Abstract
Background:
Prior studies have suggested maltreatment is a strong predictor of later weight outcomes, such that maltreatment experiences in childhood increase the likelihood of being overweight or obese in adulthood. Estimates of this relationship may be biased due to: 1) inadequate selection of covariates; 2) improper operationalization of child maltreatment; and 3) restricting analyses to cross-sectional outcomes.
Objectives:
Evaluate how latent classes of child maltreatment experiences are associated with a longitudinal BMI measure from adolescence to adulthood.
Participants:
Data from the National Longitudinal Study of Adolescent to Adult Health.
Methods:
We evaluated how previously developed latent classes of child maltreatment experiences were associated with average excess BMI from adolescence to adulthood using multivariate linear regression.
Results:
In the unadjusted model, individuals in the poly-maltreatment class (b = 0.46, s.e. = 0.20) and individuals who experienced adolescent-onset maltreatment (b = 0.36, s.e. = 0.11) had higher average excess BMI compared to individuals in the no maltreatment class. After adjusting for confounders, the relationship between poly-maltreatment and average excess BMI abated, whereas the relationship between adolescent-onset maltreatment and average excess BMI sustained (b = 0.28, s.e. = 0.11).
Conclusions:
Contrary to previous findings, our analyses suggest the association between maltreatment experiences and longitudinal weight outcomes dissipates after controlling for relevant confounders. We did find a relationship, however, between adolescent-onset maltreatment and average excess BMI from adolescence to adulthood. This suggests the importance of maltreatment timing in the relationship between maltreatment and weight.
Keywords: Child maltreatment, body mass index, obesity, latent class analysis, directed acyclic graphs, longitudinal
Introduction
By the age of 18 years, over 13% of children in the United States have experienced a confirmed case of physical abuse, sexual abuse, or neglect perpetrated by a caregiver (Wildeman et al., 2014). Such child maltreatment places individuals at risk for various poor health outcomes, including—but not limited to—depression, asthma, sleep disorders, lower self-esteem, substance use, and risky sexual behaviors (Dunn, McLaughlin, Slopen, Rosand, & Smoller, 2013; Hillberg, Hamilton-Giachritsis, & Dixon, 2011; Lauterbach & Armour, 2016; Shenk, Griffin, & O’Donnell, 2015; Vachon, Krueger, Rogosch, & Cicchetti, 2015). As such, child maltreatment is a major public health issue, and the burdens of child maltreatment can be exacerbated through an unhealthy BMI trajectory (Cornette, 2008; De Niet & Naiman, 2011; French, Story, & Perry, 1995; Kelly et al., 2013; Kelsey, Zaepfel, Bjornstad, & Nadeau, 2014; Rank et al., 2013). Prior studies have suggested maltreatment is a strong predictor of later weight outcomes, such that maltreatment experiences in childhood increase the likelihood of being overweight or obese in adulthood (Danese & Tan, 2014; J. G. Noll, Trickett, Harris, & Putnam, 2009; J. G. Noll, Zeller, Trickett, & Putnam, 2007; Richardson, Dietz, & Gordon-Larsen, 2014; Williamson, Thompson, Anda, Dietz, & Felitti, 2002). However, these estimates of the relationship between maltreatment and weight outcomes may be biased for three major reasons: 1) inadequate selection of control variables; 2) improper operationalization of child maltreatment experiences; or 3) restricting analyses to cross-sectional health outcomes.
A competing hypothesis for the observed relationship between maltreatment experiences and longitudinal weight outcomes is the potential for maltreatment experiences to serve as an indicator—rather than a predictor—of future weight gain. It may be that maltreatment is associated with a variety of other factors that increase obesity risk (e.g., social class, parenting practices), rather than maltreatment directly causing future weight gain. For example, previous findings may be biased by observed and unobserved confounding factors, such as a parent’s latent propensity to neglect a child’s needs (regardless of whether or not a child is actually neglected). Although this latent propensity is an unobserved parenting characteristic, through careful selection of observed covariates, we can control for indicators of this variable—such as infant birthweight and breastfeeding—and reduce bias in our estimates (T. J. VanderWeele, Hernan, & Robins, 2008). However, previous studies’ covariate selections may be too narrow (e.g., only include demographic controls (Clark, Yang, McClernon, & Fuemmeler, 2015; Elsenburg, Smidt, & Liefbroer, 2017; Helton & Liechty, 2014; Richardson et al., 2014)); or too broad (e.g., include several variables that actually mediate the relationship between maltreatment and weight (Alvarez, Pavao, Baumrind, & Kimerling, 2007; Bentley & Widom, 2009; Schneiderman, Negriff, Peckins, Mennen, & Trickett, 2015)). In either case, analyses may result in biased estimates.
Second, maltreatment is characterized by multiple features: type, frequency, and developmental timing. Several studies that have investigated the relationship between child maltreatment and obesity, including Williamson and colleagues 2002 Adverse Childhood Experience Study (Williamson et al., 2002), have found that maltreatment types strongly co-occur. However, rather than investigating the relationship between profiles of maltreatment experiences (that can each contain multiple maltreatment types) and body weight, it has been conventional to investigate the associations between specific maltreatment types and body weight. Operationalizing maltreatment as a set of distinct variables simplifies a complex phenomenon and does not reflect actual experiences. Because this simplification does not represent reality, important nuances for intervention implications may be lost. To advance our understanding of how overall child maltreatment experiences relate to later health, Sokol and colleagues identified four latent classes of child maltreatment experiences (Sokol, Gottfredson, Shanahan, & Halpern, 2018), and we used these classes in the present analyses.
