Abstract
Introduction
and aims: To prevent the spread of coronavirus disease (COVID19) total lockdown is in place in India from March 24, 2020 for 21 days. In this study, we aim to assess the impact of the duration of the lockdown on glycaemic control and diabetes-related complications.
Materials and methods
A systematic search was conducted using Cochrane library. A simulation model was created using glycemic data from previous disasters (taken as similar in impact to current lockdown) taking baseline HBA1c and diabetes-related complications data from India-specific database. A multivariate regression analysis was conducted to analyse the relationship between the duration of lockdown and glycaemic targets & diabetes-related complications.
Results
The predictive model was extremely robust (R2 = 0.99) and predicted outcomes for period of lockdown up to 90 days. The predicted increment in HBA1c from baseline at the end of 30 days and 45 days lockdown was projected as 2.26% & 3.68% respectively. Similarly, the annual predicted percentage increase in complication rates at the end of 30-day lockdown was 2.8% for non-proliferative diabetic retinopathy, 2.9% for proliferative diabetic retinopathy, 1.5% for retinal photocoagulation, 9.3% for microalbuminuria, 14.2% for proteinuria, 2.9% for peripheral neuropathy, 10.5% for lower extremity amputation, 0.9% for myocardial infarction, 0.5% for stroke and 0.5% for infections.
Conclusion
The duration of lockdown is directly proportional to the worsening of glycaemic control and diabetes-related complications. Such increase in diabetes-related complications will put additional load on overburdened healthcare system, and also increase COVID19 infections in patients with such uncontrolled glycemia.
Keywords: Diabetes, Lockdown, Disaster, Multivariate regression analysis, Complications
1. Introduction
The World is experiencing a viral onslaught of herculean proportion in the form of COVID-19 (Coronavirus disease 2019) caused by SARS-CoV-2 (severe acute 69 respiratory syndrome coronavirus 2) [1]. Both the infection rate as well as death from COVID 19 have exhibited an exponential growth [2]. The whole attention now is on prevention and management strategies related to it. However, as the disease evolved, we learned that not all patient population are at equal risk of morbidity and mortality. The elderly and those with additional co-morbidities in the form of diabetes, hypertension and background cardiovascular compromise are at higher risk than those without these co-morbid diseases [3].
India houses the second largest population of patient with diabetes mellitus after China [4]. Although the pandemic of COVID 19 originated in China, unlike diabetes prevalence, India is, as yet, experienced lesser impact of COVID19 [5]. In an attempt to stem the spread of the virus from individuals travelling into India from endemic areas to internal community spread, a feature of the stage 3 of the disease process, a temporary 21 days lockdown (complete restriction on all international and domestic travel, social isolation, and suspension of all non-essential services) as announced by Prime Minister of India on 24th March 2020. On one hand this could be a vital step in stemming the spread of the virus, however, on the other there are likely to be issues related to the impact of this lockdown on patients with diabetes; the worsening of hyperglycaemia an increase in diabetes-related complications. This could be due to the limitation of free space to exercise, limited resources to implement a healthy lifestyle, restrictions on the availability of anti-hyperglycaemic agents and difficulty in obtaining of physician’s guidance. Further, because of limitations of transport of goods and movement of patients, there is likely to be shortage of drugs, insulin, and glucose testing strps and glucose meters. All these factors have the potential to increase the stress level and its associated impact on the pre-existing disease.
What impact will this lockdown have on the glycaemic target and diabetes-related complications? While it is difficult to collect real data, one could use a simulation model created with the aid of a multivariate regression analysis which could predict and answer these questions. We hypothesised that this lockdown of India for period of 21 days and beyond will lead to worsening of glycemia and later, increase in diabetes-related complications.
This analysis was planned to answer above stated hypothesis. In the absence of any previous data, we searched for scenarios very similar to the lockdown situation and zeroed in to several disasters (earthquakes, tsunamis, hurricanes and wars) which closely simulatea lockdown in so far as resource limitations and challenges are concerned [[6], [7], [8], [9], [10], [11]]. For baseline glycosylated haemoglobin (HBA1c/A1c) and associated diabetes-related complications for Indian population, data from DiabCare study was taken [12]. Using these parameters as baseline, this analysis was planned aiming at predicting the end-of-lockdown HBA1c as well as the diabetes-related complication rates thereof.
