Abstract
The benefits of expanding funding for Medicaid home- and community-based long-term care services (HCBS) relative to institutional care are often taken as self-evident. However, little is known about the outcomes of HCBS, especially for racial and ethnic minorities who tend to use HCBS more, and for people with dementia who may need high intensity care. Using national Medicaid claims data on elderly dual-eligibles, we found that overall hospitalization rates were similar for HCBS and nursing facility users, despite nursing facility users generally being sicker as reflected in their claims history. Among HCBS users, blacks were more likely to be hospitalized than whites, and the gap widened among blacks and whites with dementia. Also, conditional on receiving HCBS, Medicaid HCBS spending was higher for whites than non-whites; higher Medicare and Medicaid spending on hospitalizations for blacks and Hispanics did not offset this difference. Our findings suggest that HCBS need to be carefully targeted to avoid adverse outcomes and that the racial disparities in access to high-quality institutional long-term care are also present in HCBS. Policymakers should consider the full costs and benefits of shifting care from nursing facilities to HCBS and the potential implications for equity.
Introduction
Expanding the use of home- and community-based services (HCBS) as an alternative to institutional long-term care has become a priority for many state Medicaid programs. In 1996, only 19% of Medicaid long-term care expenditures were for HCBS relative to nursing facilities; by 2016, 57% of expenditures were for HCBS (1). Policymakers have motivated this shift in funding on the grounds that HCBS better serves individuals’ preferences to age in place and the belief that HCBS are less costly than nursing facility services. The benefits of this policy shift have been taken as self-evident in much of the policy discussion, with very little focus on the outcomes of HCBS for care recipients.
States have expanded Medicaid funding for HCBS largely through 1915(c) waivers(1). Under the waiver mechanism, Medicaid beneficiaries obtain access to HCBS only if their needs meet a nursing facility level of care. In other words, HCBS funds are explicitly directed toward providing an alternative to more expensive nursing facility care, and policymakers take pains to avoid a “woodwork” effect where people who otherwise wouldn’t receive services are encouraged by the availability of HCBS to sign up. Some expansion to healthier individuals has nonetheless occurred, but the increased intensity of funding for sicker individuals-–consistent with the goal of keeping people out of nursing facilities--remains the more pronounced trend(2).
Many waivers are meant to provide HCBS options for frail, elderly beneficiaries with long-term care needs. In this study, we focus on the subset of the elderly who are enrolled in both Medicare and Medicaid, known as “dual-eligibles”, who are often physically and cognitively impaired, are disproportionately from racial or ethnic minority groups, and have high use of health care services and costs. In 2013, duals accounted for 15% of Medicaid enrollment but 32% of Medicaid expenditures and 20% of Medicare enrollment but 34% of Medicare expenditures(3). Thus, Medicaid programs may see HCBS options as a way to reduce spending on dual-eligibles. At the same time, these beneficiaries often face challenges navigating care across the Medicaid and Medicare programs, making them vulnerable to poor outcomes.
The benefits of HCBS to care recipients and their families, especially in terms of preferences to age in place and increased quality of life, may be substantial and have not been well quantified. However, it is not clear that health outcomes should be better under HCBS than in nursing facilities, and in fact outcomes might be worse. HCBS generally entails lower intensity care relative to the round-the-clock care available in a nursing facility. Furthermore, HCBS shifts some of the care burden from trained, paid staff to largely untrained family or friends who must fill the critical gaps in care intensity. Home environments may not be safe or appropriately designed to accommodate needs, home care workers may face challenges implementing high-intensity treatments in the home environment, and informal caregivers may not be well trained to handle clinical issues. Thus, HCBS could lead to worse health outcomes relative to nursing facility care.
The challenges of HCBS may have particularly large implications for racial and ethnic minorities, who are disproportionally represented among Medicaid long-term care users(4). Historically, blacks and Hispanics have demonstrated different patterns of use than non-Hispanic whites, with minority groups using fewer institutional services and more home care and informal care(5–8). Additionally, when minorities use long-term care services, they tend to receive lower quality care (9–11). Given these differences in use and quality, policies emphasizing HCBS may exacerbate differences in outcomes by race group, especially if the intensity of care in HCBS is lower than what is needed.
In addition to implications for racial and ethnic disparities, any negative outcomes of HCBS use are likely to be exacerbated for sicker care recipients, especially those with Alzheimer’s disease and other dementias (hereafter referred to as dementia). Caring for individuals with dementia can be more stressful than for other conditions. Costs to caregivers of persons with dementia, such as lost work productivity and caregiving-related health problems, are substantial(12). Caregiver stress exists even with nursing facility placement(13) but is especially burdensome in the home. As informal caregivers are a critical part of the care team under HCBS, the presence of dementia may exacerbate caregiver burden such that outcomes for the care recipient suffer.
Despite the dramatic shift in Medicaid funding, we know surprisingly little about outcomes of HCBS relative to alternatives. There have been evaluations of specific types of HCBS programs or demonstrations which find that HCBS use is beneficial to care recipients (14–16), but these results are not likely to be broadly generalizable to elderly, dual-eligible HCBS users. A recent report examines high-cost HCBS users defined by Medicaid spending only, thereby focusing largely on under-65 non-dual Medicaid beneficiaries(17). Several studies have documented high rates of potentially avoidable hospitalizations among HCBS users (18,19), but did not provide comparisons. In two key studies that compared rates of potentially preventable hospitalizations among elderly, dually eligible HCBS users relative to nursing facility residents, results suggested that HCBS users were more prone to hospitalization than similar nursing facility residents (20,21); however, these studies were limited to individuals in seven states in 2003–2005 and did not examine differences by race or dementia.
