Introduction
In the United States, hepatocellular carcinoma (HCC), a highly lethal cancer with limited treatment options, is primarily caused by chronic infection with hepatitis B virus (HBV) or hepatitis C virus (HCV), non-alcoholic steatohepatitis (NASH) and excessive alcohol consumption.1 HCC development generally requires decades-long exposure to one or more risk factor.
HCC rates in the U.S. increased over several decades.1 This trend was largely attributed an HCV epidemic HCV during the 1960s-1980s and an increase in obesity-associated NASH. Based on data from 18 Surveillance, Epidemiology and End Results (SEER) cancer registries during 2000–2012, HCC rates were projected to increase ~2.8%/year through 2030 if observed trends continued into the future.2 However, a recent analysis of 13 SEER registries suggested HCC rates plateaued during 2010–2015.3 Here, we use data from 21 SEER registries to provide updated HCC rates through 2016.
Methods
HCC incidence data were obtained from SEER-21, population-based cancer registries covering 37% of the U.S. population. Cases were identified using International Classification of Diseases for Oncology, 3rd edition codes (site: C22.0; histology: 8170–8175).
Incidence rates were age-standardized to the 2000 US population, and estimated overall and by sex, age group and race/ethnicity. Annual percent changes (APCs) were estimated using Joinpoint regression which identifies statistically significant inflection points in rate trajectories.4 Rate ratios (RRs) comparing 2015 and 2016 were also estimated. We also estimated delay-adjusted rates of all liver/intrahepatic bile duct cancers (HCC-specific estimates are unavailable) to assess the potential impact of delayed reporting.5
Results
During 2000–2016, 119,078 HCC cases occurred in SEER-21 registries (rate=5.84/100,000). In 2016, rates were higher in men (10.6/100,000) than women (2.83/100,000), increased with age (20–34-year-olds: 0.23/100,000; ≥65-year-olds: 27.6/100,000), and were highest among American Indian/Alaska Natives (14.5/100,000) and Hispanics (9.74/100,000).
