Abstract
Objectives
There are no uniform screening recommendations for anal cancer. Medical practice guidelines are now available on the use of Digital Anal Rectal Examinations (DARE) for the detection of anal cancer; however, because screening can result in more harm than benefit, our objective was to assess the evidence for use of DARE as a public health screening tool.
Materials and Methods
We conducted a current critical appraisal of anal cancer literature using World Health Organization criteria for assessing the potential utility of a public health screening program.
Results
Digital Anal Rectal Examination satisfies most, but not all, World Health Organization criteria for a public health program that seeks to detect early invasive anal cancer in populations at high risk for anal cancer, most notably HIV-positive men who have sex with men; however, DARE is not appropriate when facilities for treatment are nonexistent. In addition, there are insufficient data on DARE sensitivity and specificity.
Conclusions
The mildly invasive nature of DARE, limited likelihood of adverse procedure-related events, cost-effectiveness and patient acceptability, as well as wide availability of DARE support consideration of its integration into screening for populations at high risk of anal cancer, especially HIV-positive men who have sex with men.
Key Words: Digital Anal Rectal Examination, DARE, anal cancer, anal neoplasms, mass screening, HIV, men who have sex with men
Anal cancer incidence is stable or increasing in the general population1,2 and highest in men who have sex with men (MSM) with HIV2,3; however, no uniform screening recommendations for anal cancer exist for this population or others with increased anal cancer incidence4 including other persons with HIV, other immunosuppressed persons,5 HIV-negative MSM,6 and women with a history of human papillomavirus (HPV)-associated anogenital dysplasia.7
Although HPV vaccines are highly efficacious, their full impact on anal cancer incidence will take decades to be realized8,9; thus, secondary prevention using screening methods have been suggested in several regional and national guidelines for persons living with HIV (PHIV).4
One method cited by these recommendations for PHIV is the Digital Anal Rectal Examination (DARE)10 whose goal is to detect early stage (preferably stage 1) anal cancer. Currently, anal canal tumors have an average of greater than 3.0 cm in diameter at first presentation. These larger tumors result in poorer 5-year survival and higher morbidity.11 Given that DARE can detect abnormalities smaller than 1.0 cm,12 and new medical practice guidelines are now available for DARE,13 it may be helpful to evaluate DARE as a public health screening tool for anal cancer.
The current article assesses the evidence for use of DARE according to the application of established World Health Organization criteria for public health screening.14 Much of this evidence focuses on HIV-positive MSM; however, we will also address data from other populations with elevated risk, when available.
Of note, other proposed screening algorithms target putative precancerous lesions, rather than invasive cancer, and rely on high-resolution anoscopy (HRA)-directed biopsy to detect anal high-grade squamous intraepithelial lesions (HSILs).15 Although utility of HRA has been suggested16 and is being used to assess anal precancer therapeutics in a current trial (NCT02135419), currently, there is limited capacity for HRA even in high-resource settings and several challenges in scaling up HRA, including cost, specialized technical training required, and participant discomfort.15,17 Digital Anal Rectal Examination may be an option for health programs in areas without access to HRA if the benefits of screening with DARE outweigh the harms.
DIGITAL ANAL RECTAL EXAMINATION - DARE
The purpose of DARE is to detect abnormalities of the perianus, anal canal, distal rectum, and, in women, the rectovaginal septum. Digital Anal Rectal Examination is different than the Digital Rectal Examination, which has emphasized palpation of the posterior surface of the prostate gland.18 A health care provider performs DARE by first inquiring about anal symptoms, for example, anal bleeding, pain, and palpable masses, and then inspecting the perianus (a radius of 5 cm from the anal verge), followed by a 360-degree palpation of the anal canal and distal rectum. The procedure is short, usually taking no more than 1 minute to complete. Detailed instructions, standards, training, competencies, and quality assurance metrics for DARE have been recently published.13
WORLD HEALTH ORGANIZATION CRITERIA
Screening is the presumptive identification of unrecognized disease or defect by the application of tests, examinations, or other procedures, which can be applied rapidly.14 Screening can result in more harm than benefit, for example, if there is no treatment to give screen-positive individuals, or if the number of false-positives is high and results in substantial morbidity through unnecessary tests and examinations. The World Health Organization (WHO) publication “Principles and Practice of Screening for Disease” proposed a set of 10 criteria, which can be a useful lens in which to consider potential harms and benefits of DARE for anal cancer screening.14 Each criterion is considered in light of the evidence for cancer detection using DARE.
