Abstract
Background:
It is unclear whether the sacroiliac joint is vulnerable to adjacent segment disease. Clinical studies have suggested that many patients who have undergone lumbar arthrodesis will develop adjacent segment disease, which may contribute to sacroiliac joint degeneration. The purpose of the present study was to examine whether arthrodesis in the lumbar spine results in altered biomechanics at the sacroiliac joint that could contribute to adjacent segment disease within the joint.
Methods:
With use of human cadavers in a biomechanical laboratory study, the effects of lower-lumbar arthrodesis and sacroiliac screws on the biomechanics of the sacroiliac joint were assessed. Human cadaveric pelves with lumbar spines were biomechanically tested in flexion-extension, rotation about the vertical axis, and compression along the vertical axis with single and double-leg support. Four conditions were compared: (1) intact, (2) L4-L5 arthrodesis, (3) L4-S1 arthrodesis, and (4) left sacroiliac screw. Construct vertical and horizontal motions at the anterior and posterior surfaces of the sacroiliac joint were measured.
Results:
Significant measurable increases in motion of the sacroiliac joint related to arthrodesis of the lumbar spine occurred with flexion-extension loading (p < 0.05). No significant changes were observed for rotation about the vertical axis or compression along the vertical axis with single and double-leg support.
Conclusions:
After 360°, 1 or 2-level lumbosacral spine arthrodesis, the sacroiliac joint showed a significant increase in rotational motion with flexion-extension loading. Increases in horizontal translation with axial rotation loading and vertical translation with axial compression loading were not significant.
Clinical Relevance:
The risk of significant alteration of normal sacroiliac kinematics should be considered in all patients undergoing 360° lumbosacral arthrodesis.
Biomechanical studies have suggested that arthrodesis of the lumbar spine transfers forces to adjacent joints, causing mechanical changes that may create stress and result in pain and reduced spinal function1,2. Clinical studies have suggested that symptomatic adjacent segment disease develops in many patients who undergo lumbar or lumbosacral arthrodesis3, and other research has implicated the sacroiliac joint as a source of chronic lower back pain in 13% to 30% of patients who have undergone these procedures4. Few studies have directly addressed the relationship between distal adjacent segment disease and the sacroiliac joint as a potential cause of pain in lumbar spine arthrodesis. This study examines whether arthrodesis in the lumbar spine results in altered biomechanics at the sacroiliac joint that could contribute to adjacent segment disease in the sacroiliac joint.
Materials and Methods
Specimens
Ten fresh-frozen cadaveric pelves with lumbosacral spines (L4 to the sacrum) were harvested and denuded, preserving the iliolumbar, sacrotuberous, and sacrospinous ligaments. Radiographs of the pelves were made in order to rule out anatomic abnormalities. The specimens were harvested from 5 male and 5 female patients with an average age (and standard deviation) of 56.8 ± 7.6 years old.
Setup
Sawbones femora (Pacific Research Laboratories) were transected at the distal aspect of the diaphysis, and the proximal aspect of the femora were potted in polymethylmethacrylate and gripped in an angle vise with the diaphysis at 9° of varus and the neck at 15° of anteversion. The femora were then fixed to the pelvis at the hip joints, and a plumb line was utilized to align the center of L4 to the center of rotation of the hip joints in the sagittal plane. The fit of the femoral head was not critical because the hip joints were locked in the above alignment to prevent forward or backward flexion of the whole pelvis and lumbar spine, which could have occurred as with flexion-extension loading of the lumbar spine. The vise on the right side of the pelvis moved on linear bearings to accommodate for elastic changes within the pelvis on loading (Figs. 1-A and 1-B).
