Abstract
Background:
We enrolled patients in a prospective study in which we obtained estimates of the direct and indirect burden for families of children with traumatic brain injury (TBI) relative to a control group of families of children with orthopedic injury (OI).
Methods:
Parents were surveyed at 3 time points following injury: 3, 6, and 12 months. At each follow-up contact, we asked parents to list the number of workdays missed, number of miles traveled, amount of travel-related costs, and whether their child had an emergency department (ED) visit, hospital admission, any over-the-counter (OTC) medications, and any prescription medications during that time period. We assessed the difference in these outcomes between the TBI and OI groups using multivariable logistic and 2-part regression models to account for high concentrations of zero values.
Results:
Children with TBI had significantly greater odds of having an ED visit (3.04; 95% CI, 1.12-8.24), OTC medications (1.98; 95% CI, 1.34-2.94), and prescription medications (2.34; 95% CI, 1.19-4.59) than those with OI. In addition, parents of children with TBI missed significantly more days of work (19.91 days; 95% CI, 11.64-28.17) overall during the 12 months following injury than their OI counterparts.
Conclusion:
Extrapolating our results to the entire country, we estimate that pediatric TBI is associated with more than 670 000 lost workdays annually over the 12 months following injury, which translates into more than $150 million in lost productivity. These missed workdays and lost productivity may be prevented through safety efforts to reduce pediatric TBI.
Keywords: healthcare utilization, missed work, pediatric TBI
TRAUMATIC BRAIN INJURY (TBI) is one of the most common forms of preventable injury among children. According to recent estimates from the Centers for Disease Control and Prevention (CDC), 3082.5 emergency department (ED) visits for TBI per 100 000 occurred in the United States during 2009-2010 among children 14 years and younger.1 Other recent data suggest a substantial increase in TBI-related ED visits between 2006 and 2010.2
Several recent studies have reported estimates of the costs associated with pediatric TBI. However, most of these studies have focused on direct medical costs such as those associated with the initial ED visit or subsequent hospitalizations, medications, or outpatient encounters.3,4 For TBI in children, the parents of the injured child may face additional burdens such as the need to miss work and travel costs associated with follow-up care. These indirect and nonmedical costs are rarely captured in electronic data but are an important component of the economic burden of pediatric TBI.5
The goal of this research was to generate more complete estimates of the economic burden of pediatric TBI. To do this, we enrolled a group of pediatric TBI patients as well as a control group of children with orthopedic injuries (OIs) in a prospective study to examine outcomes at 3, 6, and 12 months following injury. We surveyed families to determine their injured child’s healthcare utilization, travel costs, days of work missed, and time spent seeking healthcare for their child associated with the injury.
METHODS
Study design and population
We recruited patients between 0 months and 15 years of age at the time of injury from 2 level 1 pediatric trauma centers, which we refer to as site 1 and site 2. Children were recruited from both the ED and the inpatient units of these hospitals if they sustained either a TBI or an OI with no evidence of a TBI. Using a definition established by the CDC, TBI was defined as a head injury accompanied with any of the following: decreased consciousness, amnesia, neuropsychological abnormality, or diagnosed intracranial lesion.6 Children with abusive head trauma (AHT) or OIs were included. Children were recruited approximately evenly by site from January 20, 2013, through September 30, 2015. Families were approached in person while in the ED or hospital at both facilities. This method of recruitment was successful at site 1 because research coordinators are often present at that facility. Because this is not common practice at site 2, families from this facility were contacted by telephone after review of ED logs. Children were recruited sequentially according to child age (0-30 months, 31 months-5 years, 6-11 years, and 12-15 years), injury type, and TBI severity to ensure adequate representation in all strata of age and injury groups. Child age groups were chosen to reflect infants/toddlers, preschoolers, school-aged children, and adolescents as sites and types of postinjury care differ by age group. Follow-up interviews were collected at 3, 6 and 12 months. English-speaking families completed interviews online through a link to the survey sent by e-mail or by telephone. Spanish-speaking families completed interviews by telephone with bilingual study coordinators. Participants received a gift card after completing each survey. Institutional review board approval for this study was obtained through both sites.
Data
Medical records were abstracted for clinical and injury mechanism data by trained study coordinators using a standardized data abstraction form. Coordinators followed a manual of operations and met weekly to review data questions. Data were reviewed during collection, and queries for out-of-range or missing data were checked against source documentation. Survey questions focused on healthcare utilization during the assessment period and the time required to obtain these services. Finally, we asked respondents to report the amount of work missed, miles traveled, and travel expenses due to their child’s health. These survey questions were adapted from instruments used in prior published studies.7,8
Outcome variables
Our outcome measures are classified as healthcare utilization, travel expenses, or indirect/time costs. The values for each of these variables were elicited from parents of the injured children through surveys at the 3 time periods (0-3, 3-6, or 6-12 months following discharge from the hospital for the initial injury).
The healthcare utilization variables included indicators for whether the injured child had any ED visits, hospital admissions, over-the-counter (OTC) medications, and prescription medications during the time period in question. Travel expenses included expenditures incurred for healthcare visits including gasoline, public transportation, or parking. Indirect costs represent the time that patients or caregivers spend pursuing healthcare activities. In our study, these costs were related to the healthcare activities of the injured child and included the number of days missed from work, the number of miles traveled, time spent in ED visits following the initial injury, and time spent for all healthcare encounters following the initial injury. These indirect “costs” are measured in their natural units including days for missed work, miles for the distance traveled, and hours for the time spent in ED and all healthcare encounters. However, in secondary calculations, we converted these estimates into dollars to enhance their usability in assessing the burden of pediatric TBI. Assuming an 8-hour workday, we multiplied the estimated mean number of work days missed for parents of children with TBI by the mean daily wage. This mean daily wage was calculated from site-specific mean hourly wages obtained from the US Department of Labor ($21.22 for site 1 and $22.38 for site 2) plus 30% for benefits. Using recently published estimates of the incidence of pediatric TBI from Koepsell et al9 and the number of children in the United States in 2016 from the US Census Bureau,10 we constructed estimates of the aggregate number of missed workdays and productivity cost in the 12 months following injury each year.
