Introduction
A novel coronavirus named 2019-nCoV was discovered in December 2019, and its resultant disease termed coronavirus disease 2019 (COVID-19) subsequently broke out in Wuhan, China. The COVID-19 epidemic then spread rapidly throughout China and the world. The front-line healthcare workers needed to use personal protective equipment (PPE) such as masks, goggles, and protective clothing for long periods of time. However, PPE may cause a series of skin problems due to long-term sealing, friction, and pressure. The present review details the characteristics of skin damage caused by several main pieces of PPE, and the corresponding prevention and care measures required based on the experience of the first-line clinicians working to treat 2019-nCoV infection.
PPE
Concept
PPE refers to the wearable personal items that are used to avoid or reduce accidental injuries and minimize occupational hazards at work. When harmful factors and the possibility of accidents cannot be eliminated or effectively reduced in the working environment, PPE becomes the main protective measure for primary prevention.1,2 The objectives of PPE are to protect against physical, chemical, and biological factors. PPE is important for ensuring safe production in a factory environment, responding to public health emergencies, and maintaining the safety and health of workers. The status and role of PPE has received increasing attention with the recent economic development, improvement in workers’ awareness of safety protection, and continuous expansion of the market demand for PPE.
Classification
PPE comprises equipment that protects the mouth, nose, eyes, ears, bare skin, and vulnerable parts (such as the head) of staff in accordance with their specific working environment.
When classified by the use objectives, PPE includes: individual protective equipment for military personnel, such as bullet-proof helmets, bullet-proof clothing, gas masks, and combat boots; protective equipment for police, such as explosion-proof clothing, anti-stab clothing, and anti-glare glasses; protective equipment for diverse types of workers, mainly industrial and agricultural production staff, medical staff, and scientific and technological workers. When classified by the protection objectives, PPE includes: physical protective equipment such as insulating gloves, hardhats, and earmuffs; chemical protective equipment such as gas masks, acid-proof clothing, and alkali-proof clothing; biological protective equipment such as medical masks, goggles, and medical protective clothing; public safety protective equipment for public places, such as escape masks and life jackets in civil aviation passenger planes; protective equipment used in personal life, such as anti-haze and anti-UV goggles.3 When classified by the protected body parts, PPE includes respiratory protectors, eye shields, face shields, ear protectors, helmets, protective clothing, gloves, and shoe covers.
Characteristics of skin damage caused by PPE
Although the PPE used in different industries is made from various materials, the skin problems caused by PPE used for the same part of the body are basically similar, as these problems are mainly caused by poor air permeability, friction, and pressure on the skin. This section describes the characteristics of skin damage caused by PPE in different parts of the body.
Facial skin damage
PPE for the face mainly includes respiratory protective equipment, such as various types of masks and goggles. Such equipment needs to be tightly attached to the skin surface, which compresses the skin at the fixed site for many hours and may result in device-related pressure injuries.4,5 The factors contributing to device-related pressure injuries include poor local blood circulation, tissue ischemia and hypoxia, skin evaporation, and the accumulation on the inside of the mask of a large amount of water vapor exhaled from the mouth and nose, keeping the facial skin in a moist environment for a long period; this softens and impregnates the skin, and reduces the ability of the stratum corneum to resist external pressure and shear forces. Thus, the skin is prone to indentations.6,7 In addition, the friction between the PPE and the skin enhances the development of erythema, blisters, or ulcers, along with pain and even secondary infection (Fig. 1).
Figure 1.
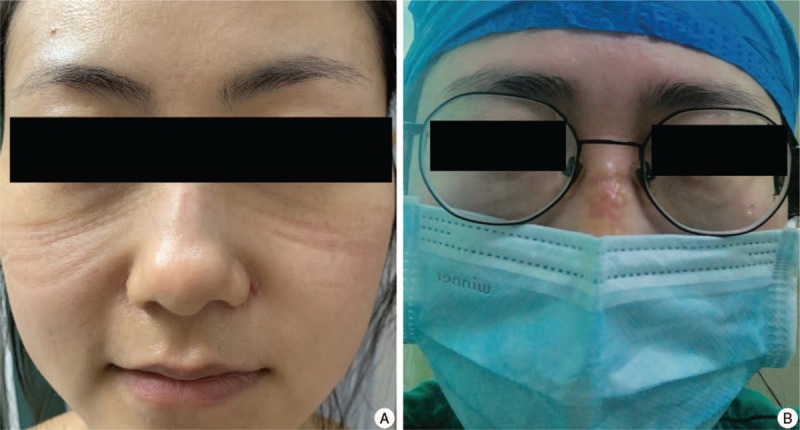
Facial pressure injuries induced by personal protective equipment. (A) Mask indentations on the nose and cheek. (B) Blisters on the nose.
