Abstract
Background:
Fractures of the distal third of the humeral shaft remain a challenge today. Plate osteosynthesis is the most commonly used method of treatment. Current minimally invasive plate osteosynthesis (MIPO) techniques applied to the distal part of the humerus have shown a high risk of radial nerve injury, and they are unable to adequately fix distal-most fractures. Our hypothesis was that using a new MIPO approach, distal humeral shaft fractures can be safely fixed. The aim of this study was to develop this new anteromedial-distal MIPO approach.
Methods:
We conducted a laboratory descriptive study using 16 arms from adult human specimens. A new anteromedial-distal MIPO approach, starting distally through a small window in the pronator teres muscle, was developed. A premolded plate was introduced in the anterior side of the medial epicondylar area, through the anterior face of the humerus, up to the proximal part of the humeral shaft. Several anatomical parameters were measured on dissection to define the distances of the plate and screws to the neurovascular structures that could be at risk.
Results:
The radial nerve was not at risk because of its pathway through the posterior and lateral aspects of the arm. The mean distance from the most distal border of the medial epicondyle to the proximal border of the coronoid fossa was 3.36 cm (95% confidence interval [CI], 3.23 to 3.50 cm). At least 3 screws could be inserted in all specimens in this area and up to 5 when the fixation area was extended 2 cm proximally. The mean width of the medial epicondylar area was 2.19 cm (95% CI, 2.03 to 2.33 cm), space enough for the distal fixation of the plate. The ulnar nerve was at risk only from the tip of the most distal screw (mean distance of 2.50 mm; 95% CI, 1.60 to 3.40 mm) in specimens with a very narrow medial epicondylar area.
Conclusions:
This approach provides adequate fixation for distal humeral shaft fractures, but proper clinical studies must be undertaken.
Clinical Relevance:
This new approach avoids the risk of radial nerve injury.
The treatment of distal-third humeral shaft fractures remains a challenge. When they are treated nonoperatively, high rates of angular deformities have been reported, >10° in 47%1 of cases. Nonoperative treatment may also lead to rigidity of the adjacent joints, and the predictability of the outcome is low. Internal fixation with plating is the method of treatment preferred by most surgeons2,3. Surgical treatment (plate osteosynthesis) is difficult. Posterior open approaches are most frequently used, but a relatively high rate of pseudarthrosis has been reported4. Some authors have used a lateral open approach, but a high rate of radial nerve palsy has been reported5.
Minimally invasive plate osteosynthesis (MIPO) has been used as an alternative method, with good results6,7. Nevertheless, current MIPO techniques are not suitable for treating distal shaft fractures because they risk radial nerve injury and they cannot adequately fix distal-most shaft fractures8.
Our hypothesis was that distal-third humeral shaft fractures can be internally fixed using a minimally invasive, anteromedial-distal approach without risk of injury to the radial nerve. The aim of this study was to develop this new approach. We describe the approach, show the relationship of neurovascular structures and the plate using the approach, and evaluate the ability to stabilize distal-most shaft fractures using a single plate.
Materials and Methods
The study was performed using 16 arms from fresh adult human specimens (8 right and 8 left, nonpaired) at the laboratory of the University of Granada in Spain. Two of the specimens were used to plan and design the technique, and the other 14 were used to perform measurements. Specimens were donated to the university, and we obtained authorization to perform the dissection from our institutional review board.
Before performing the surgical technique, two 15-hole extra-articular elbow locking compression plates (LCPs) (Extra-Articular Distal Humerus Plate [EADHP]; DePuy Synthes-Johnson & Johnson) were molded using 2 intact humerus bones from other arm specimens (1 left and 1 right) without fracture or deformity. The plate was molded with 2 forceps between the fourth and fifth most distal screws, with its posterior curve inverted slightly at the distal zone. Care was taken not to affect the distal holes of the LCP in order to preserve their characteristics. As the plate works as an internal fixator, a perfect assembly of the plate to the bone was not necessary. The molding of the plate was performed to achieve an adequate fit of the plate to an alternate anatomical area, the anterior side of the medial epicondylar area.
To develop the approach and to define the exact entry point of the new anteromedial-distal approach, 1 right arm specimen (not included in the measurements) was meticulously dissected. The pronator teres and its insertion in the medial epicondyle (humeral head) were identified and represented the most important structures to identify with the approach. An incision starting 1 cm laterally from the medial border of the medial epicondyle and extending distally 2.5 cm along the anatomical direction of the pronator teres muscular fibers was performed. Posteriorly, the premolded plate was introduced from distal to proximal and fixed distally (Fig. 1). Proximally, the plate was fixed using the anterior MIPO approach, which has been previously described6,7.
