Abstract
Background
Most individuals with knee or hip osteoarthritis do not meet recommendations for physical activity. The Social Cognitive Theory suggests that the social environment (e.g., spouses/partners) may influence the physical activity of individuals with osteoarthritis. The purpose of this study was to examine whether the physical activity of insufficiently active, coupled adults with osteoarthritis was associated with received partner support for physical activity, partner’s engagement in physical activity, and relationship satisfaction.
Methods
Cross-sectional data from 169 couples were collected. Accelerometers estimated moderate-to-vigorous physical activity and daily steps for participants with osteoarthritis and their partners. Participants with osteoarthritis reported total received partner support for physical activity and relationship satisfaction.
Results
Participants with osteoarthritis were on average 65 years old, 65% female, 86% non-Hispanic white, and 47% retired. Receiving total partner support more frequently was associated with more minutes of moderate-to-vigorous physical activity but not with steps. Relationship satisfaction moderated the association of partner’s physical activity on the daily steps of individuals with osteoarthritis such that having a partner who accomplished more daily steps was associated with participants with osteoarthritis accomplishing more daily steps themselves when they reported greater relationship satisfaction.
Conclusions
Partners and relationship satisfaction may play an important role in the physical activity of individuals with osteoarthritis. Interventions seeking to increase physical activity in this population may be enhanced by promoting partner support. Additional research is needed to further explain these associations within the context of relationship satisfaction.
Keywords: Exercise, Osteoarthritis, Spouses, Social support
Introduction
Approximately one in four adults in the United States has osteoarthritis [1]. The progression of osteoarthritis symptoms (e.g., pain, stiffness) often results in limited physical function [2]. Because osteoarthritis symptoms are improved with physical activity, most established medical guidelines for osteoarthritis recommend physical activity as a non-pharmacologic method of self-management [3]. Current physical activity guidelines recommend that adults with chronic conditions such as osteoarthritis engage in as much and as intense activity as their condition allows [4]. Achieving more than 45 min of moderate-to-vigorous physical activity per week [5] or at least 6,000 steps per day [6] has been associated with better osteoarthritis-related function. Yet, many individuals with osteoarthritis do not meet these modest guidelines [7, 8]. Clarifying the factors that relate to moderate-to-vigorous physical activity and steps among adults with osteoarthritis may help researchers increase the effectiveness of physical activity interventions for this population.
The Social Cognitive Theory posits that health behaviors (e.g., physical activity), the environment (e.g., family, spouse), and an individual’s characteristics (e.g., self-efficacy) influence each other simultaneously [9]. The majority of literature examining the determinants of physical activity among adults with osteoarthritis has demonstrated the importance of individual characteristics (e.g., self-efficacy for physical activity [10, 11], barriers to physical activity [10, 12]). However, living with osteoarthritis not only affects individuals, but also their cohabitating partners (e.g., spouses), altering individual roles and responsibilities within the couple. In return, partners can affect individuals with osteoarthritis and their health behaviors. Nevertheless, evidence of the role of the social environment on the physical activity of individuals with osteoarthritis is lacking [13].
According to the Social Cognitive Theory, the social environment consists of external factors (e.g., partners) that can affect an individual’s behavior [9]. One way that partners can positively affect physical activity is by providing social support by assisting and facilitating efforts to become more physically active [14], for example through encouragement [14] or by accompanying partners in their physical activity [15]. Studies show that social support can promote self-efficacy, remove barriers to physical activity, and motivate engagement in physical activity [16–19]. For example, in a daily diary study of 119 cohabitating overweigh/obese couples, participants engaged in 25 more minutes of moderate-to-vigorous physical activity on days when partners provided high versus low levels of social support [20].
Furthermore, Berli and colleagues [20] found that more moderate-to-vigorous physical activity occurred on days when couples engaged in physical activity together, one common way couples demonstrate that they support the other’s efforts to make a lifestyle change. However, this form of partner support may also influence individuals through another important process described by Social Cognitive Theory, for example, observational learning. That is, Social Cognitive Theory explains that if individuals with osteoarthritis observe their partners in the planning, preparation, and engagement of physical activity, they can develop the motivation and self-efficacy to engage in the behavior themselves (i.e., through observational/vicarious learning) [9]. Observational learning may partially account for why research consistently finds that couples tend to mirror each other’s active lifestyles [21–24]. However, when one partner has a potentially physically limiting health condition such as osteoarthritis, it remains unclear if observing the other partner engage in physical activity behaviors is sufficient to promote their own physical activity.
When considering environmental influences on individuals’ health behaviors, it is important to consider characteristics of the social relationships within which they enact these behaviors. Social support and observational learning may occur more frequently or may be more effective within higher functioning relationships. Empirical evidence exists for partner influence on health behaviors occurring only under favorable relationship contexts (e.g., in the presence of high relationship satisfaction) [25, 26]. Further support for the importance of relationship satisfaction was found in a study of 181 older adults who were less likely to hide unhealthy behaviors from individuals with whom they had higher relationship satisfaction [26]. Thus, when examining the role of partners in individuals’ health behaviors, it is also important to investigate these potential influences within the context of the relationship quality.
