Abstract
Background
Women of all ages and elderly patients of both genders comprise an increasing proportion of the haemodialysis population. Worldwide, significant differences in practice patterns and treatment results exist between genders and among younger versus older patients. Although efforts to mitigate sex-based differences have been attempted, significant disparities still exist.
Methods
This retrospective cohort study included all 1247 prevalent haemodialysis patients in DaVita units in Portugal (five dialysis centres, n = 730) and Poland (seven centres, n = 517). Demographic data, dialysis practice patterns, vascular access prevalence and the achievement of a variety of Kidney Disease: Improving Global Outcomes (KDIGO) treatment targets were evaluated in relation to gender and age groups.
Results
Body weight and the prescribed dialysis blood flow rate were lower in women (P < 0.001), whereas treated blood volume per kilogram per session was higher (P < 0.01), resulting in higher single-pool Kt/V in women than in men (P < 0.001). Haemoglobin was significantly higher in men (P = 0.01), but the proportion of patients within target range (10–12 g/dL) was similar. Men more often had an arteriovenous fistula than women (80% versus 73%; P < 0.01) with a similar percentage of central venous catheters. There were no gender-specific differences in terms of dialysis adequacy, anaemia parameters or mineral and bone disorder parameters, or in the attainment of KDIGO targets between women and men >80 years of age.
Conclusions
This large, multicentre real-world analysis indicates that haemodialysis practices and treatment targets are similar for women and men, including the most elderly, in DaVita haemodialysis clinics in Europe.
Keywords: age, anemia, chronic haemodialysis, dialysis adequacy, gender
INTRODUCTION
Women comprise an increasing proportion of the haemodialysis population worldwide. Previous studies have identified differences in the treatment of kidney disease between the sexes. Women start dialysis at lower estimated renal function than men [1] and slightly older average age than men, with similar use of available dialysis modalities [2]. The proportion of women using an arteriovenous (AV) fistula is lower than that for men, and their fistula patency is worse, even when routine vascular mapping is used [3]. Women undergoing maintenance haemodialysis have substantially higher risks of hospitalization and 30-day readmission than men [4]. Furthermore, the survival advantage that women have over men in the general population is markedly diminished in haemodialysis patients [5, 6]. In fact, young women on dialysis (<45 years old) have a higher risk of mortality compared with men, mainly due to non-cardiovascular events [5].
Although most clinical dialysis guidelines apply the same target values to both men and women, studies suggest intriguing sex differences with respect to both renal anaemia and chronic kidney disease–mineral and bone disorder (CKD–MBD) [7, 8]. The coinciding of World Kidney Day and International Women’s Day 2018 offered an opportunity to focus on haemodialysis therapy in women to explore potential differences in practices compared with men.
Worldwide, the incidence of end-stage renal disease (ESRD) in the elderly has risen in the past decades resulting in a rapidly growing number of older patients starting haemodialysis [9, 10]. The ageing phenomenon in the dialysis population is amplified by a more liberal acceptance of older patients on dialysis, better survival of dialysis patients and reduced access to transplantation for elderly patients. The elderly have a higher prevalence of comorbidities that increase the burden of dialysis, and a substantially higher mortality rate compared with younger counterparts [11, 12].
Treatment of ESRD in the elderly is complex and it is not clear whether the haemodialysis prescription for the elderly should be different from that of younger patients. There are no specific guidelines to inform the clinician about practice of haemodialysis in the elderly. The predominant type of vascular access used in elderly patients varies in different regions [11]. Permanent catheters are more frequently used among elderly patients in Europe, with a similar trend seen in North America [11]. Recent data have shown that elderly patients initiating haemodialysis with a central venous catheter (CVC) who underwent AV fistula placement within 6 months had fewer hospitalizations due to infections and better survival than those receiving an AV graft [13].
There are few large, international studies focusing on sex-specific differences in patient characteristics, dialysis practices and treatment in elderly individuals on haemodialysis. The aim of this large European multicentre descriptive analysis was to study the achievement of Kidney Disease: Improving Global Outcomes (KDIGO) targets in terms of haemodialysis practices, dialysis adequacy, treatment of renal anaemia and CKD–MBD, as well as the use of vascular access in relation to gender and age.
MATERIALS AND METHODS
Patients and data collection
We included 1247 patients on maintenance haemodialysis from DaVita Portugal (five dialysis centres, n = 730) and DaVita Poland (seven dialysis centres, n = 517). The cohort of patients is representative since all prevalent patients treated at all facilities were included in the analysis, thus representing a ‘real-world’ clinical experience. Patient and treatment characteristics and biochemical data were collected during the course of routine clinical practice, and all data were analysed with respect to four age categories (<60, 60–70, 71–79 and >79 years of age) and to male or female gender. We also analysed treatment prescription, use of vascular access and the achievement of KDIGO treatment targets in women and men aged >80 years.
Demographic and laboratory data and information on practices were collected in all patients in the same month of 2018. Blood samples were collected monthly or quarterly in accordance with international clinical guidelines (European Renal Best Practice guidelines and KDIGO guidelines). All laboratory analyses were performed at local laboratories in accordance with validated and recommended routine procedures. Intact parathyroid hormone (iPTH) was measured and Kt/V was assessed as single-pool Kt/V (spKt/V) values. The correction factor for darbepoetin to epoetin doses was 250.