Our study builds on prior literature to inform policy in several ways. First, we provide sorely needed evidence on HCBS use and key associated outcomes among dual-eligibles. Second, we use national claims data. Our study constitutes an important first step to help policymakers evaluate the effects of current policy in shifting resources from nursing facilities to HCBS, especially the effects of this shift on the most vulnerable groups among Medicaid long-term care users, non-whites and those with dementia.
Study Data and Methods
We use the 2012 national Medicaid Analytic eXtract (MAX) linked with Medicare claims to describe Medicaid long-term care utilization. The MAX is a claims-based dataset created by the Centers for Medicare and Medicaid Services from data submitted quarterly by the states. 2012 is the most recent year all states are included in the MAX(22). We identify Medicaid long-term care program enrollment, service use, and expenditures from the MAX person summary and claims files. We then link to Medicare records at the individual level. The Master Beneficiary Summary Files (MBSF) are used to identify demographic characteristics (age, sex, race and ethnicity), managed care enrollment, and chronic conditions. The MedPAR file is used to identify hospitalizations.
To identify the study target population, we first identify long-term care users who are dually enrolled in Medicare and Medicaid and elderly (aged 65+). Following prior literature (18)(23), we identify long-term care users through Medicaid waiver enrollment and fee-for-service (FFS) claims. HCBS is identified from 1915(c) HCBS waivers, state plan services, and Program of All-Inclusive Care for the Elderly (PACE) enrollment. Refer to Appendix Table A1 for a full list of services and associated codes used to identify long-term care users(24). We then use the MBSF to identify long-term care users who are duals and elderly, approximately 31% of all Medicaid FFS long term-care users.
We make several exclusions to the main analysis sample. First, we exclude three states from the sample, Arizona, Hawaii, and New Mexico, because more than 50% of long-term care users in those states were enrolled in managed long-term services and supports plans. We also limit to the 98% of long-term care users who have complete demographic information and with race coded as non-Hispanic white, non-Hispanic black, Hispanic, or Asian. For analysis of expenditures and hospitalizations, we make two further restrictions. First, we exclude the approximately 20% of long-term care users who are enrolled in Medicare managed care because we rely on FFS claims to identify hospitalizations. We also exclude those individuals who died during the year so all observations in the sample have the same exposure time. Refer to Appendix Table A2 for a tabulation of the sample restrictions(24).
Key variables for stratification in the analyses are race and ethnicity and dementia diagnosis. Beneficiary race and ethnicity is identified using the MBSF RTI race variable(25). An individual is identified as having dementia if he/she met the claims criteria for the Alzheimer’s disease and related disorders or senile dementia chronic conditions flag in either the MAX or Medicare chronic conditions supplement files(26). Hospitalizations are identified using the MedPAR files and are classified as potentially avoidable using the AHRQ Prevention Quality Indicator algorithms(27). Finally, Medicaid expenditures for long-term care are calculated from the MAX claims while hospital expenditures are summed over the Medicaid and Medicare payment amounts.
Analysis
We describe characteristics of Medicaid long-term care users overall and by care setting (institutional only, HCBS only, or both). Because distributions of age and sex are different across race groups, we adjust our main results for both age and sex.
To examine our subpopulations of interest, we calculate rates of use of each setting by race and dementia. To examine outcomes by care setting, we compare hospitalization rates--all hospitalizations and those that are potentially avoidable--across care settings and by race and dementia. Finally, focusing on HCBS users, we examine annual long-term care and inpatient hospital expenditures by race and dementia. We perform several sensitivity analyses, described briefly in the Results section and in more detail in the appendix(24).
Limitations
Although our study offers distinct advantages over prior evidence, our results are subject to several limitations. First, our analysis is descriptive, and the results should be interpreted as associations, rather than causal relationships. Second, our measure of dementia is binary and does not allow for analysis by stage of dementia. Third, we do not provide a full accounting of Medicare and Medicaid program costs for long-term care users, instead focusing on the subset of program expenditures that are most relevant to our purposes, namely FFS spending on hospitalization across Medicare and Medicaid and Medicaid long-term care. Finally, we only examine FFS long-term care services because we cannot reliably identify services delivered under managed care arrangements(28,29). These results may not be generalizable to beneficiaries who are non-elderly, non-dual-eligible, or in a managed care plan. In 2012, approximately 389,000 individuals, or 6.8% of long-term care users, received long-term care through managed care plans(30).
Results
We identify 5.36 million individuals as Medicaid long-term care users in 2012, of whom approximately 1.69 million are elderly, dual-eligible long-term care users. Exhibit 1 describes the characteristics of this main analysis sample. Just over half (51.7%) of the sample has been diagnosed with dementia. The mortality rate is high (14.4%) and approximately two-thirds (67.0%) of individuals had four or more chronic conditions, illustrating the relatively poor health of this group.