The condition should be an important health problem for the individual or community.
Late detection of squamous cell carcinoma of the anus carries substantial morbidity and mortality including sphincter dysfunction, permanent colostomy, and low probability of age-standardized 5-year survival when diagnosed in regional or distant stages (58.5% and 31.7%, respectively).19,20
Population-based cancer registries identify anal cancer as a very rare cancer (annual age-adjusted incidence approximately 0.5–2/100,000) with incidence generally 1.5- to 2-fold higher in women than men.1,2 Risk increases with age, reaching a maximum of 4 to 8 annual cases per 100,000 women and 3 to 5 cases per 100,000 men, 70 years or older.21 However, some subpopulations are known to be at vastly higher risk, most notably PHIV.22,23
Among MSM with HIV, anal cancer is a common cancer (see Table 1) with more than a 40-fold higher risk than the rest of the general population.2,3,24,26 Annual incidence among MSM with HIV ranges from 88 to 131 cases per 100,000 in the antiretroviral therapy era in some high-income settings3,24 and is highest in HIV-positive MSM 60 years or older.24 Indeed, Colon-Lopez et al.26 observed that in the United States, the 5-year cumulative incidence of anal cancer among HIV-positive MSM 45 years or older is at least as high as that of colorectal cancer in persons 50 years or older, for which routine, population-based screening is standardized and recommended.
TABLE 1.
Anal Squamous Cell Carcinoma Risk Estimates in Selected Populations
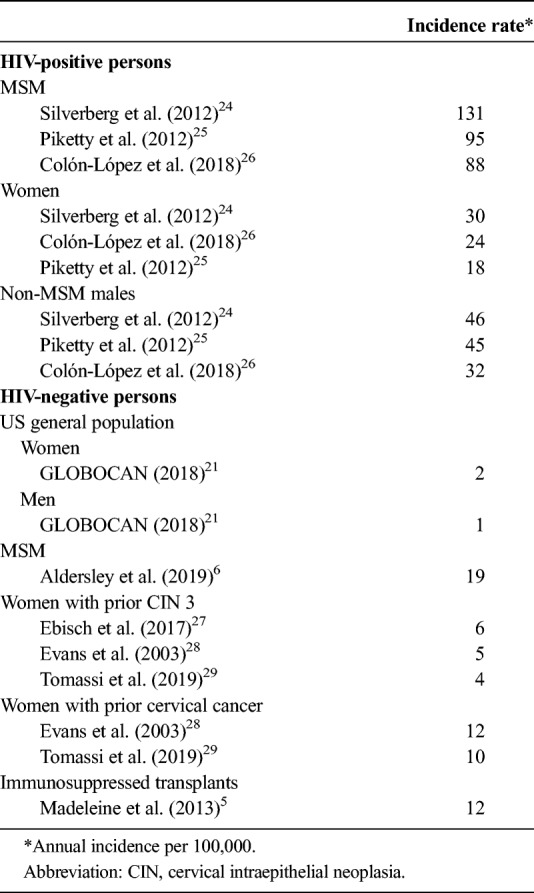
Although incidence is lower than in HIV-positive MSM, anal cancer incidence is also well established to be highly elevated among female PHIV whose annual incidence is 32 to 46 per 100,000 persons and non-MSM male PHIV whose annual incidence 32 to 46 per 100,000 persons.24,25,28
Cancer registry data and linkage studies identify other subpopulations with an excess incidence of anal cancer compared with the general population. They include HIV-negative MSM (17–19 annual cases per 100,000 persons, although anal cancer incidence data remain sparse).3,6,30 Anal cancer incidence is also elevated among persons with iatrogenic immune suppression 12 cases per 100,0005 and among women with prior anogenital HPV-associated neoplasia.7,27 For example, incidence is 4–6/100,000 among women with cervical intraepithelial neoplasia III27,29–31 and 10/100,000 among those with cervical cancer.31 These incidence data are lower than those seen for PHIV and more similar to incidence seen among women 70 years or older in the general population.