Although the above mentioned evidence demonstrates the importance of the social environment on physical activity, few studies have examined the role of the social environment among individuals with osteoarthritis [13]. One study that investigated some of these processes was conducted by Martire and colleagues [22] where they examined three types of partner influence (i.e., partner’s activity, autonomy support, social control) on daily physical activity among couples with osteoarthritis. The authors found that a partner’s activity and autonomy support were associated with more physical activity in the affected individual. The current study extends Martire and colleagues’ work by examining other potential associations between partners and physical activity including partner support for physical activity and relationship satisfaction.
Overview of current study
Using baseline data from cohabitating couples enrolled in a longitudinal study of physical activity-related social support processes, the role of received social support for physical activity, partner’s physical activity, and relationship satisfaction on the physical activity of individuals with osteoarthritis was examined (Fig. 1). It was hypothesized that individuals with osteoarthritis would perform more moderate-to-vigorous physical activity and steps if they received more frequent support for physical activity, had partners who engaged in more physical activity, and if they had a more satisfying relationship with their partners. To examine whether the aforementioned associations depend on the quality of the relationship, the role of received support and partner’s physical activity was evaluated across levels of relationship satisfaction. It was hypothesized that receiving more frequent support and having a partner who engaged in more physical activity would be positively associated participants’ physical activity when they reported greater relationship satisfaction.
Fig. 1.
Hypothesized relationships examined
Methods
Study design and sample
Couples (n = 173) were enrolled in the Partners in Active Living Study, a year-long longitudinal study designed to examine processes related to social support for physical activity in couples in which at least one partner had osteoarthritis. Couples attended a class on social support and received a workbook on physical activity as a minimal prompt to engage in physical activity and partner support. We then followed couples with repeated measures over one year to observe how partners provided support for physical activity. For this analysis, only baseline data were used. Individuals with osteoarthritis were recruited via the Johnston County Osteoarthritis Project [27]; emails to university students and employees; electronic medical records at the University of North Carolina at Chapel Hill; and community locations, including senior centers [28]. Couples consisted of the individual with osteoarthritis who was initially recruited and their partner. Individuals with osteoarthritis were eligible if they had a clinical diagnosis of hip and/or knee osteoarthritis or “probable” osteoarthritis (self-reported frequent joint pain, limitation of the hip or knee for at least six months, and 50 years or older) [29, 30]; were married and/or cohabitating with a partner who was willing to participate; were interested in increasing their physical activity; did not have medical conditions that precluded physical activity; and were insufficiently active (<120 min of self-reported moderate-vigorous physical activity per week). Partners were eligible if they were 21 years or older and English language proficient. The sample size for the current study was 169 couples with complete accelerometer data for both partners.
Procedures
The study was approved by the Institutional Review Board of the University of North Carolina at Chapel Hill. Eligible couples met with trained research staff to provide written informed consent. Participants were then shown how to wear accelerometers and sent home with baseline surveys that they completed independently and returned the following week.
Measures
Physical activity of participants with osteoarthritis and their partners
Physical Activity was measured using Actigraph GT3X+ accelerometers. Trained research staff distributed monitors and provided instructions for wear and return by mail. Participants were asked to wear the device during all waking hours for seven consecutive days. Monitors were worn at the waist, using either an elastic belt or clip. After monitors were returned, data were downloaded and converted to 60-s epoch files for processing. Non-wear time was identified using a combination of the Choi algorithm [31] and wear logs. Moderate and vigorous minutes were estimated using established cut-points (2020+ cpm) [32]. Steps were estimated in the Actilife software when converting raw acceleration data to minute-level counts and steps. Each day required 7+ hours of wear during waking hours to be included in analyses. Person-level outcomes were computed for each participant with at least four days with 7+ hours. For this sample, 92% of days had 10+ hours of wear and days with 7–9 h of wear had average activity levels that were similar to days with 10+ hours, after accounting for wear time. Individuals with osteoarthritis averaged 6.8 (SD = 1.5) days of wear and 13.8 (SD = 1.6) wear hours per day. Partners averaged 6.5 (SD = 1.5) days of wear and 13.9 (SD = 1.7) wear hours per day. Minutes of moderate-to-vigorous physical activity and steps were standardized to a 13.5 h day (e.g. (13.5/WEAR hours) * moderate-to-vigorous physical activity minutes)) to help account for the influence of daily wear time on physical activity estimates. Dichotomous outcomes for moderate-to-vigorous physical activity (> 45 min per week) [5] and steps (≥ 6000 per day) [6] were established based on person-level summary data.
Received partner support for physical activity
Received partner support for physical activity in the past three months was reported by individuals with osteoarthritis using the 13-item Social Support and Exercise Survey [33] and the 12-item multidimensional scale for assessing social influences on physical activity in older adults [34]. Each item referred only to the participating partner (i.e., not other family or friends) and participants were asked to indicate their responses using a 6-point Likert scale (1 = never, 6 = very often). Because we were interested in the positive support that participants receive from partners, we removed items from the two scales that refer to negative influences (e.g., “Complained about the time I spend doing physical activity”). The mean score for received partner support was calculated and used in the analyses (α = 0.95).