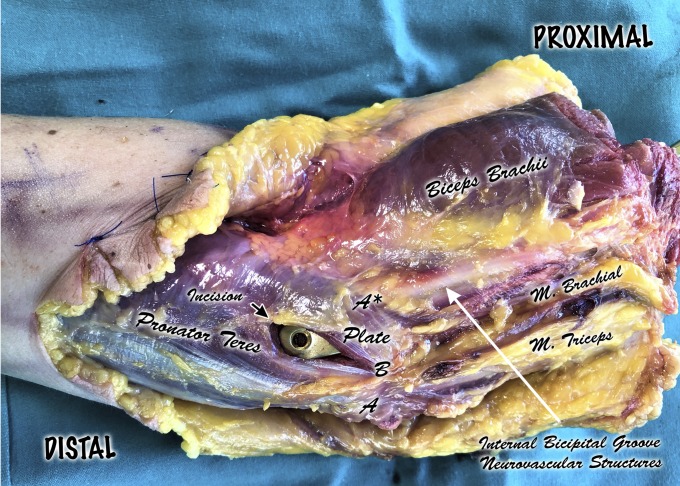
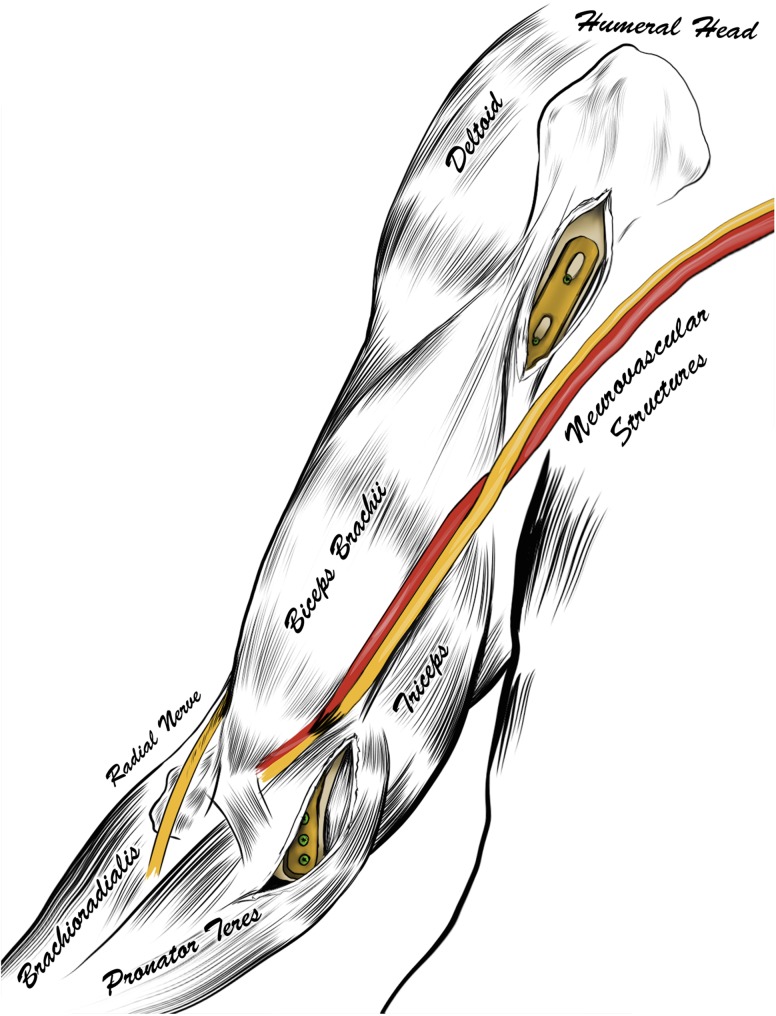
Fig. 1.
Dissection of the distal part of the right arm and elbow (semilateral view). A = apex of medial epicondyle, and A* = median nerve. Neurovascular structures run along the internal bicipital groove lying over the brachialis muscle and lateral to the pronator teres muscle belly. A to A* = the distance between the apex of the medial epicondyle and the median nerve. B = proximal tip of the incision, starting 1 cm lateral to the tip of the medial epicondyle and following its fibers distally for 2.5 cm. B to A* = the distance between the proximal tip of the muscular incision and the median nerve. A thick layer of pronator teres muscle belly was left laterally, protecting the neurovascular structures.
