Abstract
Context:
To address risks associated with prescription opioid medications, guidelines recommend lower dose, shorter duration of use, and avoidance of concurrent sedatives. Monitoring opioid-prescribing practices is critical for assessing guideline impact, comparing populations, and targeting interventions to reduce risks.
Objective:
To describe development of Washington (WA) State opioid-prescribing metrics, provide purpose and definitions, and apply metrics to prescription data for WA health care organizations.
Design:
We describe the development and testing of opioid-prescribing metrics by the WA State Bree Collaborative opioid work group.
Setting:
Washington State.
Participants:
Kaiser Permanente of Washington (KPW) Integrated Group Practice, KPW-contracted care providers, and WA Medicaid.
Main Outcome Measures:
Set of 6 strategic metrics tested across 3 different health systems adopted by WA State in 2017 for uniform tracking of opioid-prescribing guidelines and state policies. These metrics include (1) overall prevalence of any opioid use, (2) chronic use, (3) high-dose chronic use, (4) concurrent chronic sedative use, (5) days' supply of new prescriptions, and (6) transition from acute to chronic use.
Results:
In the first quarter of 2010, 10% to 12% of KPW and 14% of Medicaid patients received at least 1 opioid prescription. Among opioid users, 22% to 24% of KPW and 36% of Medicaid patients received chronic opioids. Among patients receiving chronic opioids, 16% to 22% of KPW and 32% of Medicaid patients received high doses (≥90 morphine-equivalent dose per day) and 20% to 23% of KPW and 33% of Medicaid patients received concurrent chronic sedatives. Five percent of Medicaid and 2% to 3% of KPW patients receiving new opioid prescriptions transitioned to chronic opioid use.
Conclusions:
The metrics are relatively easy to calculate from electronic health care data and yield meaningful comparisons between populations or health plans. These metrics can be used to display trends over time and to evaluate the impact of opioid-prescribing policy interventions.
Keywords: analgesics, epidemiologic surveillance, hypnotics and sedatives, opioid, prescribing patterns
Context
Surveillance of drug-prescribing trends and associated health events (positive or negative) is an important tool for guiding public health interventions to increase the effectiveness of health care services and to prevent harms from unsafe prescribing practices.1 In 2006, investigators from the United States' Centers for Disease Control and Prevention (CDC) published the first surveillance data showing that increased prescribing of opioids for chronic pain was associated with a large and increasing number of fatal overdoses involving prescription opioid analgesics.2 Subsequent analyses of national mortality data found that increased drug poisonings had contributed to an unprecedented increase in all-cause mortality.3 Chronic opioid use, high opioid doses, and concurrent use of opioids and sedatives have been associated with higher risks of fatal and nonfatal opioid overdoses.4–7 Concurrent use of opioids with sedative medications is associated with substantially increased risk of fatal overdoses even with relatively low morphine equivalent doses.7
In response to the epidemic of unintentional overdose deaths associated with prescription opioids,8 the Washington (WA) State Agency Medical Directors Group (AMDG) developed opioid-prescribing guidelines in 20078 and revised and expanded the guidelines in 2010 and again in 2015.9 In 2016, the CDC published comparable national guidelines.10 These guidelines discourage long-term use of opioids, high-dose prescribing, and prescribing opioids and benzodiazepines concurrently. In addition, the guidelines recommend that an initial opioid prescription generally be limited to 3 days or less, as longer duration of the first prescription is associated with increased risk of transitioning to chronic use.11
To support and track the impact of state and national guidelines, the Washington State Bree Collaborative12 developed and adopted 6 opioid-prescribing metrics.13 The intent of these metrics was to enable health care providers, health care systems, health plans, and public health organizations to apply pragmatic, standardized measures to data from diverse sources in efforts to decrease morbidity and mortality associated with prescription opioids.