Third, measurement and assessment of weight outcomes are often cross-sectional and do not account for the trajectory of BMI. Because longitudinal BMI is predictive of later health outcomes above and beyond cross-sectional measures (Abdullah et al., 2012; Attard, Herring, Howard, & Gordon-Larsen, 2013; Boyer, Nelson, & Holub, 2015; Ding et al., 2016; Reis et al., 2013), there is a need to evaluate the relationship between child maltreatment and BMI over time. Considering BMI only at a single time point does not capture the cumulative burden of excess BMI across development. While previous work has evaluated the relationship between child maltreatment and longitudinal weight outcomes (J. G. Noll et al., 2009; Richardson et al., 2014; Schneiderman et al., 2015; Shin & Miller, 2012), these studies are subject to the previous two sources of bias—treating maltreatment types as a set of distinct variables and/or inadequate selection of control variables. Analyses need to address all three sources of bias simultaneously.
This study addressed the aforementioned barriers and evaluated if the present analyses supported a relationship between child maltreatment experiences and longitudinal weight outcomes. Aside from sources of bias, most studies that estimate the relationship between child maltreatment and longitudinal BMI have been conducted in samples that are either a majority or exclusively female (Danese & Tan, 2014), which restricts the generalizability of findings. Therefore, this study used longitudinal, nationally representative data to determine if overall child maltreatment experiences—characterized by type, frequency, and timing—was associated with BMI over time. We provided careful examination of this relationship through our selection of potential confounders. Better understanding the relationship between maltreatment experiences and longitudinal weight outcomes can help inform when, and to whom, potential obesity prevention interventions should be delivered.
Methods
Data Source
This study used data from the National Longitudinal Study of Adolescent to Adult Health (Add Health; P01-HD31921), a longitudinal study of a nationally representative sample of 20 745 adolescents in grades 7–12 in the U.S. during 1994–95 (K. Harris et al., 2016). We used data from Wave I (ages 13–21), Wave II (ages 13–21), Wave III (ages 18–28), and Wave IV (ages 2431). The University of North Carolina Institutional Review Board granted exemption from human subjects’ research approval for present analyses.
The final sample size was 17,669. Of the original 20,745 Add Health respondents, 117 did not fall into the desired age range at any collection waves, 1,826 did not have information on sampling weights, 1,133 had no recorded BMI measurements at any wave, 27 were underweight at all time points, and 2 had no information on biological sex.
Measures
Average excess BMI.
Average excess BMI from adolescence to young adulthood, developed and validated in previous work (Sokol, Gottfredson, Poti, et al., 2018), served as the focal outcome. This measure represents a person’s average deviance above a healthy BMI over a specified period. For example, as the upper limit of a healthy BMI range for adults is 25 kg/m2 (according to the Centers for Disease Control and Prevention), a person with a BMI of 28 kg/m2 at age 25 years would have an excess BMI of 3 kg/m2. With longitudinal data containing multiple BMI measurements, we modeled a person’s latent BMI trajectory and average their model-implied excess BMI over time to arrive at a numerical value for their average excess BMI. This measure simultaneously captures the longitudinal and continuous nature of weight outcomes, but it does not capture the timing of onset of an excess BMI.
Child maltreatment.
We operationalized child maltreatment experiences in a manner that did not require the mutual exclusion of maltreatment types, in line with previous research supporting the high co-occurrence of child maltreatment types (Kim & Cicchetti, 2010; Manly, Kim, Rogosch, & Cicchetti, 2001). A previous study using Add Health data employed a Latent Class Analysis (LCA) that uncovered patterns of childhood maltreatment experiences, and we used these classes as the focal predictor in the present study (Sokol, Gottfredson, Shanahan, et al., 2018). This operationalization of child maltreatment embodies overall patterns of maltreatment that simultaneously capture maltreatment timing, frequency, type(s), and type co-occurrence, to create a more accurate representation of an individual’s lived experience.
Methods for obtaining classes of child maltreatment via LCA are described in detail in Sokol et al., 2018. Briefly, study authors used indicators of child maltreatment assessed retrospectively at Waves III and IV to inform maltreatment experience classes. Questions at both waves asked respondents about the frequency of maltreatment types perpetrated by the primary caregiver, with responses ranging from never to ten or more times. These questions asked about neglect (i.e. How often had your parents or other adult caregivers not taken care of your basic needs, such as keeping you clean or providing food or clothing?), physical abuse (i.e. How often had your parents or other adult caregivers slapped, hit, or kicked you?), and sexual abuse (i.e. How often had one of your parents or other adult caregivers touched you in a sexual way, forced you to touch him or her in a sexual way, or forced you to have sexual relations?). To account for maltreatment timing, we only considered maltreatment indicators prior to age 12 years to inform maltreatment class assignment. The recovered child maltreatment experience classes included: 1) a poly-maltreatment class with high frequency of sexual abuse and co-occurring physical abuse and neglect (n = 1,025); 2) a physical abuse class with high frequency of physical abuse (n = 3,799); 3) a physical abuse and neglect class with high frequency of neglect and co-occurring physical abuse (n = 901); and 4) a no childhood maltreatment class (n = 11,944). We represented these classes by a series of indicator variables in analyses, with the no childhood maltreatment class serving as the reference group. We added a separate variable to indicate if maltreatment began after the age of 12 years (i.e., adolescent-onset maltreatment) in all analyses. In this manner, the adolescent-onset maltreatment variable was mutually exclusive from the child-onset maltreatment classes; by definition, an individual who experienced the onset of maltreatment in childhood could not have experienced their first maltreatment encounter during adolescence.
