Hypertension, or high blood pressure, is a major risk factor for heart disease and stroke (1). The prevalence of hypertension is higher among men than among women, increases with age, is highest among non-Hispanic blacks (blacks) (2), and has been consistently highest in the Southeastern region of the United States (1). To update prevalence estimates for self-reported hypertension and use of antihypertensive medication, CDC analyzed data from the 2017 Behavioral Risk Factor Surveillance System (BRFSS). The overall (unadjusted) prevalence of self-reported hypertension was 32.4% (95% confidence interval [CI] = 32.1%–32.7%). The age-standardized, median state-specific prevalence of self-reported hypertension was 29.7% (range = 24.3%–38.6%). Overall age-standardized hypertension prevalence was higher among men (32.9%) than among women (27.0%), highest among blacks (40.0%), decreased with increasing levels of education and household income, and was generally highest in the Southeastern and Appalachian states.* Among persons reporting hypertension, the overall unadjusted prevalence of self-reported antihypertensive medication use was 76.0% (95% CI = 75.5%–76.4%). The age-standardized, median state-specific prevalence of antihypertensive medication use among persons with reported hypertension was 59.4% (range = 50.2%–71.2%). Prevalence was higher among women than men, highest among blacks compared with other racial/ethnic groups, and highest among states in the Southeast, Appalachia, and the Dakotas. These findings can help inform CDC’s initiatives to enhance hypertension awareness, treatment, and control across all states.
BRFSS† is an annual, random-digit–dialed telephone survey (both landline and mobile phone), representative of the noninstitutionalized adult population aged ≥18 years of the 50 states, the District of Columbia (DC), and U.S. territories. In 2017, a total of 450,016 adults were interviewed. The present study includes data from the 50 states and DC; the median response rate was 45.9% (range = 30.6%–64.1%).§ Respondents were classified as having hypertension if they answered “yes” to the question “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” Those with borderline and pregnancy-related hypertension were categorized as “no.” Respondents reporting hypertension were classified as currently taking antihypertensive medication if they answered “yes” to the question “Are you currently taking medicine for your high blood pressure?” All analyses incorporated methods to account for the complex survey design. Application of sampling weights accounted for nonresponse, noncoverage, and mobile telephone–only households, and were derived from an iterative proportional weighting (raking) procedure.¶
The unadjusted, age-specific, and age-standardized prevalence of self-reported hypertension and antihypertensive medication use were estimated overall, for each of the 50 states and DC, and by sociodemographic characteristics. Prevalence estimates were age-standardized to the 2000 U.S. standard population (3). Differences in prevalence across sociodemographic subgroups were tested using chi-squared tests, and differences reported were considered statistically significant for p-values <0.05. All analyses were conducted using SAS-callable SUDAAN (version 11.0.3; RTI International).
During 2017, the overall unadjusted prevalence of hypertension for the 50 states and DC was 32.4% (95% CI = 32.1%–32.7%), representing an estimated 81.7 million adults (Table 1). The age-standardized median state-specific prevalence of hypertension was 29.7% (range = 24.3% [Minnesota] to 38.6% [Alabama and West Virginia]). Age-standardized hypertension prevalences were generally highest in Southeastern and Appalachian states (Figure). Age-specific hypertension prevalence increased with increasing age group (Table 2). The age-standardized prevalence of hypertension was higher among men (32.9%) than among women (27.0%), highest among blacks (40.0%), and decreased with increasing levels of education and household income.
TABLE 1. Unadjusted and age-standardized* prevalence of self-reported hypertension (HTN)† and current antihypertensive medication use§ among adults aged ≥18 years — Behavioral Risk Factor Surveillance System, 50 U.S. states and the District of Columbia, 2017.