Surveillance of opioid prescribing is critically important for understanding what changes in opioid prescribing are occurring over time, in different settings, and across clinicians within the same setting. Currently, comparing prescribing trends state to state is difficult. Adopting a standard set of measures to track opioid prescribing would allow for accurate comparison, better cross-state comparison, and sharing of best practices for greater population health impact.
The purpose of this practice report is to describe the development of the WA opioid metrics, to provide definitions for each of the metrics, and to apply the metrics to pharmacy billing data from multiple WA health organizations to illustrate how the data can be used to guide and evaluate interventions to address the opioid epidemic.
Development and Adoption of WA Opioid-Prescribing Metrics
In 2011, the WA State Legislature established the Bree Collaborative to enable public and private health care system leaders to work together to improve health care quality, health outcomes, and cost effectiveness of care in WA.12 The Collaborative includes participants, appointed by the governor, from WA public health care purchasers, health plans, employers, providers, hospitals, and quality improvement (QI) organizations. Annually, the Collaborative selects health care topics and convenes work groups of clinical experts, health system administrators, and community members to develop recommendations on these topics. Recommendations are then disseminated for public comment with wider stakeholder input, approved by Bree Collaborative members, and submitted to the WA Health Care Authority that administers WA Medicaid, public employee benefits, and school employee benefits. Recommendations are developed for inclusion in health care purchasing contracts and to set a community standard of care. In 2015, the Bree Collaborative endorsed the 2015 AMDG interagency opioid-prescribing guideline and convened a work group to develop implementation strategies.
As part of these implementation strategies, the Collaborative developed and adopted 6 opioid-prescribing metrics13 that align with the WA and CDC opioid-prescribing guidelines. The original intent was to develop metrics for each of the CDC guidelines, but some could not be measured with electronic data. We focused on measures known to be associated with a high risk of overdose (high dose, chronic use, and concurrent sedatives) and on measures of the transition from acute to chronic prescribing that could be calculated using billing or Prescription Drug Monitoring Program data. One of the primary goals of the metric set is to be short and actionable. As such, the Collaborative designed these metrics to be limited in number, to have a strategic focus, and to be used for QI. (For more details on alignment with the WA and CDC guidelines, see the Bree Collaborative opioid metrics document).13 After developing and testing the proposed metrics, the Bree Collaborative approved and adopted the 6 opioid-prescribing metrics described later and in the Table.
TABLE. Washington State Opioid-Prescribing Metrics.
| Opioid-Prescribing Metrics | Numerator | Denominator |
|---|---|---|
| Any opioid prescription | Number of patients with ≥1 opioid Rx filled | Number in population |
| Chronic opioid prescriptions | ||
| Percentage with ≥60 d supply dispensed in calendar quarter | Number of patients with ≥60 d supply from opioid Rxs filled | Number of patients with ≥1 Rx filled |
| Prevalence of chronic opioid users | Number of patients with ≥60 d supply from opioid Rxs filled | Number in population |
| High-dose chronic opioid prescriptions | ||
| Percentage ≥90 MME/d or ≥50 MME/d among chronic opioid users | Number of patients with chronic opioids with dose ≥90 MME/d or ≥50 MME/d | Number with chronic opioid use in quarter |
| Prevalence of chronic opioid users prescribed ≥90 MME/d or ≥50 MME/d | Number of patients with chronic opioids with dose ≥90 MME/d or ≥50 MME/d | Number in population |
| Chronic concurrent opioids and sedatives | ||
| Percentage of patients with chronic sedative prescriptions, among patients prescribed chronic opioids | Number of patients with ≥60 d supply of sedatives in quarter | Number with chronic opioid use |
| Prevalence of chronic opioid users prescribed concurrent sedatives | Number of patients with ≥60 d supply of sedatives in quarter | Number in population |
| Days' supply on first opioid prescription | ||
| Percentage with ≤3, 4-7, 8-13, and ≥14 d supply on the first opioid prescription among new opioid users | Number with ≤3, 4-7, 8-13, and ≥14 d supply on the first opioid prescription | Number of new opioid users in quarter with no opioid Rx in prior quarter |
| Transition from acute to chronic opioid prescriptions | ||
| Percentage with chronic opioid use in current quarter, among new opioid users in previous quarter | Number of opioid users with ≥60 d in current quarter who were new users in previous quarter | Number of new opioid users in previous quarter |
| Prevalence of new users transitioning to chronic users | Number of opioid users with ≥60 d in current quarter who were new users in previous quarter | Number in population |
Abbreviation: MME, morphine milligram equivalents.