Covariates.
To address the potential that maltreatment experiences served as an indicator—rather than a predictor—of future weight gain, we used previous weight-related research on youth who experienced maltreatment, accompanied by our development of a Directed Acyclic Graph (DAG) using DAGitty v2.3 (Figure 1), to inform covariate selection. DAGs are conceptual tools used to represent causal relationships between variables relevant to a particular research question, with relationships specified based on existing evidence (Greenland, Pearl, & Robins, 1999; T. J. VanderWeele et al., 2008; Tyler J VanderWeele & Robins, 2007). In this manner, DAGs aid researchers in determining what variables to include as covariates to reduce confounding bias. Based on our DAG, this study controlled for variables that are direct risk factors of both the exposure (i.e., child maltreatment) and outcome (i.e., average excess BMI). In addition to controlling for direct risk factors of the exposure and outcome, DAGs demonstrate the necessity to control for some indicators of unobserved risk factors. In the present DAG, for example, whether or not an individual was breastfed directly influences an individual’s weight (Marseglia et al., 2015; Wang, Collins, Ratliff, Xie, & Wang, 2017). Although we assume that whether or not an individual was breastfed does not increase or decrease an individual’s likelihood of experiencing child maltreatment, we expect that whether or not a mother chooses to breastfed may reflect an underlying (and unobserved) propensity to neglect children (Kremer & Kremer, 2018)—this underlying propensity is a direct risk factor for child maltreatment, and thus the DAG demonstrated that the model should control for breastfeeding. The DAG also established that our model should not control for variables on the causal path between maltreatment and BMI—such as diet, physical activity, or pubertal status—as including these mediators would bias point estimates (Parsons, Power, Logan, & Summerbelt, 1999). For example, although previous work has established that early pubertal timing may cause higher BMI (Prentice & Viner, 2013), early pubertal timing is not a risk factor for child maltreatment—instead, child maltreatment places an individual at risk for earlier pubertal development (Jennie G. Noll et al., 2017). In this manner, pubertal status is an intermediate variable on the pathway between child maltreatment and average excess BMI, and controlling for it would result in biased coefficient estimates for the relationship between maltreatment and average excess BMI.
Figure 1.
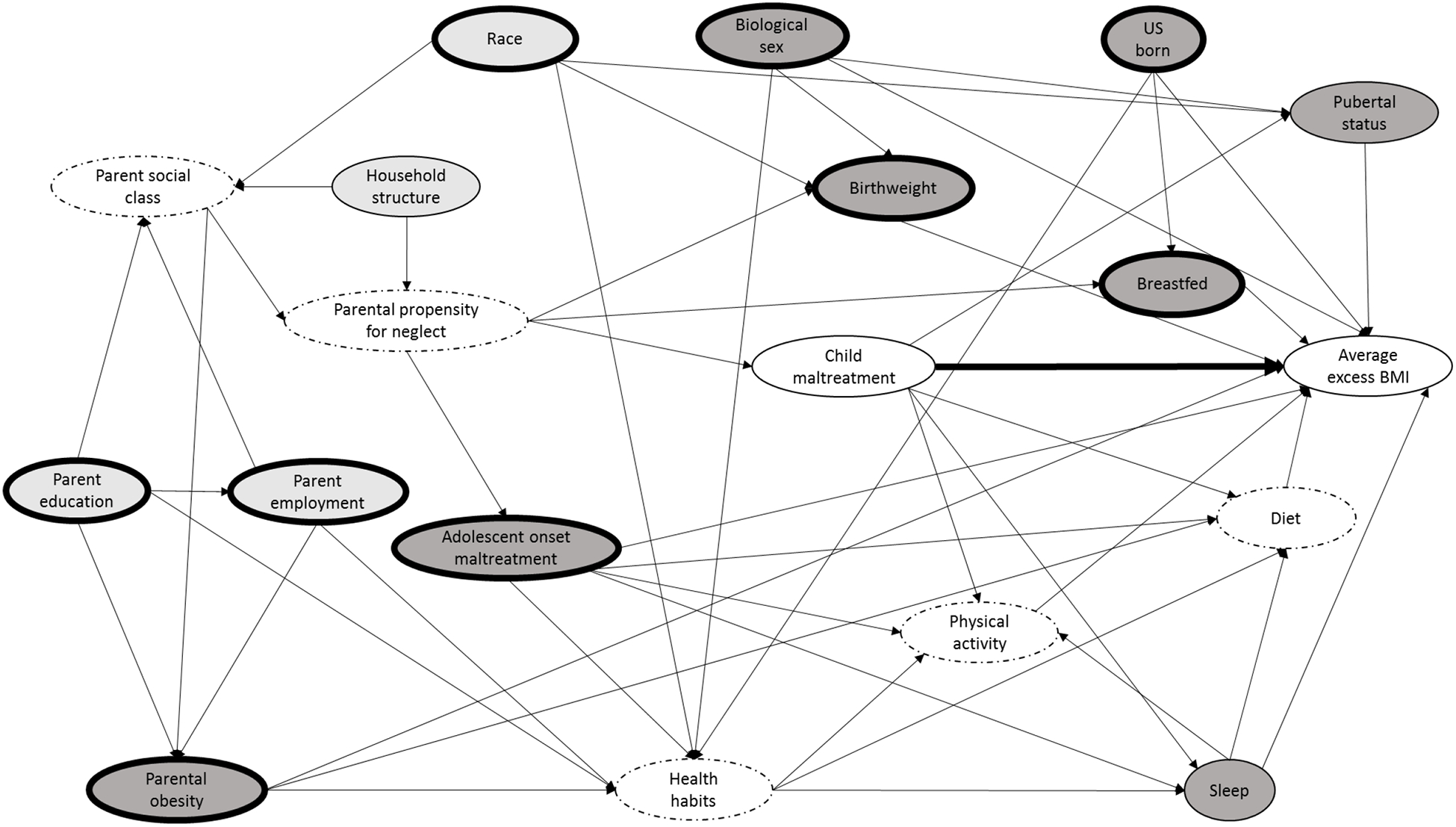
Directed acyclic graph (DAG) illustrating the causal diagram for the effect of child maltreatment on average excess BMI from adolescence to young adulthood.
Note: Arrows represent direct causal effects (i.e., the process determining the variable value at the end of an arrowhead is directly influenced by the status of the variable value at the arrow origin); Light gray ovals: Ancestor of exposure and outcome; Dark gray ovals: Ancestor of outcome; White ovals: Exposure (child maltreatment) and outcome (average excess BMI); Dotted borders: Latent (i.e., unobserved) variables; Bolded borders: Minimal sufficient adjustment set for estimating the total effect of ‘child maltreatment’ on ‘average excess BMI.’