Ear skin damage
Long-term wearing of earmuffs can cause poor local circulation because of the pressure on the auricular skin, contributing to skin pain and excessive congestion after earmuff removal. However, long-term wearing of earmuffs is generally unlikely to cause epidermal rupture, as most earmuffs are soft, and the skin is evenly compressed. Anti-noise and dustproof earplugs rarely cause pressure damage, but contain materials such as rubber that may cause contact allergies.8 The skin behind the ear is susceptible to device-related pressure injuries due to repeated friction caused by the ear ropes of facemasks.9
Head skin damage
Aside from pressure injuries, wearing a helmet may also lead to other skin disorders. The scalp is rich in hair follicles, sebaceous glands, and sweat glands, and therefore secretes large amounts of oil and sweat. Due to the poor permeability of hair, hats, and helmets, the sweat and oil secreted by the scalp mix together and remain on the skin surface of the head, consequently blocking the pores and making it easier for folliculitis to develop when bacteria colonize. Aggravation of this inflammation may lead to skin lesions such as pustules, boils, seborrheic dermatitis, and secondary fungal infection.
Hand and foot skin damage
To completely isolate the wearer from harmful substances in the environment, gloves and protective boots are mostly made of waterproof materials with poor air permeability, such as rubber and plastic. If the skin of the hands and feet is left in an air-impermeable environment for long periods, the sweat evaporation is decreased, and the skin is prone to impregnation, eczema, and sweat herpes. Furthermore, the hot and humid environment is conducive to fungal reproduction and tinea of the feet and hands. In addition to wearing gloves, hand hygiene is also essential for chemical and biological protection. Repeated washing damages the skin barrier and is partially accountable for dryness, itching, and eczema of the hands and feet. Furthermore, repeated contact with irritants such as disinfectants and gloves can cause contact dermatitis with erythema, pimples, pimples, exudation, or erosion. One study found that 52% of medical staff with hand eczema wash their hands more than 10 times per day.10 Long-term disinfectant use also influences the microbiota and changes the immune microenvironment on the skin surface, resulting in conditions such as eczema, fungal infection, bacterial infection, and allergic dermatitis.11
Skin damage in other areas
The materials used to make explosion-proof clothing, stab-resistant clothing, and other protective clothing are relatively hard, which may cause device-related pressure injuries due to friction between the clothing edge and the skin. Industrial and medical protective clothing have requirements for tightness, which keeps the skin over the whole body in a humid environment and makes it prone to impregnation. People with large amounts of sebaceous gland secretions are likely to develop acne in areas rich in sebaceous glands, such as the chest and back, due to the pores being blocked by sweat and sebum. Irritation from the sweat and contact with protective clothing might also cause an allergic skin reaction. In particular, the vulval, medial thigh, and perianal areas are predilection sites for skin inflammation and secondary bacterial and fungal infections due to excretion irritation and repeated friction during walking.
Prevention of skin damage caused by PPE
Device-related pressure injuries
The key to preventing device-related pressure injuries is to reduce local skin pressure and shorten the compression time.12 To ensure the protective effect, soft plastic PPE has strong compliance with the skin, relatively uniform pressure distribution, and relatively little local pressure. In areas where pressure is concentrated and there is repeated rubbing (such as the upper edge of goggles, the upper edge of the bridge of the nose, and the ear-closing parts of facemasks), the application of a dressing can help prevent pressure injuries by redistributing and reducing the pressure and avoiding the friction caused by relative displacement.