Overall, HCC rates increased 5.64%/year (p<0.001) during 2000–2007, 2.68%/year (p<0.001) during 2007–2013 and then plateaued starting in 2013 (APC=−1.44%/year; p=0.12; Figure 1, Supplemental table 1). Rates plateaued among men and women beginning in 2012 and 2013, respectively. For ≥65-year-olds, rates increased during the entire time period (APC=2.69%/year; p<0.001). In contrast, inflections and significant decreases occurred among 35–49-year-olds starting in 2006 (APC=−4.93%/year; p<0.001) and among 50–64-year-olds in 2014 (APC=−6.64%/year; p=0.04).
Figure 1:
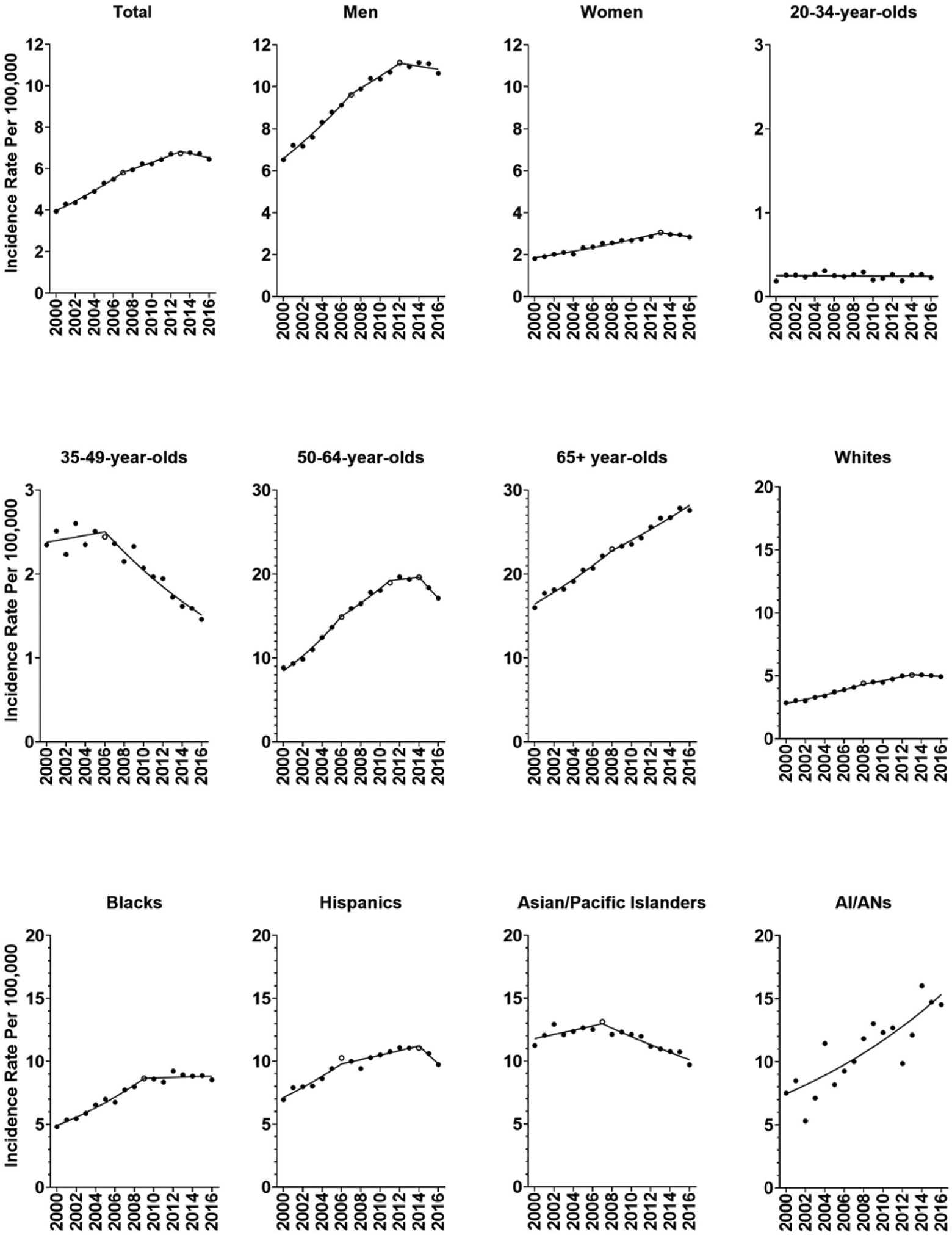
After years of strong increases, HCC rates plateaued among Whites beginning in 2013 (APC=−0.91%/year; p=0.45) and among Blacks in 2009 (APC=0.27%/year; p=0.65). Among Hispanics, HCC incidence decreased non-significantly (−6.55%/year; p=0.08) beginning in 2014. Among APIs, starting in 2007, HCC rates decreased −2.72%/year (p<0.001). In contrast, for American Indian/Alaska Natives, HCC rates increased 4.60%/year (p<0.001) across the time period.
Comparing rates in 2016 to 2015, we observed a significant decrease in HCC incidence overall (RR=0.96; p=0.007; Supplemental Table 1). Statistically significant (p<0.05) declines were present among men (RR=0.96), 50–64-year-olds (RR=0.93), Hispanics (RR=0.92) and APIs (RR=0.90). There were 171 fewer HCC cases in 2016 than 2015 (Supplemental Figure 1). The deficit was greater among men than women (−146 vs. −25 cases). By age group, the largest decrease in HCC cases was among 50–64-year-olds (−249 cases), while an increase occurred among ≥65-year-olds (+124 cases). By race/ethnicity, the largest decreases in HCC cases occurred among Hispanics (−80 cases) and APIs (−65 cases).
Similar declines occurred between 2015 and 2016 in analyses restricted to SEER-18 (RR=0.94; p=0.01) and SEER-13 (RR=0.94; p=0.0005) registries, and when liver/intrahepatic bile duct rates were estimated using delay-adjustment (RR=0.97; p<0.05).
Discussion
In the United States, HCC rates increased for decades and were projected to continue to rise through 2030.2 In that context, it is surprising that HCC rates flattened in 2013 and then declined in 2016.