According to our DAG informed by a review of the literature (K. M. Harris, Perreira, & Lee, 2009; Owen, Martin, Whincup, Smith, & Cook, 2005; Parsons et al., 1999), the minimum sufficient adjustment set for estimating the total effect of child maltreatment on average excess BMI included: biological sex (male or female); race/ethnicity (non-Hispanic Black, non-Hispanic White, Hispanic, other); parent education (less than high school, high school, some college, college graduate); parent employment (employed or unemployed); child birth weight (in ounces, mean-centered); if a child was exclusively breastfed for 6+ months (yes/no); if a child was born in the United States (yes/no); and if a biological mother or father was obese (yes/no).
Analytic Approach
We estimated linear regression models in a hierarchical manner to examine the association between child maltreatment experiences and average excess BMI. We first estimated an unadjusted model, looking at the relationship between maltreatment experience and average excess BMI. We then estimated a fully adjusted model, accounting for all covariates previously listed. We estimated models using Mplus version 7.4.© The variable with the highest degree of missingness was birthweight (missing for 6.4% of the sample). To account for missing data, we conducted 20 imputations with chained equations to impute values for all covariates, and we conducted analyses over these imputed datasets (Graham, Olchowski, & Gilreath, 2007). Due to Add Health’s complex survey design, analyses adjusted variance estimates to account for clustering and included sampling weights (Lumley, 2004).
Results
The average excess BMI of respondents—regardless of maltreatment class assignment—was 2.80 kg/m2. Notably, average excess BMI was significantly higher in the poly-maltreatment class (average: 3.11 kg/m2; range: 0–31.1 kg/m2) as compared to the no maltreatment class (average: 2.73 kg/m2; range: 0–34.3 kg/m2). Other covariates were not evenly distributed across maltreatment experience classes, and these significant differences between classes appear in Table 1. Specifically, the poly-maltreatment class had a lower percentage of male respondents (40.8%), a lower percentage of respondents who were breastfed for six months (15.9%), a lower percentage of white respondents (56.9%), and a lower percentage of parents with a college degree (21.5%), compared to individuals in the no maltreatment class. The un-stratified sample was evenly divided on biological sex (male = 50.5%), and was primarily white (65.5%), born in the United States (93.7%), normal birthweight (118.8 ounces), and not breastfed exclusively for six months (80.4%). Among the primary caregivers of respondents, at least one parent was likely to be college educated (30.2%) and employed (70.0%), and neither parent was likely to be obese (77.3%).
Table 1.