2. Materials and methods
A web-based search was conducted addressing diabetes control during times of disaster, when resources become scarce and lifestyle modification opportunities become constricted. This background was selected to simulate the proposed 21 days lockdown in India facing the menace of coronavirus outbreak. The disaster period was included to closely simulate the resource challenged atmosphere. A search of PubMed, Google Scholar and Cochrane library was conducted using following search terms; “disaster”, “diabetes mellitus”, “blood glucose targets” and “diabetic complications” as keywords. Subsequently, clubbing “disaster” and “diabetes mellitus” (yielded 7 citations) and then combined with “blood glucose targets” and “diabetes complications” (yielded 546 citations). As per pre-planned inclusion criteria, filters were imposed to include trials only, resulting in 7 studies available for analysis.
There were six citations related to disaster and diabetes mellitus which were included to analyse the predicted HBA1c at the end of the lockdown. The disasters included for analysis were hurricane Katrina (USA,2005, days considered as lockdown period - 8), Kobe earthquake (Japan,1995, days considered as lockdown period - 8), Hanshin-Awashi earthquake (Japan, 1995, days considered as lockdown period - 14), the Gulf war in Iraq (1991, days considered as lockdown period - 60), Murmura earthquake (Turkey, 1999, days considered as lockdown period – 21) and the Great Eastern Japan Earthquake and tsunami (Japan, 2011, days considered as lockdown period - 14). Data was collected in a comma separated-values (CSV) file and uploaded in Jupyter notebook and analysed with the Python 3.8.2 software (Windows 10 64 bit, USA). As a re-validation process and for simplicity of understanding, the data was also analysed using excel with XL-STAT statistical software (Windows 10 64 bit, USA). Once the post-lockdown HBA1c was available, the plan was to include the seventh citation, which was related to the Indian data on the mean HBA1c value of representative Indian population (2014) and the prevalent diabetes-related micro- & macro-vascular complications. This baseline data (DiabCare study) was collected over one year from 330 centres across the country resulting in surveying 6168 diabetic patients (12). Mean HBA1c as well as the annual rates of complications was collected in this cross-sectional study.
The final step planned was to predict the post lockdown complication rates depending on the predicted HBA1c and the duration of lockdown (in days). These data were calculated with the premise that current state of conditions of the patients and constrained resources continue, and that major intervention to control glycemia (introduction of new drugs and insulin, etc) were not carried out. .
3. Results
The results of this analysis are presented in five steps.
-
Step 1
The first step was to estimate the HBA1c increment observed during the time period of the respective disasters (Table 1).
-
Step 2
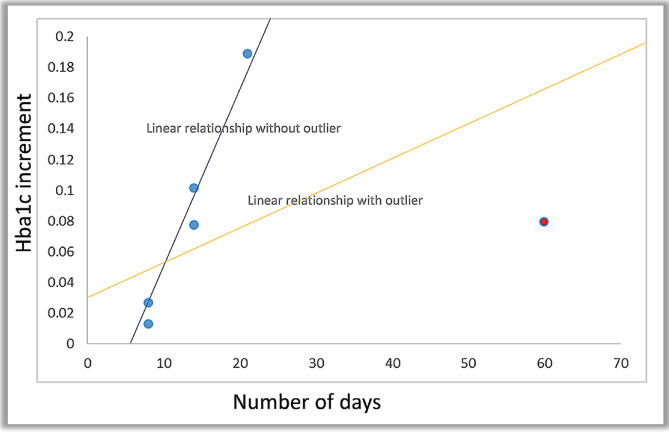
A linear regression analysis was performed between the number of days and the HBA1c increment (Fig. 1).
Table 1.
Analysis of the HBA1c increment from the pre- and post-disaster HBA1c levels with the number of days as an additional determinant.
| Disaster Name | Number of daysa | Baseline A1c | Post-disaster A1c | A1c % increment |
|---|---|---|---|---|
| KATRINA [6] | 8 | 7.5 | 7.6 | 0.01 |
| KOBE [7] | 8 | 7.44 | 7.64 | 0.03 |
| Hanshin-Awashi [8] | 14 | 7.74 | 8.34 | 0.08 |
| Gulf War [9] | 60 | 10.1 | 10.9 | 0.08 |
| Marmara [10] | 21 | 7.4 | 8.8 | 0.19 |
| GEJE Tsunami [11] | 14 | 5.9 | 6.5 | 0.10 |
Number of days indicate period where population was mostly resource challenged, facing challenges as enumerated in current lockdown in India.
Fig. 1.
Linear regression analysis between number of days and HBA1c increment with and without the significant outlier (Gulf war- )).
)).
The correlation analysis revealed a moderately good correlation between the post-disaster HBA1c & the duration of the disaster (r = 0.48) and a strong correlation with baseline HBA1C (r = 0.81)..