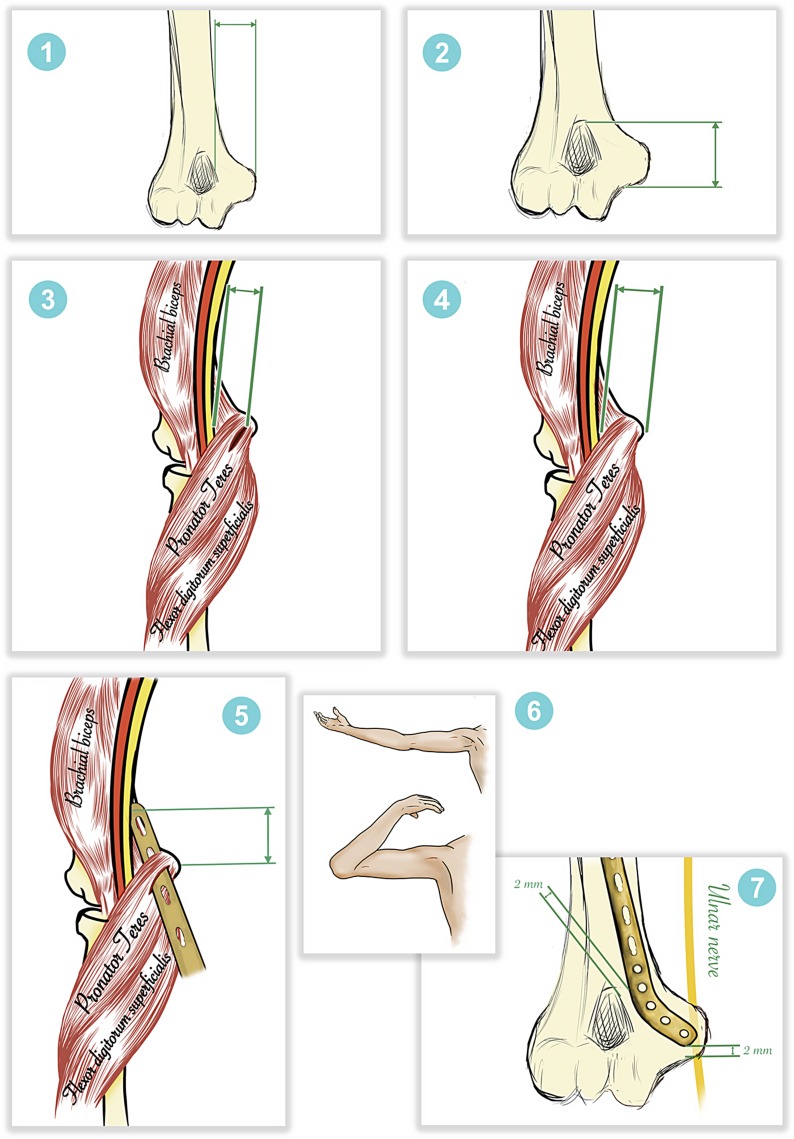
To verify the possibility of using a temporary external fixator to carry out the fracture reduction prior to fixation, if required, an anatomical model of a left humerus with a distal shaft fracture was used (Fig. 2). Posteriorly, this was also performed in another left arm specimen with a distal-third fracture in order to verify the feasibility of the approach in a humerus with a displaced fracture. Satisfactory reduction was observed under direct vision through a wide posterior approach, but we recognize that this would normally be carried out during surgery using image-intensifier control. Finally, the plate was introduced and fixed as described above, without major modifications of the technique.
Fig. 2.

Anatomical model of a left humerus with a distal shaft fracture, used to verify the possibility of using an external fixator to reduce the fracture. Two pins were introduced distally, 1 of them into the lateral center of the capitellum and the other, just above the coronoid fossa through a small incision very close to the external border of the biceps tendon. Another 2 pins were introduced proximally in the anterolateral zone.
Surgical Technique
The procedure was then carried out on 14 arm specimens in the supine position. The new approach was performed distally. The medial epicondyle was manually located. The incision was made halfway between the inner portion of the biceps tendon and the apex of the medial epicondyle. The incision began 3 cm proximal to the elbow flexion crease and extended distally another 3 cm (Fig. 3). After the skin incision was made, the medial antebrachial cutaneous nerve was identified and retracted medially, and the basilic vein was also identified and retracted laterally. Then, the proximal portion of the pronator teres belly was exposed, and the muscular incision was performed as described above to access the flat anterior portion of the medial epicondyle, where the distal part of the plate is to be fixed (Fig. 4).
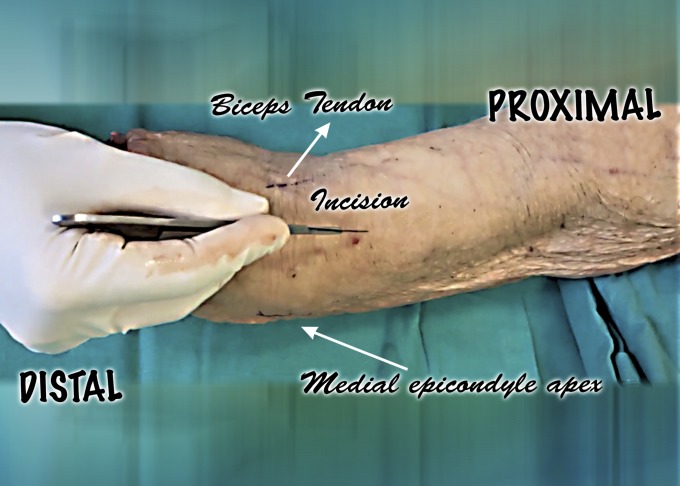
Fig. 3.
Location of the skin incision in the distal part of the right arm (frontal view). Note the relationship of the incision to the apex of the medial epicondyle and the biceps tendon.
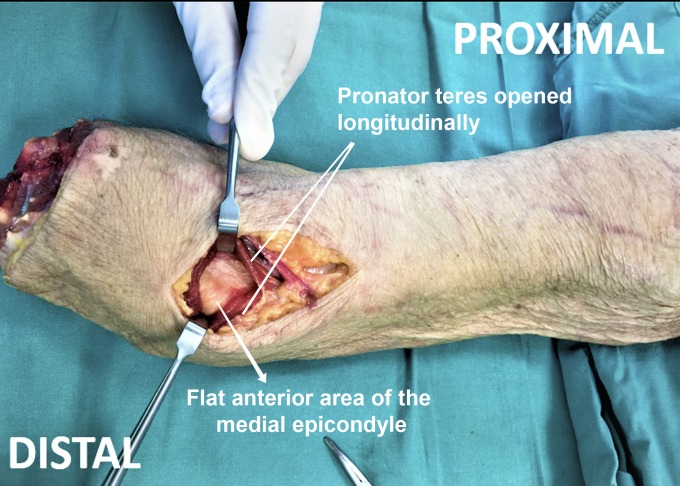
Fig. 4.