Descriptive statistics of the sample from the National Longitudinal Study of Adolescent to Adult Health (N = 17,669), stratified by latent class analysis maltreatment class.
| Variable | Total, or % | No maltreatment, or % | Physical abuse, or % | Physical abuse+ neglect, or % | Poly maltreatment, or % |
|---|---|---|---|---|---|
| Average excess BMI | 2.80 (4.19) | 2.73 (0.08) | 2.90 (0.14) | 2.97 (0.22) | 3.11 (0.18)* |
| Male | 51% | 50% | 52% | 62%*** | 41%*** |
| Parental obesity | 24% | 23% | 24% | 25% | 27% |
| Birthweight | 1.58 (19.9) | 1.65 (0.35) | 1.71 (0.60) | 1.32 (0.94) | 0.41 (1.12) |
| Breastfed | 20% | 20% | 22% | 14%** | 16%* |
| US born | 94% | 94% | 92%** | 93% | 93% |
| Parent employment | 70% | 70% | 69% | 69% | 67% |
| Race/ethnicity | |||||
| White | 66% | 68% | 64%* | 53%*** | 57%*** |
| Hispanic | 12% | 11% | 13% | 16% | 13% |
| Black | 16% | 16% | 14% | 21%* | 20%* |
| Other | 6.7% | 5.6% | 8.8%*** | 9.3%** | 9.6%* |
| Parent education | |||||
| < High school | 12% | 12% | 12% | 17% | 17%** |
| High school | 28% | 28% | 27% | 31% | 31% |
| Some college | 30% | 29% | 31%* | 33% | 31% |
| College graduate | 30% | 32% | 30% | 19%*** | 22%*** |
| n | 17,669 | 11,944 | 3,799 | 901 | 1,025 |
Note: Descriptive statistics are averaged over 20 imputed datasets and account for survey weighting and clustering. Birthweight and pubertal status are both mean-centered. Asterisks indicate significant differences from the “no maltreatment” class.
p < .05.
p < .01.
p < .001.
In the unadjusted model, both the poly-maltreatment class (b = 0.46, s.e. = 0.20) and individuals who experienced maltreatment onset during adolescence (b = 0.36, s.e. = 0.11) had significantly higher average excess BMI compared to individuals in the no maltreatment class (Table 2). After adjusting for relevant confounders, the relationship between the poly-maltreatment class and average excess BMI abated to non-significant levels (b = 0.19, s.e. = 0.20), whereas the relationship between maltreatment onset during adolescence and average excess BMI sustained (b = 0.28, s.e. = 0.11). Model fit improved upon inclusion of confounders (unadjusted: AIC = 101055.433, BIC = 101102.110; adjusted: AIC = 99586.849, BIC = 99726.881).
Table 2.
Regression analysis results for the relationship between child maltreatment class and average excess BMI, using data from the National Longitudinal Study of Adolescent to Adult Health (N = 17,669).
| Variable | Unadjusted model, coefficient (SE) | Adjusted model, coefficient (SE) |
|---|---|---|
| Physical abuse class | 0.16 (0.13) | 0.17 (0.12) |
| Physical abuse + neglect class | 0.22 (0.25) | 0.03 (0.24) |
| Poly-maltreatment class | 0.46 (0.20)* | 0.19 (0.20) |
| Adolescent onset maltreatment | 0.36 (0.11)** | 0.28 (0.11)* |
| R2 | 0.002 | 0.083 |
Note: Estimates are averaged over 20 imputed datasets and account for survey weighting and clustering. Asterisks indicate significant effects:
p < .05.
p < .01.
p < .001.
Adjusted model controls for: biological sex (male or female); race/ethnicity (non-Hispanic Black, non-Hispanic White, Hispanic, other); parent education (less than high school, high school, some college, college graduate); parent employment (employed or unemployed); child birth weight (in ounces, mean-centered); if a child was exclusively breastfed for 6+ months (yes/no); if a child was born in the United States (yes/no); and if a biological mother or father was obese (yes/no).
Discussion
The present study lends nuance to the association between child maltreatment and longitudinal weight outcomes by using a DAG-informed approach to inform covariate selection, considering the multiple features of maltreatment (type, timing, and frequency), and evaluating longitudinal weight outcomes as opposed to cross-sectional. Contrary to previous findings (Alvarez et al., 2007; Bentley & Widom, 2009; Helton & Liechty, 2014; J. G. Noll et al., 2009; Richardson et al., 2014; Schneiderman et al., 2015; Shin & Miller, 2012), our analyses suggest that the association between maltreatment experiences and longitudinal weight outcomes dissipates after controlling for relevant confounders.
This unexpected finding could be due to the motivation for this study: addressing analytic shortcomings and biases from previous analyses. Previous estimates may be biased due to: 1) inadequate selection of control variables; 2) improper operationalization of child maltreatment experiences; and 3) restricting analyses to cross-sectional health outcomes. Addressing any one of these issues may have resulted in a different pattern of results, and addressing these three issues at once provides greater confidence in our findings. However, whereas we did not detect a direct relationship between maltreatment experiences in childhood and longitudinal weight outcomes, the mechanisms driving weight outcomes might differ between individuals who have experienced maltreatment and the general population. For example, previous work has found that depressive symptoms mediate the relationship between physical abuse and BMI trajectories among girls (Sacks et al., 2017). Although equivalent longitudinal weight outcomes may be observed between individuals who have experienced child maltreatment and those who have not, intervention targets may differ between the groups—for example, targeting depressive symptoms among individuals who have experienced maltreatment versus targeting diet among the general population. Future analyses should investigate the potential for such differences.