WA Opioid-Prescribing Metrics
Overall prevalence: The first metric is a measure of overall prevalence of opioid prescribing and counts all patients who have filled 1 or more opioid prescriptions in the quarter. The prevalence of opioid prescribing is calculated by dividing the total number of patients who have filled at least 1 prescription in that quarter by the total population.
Chronic use: Chronic opioid use is defined as having 60 or more days' supply of opioids dispensed during a calendar quarter, regardless of overlapping prescriptions. This metric tracks the percentage of patients with at least 1 opioid prescription who received at least 60 days' supply of opioids during the quarter.
High-dose use: The high-dose metric is defined as the percentage of patients on chronic opioids with doses that average 50 or more or 90 or more morphine milligram equivalents (MME) per day over the calendar quarter, employing CDC-recommended dose cut points. The total MME of each prescription is calculated by multiplying the number of pills dispensed by drug strength and multiplying by a morphine conversion factor.9,14,15 The average MME per day for the calendar quarter is calculated by summing the MME from all opioid prescriptions dispensed in the quarter and dividing by 90 days.
Concurrent use: This metric tracks concurrent prescribing of chronic sedatives, defined as at least 60 days' supply in the calendar quarter, among patients receiving chronic opioids in the calendar quarter.
Days' supply of new prescriptions: This metric tracks the days' supply dispensed on the first opioid prescription among those identified with new opioid prescriptions. New opioid prescribing is defined as patients with at least 1 opioid prescription dispensed in the current calendar quarter with no opioid prescriptions dispensed in the preceding calendar quarter among those in the population during both quarters.
Transition from acute to chronic use: This metric tracks transition from acute to chronic opioid use by calculating the percentage of new users during 1 calendar quarter who transition to chronic use (≥60 days' supply) in the following calendar quarter.
The metrics are intended to be measured quarterly to track trends over time. Each metric can be calculated as percentages (percentage of patients, percentage of opioid users, percentage of chronic users, etc) or can be calculated as the prevalence per 1000 population. Methods to identify opioid medications and sedative medications are available on the Bree Web site.13 Buprenorphine and cough and cold formulations are excluded from these calculations.
Application of WA Opioid Metrics to Pharmacy Data Among WA Health Organizations
The Collaborative chose these metrics because of their strong associations with opioid overdose risk, their anticipated ease of application by diverse provider organizations, health plans, and public health organizations, and their relevance for guiding initiatives to reduce opioid-related risks and harms through QI efforts focused on patient safety. The metrics were intended to be easily calculated to measure key trends in opioid prescribing and to guide efforts to reduce opioid-related risks. As part of the development of these metrics, we tested each of these prescribing metrics using available pharmacy billing data from KPW and Medicaid and provided feedback and preliminary data to the work group developing these measures. The intention is that a demonstration of utility among diverse health systems will serve as a proof of principle before recommending wider adoption at the state or national level.
Study Sample
We calculated each of the 6 opioid-prescribing metrics using pharmacy data from Kaiser Permanente of Washington (KPW) (formerly Group Health Cooperative) and WA Medicaid. Data were available for both KPW Integrated Group Practice and for KPW-contracted care providers. The former is a staff model health maintenance organization serving about 425 000 persons, while the latter includes community practice clinics not owned by KPW serving about 225 000 persons.16 The WA Medicaid data were available for patients who filled at least 1 opioid prescription. The WA Medicaid covered approximately 500 000 adults aged 18 to 64 years in the fee-for-service programs. These analyses were approved by the KPW, the University of Washington, and the Washington State Institutional Review Boards.