Exhibit 1:
Long-term care user sample characteristics, by long-term care setting
| Overall | Inst. Only | HCBS Only | Both | |
|---|---|---|---|---|
| White, non-Hispanic | 57.3 | 73.9 | 48.2 | 65.9 |
| Black, non-Hispanic | 19.0 | 16.4 | 20.0 | 19.2 |
| Hispanic | 14.8 | 7.3 | 19.0 | 10.2 |
| Asian | 9.0 | 2.3 | 12.8 | 4.6 |
| Dementia | 51.7 | 81.6 | 34.1 | 73.1 |
| Died | 14.4 | 22.7 | 8.9 | 23.8 |
| Age 65–69 | 14.8 | 8.8 | 17.9 | 12.9 |
| Age 70–74 | 16.6 | 11.1 | 19.4 | 14.6 |
| Age 75–79 | 17.5 | 13.8 | 19.3 | 16.4 |
| Age 80–84 | 18.2 | 18.1 | 18.3 | 18.3 |
| Age 85–89 | 16.7 | 21.1 | 14.3 | 18.7 |
| Age 90+ | 16.2 | 27.1 | 10.8 | 19.0 |
| Female | 72.1 | 73.9 | 71.7 | 70.5 |
| Eligibility group - Aged | 87.9 | 96.0 | 83.7 | 90.6 |
| Disabled | 11.7 | 3.1 | 16.0 | 9.2 |
| Other (child, adult, unknown) | 0.4 | 0.8 | 0.3 | 0.2 |
| 4+ chronic conditions | 67.0 | 70.2 | 62.3 | 82.5 |
| Medicaid comprehensive managed care plan enrolled | 9.4 | 4.1 | 13.1 | 3.2 |
| Medicare Advantage enrolled | 19.3 | 14.3 | 22.7 | 13.7 |
| Any hospitalization | 33.5 | 29.3 | 29.9 | 61.4 |
| Potentially avoidable hospitalization* | 11.3 | 9.6 | 10.0 | 21.7 |
| Long-term care spending* | 25,486 | 49,038 | 13,129 | 38,683 |
| Hospital spending* | 7,341 | 5,731 | 5,997 | 17,671 |
| N | 1,659,645 | 442,998 | 1,006,565 | 210,082 |
Source: 2012 MAX linked with MBSF. Percentages reported for binary variables, means for continuous variables.
Hospitalization and spending limited to FFS Medicare, Alive full year sample.
Use
We present characteristics of users by long-term care setting in three groups: institutional settings only, HCBS only, and both institutional and HCBS during the year. 26.7% of long-term care users used institutional services only, with nearly all of those services being nursing facility services. 60.6% used HCBS only, and 12.7% received services in both settings during the year. Users of institutional services were older, more likely to be white, less likely to be enrolled in managed care, and had higher mortality, higher rates of dementia and more chronic conditions than HCBS-only users. The group that received long-term care in both settings appears in even poorer health than institutional-only users; they had the highest mortality rates. While they had the highest rates of four or more chronic conditions, the group using both long-term care settings had lower rates of dementia than users of institutional services only.
Exhibit 2 further explores differences in long-term care setting by race and dementia, adjusting for age and sex. Whites had the highest rate of institutional services use, with the highest shares of institutional only and both institutional and HCBS use. In contrast, the non-white groups had higher shares using HCBS only. Within each race group, dementia was associated with higher reliance on institutions, but stratifying by dementia did not change the overall pattern that whites relied more on institutions and non-whites relied more on HCBS. Even among care recipients with dementia, almost 44% of blacks, two-thirds of Hispanics, and three-quarters of Asians use HCBS only, whereas only one-third of whites do. Thus, examining outcomes of care and the associated potential disparities among HCBS users is critical.
EXHIBIT 2.
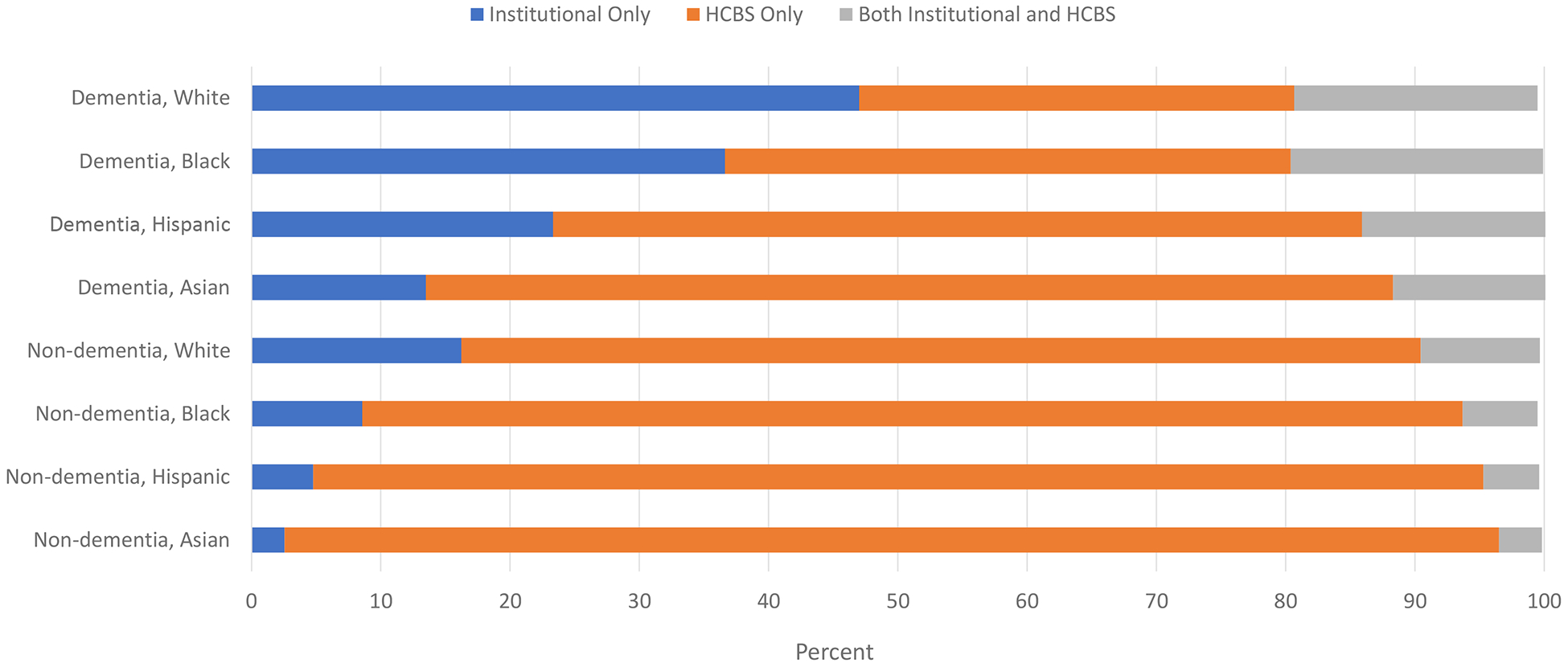
Long-term care setting by race and dementia
SOURCE 2012 MAX linked with MBSF.