Relationship satisfaction
Relationship satisfaction was assessed using the Relationship Assessment Scale (RAS) [35]. The 7-item scale asks participants to indicate how they generally feel about their relationship using a response scale from 1 to 5, with higher scores indicating greater relationship satisfaction (e.g., “How good is your relationship compared to most?”). Two negatively-worded items were reverse-coded. Scores were calculated by summing responses across the 7 items so that possible scores ranged from 7 to 35 (α = 0.92).
Sociodemographic and medical characteristics
Participants with osteoarthritis self-reported their age, race/ethnicity, education level, employment status, and household annual income. Self-reported height and weight were used to calculate body mass index (BMI, kg/m2), a potential influence on physical activity. Another potential confounder, osteoarthritis symptoms, was assessed using the 24-item Western Ontario & McMaster Universities Osteoarthritis Index [36], which measures osteoarthritis-related pain, stiffness, and function on a 5-point scale ranging from 0 (none) to 4 (extreme). Higher scores indicate worse osteoarthritis symptoms (α = 0.95).
Statistical analyses
Descriptive statistics of the sample, the outcome variables (daily moderate-to-vigorous physical activity (measured continuously and dichotomously using >45 weekly daily minutes as the cutoff) and daily steps (measured continuously and dichotomously using ≥6,000 daily steps as the cutoff)) and the predictor variables (partner’s physical activity, received support for physical activity and relationship satisfaction) were obtained. Initially, bivariate correlation analyses were used to assess relationships between the outcome and predictor variables. Then, multiple regression was used to model the association of partner’s physical activity, received support, and relationship satisfaction with the physical activity of individuals with osteoarthritis. Given that continuous physical activity minutes (skewness: 1.980, kurtosis: 4.241) and steps (skewness: 0.454, kurtosis: −0.184) were count variables and ordinary linear regression may produce negative estimates (which are impossible for these outcomes), we analyzed these data using negative binomial regression [37]. Coefficients for these variables are provided as incidence rate ratios (IRR) and 95% confidence intervals, interpreted as the multiplicative increase or decrease in the expected count of the outcome with each 1 SD increase in the predictor variable [38]. Logistic regression was used to analyze the dichotomous outcomes. Odds ratios and 95% confidence intervals are provided for these results and interpreted as the multiplicative increase or decrease in the likelihood of the outcome occurring with each 1 SD increase in the predictor variable. A series of models were tested, beginning with bivariate analyses followed by models including all predictors (received support, partner’s physical activity, and relationship satisfaction). In the final model, potential confounding variables were included: individuals with osteoarthritis’ sociodemographic and medical characteristics that were related to the outcomes (p ≤ 0.20). Finally, interactions of received support and partner’s physical activity with relationship satisfaction were generated and tested in each model. Potential modifiers were mean-centered prior to modeling interaction effects. Statistically significant interactions were further examined using the simple slopes of the mean, one standard deviation below and above the mean of relationship satisfaction [39]. Given multiple tests with each outcome (three main effects and two interactions), we have adjusted the alpha to 0.01 (0.05/5). Statistical analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC).
Results
Descriptive characteristics
The descriptive characteristics of the sample are shown in Table 1. With respect to physical activity, individuals with osteoarthritis engaged in an average of 8.6 (SD = 9.8) daily minutes of moderate-to-vigorous physical activity and 42.3% accumulated >45 weekly minutes of moderate-to-vigorous physical activity. They averaged 4,339 (SD = 1,729) daily steps and 20.2% reached the cut-off of 6,000 daily steps. Partners achieved significantly more daily moderate-to-vigorous physical activity minutes (16.1, SD = 17.0) and more partners averaged >45 weekly minutes of moderate-to-vigorous physical activity (60.2%) than individuals with osteoarthritis. Similarly, partners averaged significantly more daily steps (5,344, SD = 2,559) and more partners averaged ≥6,000 daily steps (40.4%) than individuals with osteoarthritis. The frequency of received partner support for physical activity was 2.4 (1.1). Individuals with osteoarthritis reported satisfaction with their relationships, averaging 29.6 (SD = 5.2) on the relationship satisfaction scale (range of 7–35).
Table 1.