It seems unlikely that this change reflects a decrease in HCC due to NASH or alcoholic liver disease, as the US obesity epidemic has not improved and alcohol-induced death rates have increased, including deaths due to cirrhosis.6 Improved treatment of viral hepatitis is likely to have contributed to the decline in HCC incidence. Treatment of chronic HBV, which can reduce HCC risk, has improved considerably with the introduction of effective nucleotide/nucleoside analogues in the mid-2000s.7 That timeframe is temporally consistent with the HCC decline among APIs, the demographic group most likely to have HBV-associated HCC.1
More recently, the availability of direct acting anti-viral agents (DAAs) against HCV has resulted in high cure rates even among patients with advanced fibrosis or cirrhosis who responded poorly to interferon-α based treatment.8 A prior study estimated that if 80% of HCV-infected individuals were treated with second generations DAAs, HCC rates would decline.2 These treatments were not available until late in 2014, therefore, DAA regimens cannot account for the plateau in HCC incidence starting in 2013 and are unlikely to fully account for the decrease in 2016. As HCV prevalence is highest in the “baby boomer” generation,1 an increase in HCC rates among 50–64-year-olds would have been expected with the aging of this cohort (to ~50–70 in 2016); however, rates plateaued and then declined in this age group, perhaps reflecting better HCV treatments. The Hispanic population contributed disproportionately to the decrease in HCC cases from 2015 to 2016 - the drivers behind this decline deserve further investigation. Trends varied across registries. Declines or plateaus observed in recent years occurred in 8 registries (representing 55% of HCCs), likely reflecting etiologic heterogeneity in HCC by region.
As SEER does not capture information about etiologic factors, possible explanations for changing HCC trends are speculative. Increased competing risk of death may also contribute to the decline in HCC risk, particularly given rising US death rates due to cirrhosis and drug use,9 which are both associated with viral hepatitis. Though it is premature to conclude that a long-term decrease in HCC has begun, the sensitivity analysis based on delay-adjusted rates provides reassurance that the decrease in 2016 is not an artifact. Further, the proportion of HCCs that were distant stage decreased from 15.9% (2004) to 13.9% (2016), suggesting that under-ascertainment is unlikely to have driven these findings.
Our analysis suggests the tide has begun to turn for HCC incidence in the United States. Future studies should monitor this trend and assess the factors that underlie these changing rates.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest to report. The study concept and design, interpretation of data and drafting of the manuscript were shared by Drs. Shiels and O’Brien. Dr. Shiels carried out the statistical analysis. This work was funded by the Intramural Research Program of the National Cancer Institute.
References
- 1.Islami F, Miller KD, Siegel RL, et al. Disparities in liver cancer occurrence in the United States by race/ethnicity and state. CA Cancer J Clin 2017;67:273–289. [DOI] [PubMed] [Google Scholar]
- 2.Petrick JL, Kelly SP, Altekruse SF, et al. Future of Hepatocellular Carcinoma Incidence in the United States Forecast Through 2030. Journal of Clinical Oncology 2016;34:1787–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rich NE, Yopp AC, Singal AG, et al. Hepatocellular Carcinoma Incidence Is Decreasing Among Younger Adults in the United States. Clinical Gastroenterology and Hepatology 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000;19:335–51. [DOI] [PubMed] [Google Scholar]
- 5.Midthune DN, Fay MP, Clegg LX, et al. Modeling reporting delays and reporting corrections in cancer registry data. Journal of the American Statistical Association 2005;100:61–70. [Google Scholar]
- 6.QuickStats: Age-Adjusted Death Rates* Attributable to Alcohol-Induced Causes,(dagger) by Race/Ethnicity - United States, 1999–2015. MMWR Morb Mortal Wkly Rep 2017;66:491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology 2018;67:1560–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Serag HB, Kanwal F, Richardson P, et al. Risk of hepatocellular carcinoma after sustained virological response in Veterans with hepatitis C virus infection. Hepatology 2016;64:130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shiels MS, Chernyavskiy P, Anderson WF, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet 2017;389:1043–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


