Dear Editor:
With great interest, we read the paper “Nervous system involvement after infection with COVID-19 and other coronaviruses”. The authors speculated that SARS-CoV-2 may cause neurological damages (Wu et al., 2020). Herein, we provided clinical evidence showing the central nervous system (CNS) involvement for SARS-CoV-2.
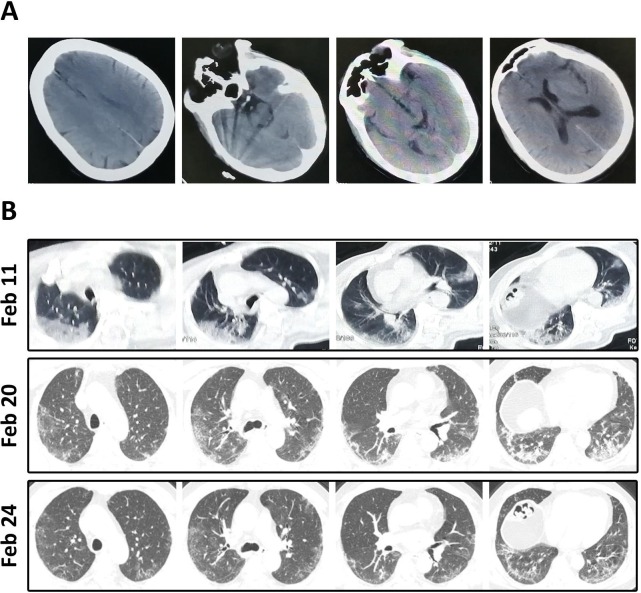
A Wuhan male had fever, shortness of breath, and myalgia since Jan 28. On Feb 10, his disease deteriorated and his consciousness suddenly progressed to confusion. Laboratory test indicated low WBC count (3.3 × 109/L) and lymphopenia (0.8 × 109/L). Skull computer tomography (CT) was normal (Fig. 1 A), while chest CT showed multiple subpleural ground glass opacities (GGOs) (Fig. 1B). The patient was positive for SARS-CoV-2 and sent to our institution. On physical examination, vital signs were stable without altered consciousness. Meningeal irritation signs (including nuchal rigidity, Kernig sign and Brudzinski sign) and extensor plantar response were present. Arterial blood gas analysis indicted PO2/FiO2 ratio of 240 mmHg. This COVID-19 patient was treated with arbidol and oxygen therapy, whereas his consciousness was not improved. Lumbar puncture was performed on Feb 16, and the cerebrospinal fluid (CSF) pressure was 220 mmHg. Laboratory tests with CSF showed WBC (0.001 × 109/L), protein (0.27 g/L), ADA (0.17 U/L) and sugar (3.14 mmol/L) contents within normal limits. The CSF specimen was further tested for SARS-CoV-2 but the result was negative. This patient did not have evidence of bacterial or tuberculous infection of the CNS. After careful evaluation by neurologic experts, encephalitis associated with SARS-CoV-2 infection was concluded. Treatment at this moment was largely supportive, including mannitol infusion. Intriguingly, the patient’s consciousness generally ameliorated since Feb 20, and chest CT suggested a resolution of GGOs (Fig. 1B). His consciousness was completely clear on Feb 24. Two consecutive throat swab tests were negative for SARS-CoV-2. The patient was discharged from hospital on Feb 27.
Fig. 1.
Representative CT images of the patient. (A) Skull CT was mostly normal. (B) On Feb 11, chest CT showed multiple GGOs in bilateral lungs. After indicated treatment, these GGOs were gradually resolved on Feb 20 and Feb 24, respectively.
This letter describes a COVID-19 case who presented as encephalitis. To the best of our knowledge, this is an unusual manifestation of COVID-19. Fortunately, encephalitic associate with SARS-CoV-2 is self-limited. Although the definitive diagnosis of viral encephalitis largely depends on virus isolation, this is difficult for COVID-19 because SARS-CoV-2 dissemination is transient and its CSF titer may be extremely low. Consistently, anti-SARS-CoV-2 IgM and IgG were not detectable in the patient’s CSF sample (unpublished data). Therefore, physical evaluation of neurological symptom is important to lead a presumptive diagnosis, as we have mentioned in this case. The pathophysiological characteristic of SARS-CoV-2 associated encephalitis is not fully understood. In agreement with Wu and colleagues (Wu et al., 2020), we speculate that SARS-CoV-2-induced immunologic response may cause inflammatory injury and edema, as a consequence, leading to alterations in consciousness. With the clearance of virus and the use of mannitol, the CSF pressure gradually reduces and the patient’s consciousness gradually improves. This might be a rational explanation for the self-limited property of SARS-CoV-2 associated encephalitis. Collectively, this report indicated that CNS may be involved in COVID-19 and highlights the diagnostic and therapeutic approaches to SARS-CoV-2 associated encephalitis.
Disclosure
Drs. Ye, Ren, and Lv are voluntary front-line clinicians in Wuhan Huoshensha Hospital.
Written informed consent was obtained from the patient.
References
- Wu Y. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]