Statistical Analyses
We had pharmacy billing data available from both Kaiser and Medicaid for 2010. For this report, the metrics are presented for the first calendar quarter of 2010. For this analysis, the percentage with any opioid use was calculated among all enrollees in the health plan each quarter. We calculated chronic opioid use as the percentage of all opioid users. The metrics for high dose and concurrent sedatives were calculated as a percentage of all chronic opioid users in that quarter. Days' supply of new prescriptions and transition to chronic use were calculated among new users.
Review of Opioid Metrics From KPW and WA Medicaid Pharmacy Data
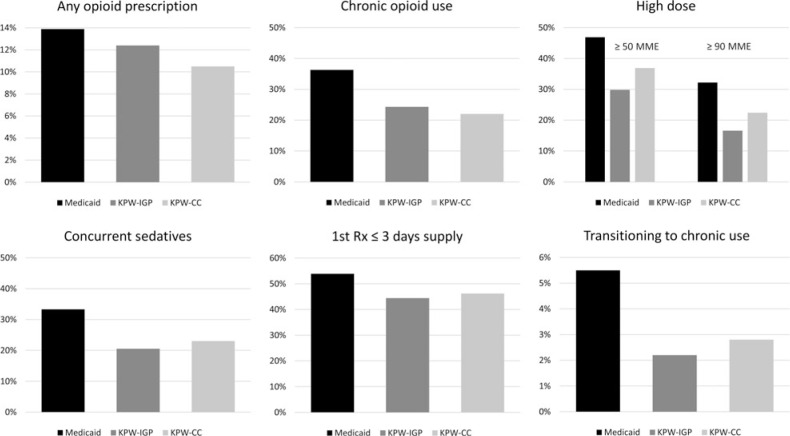
The Figure shows the opioid-prescribing metrics for the 2 KPW networks and Medicaid for the first quarter of 2010. Overall, 10% to 12% of KPW and 14% of Medicaid enrollees had at least 1 opioid prescription dispensed. Overall, 22% to 24% of KPW opioid users and 36% of Medicaid opioid users had 60 or more days' supply of opioids in the quarter, an indicator of chronic opioid use. Among patients with chronic opioid use in the KPW population, 30% to 37% had doses of 50 MME or more, 16% to 22% had doses of 90 MME per day or more, and 20% to 23% had concurrent chronic sedatives. Among patients receiving chronic opioids in the Medicaid population, 47% had doses of 50 MME or more, 32% had doses of 90 MME per day or more, and 33% had concurrent chronic sedatives. Among new opioid users, the first prescription was 3 days or less in 44% to 46% of KPW patients and in 54% of Medicaid. Among new opioid users, 2% to 3% of KPW and 5% of Medicaid patients had at least 60 days' supply of opioids in the following quarter, an indicator of transitioning to chronic opioid use.
FIGURE.
Opioid-Prescribing Metrics—Washington State, January to March 2010a
Abbreviations: KPW, Kaiser Permanente of Washington; MME, morphine milligram equivalents.
aAny opioid prescription: percentage with at least 1 opioid prescription filled in the calendar quarter in the population. Transition to chronic use: percentage with 60 or more days' supply of opioids in the current quarter among new users in the previous quarter. 1st Rx ≤3 days' supply: percentage of new opioid users with 3 or less days' supply on the first opioid prescription. Chronic opioid use: percentage of patients with 60 or more days' supply of opioids in calendar quarter among patients with 1 or more Rx filled in quarter. High dose: percentage of patients with chronic opioids with dose of 50 MME or more per day or dose of 90 MME or more per day. Concurrent sedatives: percentage of patients with chronic opioids with chronic sedatives.