NOTES Adjusted for age and sex.
Hospital admissions
Restricting the sample to those long-term care users enrolled in fee-for-service Medicare and who are alive for the full year, we explore differences in hospital admissions by race and dementia. Because our focus is on the comparison between HCBS and institutional care, we limit the main analysis of hospitalizations to the institutional-only and HCBS-only groups, setting aside the unique issues of individuals that use both care settings. Table 1 shows that beneficiaries who use either institutional services or HCBS have similar rates of overall hospitalization and potentially avoidable hospitalization, even though institutional service users tend to be older, have more chronic conditions, and higher mortality.
Exhibit 3 repeats this comparison, separately by race and dementia groups. Among those without dementia, HCBS users have lower hospitalization rates than institutional users (27.4% vs 32.5%, not shown), consistent with our sample characteristics showing that institutional-only users were in poorer health than HCBS-only users. However, among those with dementia, the pattern is reversed: Hospitalization rates were higher among HCBS users than institutional users (34.3% vs 28.7%, not shown) and this finding is consistent for the white and black race groups. For the Hispanic and Asian groups, while hospitalization rates are higher for institutional users regardless of dementia status, the difference in hospitalization rates between the two settings is smaller for the dementia group. Thus, among sicker individuals – those with dementia – HCBS is associated with worse outcomes than nursing facility care.
EXHIBIT 3.
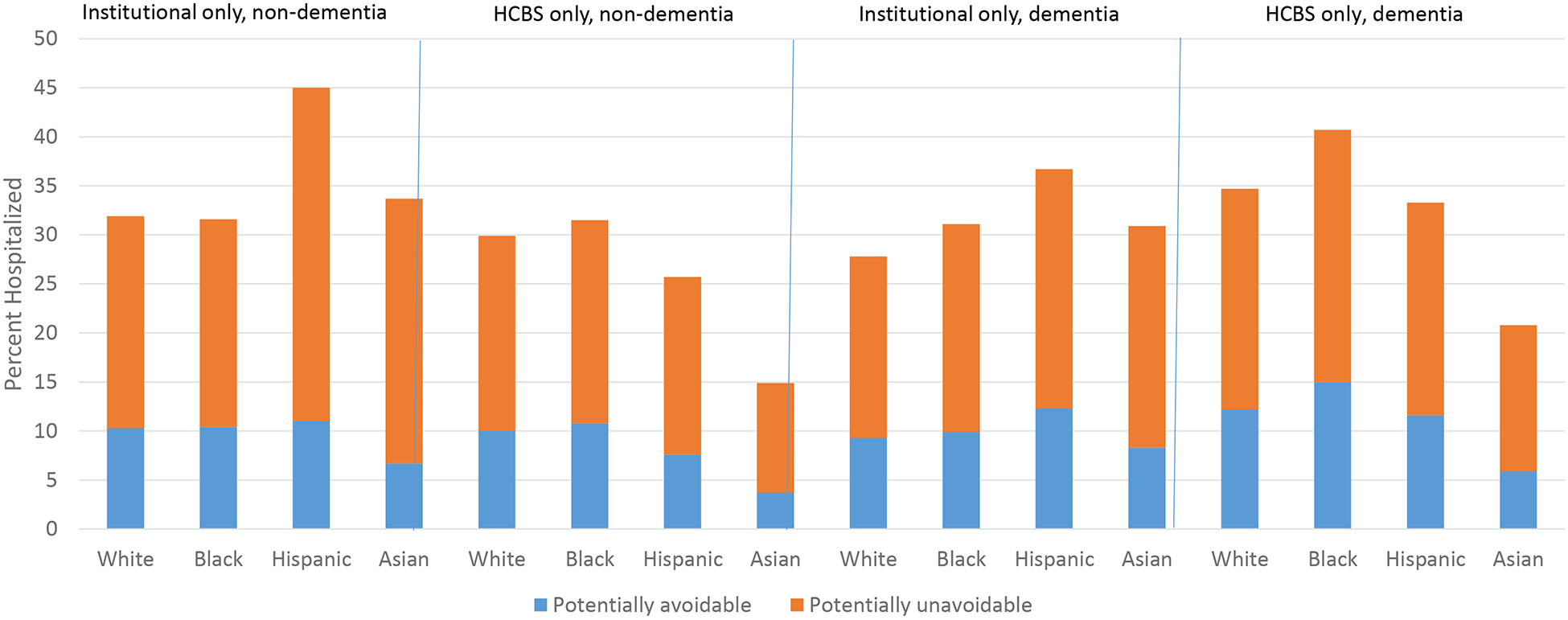
Hospitalization among long-term care users
SOURCE 2012 MAX linked with MEDPAR. Limited to FFS Medicare, alive full year sub-sample.