| Area | Hypertension |
Current antihypertensive medication use among adults with hypertension |
||||||
|---|---|---|---|---|---|---|---|---|
| Sample with HTN | Population with HTN (x 1,000)¶ | % (95% CI) |
Sample using antihypertensive medication | Population using antihypertensive medication (x 1,000)¶ | % (95% CI) |
|||
| Unadjusted | Age-standardized* | Unadjusted | Age-standardized* | |||||
|
Overall
|
178,312
|
81,674
|
32.4 (32.1–32.7)
|
29.9 (29.6–30.2)
|
146,754
|
61,927
|
76.0 (75.5–76.4)
|
59.6 (58.8–60.3)
|
|
State
| ||||||||
| Alabama |
3,435 |
1,582 |
41.9 (40.3–43.4) |
38.6 (37.1–40.1) |
2,954 |
1,281 |
81.1 (79.1–83.1) |
70.5 (67.1–73.9) |
| Alaska |
1,245 |
176 |
31.8 (29.2–34.5) |
31.8 (29.4–34.2) |
875 |
113 |
64.4 (59.8–69.0) |
53.0 (46.7–59.2) |
| Arizona |
6,005 |
1,655 |
30.7 (29.8–31.5) |
28.0 (27.1–28.8) |
4,891 |
1,236 |
74.8 (73.2–76.3) |
56.0 (53.6–58.4) |
| Arkansas |
2,892 |
949 |
41.4 (39.0–43.7) |
38.5 (36.1–40.8) |
2,547 |
754 |
79.6 (76.5–82.8) |
69.3 (64.2–74.4) |
| California |
2,854 |
8,647 |
28.4 (27.1–29.6) |
27.0 (25.9–28.1) |
2,060 |
6,141 |
71.1 (68.8–73.4) |
53.0 (50.0–56.0) |
| Colorado |
3,189 |
1,130 |
26.0 (24.9–26.9) |
24.8 (23.8–25.7) |
2,395 |
764 |
69.9 (67.8–72.0) |
52.7 (49.6–55.8) |
| Connecticut |
3,991 |
859 |
30.5 (29.3–31.6) |
27.2 (26.1–28.3) |
3,313 |
658 |
76.8 (74.8–78.9) |
57.3 (54.0–60.6) |
| Delaware |
1,683 |
263 |
34.9 (32.9–36.9) |
31.1 (29.2–33.0) |
1,367 |
203 |
77.3 (74.2–80.4) |
58.8 (53.5–64.1) |
| District of Columbia |
1,505 |
149 |
26.4 (24.8–28.1) |
28.2 (26.7–29.6) |
1,241 |
111 |
74.5 (71.3–77.8) |
61.7 (57.3–66.0) |
| Florida |
9,360 |
5,810 |
34.6 (33.2–36.0) |
29.7 (28.5–31.0) |
7,568 |
4,496 |
77.5 (75.5–79.5) |
58.3 (54.8–61.7) |
| Georgia |
2,520 |
2,624 |
33.1 (31.6–34.6) |
31.6 (30.2–33.0) |
2,153 |
2,042 |
77.9 (75.4–80.3) |
62.7 (59.0–66.4) |
| Hawaii |
2,657 |
343 |
30.6 (29.2–32.0) |
28.1 (26.9–29.4) |
2,067 |
257 |
75.0 (72.5–77.4) |
57.9 (54.3–61.5) |
| Idaho |
1,806 |
379 |
29.8 (28.1–31.5) |
27.5 (26.0–29.0) |
1,378 |
260 |
69.0 (65.8–72.0) |
50.2 (46.2–54.2) |
| Illinois |
2,190 |
3,187 |
32.2 (30.8–33.7) |
29.9 (28.5–31.3) |
1,788 |
2,410 |
75.7 (73.3–78.2) |
59.8 (55.4–64.1) |
| Indiana |
6,226 |
1,796 |
35.2 (34.2–36.3) |
32.6 (31.7–33.6) |
5,262 |
1,372 |
76.5 (74.8–78.2) |
60.4 (57.8–63.0) |
| Iowa |
2,906 |
762 |
31.5 (30.3–32.6) |
28.3 (27.3–29.4) |
2,384 |
589 |
77.5 (75.5–79.4) |
60.7 (57.4–64.0) |
| Kansas |
8,757 |
718 |