The study was approved by the regional ethics committee at the Karolinska Institutet, Stockholm, Sweden. All clinical and laboratory patient data were abstracted in de-identified form from the respective country. All statistical analyses were performed at the Department of Clinical Sciences at the Karolinska Institutet, Stockholm, Sweden.
Statistical analyses
Statistical analyses were performed using International Business Machines Corporation (IBM) Statistical Package for the Social Sciences (SPSS) Statistics version 25. All values are presented as mean and standard deviation or counts and proportions. Comparisons were made using Student’s t-test and Chi-squared analysis as appropriate. A P < 0.05 was considered statistically significant.
RESULTS
Results in relation to gender
Demographic data, haemodialysis prescription and laboratory parameters related to the use of vascular access, haemodialysis adequacy, renal anaemia and CKD–MBD in all female and male patients are shown in Table 1. The most common cause of ESRD in both Portugal (42%) and Poland (35%) was classified as ‘unknown’ or ‘other’. Diabetes mellitus, nephrosclerosis and glomerulonephritis were the causes of ESRD in 30, 10 and 11% of haemodialysis patients in Portugal and 25, 13 and 20%, respectively, for patients in Poland (P < 0.001).
Table 1.
Prescription of haemodialysis, patient characteristics and laboratory results in relation to gender in all 1247 patients
| Patient characteristics | Women, | Men, | P-value |
|---|---|---|---|
| mean (SD) | mean (SD) | ||
| Age (years) | 68.3 (14.1) | 67.7 (14.5) | NS |
| Dialysis vintage (months) | 61.4 (55.8) | 60.2 (60.5) | NS |
| BW (kg) | 67.7 (15.3) | 72.2 (15.0) | <0.001 |
| BMI (kg/m2) | 26.0 (5.4) | 25.7 (5.0) | NS |
| Treatment time (min) | 730 (59) | 728 (55) | NS |
| Prescribed Qb (mL/min) | 370 (46) | 379 (50) | 0.001 |
| Treated blood volume (L/kg) | 1.4 (0.4) | 1.3 (0.3) | 0.001 |
| Kt/V | 1.9 (0.4) | 1.8 (0.3) | <0.001 |
| URR (%) | 79 (8) | 77 (8) | <0.001 |
| Hb (g/dL) | 10.9 (1.1) | 11.0 (1.4) | 0.01 |
| TSAT (%) | 31.2 (14.1) | 31.4 (14.8) | NS |
| Ferritin (µg/L) | 649 (546) | 573 (445) | <0.01 |
| Prescribed total weekly ESA dose (corrected) (U) | 4508 (5092) | 4156 (5164) | NS |
| Albumin (g/L) | 40.9 (26.8) | 40.6 (21.0) | NS |
| Calcium (mg/dL) | 8.9 (0.8) | 8.8 (0.7) | NS |
| Phosphorus (mg/dL) | 4.4 (1.3) | 4.3 (1.4) | NS |
| iPTH (pg/mL) | 576 (572) | 553 (499) | NS |
| Mean arterial pressure predialysis (mmHg) | 90 (21) | 90 (14) | NS |
| IDBWG, percentage of BW | 2.2 (1.3) | 2.4 (1.9) | NS |
| Charlson comorbidity index | 6.9 (3.0) | 7.0 (3.0) | NS |
| Diabetes mellitus (%) | 25.5 | 29.4 | NS |
Dialysis adequacy
Age, dialysis vintage, treatment time, body mass index (BMI), Charlson comorbidity index, the proportion of patients with diabetes mellitus and blood pressure control were similar in women and men. Body weight (BW) was significantly lower in women (P < 0.001) and the prescribed dialysis blood flow rate (Qb) lower (P < 0.001), but the treated blood volume per kilogram per session was significantly higher (P < 0.01), resulting in significantly higher spKt/V (P < 0.001) and urea reduction ratio (URR; P < 0.001) in women than in men (Table 1). The proportion of patients with spKt/V >1.2 was higher in women (P < 0.001; Table 2) but more men than women had treatment time >12 h/week (P < 0.05). Mean interdialytic BW gain (IDBWG) and mean arterial blood pressure were similar, with satisfactory control in both women and men (Table 1).
Table 2.