NOTES Adjusted for age and sex. Differences by race statistically significant, p<0.001.
Examining HCBS users more closely, we find that blacks had the highest rates of hospitalization, including potentially avoidable hospitalization, followed by whites and Hispanics, and finally Asians with the lowest rates. These patterns hold across both beneficiaries with dementia and beneficiaries without dementia. For each race group, not surprisingly, there is a higher rate of any hospitalization and potentially avoidable hospitalization among care recipients with dementia, but the presence of dementia exacerbates the differences in hospitalization rates by race. In other words, blacks have higher rates of hospitalization than other races in the population without dementia, but among HCBS recipients with dementia, the difference between blacks and other races becomes more pronounced.
Spending
Finally, we examine Medicaid long-term care and hospital (Medicare and Medicaid) spending, by race and dementia status, focusing on HCBS users. Exhibit 4 shows that, not surprisingly, total HCBS plus hospital spending is higher for care recipients with dementia than for those without. Within the groupings by dementia status, total HCBS plus hospital spending is highest for whites, followed by blacks, Hispanics, and then Asians, and HCBS spending alone is higher for whites than for other races. However, consistent with the hospitalization rates shown in Exhibit 3, hospital spending is higher for blacks than for other races. Thus, overall, HCBS expenditures are highest for whites and hospital expenditures are highest for blacks and Hispanics, but total expenditures are still higher for whites. The higher HCBS expenditures for whites more than outweighs the difference in hospitalization expenditures.
EXHIBIT 4.
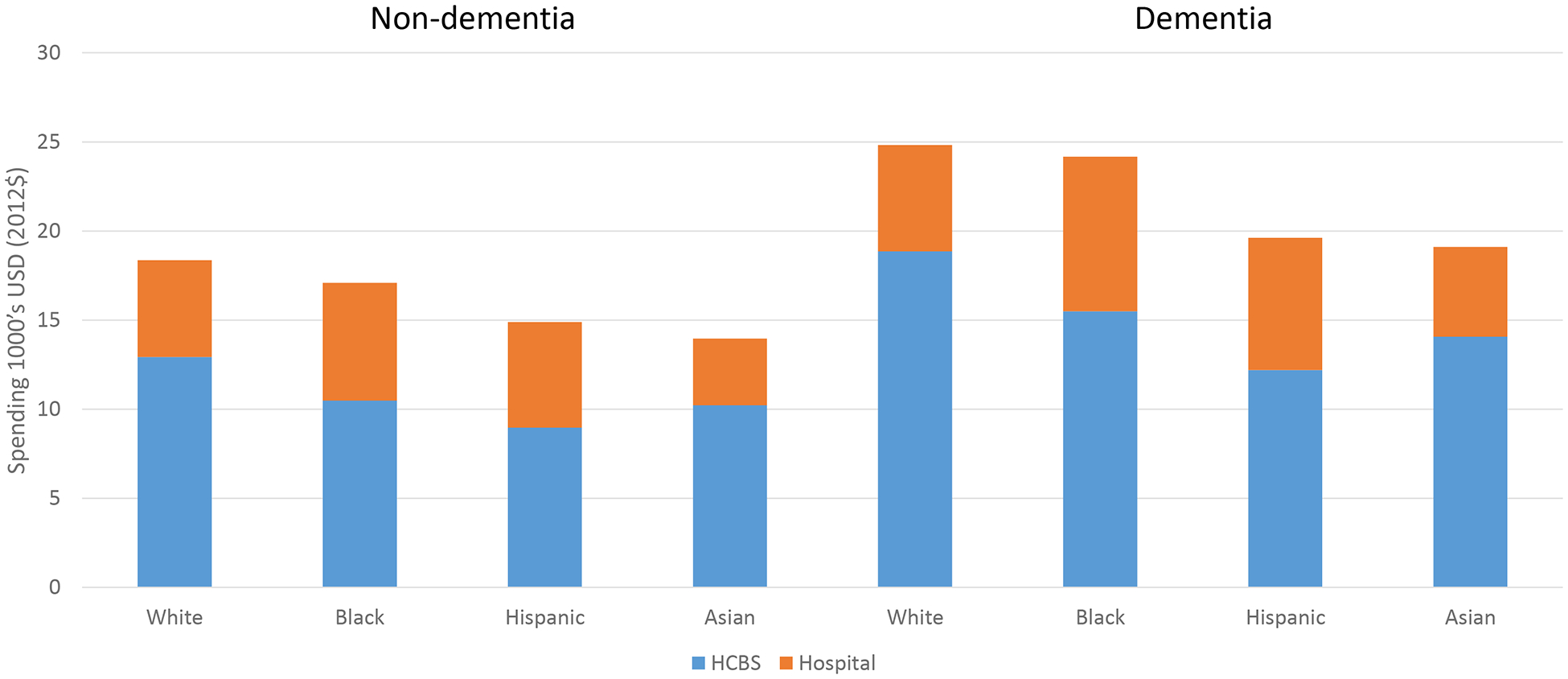
Spending among HCBS Users
SOURCE 2012 MAX linked with MEDPAR. Limited to FFS Medicare, alive full year sub-sample.