32.8 (32.0–33.5) |
30.5 (29.8–31.2) |
7,187 |
544 |
75.8 (74.6–77.1) |
59.2 (57.3–61.2) |
| Kentucky |
4,214 |
1,356 |
39.4 (37.7–41.0) |
36.1 (34.6–37.6) |
3,600 |
1,094 |
80.8 (78.7–82.9) |
67.5 (64.1–70.9) |
| Louisiana |
2,208 |
1,400 |
39.0 (37.3–40.7) |
36.8 (35.2–38.4) |
1,849 |
1,123 |
80.3 (78.0–82.5) |
69.0 (65.3–72.6) |
| Maine |
3,909 |
376 |
34.8 (33.4–36.2) |
29.9 (28.5–31.3) |
3,117 |
279 |
74.5 (72(2–76.9) |
56.5 (52.7–60.8) |
| Maryland |
5,982 |
1,522 |
32.4 (31.2–33.5) |
29.8 (28.7–30.9) |
5,179 |
1,211 |
79.7 (77.8–81.5) |
62.6 (59.1–66.1) |
| Massachusetts |
2,475 |
1,564 |
28.6 (26.8–30.3) |
25.7 (24.3–27.2) |
2,053 |
1,220 |
78.1 (75.2–81.0) |
59.7 (54.4–65.0) |
| Michigan |
4,397 |
2,697 |
34.7 (33.6–35.8) |
31.3 (30.3–32.3) |
3,625 |
2,067 |
76.7 (75.0–78.4) |
59.4 (56.5–62.2) |
| Minnesota |
5,533 |
1,134 |
26.6 (25.8–27.4) |
24.3 (23.5–25.0) |
4,492 |
861 |
76.0 (74.3–77.6) |
58.0 (55.3–60.5) |
| Mississippi |
2,621 |
926 |
40.8 (38.8–42.7) |
38.2 (36.4–40.0) |
2,314 |
750 |
81.0 (78.3–83.8) |
71.2 (66.8–75.5) |
| Missouri |
3,133 |
1,513 |
32.0 (30.6–33.4) |
29.0 (27.7–30.3) |
2,671 |
1,204 |
79.7 (77.4–82.0) |
64.0 (59.8–68.0) |
| Montana |
2,211 |
238 |
29.0 (27.5–30.5) |
25.7 (24.2–27.1) |
1,750 |
170 |
71.8 (68.8–74.7) |
51.7 (47.5–56.0) |
| Nebraska |
5,895 |
443 |
30.6 (29.5–31.7) |
28.2 (27.3–29.2) |
4,957 |
348 |
78.6 (76.8–80.4) |
61.5 (58.3–64.7) |
| Nevada |
1,471 |
757 |
32.6 (30.5–34.8) |
30.0 (28.1–32.0) |
1,149 |
548 |
72.5 (68.9–76.2) |
55.1 (49.2–61.1) |
| New Hampshire |
2,284 |
324 |
30.0 (28.4–31.6) |
25.9 (24.4–27.4) |
1,915 |
257 |
79.7 (77.0–82.3) |
62.2 (56.0–68.3) |
| New Jersey |
4,897 |
2,305 |
33.0 (31.6–34.4) |
30.1 (28.8–31.4) |
4,096 |
1,750 |
76.0 (73.7–78.4) |
58.3 (54.7–62.0) |
| New Mexico |
2,496 |
484 |
30.5 (29.0–32.0) |
28.0 (26.6–29.4) |
1,952 |
353 |
73.2 (70.5–75.8) |
57.1 (52.9–61.3) |
| New York |
4,329 |
4,574 |
29.4 (28.3–30.5) |
27.1 (26.2–28.1) |
3,485 |
3,449 |
75.6 (73.7–77.5) |
57.4 (54.6–60.2) |
| North Carolina |
2,002 |
2,775 |
34.7 (33.0–36.5) |
31.8 (30.2–33.3) |
1,662 |
2,217 |
80.0 (77.6–82.5) |
64.1 (59.9–68.4) |
| North Dakota |
2,813 |
173 |
29.5 (28.2–30.8) |
28.2 (27.0–29.4) |
2,401 |
135 |
78.2 (75.9–80.6) |
63.2 (59.2–67.3) |
| Ohio |
5,394 |
3,130 |
34.7 (33.5–35.9) |
31.4 (30.2–32.6) |
4,618 |
2,433 |
77.9 (75.9–79.9) |
61.5 (58.3–64.6) |
| Oklahoma |
3,176 |
1,124 |
37.7 (36.2–39.2) |
35.4 (34.0–36.7) |
2,719 |
874 |
77.8 (75.6–80.0) |
64.0 (60.6–67.5) |