Descriptive characteristics of participants, received partner support characteristics, and relationship satisfaction (N = 169 couples)
| Participants with osteoarthritis % (n) or mean ± SD | Partners | |
|---|---|---|
| Participants’ individual characteristics | ||
| Age | 65.4 ± 8.9 | 65.9 ± 9.7 |
| Gender (female)** | 65.1 (110) | 36.1 (61) |
| Race (non-Hispanic white)** | 86.4 (146) | 88.0 (147) |
| Education (≥ 4 year degree)** | 58.6 (99) | 55.1 (92) |
| Employment** | ||
| Retired or on disability | 47.0 (77) | 46.0 (75) |
| < 32 h or unpaid work/volunteer | 23.8 (39) | 21.5 (35) |
| ≥32h | 29.3 (48) | 32.5 (53) |
| Annual household income (≥ $75,000) | 56.3 (90) | |
| BMI* | 30.0 ± 5.6 | 28.2 ± 5.7 |
| Osteoarthritis symptomsa* | 28.1 ± 13.4 | 16.8 ± 14.6 |
| Daily minutes of MVPA* | 8.6 ± 9.8 | 16.1 ± 17.0 |
| Achieves >45 weekly minutes of MVPA** | 42.3 (71) | 60.2 (100) |
| Daily steps* | 4,339 ± 1,729 | 5,344 ± 2,559 |
| Achieves ≥6,000 daily steps** | 20.2 (34) | 40.4 (67) |
| Relationship characteristics | ||
| Received support for physical activityb | 2.4 ± 1.1 | |
| Relationship satisfactionc | 29.6 ± 5.2 | |
Note: MVPA = moderate-to-vigorous physical activity
Western Ontario & McMaster Universities Osteoarthritis Index scores range from 0–96, higher scores indicate worse pain, stiffness, and functional limitations
Scores range from 1–6, higher scores indicate type of support was received more frequently
Scores range from 7–35, higher scores indicate greater relationship satisfaction
Statistically significant difference between main participant and partner (p ≤ 0.05) based on paired t-tests
Statistically significant difference between main participant and partner (p ≤ 0.05) based on chi square tests
Correlations between study variables
Correlations between the study variable are presented in Table 2. Moderate-to-vigorous physical activity (but not daily steps) of participants with osteoarthritis was modestly positively correlated with received partner support. Both moderate-to-vigorous physical activity and daily steps of participants with osteoarthritis were positively correlated with partner’s physical activity. On the other hand, relationship satisfaction was negatively correlated with the physical activity of participants with osteoarthritis.
Table 2.
Correlations between study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| l.MVPA(OA) | ─ | 0.72* | 0.73* | 0.64* | 0.20* | 0.34* | 0.34* | 0.32* | 0.28* | −0.20* |
| 2. > 45 min MVPA (OA) | ─ | 0.58* | 0.44* | 0.17* | 0.30* | 0.35* | 0.32* | 0.27* | −0.12 | |
| 3. Steps (OA) | ─ | 0.77* | 0.08 | 0.22* | 0.31* | 0.30* | 0.28* | −0.22* | ||
| 4. ≥ 6,000 steps (OA) | ─ | 0.09 | 0.18* | 0.27* | 0.25* | 0.23* | −0.16* | |||
| 5. Received partner support | ─ | 0.30* | 0.24* | 0.24* | 0.13 | 0.24* | ||||
| 6. MVPA (P) | ─ | 0.65* | 0.73* | 0.62* | −0.03 | |||||
| 7. > 45 min MVPA (P) | ─ | 0.67* | 0.57* | 0.02 | ||||||
| 8. Steps (P) | ─ | 0.84* | −0.002 | |||||||
| 9. ≥ 6,000 steps (P) | ─ | −0.06 | ||||||||
| 10. Relationship satisfaction | ─ |
Note: MVPA = moderate-to-vigorous physical activity; OA = participants with osteoarthritis; P = partners
p < 0.05
Role of received partner support, partner’s physical activity, and relationship satisfaction on the physical activity of participants with OA
Findings from the adjusted models are summarized in Table 3. Each adjusted model included received partner support for physical activity, partner’s physical activity, relationship satisfaction, and covariates: individuals with osteoarthritis’ age, education, employment, household income, BMI, and osteoarthritis symptoms. These variables were adjusted for in the final model because they were are at least marginally (p ≤ 0.20) related to the outcomes in bivariate analyses (data not shown).
Table 3.
Regression associations of received partner support for physical activity, partner physical activity, and relationship satisfaction with the physical activity outcomes of participants with osteoarthritisa
| Participant with osteoarthritis’ physical activity | ||||||||
|---|---|---|---|---|---|---|---|---|
| MVPA1 | Averaged > 45 daily MVPA minutes2 | Daily steps1 | Averaged ≥ 6,000 daily steps2 | |||||
| IRR | 95% CI | OR | 95% CI | IRR | 95% CI | OR | 95% CI | |
| Received partner support for PA | 1.333* | 1.156,1.555 | 1.666 | 0.999, 2.778 | 1.057 | 1.000, 1.116 | 1.251 | 0.728, 2.151 |
| Partner PA3 | 1.005 | 0.995, 1.015 | 2.728 | 0.881, 8.454 | 1.003 | 1.001, 1.005 | 3.471 | 1.142, 10.554 |
| Relationship satisfaction | 0.974 | 0.946, 1.002 | 0.953 | 0.855, 1.061 | 0.988 | 0.977, 0.999 | 0.931 | 0.834, 1.038 |
Note: PA = physical activity; MVPA = moderate-to-vigorous physical activity
Models include all predictors and are adjusted for main participants’ age, education, employment, household income, BMI, and WOMAC total score
Negative binomial regression
Logistic regression
Partner’s physical activity = physical activity outcome corresponding to the participant with osteoarthritis’ outcome in a given model
p ≤ 0.01
Moderate-to-vigorous physical activity
Only one effect reached the adjusted alpha for statistical significance (p ≤ 0.01). In adjusted models, more frequent received partner support was associated with more daily minutes of moderate-to-vigorous physical activity (IRR = 1.333, 95% CI = 1.156, 1.555). None of the predictors were associated with the likelihood of accumulating >45 weekly minutes of moderate-to-vigorous physical activity.