NOTES Adjusted for age and sex. Differences by race statistically significant, p<0.001.
In addition to differences between whites and non-whites, interesting differences emerge among the non-white groups. While each non-white group relies more on HCBS than their white counterparts, Asians are most likely to rely only on HCBS followed by Hispanics and then blacks. Among HCBS only users, Asians and Hispanics had rates of hospitalization that were lower than that of whites, while blacks had higher hospitalization rates than whites. On average, the three non-white subgroups had lower spending on HCBS than their white counterparts. While Hispanics had lower hospitalization rates than whites, they had higher average spending due to hospitalization. These differences among the non-white groups illustrate the importance of examining patterns of long-term care separately, as each race group may experience effects of HCBS expansions differently.
We conducted several sensitivity analyses to explore the consequences of health-related controls, the age of our data, and our exclusion of beneficiaries who died, the results of which were generally reassuring. Details of these tests and their results are in the appendix(24).
Discussion
We show that among elderly, dual-eligible long-term care users, beneficiaries who use either institutional services or HCBS have similar rates of hospitalization and potentially avoidable hospitalization overall, even though institutional service users tend to be older, have more chronic conditions, and higher mortality rates. Among those with dementia, HCBS users actually have higher rates of hospitalization than nursing facility users.
We also see distinct patterns of use and outcomes by race. Whites rely more on nursing facilities while non-whites rely on HCBS, and this pattern persists among care recipients with dementia. Importantly, we find that among HCBS users, whites spend more on HCBS, but they have lower hospitalization rates and hospital spending than blacks and Hispanics. Thus, disparities by race and ethnicity that have been well-documented in nursing facilities also appear to extend to the HCBS setting.
There are several possible explanations for the patterns we find. First, differences in health status may explain some of the patterns we see but cannot consistently explain our key findings. For example, if we posit that lower HCBS spending on blacks is due to better health, then hospitalization rates should not be higher among blacks. Our sensitivity analysis adding health-related controls reinforces the inadequacy of this explanation to the extent that we can control for health using claims data. Second, cultural preferences have sometimes been used to explain racial and ethnic differences in use of home-based versus institutional care and may play a role in patterns of use, but people do not generally prefer to have high hospitalization rates. Third, differences by race in the availability of informal care could lead to differential use of HCBS and hospitalization, but if greater availability of informal care leads to HCBS use, it does not necessarily follow that greater availability of informal care is associated with higher hospitalization rates.
Although combinations of the above explanations might play a role in our results, several other explanations seem more plausible. First, social determinants of health and the availability of medical services, such as physician home visits(31,32), may vary by geography in a way that is correlated with race. If black HCBS users have less access to medical services than whites, higher hospitalization rates could result even if there were equal spending on HCBS. Second, high hospitalization rates may mean that HCBS itself is inadequate in quality or quantity, especially for beneficiaries with dementia and for non-whites. The inadequacy may be due to too few or not the right services, insufficient frequency of care, low-quality providers, or inadequate attention to coordinating services, which may be harder with HCBS than in a nursing facility setting where staff are available to help.
The inadequacy of HCBS could also be related to geography, since HCBS services are heterogeneous across and within states, and whites may live in areas with more HCBS funding or looser eligibility standards. To explore whether geography plays a role, we tested our findings including county-level fixed effects, effectively looking at whether our results hold within counties. (See Appendix page 16 for predicted rates of hospitalization and spending adjusted for county fixed effects(24).) This controls for differences across counties in supply and quality of HCBS and other medical services. Our key findings remain, suggesting that local (county) supply and quality of medical services and HCBS may not explain our results. A caveat is that counties may be too large to represent markets, and differences in access by race within counties may still exist.
Although our main focus is on national results, as an exploration of potential heterogeneity we examine a subset of high and low HCBS spending states (see Appendix pages 12–15 for details(24)). While there is more HCBS use among high HCBS spending states, the patterns we observe by care setting, race, and dementia status are generally consistent in both high and low HCBS spending states.
These results have several policy implications. First, the high rates of hospitalization among HCBS-only users suggest that outcomes of HCBS need additional scrutiny, especially for racial and ethnic minorities and people with serious health issues such as dementia. If hospitalization rates are high due to limited access to medical services, policymakers may wish to focus HCBS provision on areas where medical services and HCBS can work in tandem or to encourage supply of medical services in underserved areas. If hospitalization rates are high due to inadequacy of HCBS, it may be necessary to enhance HCBS service packages such that they become a true alternative to nursing facility care without resulting in adverse outcomes. This may include spending more on caregiver support, which is a neglected area of importance to HCBS. Development of validated measures of HCBS quality would help states determine how to improve their HCBS offerings.