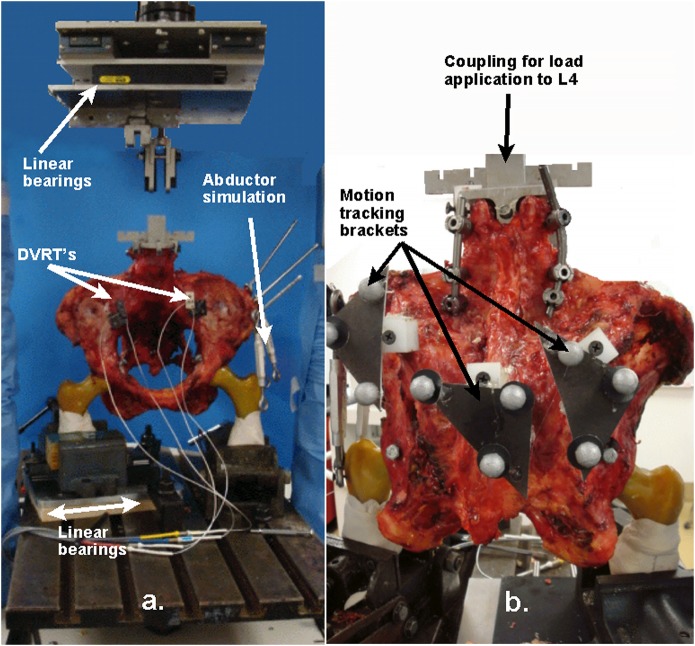
Fig. 1.
Photographs of the pelvis and lumbar spine showing the location of transducers, movement-tracking hardware, and the linear bearing sandwich (Fig. 1-A), and universal joint coupling to the MTS machine. DVRT = differential variable reluctance transducer (Fig. 1-B).
Across the anterior surface of each sacroiliac joint, at approximately the apex of the convex surface of the joint, 2 MicroStrain (LORD Sensing Systems) differential variable reluctance transducers (9 mm excursion, 4.5 µm accuracy) were aligned to measure the vertical and horizontal translations across each joint (Figs. 1-A and 1-B; Appendix A1). Brackets with 3 reflectors of the MaxPro 3-D motion analysis system (Innovision-Systems) were mounted posteriorly to track translation between the sacrum and both ilia.
All measures of each construct were assessed in the same sequence in each specimen. Each construct measure was normalized to the intact value for the same parameter. Statistical comparisons were made between each construct and the intact value with use of paired Student t tests with the Bonferroni correction for multiple comparisons. Significance was set at p = 0.05.
Loading
A loading fixture on the superior end plate of L4 was aligned to ensure that the vertical compression loads and rotations about the vertical axis would be in line with the gravity load line of the lumbar spine. Turnbuckles were attached to the iliac crest and the proximal aspect of the femur near the greater trochanter on the left side of the pelvis to simulate the abductor loads in single-leg loading. Although the hip joints were locked, the elasticity of the pelvic ring allowed for adduction between the femur and pelvis. We believed this was more of a natural construct, wherein abductor forces helped support the pelvis.
Four modes of loading—flexion-extension (Fig. 2), compression along the vertical axis in single and double-leg support, and rotation about the vertical axis (axial rotation)—were applied with use of the MTS 858 Mini Bionix II (MTS Systems Corporation). All loads, torques, vertical displacements, and rotations of the MTS load cell and ram were recorded and synchronized with all other measures during testing.
Fig. 2.