Many types of hydrogel dressings, hydrocolloid dressings, and foam dressings are used in clinical practice to prevent stress injuries. Hydrogel has a rich water content and three-dimensional network structure, and has many characteristics that are beneficial to wound healing. Hydrogel dressings have good biocompatibility and compliance, as the porous structure guarantees breathability and absorbs and releases moisture to ensure that the skin moisture content is appropriate. Hydrogel also has cooling and analgesic effects. The hydrocolloid dressing also has good compliance and can be fitted to the skin of irregularly shaped body parts with minimal effect on the tightness of PPE.13 The application of hydrogel or hydrocolloid dressings to the skin that is under pressure reduces the maximum pressure caused by the device, avoids friction between the device and the skin, and largely prevents pressure injuries14 (Fig. 2A–D). The position of the PPE must be adjusted to ensure the tightness (Fig. 2E). In addition, hydrogel and hydrocolloid dressings have self-adhesive properties, are easy to apply, and do not damage the skin during dressing removal15,16 (Fig. 2F). Foam dressing is a decompression dressing that is often used clinically to prevent pressure ulcers. Foam dressing is very protective against pressure and shear force, and has a good liquid absorption capacity.17 However, the thickness and material characteristics of foam dressing means that its compliance is not as good as that of hydrogel and hydrocolloid dressings, and care must be taken not to affect the tightness of the PPE during use. In addition, continuous compression and prolonged exposure to a humid environment increase the risk of pressure-related injuries. Workers should remove PPE as soon as possible after leaving the working environment, as this is conducive to skin self-repair.
Figure 2.

Hydrogel dressings used to prevent facial pressure injury induced by personal protective equipment. (A) A hydrogel eye patch on the left side of the face. (B) The patch is positioned under the edge of a N95 mask. (C) After wearing the N95 mask for 4 hours continuously, there is obvious indentation and erythema on the right side of the face, but no obvious indentation on the left side of the face. (D) “W” type adhesive hydrogel eye paste to prevent pressure damage on the nose and face induced by the mask. (E) Proper use of the hydrogel patch does not affect the tightness of the mask. (F) The hydrogel patch is easily removed.
Daily skincare routine
A healthy and complete skin barrier is important to resist skin damage caused by PPE. Adequate cleaning and moisturizing are the basis of skin barrier maintenance. An appropriate cleaning frequency removes dirt, bacteria, and some sweat and oil from the skin surface, which reduces the irritation caused by their long-term presence and reduces the risk of infection. Adequate moisturizing helps maintain the moisture content of the corneum, maintains the “brick-wall” structure of the epidermis, and facilitates cell self-repair.18 Basic moisturizing usually consists of two categories: the application of a water-soluble moisturizer (including glycerin and sodium hyaluronate) that supplements natural moisturizing factors to lock in moisture,19 and the application of squalane, mineral oils, and various natural oils to replenish sebum, which forms an oil film on the skin surface to prevent water loss. People with rich sebum in a closed equipment environment should use water-soluble moisturizers to prevent excessive oil from blocking the pores and causing acne.
Treatment of skin injury caused by PPE
Device-related pressure injuries
For simple indentation with a complete epidermis, no special treatment is required, as the skin will recover without intervention. For small sterile blisters, the epidermis is kept intact, and the blister fluid will be absorbed without intervention. For blisters with a large area or high tension, a sterile syringe is used to suction out the fluid from the bottom of the blister, topical antibiotic ointment is applied, and epidermal loss should be avoided. If there is erosion and exudation, the wound is washed with physiological saline after disinfection. Antibiotic ointment is required for infection prevention. Moreover, a suitable dressing is selected in accordance with the exudate. If there is a lot of exudate, an alginate dressing or foam dressing with good absorptivity is used. The hydrocolloid dressing is suitable for a medium amount of exudate, while a hydrogel dressing or a film dressing is suitable for wounds with less exudate or dry wounds. If ulcers appear on the skin, a wet dressing is also required to promote wound convergence. Silver ion dressings that resist bacteria and reduce the secondary damage caused by frequent dressing replacements are appropriate for infected ulcers. In addition, epidermal growth factor and fibroblast growth factor can be used to promote cell proliferation and accelerate wound healing. Debridement may be needed for deep and chronic ulcers.20
Allergic skin conditions
The appearance of eczema is often related to the impaired permeability of PPE or skin barrier damage caused by excessive washing. Moisturizing is important to restore the skin barrier. Eczema lesions are topically treated with a glucocorticoid ointment or calcineurin inhibitor such as tacrolimus ointment or pimecrolimus cream. If the eczema area is large or there is marked pruritus, a second-generation antihistamine can be taken orally.