Independent variables
The key exposure for our primary analyses was the presence of TBI versus OI. In secondary analyses, TBI was further categorized into levels of severity based on the Glasgow Coma Scale (GCS)11: mild, complicated mild/moderate, and severe. TBI cases were deemed to be mild, according to the CDC and World Health Organization (WHO) definitions, if these injuries had a GCS score of 13 or higher when the child presented in a healthcare setting, a score of at least 15 at discharge or after 24 hours if hospitalized, and 1 or more of the following: a period of transient confusion, loss of consciousness for 30 minutes or less, posttraumatic amnesia for less than 2 hours, or transient neurological abnormalities. Computed tomographic scans were read by pediatric neuroradiologists at each site and used to subclassify the children with mild TBI as having mild or complicated mild TBI based on the presence of intracranial hemorrhage. We categorized children with GCS scores between 9 and 12 as having moderate TBI and those with GCS scores between 3 and 8 as having severe TBI. Very few of the children in our cohort had moderate TBI, so because of similarities in outcomes noted in previous studies,12 we grouped these individuals with those with complicated mild TBI.
Our multivariable analyses controlled for a number of covariates, including patient demographic characteristics (age, race, and sex), parent demographic characteristics (education level, marital status, and employment), family characteristics (insurance type, rurality, below the poverty level, receipt of financial assistance, General Functioning Scale of the McMaster Family Assessment Device,13 and Social Capital Index14), and admission type (ED-only, inpatient admission, pediatric intensive care unit admission).
Statistical analysis
To determine the healthcare utilization, healthcare-related travel expenses, and indirect costs associated with TBI, we estimated multivariable regression models appropriate for each outcome. These models controlled for the covariates outlined earlier. We used logistic models for binary outcomes (healthcare utilization) and 2-part models for outcomes with excessive zeros and continuous, nonzero values (healthcare-related travel expenses and indirect cost outcomes).15 For the 2-part models, we used logistic models for part 1 and generalized linear models (GLMs) for part 2. We used the modified Park test to determine the appropriate distributional family for our GLM regressions. Each model was run separately for each of the 3 outcome time periods (0-3, 3-6, and 6-12 months). Results of the 2-part models were converted to their natural units (ie, dollars, days, miles, and hours) to examine the impact of TBI on the outcome across both the first and second parts of the model using the method of recycled predictions.16 We restricted the models for days of missed work outcomes to just those respondents who were employed at the baseline interview. We ran each model first with all patients included and then separately for each site. Finally, we ran regression analyses for the missed work outcome variable stratified on age, marital status, and poverty-level variables. Our age groups for stratification (0-4, 5-9, 10-14, and 15 years) were based on those used in a recent study that reported incident rates for pediatric TBI in the United States.9 We aligned our age groups in this way so as to apply the age group–specific estimates of missed work associated with pediatric TBI with the age group-specific incidence rates of pediatric TBI from the Koepsell et al9 article to generate estimates of the aggregate burden of missed work due to these injuries. To construct these estimates, we summed the significant effects from the age-stratified missed work regressions using the TBI variable categorized by severity across each of the 3 time periods and then multiplied this sum by the estimated number of pediatric TBIs per year by age and severity. The number of pediatric TBIs in the United States per year was calculated by applying the incidence rates from Koepsell et al9 to the number of children in the United States in 2016 from the US Census Bureau.10
RESULTS
Patient characteristics
We enrolled a total of 715 patients across the 2 sites (see Supplemental Figure 1, available at: http://links.lww.com/JHTR/A273), of whom, 531 had TBI and 184 had OI (see Table 1). Of those with TBI, 201 (37.9%) had mild TBI, 215 (40.5%) had complicated mild or moderate TBI, and 115 (21.7%) had severe TBI.
TABLE 1.
patient characteristicsa
| Overall (n = 715) |
Site 1 (n = 401) |
Site 2 (n = 314) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Orthopedic (n = 184) |
TBI (n = 531) |
