Highlights
-
•
Adults who did not work in the outbreak were worse in mental and physical health, distress and life satisfaction.
-
•
The identification of whose health and wellbeing is more affected by the disruption enables more targeted assistance.
-
•
The early evidence from China can help countries that consider implementing confinement policies to contain COVID-19.
Keywords: Mental health, Physical health, Coronavirus, 2019-nCoV, Life disruptions, Exercising hours, Early evidence
Abstract
We assess the health and wellbeing of normal adults living and working after one month of confinement to contain the COVID-19 outbreak in China. On Feb 20–21, 2020, we surveyed 369 adults in 64 cities in China that varied in their rates of confirmed coronavirus cases on their health conditions, distress and life satisfaction. 27% of the participants worked at the office, 38% resorted to working from home, and 25% stopped working due to the outbreak. Those who stopped working reported worse mental and physical health conditions as well as distress. The severity of COVID-19 in an individual's home city predicts their life satisfaction, and this relationship is contingent upon individuals’ existing chronic health issues and their hours of exercise. Our evidence supports the need to pay attention to the health of people who were not infected by the virus, especially for people who stopped working during the outbreak. Our results highlight that physically active people might be more susceptible to wellbeing issues during the lockdown. Policymakers who are considering introducing restrictive measures to contain COVID-19 may benefit from understanding such health and wellbeing implications.
1. Introduction
Since the escalation of COVID-19 to a public health emergency in China on Jan 21, 2020, over a billion people across China have faced restrictions due to varying degrees of confinement such as banning public transport, restricting movement, and imposing a 14-day quarantine after travel (Li et al., 2020; Wang et al., 2020). One month into the outbreak, many people were still not working or exercising as usual, which may have associated implications on health and wellbeing. Yet, the implications of the unusually prolonged state of not working and exercising on individuals’ health and wellbeing remain unknown. It is important to understand not only the implications of the restrictions on COVID-19 disease prevalence rates but also the implications of such unprecedented disruptions on the health and wellbeing of the community (Brooks et al., 2020). From a policy perspective, understanding the health and wellbeing of people under the varying degrees of lockdown in China has implications for countries that are just starting to fight coronavirus, as such restrictions started in Korea, Italy, parts of the US, etc. in March (Moodie Davitt Report, 2020).
To control the COVID-19 outbreak, China has enacted restrictive measures “unprecedented in public health history” as stated by WHO (Reuters, 2020). On January 23, 2020, China locked down Wuhan, a metropolitan area of 12 million people (ABC News, 2020). The lockdown in Wuhan soon triggered similar measures in all 15 other cities in Hubei province with a total of 57 million people. Other prefectures (the administrative areas of a city) in China subsequently implemented varying levels of restrictive measures. For instance, the prefecture of Wenzhou in Zhejiang province restricted its citizens in such a way that only one person per household could leave home once every two days.
Such restrictive measures in China seemed to be effective in containing the spread of COVID-19 by mid-February and were applauded by WHO (The Washington Post, 2020). However, those measures have disrupted people's jobs and lives immensely and hence may have important implications for their health and wellbeing (Lima et al., 2020). For example, evidence from the SARS crisis indicated that reduced mobility affected the wellbeing of quarantined residents in a complex manner. Cao et al., 2020 found students in their medical college in China experienced more stress and anxiety during the outbreak. A paper in BMJ designed a COVID-19 Peritraumatic Distress Index to assess the distress level of people during Covid-19 outbreak (Qiu et al., 2020). These papers are critical because across the world people who did not carry the virus epidemiologically but had their work and life disrupted to varying degrees (Duan and Zhu, 2020; Xiang et al., 2020; Bao et al., 2020). In this article, we aim to use existing scales of health, distress and life satisfaction to identify the health and wellbeing of people one month into the disruption caused by confinement measures to contain COVID-19 outbreak by their work status, chronic health conditions, and exercising hours.
Understanding the health and wellbeing implications of the measures introduced to reduce the COVID-19 infection allows better-informed decisions. As many parts of the world are starting to consider measures to contain COVID-19, with South Korea and Italy having introduced lockdowns in early March 2020 (Cohen and Kupferschmidt, 2020), we may benefit from understanding the health and wellbeing implications of the measures implemented early on in China.