Anal cancer incidence data outside of high-resource countries are sparse, although recent studies indicate that in some middle-income countries, anal cancer incidence is also increasing.1 High-risk anal HPV infection and anal precancers have also been shown to be very common among PHIV and HIV-negative MSM in some middle- and low-income countries32,33; thus, increased anal cancer incidence in these subpopulations may not be restricted to high-resource settings.
2. There should be an accepted treatment for persons with recognized disease.
Excisional biopsies with adequate margins are an appropriate treatment for perianal squamous cancers of less than 2 cm or anal canal cancers with less than 3-mm invasion and less than 7-mm horizontal spread. Treatment with chemoradiation for nonmetastatic invasive anal canal tumors is noncontroversial with treatment protocols established 45 years ago.34,35 Most patients treated with chemoradiation experience low morbidity and mortality with better prognosis the earlier the cancer is detected.19
There are reports of high survival rates for small tumors. For example, one publication reported 100% disease-specific survival in 66 persons with tumors of 1 cm or less at 5 years.36 Another study used local excision only for squamous cell carcinomas below the dentate line. For 15 PHIV with tumors of 2 cm or less, the publication reported 100% survival at 4 years.37
3. Facilities for diagnosis and treatment should be available.
Although diagnostic and treatment resources for anal cancer are widely available in high-income countries, the extent of training needed to perform an accurate DARE is unknown but may require some or all of the following: knowledge of anal anatomy and physiology, training on clinical features of anal disease, experience performing the procedure, and feedback from patients undergoing the examination.13 The training could conceivably be accommodated in medical or nursing schools or specialized training courses using in-person or online formats.38 Initial research suggests that underutilization of DARE by clinicians is associated with a lack of training and other factors.39
Access to surgery and radiotherapy resources may be very limited or absent in many low- and middle-income countries.40,41 Use of DARE for anal cancer screening is not appropriate when diagnostic and treatment resources are not available.
4. There should be a recognizable latent or early symptomatic stage.
Most anal cancers are visible at the perianus and/or have palpable tumors in the anal canal.42,43 In one study, palpable masses as small as 0.3 cm were recognized during DARE12; thus, a DARE public health screening program may detect invasive cancers in an early stage when the tumor may not be obvious to the patient. Provider questions about anal symptoms, for example, anal bleeding and pain, may increase detection of anal cancer.13
5. There should be a suitable test or examination.
To be a suitable screening test, DARE should recognize very early invasive disease, for example, tumors of 2 cm or less. Although robust sensitivity and specificity data for DARE are lacking, some data shed light on DARE accuracy. In a prospective study of progression of HSIL to invasive anal cancer, a total of 23 (85%) of 27 anal cancers were detected by palpation.43 In a retrospective chart review of 128 anal cancers in a single radiotherapy center in Australia, 52% were visible at the perianal region, which may act as a lower bound for sensitivity.42
Other data imply that there may be a low number of unnecessary referrals after a DARE. The Anal Cancer Examination Study included 327 MSM with HIV and resulted in referral of 30 persons to a colorectal surgeon after a total of 862 DARE examinations over 2 years. Of 24 men who completed the referral, 5 had no lesion upon a colorectal surgeon's examination, 1 had anal cancer, 8 had incidental HSIL lesions after biopsy of an abnormality, and the remaining 10 had benign warts, skin tags, polyps, or anal fissures. Adverse events after DARE were rare.44 Thus, the potential for substantial morbidity among MSM with HIV from unnecessary DARE follow-up may be low.