Discussion
The WA Bree Collaborative, representing a broad array of both public and private health organizations, endorsed the 2015 AMDG opioid guideline9 and then developed a relevant set of opioid metrics for health systems and health plans to assist with implementation of the guideline. To accomplish this, the Bree Collaborative opioid work group focused on measures that aligned with both the WA and the CDC opioid guidelines. Washington State Department of Health, provider organizations, and health plans are now beginning to use these opioid-prescribing metrics to monitor prescribing trends over time.
Most participating payers were interested in the practicality of measurement using readily available data in their systems. Overall, we found that the metrics were relatively simple to operationalize, a key point stressed by the health plans in the opioid work group. As demonstrated, 4 of these metrics (prevalence of opioid use, chronic use, high-dose use, and concurrent sedatives) can be calculated using prescribing data for 1 calendar quarter. The metrics for days' supply of first prescription require 2 quarters and transition from short term to long term requires 3 quarters. Measures of transition to long-term prescribing may be more challenging to calculate, but monitoring this transition is critically important to reducing long-term opioid use.17 A large number of recent studies have used this type of measure to determine postoperative transition from acute to chronic opioid, and this type of data supported a recent WA State postoperative opioid guideline.18 Each additional week or refill of opioids postoperatively substantially increases subsequent risk of misuse, abuse, or overdose.19
The comparison of KPW and Medicaid data demonstrates that these prescribing metrics can be used not only to collect data but also to compare populations or health plans, to evaluate the impact of opioid-prescribing interventions, and to display trends over time. The large differences between Medicaid and the 2 Kaiser health plans' data reported here highlight the importance of tracking opioid prescribing for different health plans as the populations and the QI strategies may vary. As another example, more recent data suggest that the 2 KP networks reported here have experienced very different impacts from systemwide efforts to reduce inappropriate opioid prescribing with much larger decreases in doses in the Integrated Group Practice physicians than in the contracted care providers.20 While descriptive data for individual health plans or health systems are quite valuable, formal comparisons may need to adjust for sociodemographic differences.
In addition, opioid-prescribing metrics have been used by Medicaid21 and workers' compensation in WA22 to produce provider prescriber reports. Since there are large variations in prescribing by provider specialty,23 both of these agencies analyzed prescribing by provider type and specialty. The Department of Health, Washington Tracking Network is now producing county and statewide reports to track trends in the prevalence of opioid prescribing from 2012 through 2018 using Prescription Monitoring Program data.24 Similar opioid-prescribing metrics are being used on the Oregon Health Authority opioid dashboard to show differences county by county25,26 and in other states (eg, Colorado, Oregon, Pennsylvania).25,27,28
Although prescribing guidelines now recommend avoiding concurrent opioid and sedative prescriptions,9,10 concurrent sedative use among patients on chronic opioids was high in 2010. About one-third of Medicaid patients and more than 20% of KPW patients on chronic opioids also received chronic sedatives. Chronic sedative prescribing among patients also receiving chronic opioid prescriptions can be calculated easily by totaling days' supply of sedatives dispensed in a quarter; however, this provides a low estimate of the extent of concurrent use of the 2 medication classes. An alternative method is to determine whether there are any overlapping days of opioid and sedative prescriptions, but the algorithms are more complex and the health plans participating in the development of the metrics requested simpler calculations. An evaluation of the impact of the CDC guidelines recently reported that approximately 20% of patients with an opioid prescription had at least 1 day of overlap with a benzodiazepine.29 Regardless of different definitions of concurrent sedatives (different medications and different amounts of overlap), concurrent prescribing of opioids and sedatives is common, increasing the risk of overdose.