Although the present findings suggested that child maltreatment in childhood is not causally associated with longitudinal weight outcomes, the unadjusted model indicates that individuals who have experienced multiple types of maltreatment in childhood have an average excess BMI that is, on average, 0.46 kg/m2 higher than that among individuals who have never experienced child maltreatment—a 17% increase in average excess BMI. Even though childhood maltreatment may not be the direct cause of this higher average excess BMI, clinicians should seek to understand patients’ maltreatment histories because these histories may represent a constellation of risk factors that increase an individual’s risk for poor weight outcomes. Moreover, future work should explore if obesity treatment and prevention strategies may be more effective among individuals who have experienced child maltreatment if delivered in a trauma-informed manner.
Whereas our adjusted model did not find a relationship between maltreatment experiences in childhood and average excess BMI, we did find a significant relationship between adolescent-onset maltreatment and average excess BMI from adolescence to young adulthood. No studies to our knowledge have considered if the relationship between maltreatment and weight is influenced by the age of maltreatment, yet the present analyses suggest the distinction between maltreatment onset in childhood versus adolescence may be important. Timing of first child maltreatment experience may influence health outcomes through various mechanisms, and these mechanisms likely depend on the health outcome of interest. For example, research has demonstrated early maltreatment is more deleterious than later maltreatment for psychopathology outcomes (Dunn et al., 2013), perhaps because early maltreatment compromises a child’s ability to master developmental milestones (Cicchetti & Rogosch, 2002). However, later exposures, such as those occurring during adolescence, might be more harmful for other health outcomes. The present analyses suggest later onset of maltreatment may carry consequences for longitudinal weight outcomes, whereas child onset maltreatment may not be as salient, perhaps because children have not developed the cognitive skills to realize maltreatment experiences (Garbarino, 1989; Garmezy & Rutter, 1983).
The present study carries limitations. Because maltreatment data were retrospectively reported by respondents without a validated instrument for assessing child maltreatment, the data are subject to recall and reporter bias. Due to the nature of the data, we were only able to capture maltreatment timing with respect to when maltreatment began—we did not have information regarding the duration of maltreatment, which may be an important aspect to consider in these relationships. Moreover, in selecting control variables, our DAG model may be subject to our own researcher biases. Additionally, although the present analyses accounted for maltreatment type, timing, and frequency in childhood, we did not account for these same features within adolescent-onset maltreatment. Future analyses should explore the relationship between adolescent-onset maltreatment experiences and longitudinal weight outcomes by considering both the type and frequency of maltreatment.
Conclusion
Although we did not find a relationship between various child maltreatment experiences and average excess BMI from adolescence to adulthood, we did find a significant, positive relationship between adolescent-onset maltreatment and average excess BMI. Future research should consider mechanisms underlying the relationships between adolescent-onset maltreatment and longitudinal weight outcomes in an effort to inform policy and intervention to improve health outcomes among this population.
Acknowledgments:
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Funding source: This work was supported by the National Institute of Child Health and Human Development (T32-HD07376), and by the National Institute on Drug Abuse of the National Institutes of Health (K01 DA035153). The funding sources had no involvement in the study design, data collection, analysis, interpretation, or writing of the report.
Footnotes
Declarations of interest: None
References
- Abdullah A, Wolfe R, Mannan H, Stoelwinder JU, Stevenson C, & Peeters A (2012). Epidemiologic merit of obese-years, the combination of degree and duration of obesity. Am J Epidemiol, 176(2), 99–107. doi: 10.1093/aje/kwr522 [DOI] [PubMed] [Google Scholar]
- Alvarez J, Pavao J, Baumrind N, & Kimerling R (2007). The relationship between child abuse and adult obesity among California women. American journal ofpreventive medicine, 33(1), 28–33. [DOI] [PubMed] [Google Scholar]
- Attard SM, Herring AH, Howard AG, & Gordon-Larsen P (2013). Longitudinal trajectories of BMI and cardiovascular disease risk: the national longitudinal study of adolescent health. Obesity, 21(11), 2180–2188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley T, & Widom CS (2009). A 30-year follow-up of the effects of child abuse and neglect on obesity in adulthood. Obesity, 17(10), 1900–1905. [DOI] [PubMed] [Google Scholar]