Achievement of KDIGO treatment targets by gender
| Treatment targets | Women (%) | Men (%) | P-value* |
|---|---|---|---|
| spKt/V >1.2 | 98.5 | 95.6 | <0.01 |
| URR ≥70% | 91.2 | 90.5 | NS |
| Treatment time ≥12 h/week | 92.2 | 95.0 | <0.05 |
| Prescribed Qb ≥300 mL/min | 93.0 | 94.8 | NS |
| Treated blood volume ≥1 L/kg BW | 90.5 | 89.6 | NS |
| Hb 10–12 g/dL | 70.2 | 65.2 | NS |
| Hb >12 g/dL | 11.9 | 17.7 | <0.01 |
| Ferritin ≥200 µg/L | 86.1 | 83.2 | NS |
| Ferritin ≥800 µg/L | 26.2 | 22.4 | NS |
| TSAT ≥20% | 81.2 | 81.7 | NS |
| TSAT ≥50% | 10.2 | 8.9 | NS |
| Treatment with ESA | 81.1 | 73.0 | 0.001 |
| Phosphorus ≤5.5 mg/dL | 80.3 | 83.2 | NS |
| Calcium ≤10.2 mg/dL | 97.5 | 98.6 | NS |
| PTH 150–600 pg/mL | 51.9 | 55.4 | NS |
| CVC (%) | 18.1 | 15.3 | NS |
| AV fistula (%) | 73.0 | 79.7 | <0.01 |
| S-Albumin ≥35 g/l | 87.4 | 91.5 | <0.05 |
| Charlson comorbidity index | NS | ||
| <7 | 44.4 | 44.6 | |
| 7–12 | 52.0 | 51.8 | |
| >12 | 3.6 | 3.6 |
Chi square analysis.
Renal anaemia
Haemoglobin (Hb) was significantly higher in men than in women (P = 0.01; Table 1). Men had higher ferritin (P < 0.01), but similar transferrin saturation (TSAT) and erythropoiesis-stimulating agent (ESA) doses compared to (or than) women. However, the proportion of patients with Hb 10–12 g/dL was similar in women and men, while more men had Hb >12 g/dL (P < 0.01). There were no gender differences in the proportion of patients with ferritin ≥200 or ≥800 µg/L and TSAT ≥20 or ≥50% (Table 2).
CKD–MBD
There were no significant differences in calcium, phosphorus or iPTH between women and men (Table 1) and no gender differences in the achievement of corresponding KDIGO targets (Table 2). Mean serum albumin was similar (>40 g/L), indicating adequate nutritional status, but the proportion of patients with a serum albumin ≥35 g/L was higher in men (P < 0.05; Table 2).
Vascular access
The majority of women (73%) and men (80%) had an AV fistula for haemodialysis—significantly higher in men (P < 0.01; Table 2). Eighteen and fifteen per cent of all women and men, respectively, had a CVC (not significant, NS). Mean prescribed Qb was slightly, but significantly, higher in men compared with women (379 versus 370 mL/min, P = 0.001), but the proportion of women and men with prescribed Qb ≥300 mL/min was similar (Table 2).
Results in relation to gender and age
Dialysis adequacy
Dialysis vintage, treatment time, BMI, IDBWG and blood pressure control were similar in women and men in all age groups (Table 3). Charlson comorbidity index was significantly higher in women in the youngest age group (P < 0.05). BW was significantly lower in women in three of four age groups (Table 3), and the prescribed Qb was lower in women in the youngest age group (P = 0.01). spKt/V was significantly higher in women in three of four age groups, but the proportion of patients with spKt/V >1.2 was high and similar in women and men (Table 3).
Table 3.
Patient characteristics by age and gender
| Patient characteristics | <60 years |
60–69 years |
70–79 years |
>79 years |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women | Men | P-value | Women | Men | P-value | Women | Men | P-value | Women | Men | P-value | |
| Age, mean ± SD (years) | 49.6 ± 8.9 | 48.2 ± 9.7 | NS | 65.7 ± 2.9 | 65.7 ± 3.0 | NS | 75.5 ± 2.6 | 75.3 ± 2.5 | NS | 84.1 ± 3.7 | 84.4 ± 3.6 | NS |