| Oregon |
1,835 |
987 |
30.1 (28.7–31.5) |
27.2 (25.9–28.5) |
1,374 |
699 |
71.0 (68.4–73.5) |
53.3 (49.5–57.0) |
| Pennsylvania |
2,337 |
3,295 |
32.6 (31.1–34.1) |
28.9 (27.6–30.2) |
1,896 |
2,586 |
78.6 (76.4–80.9) |
60.9 (56.9–64.8) |
| Rhode Island |
2,303 |
280 |
33.1 (31.4–34.8) |
29.9 (28.3–31.5) |
1,969 |
226 |
81.0 (78.4–83.7) |
65.5 (60.3–70.6) |
| South Carolina |
5,632 |
1,498 |
38.1 (36.9–39.3) |
34.4 (33.3–35.6) |
4,916 |
1,206 |
80.6 (78.9–82.4) |
68.5 (65.2–71.8) |
| South Dakota |
2,862 |
203 |
30.8 (28.9–32.7) |
28.0 (26.2–29.7) |
2,420 |
161 |
79.4 (76.3–82.5) |
64.8 (59.0–70.5) |
| Tennessee |
2,638 |
2,012 |
38.7 (36.9–40.4) |
35.5 (33.9–37.2) |
2,210 |
1,580 |
78.6 (76.0–81.1) |
65.0 (60.9–69.1) |
| Texas |
5,299 |
6,853 |
32.5 (30.8–34.2) |
31.9 (30.3–33.5) |
4,446 |
4,958 |
72.4 (69.4–75.3) |
57.5 (53.5–61.6) |
| Utah |
3,044 |
534 |
24.5 (23.4–25.5) |
25.4 (24.5–26.4) |
2,224 |
359 |
67.4 (65.1–69.7) |
52.3 (49.6–55.1) |
| Vermont |
2,313 |
153 |
30.4 (28.9–31.9) |
26.4 (25.1–27.8) |
1,804 |
112 |
73.5 (71.0–76.1) |
51.7 (47.8–55.6) |
| Virginia |
3,895 |
2,136 |
32.4 (31.1–33.6) |
30.3 (29.1–31.5) |
3,245 |
1,613 |
75.7 (73.5–77.9) |
58.3 (55.1–61.5) |
| Washington |
4,840 |
1,700 |
29.5 (28.6–30.5) |
27.6 (26.6–28.5) |
3,696 |
1,184 |
69.9 (68.0–71.7) |
54.5 (51.9–57.2) |
| West Virginia |
2,769 |
631 |
43.5 (28.6–30.5) |
38.6 (37.0–40.2) |
2,380 |
502 |
79.6 (77.5–81.7) |
61.7 (58.4–65.1) |
| Wisconsin |
2,143 |
1,387 |
30.8 (29.2–32.4) |
27.9 (26.4–29.4) |
1,743 |
1,041 |
75.4 (72.6–78.2) |
57.0 (52.4–61.5) |
| Wyoming |
1,741 |
138 |
30.8 (29.2–32.4) |
28.5 (27.0–30.0) |
1,397 |
98 |
71.7 (68.8–74.7) |
53.5 (49.4–57.6) |
| Median |
— |
— |
32.2 |
29.7 |
— |
— |
76.7 |
59.4 |
| Range | — | — | 24.5–43.5 | 24.3–38.6 | — | — | 64.4–81.1 | 50.2–71.2 |
Abbreviation: CI = confidence interval.
* Age standardized to the 2000 U.S. projected population using three age groups: 18–44, 45–64, and ≥65 years.
† Hypertension was defined as an affirmative response to “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” Preeclampsia or borderline high or prehypertensive was categorized as “no.”
§ Current antihypertensive medication use was defined as affirmative response to “Are you currently taking medicine prescribed by a doctor or other health professional for your high blood pressure?”
¶ Weighted number of adults in the population with hypertension or currently using antihypertensive medication.
FIGURE.