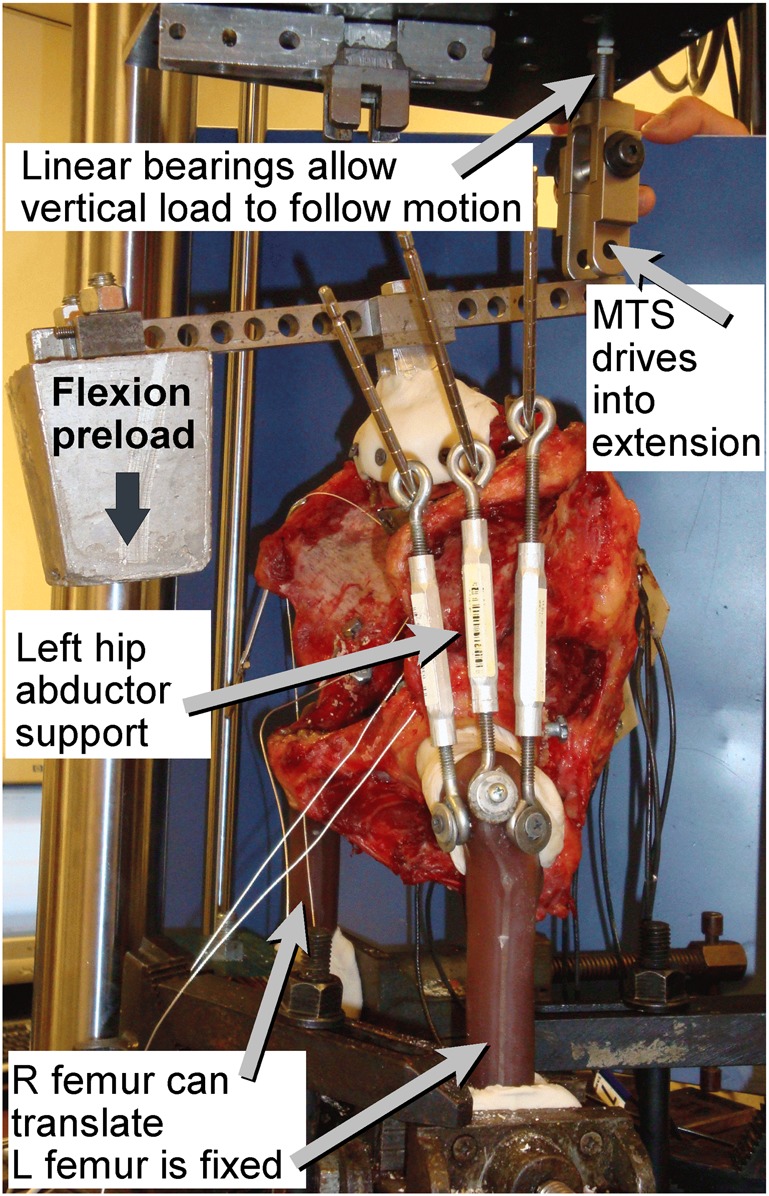
Schematic diagram of the flexion-extension test setup. A passive 60-N preload was applied to the load arm mounted on the superior surface of L4 at 14.2 cm from the center of L4. This created an 8.5-Nm flexion moment to the lumbar spine at L4 when the MTS load was zero. Next, a compression load from the MTS ram was applied to the posterior lever arm to move the spine into extension and generate an 8.5-Nm extension moment at L4. The linear bearings on the MTS ram assured that, as the spinopelvic specimen moved from a position of flexion to extension, the vertical load followed the motion and did not create any side loads.
The constructs were cyclically loaded at 0.25 Hz with the MTS to ±8.5 Nm in flexion-extension with the lever arms in load control (Fig. 2). The static preload of 60 N, applied at 14.2 cm anterior to the center of L4, created an 8.5 Nm flexion moment. The MTS ram applied a load to the lever arm at 10 cm posterior to the center of L4 to create an extension moment to first overcome the flexion preload moment (at 85 N) and then create a net extension moment of 8.5 Nm when the cycle peaked at 170 N. In this way, the vertical compression load that creates the flexion and extension moments also followed the motion of the spine and center of gravity as the spine flexes and extends.
The lever arms were replaced by a universal joint to apply the ±7.5 Nm in torsion (axial rotation) under load control. In double-leg support, L4 was loaded in compression through a universal joint and cycled at 0.25 Hz under stroke control. Loads were cycled from 150 to 1,500 N for male specimens and 100 to 1,000 N for female specimens. In single-leg support, the support was removed from the right femur and load was applied directly to L4 through the universal joint. The load was cycled from 60 to 600 N for male specimens and 40 to 400 N for female specimens. These load levels produced measurable movements that did not threaten mechanical failure of the specimens. X-Y linear bearings were attached to the crosshead of the MTS during all testing parameters to allow for free horizontal translation in the anteroposterior and mediolateral planes and to eliminate shear loads from the MTS ram. An 8.5-Nm preload was applied to the test specimen in flexion to induce proper coupled flexion-extension motion by placing a 60-N weight on a lever arm attached to L4. A clevis joint, secured to the X-Y roller plates, was attached to the extension end of the lever arm. A vertical compression load was applied to the extension lever arm to drive the construct from full flexion to full extension. The flexion-extension test setup is depicted in Figure 2. The level of load for each simulation was chosen to provide a safe, but large enough, load to create measurable movements at the sacroiliac joints. The normal loading of the sacroiliac joint is not well understood, but vertical compression loads of 1,000 N or more are expected5.