| Vintage, mean ± SD (months) | 69.7 ± 68.4 | 65.5 ± 71.7 | NS | 61.9 ± 60.0 | 60.9 ± 66.6 | NS | 51.8 ± 44.8 | 55.8 ± 43.6 | NS | 61.1 ± 43.6 | 58.5 ± 56.2 | NS |
| BW, mean ± SD (kg) | 67.6 ± 17.2 | 73.8 ± 17.5 | 0.001 | 71.4 ± 16.7 | 74.1 ± 15.4 | NS | 68.6 ± 14.6 | 72.9 ± 13.5 | <0.01 | 63.1 ± 10.9 | 67.3 ± 11.7 | <0.01 |
| BMI, mean ± SD (kg/m2) | 25.3 ± 5.9 | 25.6 ± 5.6 | NS | 27.1 ± 5.9 | 26.3 ± 5.2 | NS | 26.5 ± 5.1 | 26.2 ± 4.7 | NS | 25.1 ± 4.5 | 24.7 ± 4.1 | NS |
| Kt/V, mean ± SD | 1.9 ± 0.42 | 1.7 ± 0.37 | <0.001 | 1.9 ± 0.39 | 1.7 ± 0.29 | <0.01 | 1.9 ± 0.44 | 1.8 ± 0.32 | NS | 2.0 ± 0.46 | 1.8 ± 0.29 | <0.001 |
| Kt/V > 1.2 (%) | 96 | 96 | NS | 98 | 98 | NS | 98 | 98 | NS | 98 | 97 | NS |
| Treatment time, mean ± SD (min) | 738 ± 63 | 737 ± 52 | NS | 737 ± 65 | 732 ± 70 | NS | 723 ± 49 | 728 ± 44 | NS | 719 ± 55 | 715 ± 47 | NS |
| Prescribed Qb, mean ± SD (mL/min) | 373 ± 48 | 384 ± 56 | 0.01 | 371 ± 46 | 384 ± 49 | NS | 370 ± 50 | 377 ± 46 | NS | 366 ± 39 | 370 ± 44 | NS |
| Treated blood volume, mean ± SD (L/kg) | 1.4 ± 0.4 | 1.3 ± 0.3 | NS | 1.3 ± 0.3 | 1.3 ± 0.3 | NS | 1.3 ± 0.4 | 1.3 ± 0.3 | NS | 1.4 ± 0.3 | 1.4 ± 0.3 | NS |
| Hb, mean ± SD (g/dL) | 10.9 ± 1.2 | 11.1 ± 1.4 | NS | 10.9 ± 1.1 | 11.2 ± 1.4 | NS | 11.0 ± 1.0 | 11.0 ± 1.4 | NS | 10.7 ± 1.2 | 10.9 ± 1.3 | NS |
| Hb 10–12 g/dL (%) | 65 | 64 | NS | 72 | 65 | NS | 76 | 64 | <0.05 | 69 | 69 | NS |
| TSAT, mean ± SD (%) | 31.6 ± 14.1 | 31.4 ± 15.3 | NS | 31.6 ± 14.6 | 31.2 ± 14.2 | NS | 30.1 ± 13.2 | 32.3 ± 16.0 | NS | 31.5 ± 14.5 | 30.6 ± 13.1 | NS |
| Ferritin, mean ± SD (µg/L) | 553 ± 439 | 514 ± 418 | NS | 653 ± 503 | 547 ± 401 | NS | 701 ± 683 | 598 ± 465 | NS | 698 ± 532 | 645 ± 487 | NS |
| Corrected weekly ESA, mean ± SD (U) | 4793 ± 5688 | 4229 ± 5740 | NS | 4224 ± 4714 | 4054 ± 4865 | NS | 4752 ± 5541 | 4029 ± 4943 | NS | 4244 ± 4283 | 4338 ± 5043 | NS |
| Albumin, mean ± SD (g/L) | 45.5 ± 4.3 | 44.4 ± 3.9 | NS | 41.3 ± 2.9 | 39.7 ± 4.2 | NS | 38.4 ± 3.9 | 39.5 ± 3.8 | <0.05 | 37.8 ± 5.0 | 38.3 ± 4.5 | NS |
| Calcium, mean ± SD (mg/dL) | 8.9 ± 0.8 | 8.8 ± 0.7 | NS | 8.8 ± 0.7 | 8.8 ± 0.7 | NS | 8.8 ± 0.7 | 8.8 ± 0.6 | NS | 8.9 ± 0.9 | 8.8 ± 0.7 | NS |
| Phosphorus, mean ± SD (mg/dL) | 4.8 ± 1.3 | 5.1 ± 1.5 | NS | 4.6 ± 1.3 | 4.4 ± 1.3 | NS | 4.3 ± 1.3 | 4.0 ± 1.2 | NS | 3.8 ± 1.2 | 3.8 ± 1.2 | NS |
| Phosphorus <5.5 mg/dL (%) | 70 | 68 | NS | 74 | 80 | NS | 85 | 93 | <0.05 | 93 | 93 | NS |
| iPTH, mean ± SD (pg/mL) | 648 ± 637 | 705 ± 531 | NS | 652 ± 708 | 548 ± 593 | NS | 501 ± 387 | 479 ± 392 | NS | 495 ± 480 | 464 ± 419 | NS |
| PTH 150–600 pg/mL (%) | 47 | 42 | NS | 50 | 62 | <0.05 | 54 | 57 | NS | 57 | 62 | NS |
| Pre-dialysis MAP, mean ± SD (mmHg) | 94 ± 15 | 97 ± 14 | NS | 93 ± 14 | 91 ± 13 | NS | 89 ± 12 | 88 ± 12 | NS | 83 ± 12 | 83 ± 12 | NS |
| IDBWG, percentage of BW, mean ± SD | 2.6 ± 1.4 | 2.7 ± 1.4 | NS | 2.3 ± 1.3 | 2.4 ± 1.4 | NS | 2.0 ± 1.2 | 2.1 ± 1.1 | NS | 2.0 ± 1.3 | 2.3 ± 3.3 | NS |
| Charlson comorbidity index, mean ± SD | 7.3 ± 3.1 | 6.6 ± 3.2 | 0.05 | 6.4 ± 2.8 | 7.0 ± 2.9 | NS | 6.9 ± 3.1 | 7.3 ± 2.9 | NS | 7.0 ± 2.9 | 7.3 ± 3.0 | NS |
| CVC (%) | 10 | 9 | NS | 19 | 11 | NS | 16 | 18 | NS | 28 | 24 | NS |
| AV fistula (%) | 78 | 83 | NS | 73 | 85 | <0.01 | 79 | 76 | NS | 61 | 73 | <0.05 |
Renal anaemia
Hb was similar in women and men in all age groups, with mean values in all instances within KDIGO guidelines. The proportion of patients with Hb between 10–12 g/dL and ≥12 g/dL was similar in women and men in all age groups.