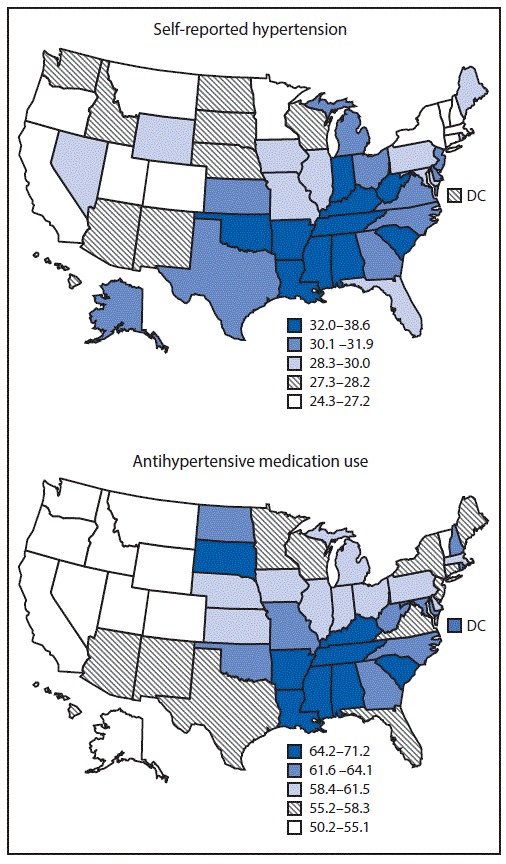
Age-standardized percentage of self-reported hypertension and antihypertensive medication use among adults aged ≥18 years, by state — Behavioral Risk Factor Surveillance System, United States, 2017
Abbreviation: DC = District of Columbia.
TABLE 2. Unadjusted and age-standardized* prevalence of self-reported hypertension (HTN)† and antihypertensive medication use§ among adults aged ≥18 years, by selected characteristics — Behavioral Risk Factor Surveillance System, United States, 2017.
| Characteristic | Hypertension |
Antihypertensive medication use among adults with hypertension |
||||||
|---|---|---|---|---|---|---|---|---|
| Sample with HTN | Population with HTN (x 1000)¶ | % (95% CI) |
Sample using antihypertensive medication | Population using antihypertensive medication (x 1,000)¶ | % (95% CI) |
|||
| Unadjusted | Age-standardized* | Unadjusted | Age-standardized* | |||||
|
Overall
|
178,312
|
81,674
|
32.4 (32.1–32.7)
|
29.9 (29.6–30.2)
|
146,754
|
61,927
|
76.0 (75.5–76.4)
|
59.6 (58.8–60.3)
|
|
Age group (yrs)
| ||||||||
| 18–44 |
18,432 |
16,429 |
14.1 (13.7–14.5) |
14.1 (13.8–14.5) |
7,512 |
6,195 |
37.9 (36.5–39.2) |
37.9 (36.5–39.2) |
| 45–64 |
66,699 |
34,048 |
40.5 (40.0–41.0) |
40.5 (40.0–41.0) |
53,783 |
27,085 |
79.6 (78.9–80.3) |
79.6 (78.9–80.3) |
| ≥65 |
93,181 |
31,198 |
60.5 (60.0–61.1) |
60.5 (60.0–61.1) |
85,459 |
28,647 |
92.0 (91.5–92.4) |
92.0 (91.5–92.4) |
|
Sex*
| ||||||||
| Men |
81,648 |
42,260 |
34.5 (34.0–34.9) |
32.9 (32.5–33.3) |
64,010 |
30,136 |
71.5 (70.7–72.2) |
56.7 (55.8–57.6) |
| Women |
96,569 |
39,363 |
30.4 (30.0–30.8) |
27.0 (26.6–27.3) |
82,669 |
31,747 |
80.8 (80.1–81.4) |
64.0 (62.7–65.2) |
|
Race/Ethnicity*
| ||||||||
| White, non-Hispanic |
136,668 |
53,179 |
34.0 (33.7–34.3) |
29.0 (28.7–29.3) |
113,525 |
41,278 |
77.7 (77.2–78.2) |
59.0 (58.1–59.9) |
| Black, non-Hispanic |
18,628 |
12,127 |
41.1 (40.1–42.1) |
40.0 (39.2–40.9) |
16,116 |
9,649 |
79.6 (78.3–80.9) |
68.1 (66.2–70.0) |
| Hispanic |
9,081 |
9,510 |
23.9 (23.0–24.7) |
28.2 (27.3–29.1) |
6,359 |
6,133 |
64.8 (62.8–66.8) |
54.0 (51.9–56.0) |
| American Indian/Alaska Native, non-Hispanic |
3,624 |
976 |
38.8 (36.4–41.3) |
37.1 (34.7–39.5) |
2,784 |
690 |
70.7 (66.7–74.7) |
58.6 (53.6–63.5) |
| Asian, non-Hispanic |
2,290 |
2,659 |
19.6 (17.8–21.4) |
23.8 (21.9–25.8) |
1,786 |
1,835 |
69.2 (64.5–73.9) |
58.0 (52.8–63.0) |