-
Step 3
A multivariate regression analysis was done revealing a very strong association between the inputs (days count and the baseline HBA1c) and the output (post-disaster HBA1c). The relationship between days count and post-disaster HBA1c was statistically significant (P = 0.009), as was the relationship between the baseline HBA1c and the post-disaster HBA1c (P = 0.004). The multivariate linear model was robust with a R2 = 0.99 and an adjusted R2 = 0.98 (Table 2).
Table 2.
Summary output of the multivariate regression analysis done between the inputs (days count and the baseline HBA1c) and the output (post-disaster HBA1c).
| SUMMARY OUTPUT | |
|---|---|
| Regression Statistics | |
| Multiple R | 0.996689185 |
| R Square | 0.993389331 |
| Adjusted R Square | 0.986778662 |
| Standard Error | 0.100311991 |
| Observations | 5 |
| ANOVA | |||||
|---|---|---|---|---|---|
| df | SS | MS | F | Significance F | |
| Regression | 2 | 3.024195009 | 1.512097504 | 150.2706253 | 0.006610669 |
| Residual | 4 | 0.020124991 | 0.010062496 | ||
| Total | 4 | 3.04432 | |||
| Coefficients | Standard Error | t Star | P-value | Lower 95% | Upper 95% | |
|---|---|---|---|---|---|---|
| Intercept | 0.947434847 | 0.523979061 | −1.808154022 | 0.212312463 | −3.201934786 | 1.307065091 |
| Days count | 0.094627913 | 0.009378432 | 10.08995067 | 0.009680104 | 0.054275779 | 0.134980048 |
| Baseline A1c | 1.041310725 | 0.06858315 | 15.18318611 | 0.004309824 | 0.746221249 | 1.336400201 |
The formula generated by the multivariate regression analysis was: Post-disaster A1c = b0+ (b1∗ number of days of lock-down) + (b2∗Baseline A1c). Inserting all the intercepts, the equation turns out to be: Post-disaster A1c = 0.95+ (0.09∗ number of days of lock-down) + (1.04∗Baseline A1c).
-
Step 4
The DiabCare India study (12) was taken as the reference for all baseline characteristics (baseline mean HBA1c in India as well as the diabetes-related complication rates prevalent at that HBA1c). Hence inserting the mean baseline HBA1c from the DiabCare study i.e. 8.9%, we calculated the post-disaster predicted HBA1c (Table 3). These predicted data should be accepted only if no major intervention (major changes in treatment by physician, initiation of insulin therapy etc.) is done.
-
Step 5
Having established the relationship between the days of lockdown and the predicted end-of-lockdown HBA1c, the posterior diabetes-related complication rates were calculated, taking the baseline data from the DiabCare study (12) at a baseline HBA1c of 8.9% (Table 3).
Table 3.
Predicted diabetes-related complication rates in proportion to the increasing duration of lockdown (30–90 days) and associated increase in HBA1C.
| Number of days of lock-down | Baseline A1c | Post-disaster A1c | Non-Proliferative diabetic retinopathy | Proliferative diabetic retinopathy | Photocoagulation | Microalbuminuira | Overt proteinuria | DPN | Amputation | MI | CVA | Infections | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ∗ | 8.9 | 11.0% | 11.6% | 5.8% | 36.5% | 11.3% | 41.4% | 11.6% | 3.4% | 1.9% | 2.1% | ||
| 30 | 8.9 | 11.16 | 13.8% | 14.5% | 7.3% | 45.8% | 14.2% | 51.9% | 14.5% | 4.3% | 2.4% | 2.6% | |
| 45 | 8.9 | 12.58 | 15.5% | 16.4% | 8.2% | 51.6% | 16.6% | 58.5% | 15.4% | 4.8% | 2.7% | 3.0% | |
| 60 | 8.9 | 14.00 | 17.3% | 18.2% | 9.1% | 57.4% | 17.8% | 65.1% | 18.2% | 5.3% | 3.0% | 3.3% | |
| 75 | 8.9 | 15.42 | 19.1% | 20.1% | 10.0% | 63.2% | 19.6% | 74.7% | 20.1% | 5.9% | 3.3% | 3.6% | |
| 90 | 8.9 | 16.84 | 20.8% | 21.9% | 11.0% | 69.0% | 21.4% | 78.3% | 21.9% | 6.4% | 3.6% | 4.0% | |
With increasing duration of the lockdown, the increment in HBA1c from baseline continues to increase and carries along with it the increasing annual complication rates. The annual predicted percentage increment in complication rates from baseline at the end of 30-day lockdown due to COVID19 pandemic was 2.8% for non-proliferative diabetic retinopathy, 2.9% for proliferative diabetic retinopathy, 1.5% for retinal photocoagulation, 9.3% for microalbuminuria, 14.2% for overt proteinuria, 2.9% for peripheral neuropathy, 10.5% for amputation, 0.9% for myocardial infarction, 0.5% for stroke and 0.5% for infections. The annual predicted percentage increment in complication rates from baseline at the end of 45-day lockdown due to COVID19 pandemic was 4.5% for non-proliferative diabetic retinopathy, 4.8% for proliferative diabetic retinopathy, 2.4% for retinal photocoagulation, 15.1% for microalbuminuria, 4.7% for overt proteinuria, 17.1% for peripheral neuropathy, 4.8% for amputation, 1.4% for myocardial infarction, 0.8% for stroke and 0.9% for infections..