CKD–MBD
Calcium, phosphorus and iPTH were similar in women and men in all age groups, but the proportion of patients within KDIGO target for phosphorus (<5.5 mg/dL) and iPTH (150–600 pg/mL) was significantly lower in women 70–79 years and 60–69 years old, respectively (Table 3).
Vascular access in relation to gender and age
The use of CVCs was low in younger patients: 10 and 9% in women and men, respectively (NS), but higher among women and men >79 years old: 28 and 24%, respectively (NS; Table 3). In contrast, the percentage of patients with an AV fistula was significantly lower in women between 60–69 years and >79 years (P < 0.01 and P < 0.05, respectively).
Results in relation to gender in elderly patients (>80 years old)
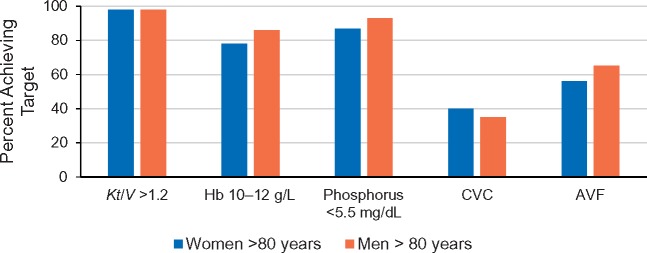
We also examined attainment of treatment goals in relation to gender in patients aged >80 years since there is a lack of information in the literature on this. Table 4 shows comparisons between female and male patients aged <80 and >80 years. There were no gender-specific differences in terms of dialysis adequacy between women and men in either age group, with the exception that a higher percentage of women ≥80 years had a treatment time >12 h/week (Table 4). Parameters related to the management and control of renal anaemia were similar in women and men ≥80 years old; findings were similar for indices of CKD–MBD and vascular access use. There were no significant differences in achievement of KDIGO treatment targets between women and men aged >80 years (Figure 1).
Table 4.
Achievement of KDIGO targets in women and men younger and older than 80 years
| Treatment targets | <80 years |
>80 years |
||||
|---|---|---|---|---|---|---|
| Women (%) | Men (%) | P-value | Women (%) | Men (%) | P-value | |
| spKt/V >1.2 | 96 | 94 | NS | 98 | 98 | NS |
| URR ≥70% | 85 | 82 | NS | 85 | 93 | NS |
| Treatment time ≥12 h/week | 95 | 95 | NS | 96 | 82 | <0.05 |
| Prescribed Qb ≥300 mL/min | 91 | 88 | NS | 90 | 88 | NS |
| Treated blood volume ≥1 L/kg BW | 81 | 78 | NS | 90 | 92 | NS |
| Hb 10–12 g/dL | 69 | 63 | NS | 78 | 86 | NS |
| Hb > 12g/dL | 13 | 19 | <0.05 | 9 | 13 | NS |
| Ferritin ≥200 µg/L | 84 | 85 | NS | 92 | 93 | NS |
| Ferritin ≥800 µg/L | 25 | 22 | NS | 30 | 26 | NS |
| TSAT ≥20% | 87 | 89 | NS | 92 | 93 | NS |
| TSAT ≥50% | 10 | 9 | NS | 11 | 9 | NS |
| Treatment with ESA | 80 | 71 | <0.01 | 84 | 79 | NS |
| Phosphorus ≤5.5 mg/dL | 69 | 70 | NS | 87 | 93 | NS |
| Calcium ≤10.2 mg/dL | 97 | 99 | NS | 98 | 98 | NS |
| PTH 150–600 pg/mL | 56 | 51 | NS | 70 | 65 | NS |
| CVC (%) | 17 | 12 | NS | 40 | 35 | NS |
| AV fistula (%) | 79 | 82 | NS | 56 | 65 | NS |
| S-Albumin ≥35 g/L | 88 | 94 | <0.01 | 71 | 69 | NS |
| Charlson comorbidity index | NS | NS | ||||
| <7 | 56 | 53 | 10 | 15 | ||
| 7–12 | 42 | 45 | 83 | 76 | ||
| >12 | 2 | 2 | 8 | 9 | ||
FIGURE 1.
Achievement of KDIGO treatment targets (%) in women and men >80 years of age. Percentage of patients achieving the indicated KDIGO target is shown for women (blue) and men (orange) aged >80 years. None of the comparisons between women and men were statistically significant. AVF, AV fistula.
DISCUSSION
In this large multicentre descriptive and representative analysis, including all prevalent patients in all DaVita clinics in Poland and Portugal, we show that women are prescribed similar haemodialysis treatment to men, and that those women also achieve international treatment targets to the same extent as men. As World Kidney Day and International Women’s Day coincided in 2018, it is important to highlight and analyse potential gender differences in treatment prescription in haemodialysis. Several previous observational studies have revealed significant differences in care and many argue to minimize barriers for women to receive adequate haemodialysis and to improve practices in areas in which outcomes differ by sex [3–8, 14, 15].