Surgical Interventions
Four constructs were simulated in each specimen: (1) intact, (2) 360° (anterior and posterior) instrumented L4-L5 arthrodesis, (3) the addition of a 360° instrumented lumbosacral L4-S1 arthrodesis, and (4) the addition of unilateral screw fixation across the left sacroiliac joint. The posterior arthrodeses were simulated by 4 pedicle screws and two 5.5-mm titanium rods. The lumbar arthrodeses were simulated by replacing the disc at the motion segment unit with an anterior lumbar interbody arthrodesis cage with screw fixation into the superior and inferior end plates of the motion segment union and an anterior bone plate to span the motion segment union.
Results
All intact specimens in this study demonstrated motion at the sacroiliac joints, albeit with high variability between specimens. Horizontal movements measured posteriorly ranged from 0.001 to 0.38 mm in the mediolateral plane, from 0.22 to 1.96 mm in the anteroposterior plane, and from 0.21 to 1.63 mm in the vertical plane. In general, female specimens displayed greater motion at the sacroiliac joints. The ratio of measures between right and left sacroiliac joints in the same pelvis ranged from 0.02 to 5.95, but most right-versus-left sacroiliac joint comparisons in a given pelvis were quite similar. Because of this wide variation in absolute measures between specimens, only the relative changes with each intervention for each individual measure were meaningful and able to be compared statistically.
Flexion-Extension Loading
The MTS load-deflection curves had a definable neutral zone of motion with minimal resistance. Motion of the individual joints was not measured, so a description of flexion-extension stiffness was not meaningful. The neutral zone decreased progressively after each additional level of arthrodesis and after adding the screw across the left sacroiliac joint. These changes were significant for all levels of arthrodesis and for the sacroiliac screw when paired with the neutral-zone measures of the intact specimens (Fig. 3). Examples of load-displacement measures are given in the Appendix (Figs. A-2 through A-4).
Fig. 3.
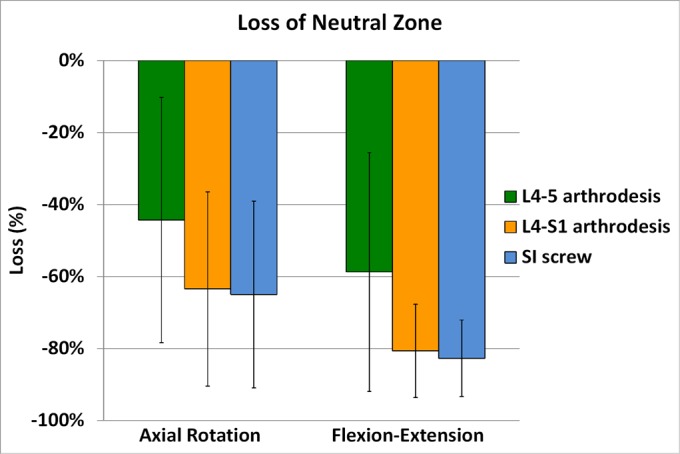
Graph showing mean and standard deviation of the relative change in the neutral zone compared with the intact measures related to each of the interventions. The neutral zone for flexion-extension loading of the whole construct, as expected, changed significantly with increases in levels of arthrodesis of the lumbar spine. SI = sacroiliac.
The relative vertical motion between the sacrum and ilium measured posteriorly averaged 0.61 ± 0.39 mm for the intact spinopelvic specimens, 0.78 ± 0.49 mm after fusing the L4-L5 motion segment unit, 0.90 ± 0.54 mm after adding the L5-S1 motion segment unit to the arthrodesis, and finally 0.92 ± 0.62 mm at the right sacroiliac joint and 0.83 ± 0.49 mm at the left sacroiliac joint after adding the screw across the left sacroiliac joint. Vertical motion on the anterior side averaged 0.078 ± 0.089 mm for the intact spinopelvic specimens, 0.096 ± 0.131 mm after fusing the L4-L5 motion segment unit, 0.099 ± 0.141 mm after adding the L5-S1 motion segment unit to the arthrodesis, and finally 0.101 ± 0.186 mm at the right sacroiliac joint and 0.053 ± 0.057 mm at the left sacroiliac joint after adding the screw across the left sacroiliac joint. The posterior vertical motions were in the opposite direction from the anterior motions, indicating that the sacroiliac joint was rotating with flexion-extension loading.