4. Discussion
In this first of the kind analysis, we show substantial increase in HbA1C and diabetes-related complications in people with diabetes. While these data are estimates based on some assumptions, numbers generated are good enough to alert us to strengthen already challenged healthcare resources toward this high-risk population.
Achieving and maintaining good glycemic control (defined as an HBA1c <7.0%) is one of the primary requirements to reduce diabetes related complications [13,14]. It is also important to take into consideration that while the whole world is struggling to contain this deadly viral illness, focus on the co-morbidities facilitating the viral-related morbidities and mortality cannot be compromised. There is sufficient evidence to indicate that poor glycemic control and presence of organ dysfunction predisposes an individual infected with COVID19 to far greater risk of mortality than those without. Hence, it is of paramount importance to achieve as well as maintain good glycemic control for short as well as long term benefits during this pandemic.
One of the most worrisome factors is restriction to routine physician consultations. As a result, patients suffering from chronic diseases, although stable, are not offered the usual standards of care. Not only physicians, but also the para-medical staff numbers are reduced and channelized toward dedicated COVID19-related care. As a result, non-COVID related complications rate are expected to rise, which independently predispose these patients to acquire COVID19 infection.
This analysis was therefore designed to deduce the adverse impact of a total lockdown on glycemic targets and associated complications. This is likely to be the first study to make such a deduction. In the absence of any prior data on the same, a simulation model was created from the natural and unnatural disasters we faced in the past. Based on the simulation, a model was created to predict the adverse impact of COVID19 related lockdown on diabetes and related complications. There was a moderate correlation between the post-disaster HBA1c and the duration of the disaster (r = 0.48) and a strong correlation with the baseline HBA1c (r = 0.81). Based on this result a multivariate regression analysis was done revealing a very strong model to predict the post-lockdown HBA1c depending on the duration (in days) of the lockdown. Assuming a uniform baseline HBA1c derived from the DiabCare study which is the latest epidemiological database on diabetes and its complications in India, the post-lockdown HBA1c increases from baseline as the duration of lockdown got extended (example- HBA1c of +2.26% with a 30 days lockdown to +3.68% with 90 days lockdown). In addition, this increment in HBA1c permitted us to calculate the annual proportional increase in diabetes-related complications rate, which increased as the duration of lockdown increased.
To prevent the increase in HBA1c and associateddiabetes-related complications, a system must be put in place to facilitate patent doctor interface through telecommunication, online consultations, use of social media platforms which can bring the whole medical care at home in a virtual sense. Dedicated campaigns can be launched utilizing the audio-visual media encouraging lifestyle modifications at home. Further, government must put required mechanism to prevent shortages of medicines and insulins.
5. Limitations of this study
One of the main limitations of this study is the non-availability of diabetes-related outcomes in a lockdown. This was replicated by bringing in a scenario (natural & non-natural disasters) which is similar to, but not the same to as may occur in a lockdown. Clearly, there are a lot of differences, between a lockdown and a hurricane, earthquake or a tsunami.
The disasters that we have taken for analysis have occurred several years before (Gulf war was 29 years ago). Since then information flow and modes of virtual consultations have increased, and may help patients control their diabetes better. Further, information flow, availability of physicians, and drugs and resources varied in different countries, and may be, in general, better now than previously. These factors may lead to overestimation of risk in our model. However, the limited availability of resources needed to manage diabetes, being a bridging factor made us choose disasters as a prior for the analysis. Finally, any model-based prediction has its problem related to over-estimating the risk profile.