Orthopedic (n = 101) |
TBI (n = 300) |
Orthopedic (n = 83) |
TBI (n = 231) |
||||||||||
| Variable | n | % | n | % | P | n | % | n | % | P | n | % | n | % | P |
| TBI type | |||||||||||||||
| No TBI | 184 | 100.0 | 101 | 100.0 | 83 | 100.0 | |||||||||
| Mild TBI | 0 | 0.0 | 201 | 37.9 | 0 | 0.0 | 109 | 36.3 | 0 | 0.0 | 92 | 39.8 | |||
| Complicated mild TBI/moderate TBI | 0 | 0.0 | 215 | 40.5 | 0 | 0.0 | 121 | 40.3 | 0 | 0.0 | 94 | 40.7 | |||
| Severe TBI | 0 | 0.0 | 115 | 21.7 | 0 | 0.0 | 70 | 23.3 | 0 | 0.0 | 45 | 19.5 | |||
| Age | |||||||||||||||
| 0-30 mo | 45 | 24.5 | 127 | 23.9 | .999 | 25 | 24.8 | 65 | 21.7 | .937 | 20 | 24.1 | 62 | 26.8 | .969 |
| 31 mo to 5 y | 46 | 25.0 | 132 | 24.9 | 24 | 23.8 | 73 | 24.3 | 22 | 26.5 | 59 | 25.5 | |||
| 6-11 y | 46 | 25.0 | 134 | 25.2 | 24 | 23.8 | 76 | 25.3 | 22 | 26.5 | 58 | 25.1 | |||
| 12-15 y | 47 | 25.5 | 138 | 26.0 | 28 | 27.7 | 86 | 28.7 | 19 | 22.9 | 52 | 22.5 | |||
| Female | 69 | 37.5 | 200 | 37.7 | 1.000 | 39 | 38.6 | 108 | 36.0 | .635 | 30 | 36.1 | 92 | 39.8 | .601 |
| Race | |||||||||||||||
| Black, non-Hispanic | 13 | 7.1 | 44 | 8.3 | .711 | 3 | 3.0 | 0 | 0.0 | .055 | 10 | 12.0 | 44 | 19.0 | .613 |
| Hispanic or Latino | 57 | 31.0 | 141 | 26.6 | 14 | 13.9 | 36 | 12.0 | 43 | 51.8 | 105 | 45.5 | |||
| Other, non-Hispanic | 10 | 5.4 | 39 | 7.3 | 6 | 5.9 | 27 | 9.0 | 4 | 4.8 | 12 | 5.2 | |||
| White, non-Hispanic | 102 | 55.4 | 297 | 55.9 | 77 | 76.2 | 229 | 76.3 | 25 | 30.1 | 68 | 29.4 | |||
| Missing | 2 | 1.1 | 10 | 1.9 | 1 | 1.0 | 8 | 2.7 | 1 | 1.2 | 2 | 0.9 | |||
| Admission type | |||||||||||||||
| ED/OBS only | 124 | 67.4 | 128 | 24.1 | .000 | 89 | 88.1 | 57 | 19.0 | .000 | 35 | 42.2 | 71 | 30.7 | .000 |
| Hospital but not PICU | 59 | 32.1 | 158 | 29.8 | 12 | 11.9 | 109 | 36.3 | 47 | 56.6 | 49 | 21.2 | |||
| PICU | 1 | 0.5 | 245 | 46.1 | 0 | 0.0 | 134 | 44.7 | 1 | 1.2 | 111 | 48.1 | |||
| Insurance type | |||||||||||||||
| Commercial/private/military | 108 | 58.7 | 266 | 50.1 | .046 | 79 | 78.2 | 188 | 62.7 | .007 | 29 | 34.9 | 78 | 33.8 | .978 |
| Medicaid/CHIP | 68 | 37.0 | 213 | 40.1 | 19 | 18.8 | 76 | 25.3 | 49 | 59.0 | 137 | 59.3 | |||
| None | 8 | 4.3 | 51 | 9.6 | 3 | 3.0 | 35 | 11.7 | 5 | 6.0 | 16 | 6.9 | |||
| Missing | 0 | 0.0 | 1 | 0.2 | 0 | 0.0 | 1 | 0.3 | 0 | 0.0 | 0 | 0.0 | |||
| One of parents currently employed | 160 | 87.0 | 476 | 89.6 | .371 | 92 | 91.1 | 280 | 93.3 | .505 | 68 | 81.9 | 196 | 84.8 | .609 |
| Parental education | |||||||||||||||
| Bachelor’s degree or higher | 67 | 36.4 | 130 | 24.5 | .002 | 50 | 49.5 | 88 | 29.3 | .000 | 17 | 20.5 | 42 | 18.2 | .621 |
| High school | 26 | 14.1 | 129 | 24.3 | 8 | 7.9 | 67 | 22.3 | 18 | 21.7 | 62 | 26.8 | |||
| Less than high school | 30 | 16.3 | 70 | 13.2 | 8 | 7.9 | 24 | 8.0 | 22 | 26.5 | 46 | 19.9 | |||
| Vocational/some college | 61 | 33.2 | 200 | 37.7 | 35 | 34.7 | 121 | 40.3 | 26 | 31.3 | 79 | 34.2 | |||
| Missing | 0 | 0.0 | 2 | 0.4 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 0.9 | |||
| Marital status | |||||||||||||||
| No | 54 | 29.3 | 159 | 29.9 | .978 | 22 | 21.8 | 57 | 19.0 | .757 | 32 | 38.6 | 102 | 44.2 | .653 |
| Yes | 128 | 69.6 | 365 | 68.7 | 79 | 78.2 | 241 | 80.3 | 49 | 59.0 | 124 | 53.7 | |||
| Missing | 2 | 1.1 | 7 | 1.3 | 0 | 0.0 | 2 | 0.7 | 2 | 2.4 | 5 | 2.2 | |||
| Rural | 24 | 13.0 | 110 | 20.7 | .028 | 11 | 10.9 | 81 | 27.0 | .001 | 13 | 15.7 | 29 | 12.6 | .603 |
| Below poverty level | |||||||||||||||
| No | 127 | 69.0 | 346 | 65.2 | .158 | 82 | 81.2 | 223 | 74.3 | .158 | 45 | 54.2 | 123 | 53.2 | .610 |
| Yes | 49 | 26.6 | 139 | 26.2 | 17 | 16.8 | 57 | 19.0 | 32 | 38.6 | 82 | 35.5 | |||
| Missing | 8 | 4.3 | 46 | 8.7 | 2 | 2.0 | 20 | 6.7 | 6 | 7.2 | 26 | 11.3 | |||
| Family receives any assistanceb | 63 | 34.2 | 203 | 38.2 | .349 | 20 | 19.8 | 84 | 28.0 | .221 | 43 | 51.8 | 119 | 51.5 | .101 |
| Problematic family functioningc | 21 | 11.4 | 66 | 12.4 | .794 | 10 | 9.9 | 32 | 10.7 | 1.000 | 11 | 13.3 | 34 | 14.7 | .856 |
| Social Capital Indexd | 3.6 | 1.1 | 3.5 | 1.1 | .404 | 3.7 | 1.0 | 3.6 | 1.0 | .593 | 3.4 | 1.1 | 3.3 | 1.2 | .503 |
Abbreviations: ED, emergency department; OBS, observation unit; PICU; pediatric intensive care unit; TBI, traumatic brain injury;
Statistical comparisons were made using χ2 tests for categorical variables and t tests for continuous variables.
Any assistance = public housing; supplemental security income; food stamps/Supplemental Nutrition Assistance Program (SNAP); Temporary Assistance for Needy Families; Special Supplemental Nutrition Program for Women, Infants, and Children (WIC).
Problematic family functioning = McMaster Family Assessment Device score 2 or more.
Social Capital Index = scored 0 to 5, with higher numbers indicating better function.