Frontal view of a right arm specimen, showing the distal approach. A 6-cm skin incision has been performed between the inner portion of the biceps tendon and the apex of the medial epicondyle. The medial antebrachial cutaneous nerve and the basilic vein have been retracted (not shown). The pronator teres muscle is then longitudinally dissected to access the anterior flat area of the medial epicondyle.
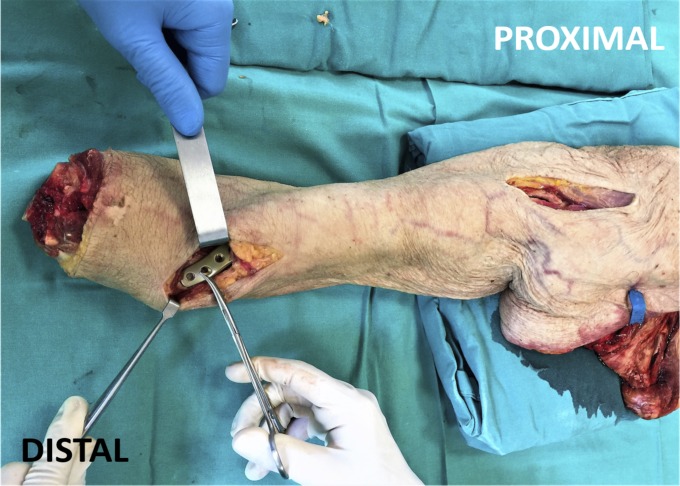
The plate was introduced from distal to proximal (Figs. 5 and 6) through the anterior face of the humerus, up to the proximal part of the humeral shaft. Distally, it was positioned 2 mm away from the medial border of the coronoid fossa. A distance of 2 mm was left from the distal border of the plate to the medial epicondyle. Five distal screws were inserted through the same distal approach under direct vision, and 3 screws were inserted through the proximal incision, in the usual MIPO way, as previously reported6,7. Small modifications to the shape of the plate were made for some arms.
Fig. 5.
Right arm specimen showing the final position of the plate and both proximal and distal MIPO approaches.
Fig. 6.
Illustration of Figure 5 showing the approach and relationship to the main neurovascular structures of the arm.
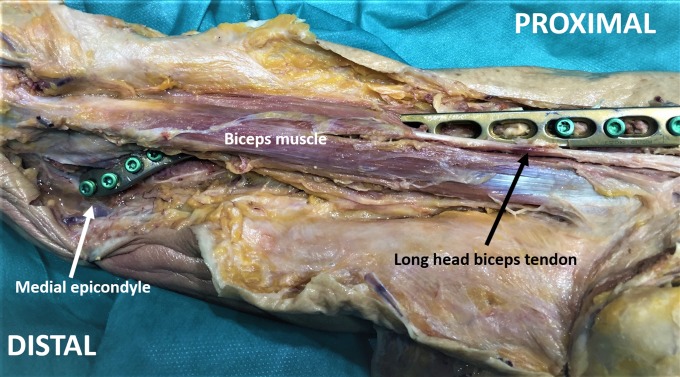
On complete dissection of the arm specimen, it was observed that the proximal portion of the plate was fixed lateral to the long head of the biceps tendon (Fig. 7). The plate did not interfere at any location with the radial nerve pathway; however, in some arm specimens, the plate approximated the long head of the biceps tendon (Fig. 8).
Fig. 7.
Right arm specimen completely dissected after the final assembly of the plate. It is observed that the proximal portion of the plate was fixed with 3 LCP screws lateral to the long head of the biceps tendon. Distally, 4 LCP screws were introduced.
Fig. 8.
Deep dissection of a right arm specimen after the procedure. The biceps muscle is retracted medially to show that the plate does not interfere with the radial nerve pathway. Proximally, it is observed that the plate approximates the long head of the biceps tendon.
Data Analysis
Several anatomical parameters were measured during dissection to ensure the safety and feasibility of the approach (Fig. 9, Table I). Measurements were performed twice by 2 independent surgeons and were made using a conventional metric tape. Anatomical sites were marked with an ink pen prior to measuring, to decrease the error rate.
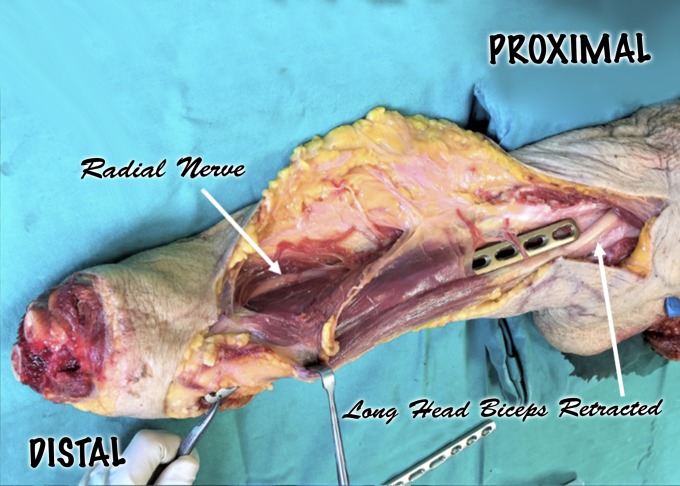
Fig. 9.