Second, because hospitalization costs among HCBS users are not insignificant, calculations of the cost-effectiveness of HCBS programs should consider Medicare hospital spending, rather than just Medicaid spending. Furthermore, accounting of full social costs of these programs must also include costs to caregivers and to care recipients for adverse outcomes. Almost by definition, HCBS places a greater responsibility on families to support the formal care being received, and this mostly unpaid support is likely to be one reason that Medicaid finds it cheaper to fund HCBS than institutional care. Yet it is well-established that informal care is not “free” in that caregivers incur substantial costs in the form of reduced labor market participation and poorer health; these costs have been estimated to be substantial in long-term care(33,34). At the same time, calculations of the cost-effectiveness of HCBS need to include the full benefits of HCBS, including quality of life outcomes, an area in which measurement is still in need of substantial development.
Finally, the high rates of institutional service use among elderly, dual Medicare-Medicaid beneficiaries with dementia suggests that, among some individuals, institutional care may be required or even preferred by beneficiaries and their families due to high needs for intensive long-term care that may not be met in the home setting. Even as HCBS options are expanded, the need for access to high-quality nursing facilities should remain on the agenda as policymakers consider ways to improve the long-term care options available to Medicaid beneficiaries.
Our study provides compelling evidence that Medicaid’s push to shift long-term care from institutions to the community, although intuitively appealing, is in need of a closer look and more careful targeting. If HCBS is promoted as a preferred setting of care to Medicaid beneficiaries who need a higher intensity of care, or who lack appropriate support at home, access to high-quality HCBS, or access to essential medical services, unintended consequences can result unless these gaps are addressed. Our findings also show that racial and ethnic disparities exist in HCBS just as in nursing facilities. It will be important for further research to examine the causes and mechanisms for our findings, especially differences by race, to develop more specific policy strategies.
Supplementary Material
References
- 1.Eiken S, Sredl K, Burwell B, Amos A. Medicaid Expenditures for Long-Term Services and Supports in FY 2016. 2018. May. [Google Scholar]
- 2.Gonçalves J, Weaver F, Konetzka RT. Measuring State Medicaid Home Care Participation and Intensity Using Latent Variables. J Appl Gerontol. 2018. July 6. [DOI] [PubMed] [Google Scholar]
- 3.MedPAC, MACPAC. Data book: Beneficiaries dually eligible for Medicare and Medicaid. 2018. January Available from: http://medpac.gov/docs/default-source/data-book/jan18_medpac_macpac_dualsdatabook_sec.pdf?sfvrsn=0
- 4.Thach NT, Wiener JM. An Overview of Long-Term Services and Supports and Medicaid: Final Report. Washington DC: U.S. Department of Health and Human Services Assistant Secretary for Planning and Evaluation Office of Disability, Aging and Long-Term Care Policy; 2018. May p. 34. [Google Scholar]
- 5.Miller EA, Weissert WG. Predicting Elderly People’s Risk for Nursing Home Placement, Hospitalization, Functional Impairment, and Mortality: A Synthesis. Med Care Res Rev. 2000. September 1;57(3):259–97. [DOI] [PubMed] [Google Scholar]
- 6.Wallace SP, Levy-Storms L, Kington RS, Andersen RM. The Persistence of Race and Ethnicity in the use of Long-Term Care. J Gerontol Ser B. 1998. March 1;53B(2):S104–12. [DOI] [PubMed] [Google Scholar]
- 7.Konetzka RT, Werner RM. Review: Disparities in Long-Term Care: Building Equity Into Market-Based Reforms. Med Care Res Rev. 2009. October 1;66(5):491–521. [DOI] [PubMed] [Google Scholar]
- 8.Kaye HS, Harrington C, LaPlante MP. Long-Term Care: Who Gets It, Who Provides It, Who Pays, And How Much? Health Aff (Millwood). 2010. January 1;29(1):11–21. [DOI] [PubMed] [Google Scholar]
- 9.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to Tiers: Socioeconomic and Racial Disparities in the Quality of Nursing Home Care. Milbank Q. 2004. June 1;82(2):227–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brega AG, Goodrich GK, Powell MC, Grigsby J. Racial and Ethnic Disparities in the Outcomes of Elderly Home Care Recipients. Home Health Care Serv Q. 2005. September 26;24(3):1–21. [DOI] [PubMed] [Google Scholar]
- 11.Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate And Unequal: Racial Segregation And Disparities In Quality Across U.S. Nursing Homes. Health Aff (Millwood). 2007. September 1;26(5):1448–58. [DOI] [PubMed] [Google Scholar]
- 12.Sansoni J, Anderson K, Varona L, Varela G. Caregivers of Alzheimer’s patients and factors influencing institutionalization of loved ones: some considerations on existing literature. Ann Ig Med Prev E Comunita. 2013. June;25(3):235–46. [DOI] [PubMed] [Google Scholar]