None of these absolute measures were significantly different because of the variability of the specimens; however, the percent increase in each measure as a result of arthrodesis was significantly different for flexion-extension loading (Fig. 4). The addition of the screw to the left sacroiliac joint reduced vertical motion on that joint, but the unfixed right side increased and was quite variable.
Fig. 4.
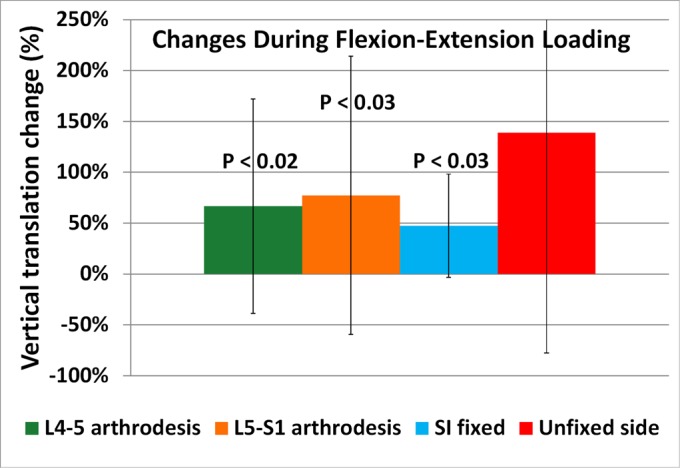
Graph showing the mean and standard deviation of the change in vertical translations measured at the sacroiliac joints created by the increase in each level of arthrodesis of the lumbar spine during flexion-extension loading. The change in vertical translation at the right sacroiliac joint before and after the left sacroiliac joint was fixed with a screw is labeled “unfixed side.” SI = sacroiliac.
Vertical Axis Loading of All Types
All axial compression loading (double and single-leg support) vertical translations were within the same range (0.4 to 0.6 mm), and none were significantly affected by lumbar arthrodesis. Horizontal motions were significantly less than vertical and were not significant. Examples of measures are in the Appendix (Figs. A5 and A6). Similarly, rotational loading created horizontal motions within the same range (0.4 to 0.6 mm), and none were significantly affected by lumbar arthrodesis. Examples of measures are in the Appendix (Figs. A7 through A9).
Discussion
Froning and Frohman were the first to suggest sacroiliac joint involvement in patients with persistent lumbar pain following successful surgical procedures in the lumbar spine2; however, they were unable to confirm that hypothesis with radiographs. They and other investigators found that sacroiliac joint dysfunction with persistent, unresponsive pain following lumbar arthrodesis could be documented by computed tomography (CT) imaging and bone scintigraphy, which demonstrated increased uptake in the sacroiliac joint in symptomatic patients5,6. In a study utilizing an analytical lumbar spinopelvic model to assess the motion and stress on the sacroiliac joint as a function of lumbar arthrodesis, Ivanov et al.7 showed increased motion at the sacroiliac joint with lumbar arthrodesis, which may account for pain in patients who undergo that procedure. In a study in which 34 symptomatic patients with a prior lumbar arthrodesis received a sacroiliac joint injection, Katz et al. hypothesized the pain was related to the arthrodesis8.
In a study using CT imaging preoperatively and at 1 and 5 years postoperatively, Ha et al. found that sacroiliac joint degeneration correlated with instrumented posterolateral lumbar arthrodesis9. The incidence of sacroiliac degeneration in the arthrodesis group was 75% compared with 38.2% in a comparably sized, age-matched control group.