A total of 401 patients (300 with TBI and 101 with OI) were enrolled at site 1 and 314 patients (231 with TBI and 83 with OI) were enrolled at site 2. Patients with AHT made up 61% (n = 11) of the severe TBI patients in our sample younger than 2 years, which is slightly higher than the 53% reported in other published studies.17
Unadjusted cost estimates
Parents of children with TBI missed more days of work during months 0 to 3 (8.2 vs 2.4, P < .0001) and 3 to 6 (4.9 vs 2.1, P = .015) than parents of those with OI. In addition, more patients with TBI had OTC (44.5% vs 33.8%, P = .009) and prescription medications (13.5% vs 6.6%, P = .009) during the 3- to 6-month period than those with OI (see Figure 1).
Figure 1.
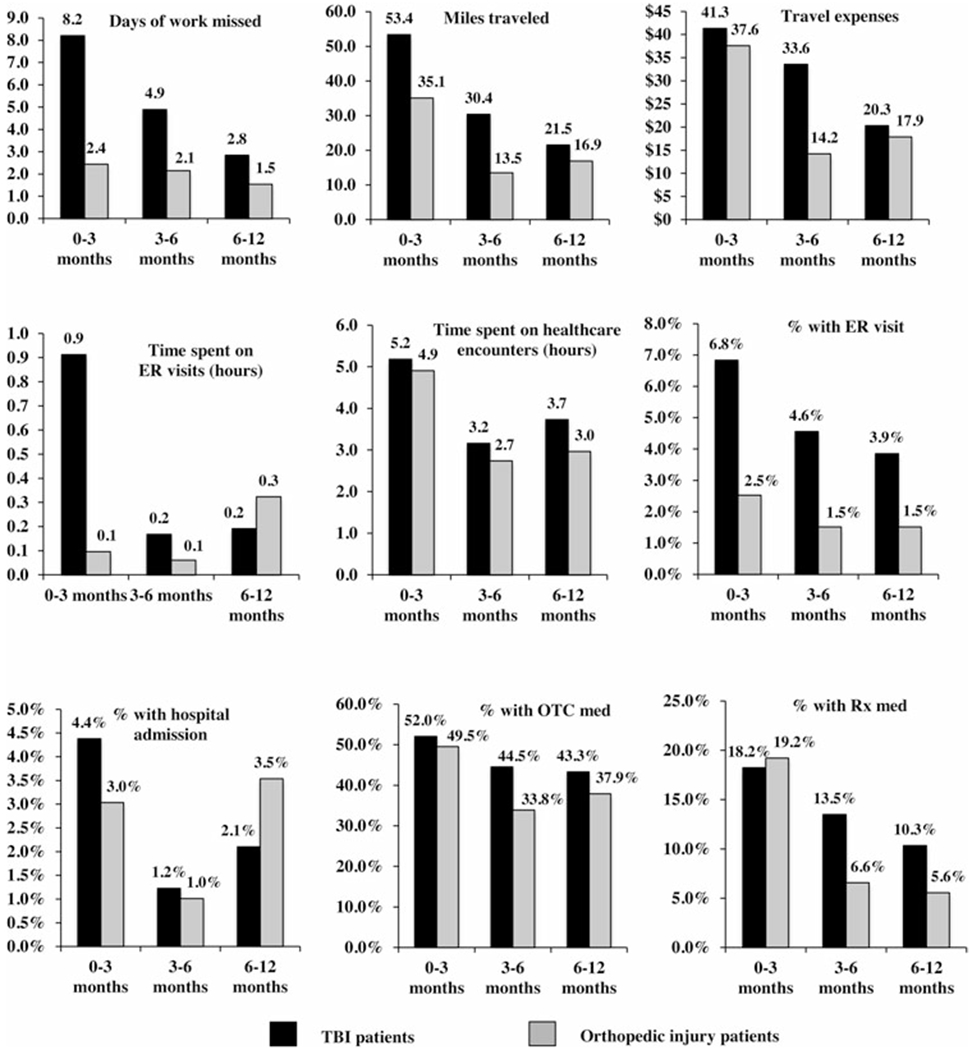
Descriptive statistics for outcome variables.
Multivariable regression models
Table 2 contains the results for the multivariable regression analyses for TBI compared with OI. Parents of children with TBI missed 6.23 (95% CI, 5.35-7.11) and 13.22 (95% CI, 9.22-17.22) more days of work than those with OI during the first 3 months and months 3 to 6 following their injury, respectively. In addition, during months 3 to 6 after their injury, parents of children with TBI traveled 3.09 (95% CI, 2.17-4.01) more miles for their child’s healthcare encounters than those of children with OI. For direct healthcare costs, children with TBI had greater odds of having an ED visit in the first 3 months (odds ratio [OR] = 3.04; 95% CI, 1.12-8.24) and months 3 to 6 (OR = 5.00; 95% CI, 1.08-23.24) after their injury and both OTC (OR = 1.98; 95% CI, 1.34-2.94) and prescription medications (OR = 2.34; 95% CI, 1.19-4.59) during months 3 to 6 following their injury.
TABLE 2.