Measured as Kt/V and URR, all women and women in most age groups in the present study had a slightly, but significantly, higher urea removal than corresponding men, and the percentage of women with spKt/V > 1.2 was significantly higher. Previous studies have shown that a high dialysis dose is associated with lower mortality among women, but not among men [16]. It has, however, been proposed that the Kt/V formula may overestimate dialysis clearance in women because of a sex-specific difference in urea distribution volume (V) [17]. When V is replaced by body surface area, the recalculated formula showed that gender differences were largely attenuated [18]. Other studies have shown that women are more often prescribed shorter treatment sessions than men [6, 19] even though studies have demonstrated a survival benefit in women with increased dialysis time [20]. Women treated at the DaVita units in the present study were prescribed equally long dialysis sessions as men, irrespective of age group.
Renal anaemia is a cornerstone in management of dialysis patients. In the present study, women on haemodialysis had slightly, but significantly, lower Hb, despite similar TSAT and higher ferritin concentration than men. There were, however, no significant gender differences in the achievement of Hb in the target range of 10–12 g/dL. It is well established that healthy women have lower Hb levels than men, and consequently the definition of anaemia in the general population is sex-specific [21]. It is, therefore, noteworthy that dialysis treatment guidelines do not consider different sex-specific targets for renal anaemia, despite Hb levels remaining lower among women throughout all stages of CKD [22, 23]. Accordingly, several studies have reported that women require more ESAs to achieve similar haematocrits as men [24, 25]. Sex also modulates the response to ESAs, and women may be more likely than men to be poor responders to ESAs [25, 26]. In the current study, no differences in weekly ESA doses were observed between women and men of all ages. Since higher ESA doses have been associated with worse outcomes [27, 28], a gender perspective may be important from both a physiological and an economic perspective.
Prevention and treatment of CKD–MBD are important to retard the development and progression of vascular calcifications in patients on dialysis. Most international clinical guidelines apply the same target values to both men and women even though studies suggest sex differences in the influence of phosphorus on calcification [7, 29]. Community-based studies and studies in patients with kidney disease have shown higher phosphate levels in women compared with men [30–32]. Increased serum phosphate levels in men seem to be more associated with all-cause mortality than in women [32]. Studies from the Dialysis Outcomes and Practice Patterns Study (DOPPS) have shown significantly higher iPTH in women than men [6]. In contrast, there were no significant differences in levels of phosphorus, calcium or iPTH between men and women treated at the DaVita centres in the present study.
AV fistulas are considered the first choice of vascular access for patients on haemodialysis. In the present study, significantly fewer women had an AV fistula than men, a finding that was consistent and significant in two of four age groups. There were no significant differences between sexes in the use of a CVC. In both Europe and in the USA, most patients initiate haemodialysis using a CVC, and the use is more common in women than men [33]. It has also been reported that women are less likely to receive AV fistulas [3, 34] and that the presence of a CVC for vascular access is associated with a higher risk of mortality in women, which may be linked to a higher risk of access-related bacteraemia [35]. The presumably smaller and thinner vessels in women may prevent surgeons and nephrologists from placing an AV fistula in some cases. However, duplex ultrasonography studies of vessel diameters do not differ between the sexes [36]. Factors such as lack of surgical training and women opting more often for catheters over AV fistulas, owing to cosmetic reasons, have been proposed as explanations for physicians’ preferences regarding vascular access in women [36, 37]. Furthermore, despite demonstration of similar AV fistula failure rates in both sexes [38], a recent analysis reported that women still receive AV fistulas less often than men [34].
Taken together, these findings in renal anaemia, CKD–MBD and vascular access in ‘real world’ clinical practice indicate that the haemodialysis practices and the treatment targets for women and men are similar in these European DaVita haemodialysis clinics.
There are few previous descriptive studies in the literature focusing on gender-specific differences in practices, patient and treatment characteristics, and biochemical results also focusing on differences within and between age groups.
Demographic data from DOPPS have shown that patient age and time on haemodialysis differed slightly between sexes, with women on average being >1.2 years and having 0.3 years longer time on dialysis than men [6]. In the DOPPS analysis, women also had higher BMI and accordingly were more frequently obese than men. This was not observed in our cohort.
In addition, we analysed the achievement of KDIGO guideline targets and practices in elderly patients (≥80 years) in relation to gender. In both the USA and European countries, there has been a rapid rise in elderly patients aged ≥65 years, initiating haemodialysis treatment, compared with patients between 18 and 65 years old [9]. The nephrology community has become increasingly aware of the special considerations for the care of the elderly with CKD and the challenges surrounding decision-making regarding renal replacement therapy. Most elderly haemodialysis patients experience a reasonable life expectancy on dialysis, but a significant majority does not. In addition to older age, several negative prognostic factors have been identified in observational studies. The elderly >80 years have a high prevalence of comorbid conditions, including dementia and disability, sometimes leading to controversy about the appropriateness of dialysis initiation in these patients [39]. Furthermore, most elderly patients will have too many comorbidities to be eligible for transplantation or will develop complications making them ineligible while waiting for a kidney [40]. The impact of adequacy of haemodialysis on quality of life and the well-being of the individual patient is therefore particularly important. In the present study, there were no significant differences in practices or alignment with guideline targets between women and men ≥80 years.