2. Methods
We conducted a cross-sectional survey one month into the COVID-19 outbreak on February 20–21, 2020, about one month into the COVID-19 emergency in China. All the participants were adults not infected by the virus epidemiologically but they lived in locations that were affected by COVID-19 to varying degrees. To cover people in areas of varying severity of COVID-19, we surveyed adults from 64 prefectures across China. The 64 prefectures were chosen to cover a wide spectrum of regions based on the severity of COVID-19 and should not be taken as a representative national sample. All respondents agreed to participate in the study, which was approved by the ethics committee at Tongji University (#20200211). We reached 529 adults, and 369 of them answered the survey, with a response rate of 69.8%. The participants were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
We assessed individual health by the Short Form-12 (SF12), a standard scale on mental and physical health function (Ware et al., 1996). The scale had been translated into Chinese and validated in China (Zhang et al., 2011). SF12 contains 12 items and 8 dimensions: physical functioning (2 items), role physical (2 items), bodily pain (1 item), general health (1 item), vitality (1 item), social functioning (1 item), role emotional (2 items) and mental health (2 items). The eight dimensions form two composite scores of physical and mental composite scale (PCS and MCS), with a possible score ranging from 0 to 100 (Ware et al., 2002). As a formative score, a higher SF12 score indicates a better health condition.
We measured distress by the six-item Kessler psychological distress scale (K6) with a Cronbach's alpha of 0.79 (Kessler et al., 2002). We measured life satisfaction with the Satisfaction With Life Scale (SWLS) (Diener et al., 1985), which consists of five items with a Cronbach's alpha of 0.72.
The adults also provided their socio-demographic characteristics, such as gender, age, education, and their location (prefecture). Using their locations, we searched for the number of confirmed COVID-19 cases in their prefectures on February 20 as well as the total population to calculate the number of confirmed cases per 10,000 people as an indicator of the severity of COVID-19 at their location. The number of cases per 10,000 people (i.e. infected rate) varied from 42.45 (Wuhan) to 0.01 on February 21 (National Health Commission of the PRC, 2020).
Because COVID-19 is more dangerous for people with comorbidity (Gates, 2020), it is likely that people who have ongoing medical issues would suffer more during the outbreak and therefore we asked whether the participants had any chronic disease. On the contrary, people who lead a healthy lifestyle and exercise often would be expected to fare better during the outbreak. Hence, we also asked the participants to indicate ‘how many hours did you exercise per day during the past week’.
The restrictive measures of COVID-19 also caused major disruption to people's work. By the time of our survey on February 20, the growth rate of COVID-19 cases in China had fallen to single percentages per day. Some people still stopped work, while some had returned to work in offices, and others were working at home. All individuals reported their work status.
We report the descriptive statistics of the study variables and the regression models to examine the relationships. The first and second author did the analyses on unweighted data with STATA 16.0, and statistical significance was assessed by p < 0.05.
3. Results
Table 1 presents the descriptive characteristics of the participants. From January 21 to February 20, in the one month of the restrictive measures, 124 (33.6%) of the participants had not left home at all, 51 (13.8%) had left their home only once, and 81 (22.0%) had left their home more than five times. At the time of the survey, 99 (26.8%) were going to work at their office; 93 (25.2%) had stopped working; and 139 (37.7%) resorted to working from home; 32 (8.7%) participants had not been working before the outbreak started; and 6 (1.6%) reported losing their work during the COVID-19 outbreak.
Table 1.
Descriptions of the participants (n = 369).