Schematic representation of measurements performed, including: (1) the width of the osseous medial epicondylar area; (2) the distance from the most distal border of the medial epicondyle to the proximal border of the coronoid fossa; (3) the distance from the start of the incision in the pronator teres to the point of crossing the neurovascular structures; (4) the distance between the apex of the medial epicondyle and the median nerve; (5) the distance between the apex of the medial epicondyle and the point where the plate tunnel crosses below the median nerve; (6) elbow flexion and extension, in full supination, after the procedure; and (7) the distance from the tip of each of the most distal screws to the ulnar nerve. (The plate was positioned 2 mm away from the medial border of the coronoid fossa. Distally, a distance of 2 mm was left from the distal border of the plate to the medial epicondyle. All screws were then introduced through both cortices of the bone).
TABLE I.
Measurements of Anatomical Parameters in Dissected Specimens
| Measurement* | Specimen No./Side† | |||||||||||||
| 1/R | 2/R | 3/R | 4/R | 5/R | 6/R | 7/R | 8/L | 9/L | 10/L | 11/L | 12/L | 13/L | 14/L | |
| (1) Width of the osseous medial epicondylar area (cm) | 1.9 | 2.5 | 2.1 | 2.7 | 1.9 | 2.4 | 2.2 | 2.0 | 2.2 | 2.2 | 1.7 | 2.2 | 2.2 | 2.3 |
| (2) Distance from the most distal border of the medial epicondyle to the proximal border of the coronoid fossa (cm) | 3.3 | 3.7 | 3.4 | 3.7 | 3.1 | 3.4 | 3.5 | 3.1 | 3.5 | 3.4 | 2.9 | 3.3 | 3.2 | 3.6 |
| a. No. of screws that could be inserted in this area | 3 | 4 | 4 | 4 | 3 | 4 | 4 | 3 | 4 | 4 | 3 | 3 | 3 | 4 |
| b. No. of screws inserted in this area when the fixation area was extended 2 cm proximally | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| (3) Distance from the muscular incision to the median nerve and neurovascular structures (cm) | 2.4 | 2.3 | 2.7 | 2.6 | 2.1 | 2.5 | 2.5 | 2.0 | 2.5 | 1.9 | 1.9 | 2.3 | 2.4 | 2.7 |
| (4) Distance between the apex of the medial epicondyle and the median nerve (cm) | 3.4 | 3.3 | 3.7 | 3.6 | 3.1 | 3.5 | 3.5 | 3.0 | 3.5 | 2.9 | 2.9 | 3.3 | 3.4 | 3.7 |
| (5) Distance between the apex of the medial epicondyle and the point where the plate tunnel crosses below the median nerve (cm) | 6.8 | 7.2 | 6.6 | 7.4 | 6.7 | 7.2 | 6.8 | 7.4 | 6.4 | 6.6 | 6.8 | 7.1 | 6.7 | 7.3 |
| (6) Elbow flexion/extension limitation in full supination after the plate assembly | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| (7) Distance from the tip of the distal screws to the ulnar nerve (mm) | ||||||||||||||
| a. Most distal screw | 1 | 5 | 2 | 4 | 0 | 3 | 3 | 1 | 4 | 2 | 0 | 3 | 3 | 4 |
| b. Second most distal screw | 5 | 11 | 5 | 10 | 4 | 8 | 6 | 4 | 10 | 7 | 3 | 10 | 8 | 9 |
| c. Third most distal screw | 14 | 19 | 10 | 16 | 13 | 14 | 14 | 15 | 18 | 14 | 11 | 15 | 16 | 14 |
| d. Fourth most distal screw | 21 | 23 | 23 | 22 | 20 | 19 | 19 | 22 | 23 | 22 | 19 | 22 | 20 | 18 |
See also Figure 9.
R = right arm, and L = left arm.
The most relevant measurements were as follows: (1) the width of the osseous medial epicondylar area between its medial border (apex) and the medial edge of the coronoid fossa; (2) the distance from the most distal border of the medial epicondyle to the proximal border of the coronoid fossa, measured parallel to the long axis of humerus, and also including measurement of the number of screws that could be inserted in this area and the number when the fixation area was extended 2 cm proximal to the proximal border of coronoid fossa; (3) the distance from the start of the incision in the pronator teres to the point of crossing the median nerve and neurovascular structures, measured perpendicular to the long axis of humerus; (4) the distance between the apex of the medial epicondyle and the median nerve, measured perpendicular to the long axis of the humerus; (5) the distance between the apex of the medial epicondyle and the point where the plate tunnel crosses below the median nerve, measured parallel to the long axis of the humerus; (6) any limitation in elbow flexion and extension, in full supination, checked after the procedure; and (7) the distance from the tip of each of the 4 most distal screws to the ulnar nerve (the screws were introduced bicortically).
Results
In all specimens, the plate was placed beneath the brachialis muscle except in its most distal portion, which was protected by the muscle belly of the pronator teres. The radial nerve was not endangered by the technique because of its particular pathway through the posterior and lateral aspects of the arm (Fig. 8). Measurements for the 14 specimens are reported, as are the ranges, mean values, and 95% confidence interval (CIs). Results are shown in Tables I and II and Figure 10.