Given a high burden of vascular disease in the elderly, vascular access can often be difficult to achieve with resultant dependence on a CVC and its associated risk for thrombosis and infections. Elderly patients can still benefit from the survival advantages of an AV fistula compared with a CVC [41]. In the present analysis, the use of an AV fistula was relatively high in patients ≥80 years, with no differences between sexes.
The knowledge base on gender differences in the treatment of patients with haemodialysis has grown over the past years, but efforts and studies must continue to explore the existence of systematic underlying mechanisms of gender differences in dialysis practices.
ACKNOWLEDGEMENTS
The authors acknowledge the editorial assistance of Dena E. Cohen, PhD, an employee of DaVita Clinical Research (Minneapolis, MN, USA) during manuscript preparation.
CONFLICT OF INTEREST STATEMENT
Part of these results was presented in abstract form at the American Society for Nephrology Kidney Week, San Diego, CA, 23–28 October 2018. Other than this, the results have not been previously published in whole or in part. W.K. has received speaker fees from Boehringer Ingelheim, Hexal, Profil Deutschland, IAD, Sanofi Aventis, Astra Zeneca, Amgen and Abbvie. All other authors have no competing interests to declare.
REFERENCES
- 1. Obrador GT, Arora P, Kausz AT. et al. Level of renal function at the initiation of dialysis in the U.S. end-stage renal disease population. Kidney Int 1999; 56: 2227–2235 [DOI] [PubMed] [Google Scholar]
- 2. USRDS annual data report: epidemiology of kidney disease in the United States Vol. 1: CKD in the United States, USRDS, 2016, pp. 1–216
- 3. Miller CD, Robbin ML, Allon M.. Gender differences in outcomes of arteriovenous fistulas in hemodialysis patients. Kidney Int 2003; 63: 346–352 [DOI] [PubMed] [Google Scholar]
- 4. Adams SV, Rivara M, Streja E. et al. Sex differences in hospitalizations with maintenance hemodialysis. J Am Soc Nephrol 2017; 28: 2721–2728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carrero JJ, de Jager DJ, Verduijn M. et al. Cardiovascular and noncardiovascular mortality among men and women starting dialysis. Clin J Am Soc Nephrol 2011; 6: 1722–1730 [DOI] [PubMed] [Google Scholar]
- 6. Hecking M, Bieber BA, Ethier J. et al. Sex-specific differences in hemodialysis prevalence and practices and the male-to-female mortality rate: the Dialysis Outcomes and Practice Patterns Study (DOPPS). PLoS Med 2014; 11: e1001750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ho LT, Sprague SM.. Women and CKD-mineral and bone disorder. Adv Chronic Kidney Dis 2013; 20: 423–426 [DOI] [PubMed] [Google Scholar]
- 8. Hsu CY, Bates DW, Kuperman GJ. et al. Relationship between hematocrit and renal function in men and women. Kidney Int 2001; 59: 725–731 [DOI] [PubMed] [Google Scholar]
- 9. Jager KJ, van Dijk PC, Dekker FW. et al. The epidemic of aging in renal replacement therapy: an update on elderly patients and their outcomes. Clin Nephrol 2003; 60: 352–360 [DOI] [PubMed] [Google Scholar]
- 10. Kurella M, Covinsky KE, Collins AJ. et al. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 2007; 146: 177–183 [DOI] [PubMed] [Google Scholar]
- 11. Canaud B, Tong L, Tentori F. et al. Clinical practices and outcomes in elderly hemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Clin J Am Soc Nephrol 2011; 6: 1651–1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chauveau P, Combe C, Laville M. et al. Factors influencing survival in hemodialysis patients aged older than 75 years: 2.5-year outcome study. Am J Kidney Dis 2001; 37: 997–1003 [DOI] [PubMed] [Google Scholar]
- 13. Lee T, Thamer M, Zhang Q. et al. Vascular access type and clinical outcomes among elderly patients on hemodialysis. Clin J Am Soc Nephrol 2017; 12: 1823–1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carrero JJ, Hecking M, Chesnaye NC. et al. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat Rev Nephrol 2018; 14: 151–164 [DOI] [PubMed] [Google Scholar]
- 15. Sehgal AR. Impact of quality improvement efforts on race and sex disparities in hemodialysis. JAMA 2003; 289: 996–1000 [DOI] [PubMed] [Google Scholar]
- 16. Port FK, Wolfe RA, Hulbert-Shearon TE. et al. High dialysis dose is associated with lower mortality among women but not among men. Am J Kidney Dis 2004; 43: 1014–1023 [DOI] [PubMed] [Google Scholar]
- 17. Spalding EM, Chandna SM, Davenport A. et al. Kt/V underestimates the hemodialysis dose in women and small men. Kidney Int 2008; 74: 348–355 [DOI] [PubMed] [Google Scholar]
- 18. Daugirdas JT, Greene T, Chertow GM. et al. Can rescaling dose of dialysis to body surface area in the HEMO study explain the different responses to dose in women versus men? Clin J Am Soc Nephrol 2010; 5: 1628–1636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Couchoud C, Kooman J, Finne P. et al. From registry data collection to international comparisons: examples of haemodialysis duration and frequency. Nephrol Dial Transplant 2009; 24: 217–224 [DOI] [PubMed] [Google Scholar]