| Variable | Count or mean | Percentage |
|---|---|---|
| Gender | ||
| Male | 204 | 55.0% |
| Female | 165 | 45.0% |
| Age (years)Mean (SD) | 36.6 (10.5) | |
| Education level | ||
| Secondary school or below | 40 | 10.8% |
| High school or vocational school | 43 | 11.7% |
| Two-year college degree | 57 | 15.5% |
| Bachelor degree | 157 | 42.5% |
| Postgraduate degree | 72 | 19.5% |
| Marital status | ||
| Single | 105 | 28.5% |
| Married | 252 | 68.3% |
| Others (divorced, widowed, etc.) | 12 | 3.2% |
| Chronic disease | ||
| Yes | 45 | 12.2% |
| No | 324 | 87.8% |
| Job status | ||
| Worked at office | 99 | 26.8% |
| Worked at home | 139 | 37.7% |
| Stopped working | 93 | 25.2% |
| Not working before and during outbreak | 32 | 8.7% |
| Lost job during the outbreak | 6 | 1.6% |
| Total number of times out of home in the last month | ||
| Never | 124 | 33.6% |
| Once | 51 | 13.8% |
| Twice to five times | 113 | 30.6% |
| More than five times | 81 | 22.0% |
| Exercise hours per day in the past week | ||
| 0 | 51 | 13.8% |
| 0–1 | 226 | 61.2% |
| 1–2.5 | 63 | 17.1% |
| ≥2.5 | 29 | 7.9% |
| Health condition | ||
| Physical composite scale: Mean (SD) | 49.55 (7.00) | |
| Mental composite scale: Mean (SD) | 48.74 (9.30) | |
| Distress:Mean (SD) | 1.41 (0.46) | |
| Life satisfaction:Mean (SD) | 3.22 (0.64) |
Note: The scores of physical composite scale range from 27.54 to 63.83; the scores of mental composite scale range from 18.83 to 68.06; the scores of distress and life satisfaction both range from 1 to 5.
In terms of exercise, 51 (13.8%) people had not exercised at all during the past week; 226 (61.2%) exercised but for less than 1 h per day; 63 (17.1%) exercised 1–2.5 h per day; and 29 (7.9%) exercised more than 2.5 h per day. Of the participants, 45 (12.2%) had chronic diseases.
Based on the scoring algorithm of SF12,16 the participants scored 48.74 (SD 9.30) in mental health (MCS) and 49.55 (SD 7.00) in physical health (PCS). The mean values of distress and life satisfaction of the participants were 1.41 (SD 0.46) and 3.22 (SD 0.64) respectively.
3.1. People who worked in the office, worked at home, or had stopped working differed in health (SF12) and distress (K6)
Table 2 shows the results of regressing SF12 on the job status of the participants one month into the COVID-19 outbreak. Compared with people who stopped working during the outbreak, people who worked at their office had better mental health (β = 3.46, p = 0.01, 95% CI 0.79–6.14) and physical health (β = 2.19, p = 0.01, 95% CI 0.20–4.18). Moreover, people who worked at home also had better mental health than those who stopped working (β = 2.60, p = 0.03, 95% CI 0.05–5.16).
Table 2.
OLS regression results on the Mental Composite Scale (MCS) and Physical Composite Scale (PCS) of SF12 by job status.
| MCS | PCS | |||
|---|---|---|---|---|
| Coef. (s.e.) | 95% CI | Coef. (s.e.) | 95% CI | |
| Controls | ||||
| Gender | −0.28 (0.98) | [−2.21, 1.64] | 0.00(0.73) | [−1.43, 1.43] |
| Age | 0.03 (0.05) | [−0.07, 0.13] | −0.05 (0.04) | [−0.12, 0.02] |
| Education | −0.65 (0.41) | [−1.45, 0.15] | 0.44 (0.3) | [−0.15, 1.04] |
| Severity of COVID-19 | −0.01 (0.13) | [−0.26, 0.24] | 0.18 (1.01) | [0.00, 0.37] |
| Job status (stopped working is the default category) | ||||
| Worked at office | 3.46* (1.36) | [0.79, 6.14] | 2.19* (1.01) | [0.20, 4.18] |
| Worked at home | 2.60* (1.30) | [0.05, 5.16] | 0.96 (0.97) | [−0.95, 2.86] |
| Not working before and during outbreak | 0.62 (1.95) | [−3.20, 4.45] | 0.61 (1.45) | [−2.24, 3.46] |
| Lost work during the outbreak | 3.97 (3.92) | [−3.73, 11.67] | −4.80 (2.92) | [−10.53, 0.93] |
| Job status (worked at home is the default category) | ||||
| Worked at office | 0.86 (1.24) | [−1.57, 3.29] | 1.23 (0.92) | [−0.58, 3.04] |
| Stopped working | −2.60* (1.30) | [−5.16, −0.05] | −0.96 (0.97) | [−2.86, 0.95] |
| Not working before and during outbreak | −1.98 (1.89) | [−5.69, 1.73] | −0.35 (1.41) | [−3.11, 2.42] |
| Lost work during the outbreak | 1.36 (3.91) | [−6.33, 9.06] | −5.76* (2.91) | [−11.49, 0.03] |
Note: n = 369.