6. The test should be acceptable to the population.
Multiple studies observe DARE to be well tolerated and acceptable among HIV-positive and HIV-negative MSM in western countries.44,45 Nevertheless, some providers incorrectly believe that the procedure is generally unacceptable among MSM and thus avoid using it.46
Studies of DARE acceptability among other populations are lacking.45 It is worth noting that Digital Rectal Examination, which is also a mildly invasive manual procedure involving the anal canal, may be somewhat less acceptable among the overall population of African-American men.47
7. The natural history of the disease should be adequately understood.
Unlike the natural history of HPV infection, the natural history of anal cancer is well known in that smaller tumors usually become larger and the smaller tumors are more easily treated than larger tumors; thus, smaller tumors can be targeted for detection and yield a better prognosis.11 Although the median age at presentation is approximately 60 years in HIV-negative persons,48 the median age at presentation for HIV-positive MSM is approximately 10 years younger.49
8. There should be agreement on whom to treat as patients.
There is agreement that suspicious masses detected on DARE, regardless of lesion location, size, or patient age, should be further evaluated.13
9. Cost-effectiveness should be established.
Using mathematical modeling, an Australian study determined that DARE is likely to be cost-effective when conducted on a regular basis among HIV-positive MSM 50 years or older. The investigators found that biennial screening resulted in incremental cost-effectiveness ratios of US $45,484 per quality-adjusted life year gained.50
10. Screening should be a continuing process.
Digital Anal Rectal Examination's high acceptability among MSM likely facilitates repeated use of DARE. In one study that used screening reminders that mimicked standard clinical reminders, 71% of participants returned for 3 DAREs scheduled at 0, 12, and 24 months. Of the remainder, 22% of men returned for 2 DAREs and 7% returned for only 1 DARE.44
Repeat screening will be affected by recommended screening intervals, and currently, only expert opinion guides the recommended intervals. For example, a minimum of an annual DARE among HIV-positive MSM 37 years or older has been suggested,13 whereas other intervals are recommended for other populations at increased risk for anal cancer.13,51,52
CONCLUSIONS
Digital Anal Rectal Examination satisfies most, but not all, WHO criteria for detecting an outcome of early invasive anal cancer in subpopulations at high risk for anal cancer, most notably HIV-positive MSM, followed by other persons with HIV. The mildly invasive nature of DARE, limited likelihood of adverse procedure-related events, and wide availability of the test (compared with HRA) support consideration of its integration into screening for these populations at high risk of anal cancer. However, lack of facilities for treatment in some low and middle-income regions and insufficient data on sensitivity and specificity of DARE, caution against using DARE in all settings.
Although DARE might also be considered for other groups with elevated anal cancer risk in comparison with the general population, such as recipients of solid organ transplants, HIV-negative MSM, and women with prior HPV-associated anogenital disease, their absolute anal cancer incidence rates are lower. In addition, fewer published data regarding some WHO screening criteria among these populations provide less support for their inclusion in DARE public health screening programs at this time.
Nevertheless, there is evidence that the following WHO criteria are supported for anal cancer screening among these high-risk populations:
anal cancer is an important health problem.
noncontroversial treatment modalities exist for invasive anal cancer.
resources for conducting DARE may be available in most places (but should only be used when there is access to diagnostic and treatment facilities).
invasive anal cancer has a recognizable early symptomatic phase.
DARE may recognize common anal cancer signs and symptoms including palpable anal canal tumors and visible perianal lesions.
the natural history of invasive anal cancer is well understood, in comparison with HPV infection natural history.
there is agreement on whom to treat.
Among MSM with HIV, the use of DARE is further supported by its acceptability, cost-effectiveness, and patient compliance with repeated screening.
To support implementation of DARE screening, further studies are needed, most importantly to better understand sensitivity and specificity of DARE for anal cancer. Cost-effectiveness data are needed in additional populations and more data are needed on barriers to physician use. In addition, better anal cancer incidence data are needed for HIV-negative MSM.53 However, given the potential for rapidly educating clinicians and the lack of need for technical and costly equipment, it may be possible to rapidly scale up the infrastructure for a DARE public health screening program for HIV-positive MSM.
There are few ongoing studies whose primary outcomes include the assessment of DARE to detect early invasive anal cancer. The Prevent Anal Cancer Study will use modeling strategies to evaluate the cost-effectiveness of DARE among HIV-positive and HIV-negative MSM and the impact of DARE on survival and quality of life (1R01CA232892-01). This study will also assess compliance with anal cancer screening among MSM and provide additional data on the clinical utility of DARE (7R01CA215403-02). Though not a screening study, the ANCHOR Study, designed to assess whether treatment for anal HSIL prevents progression to anal cancer may provide data that support a better understanding of DARE's utility.