Depending on the setting or the purpose of the prescribing metrics, the opioid-prescribing metrics can be calculated as a percentage or as a population prevalence. In this analysis, we chose to present each of these metrics as percentages, instead of population prevalence, because not all clinics have population denominators and because the percentage of patients may be more meaningful for clinicians than prevalence per 1000 population. For example, knowing that 25% of a physician's patients on chronic opioids are also on concurrent sedatives may be more compelling and more likely to change provider-prescribing behavior than reporting that 5 of every 1000 patients in the practice are on concurrent sedatives. The CDC recently published similar clinical QI opioid measures.30 The QI measures include the percentage of patients with new opioid prescriptions for 3 days or less, the percentage of patients on long-term therapy with at least 50 or at least 90 MME per day, and the percentage of patients on long-term opioids who received a prescription for a benzodiazepine. However, one of the limitations of presenting prescribing metrics as percentages is the difficulty of interpreting trends if both the numerator and the denominator are changing over time. Similar issues have been described around the choice of numerators and denominators and the interpretation of various measures of abuse of prescription opioids.31 For QI for providers, it may be important to know the percentage of patients with high opioid doses or the percentage of patients with opioids and concurrent sedatives. However, for surveillance of opioid-prescribing trends over time, the prevalence of each measure may be a better measure of population trends. The DOH Washington Tracking Network displays age- and sex-adjusted population rates for each of these measures; these adjustments allow for comparisons of 1 geographic region to another or to the state rate.24
Limitations of using pharmacy billing data include not knowing actual consumption and missing prescription data. First, these calculations (eg, dose, duration, concurrent use, etc) are based on the dispensed amounts of opioids and other medications, not on the actual timing or use of ingested medication. In addition, pharmacy billing data may miss opioids dispensed in a hospital, covered by other insurance, or paid for in cash.
In Washington State, the process of developing and adopting opioid-prescribing metrics was coordinated by The Bree Collaborative. In other states (eg, Oregon), various state agencies have coordinated their efforts to define and track opioid prescribing. One of the limitations associated with the collaborative process used in WA is the large time investment of the many participants. However, this collaborative process allows the health care community to develop priorities and methods of impacting quality that are meaningful, pragmatic, and foster ownership through consensus and support of participating organizations. Although these benefits help with adoption, for states without prescribing metrics, it is probably much more efficient to consider adopting metrics that have already been developed.
The development, testing, and implementation of opioid-prescribing metrics are relatively new but are expanding in practice nationwide. In addition to Washington, other states and national organizations are measuring similar concepts, such as high dose, concurrent sedatives, and days' supply, among others. However, at this time, the actual definitions of these measures differ in ways that make comparing data state-to-state and organization-to-organization difficult. For example, the WA high-dose metric calculates morphine equivalent dose at a person level per quarter, while others have calculated dose at the prescription level.29 Similarly, the metric measuring days' supply can be calculated among new prescriptions13 or among all prescriptions.29 Over the next few years, as more data on opioid prescribing become available, the various metrics should be evaluated, compared, and revised as necessary. There should be an emphasis on publicly available metrics and methods, so that all health systems, health plans, and states may freely use them.
Conclusion
Washington State developed and adopted metrics for monitoring opioid prescribing relevant to key recommendations of both CDC and WA opioid-prescribing guidelines. The metrics were designed to be relatively simple to calculate from available pharmacy data and are suitable for tracking prescribing trends over time on a quarterly basis. These measures are critical for tracking progress on the adoption of state and federal guidelines and reversing the opioid epidemic. Many clinics, health plans, and government agencies are beginning to produce prescribing reports for providers. States are creating opioid dashboards, and in WA State, 3 of the metrics reported here have been adopted into the WA State Common Measure set.32 We see value in adopting standard measures to coordinate and leverage efforts to reverse this epidemic.
Implications for Policy & Practice
Monitoring opioid prescribing can help guide interventions to reduce opioid-related risks.
Opioid-prescribing metrics can be used for evaluating quality improvement initiatives, for comparing populations or health plans, and for tracking trends over time.