*p < 0.05.
We did further analysis on the eight specific dimensions of SF12. Compared with people who returned to work at their office, those who stopped working reported lower general health (β = −0.28, p = 0.03, 95% CI −0.55 to −0.03), mental health (β = −0.38, p = 0.002, 95% CI −0.63 to −0.14), and increased limitations for physical issues (β = −0.16, p = 0.009, 95% CI −0.28 to −0.04) and emotional issues (β = −0.13, p = 0.03, 95% CI −0.26 to −0.01). There were fewer differences between people who worked at home and worked at offices, except those who worked at home reported more limitations for physical issues than those who worked at offices (β = −0.13, p = 0.02, 95% CI −0.24 to −0.02).
There were also certain dimensions of SF12 that did not vary much by job status. For instance, people who stopped working and those who worked at their offices did not differ in bodily pain (β = 0.16, p = 0.16, 95% CI −0.06 to 0.39), physical function (β = 0.10, p = 0.14, 95% CI −0.03 to 0.24), and social function (β = 0.22, p = 0.26, 95% CI −0.16 to 0.59). Those who stopped working and those who worked at home respectively also did not differ in the same dimensions of bodily pain (β = 0.15, p = 0.19, 95% CI −0.07 to 0.36), physical function (β = 0.00, p = 0.96, 95% CI −0.13 to 0.13), and social function (β = 0.19, p = 0.29, 95% CI −0.17 to 0.55).
Similar findings emerged from the regression results on distress (K6) and life satisfaction (Table 3 ). People who worked at their office suffered less distress than people who stopped working (β = −0.13, p = 0.05, 95% CI −0.25 to 0.00). Also, people who worked at their office reported higher life satisfaction than those who stopped working (β = 0.23, p = 0.02, 95% CI 0.03–0.43).
Table 3.
OLS regression results on distress and life satisfaction by job status.
| Distress (K6) | Life satisfication | |||
|---|---|---|---|---|
| Coef. (s.e.) | 95% CI | Coef. (s.e.) | 95% CI | |
| Controls | ||||
| Gender | 0.03 (0.05) | [−0.06, 0.12] | 0.25⁎⁎ (0.05) | [0.11, 0.39] |
| Age | −0.00 (0.00) | [−0.01, 0.00] | 0.02⁎⁎⁎(0.00) | [0.01, 0.03] |
| Education | 0.05⁎⁎ (0.02) | [0.01, 0.08] | 0.03 (0.03) | [−0.03, 0.09] |
| Severity of COVID-19 | −0.00 (0.01) | [−0.01, 0.01] | −0.01 (0.01) | [−0.02, 0.01] |
| Job status (stopped working is the default category) | ||||
| Worked at office | −0.13* (0.06) | [−0.25, 0.00] | 0.23* (0.10) | [0.03, 0.43] |
| Worked at home | −0.06 (0.06) | [−0.18, 0.06] | 0.06 (0.10) | [−0.14, 0.25] |
| No work before and during outbreak | −0.15 (0.10) | [−0.34, 0.04] | 0.15 (0.15) | [−0.14, 0.44] |
| Lost work during outbreak | 0.22 (0.20) | [−0.17, 0.61] | 0.02 (0.29) | [−0.56, 0.59] |
| Job status (work at home is the default category) | ||||
| Worked at office | −0.07 (0.06) | [−0.18, 0.04] | 0.17 (0.09) | [−0.01, 0.36] |
| Stopped working | 0.06 (0.06) | [−0.06, 0.28] | −0.06 (0.09) | [−0.25, 0.14] |
| No working before and during outbreak | −0.09 (0.09) | [−0.27, 0.09] | 0.09 (0.14) | [−0.18, 0.37] |
| Lost work during the outbreak | 0.28 (0.20) | [−0.11, 0.66] | −0.04 (0.29) | [−0.61, 0.54] |
Note: n = 369.