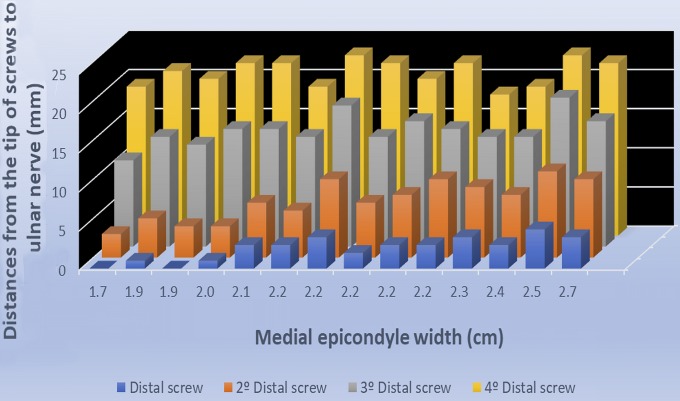
Fig. 10.
Risk of ulnar nerve injury from distal screws. It can be observed that only in 4 specimens with a very narrow osseous epicondylar area (≤2 cm), the ulnar nerve could be at risk with the most distal screw (touching or ≤1 mm). For the rest of the screws, regardless of the width of the osseous area, there was not a risk of injury to the ulnar nerve.
TABLE II.
Analysis of Variability of Measurements
| Measurement | Range | Mean | 95% CI |
| (1) Width of the medial epicondylar area (cm) | 1.7-2.7 | 2.19 | 2.03-2.33 |
| (2) Distance from the most distal border of the medial epicondyle to the proximal border of the coronoid fossa (cm) | 2.9-3.7 | 3.36 | 3.23-3.50 |
| a. No. of screws that could be inserted in this area | 3-4 | 3.60 | 3.27-3.87 |
| b. No. of screws inserted in this area when the fixation area was extended 2 cm proximally | 5-5 | 5 | 5.00-5.00 |
| (3) Distance from the muscular incision to the median nerve and neurovascular structures (cm) | 1.9-2.7 | 2.34 | 2.18-2.50 |
| (4) Distance between the apex of the medial epicondyle and the median nerve (cm) | 2.9-3.7 | 3.34 | 3.18-3.50 |
| (5) Distance between the apex of the medial epicondyle and the point where the plate tunnel crosses below the median nerve (cm) | 6.4-7.4 | 6.93 | 6.74-7.12 |
| (6) Flexion/extension limitation | NA* | NA* | NA* |
| (7) Distance from the tip of the distal screws to the ulnar nerve (mm) | |||
| a. Most distal screw | 0-5 | 2.50 | 1.60-3.40 |
| b. Second most distal screw | 3-11 | 7.14 | 5.61-8.68 |
| c. Third most distal screw | 10-19 | 14.50 | 13.13-15.87 |
| d. Fourth most distal screw | 18-23 | 20.93 | 19.93-21.93 |
NA = not applicable; no loss of elbow mobility in extension or flexion was found.
We found that there was variability in the shape of the medial epicondyle, but the technique could still be carried out correctly in all cases. The mean width of the medial epicondylar area was 2.19 cm (95% CI, 2.03 to 2.33 cm), space enough for the secure distal fixation of the plate (Table II, measurement 1).
The mean distance from the most distal border of the medial epicondyle to the proximal border of the coronoid fossa was 3.36 cm (95% CI, 3.23 to 3.50 cm) (Table II, measurement 2), and at least 3 LCP screws could be inserted in this area in all arms (Table I, measurement 2a). In addition, up to 5 screws could be inserted in this area in all specimens when the fixation zone was extended 2 cm proximally (Table I, measurement 2b).
The median nerve was identified lying over the brachialis muscle, and because of its proximity to the muscular incision, it was the main structure at risk while performing the distal approach. The mean distance between the apex of the medial epicondyle and the median nerve was 3.34 cm (95% CI, 3.18 to 3.50 cm) (Table II, measurement 4). As the pronator teres incision was performed 1 cm lateral to the apex of the medial epicondyle, the mean distance from the incision to the median nerve was 2.34 cm (95% CI, 2.18 to 2.50 cm) (Table II, measurement 3). Therefore, at least a 1.9-cm (range, 1.9 to 2.7-cm) layer of muscle belly was left laterally from the muscular incision to the median nerve in all specimens dissected (Table II, measurement 3). This distance was wide enough to ensure no damage to the neurovascular structures when performing the incision.
The mean distance between the apex of the medial epicondyle and the point where the plate tunnel crossed below the median nerve was 6.93 cm (95% CI, 6.74 to 7.12 cm) (Table II, measurement 5). Importantly, the CI suggests that, after 7.12 cm of plate introduction, the plate remained perfectly placed right above the periosteum of the humeral shaft, avoiding potential damage of the neurovascular structures.
There was no impingement of the coronoid fossa by the distal portion of the plate in any of the 14 specimens, and therefore, there was no loss of elbow mobility in either extension or flexion (Table I, measurement 6).