6. Strengths of this analysis
The principle strength of this analysis is the robustness of the multivariate regression model. It was both robust and statistically significant. Secondly, in the absence of any previous data available on a lockdown related situation, this was the case best scenario which could have been created in spite of all the limitations.
7. Conclusion
This is probably the first analysis to predict the adverse effect of a total lockdown on glycemic targets as well as diabetes-related complications. We demonstrated an incremental increase in both HBA1c as well as diabetes-related complications, with the increase in the duration of lockdown days. A pre-planned strategy must be put in place to prevent such a scenario as poorly controlled diabetes is an independent risk factor of mortality from COVID19.
Funding
None.
Declaration of competing interest
None to declare.
References
- 1.Chen Y., Li L. SARS-CoV-2: virus dynamics and host response. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30235-8. https://www.thelancet.com/action/showPdf?pii=S1473-3099%2820%2930235-8 [Online] Available at: Accessed on: 28th March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koczkodaj W.W., Mansournia M.A., Pedrycz W., Wolny-Dominiak A., Zabrodskii P.F., Strzaška D. 1000,000 cases of COVID 19 outside of China: the date predicted by a simple heuristic. Global Epidemiology. 2020 doi: 10.1016/j.gloepi.2020.100023. [Online] Available at:, Accessed on: 28th March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jordan R.E. Covid-19: risk factors for severe disease and death. A long list is emerging from largely unadjusted analyses, with age near the top. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 4.IDF diabetes Atlas. ninth ed. 2019. https://diabetesatlas.org/en/sections/demographic-and-geographic-outline.html [Online] Available at: Accessed on: 28th March 2020. [Google Scholar]
- 5.India COVID-19 tracker. 2020. https://www.covid19india.org/ [Online] Available at: Accessed on: 28nd March 2020. [Google Scholar]
- 6.Fonseca V.A., Smith H., Kuhadiya N., Leger S.M., Yau C.L., Reynolds K. Impact of a natural disaster on diabetes. Diabetes Care. 2009;32:1632–1638. doi: 10.2337/dc09-0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Inui A., Kitaoka H., Majima M., Takamiya S., Uemoto M., Yonenaga C. Effect of the Kobe earthquake on stress and glycemic control in patients with diabetes mellitus. Arch Intern Med. 1998;158:274–278. doi: 10.1001/archinte.158.3.274. [DOI] [PubMed] [Google Scholar]
- 8.Kirizuka K., Nishizaki H., Kohriyama K., Nukata O., Arioka Y., Motobuchi M. Influences of the Great Hanshin-Awaji earthquake on glycemic control in diabetic patients. Diabetes Res Clin Pract. 1997;36(3):193–196. doi: 10.1016/s0168-8227(97)00030-2. [DOI] [PubMed] [Google Scholar]
- 9.Rubinstein A., Koffler M., Villa Y., Graff E. The Gulf War and diabetes mellitus. Diabet Med. 1993;10:774–776. doi: 10.1111/j.1464-5491.1993.tb00163.x. [DOI] [PubMed] [Google Scholar]
- 10.Sengul A., Ozer E., Salman S., Salman F., Saglam Z., Sergin M. Lessons learnt from influences of the Marmara earthquake on glycemic control and quality of life in people with type 1 diabetes. Endocr J. 2004;51(4):407–414. doi: 10.1507/endocrj.51.407. [DOI] [PubMed] [Google Scholar]
- 11.Fujihara K., Saito A., Heianza Y., Gibo H., Suzuki H., Shimano H. Impact of psychological stress caused by the Great East Japan earthquake on glycemic control in patients with diabetes. Exp Clin Endocrinol Diabetes. 2012;120(9):560–563. doi: 10.1055/s-0032-1314873. [DOI] [PubMed] [Google Scholar]
- 12.Mohan V., Shah S.N., Joshi S.R., Seshiah V., Sahay B.K., Banerjee S. Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: results from the DiabCare India 2011 Study. Indian Journal of Endocrinology and Metabolism. 2014;18(3):370–378. doi: 10.4103/2230-8210.129715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bate K.L., Jerums G. Preventing complications of diabetes. Med J Aust. 2003;179(9):498–503. doi: 10.5694/j.1326-5377.2003.tb05655.x. [DOI] [PubMed] [Google Scholar]
- 14.Glycemic targets: standards of medical care in diabetes—2019. American Diabetes Association. Diabetes Care. 2019 Jan;42(Supplement 1):S61–S70. doi: 10.2337/dc19-S006. [DOI] [PubMed] [Google Scholar]