Steps
There were no main effects on steps (regardless of whether steps were measured continuously or dichotomously). However, in the model estimating daily steps, an interaction was observed between relationship satisfaction and partner’s daily steps (IRR = 1.074, 95% CI = 1.017, 1.138). As depicted in Fig. 2, having a partner who accomplished more daily steps was associated with participants with osteoarthritis accomplishing more daily steps themselves if they reported average (IRR = 1.004, 95% CI: 1.001, 1.006) or above average (IRR = 1.007, 95% CI = 1.003, 1.011) relationship satisfaction.
Fig. 2.
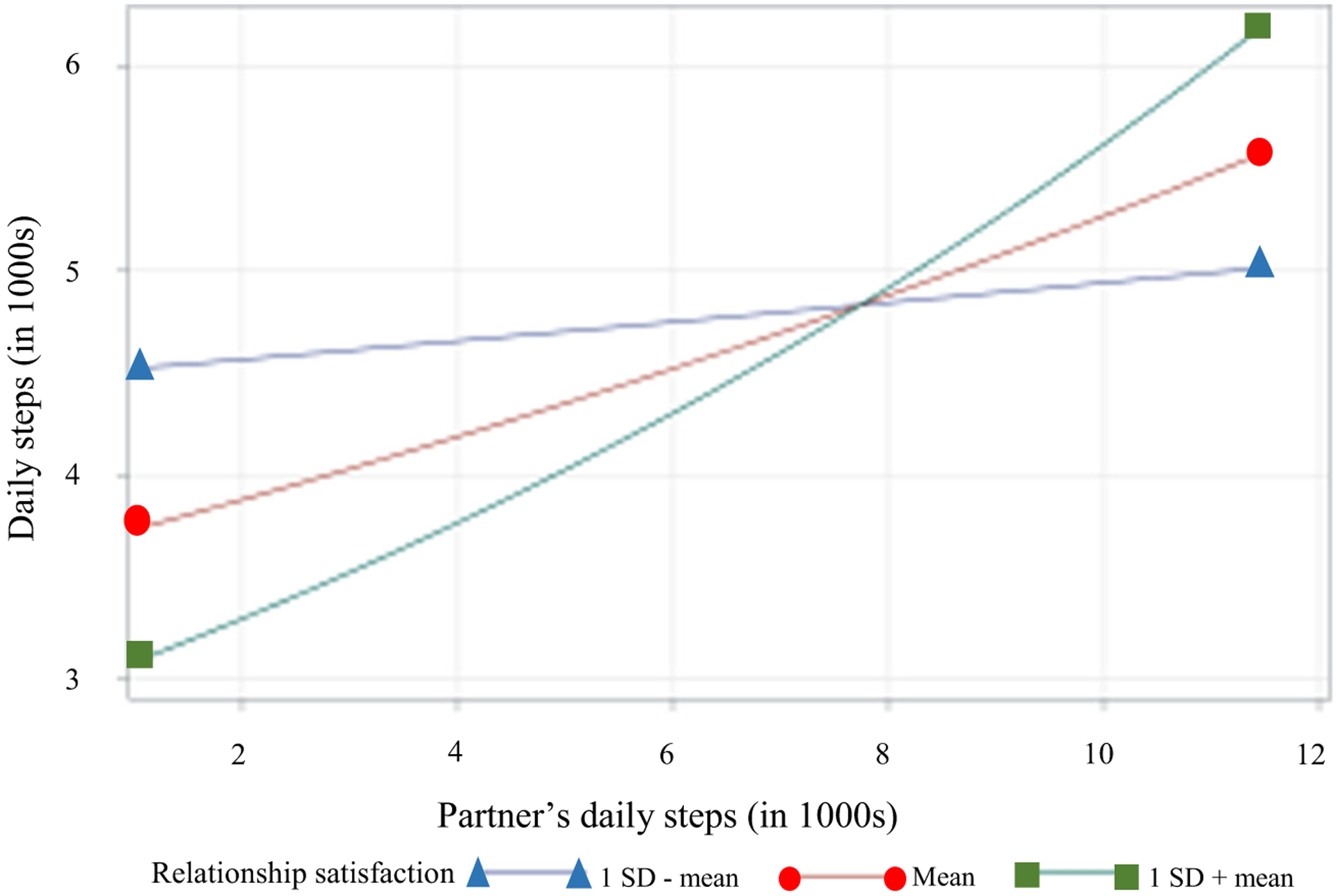
Interaction between relationship satisfaction and partner’s daily steps on participants with osteoarthritis’ daily steps. Figure shows the association between the partner’s daily steps and participant’s daily steps by relationship satisfaction at 1 SD below the mean (IRR = 1.001, 95% CI = 0.998, 1.004), the mean (IRR = 1.004, 95% CI = 1.001, 1.006), and 1 SD above the mean (IRR = 1.007, 95% CI = 1.003, 1.011). Note: PA = physical activity, SD = standard deviation
Discussion
In the current study, Social Cognitive Theory was used to examine the role of received support, partner’s engagement in physical activity, and relationship satisfaction on the moderate-to-vigorous physical activity and steps of individuals with osteoarthritis. Findings show that only received partner support for physical activity was associated with moderate-to-vigorous physical activity and no predictors were associated with steps.