The ulnar nerve was identified in each specimen medial to the tips of the 4 distal screws in its retro-epicondylar groove. The mean distance between the tip of the most distal screw and the ulnar nerve was 2.50 mm (95% CI, 1.60 to 3.40 mm) (Table II, measurement 7a). There was 1 mm or less from the tip of this screw to the ulnar nerve (placing it at real risk) only in specimens with a very narrow epicondylar area (4 of 14 specimens) (Table I, measurement 7a).
The mean distance between the tip of the second most distal screw and the ulnar nerve was 7.14 mm (95% CI, 5.61 to 8.68 mm); between the third most distal and the ulnar nerve, 14.50 cm (95% CI, 13.13 to 15.87 mm); and between the fourth most distal and the ulnar nerve, 20.93 mm (95% CI, 19.93 to 21.93 mm) (Table II, measurements 6b, 6c, and 6d). Therefore, there was no risk of injury to the ulnar nerve from the second, third, or fourth most distal screws, even in specimens with a very narrow osseous medial epicondylar area, and no risk of injury from any of the 4 most distal screws in specimens in which the width of the osseous medial epicondylar area was >2 cm (Fig. 10).
Discussion
The results of this anatomical study showed that MIPO via an anteromedial-distal approach is a safe and useful technique for distal fractures of the humeral shaft on an anatomical basis. The risk of injury to the median nerve and brachial artery was avoided because they were protected by the belly of the pronator teres and brachialis muscle. The mean distance from the muscular incision to the median nerve was 2.34 cm (95% CI, 2.18 to 2.50 cm). Therefore, a thick muscular layer was left laterally from the neurovascular structures to the pronator teres incision (Fig. 1). A wider lateral dissection may be performed to identify the neurovascular structures under direct vision. This step will ensure that they will not be directly damaged during the performance of the approach if anatomical variants are present.
The risk of injury to the radial nerve is avoided with this approach. The radial nerve runs from the posterior aspect to the anterolateral aspect of the humerus9. In this way, an injury using this anteromedial approach is avoided (Fig. 8). Radial nerve palsy was described as a complication of classic anterior MIPO in the largest series, to our knowledge, published to date10. Other MIPO approaches have been used for distal-third humeral shaft fractures, with larger postoperative rates of radial nerve palsy. Posterior MIPO approaches have shown a rate of 5.4%11. A MIPO technique using a distal lateral Kocher approach to the humerus demonstrated a radial nerve palsy rate of 42%12. With these techniques, the radial nerve has to be identified and isolated during surgery, and these techniques are uncomfortable for the surgeon and dangerous to the nerve. Some modifications of these techniques using the same distal Kocher approach and without identification of the radial nerve have been reported13,14. Nevertheless, those modifications are dangerous, and they are, in fact, a blind radial nerve MIPO technique that implies important stress for the surgeon and a lack of predictability about radial nerve palsy.
Ulnar nerve damage is also a concern. The ulnar nerve runs posteriorly near the medial apex of the medial epicondyle, so the plate holes are lateral to the ulnar nerve. In 4 specimens with a very narrow osseous medial epicondylar area (≤2 cm), the tip of the most distal screw was very close to (≤1 mm) or touching the ulnar nerve, putting the nerve at risk. In small patients, it is recommended not to introduce the most distal screw through the posterior cortex (i.e., use unicortical fixation instead).
The proximal fixation of the plate may interfere with the long head of the biceps tendon, harming its gliding, as described Fernández Dell’Oca15. In our study, the plate was laid lateral to the crest of the greater tubercle in the majority of our specimens. The use of a shorter plate would avoid this problem. In this way, proximally, the plate would not reach the insertion of the pectoralis major and would be set below the muscular belly of the biceps muscle instead of its proximal tendon portion.
Distal-most shaft fractures can be addressed through this new approach. Apivatthakakul et al.8, among the pioneers of the anterior classic MIPO, reported that distal fractures cannot be fixed and that at least 6 cm without fracture above the coronoid fossa were needed to achieve a stable osteosynthesis of the distal fragment. Lee and Yoon14 stated that only 3 cm of distance from the upper border of the coronoid fossa were needed, using the distal Kocher approach. In our study, because of the particular “J” form of the plate and its distal fixation on the anterior area of the medial epicondyle, up to 5 distal screws can be inserted in fractures that occur only 2 cm proximally from the upper border of the coronoid fossa (Table I, measurement 2b). In addition, this is a well-protected muscular zone and so, no discomfort of the plate might be created and it is believed that no implant removal would be necessary.
Recently, an anteromedial-distal MIPO approach was described in a cadaveric study16. That approach is quite different than ours, as it does not open the pronator teres muscle. The brachialis muscle is detached from the medial septum in its distal zone. That approach16 offers no advantage in capacity of fixation of more distal fractures, the plate is fixed over an uncomfortable anatomical area (the medial distal edge of the humerus), and it is not risk-free with respect to radial nerve injury. Patients would be operated on in the supine position instead of the lateral decubitus11 or prone position17. Other distal lateral MIPO approaches require a specific position of the forearm to avoid injury to the radial nerve13,14. This new approach does not require a specific position of the forearm, making surgery more comfortable.