- Boyer BP, Nelson JA, & Holub SC (2015). Childhood body mass Index trajectories predicting cardiovascular risk in adolescence. Journal of Adolescent Health, 56(6), 599–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, & Rogosch FA (2002). A developmental psychopathology perspective on adolescence. Journal of consulting and clinical psychology, 70(1), 6. [DOI] [PubMed] [Google Scholar]
- Clark TT, Yang C, McClernon FJ, & Fuemmeler BF (2015). Racial differences in parenting style typologies and heavy episodic drinking trajectories. Health Psychol, 34(7), 697–708. doi: 10.1037/hea0000150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornette R (2008). The emotional impact of obesity on children. Worldviews Evid BasedNurs, 5(3), 136–141. doi: 10.1111/j.1741-6787.2008.00127.x [DOI] [PubMed] [Google Scholar]
- Danese A, & Tan M (2014). Childhood maltreatment and obesity: systematic review and meta-analysis. Molecular psychiatry, 19(5), 544–554. [DOI] [PubMed] [Google Scholar]
- De Niet JE, & Naiman DI (2011). Psychosocial aspects of childhood obesity. Minerva Pediatr, 63(6), 491–505. [PubMed] [Google Scholar]
- Ding M, Hu Y, Schwartz J, Koh WP, Yuan JM, Sesso HD, … Pan A (2016). Delineation of body mass index trajectory predicting lowest risk of mortality in U.S. men using generalized additive mixed model. Ann Epidemiol, 26(10), 698–703.e692. doi: 10.1016/j.annepidem.2016.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, McLaughlin KA, Slopen N, Rosand J, & Smoller JW (2013). Developmental timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: results from the National Longitudinal Study of Adolescent Health. Depress Anxiety, 30(10), 955–964. doi: 10.1002/da.22102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsenburg LK, Smidt N, & Liefbroer AC (2017). The Longitudinal Relation Between Accumulation of Adverse Life Events and Body Mass Index From Early Adolescence to Young Adulthood. PsychosomMed, 79(3), 365–373. doi: 10.1097/psy.0000000000000401 [DOI] [PubMed] [Google Scholar]
- French SA, Story M, & Perry CL (1995). Self-esteem and obesity in children and adolescents: a literature review. Obes Res, 3(5), 479–490. [DOI] [PubMed] [Google Scholar]
- Garbarino J (1989). Troubled youth, troubled families: The dynamics of adolescent maltreatment. Paper presented at the This chapter is based in part upon an invited address to Division 37 (Children, Youth, and Families) of the American Psychological Association annual convention, Aug 25, 1984, Toronto, Canada. [Google Scholar]
- Garmezy NE, & Rutter ME (1983). Stress, coping, and development in children. Paper presented at the Seminar on Stress and Coping in Children, 1979, Ctr for Advanced Study in the Behavioral Sciences, Stanford, CA, US. [Google Scholar]
- Graham JW, Olchowski AE, & Gilreath TD (2007). How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prevention Science, 8(3), 206–213. [DOI] [PubMed] [Google Scholar]
- Greenland S, Pearl J, & Robins JM (1999). Causal diagrams for epidemiologic research. Epidemiology, 37–48. [PubMed] [Google Scholar]
- Harris K, Halpern C, Whitsel E, Hussey J, Tabor J, Entzel P, & Udry J (2016). The National Longitudinal Study of Adolescent to Adult Health: Research Desig. 2009. URL: http://www.cpc.unc.edu/projects/addhealth/design. Accessed, 5.
- Harris KM, Perreira KM, & Lee D (2009). Obesity in the transition to adulthood: predictions across race/ethnicity, immigrant generation, and sex. Archives of pediatrics & adolescent medicine, 163(11), 1022–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helton JJ, & Liechty JM (2014). Obesity prevalence among youth investigated for maltreatment in the United States. Child abuse & neglect, 38(4), 768–775. [DOI] [PubMed] [Google Scholar]
- Hillberg T, Hamilton-Giachritsis C, & Dixon L (2011). Review of meta-analyses on the association between child sexual abuse and adult mental health difficulties: a systematic approach. Trauma Violence Abuse, 12(1), 38–49. doi: 10.1177/1524838010386812 [DOI] [PubMed] [Google Scholar]
- Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, … Daniels SR (2013). Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation, 128(15), 1689–1712. doi: 10.1161/CIR.0b013e3182a5cfb3 [DOI] [PubMed] [Google Scholar]
- Kelsey MM, Zaepfel A, Bjornstad P, & Nadeau KJ (2014). Age-related consequences of childhood obesity. Gerontology, 60(3), 222–228. doi: 10.1159/000356023 [DOI] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 51(6), 706–716. doi: 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremer KP, & Kremer TR (2018). Breastfeeding Is Associated with Decreased Childhood Maltreatment. Breastfeed Med, 13(1), 18–22. doi: 10.1089/bfm.2017.0105 [DOI] [PubMed] [Google Scholar]
- Lauterbach D, & Armour C (2016). Symptom Trajectories Among Child Survivors of Maltreatment: Findings from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN). J Abnorm Child Psychol, 44(2), 369–379. doi: 10.1007/s10802-015-9998-6 [DOI] [PubMed] [Google Scholar]
- Lumley T (2004). Analysis of complex survey samples. Journal of Statistical Software, 9(1), 1–19. [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, & Cicchetti D (2001). Dimensions of child maltreatment and children’s adjustment: contributions of developmental timing and subtype. Dev Psychopathol, 13(4), 759–782. [PubMed] [Google Scholar]
- Marseglia L, Manti S, D’Angelo G, Cuppari C, Salpietro V, Filippelli M, … Arrigo T (2015). Obesity and breastfeeding: The strength of association. Women Birth, 28(2), 81–86. doi: 10.1016/j.wombi.2014.12.007 [DOI] [PubMed] [Google Scholar]