Received partner support appeared to be important to moderate-to-vigorous physical activity though not important to daily steps. This may be because more intense forms of activity typically occur via planned activities, possibly making them more amenable to social support (e.g., encouragement, problem solving). A study among 903 university students supported this hypothesis by demonstrating that social support for physical activity was associated with planning for physical activity [40]. Conversely, steps, which may be accumulated with lighter forms of activity and with less advanced planning, may not require partner support. Research has largely shown positive associations between social support and physical activity [40–43]. However, given the barriers to physical activity experienced by individuals with osteoarthritis (e.g., pain and stiffness [44]), our study contributes to the literature by examining the association between social support and two types of physical activity: moderate-to-vigorous physical activity and daily steps. The current study supports and extends prior work on support for physical activity among people with osteoarthritis by suggesting moderate-to-vigorous physical activity may benefit from social support.
We observed that relationship satisfaction moderated the association of partner’s physical activity on the daily steps of individuals with osteoarthritis. Previous research has found similar associations between relationship satisfaction and physical activity. For instance, in their study of marital satisfaction and cardiovascular risk factors among 493 women, Gallo et al. [45] found that, compared to women who reported high marital satisfaction, women who reported low satisfaction engaged in less exercise. This finding was replicated in a recent daily diary study of 191 older couples, which found that higher marital satisfaction was reported on days when participants engaged in more exercise [46]. Our results highlight the value of investigating partner effects on health behaviors within the context of the relationship.
Our findings regarding the importance of relationship satisfaction suggest it may be worthwhile to study whether observational learning is an important mechanism underlying physical activity for some couples but not for others. For instance, individuals who are not satisfied with their relationship may not want to emulate their partner’s health behaviors. For these individuals, couples-level interventions may not be effective. On the other hand, within a higher quality relationship, having a partner who engages in physical activity may be sufficient to overcome personal barriers (e.g., low self-efficacy, low motivation) to engage in walking. Future studies can explore whether observational learning influences the barriers to physical activity experienced by those with osteoarthritis and how relationship quality plays a role.
This study builds evidence to support the importance of the social environment, specifically the role of partners and relationship satisfaction on physical activity. Furthermore, we focus on individuals with osteoarthritis who may experience symptoms that limit their engagement in physical activity. Other than the Social Cognitive Theory, potentially useful models, including interdependence theory and communal coping, use the context of the couples’ environment to explain health behaviors, particularly when data have been collected from both partners [47–49]. For example, with data from wives and husbands, Ayotte and colleagues used interdependence theory to show that wives’ self-efficacy was associated with husbands’ received support for physical activity and husband’s self-efficacy was associated with wives’ physical activity. As this study demonstrated, one reason why an individual’s support and physical activity may impact their partner’s physical activity is the interdependence that exists within the couple [49], a feature that becomes a key to uncovering reciprocating dynamics within dyads. An extension of interdependence theory, communal coping, is a framework for examining the extent to which partners share in the responsibility of managing a chronic condition as a couple [47]. For example, data collected from prostate cancer survivors and their spouses were used to show that support for physical activity (but not relationship satisfaction) was associated with meeting physical activity guidelines as a couple (i.e., both partners engaged in ≥150 min of moderate or 75 min of vigorous or a combination of vigorous/moderate per week) [50]. These frameworks extend beyond the Social Cognitive Theory by acknowledging the role of the social environment on behavior and incorporating dyadic effects that can be useful in identifying important influences in the context of a chronic disease. Future research may benefit from testing these models with dyadic data to develop a more comprehensive understanding of partners’ influence on each other’s physical activity.
Strengths and limitations
With the exception of Martire and colleagues’ work [22], the current study addresses an important gap in the literature by examining the role of partner and relationship satisfaction in the physical activity of individuals with osteoarthritis. This study is strengthened by the use of accelerometers to objectively measure physical activity rather than self-report. However, because cross-sectional data were used, it is impossible to evaluate the causality of the relationships observed. In this study, the focus was on baseline associations to examine naturalistic behaviors in couples who had not yet been asked to work together later in the study. However, longitudinal studies with couples are needed to confirm the directionality of the findings. Furthermore, the sample consisted of participants who were insufficiently active and were interested in becoming more active. Additional studies with other samples that examine the associations tested here will help clarify the generalizability of the findings.
Conclusion
Physical activity is imperative to achieving optimal health and quality of life, especially among individuals with osteoarthritis [51]. The current study found that partners and relationship satisfaction may play an important role in the physical activity of those with osteoarthritis. Interventions seeking to increase moderate-to-vigorous physical activity and steps among individuals with osteoarthritis would likely benefit from testing methods of participating partners’ support and physical activity. The role of relationship satisfaction with physical activity was found to be an important effect modifier, thus further investigation is required to better understand how relationship satisfaction subgroups may differ in their response to physical activity-promoting efforts. Given the dearth of evidence for how relationships may contribute to physical activity within the context of osteoarthritis [22], these findings add to the limited body of research.