This new anteromedial-distal approach also allows another important advantage: the use of an external fixator placed laterally to achieve and maintain reduction throughout the procedure, without disturbing the surgery, instead of using Kirschner wires or only manipulation14. With this new technique, the identification of the anatomical references is easier than with other techniques12,13. The location of the medial epicondyle and the identification of the pronator teres muscle belly, required in this approach, is relatively simple.
This approach has some limitations. With respect to injury, it is not completely risk-free. Specifically, the brachial artery and the median nerve can be damaged while performing tunneling, and the ulnar nerve could also be damaged by the most distal screw in patients with a narrow epicondylar area.
In conclusion, this new approach is useful for distal-most humeral shaft fractures and has a low risk of nerve lesions. Nevertheless, it cannot be recommended until proper clinical studies are performed.
Footnotes
Investigation performed at the Department of Human Anatomy, University of Granada, Granada, Spain
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A146).
References
- 1.Jawa A, McCarty P, Doornberg J, Harris M, Ring D. Extra-articular distal-third diaphyseal fractures of the humerus. A comparison of functional bracing and plate fixation. J Bone Joint Surg Am. 2006. November;88(11):2343-7. [DOI] [PubMed] [Google Scholar]
- 2.Capo JT, Debkowska MP, Liporace F, Beutel BG, Melamed E. Outcomes of distal humerus diaphyseal injuries fixed with a single-column anatomic plate. Int Orthop. 2014. May;38(5):1037-43. Epub 2013 Dec 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prasarn ML, Ahn J, Paul O, Morris EM, Kalandiak SP, Helfet DL, Lorich DG. Dual plating for fractures of the distal third of the humeral shaft. J Orthop Trauma. 2011. January;25(1):57-63. [DOI] [PubMed] [Google Scholar]
- 4.Algarín-Reyes JA, Bello-González A, Pérez-Calzadilla M, Flores-Girón J. [Treatment of distal humeral shaft fractures at Polanco Mexican Red Cross]. Acta Ortop Mex. 2011. Sep-Oct;25(5):264-72. Spanish. [PubMed] [Google Scholar]
- 5.Claessen FMAP, Peters RM, Verbeek DO, Helfet DL, Ring D. Factors associated with radial nerve palsy after operative treatment of diaphyseal humeral shaft fractures. J Shoulder Elbow Surg. 2015. November;24(11):e307-11. Epub 2015 Sep 2. [DOI] [PubMed] [Google Scholar]
- 6.Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury. 2004. June;35(6):587-95. [DOI] [PubMed] [Google Scholar]
- 7.Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H. Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma. 2007. October;21(9):628-33. [DOI] [PubMed] [Google Scholar]
- 8.Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005. April;36(4):530-8. [DOI] [PubMed] [Google Scholar]
- 9.Gerwin M, Hotchkiss RN, Weiland AJ. Alternative operative exposures of the posterior aspect of the humeral diaphysis with reference to the radial nerve. J Bone Joint Surg Am. 1996. November;78(11):1690-5. [DOI] [PubMed] [Google Scholar]
- 10.López-Arévalo R, de Llano-Temboury AQ, Serrano-Montilla J, de Llano-Giménez EQ, Fernández-Medina JM. Treatment of diaphyseal humeral fractures with the minimally invasive percutaneous plate (MIPPO) technique: a cadaveric study and clinical results. J Orthop Trauma. 2011. May;25(5):294-9. [DOI] [PubMed] [Google Scholar]
- 11.Balam KM, Zahrany AS. Posterior percutaneous plating of the humerus. Eur J Orthop Surg Traumatol. 2014. July;24(5):763-8. Epub 2013 Nov 16. [DOI] [PubMed] [Google Scholar]
- 12.Zogbi DR, Terrivel AM, Mouraria GG, Mongon MLD, Kikuta FK, Filho AZ. Fracture of distal humerus: MIPO technique with visualization of the radial nerve. Acta Ortop Bras. 2014;22(6):300-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ji F, Tong D, Tang H, Cai X, Zhang Q, Li J, Wang Q. Minimally invasive percutaneous plate osteosynthesis (MIPPO) technique applied in the treatment of humeral shaft distal fractures through a lateral approach. Int Orthop. 2009. April;33(2):543-7. Epub 2008 Mar 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee T, Yoon J. Newly designed minimally invasive plating of a humerus shaft fracture; a different introduction of the plate. Int Orthop. 2016. December;40(12):2597-602. Epub 2016 Jan 21. [DOI] [PubMed] [Google Scholar]
- 15.Fernández Dell’Oca AA. The principle of helical implants. Unusual ideas worth considering. Injury. 2002. April;33(Suppl 1):SA1-27. [DOI] [PubMed] [Google Scholar]
- 16.Buranaphatthana T, Apivatthakakul T, Apivatthakakul V. Anteromedial minimally invasive plate osteosynthesis (MIPO) for distal third humeral shaft fractures - is it possible?: a cadaveric study. Injury. 2019. June;50(6):1166-74. Epub 2019 May 6. [DOI] [PubMed] [Google Scholar]
- 17.Gallucci G, Boretto J, Vujovich A, Alfie V, Donndorff A, De Carli P. Posterior minimally invasive plate osteosynthesis for humeral shaft fractures. Tech Hand Up Extrem Surg. 2014. March;18(1):25-30. [DOI] [PubMed] [Google Scholar]