In summary, although these studies' forthcoming data may shed more light on public health screening strategies that incorporate DARE, we believe that there is substantial evidence at hand that supports its use in high-risk populations now.
Footnotes
The authors have declared they have no conflicts of interest.
This study was supported by National Cancer Institute, National Institutes of Health (USA), 1R01CA232892 (A.G.N.); U01-HL146193 (NIH, G.D.). Publication and report contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCI or of the International Agency for Research on Cancer/World Health Organization.
REFERENCES
- 1.Islami F, Ferlay J, Lortet-Tieulent J, et al. International trends in anal cancer incidence rates. Int J Epidemiol 2017;46:924–38. [DOI] [PubMed] [Google Scholar]
- 2.van der Zee RP, Richel O, de Vries HJ, et al. The increasing incidence of anal cancer: can it be explained by trends in risk groups? Neth J Med 2013;71:401–11. [PubMed] [Google Scholar]
- 3.Machalek DA, Poynten M, Jin F, et al. Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: a systematic review and meta-analysis. Lancet Oncol 2012;13:487–500. [DOI] [PubMed] [Google Scholar]
- 4.Ong JJ, Chen M, Grulich AE, et al. Regional and national guideline recommendations for digital ano-rectal examination as a means for anal cancer screening in HIV positive men who have sex with men: a systematic review. BMC Cancer 2014;14:557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madeleine MM, Finch JL, Lynch CF, et al. HPV-related cancers after solid organ transplantation in the United States. Am J Transplant 2013;13:3202–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aldersley J, Lorenz DR, Misra V, et al. Increased risk of anal squamous cell carcinoma in HIV-positive men with prior hepatitis B virus infection. AIDS 2019;33:145–52 (Dana Gabuzda personal communication). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilbert DC, Wakeham K, Langley RE, et al. Increased risk of second cancers at sites associated with HPV after a prior HPV-associated malignancy, a systematic review and meta-analysis. Br J Cancer 2019;120:256–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palefsky JM, Giuliano AR, Goldstone S, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. New Engl J Med 2011;365:1576–85. [DOI] [PubMed] [Google Scholar]
- 9.Woestenberg PJ, King AJ, Van Benthem BHB, et al. Bivalent vaccine effectiveness against anal human papillomavirus positivity among female sexually transmitted infection clinic visitors in the Netherlands. J Infect Dis 2019. doi: 10.1093/infdis/jiz187. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 10.Steele SR, Varma MG, Melton GB, et al. Practice parameters for anal squamous neoplasms. Dis Colon Rectum 2012;55:735–49. [DOI] [PubMed] [Google Scholar]
- 11.Madeleine MM, Newcomer LM. Cancer of the anus. In: Ries LAG, Young JL, Keel GE, Eisner MP, Lin YD, eds. SEER Survival Monograph: Cancer Survival Among Adults: U.S. SEER Program, 1988-2001, Patient and Tumor Characteristics, Pub. No. 07-6215. Bethesda, MD: National Cancer Institute, SEER Program; 2007. [Google Scholar]
- 12.Nyitray AG, Hicks JT, Hwang LY, et al. A phase II clinical study to assess the feasibility of self and partner anal examinations to detect anal canal abnormalities including anal cancer. Sex Transm Infect 2018;94:124–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hillman RJ, Berry-Lawhorn JM, Ong JJ, et al. International Anal Neoplasia Society guidelines for the practice of digital anal rectal examination. J Low Genit Tract Dis 2019;23:138–46. [DOI] [PubMed] [Google Scholar]
- 14.Wilson JMG, Jungner G. Public Health Papers, #34: Principles and Practice of Screening for Disease. Geneva: World Health Organization; 1968. [Google Scholar]
- 15.Hillman RJ, Cuming T, Darragh T, et al. 2016 IANS International Guidelines for Practice Standards in the Detection of Anal Cancer Precursors. J Low Genit Tract Dis 2016;20:283–91. [DOI] [PubMed] [Google Scholar]