*p < 0.05; ⁎⁎p < 0.01; ⁎⁎⁎p < 0.001.
3.2. Are people in areas more affected by COVID-19 less satisfied with their life? It depends
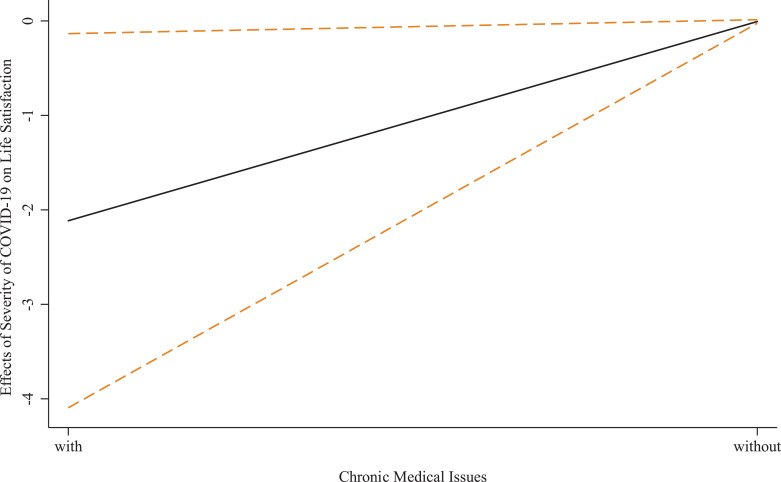
Next, we analysed how the severity of COVID-19 in individual locations predicts individuals’ life satisfaction. Table 4 shows that the relationship between the severity of COVID-19 and individual life satisfaction depends on individuals’ existing health and exercise status. The severity of COVID-19 had a negative relationship with the life satisfaction only for people with chronic medical issues (β = −2.11, p = 0.04, 95% CI −4.09 to −0.13) but not for people without chronic medical issues (β = −0.01, p = 0.51, 95% CI −0.02 to 0.01). We plot the effect of the severity of COVID-19 on life satisfaction by whether the individuals had chronic medical issues in Fig. 1 .
Table 4.
The severity of COVID-19 in a location interacts with individuals’ chronic health condition and exercise time to predict their life satisfaction.
| Life satisfaction | ||
|---|---|---|
| Coef. (s.e.) | 95% CI | |
| Controls | ||
| Gender | 0.25⁎⁎⁎ (0.07) | [0.10, 0.39] |
| Age | 0.02⁎⁎⁎ (0.00) | [0.01, 0.03] |
| Education | 0.04 (0.03) | [−0.01, 0.11] |
| Job status (worked at office is the default category) | ||
| Worked at home | 0.07 (0.06) | [−0.04, 0.18] |
| Stopped working | 0.13* (0.06) | [0.00, 0.25] |
| Not working before and during outbreak | −0.03 (0.09) | [−0.21, 0.16] |
| Lost work during the outbreak | 0.34 (0.20) | [−0.04, 0.73] |
| Severity of COVID-19 | −2.04* (0.99) | [−4.00, −0.08] |
| Chronic health condition1 | −0.20 (0.21) | [−0.61, 0.20] |
| Exercise hour | 0.04 (0.03) | [−0.01, 0.09] |
| Interaction | ||
| Severity of COVID-19 × chronic health condition | 2.08* (0.99) | [0.13, 4.04] |
| Severity of COVID-19 × exercise hours | −0.02⁎⁎ (0.01) | [−0.04, −0.01] |
Note: n = 369.
*p < 0.05; ⁎⁎p < 0.01. 1 = people with chronic disease, 2 = people without chronic disease.
Fig. 1.
.The effect of the severity of COVID-19 on life satisfaction depends on the chronic medical issues of the individuals.
Note: the dashed lines indicate 95% CIs.