Contact dermatitis is an allergic reaction to the components of PPE. Care should be taken to avoid re-exposure to the allergen. Treatment comprises oral antihistamines and topical glucocorticoids. Wet compresses are often required for exudation, and topical antibiotic ointments are required for ulceration.
Infectious skin conditions
Intact skin is most likely to develop fungal infections in hot and humid environments. The most common of these fungal infections is tinea of the feet and hands, which causes macerative erosion. Topical treatments include antifungal cream and a 3% boric acid solution. For onychomycosis or a large area of fungal infection, the systemic application of antifungal drugs, such as oral itraconazole, should be considered. The most commonly seen bacterial skin conditions caused by PPE are folliculitis and furuncles, mainly due to Staphylococcus aureus infection. Folliculitis is treated topically with an antibacterial agent, such as 2.5% iodine tincture or mupirocin ointment. In the early stage of furuncles, 2.5% iodine tincture and 10% fishstone fat ointment can be used externally, combined with topical antibiotic ointments such as mupirocin, fusidic acid cream, erythromycin ointment, and recurring polymyxin B ointment. Mature lesions should be excised and drained, and systemic antibiotics may be needed.
Acne
The pathogenesis of acne involves four factors: increased secretion of sebaceous glands, abnormal keratinization of the sebaceous ducts of the hair follicles, Propionibacterium acnes infection, and secondary inflammation. Apart from wearing appropriate PPE and avoiding prolonged use, general treatments include: proper skin cleansing, a reasonable selection of skincare products (mainly water-soluble moisturizers and no hormones), a low-sugar diet, and avoidance of squeezing pimples with the hands. Topical choices include retinoids (to regulate keratinization of the epithelium), benzoyl peroxide (to kill P. acnes), and salicylic acid (to dissolve acne and reduce inflammation), as well as erythromycin, clindamycin, chloramphenicol tincture, and other antibiotic preparations. When these topical treatments do not achieve a good effect, a combination of red and blue light treatment should be applied. Those with moderate and severe acne need oral medicine under specialist guidance, such as minocycline, isotretinoin capsules. Traditional Chinese medicine or photodynamic therapy can also be used.
Summary
This review summarizes the causes and characteristics of skin damage caused by the use of various types of PPE, and introduces the corresponding skin protection and treatment countermeasures. The aim of this review was to provide reference material for workers in harsh environments. Especially in the wake of the current outbreak of COVID-19, we hope that this review helps the frontline medical staff to better protect their skin health and their own safety in their work.
Acknowledgements
This work was supported by the Hubei Provincial Science and Technology Department Fund for New Pneumonia Emergency Science and the Technology and Huazhong University of Science and Technology Independent Innovation Research Fund: New Coronavirus Pneumonia Emergency Special Fund.