- 16.Panther LA, Wagner K, Proper J, et al. High resolution anoscopy findings for men who have sex with men: Inaccuracy of anal cytology as a predictor of histologic high-grade anal intraepithelial neoplasia and the impact of HIV serostatus. Clin Infect Dis 2004;38:1490–2. [DOI] [PubMed] [Google Scholar]
- 17.Neukam K, Milanes Guisado Y, Fontillon M, et al. High-resolution anoscopy in HIV-infected men: assessment of the learning curve and factors that improve the performance. Papillomavirus Res 2019;7:62–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reis LO, Simao AF, Baracat J, et al. Digital rectal examination standardization for inexperienced hands: teaching medical students. Adv Urol 2013;2013:797096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shridhar R, Shibata D, Chan E, et al. Anal cancer: current standards in care and recent changes in practice. CA Cancer J Clin 2015;65:139–62. [DOI] [PubMed] [Google Scholar]
- 20.Razzaghi H, Saraiya M, Thompson TD, et al. Five-year relative survival for human papillomavirus-associated cancer sites. Cancer 2018;124:203–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. Available at: https://gco.iarc.fr/today. Accessed July 6, 2019.
- 22.Silverberg MJ, Lau B, Achenbach CJ, et al. Cumulative incidence of cancer among persons with HIV in North America: a cohort study. Ann Intern Med 2015;163:507–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Franceschi S, Lise M, Clifford GM, et al. Changing patterns of cancer incidence in the early- and late-HAART periods: The Swiss HIV Cohort Study. Br J Cancer 2010;103:416–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silverberg MJ, Lau B, Justice AC, et al. Risk of anal cancer in HIV-infected and HIV-uninfected individuals in North America. Clin Infect Dis 2012;54:1026–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Piketty C, Selinger-Leneman H, Bouvier AM, et al. Incidence of HIV-related anal cancer remains increased despite long-term combined antiretroviral treatment: results from the French Hospital Database on HIV. J Clin Oncol 2012;30:4360–6. [DOI] [PubMed] [Google Scholar]
- 26.Colon-Lopez V, Shiels MS, Machin M, et al. Anal cancer risk among people with HIV infection in the United States. J Clin Oncol 2018;36:68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ebisch RMF, Rutten DWE, IntHout J, et al. Long-lasting increased risk of human papillomavirus-related carcinomas and premalignancies after cervical intraepithelial neoplasia grade 3: a population-based cohort study. J Clin Oncol 2017;35:2542–50. [DOI] [PubMed] [Google Scholar]
- 28.Evans HS, Newnham A, Hodgson SV, et al. Second primary cancers after cervical intraepithelial neoplasia III and invasive cervical cancer in Southeast England. Gynecol Oncol 2003;90:131–6. [DOI] [PubMed] [Google Scholar]
- 29.Tomassi MJ, Abbas MA, Klaristenfeld DD. Expectant management surveillance for patients at risk for invasive squamous cell carcinoma of the anus: a large US healthcare system experience. Int J Colorectal Dis 2019;34:47–54. [DOI] [PubMed] [Google Scholar]
- 30.D'Souza G, Wiley DJ, Li X, et al. Incidence and epidemiology of anal cancer in the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr 2008;48:491–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pan J, Kavanagh K, Cuschieri K, et al. Increased risk of HPV-associated genital cancers in men and women as a consequence of pre-invasive disease. Int J Cancer 2019;145:427–34. [DOI] [PubMed] [Google Scholar]
- 32.Nowak RG, Gravitt PE, He X, et al. Prevalence of anal high-risk human papillomavirus infections among HIV-positive and HIV-negative men who have sex with men in Nigeria. Sex Transm Dis 2016;43:243–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cranston RD, Carballo-Dieguez A, Gundacker H, et al. Prevalence and determinants of anal human papillomavirus infection in men who have sex with men and transgender women. Int J STD AIDS 2019;30:154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nigro ND, Vaitkevicius VK, Considine B., Jr Combined therapy for cancer of the anal canal: a preliminary report. Dis Colon Rectum 1974;17:354–6. [DOI] [PubMed] [Google Scholar]