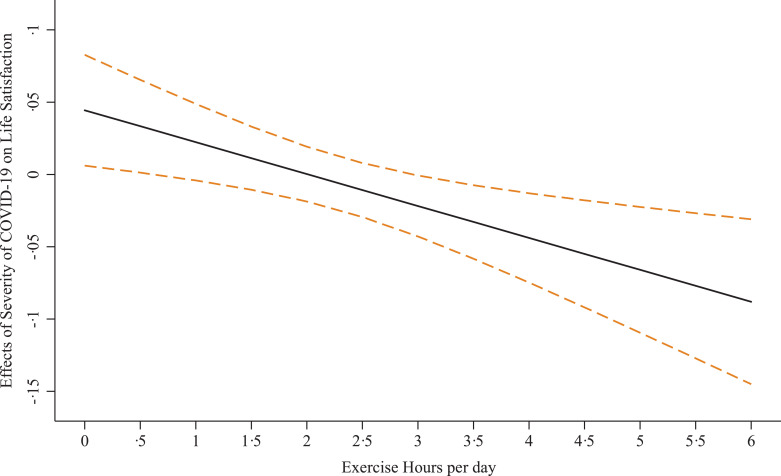
The results also indicate that the relationship between the severity of COVID-19 in a location and life satisfaction depends on individuals’ level of exercise, but in a direction opposite to our expectation. While we expected people who exercised more during the outbreak had a healthy lifestyle and would be less influenced, for people who exercised more than 2.5 h per day during the outbreak, the relationship between the severity of COVID-19 in their location and life satisfaction was significantly negative (e.g. for people who exercised 3 h per day: β = −0.02, p = 0.04, 95% CI −0.04 to 0.00). The relationship is not significant for people who exercised between 1 and 2.5 h a day during the outbreak. Surprisingly, for people who exercised 0.5 h or less per day during the outbreak, their life satisfaction was significantly positively associated with more affected locations (e.g. for people who did not exercise: β = 0.04, p = 0.02, 95% CI 0.01–0.08). We plot the effect of the severity of COVID-19 in the location on life satisfaction by the exercise hours of individuals in Fig. 2 .
Fig. 2.
The effect of the severity of COVID-19 on life satisfaction depends on the exercising hours of the individuals.
Note: the dashed lines indicate 95% CIs.
4. Discussion
Although the hardline restrictive measures in China showed success in containing COVID-19 after a month, there is little research on the extent to which the disruptions affected people in the community. Our findings show that adults who were not working reported worse health, as captured by SF12 in certain dimensions as well as distress (K6). The insignificant differences in the dimensions of SF12 in bodily pain, physical function and social function are expected, because people who were not infected by the virus directly would not differ much in those dimensions.
The results on life satisfaction are more nuanced. Overall, the severity of COVID-19 in a prefecture did negatively predict people's life satisfaction in that prefecture, with this relationship depending on individuals’ existing medical conditions and exercise levels. For individuals who exercised a lot during the outbreak (>2.5 h per day), life satisfaction was significantly negatively associated with more affected locations; on the contrary, for individuals who exercised half an hour a day or less, life satisfaction was significantly positively associated with more affected locations. Maybe these people could better justify or rationalize their inactive lifestyles in more severely affected cities. The finding that those who exercised a lot (>2.5 h per day) were less satisfied in more affected cities suggests we may need to pay attention to more physically active individuals, who might be more frustrated by the restrictions due to the outbreak.
The study has certain limitations. First, this study relied on an observational survey. Because the measures of the dependent variables of SF12, distress and life satisfaction used Likert scales, we tried to use predictors that were non-Likert scales, such as job status and severity of COVID-19 calculated based on archival data using the reported locations. Second, our sample is not a national representative sample. Our focus was to examine the differential effects on adults depending on the level of disruption, as captured by their job status, existing chronic issues, and exercise levels to identify who in the community of non-COVID-19 cases might need the most help for policymakers and potential caregivers. Third, even though we had data from people who had not been working even before the outbreak started (8.7%) and people who went out of work during the outbreak (1.6%), the sample size of those two groups was small and we are cautious not to report them in the findings. Nevertheless, people with these two job statuses could be important targets for future studies.