Multivariable regression results—traumatic brain injury overall compared with orthopedic injurya
| 3 mo 95% CI |
3-6 mo 95% CI |
6-12 mo 95% CI |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Effect | LL | UL | P | Effect | LL | UL | P | Effect | LL | UL | P |
| Overall | ||||||||||||
| Indirect costs (absolute difference) | ||||||||||||
| Days of work missed | 6.23 | 5.35 | 7.11 | <.0001 | 13.22 | 9.22 | 17.22 | <.0001 | 0.46 | −0.54 | 1.45 | .366 |
| Miles traveled | 6.26 | −8.73 | 21.24 | .413 | 3.09 | 2.17 | 4.01 | <.0001 | 2.14 | −2.23 | 6.52 | .338 |
| Travel expenses, $ | 0.07 | −17.19 | 17.32 | .994 | 10.39 | −1.88 | 22.65 | .097 | −3.19 | −16.90 | 10.51 | .648 |
| Time spent on healthcare encounters, h | −0.16 | −1.84 | 1.51 | .850 | 0.81 | −0.15 | 1.77 | .099 | 1.11 | −0.18 | 2.39 | .092 |
| Direct costs (odds ratio) | ||||||||||||
| ED visit | 3.04 | 1.12 | 8.24 | .029 | 5.00 | 1.08 | 23.24 | .040 | 2.38 | 0.64 | 8.90 | .198 |
| Hospital admission | 1.29 | 0.49 | 3.40 | .608 | 0.28 | 0.01 | 10.63 | .492 | 0.79 | 0.24 | 2.60 | .697 |
| OTC medications | 1.17 | 0.79 | 1.73 | .437 | 1.98 | 1.34 | 2.94 | .001 | 1.43 | 0.98 | 2.09 | .066 |
| Prescription medications | 0.81 | 0.51 | 1.27 | .353 | 2.34 | 1.19 | 4.59 | .013 | 1.74 | 0.84 | 3.58 | .135 |
| Site 1 | ||||||||||||
| Indirect costs (absolute difference) | ||||||||||||
| Days of work missed | 8.12 | 6.89 | 9.34 | <.0001 | 3.75 | 2.44 | 5.06 | <.0001 | 3.65 | 2.01 | 5.28 | <.0001 |
| Miles traveled | 34.36 | 13.04 | 55.67 | .002 | 28.65 | 21.70 | 35.60 | <.0001 | 11.15 | 4.23 | 18.06 | .002 |
| Travel expenses, $ | 29.28 | 21.60 | 36.96 | <.0001 | 39.94 | −12.79 | 92.67 | .138 | 3.54 | −13.22 | 20.31 | .679 |
| Time spent on healthcare encounters, h | 0.67 | −0.47 | 1.80 | .248 | 2.27 | 0.86 | 3.68 | .002 | 1.78 | −0.26 | 3.82 | .087 |
| Direct costs (odds ratio) | ||||||||||||
| ED visit | 2.39 | 0.57 | 9.99 | .232 | 22.06 | 1.16 | 420.65 | .040 | … | … | … | … |
| Hospital admission | 4.40 | 0.40 | 48.58 | .226 | … | … | … | … | 2.14 | 0.32 | 14.33 | .431 |
| OTC medications | 1.40 | 0.79 | 2.49 | .254 | 2.30 | 1.33 | 3.98 | .003 | 1.50 | 0.88 | 2.55 | .132 |
| Prescription medications | 0.96 | 0.47 | 1.95 | .913 | 6.53 | 1.78 | 23.91 | .005 | 2.94 | 0.91 | 9.53 | .072 |
| Site 2 | ||||||||||||
| Indirect costs (absolute difference) | ||||||||||||
| Days of work missed | 5.21 | 3.91 | 6.52 | <.0001 | 4.13 | 2.23 | 6.03 | <.0001 | 1.12 | −1.03 | 3.27 | .307 |
| Miles traveled | −28.64 | −35.63 | −21.65 | <.0001 | −3.17 | −8.91 | 2.57 | .280 | −8.08 | −13.10 | −3.06 | .002 |
| Travel expenses, $ | −46.02 | −80.22 | −11.82 | .008 | −9.59 | −18.56 | −0.63 | .036 | −9.77 | −37.57 | 18.04 | .491 |
| Time spent on healthcare encounters, h | −3.12 | −6.17 | −0.06 | .045 | 0.04 | −1.45 | 1.54 | .954 | 0.06 | −0.76 | 0.88 | .894 |
| Direct costs (odds ratio) | ||||||||||||
| ED visit | 6.61 | 1.11 | 39.37 | .038 | 2.25 | 0.13 | 39.92 | .581 | … | … | … | … |
| Hospital admission | 0.72 | 0.17 | 3.04 | .660 | … | … | … | … | 0.22 | 0.01 | 4.49 | .325 |
| OTC medications | 1.04 | 0.56 | 1.93 | .889 | 1.73 | 0.92 | 3.26 | .092 | 1.48 | 0.81 | 2.71 | .201 |
| Prescription medications | 0.69 | 0.34 | 1.39 | .303 | 2.00 | 0.79 | 5.08 | .145 | 1.22 | 0.40 | 3.72 | .726 |
Abbreviations: CI, confidence interval; ED, emergency department; LL, lower limit; OTC, over-the-counter; UL, upper limit.
Regressions controlled for age, sex, race, admission type, insurance type, parental employment, parental education, marital status, rurality, poverty level, receipt of government financial assistance, indicator for problematic family functioning, and Social Capital Index. Site-specific estimates for hospital admission during months 3 to 6 and ED visits during months 6 to 12 could not be generated because of insufficient number of events.
Parents of children with TBI missing significantly more days of work than those of children with OI in both sites. However, there were large differences between the 2 sites in the effect on miles traveled and travel expenses, with a positive effect for both outcomes at site 1 and a negative effect for both outcomes at site 2.
Table 3 contains the results of our multivariable regression models in which TBI was further characterized by severity. While the results generally follow those from models in which TBI was considered overall, the magnitude of the effects shown in Table 3 increases with TBI severity. For example, compared with parents of children with OI, those whose children had mild, complicated mild/moderate, or severe TBI missed 2.82 (95% CI, 1.92-3.72), 5.03 (95% CI, 3.93-6.3), and 14.68 (95% CI, 11.84-17.53) days of work during the first 3 months following injury, respectively. For months 3 to 6 following injury, the missed workdays were 2.40 (95% CI, 1.31-3.49) for those of children with complicated mild/moderate TBI and 11.78 (95% CI, 8.49-15.06) for those of children with severe TBI; for months 6 to 12, missed workdays were 3.14 (95% CI, 1.10-5.18) for those of children with severe TBI. In addition, those with severe TBI had elevated odds of having ED visits, hospital admissions, OTC medications, and prescription medications compared with those with OI. Supplemental Digital Content Table 1 (available at: http://links.lww.com/JHTR/A275) and Table 2 (available at: http://links.lww.com/JHTR/A276) show similar results at site 1 and site 2, respectively.