- 20. Miller JE, Kovesdy CP, Nissenson AR. et al. Association of hemodialysis treatment time and dose with mortality and the role of race and sex. Am J Kidney Dis 2010; 55: 100–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ferrucci L, Maggio M, Bandinelli S. et al. Low testosterone levels and the risk of anemia in older men and women. Arch Intern Med 2006; 166: 1380–1388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ifudu O. Patient characteristics determining rHuEPO dose requirements. Nephrol Dial Transplant 2002; 17 (Suppl 5): 38–41 [DOI] [PubMed] [Google Scholar]
- 23. Locatelli F, Nissenson AR, Barrett BJ. et al. Clinical practice guidelines for anemia in chronic kidney disease: problems and solutions. A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 2008; 74: 1237–1240 [DOI] [PubMed] [Google Scholar]
- 24. Frankenfield DL, Rocco MV, Frederick PR. et al. Racial/ethnic analysis of selected intermediate outcomes for hemodialysis patients: results from the 1997 ESRD Core Indicators Project. Am J Kidney Dis 1999; 34: 721–730 [DOI] [PubMed] [Google Scholar]
- 25. Madore F, Lowrie EG, Brugnara C. et al. Anemia in hemodialysis patients: variables affecting this outcome predictor. J Am Soc Nephrol 1997; 8: 1921–1929 [DOI] [PubMed] [Google Scholar]
- 26. Ifudu O, Uribarri J, Rajwani I. et al. Gender modulates responsiveness to recombinant erythropoietin. Am J Kidney Dis 2001; 38: 518–522 [DOI] [PubMed] [Google Scholar]
- 27. Bae MN, Kim SH, Kim YO. et al. Association of erythropoietin-stimulating agent responsiveness with mortality in hemodialysis and peritoneal dialysis patients. PLoS One 2015; 10: e0143348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Suttorp MM, Hoekstra T, Rotmans JI. et al. Erythropoiesis-stimulating agent resistance and mortality in hemodialysis and peritoneal dialysis patients. BMC Nephrol 2013; 14: 200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Onufrak SJ, Bellasi A, Shaw LJ. et al. Phosphorus levels are associated with subclinical atherosclerosis in the general population. Atherosclerosis 2008; 199: 424–431 [DOI] [PubMed] [Google Scholar]
- 30. Martin M, Valls J, Betriu A. et al. Association of serum phosphorus with subclinical atherosclerosis in chronic kidney disease. Sex makes a difference. Atherosclerosis 2015; 241: 264–270 [DOI] [PubMed] [Google Scholar]
- 31. Onufrak SJ, Bellasi A, Cardarelli F. et al. Investigation of gender heterogeneity in the associations of serum phosphorus with incident coronary artery disease and all-cause mortality. Am J Epidemiol 2009; 169: 67–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yoo KD, Kang S, Choi Y. et al. Sex, age, and the association of serum phosphorus with all-cause mortality in adults with normal kidney function. Am J Kidney Dis 2016; 67: 79–88 [DOI] [PubMed] [Google Scholar]
- 33. Noordzij M, Jager KJ, van der Veer SN. et al. Use of vascular access for haemodialysis in Europe: a report from the ERA-EDTA Registry. Nephrol Dial Transplant 2014; 209: 1956–1964 [DOI] [PubMed] [Google Scholar]
- 34. Shah S, Leonard AC, Meganathan K. et al. Gender and racial disparities in initial hemodialysis access and outcomes in incident end-stage renal disease patients. Am J Nephrol 2018; 48: 4–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tokars JI, Light P, Anderson J. et al. A prospective study of vascular access infections at seven outpatient hemodialysis centers. Am J Kidney Dis 2001; 37: 1232–1240 [DOI] [PubMed] [Google Scholar]
- 36. Caplin N, Sedlacek M, Teodorescu V. et al. Venous access: women are equal. Am J Kidney Dis 2003; 41: 429–432 [DOI] [PubMed] [Google Scholar]
- 37. Shenoy S. Surgical anatomy of upper arm: what is needed for AVF planning. J Vasc Access 2009; 10: 223–232 [DOI] [PubMed] [Google Scholar]
- 38. Saran R, Elder SJ, Goodkin DA. et al. Enhanced training in vascular access creation predicts arteriovenous fistula placement and patency in hemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study. Ann Surg 2008; 247: 885–891 [DOI] [PubMed] [Google Scholar]
- 39. Joly D, Anglicheau D, Alberti C. et al. Octogenarians reaching end-stage renal disease: cohort study of decision-making and clinical outcomes. J Am Soc Nephrol 2003; 14: 1012–1021 [DOI] [PubMed] [Google Scholar]
- 40. Schaeffner ES, Rose C, Gill JS.. Access to kidney transplantation among the elderly in the United States: a glass half full, not half empty. Clin J Am Soc Nephrol 2010; 5: 2109–2114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pisoni RL, Arrington CJ, Albert JM. et al. Facility hemodialysis vascular access use and mortality in countries participating in DOPPS: an instrumental variable analysis. Am J Kidney Dis 2009; 53: 475–491 [DOI] [PubMed] [Google Scholar]