- 13.Schulz R, Martire LM. Family Caregiving of Persons With Dementia: Prevalence, Health Effects, and Support Strategies. Am J Geriatr Psychiatry. 2004. May 1;12(3):240–9. [PubMed] [Google Scholar]
- 14.Carlson BL, Foster L, Dale SB, Brown R. Effects of Cash and Counseling on Personal Care and Well-Being. Health Serv Res. 2007. February 1;42(1p2):467–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Darryl Wieland, Lamb Vicki L., Sutton Shae R., Boland Rebecca, Clark Marleen, Friedman Susan, et al. Hospitalization in the Program of All‐inclusive Care for the Elderly (PACE): Rates, Concomitants, and Predictors. J Am Geriatr Soc. 2015. April 27;48(11):1373–80. [DOI] [PubMed] [Google Scholar]
- 16.Coughlin R, Ward J, Denny-Brown N, Hagen B, Maurer K, Morris E, et al. Money Follows the Person Demonstration: Overview of State Grantee Progress, January to December 2016. Cambridge, MA: Mathematica Policy Research; 2017. September. [Google Scholar]
- 17.Peebles V, Kim M-Y, Bohl A, Morales N, Lipson D. HCBS Claims Analysis Chartbook: Final Report. Mathematica Policy Research; 2017. December Available from: https://www.mathematica-mpr.com/our-publications-and-findings/publications/hcbs-claims-analysis-chartbook-final-report [Google Scholar]
- 18.Konetzka RT, Karon SL, Potter DEB. Users Of Medicaid Home And Community-Based Services Are Especially Vulnerable To Costly Avoidable Hospital Admissions. Health Aff (Millwood). 2012. June 1;31(6):1167–75. [DOI] [PubMed] [Google Scholar]
- 19.Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, Ouslander JG. Potentially Avoidable Hospitalizations of Dually Eligible Medicare and Medicaid Beneficiaries from Nursing Facility and Home- and Community-Based Services Waiver Programs. J Am Geriatr Soc. 2012. May 1;60(5):821–9. [DOI] [PubMed] [Google Scholar]
- 20.Andrea Wysocki, Kane Robert L., Dowd Bryan, Golberstein Ezra, Lum Terry, Shippee Tetyana. Hospitalization of Elderly Medicaid Long‐Term Care Users Who Transition from Nursing Homes. J Am Geriatr Soc. 2014. January 2;62(1):71–8. [DOI] [PubMed] [Google Scholar]
- 21.Wysocki A, Kane RL, Golberstein E, Dowd B, Lum T, Shippee T. The Association between Long-Term Care Setting and Potentially Preventable Hospitalizations among Older Dual Eligibles. Health Serv Res. 2014. June;49(3):778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Medicare C for, Baltimore MS 7500 SB, Usa M. MAXGeneralInformation. 2017. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidDataSourcesGenInfo/MAXGeneralInformation.html
- 23.Eiken S Medicaid Long-Term Services and Supports Beneficiaries in 2012. Truven Health Analytics; 2016. September Available from: https://www.medicaid.gov/medicaid/ltss/downloads/ltss-beneficiaries-2012.pdf [Google Scholar]
- 24. To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 25.Eicheldinger C, Bonito A. More Accurate Racial and Ethnic Codes for Medicare Administrative Data. Health Care Financ Rev. 2008;29(3):27–42. [PMC free article] [PubMed] [Google Scholar]
- 26.Condition Categories - Chronic Conditions Data Warehouse. Available from: https://www.ccwdata.org/web/guest/condition-categories
- 27.AHRQ - Quality Indicators. Prevention Quality Indicators Technical Specifications Updates - Version 6.0 (ICD-9), October 2016. Available from: http://www.qualityindicators.ahrq.gov/Modules/PQI_TechSpec_ICD09_v60.aspx
- 28.Libersky J, Liu S, Ruttner L, Collins A, Geller J, Irvin C. Managed Long-Term Services and Supports Design Supplement: Interim Outcomes Evaluation. Mathematica Policy Research; 2017. June Available from: https://www.medicaid.gov/medicaid/section-1115-demo/downloads/evaluation-reports/eval-dsgn-mltss.pdf [Google Scholar]
- 29.Byrd VLH, Dodd AH. Assessing the Usability of Encounter Data for Enrollees in Comprehensive Managed Care 2010–2011. Mathematica Policy Research; 2015. August (Medicaid Policy Brief). Report No.: 22. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidDataSourcesGenInfo/Downloads/MAX_Encounter_Brief_2010_2011.pdf [Google Scholar]
- 30.Saucier P, Kasten J, Burwell B, Gold L. The Growth of Managed Long-Term Services and Supports (MLTSS) Programs: A 2012 Update. Centers for Medicare &Medicaid Services; 2012. July Available from: https://www.medicaid.gov/medicaid-chip-program-information/by-topics/delivery-systems/downloads/mltssp_white_paper_combined.pdf [Google Scholar]
- 31.Yao N (Aaron), Ritchie C, Cornwell T, Leff B. Use of Home-Based Medical Care and Disparities. J Am Geriatr Soc. 2018;66(9):1716–20. [DOI] [PubMed] [Google Scholar]
- 32.Yao N, Ritchie C, Camacho F, Leff B. Geographic Concentration Of Home-Based Medical Care Providers. Health Aff (Millwood). 2016. August 1;35(8):1404–9. [DOI] [PubMed] [Google Scholar]
- 33.Coe NB, Van Houtven CH. Caring for Mom and Neglecting Yourself? The Health Effects of Caring for an Elderly Parent. Health Econ. 2009. September;18(9):991–1010. [DOI] [PubMed] [Google Scholar]
- 34.Skira MM. Dynamic Wage and Employment Effects of Elder Parent Care. Int Econ Rev. 2015. February;56(1):63–93. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