In the present study, there was a well-defined neutral zone for the entire construct with flexion-extension and axial-rotation loading, reflecting the relatively large movements of the lumbar spine compared with the limited motion measured at the sacroiliac joints. For axial compression loading, the motion segments had minimal movement, and there were no clear neutral-zone measures for the entire construct; thus, axial compression loading, with or without lumbar arthrodesis, transmitted the compression to the sacroiliac joint. With flexion-extension loading, the motion of the lumbar spine was altered, creating significant changes in measures of sacroiliac motion (p < 0.05). Because flexion loading specifically creates increased loading on the spine as a result of the anterior shift of the center of mass of the upper body, altering spinal motion could have effects on the adjacent segment sacroiliac joint.
The intact sacroiliac joint sagittal plane rotation during lumbosacral spine flexion-extension testing observed in the present study corroborates the descriptions made by Kapandji (as nutation and counter-nutation, similar to a nodding head)10, and further supports the current belief that normal sacroiliac joint motion between the sacrum and ilium consists of a rotational movement in the sagittal plane. During axial compression testing (double and single-leg stance), sacroiliac joint motion was predominantly translational, or shearing, within the vertical plane and without evidence of rotation. Torsion testing likewise resulted in predominantly translational motion, although in the coronal plane.
Although a few studies have suggested an association between lumbosacral arthrodesis and possible adjacent segment disease extending to the sacroiliac joint, the present study is the first, to our knowledge, to provide biomechanical substantiation7-9. The results of this study demonstrate progressively increasing motion across the sacroiliac joint with lumbosacral arthrodesis constructs. Sacroiliac joint vertical translational motion during flexion-extension loading increased 67% with L4-L5 instrumentation and 77% with L4-S1 instrumentation. Similar to the complications of proximal adjacent segment disease typically associated with a lumbar spine arthrodesis, the adjacent distal motion segment unit following lumbosacral arthrodesis is the sacroiliac joint, and the increased motion transferred to the adjacent sacroiliac joint secondary to lumbosacral arthrodesis may accelerate sacroiliac joint degeneration and, subsequently, pain generator transformation3,11-17.
There were several limitations to this study. Firstly, the pelves and associated sacroiliac joints represented a broad variation in geometry and size, and this dissimilarity may have resulted in variable motion between intact specimens. To address this, measurements made prior to arthrodesis or screwing served as control values for each respective specimen. The differential variable reluctance transducers were placed at the anterior surface of the sacroiliac joint so that the linear measures were fairly close to the theoretical center of rotation of the joint, but the brackets for the tracking system were placed on the most posterior extensions of the iliac wing and the sacral spinous processes. Thus, the movements measured by the camera system were further away from the theoretical center of rotation of the sacroiliac joint. Those measures may have been magnified compared with the differential variable reluctance transducers measures when the sacroiliac joint was rotating. For this reason, the measures of both systems were in the same direction and of similar magnitude when the sacroiliac joint moved in vertical shearing motion, but in flexion-extension loading, as the sacroiliac rotated, the posterior measures were greater in magnitude and in the opposite direction to the anterior measures.
The loading of the pelvis and the sacroiliac joints is very complex and is influenced by many muscles in multiple directions, exerting forces over large osseous areas that are quite compliant, as well as abdominal pressure5. The model utilized in the present study did not attempt to replicate this complexity; we only attempted to apply the simple external loads. The loading in flexion-extension could only control the moments applied to the L4 vertebral body. It was impossible to measure the moments created at the sacroiliac joint itself. However, as the lumbar spine moves from flexion to extension, the center of gravity also moves from anterior to posterior, as did the vertical load on the MTS ram. Although imperfect, this movement of the vertical load was similar to normal loading. The loading through the hip joints was also compromised in order to stabilize the pelvis during loading, but the position of the hip joints was allowed to adjust to the elasticity of the pelvic ring to prevent side loading as the pelvis expanded under load. Additionally, because interspecimen variability forced us to measure the relative change in each measure after each intervention, it is possible that some of the changes were related to the length of time it took to go through each of the interventions and loading regimens.
With axial compression loading, minimal rotation was noted at the sacroiliac joints, so those translations reported for the brackets better reflected the true translations of the sacroiliac joint. Lastly, this study evaluated only the motion changes of the sacroiliac joint associated with lumbosacral arthrodesis, warranting more in-depth analysis to correlate these alterations in sacroiliac joint motion with radiographic and clinical outcomes. The interspecimen differences in reaction to the surgical interventions may also hold important information clinically and could be addressed in further studies.
