanced trimodal porphyrin shell microbubbles for ultrasound, photoacoustic, and fluorescence imaging. Bioconjugate Chemistry 25 796–801 [DOI] [PubMed] [Google Scholar]
- [35].Ju K-Y, Kang J, Pyo J, Lim J, Chang J and Lee J-K 2016. pH-Induced aggregated melanin nanoparticles for photoacoustic signal amplification Nanoscale 8 14448–14456 [DOI] [PubMed] [Google Scholar]
- [36].Moon H, Kang J, Sim C, Kim J, Lee H, Chang J and Kim H 2015. Multifunctional theranostic contrast agent for photoacoustics-and ultrasound-based tumor diagnosis and ultrasound-stimulated local tumor therapy J Control Release 218 63–71 [DOI] [PubMed] [Google Scholar]
- [37].Deán-Ben LX, Sela G, Lauri A, Kneipp M, Ntziachristos V, Westmeyer GG, Shoham S and Razansky D 2016. Functional optoacoustic neuro-tomography for scalable whole-brain monitoring of calcium indicators Light: Science Applications 5 e16201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Roberts S, Seeger M, Jiang Y, Mishra A, Sigmund F, Stelzl A, Lauri A, Symvoulidis P, Rolbieski H, Preller M, Deán-Ben LX, Razansky D, Orschmann T, Desbordes SC, Vetschera P, Bach T, Ntziachristos V and Westmeyer GG 2018. Calcium Sensor for Photoacoustic Imaging. J Am Chem Soc 140 2718–2721 [DOI] [PubMed] [Google Scholar]
- [39].Ruo B, Zhang R, Li L, Shao J-Y and Wang LV 2017. Photoacoustic imaging of voltage responses beyond the optical diffusion limit. Scientific Reports 7 2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Nowak K, Mix E, Nowak K, Strauss U, Gimsa J, Benecke R, perumbudur K and Gimsa U 2011. Optimizing a Rodent Model of Parkinson’s Disease for Exploring the Effects and Mechanisms of Deep Brain Stimulation Parkinson’s Disease 2011 414682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Zhang HK, Yan P, Kang J, Abou DS, Le HN, Jha AK, Thorek DL, Kang JU, Rahmim A, Wong DF, Boctor EM and Loew LM 2017. Listening to membrane potential: photoacoustic voltage-sensitive dye recording J Biomed Opt 22 045006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Johnston MV, Ammanuel S, O’Driscoll C, Wozniak A, Naidu S and Kadam SD 2014. Twenty-four hour quantitative-EEG and in-vivo glutamate biosensor detects activity and circadian rhythm dependent biomarkers of pathogenesis in Mecp2 null mice. Frontiers in Systems Neuroscience 8 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Medina-Ceja L, Pardo-Peña K, Morales-Villagrán A, Ortega-Ibarra J and López-Pérez S 2015. Increase in the extracellular glutamate level during seizures and electrical stimulation determined using a high temporal resolution technique BMC Neurosci 16 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Clay M and Monbouquette HG 2018. A Detailed Model of Electroenzymatic Glutamate Biosensors To Aid in Sensor Optimization and in Applications in Vivo. ACS Chem Neurosci 9 241–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Moon J-M, Thapliyal N, Hussain K, Goyal RN and Shim Y-B 2018. Conducting polymer-based electrochemical biosensors for neurotransmitters: A review. Biosensors & Bioelectronics 102 540–552 [DOI] [PubMed] [Google Scholar]
- [46].Sauleau P, Lapouble E, Val-Laillet D and Malbert C 2009. The pig model in brain imaging and neurosurgery Animal 3 1138–1151 [DOI] [PubMed] [Google Scholar]
- [47].Kang J, Boctor EM, Adams S, Kulikowicz E, Zhang HK, Koehler RC and Graham EM 2018. Validation of noninvasive photoacoustic measurements of sagittal sinus oxyhemoglobin saturation in hypoxic neonatal piglets. Journal of Applied Physiology 125 983–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].American National Standard for the Safe Use of Lasers. 1975. Annals of Internal Medicine 82 132 [Google Scholar]
- [49].Baumann MH, Ayestas MA, Partilla JS, Sink JR, Shulgin AT, Daley PF, Brandt SD, Rothman RB, Ruoho AE and Cozzi NV 2012. The designer methcathinone analogs, mephedrone and methylone, are substrates for monoamine transporters in brain tissue Neuropsychopharmacology 37 1192–1203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Elmore JS, Dillon-Carter O, Partilla JS, Ellefsen KN, Concheiro M, Suzuki M, Rice KC, Huestis MA and Baumann MH 2017. Pharmacokinetic Profiles and Pharmacodynamic Effects for Methylone and Its Metabolites in Rats Neuropsychopharmacol 42 649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Ludvig N, Mishra PK, Yan QS, Lasley SM, Burger RL and Jobe PC 1992. The combined EEG-intracerebral microdialysis technique: a new tool for neuropharmacological studies on freely behaving animals J Neurosci Meth 43 129–37 [DOI] [PubMed] [Google Scholar]
- [52].Westerink BH and Vries J 2001. A method to evaluate the diffusion rate of drugs from a microdialysis probe through brain tissue J Neurosci Meth 109 53–58 [DOI] [PubMed] [Google Scholar]
- [53].Paul DW and Stenken JA 2015. A review of flux considerations for in vivo neurochemical measurements Analyst 140 3709–3730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Bruhn T, Christensen T and Diemer NH 1995. Microdialysis as a tool for in vivo investigation of glutamate transport capacity in rat brain J Neurosci Meth 59 169–174 [DOI] [PubMed] [Google Scholar]
- [55].Airan RD, Meyer RA, Ellens NP, Rhodes KR, Farahani K, Pomper MG, Kadam SD and Green JJ 2017. Noninvasive Targeted Transcranial Neuromodulation via Focused Ultrasound Gated Drug Release from Nanoemulsions. Nano Lett 17 652–659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Kang S, Ammanuel S, Thodupunuri S, Adler D, Johnston M and Kadam S 2018. Sleep dysfunction following neonatal ischemic seizures are differential by neonatal age of insult as determined by qEEG in a mouse model. Neurobiology of Disease 116 1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.