States without opioid-prescribing metrics can adopt these tested metrics.
There is value in adopting standard measures across public and private insurers, public health organizations, practicing clinicians, and delivery systems.
Footnotes
Additional members of the Bree Collaborative opioid work group are as follows: Amanda Avalos, Health Care Authority; Chris Baumgartner, Department of Health; David Buchholz, MD, Premera Susie Dade, Washington Health Alliance; Chris Dale, MD, Swedish Mary Fliss, Health Care Authority; Charissa Fotinos, MD, Health Care Authority; Dan Kent, MD, United Health; Dan Lessler, MD, MHA, Health Care Authority; David Mancuso, PhD, Department of Social and Health Services; Mark Murphy, MD, MultiCare; Eric Ossiander, PhD, Department of Health; Yusuf Rashid, PharmD, Community Health Plan of Washington; Shirley Reitz, PharmD, Omedarx; Greg Rudolf, MD, Swedish Medical Center; Jeanne Sears, PhD, MS, University of Washington; Angie Sparks, MD, Group Health Cooperative; Mark Stephens, CareSync Consulting, LLC; and Gregory Terman, MD, PhD, University of Washington.
University of Washington staff who assisted with this article are as follows: Rui Wu, Renu Garg, Brian Chin, Beryl Schulman, and Ryan Sterling.
Dr Deborah Fulton-Kehoe's work on the article was partially funded by the Centers for Disease Control and Prevention (CDC) grant number 5 NU17CE002734–02-00 titled Washington State Department of Health's Prescription Drug Overdose for States grant. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
All authors were active participants in the development and testing of the Bree Collaborative opioid-prescribing metrics and fully participated in writing and revising this manuscript.
The authors declare no conflicts of interest.
References
- 1.Thacker SB, Berkelman RL. Public health surveillance in the United States. Epidemiol Rev. 1988;10(1):164–190. [DOI] [PubMed] [Google Scholar]
- 2.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–627. [DOI] [PubMed] [Google Scholar]
- 3.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. [DOI] [PubMed] [Google Scholar]
- 6.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171(7):686–691. [DOI] [PubMed] [Google Scholar]
- 7.Garg RK, Fulton-Kehoe D, Franklin GM. Patterns of opioid use and risk of opioid overdose death among Medicaid patients. Med Care. 2017;55(7):661–668. [DOI] [PubMed] [Google Scholar]
- 8.Franklin GM, Sabel J, Jones CM, et al. A comprehensive approach to address the prescription opioid epidemic in Washington State—milestones and lessons learned. Am J Public Health. 2015;105(3):463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Washington State Agency Medical Directors' Group. Interagency guideline on prescribing opioids for pain. http://www.agencymeddirectors.wa.gov/Files/2015AMDGOpioidGuideline.pdf. Published 2015. Accessed August 8, 2018.
- 10.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65(No. RR-1):1–49. http://dx.doi.org/10.15585/mmwr.rr6501e1externalicon. [DOI] [PubMed] [Google Scholar]
- 11.Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Bree Collaborative. http://www.breecollaborative.org/. Accessed July 19, 2018.
- 13.Dr Robert Bree Collaborative. Opioid prescribing metrics. http://www.breecollaborative.org/wp-content/uploads/Bree-Opioid-Prescribing-Metrics-Final-2017.pdf. Published 2017. Accessed July 19, 2018.