TABLE 3.
Multivariable regression results—traumatic brain injury characterized by severity compared with orthopedic injurya
| 3 mo 95% CI |
3-6 mo 95% CI |
6-12 mo 95% CI |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Effect | LL | UL | P | Effect | LL | UL | P | Effect | LL | UL | P |
| Indirect costs (absolute difference) | ||||||||||||
| Days of work missed | ||||||||||||
| Mild | 2.82 | 1.92 | 3.72 | <.0001 | 0.57 | −0.30 | 1.45 | .201 | −1.44 | −2.39 | −0.49 | .003 |
| Complicated mild/moderate | 5.03 | 3.93 | 6.13 | <.0001 | 2.40 | 1.31 | 3.49 | <.0001 | 0.68 | −0.57 | 1.94 | .286 |
| Severe | 14.68 | 11.84 | 17.53 | <.0001 | 11.78 | 8.49 | 15.06 | <.0001 | 3.14 | 1.10 | 5.18 | .003 |
| Miles traveled | ||||||||||||
| Mild | −16.37 | −31.26 | −1.48 | .031 | 6.91 | 1.90 | 11.92 | .007 | −8.13 | −12.30 | −3.96 | <.0001 |
| Complicated mild/moderate | 4.49 | −12.38 | 21.36 | .602 | 9.47 | 4.58 | 14.36 | <.0001 | −2.11 | −6.87 | 2.65 | .385 |
| Severe | 54.51 | 19.68 | 89.33 | .002 | 32.14 | 25.09 | 39.19 | <.0001 | 31.61 | 21.94 | 41.28 | <.0001 |
| Travel expenses, $ | ||||||||||||
| Mild | −16.07 | −32.93 | 0.79 | .062 | −0.06 | −12.35 | 12.23 | .992 | −9.85 | −21.61 | 1.91 | .101 |
| Complicated mild/moderate | −11.76 | −28.70 | 5.18 | .174 | −0.11 | −11.76 | 11.54 | .986 | −7.34 | −19.17 | 4.50 | .224 |
| Severe | 53.74 | 11.92 | 95.55 | .012 | 55.14 | 16.44 | 93.83 | .005 | 35.11 | −1.47 | 71.70 | .060 |
| Time spent on healthcare encounters, h | ||||||||||||
| Mild | −1.98 | −3.72 | −0.24 | .026 | 0.01 | −1.17 | 1.20 | .984 | −0.48 | −1.63 | 0.67 | .415 |
| Complicated mild/moderate | 0.15 | −1.82 | 2.11 | .884 | 0.87 | −0.39 | 2.13 | .175 | 1.49 | −0.39 | 3.38 | .121 |
| Severe | 2.49 | −0.95 | 5.92 | .156 | 2.17 | 0.36 | 3.98 | .019 | 3.61 | 0.31 | 6.91 | .032 |
| Direct costs (odds ratio) | ||||||||||||
| ED visit | ||||||||||||
| Mild | 1.87 | 0.58 | 6.05 | .297 | 5.14 | 0.98 | 27.09 | .053 | 1.22 | 0.24 | 6.26 | .812 |
| Complicated mild/moderate | 2.62 | 0.85 | 8.07 | .093 | 1.71 | 0.25 | 11.49 | .580 | 1.72 | 0.36 | 8.22 | .496 |
| Severe | 8.41 | 2.56 | 27.64 | <.0001 | 15.60 | 2.74 | 88.79 | .002 | 8.04 | 1.72 | 37.63 | .008 |
| Hospital admission | ||||||||||||
| Mild | 0.58 | 0.15 | 2.20 | .425 | 0.29 | 0.00 | 61.10 | .650 | 0.96 | 0.23 | 4.02 | .954 |
| Complicated mild/moderate | 0.74 | 0.21 | 2.63 | .646 | 0.03 | 0.00 | 22.55 | .293 | 0.43 | 0.07 | 2.52 | .352 |
| Severe | 5.21 | 1.68 | 16.15 | .004 | … | … | … | … | 1.15 | 0.22 | 5.95 | .870 |
| OTC medications | ||||||||||||
| Mild | 1.09 | 0.69 | 1.74 | .701 | 1.84 | 1.16 | 2.90 | .009 | 1.14 | 0.73 | 1.78 | .576 |
| Complicated mild/moderate | 1.08 | 0.68 | 1.71 | .749 | 1.97 | 1.25 | 3.11 | .003 | 1.43 | 0.92 | 2.24 | .112 |
| Severe | 1.57 | 0.90 | 2.74 | .115 | 2.33 | 1.36 | 4.00 | .002 | 2.21 | 1.30 | 3.77 | .004 |
| Prescription medications | ||||||||||||
| Mild | 0.27 | 0.14 | 0.53 | <.0001 | 1.39 | 0.63 | 3.09 | .417 | 0.94 | 0.38 | 2.32 | .888 |
| Complicated mild/moderate | 0.84 | 0.49 | 1.46 | .546 | 2.15 | 1.00 | 4.63 | .050 | 1.62 | 0.70 | 3.72 | .259 |
| Severe | 2.68 | 1.47 | 4.90 | .001 | 5.33 | 2.40 | 11.87 | <.0001 | 4.06 | 1.71 | 9.66 | .002 |
Abbreviations: CI, confidence interval; ED, emergency department; LL, lower limit; OTC, over-the-counter; UL, upper limit.
Regressions controlled for age, sex, race, admission type, insurance type, parental employment, parental education, marital status, rurality, poverty level, receipt of government financial assistance, indicator for problematic family functioning, and Social Capital Index.