- Noll JG, Trickett PK, Harris WW, & Putnam FW (2009). The cumulative burden borne by offspring whose mothers were sexually abused as children: descriptive results from a multigenerational study. JInterpers Violence,24(3), 424–449. doi: 10.1177/0886260508317194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noll JG, Trickett PK, Long JD, Negriff S, Susman EJ, Shalev I, … Putnam FW (2017). Childhood Sexual Abuse and Early Timing of Puberty. Journal of Adolescent Health, 60(1), 6571. doi: 10.1016/j.jadohealth.2016.09.008 [DOI] [PubMed] [Google Scholar]
- Noll JG, Zeller MH, Trickett PK, & Putnam FW (2007). Obesity risk for female victims of childhood sexual abuse: a prospective study. Pediatrics, 120(1), e61–67. doi: 10.1542/peds.2006-3058 [DOI] [PubMed] [Google Scholar]
- Owen CG, Martin RM, Whincup PH, Smith GD, & Cook DG (2005). Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics, 115(5), 1367–1377. [DOI] [PubMed] [Google Scholar]
- Parsons TJ, Power C, Logan S, & Summerbelt C (1999). Childhood predictors of adult obesity: a systematic review. International journal of obesity, 23. [PubMed] [Google Scholar]
- Prentice P, & Viner RM (2013). Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int J Obes (Lond), 37(8), 1036–1043. doi: 10.1038/ijo.2012.177 [DOI] [PubMed] [Google Scholar]
- Rank M, Siegrist M, Wilks DC, Langhof H, Wolfarth B, Haller B, … Halle M (2013). The cardio-metabolic risk of moderate and severe obesity in children and adolescents. J Pediatr, 163(1), 137–142. doi: 10.1016/j.jpeds.2013.01.020 [DOI] [PubMed] [Google Scholar]
- Reis JP, Loria CM, Lewis CE, Powell-Wiley TM, Wei GS, Carr JJ, … Liu K (2013). Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA, 310(3), 280–288. doi: 10.1001/jama.2013.7833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson AS, Dietz WH, & Gordon-Larsen P (2014). The association between childhood sexual and physical abuse with incident adult severe obesity across 13 years of the National Longitudinal Study of Adolescent Health. Pediatr Obes, 9(5), 351–361. doi: 10.1111/j.2047-6310.2013.00196.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks RM, Takemoto E, Andrea S, Dieckmann NF, Bauer KW, & Boone-Heinonen J (2017). Childhood Maltreatment and BMI Trajectory: The Mediating Role of Depression. Am JPrev Med, 53(5), 625–633. doi: 10.1016/j.amepre.2017.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneiderman J, Negriff S, Peckins M, Mennen F, & Trickett P (2015). Body mass index trajectory throughout adolescence: a comparison of maltreated adolescents by maltreatment type to a community sample. Pediatric obesity, 10(4), 296–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shenk CE, Griffin AM, & O’Donnell KJ (2015). Symptoms of major depressive disorder subsequent to child maltreatment: Examining change across multiple levels of analysis to identify transdiagnostic risk pathways. Dev Psychopathol, 27(4 Pt 2), 1503–1514. doi: 10.1017/s0954579415000905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SH, & Miller DP (2012). A longitudinal examination of childhood maltreatment and adolescent obesity: results from the National Longitudinal Study of Adolescent Health (AddHealth) Study. Child abuse & neglect, 36(2), 84–94. [DOI] [PubMed] [Google Scholar]
- Sokol RL, Gottfredson NC, Poti JM, Halpern CT, Shanahan ME, Fisher EB, & Ennett ST (2018). Does a parsimonious measure of complex body mass index trajectories exist? International journal of obesity. doi: 10.1038/s41366-018-0194-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol RL, Gottfredson NC, Shanahan ME, & Halpern CT (2018). Relationship between child maltreatment and adolescent body mass index trajectories. Children and Youth Services Review, 93, 196–202. doi: 10.1016/j.childyouth.2018.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vachon DD, Krueger RF, Rogosch FA, & Cicchetti D (2015). Assessment of the Harmful Psychiatric and Behavioral Effects of Different Forms of Child Maltreatment. JAMA Psychiatry, 72(11), 1135–1142. doi: 10.1001/jamapsychiatry.2015.1792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ, Hernan MA, & Robins JM (2008). Causal directed acyclic graphs and the direction of unmeasured confounding bias. Epidemiology, 19(5), 720–728. doi: 10.1097/EDE.0b013e3181810e29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ, & Robins JM (2007). Directed acyclic graphs, sufficient causes, and the properties of conditioning on a common effect. American Journal of Epidemiology, 166(9), 1096–1104. [DOI] [PubMed] [Google Scholar]
- Wang L, Collins C, Ratliff M, Xie B, & Wang Y (2017). Breastfeeding Reduces Childhood Obesity Risks. Child Obes, 13(3), 197–204. doi: 10.1089/chi.2016.0210 [DOI] [PubMed] [Google Scholar]
- Wildeman C, Emanuel N, Leventhal JM, Putnam-Hornstein E, Waldfogel J, & Lee H (2014). The prevalence of confirmed maltreatment among US children, 2004 to 2011. JAMA Pediatr, 168(8), 706–713. doi: 10.1001/jamapediatrics.2014.410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson D, Thompson TJ, Anda R, Dietz W, & Felitti V (2002). Body weight and obesity in adults and self-reported abuse in childhood. International journal of obesity. [DOI] [PubMed] [Google Scholar]