- 14.Von Korff M, Saunders K, Thomas Ray G, et al. De facto long-term opioid therapy for noncancer pain. Clin J Pain. 2008;24(6):521–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nielsen S, Degenhardt L, Hoban B, Gisev N. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol Drug Saf. 2016;25(6):733–737. [DOI] [PubMed] [Google Scholar]
- 16.Saunders KW, Davis RL, Stergachis A. Group Health Cooperative of Puget Sound. Pharmacoepidemiology. 4th ed. West Sussex, England: John Wiley & Sons, Ltd; 2000:247. [Google Scholar]
- 17.Von Korff M, Turner JA, Shortreed SM, et al. Timeliness of care planning upon initiation of chronic opioid therapy for chronic pain. Pain Med. 2016;17(3):511–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prescribing opioids for postoperative pain—supplemental guidance. Developed by the Dr. Robert Bree Collaborative and Washington State Agency Medical Directors' Group in collaboration with academics, pain experts, and practicing surgeons. http://www.breecollaborative.org/wp-content/uploads/Final-Supplemental-Bree-AMDG-Postop-pain-091318-wcover.pdf. Published July 2018. Accessed February 4, 2019.
- 19.Brat GA, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ. 2018;360:j5790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saunders KW, Shortreed S, Thielke S, et al. Evaluation of health plan interventions to influence chronic opioid therapy prescribing. Clin J Pain. 2015;31(9):820–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Washington State Health Care Authority. Washington Apple Health (Medicaid) opioid prescribing report. https://www.hca.wa.gov/about-hca/clinical-collaboration-and-initiatives/opioid-crisis. Accessed July 19, 2018.
- 22.Washington State Department of Labor & Industries. opioid prescribing report. http://www.lni.wa.gov/claimsins/providers/treatingpatients/ByCondition/OpioidPrescribing/default.asp. Accessed July 19, 2018.
- 23.Weiner SG, Baker O, Rodgers AF, et al. Opioid prescriptions by specialty in Ohio, 2010-2014. Pain Med. 2018;19(5):978–989. [DOI] [PubMed] [Google Scholar]
- 24.Washington State Department of Health. Washington Tracking Network—Opioids. https://www.doh.wa.gov/DataandStatisticalReports/EnvironmentalHealth/WashingtonTrackingNetworkWTN/Opioids. Accessed July 19, 2018.
- 25.Oregon Health Authority. Opioid overdose data dashboard. https://www.oregon.gov/oha/PH/PREVENTIONWELLNESS/SUBSTANCEUSE/OPIOIDS/Pages/data.aspx. Accessed August 8, 2018.
- 26.Hedberg K, Bui LT, Livingston C, Shields LM, Van Otterloo J. Integrating public health and health care strategies to address the opioid epidemic: the Oregon Health Authority's opioid initiative. J Public Health Manag Pract. 2019;25(3):214–220. [DOI] [PubMed] [Google Scholar]
- 27.Denver Public Health. Substance use exposure dashboard. http://www.denverpublichealth.org/community-health-promotion/substance-misuse/substance-use-exposure-dashboard. Accessed June 6, 2019.
- 28.Pennsylvania Department of Health. Prescription drug monitoring program interactive data report. https://www.health.pa.gov/topics/programs/PDMP/Pages/Data.aspx. Accessed June 6, 2019.
- 29.Bohnert ASB, Guy GP, Jr, Losby JL. Opioid prescribing in the United States before and after the Centers for Disease Control and Prevention's 2016 opioid guideline. Ann Intern Med. 2018;169(6):367–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Quality Improvement and Care Coordination: Implementing the CDC Guideline for Prescribing Opioids for Chronic Pain. Atlanta, GA: National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention; https://www.cdc.gov/drugoverdose/pdf/prescribing/CDC-DUIP-QualityImprovementAndCareCoordination-508.pdf. Published 2018. Accessed July 9, 2019. [Google Scholar]
- 31.Secora AM, Dormitzer CM, Staffa JA, Dal Pan GJ. Measures to quantify the abuse of prescription opioids: a review of data sources and metrics. Pharmacoepidemiol Drug Saf. 2014;23(12):1227–1237. [DOI] [PubMed] [Google Scholar]
- 32.Washington Health Alliance. Washington State common measure set for health care quality and cost. https://wacommunitycheckup.org/about/common-measure-set/. Accessed January 8, 2019.