References
- [1].Honda H, Iwata K. Personal protective equipment and improving compliance among healthcare workers in high-risk settings. Curr Opin Infect Dis 2016;29 (4):400–406. doi:10.1097/QCO.0000000000000280. [DOI] [PubMed] [Google Scholar]
- [2].Holland MG, Cawthon D. Personal protective equipment and decontamination of adults and children. Emerg Med Clin North Am 2015;33 (1):51–68. doi:10.1016/j.emc.2014.09.006. [DOI] [PubMed] [Google Scholar]
- [3].Villano JS, Follo JM, Chappell MG, et al. Personal protective equipment in animal research. Comp Med 2017;67 (3):203–214. [PMC free article] [PubMed] [Google Scholar]
- [4].Black JM, Cuddigan JE, Walko MA, et al. Medical device related pressure ulcers in hospitalized patients. Int Wound J 2010;7 (5):358–365. doi:10.1111/j.1742-481X.2010.00699.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Arnold-Long M, Ayer M, Borchert K. Medical device-related pressure injuries in long-term acute care hospital setting. J Wound Ostomy Continence Nurs 2017;44 (4):325–330. doi:10.1097/WON.0000000000000347. [DOI] [PubMed] [Google Scholar]
- [6].Pailler-Mattei C, Pavan S, Vargiolu R, et al. Contribution of stratum corneum in determining bio-tribological properties of the human skin. Wear 2007;263 (7):1038–1043. [Google Scholar]
- [7].Ham WH, Schoonhoven L, Schuurmans MJ, et al. Pressure ulcers, indentation marks and pain from cervical spine immobilization with extrication collars and headblocks: an observational study. Injury 2016;47 (9):1924–1931. doi:10.1016/j.injury.2016.03.032. [DOI] [PubMed] [Google Scholar]
- [8].Lazzarini R, Duarte IA, Sumita JM, et al. Allergic contact dermatitis among construction workers detected in a clinic that did not specialize in occupational dermatitis. An Bras Dermatol 2012;87 (4):567–571. doi:10.1590/s0365-05962012000400008. [DOI] [PubMed] [Google Scholar]
- [9].Qin Z, Jiao X, Lina W, et al. Nursing strategies for skin injuries caused by facial medical grade protective gear. Chin J Burns 2020;36. doi:10.3760/cma.j.issn.1009-2587.2020.0001. [DOI] [PubMed] [Google Scholar]
- [10].Ibler KS, Jemec GB, Agner T. Exposures related to hand eczema: a study of healthcare workers. Contact Dermatitis 2012;66 (5):247–253. doi:10.1111/j.1600-0536.2011.02027.x. [DOI] [PubMed] [Google Scholar]
- [11].Rosenthal M, Goldberg D, Aiello A, et al. Skin microbiota: microbial community structure and its potential association with health and disease. Infect Genet Evol 2011;11 (5):839–848. doi:10.1016/j.meegid.2011.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Apold J, Rydrych D. Preventing device-related pressure ulcers: using data to guide statewide change. J Nurs Care Qual 2012;27 (1):28–34. doi:10.1097/NCQ.0b013e31822b1fd9. [DOI] [PubMed] [Google Scholar]
- [13].Wyatt D, McGowan DN, Najarian MP. Comparison of a hydrocolloid dressing and silver sulfadiazine cream in the outpatient management of second-degree burns. J Trauma 1990;30 (7):857–865. doi:10.1097/00005373-199007000-00016. [DOI] [PubMed] [Google Scholar]
- [14].Dumville, Jo C. Cochrane Database of Systematic Reviews (Reviews) || Hydrogel dressings for treating pressure ulcers [J]. 1996 [DOI] [PMC free article] [PubMed]
- [15].Han L, Lu X, Liu K, et al. Mussel-Inspired adhesive and tough hydrogel based on nanoclay confined dopamine polymerization. ACS Nano 2017;11 (3):2561–2574. doi:10.1021/acsnano.6b05318. [DOI] [PubMed] [Google Scholar]
- [16].Lu H, Liwei Y, Menghao W, et al. Transparent, adhesive and conductive hydrogel for soft bioelectronics based on light transmitting polydopamine-doped polypyrrole nanofibrils. Chem Mater 2018;30 (16):5561–5572. doi:10.1021/acs.chemmater.8b01446. [Google Scholar]
- [17].Walker RM, Gillespie BM, Thalib L, et al. Foam dressings for treating pressure ulcers. Cochrane Database Syst Rev 2017;10 (10):CD011332. doi:10.1002/14651858.CD011332.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Treffel P, Gabard B. Stratum corneum dynamic function measurements after moisturizer or irritant application. Arch Dermatol Res 1995;287 (5):474–479. doi:10.1007/bf00373431. [DOI] [PubMed] [Google Scholar]
- [19].Rawlings AV, Harding CR. Moisturization and skin barrier function. Dermatol Ther 2004;17 (Suppl 1):43–48. doi:10.1111/j.1396-0296.2004.04s1005.x. [DOI] [PubMed] [Google Scholar]
- [20].Graninger M, Grassberger M, Galehr E, et al. Comments, opinions, and brief case reports: biosurgical debridement facilitates healing of chronic skin ulcers. Arch Intern Med 2002;162 (16):1906–1907. doi:10.1001/archinte.162.16.1906. [DOI] [PubMed] [Google Scholar]