In stratified analyses with TBI as a binary variable (see Supplemental Digital Content Table 3, available at: http://links.lww.com/JHTR/A277), parents of children in the 10- to 14-year age group had the most missed workdays: 10.20 (95% CI, 5.31-14.10) for the first 3 months; 9.24 (95% CI, 4.45-14.03) for months 3 to 6; and 3.45 (95% CI, 0.06-1.73) for months 6 to 12. TBI had a similar impact on missed workdays for parents who were and were not married across all 3 time periods, and TBI was significantly associated with parents missing work in those above the poverty line, 12.77 (95% CI, 7.76-17.78) for months 0 to 3 and 5.63 (95% CI, 1.20-10.06) for months 3-6, but not in those below the poverty line. Finally, for the most part, the number of days of missed work increased with severity of for each stratified analysis (see Supplemental Digital Content Table 4, available at: http://links.lww.com/JHTR/A278).
Aggregate burden estimates
Results from our aggregate burden calculations are presented in Supplemental Digital Content Figure 2 (http://links.lww.com/JHTR/A274). Using the Koepsell et al9 incidence rates, we estimate that 243 623 cases of pediatric TBI occur in the United States each year, with the vast majority of those cases (97.2%) being mild. Applying our estimates of the number of missed workdays per case to this estimate of the total number of pediatric TBIs, we calculated a total of 791 657 (95% CI, 755 232-828 081) missed workdays due to pediatric TBI per year in the United States, which translates into $179.5 million (95% CI, 171.2-187.8) in lost productivity.
DISCUSSION
This study is the first to estimate the impact of childhood TBI on parents’ missed work, travel expenses, and time spent on healthcare encounters for their injured children. We found that parents of children with TBI at site 1 missed 15.51 (95% CI, 10.76-20.27) days of work whereas those at site 2 missed 10.47 (95% CI, 4.29-16.65) days of work during the 12 months following injury. These costs represent lost productivity to the society and lost wages for parents whose employment does not allow them to take paid leave for personal matters. In secondary analyses, we calculate that pediatric TBIs are associated with an estimated 791 657 (95% CI, 755 232-828 081) days of work are missed each year, amounting to $179.5 million (95% CI, 171.2-187.8) in lost productivity.
In addition, we found that parents of TBI patients at site 1 traveled 74.15 (95% CI, 28.16-120.14) miles more than those of children with OI controls during this 1-year period whereas those at site 2 traveled 39.89 (95% CI, 19.61-60.16) miles less. Rural families, who were more concentrated in site 1, frequently must travel long distances to receive specialty care and incur higher costs.
The results for healthcare utilization are consistent with those reported in other studies. For example, Graves et al3 compared total healthcare costs for those with moderate and severe TBIs with those with mild TBIs using data from the MarketScan Commercial Claims and Encounters database. In the 12 months following TBI diagnosis, they found that, relative to mild TBI, cost ratios ranged from 1.84 to 11.07 for severe TBI and 1.33 to 4.91 for moderate TBI depending on age. Leibson and coauthors,4 using data from the Rochester Epidemiology Project and matched TBI patients with randomly selected non-TBI patients on patient characteristics. Individuals with TBI had $3418 higher costs over a 6-year period than their matched counterparts. Finally, TeAoet al18 conducted an incidence-based cost-of-illness analysis of direct and indirect costs of TBI in adults in New Zealand. They estimated that for the 17% of individuals in their cohort who incurred any indirect costs in the year following injury, these costs averaged $2000 (95% CI, 1658-2385).
Our analysis improves on these previous studies in several important ways. First, we included non-TBI control patients with non-head-injured patients. Therefore, the increased healthcare utilization and indirect costs found here are more likely to truly represent the costs associated with TBI. Second, our study is the first to include measures of parental time in an assessment of the burden of pediatric TBI. As we have found, missed workdays and travel costs are substantial and give new insight into the burden borne by families of children with TBI. Third, our study was conducted in 2 sites in the United States, allowing us to examine similarities and differences across these settings. For instance, the positive relationship between TBI severity and missed workdays was seen in both site 1 and site 2 study participants. However, while the number of miles traveled to receive care for participants in site 1 was positive and higher for more severe TBI cases, families of children with TBI in site 2 traveled significantly fewer miles than controls. These stark differences are likely due to differences in geography and referral patterns at each institution.
Our study had several limitations. First, because our data were collected through surveys, they may be inaccurate due to recall bias. Second, while children were enrolled from 2 states, our results may not be generalizable to children and their families from other regions. For example, several recent publications have documented differences in a variety of pediatric TBI outcomes such as discharge to rehabilitation and inpatient mortality by region or state in the United States.19,20 An additional study described factors that are important for successful recovery for pediatric TBI patients (including identifying at-risk children at the time of injury and receiving follow-up medical, transitional, and educational services).21 These studies suggest that the availability and adequacy of acute and follow-up care may be quite different in different areas of the country, which could lead to differences in the outcomes of our study. It is also true that the generalizability of our results may be limited by the extent to which the participants in our study differ from the general population of children with TBI. For example, the contribution of AHT to our estimates of the postinjury consequences of TBI may be slightly higher because of small differences, relative to other published studies, in the proportion of children with severe TBI younger than 2 years than the proportion of those with AHT (61% in our study vs 53% in the Keenan et al17 study) and in the proportion of younger children in our cohort (44% in our study vs 39% in the Koepsell et al9). Third, while our study expands the previously understood estimates of total societal burden of pediatric TBI, there may be additional costs to families that we were not able to measure. For example, some families may need to make modifications to their home to accommodate their injured child such as installing ramps or handrails. Fourth, our utilization and missed work outcomes were not TBI specific. By performing regression models with both TBI and non-TBI patients that controlled for a number of observable patient characteristics, we did our best to tease out the outcomes that were attributable to TBI but our estimated effects likely still contain some non–TBI-related healthcare utilization and missed work. Finally, the patients in our TBI group may have had additional injuries that could have contributed to the direct and indirect cost outcomes analyzed here. However, in additional analyses, we restricted our TBI patients to those with no additional injuries and our results were consistent with those reported here.