We provide preliminary evidence on the health conditions of adults in COVID-19 affected regions. The identification of who might be more affected by COVID-19, not epidemiologically but simply by working and living in affected regions, carries important implications. Such identification can help to prioritize those who might need more help, and psychologists, mental health professionals and social workers can provide services to start addressing at least the mental health issues, even during the lockdown. Affected regions are growing globally by the day, and COVID-19 is no longer confined to China (Cohen and Kupferschmidt, 2020). To contain COVID-19 transimission (Li et al., 2020), policymakers in other countries are considering implementing restrictive measures (Kupferschmidt and Cohen, 2020). We present this early evidence of disruptions one month into the outbreak to provide evidence on the health of the general community living and working under restrictive measures.
CRediT authorship contribution statement
Stephen X. Zhang: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing, Supervision. Yifei Wang: Validation, Visualization, Writing - original draft. Andreas Rauch: Writing - original draft, Writing - review & editing. Feng Wei: Investigation, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgement
The data collection was funded by the Chinese National Funding of Social Sciences (Grant number: 1509093).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.112958.
Appendix. Supplementary materials
References
- ABC News, 2020. Timeline: how coronavirus got started. https://abcnews.go.com/Health/timeline-coronavirus-started/story?id=69435165 (accessed 8 March 2020).
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G. The psychological impact of the COVID-19 epidemic on college students in China. Psychiat. Res. 2020 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J., Kupferschmidt K. Strategies shift as coronavirus pandemic looms. Science. 2020;367(6481):962–963. doi: 10.1126/science.367.6481.962. [DOI] [PubMed] [Google Scholar]
- Diener E.D., Emmons R.A., Larsen R.J., Griffin S. The satisfaction with life scale. J. Pers. Assess. 1985;49(1):71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiat. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates B. Responding to COVID-19—a once-in-a-century pandemic? N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Andrews G., Colpe L.J. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kupferschmidt K., Cohen J. Can china's COVID-19 strategy work elsewhere? Science. 2020;367(6482):1061–1062. doi: 10.1126/science.367.6482.1061. [DOI] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Zhao X., Sun Y. The lockdown of Hubei Province causing different transmission dynamics of the novel coronavirus (2019-nCoV) in Wuhan and Beijing. medRxiv. 2020 doi: 10.1101/2020.02.09.20021477. [DOI] [Google Scholar]
- Moodie Davitt Report, 2020. COVID-19 update: encouraging numbers from Korea; Italian lockdown; Japan suspends visas for Chinese and Korean visitors. https://www.moodiedavittreport.com/covid-19-update-encouraging-numbers-from-korea-italian-lockdown-japan-suspends-visas-for-chinese-and-korean-visitors/ (accessed 8 March 2020).
- National Health Commission of the PRC, 2020. Real-time tracking of new coronavirus outbreaks (in Chinese). https://news.qq.com/zt2020/page/feiyan.htm#/ (accessed 21 Feb 2020).
- Lima C.K.T., de Medeiros Carvalho P.M., Lima I.A.S. The emotional impact of coronavirus 2019-Ncov (New Coronavirus Disease) Psychiat. Res. 2020 doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuters, 2020. Wuhan lockdown 'unprecedented', shows commitment to contain virus: WHO representative in China. https://www.reuters.com/article/us-china-health-who-idUSKBN1ZM1G9 (accessed 8 March 2020).
- The Washington Post, 2020. Chinese officials note serious problems in coronavirus response. The World Health Organization keeps praising them.https://www.washingtonpost.com/world/asia_pacific/chinese-officials-note-serious-problems-in-coronavirus-response-the-world-health-organization-keeps-praising-them/2020/02/08/b663dd7c-4834-11ea-91ab-ce439aa5c7c1_story.html (accessed 10 March 2020).
- Qiu J., Shen B., Zhao M. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware J., Jr, Kosinski M., Keller S.D. A 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med. Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Ware J.E., Kosinski M., Turner-Bowker D.M., Gandek B. QualityMetric Incorporated; Boston: 2002. How to Score Version 2 of the SF-12 Health Survey (with a Supplement Documenting Version 1) [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiat. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Tian J., Liu Q.L., Zhou H.Y., He F.R., Ma X. Reliability and validity of SF-12 among floating population (in Chinese) Chin. J. Public Health. 2011;27(2):226–227. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.