Acknowledgements
This study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases under award P60AR062760 and the National Institute of Nursing Research of the National Institutes of Health under Award T32NR007091. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hootman JM, Helmick CG, Barbour KE, Theis KA, Boring MA. Updated Projected Prevalence of Self-Reported Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation Among US Adults, 2015–2040. Arthritis Rheum. 2016;68(7):1582–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84(3):351–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson AE, Kelli KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: The Chronic Osteoarthritis Management Initiative of the US Bone and Joint Initiative. Semin Arthritis Rheum. 2014;43(6):701–12. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans 2008 ODPHP Publication No U0036. Washington: Office of Disease Prevention and Health Promotion; - https://health.gov/paguidelines/2008/pdf/paguide.pdf [Google Scholar]
- 5.Dunlop DD, Song J, Lee J, Gilbert AL, Semanik PA, Ehrlich-Jones L, et al. Physical Activity Minimum Threshold Predicting Improved Function in Adults With Lower-Extremity Symptoms. Arthritis Care Res. 2017;69(4):475–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.White DK, Tudor-Locke C, Zhang Y, Fielding R, LaValley M, Felson DT, et al. Daily walking and the risk of incident functional limitation in knee osteoarthritis: an observational study. Arthritis Care Res. 2014;66(9):1328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Master H, Thoma LM, Christiansen MB, Polakowski E, Schmitt LA, White DK. Minimum Performance on Clinical Tests of Physical Function to Predict Walking 6,000 Steps/Day in Knee Osteoarthritis: An Observational Study. Arthritis Care Res. 2018;70(7):1005–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wallis J, Webster K, Levinger P, Taylor N. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthr Cartil. 2013;21(11):1648–59. [DOI] [PubMed] [Google Scholar]
- 9.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13(4):623–49. [Google Scholar]
- 10.Gyurcsik NC, Brawley LR, Spink KS, Brittain DR, Fuller DL, Chad K. Physical activity in women with arthritis: Examining perceived barriers and self-regulatory efficacy to cope. Arthritis Care Res. 2009;61(8):1087–94. [DOI] [PubMed] [Google Scholar]
- 11.Zhaoyang R, Martire LM, Sliwinski MJ. Morning Self-Efficacy Predicts Physical Activity Throughout the Day in Knee Osteoarthritis. Health Psychol. 2017;36(6):568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy SL, Smith DM, Clauw DJ, Alexander NB. The impact of momentary pain and fatigue on physical activity in women with osteoarthritis. Arthritis Care Res. 2008;59(6):849–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stubbs B, Hurley M, Smith T. What are the factors that influence physical activity participation in adults with knee and hip osteoarthritis? A systematic review of physical activity correlates. Clin Rehabil. 2015;29(1):80–94. [DOI] [PubMed] [Google Scholar]
- 14.Newsom JT, Shaw BA, August KJ, Strath SJ. Physical activity–related social control and social support in older adults: Cognitive and emotional pathways to physical activity. J Health Psychol. 2016;23(11):1389–404. [DOI] [PubMed] [Google Scholar]
- 15.Shores KA, West ST, Theriault DS, Davison EA. Extra-individual correlates of physical activity attainment in rural older adults. J Rural Health. 2009;25(2):211–8. [DOI] [PubMed] [Google Scholar]
- 16.Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34(12):1996–2001. [DOI] [PubMed] [Google Scholar]
- 17.Heath GW, Parra DC, Sarmiento OL, Andersen LB, Owen N, Goenka S, et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380(9838):272–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ranby KW, Aiken LS. Incorporating husband influences into a model of physical activity among older women. Br J Health Psychol. 2016;21(3):677–93. - 10.1007/s12529-019-09806-2. [DOI] [PubMed] [Google Scholar]
- 19.Tay L, Tan K, Diener E, Gonzalez E. Social relations, health behaviors, and health outcomes: A survey and synthesis. Appl Psychol Health Well Being. 2013;5(1):28–78. [DOI] [PubMed] [Google Scholar]
- 20.Berli C, Bolger N, Shrout PE, Stadler G, Scholz U. Interpersonal processes of couples’ daily support for goal pursuit: The example of physical activity. Personal Soc Psychol Bull. 2018;44(3):332–44. [DOI] [PubMed] [Google Scholar]
- 21.Li K, Cardinal BJ, Acock AC. Concordance of physical activity trajectories among middle-aged and older married couples: Impact of diseases and functional difficulties. J Gerontol B Psychol Sci Soc Sci. 2013;68(5):794–806. [DOI] [PubMed] [Google Scholar]
- 22.Martire LM, Stephens MAP, Mogle J, Schulz R, Brach J, Keefe FJ. Daily spousal influence on physical activity in knee osteoarthritis. Ann Behav Med. 2013;45(2):213–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mesquita R, Nakken N, Janssen DJA, van den Bogaart EHA, Delbressine JML, Essers JMN, et al. Activity Levels and Exercise Motivation in Patients With COPD and Their Resident Loved Ones. Chest. 2017;151(5):1028–38. [DOI] [PubMed] [Google Scholar]