In conclusion, we found that children with TBI were more likely to have ED visits and use both OTC and prescription medications than the OI control children. In addition, parents of children with TBI missed significantly more workdays than parents of OI children and the magnitude of this effect increased with TBI severity. These missed workdays, extrapolated to the whole country using age-specific incidence rates, represent a substantial amount of lost productivity. Future research should investigate predictors of missed workdays and travel cost among families of pediatric TBI patients and to identify additional factors that modify this effect including socioeconomic status (which has been shown to be associated with pediatric injury risk22), community and family support, and geographic location.
Supplementary Material
Acknowledgments
This material is the result of work supported with resources and the use of facilities at the George E. Wahlen Department of Veterans Affairs Medical Center, Salt Lake City, Utah. This study was supported with funding from the Centers for Disease Control and Prevention (co-PIs: Keenan and Ewing-Cobbs) and the VA Health Services Research and Development Service (I50HX001240–Center of Innovation, Informatics, Decision-Enhancement and Analytic Sciences [IDEAS] 2.0 Center and IK2 HX000860-01 A2, Nelson).
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.headtraumahab.com).
The authors declare no conflicts of interest.
Contributor Information
Richard E. Nelson, Veterans Affairs Salt Lake City Health Care System, Salt Lake City, Utah; Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City.
Junjie Ma, Veterans Affairs Salt Lake City Health Care System, Salt Lake City, Utah; Department of Pharmacotherapy, University of Utah College of Pharmacy, Salt Lake City.
Yan Cheng, George Washington University Informatics Center, Washington, District of Columbia.
Linda Ewing-Cobbs, Department of Pediatrics, University of Texas Houston Health Sciences Center.
Amy Clark, Department of Pediatrics, University of Utah, Salt Lake City.
Heather Keenan, Department of Pediatrics, University of Utah, Salt Lake City.
REFERENCES
- 1.Centers for Disease Control and Prevention. TBI data and statistics. https://www.cdc.gov/traumaticbraininjury/data. Accessed January 2, 2017. [Google Scholar]
- 2.Marin JR, Weaver MD, Yealy DM, Mannix RC. Trends in visits for traumatic brain injury to emergency departments in the United States. JAMA. 2014;311(18):1917–1919. [DOI] [PubMed] [Google Scholar]
- 3.Graves JM, Rivara FP, Vavilala MS. Health care costs 1 year after pediatric traumatic brain injury. Am J Public Health. 2015; 105(10):e35–e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leibson CL, Brown AW, Hall Long K, et al. Medical care costs associated with traumatic brain injury over the full spectrum of disease: a controlled population-based study. J Neurotrauma. 2012;29(11):2038–2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krol M, Brouwer W, Rutten F. Productivity costs in economic evaluations: past, present, future. Pharmacoeconomics. 2013;31(7):537–549. [DOI] [PubMed] [Google Scholar]
- 6.Marr AL, Coronado VG. Central Nervous System Injury Surveillance Data Submission Standards: 2002. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2002. [Google Scholar]
- 7.Lee GM, Lett S, Schauer S, et al. Societal costs and morbidity of pertussis in adolescents and adults. Clin Infect Dis. 2004;39(11):1572–1580. [DOI] [PubMed] [Google Scholar]
- 8.Pfoh E, Wessels MR, Goldmann D, Lee GM. Burden and economic cost of group A streptococcal pharyngitis. Pediatrics. 2008;121(2):229–234. [DOI] [PubMed] [Google Scholar]
- 9.Koepsell TD, Rivara FP, Vavilala MS, et al. Incidence and descriptive epidemiologic features of traumatic brain injury in King County, Washington. Pediatrics. 2011;128(5):946–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Census Bureau. National population by characteristics datasets: 2010-2016. https://www.census.gov/data/datasets/2016/demo/popest/nation-detail.html. Published 2017. Accessed May 15,2017. [Google Scholar]
- 11.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. [DOI] [PubMed] [Google Scholar]
- 12.Levin HS, Hanten G, Roberson G, et al. Prediction of cognitive sequelae based on abnormal computed tomography findings in children following mild traumatic brain injury. J Neurosurg Pediatr. 2008;1(6):461–470. [DOI] [PubMed] [Google Scholar]
- 13.Miller IW, Bishop DS, Epstein NB, Kietner GI. The McMaster Family Assessment Device: reliability and validity. J Marital Fam Ther. 1985;11:345–356. [Google Scholar]
- 14.Runyan DK, Hunter WM, Socolar RR, et al. Children who prosper in unfavorable environments: the relationship to social capital. Pediatrics. 1998;101(1, pt 1):12–18. [DOI] [PubMed] [Google Scholar]
- 15.Mullahy J Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J Health Econ. 1998;17(3):247–281. [DOI] [PubMed] [Google Scholar]
- 16.Basu A, Rathouz PJ. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics. 2005;6(1):93–109. [DOI] [PubMed] [Google Scholar]
- 17.Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH. A population-based study of inflicted traumatic brain injury in young children. JAMA. 2003;290(5):621–626. [DOI] [PubMed] [Google Scholar]
- 18.Te Ao B, Tobias M, Ameratunga S, et al. Burden of traumatic brain injury in New Zealand: incidence, prevalence and disability-adjusted life years. Neuroepidemiology. 2015;44(4):255–261. [DOI] [PubMed] [Google Scholar]
- 19.Greene NH, Kernic MA, Vavilala MS, Rivara FP. Variation in pediatric traumatic brain injury outcomes in the United States. Arch Phys Med Rehabil. 2014;95(6):1148–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mills B, Rowhani-Rahbar A, Simonetti JA, Vavilala MS. Facility characteristics and inhospital pediatric mortality after severe traumatic brain injury. J Neurotrauma. 2015;32(11):841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haarbauer-Krupa J, Ciccia A, Dodd J, et al. Service delivery in the healthcare and educational systems for children following traumatic brain injury: gaps in care. J Head Trauma Rehabil. 2017;32(6):367–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amram O, Schuurman N, Pike I, et al. Socio economic status and traumatic brain injury amongst pediatric populations: a spatial analysis in Greater Vancouver. Int J Environ Res Public Health. 2015;12(12):15594–15604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