- 35.Benson AB, Venook AP, Al-Hawary MM, et al. Anal Carcinoma, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2018;16:852–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ortholan C, Ramaioli A, Peiffert D, et al. Anal canal carcinoma: Early-stage tumors ≤10 mm (T1 or Tis): therapeutic options and original pattern of local failure after radiotherapy. Int J Radiat Oncol Biol Physics 2005;62:479–85. [DOI] [PubMed] [Google Scholar]
- 37.Alfa-Wali M, Dalla Pria A, Nelson M, et al. Surgical excision alone for stage T1 anal verge cancers in people living with HIV. Eur J Surg Oncol 2016;42:813–6. [DOI] [PubMed] [Google Scholar]
- 38.Nensi A, Chande N. A survey of digital rectal examination training in Canadian medical schools. Can J Gastroenterol 2012;26:441–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ong J, Chen M, Temple-Smith M, et al. The inside story. Physicians' views on digital ano-rectal examination for anal cancer screening of HIV positive men who have sex with men. J Med Screen 2013;20:188–91. [DOI] [PubMed] [Google Scholar]
- 40.Alkire BC, Raykar NP, Shrime MG, et al. Global access to surgical care: a modelling study. Lancet Glob Health 2015;3:e316–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zubizarreta EH, Fidarova E, Healy B, et al. Need for radiotherapy in low and middle income countries - the silent crisis continues. Clin Oncol 2015;27:107–14. [DOI] [PubMed] [Google Scholar]
- 42.Read TR, Huson KL, Millar JL, et al. Size of anal squamous cell carcinomas at diagnosis: a retrospective case series. Int J STD AIDS 2013;24:879–82. [DOI] [PubMed] [Google Scholar]
- 43.Berry JM, Jay N, Cranston RD, et al. Progression of anal high-grade squamous intraepithelial lesions to invasive anal cancer among HIV-infected men who have sex with men. Int J Cancer 2014;134:1147–55. [DOI] [PubMed] [Google Scholar]
- 44.Ong JJ, Walker S, Grulich A, et al. Incorporating digital anorectal examinations for anal cancer screening into routine HIV care for men who have sex with men living with HIV: a prospective cohort study. J Int AIDS Soc 2018;21:e25192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Davis TW, Goldstone SE, Chen G. Tolerability of anal dysplasia screening. J Low Genit Tract Dis 2013;17:404–8. [DOI] [PubMed] [Google Scholar]
- 46.Ong JJ, Temple-Smith M, Chen M, et al. Why are we not screening for anal cancer routinely - HIV physicians' perspectives on anal cancer and its screening in HIV-positive men who have sex with men: a qualitative study. BMC Public Health 2015;15:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee DJ, Consedine NS, Spencer BA. Barriers and facilitators to digital rectal examination screening among African-American and African-Caribbean men. Urology 2011;77:891–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ouhoummane N, Steben M, Coutlee F, et al. Squamous anal cancer: patient characteristics and HPV type distribution. Cancer Epidemiol 2013;37:807–12. [DOI] [PubMed] [Google Scholar]
- 49.Jin F, Vajdic CM, Law M, et al. Incidence and time trends of anal cancer among people living with HIV in Australia. AIDS 2019;33:1361–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ong JJ, Fairley CK, Carroll S, et al. Cost-effectiveness of screening for anal cancer using regular digital ano-rectal examinations in men who have sex with men living with HIV. J Int AIDS Soc 2016;19:20514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wright JL, Patil SM, Temple LK, et al. Squamous cell carcinoma of the anal canal: Patterns and predictors of failure and implications for intensity-modulated radiation treatment planning. Int J Radiat Oncol Biol Phys 2010;78:1064–72. [DOI] [PubMed] [Google Scholar]
- 52.Moscicki AB, Darragh TM, Berry-Lawhorn JM, et al. Screening for anal cancer in women. J Low Genit Tract Dis 2015;19(3 suppl 1):S27–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Institute of Medicine. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Acadamies Press; 2011. [PubMed] [Google Scholar]