- 24.Cobb LK, Godino JG, Selvin E, Kucharska-Newton A, Coresh J, Koton S. Spousal influence on physical activity in middle-aged and older adults: The ARIC study. Am J Epidemiol. 2015;183(5):444–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Knoll N, Burkert S, Scholz U, Roigas J, Gralla O. The dual-effects model of social control revisited: Relationship satisfaction as a moderator. Anxiety Stress Coping. 2012;25(3):291–307. [DOI] [PubMed] [Google Scholar]
- 26.Tucker JS. Health-related social control within older adults’ relationships. J Gerontol Ser B Psychol Sci Soc Sci. 2002;57(5):P387–95. [DOI] [PubMed] [Google Scholar]
- 27.Jordan JM. An Ongoing Assessment of Osteoarthritis in African Americans and Caucasians in North Carolina: The Johnston County Osteoarthritis Project. Trans Am Clin Climatol Assoc. 2015;126: 77–86. [PMC free article] [PubMed] [Google Scholar]
- 28.Carthron DL, Phillips AJ, Cuthbertson CC, Ellis K, Altpeter M, Callahan LF, et al. Four Methods of Recruiting Couples into a Longitudinal Study of Physical Activity in People with Osteoarthritis: Recruitment, Retention, and Lessons Learned. Front Public Health. 2018;6:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gardner MJ, Altman DG. Confidence intervals rather than P values: estimation rather than hypothesis testing. Br Med J (Clin Res Ed). 1986;292(6522):746–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Altman RD. Classification of disease: osteoarthritis. Semin Arthritis Rheum. 1991;20(6):40–7. [DOI] [PubMed] [Google Scholar]
- 31.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. [DOI] [PubMed] [Google Scholar]
- 33.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–36. [DOI] [PubMed] [Google Scholar]
- 34.Chogahara M. A multidimensional scale for assessing positive and negative social influences on physical activity in older adults. J Gerontol Ser B Psychol Sci Soc Sci. 1999;54(6):S356–67. [DOI] [PubMed] [Google Scholar]
- 35.Hendrick SS. A generic measure of relationship satisfaction. J Marriage Fam. 1988:93–8. [Google Scholar]
- 36.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40. [PubMed] [Google Scholar]
- 37.Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol Bull. 1995;118(3):392. [DOI] [PubMed] [Google Scholar]
- 38.Coxe S, West SG, Aiken LS. The analysis of count data: A gentle introduction to Poisson regression and its alternatives. J Pers Assess. 2009;91(2):121–36. [DOI] [PubMed] [Google Scholar]
- 39.Aiken LS, West SG, Reno RR. Multiple regression: Testing and interpreting interactions: Sage; 1991.
- 40.Molloy GJ, Dixon D, Hamer M, Sniehotta FF. Social support and regular physical activity: Does planning mediate this link? Br J Health Psychol. 2010;15(4):859–70. [DOI] [PubMed] [Google Scholar]
- 41.Eyler AA, Brownson RC, Bacak SJ, Housemann RA. The epidemiology of walking for physical activity in the United States. Med Sci Sports Exerc. 2003;35(9):1529–36. [DOI] [PubMed] [Google Scholar]
- 42.Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity social support and middle- and older-aged minority women: results from a US survey. Soc Sci Med. 1999;49(6): 781–9. [DOI] [PubMed] [Google Scholar]
- 43.Anderson-Bill ES, Winett RA, Wojcik JR. Social cognitive determinants of nutrition and physical activity among web-health users enrolling in an online intervention: The influence of social support, self efficacy, outcomes expectations, and self-regulation. J Med Internet Res. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brown DR, Carroll DD, Workman LM, Carlson SA, Brown DW. Physical activity and health-related quality of life: US adults with and without limitations. Qual Life Res. 2014;23(10):2673–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gallo LC, Troxel WM, Matthews KA, Kuller LH. Marital status and quality in middle-aged women: Associations with levels and trajectories of cardiovascular risk factors. Health Psychol. 2003;22(5):453. [DOI] [PubMed] [Google Scholar]
- 46.Yorgason JB, Johnson LN, Hill MS, Selland B. Marital Benefits of Daily Individual and Conjoint Exercise Among Older Couples. Fam Relat. 2018;67(2):227–39. [Google Scholar]
- 47.Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, Emmons KM. Understanding health behavior change among couples: An interdependence and communal coping approach. Soc Sci Med. 2006;62(6):1369–80. [DOI] [PubMed] [Google Scholar]
- 48.Lyons RF, Mickelson KD, Sullivan MJ, Coyne JC. Coping as a communal process. J Soc Pers Relat. 1998;15(5):579–605. [Google Scholar]
- 49.Kelley HH, Thibaut JW. Interpersonal relations: A theory of interdependence. New York: Wiley; 1978. [Google Scholar]
- 50.Myers Virtue S, Manne SL, Kashy D, Heckman CJ, Zaider T, Kissane DW, et al. Correspondence of physical activity and fruit/vegetable consumption among prostate cancer survivors and their spouses. Eur J Cancer Care (Engl). 2015;24(6):827–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brown DW, Balluz LS, Heath GW, Moriarty DG, Ford ES, Giles WH, et al. Associations between recommended levels of physical activity and healthrelated quality of life Findings from the 2001 Behavioral Risk Factor Surveillance System (BRFSS) survey. Prev Med. 2003;37(5):520–8. [DOI] [PubMed] [Google Scholar]