In conclusion, following 360°, 1 or 2-level lumbosacral spine arthrodesis, the sacroiliac joint experienced an increase in motion during flexion-extension loading, but not in axial loading, in this laboratory model.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A140).
Footnotes
Investigation performed at the Max Biedermann Institute for Biomechanics, Mount Sinai Medical Center, Miami Beach, Florida
Disclosure: The authors indicated that no external fundissssng was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a patent and/or copyright, planned, pending, or issued, broadly relevant to this work and “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (http://links.lww.com/JBJSOA/A139).
References
- 1.Dreyfuss P, Dreyer SJ, Cole A, Mayo K. Sacroiliac joint pain. J Am Acad Orthop Surg. 2004. Jul-Aug;12(4):255-65. [DOI] [PubMed] [Google Scholar]
- 2.Froning EC, Frohman B. Motion of the lumbosacral spine after laminectomy and spine fusion. Correlation of motion with the result. J Bone Joint Surg Am. 1968. July;50(5):897-918. [PubMed] [Google Scholar]
- 3.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004. September1;29(17):1938-44. [DOI] [PubMed] [Google Scholar]
- 4.Buchowski JM, Kebaish KM, Sinkov V, Cohen DB, Sieber AN, Kostuik JP. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J. 2005. Sep-Oct;5(5):520-8; discussion 529. [DOI] [PubMed] [Google Scholar]
- 5.Gates GF, McDonald RJ. Bone SPECT of the back after lumbar surgery. Clin Nucl Med. 1999. June;24(6):395-403. [DOI] [PubMed] [Google Scholar]
- 6.Onsel C, Collier BD, Kir KM, Larson SJ, Meyer GA, Krasnow AZ, Isitman AT, Hellman RS, Carrera GF. Increased sacroiliac joint uptake after lumbar fusion and/or laminectomy. Clin Nucl Med. 1992. April;17(4):283-7. [DOI] [PubMed] [Google Scholar]
- 7.Ivanov AA, Kiapour A, Ebraheim NA, Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine (Phila Pa 1976). 2009. March 1;34(5):E162-9. [DOI] [PubMed] [Google Scholar]
- 8.Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech. 2003. February;16(1):96-9. [DOI] [PubMed] [Google Scholar]
- 9.Ha KY, Lee JS, Kim KW. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine (Phila Pa 1976). 2008. May 15;33(11):1192-8. [DOI] [PubMed] [Google Scholar]
- 10.Kapandji IA. The physiology of the joints. Vol. 3 The trunk and the vertebral column. New York: Churchill Livingstone; 1982. [Google Scholar]
- 11.White AA, Panjabi MM. Clinical biomechanics of the spine. 2nd ed. Philadelphia: Lippincott; 1990. [Google Scholar]
- 12.Lee CK, Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine (Phila Pa 1976). 1984. September;9(6):574-81. [DOI] [PubMed] [Google Scholar]
- 13.Ha KY, Schendel MJ, Lewis JL, Ogilvie JW. Effect of immobilization and configuration on lumbar adjacent-segment biomechanics. J Spinal Disord. 1993. April;6(2):99-105. [PubMed] [Google Scholar]
- 14.Bastian L, Lange U, Knop C, Tusch G, Blauth M. Evaluation of the mobility of adjacent segments after posterior thoracolumbar fixation: a biomechanical study. Eur Spine J. 2001. August;10(4):295-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Esses SI, Doherty BJ, Crawford MJ, Dreyzin V. Kinematic evaluation of lumbar fusion techniques. Spine (Phila Pa 1976). 1996. March 15;21(6):676-84. [DOI] [PubMed] [Google Scholar]
- 16.Nagata H, Schendel MJ, Transfeldt EE, Lewis JL. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine (Phila Pa 1976). 1993. December;18(16):2471-9. [DOI] [PubMed] [Google Scholar]
- 17.Dekutoski MB, Schendel MJ, Ogilvie JW, Olsewski JM, Wallace LJ, Lewis JL. Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine (Phila Pa 1976). 1994. August 1;19(15):1745-51. [DOI] [PubMed] [Google Scholar]