| Native Hawaiian/Pacific Islander, non-Hispanic |
316 |
127 |
26.4 (21.2–31.7) |
33.0 (28.3–38.0) |
200 |
87 |
68.4 (59.1–77.6) |
54.9 (45.8–63.6) |
| Multiracial, non-Hispanic |
3,373 |
1,060 |
30.1 (28.3–32.0) |
31.6 (29.9–33.4) |
2,504 |
731 |
69.1 (65.9–72.3) |
56.7 (52.8–60.6) |
| Other, non-Hispanic |
880 |
368 |
33.1 (28.8–37.3) |
28.9 (25.3–32.8) |
703 |
276 |
75.2 (67.9–82.5) |
54.9 (45.4–64.0) |
|
Education level*
| ||||||||
| Less than high school |
15,316 |
13,232 |
39.1 (38.1–40.2) |
35.4 (34.4–36.3) |
12,605 |
10,020 |
75.9 (74.4–77.4) |
58.6 (56.4–60.8) |
| High school or equivalent |
54,498 |
24,742 |
35.2 (34.6–35.7) |
32.3 (31.8–32.8) |
45,423 |
18,944 |
76.7 (75.9–77.6) |
59.6 (58.4–60.9) |
| More than high school |
107,886 |
43,411 |
29.5 (29.2–29.9) |
27.5 (27.2–27.8) |
88,234 |
32,756 |
75.6 (74.9–76.2) |
59.8 (58.8–60.8) |
|
Household income*
| ||||||||
| <$15,000 |
17,836 |
9,145 |
40.7 (39.6–41.8) |
37.9 (36.9–39.0) |
14,384 |
6,889 |
75.5 (73.9–77.1) |
61.5 (59.3–63.7) |
| $15,000 to <$25,000 |
28,614 |
13,017 |
36.9 (36.1–37.7) |
34.3 (33.6–35.1) |
23,605 |
9,895 |
76.1 (74.9–77.4) |
59.7 (57.9–61.5) |
| $25,000 to <$35,000 |
17,502 |
7,731 |
35.5 (34.5–36.6) |
31.9 (30.9–32.9) |
14,589 |
5,928 |
76.8 (75.3–78.4) |
60.4 (57.5–63.2) |
| $35,000 to <$50,000 |
22,129 |
9,213 |
33.1 (32.3–34.0) |
29.9 (29.1–30.7) |
18,451 |
7,029 |
76.4 (75.0–77.8) |
56.9 (54.9–58.8) |
| ≥$50,000 | 61,667 | 29,012 | 28.2 (27.8–28.7) | 26.9 (26.5–27.3) | 49,890 | 21,529 | 74.3 (73.5–75.1) | 59.7 (58.5–60.9) |
Abbreviation: CI = confidence interval.
*Age standardized to the 2000 U.S. projected population using three age groups: 18–44, 45–64, and ≥65 years.
† Hypertension was defined as an affirmative response to “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?” Preeclampsia or borderline high or pre-hypertensive was categorized as “no.”
§ Current antihypertensive medication use was defined as affirmative response to “Are you currently taking medicine prescribed by a doctor or other health professional for your high blood pressure?”
¶ Weighted number of adults in the population with hypertension or currently using antihypertensive medication.
Among those reporting hypertension, the overall, unadjusted prevalence of antihypertensive medication use was 76.0% (95% CI = 75.5%–76.4%), representing an estimated 61.9 million adults (Table 1). The age-standardized, median, state-specific prevalence of antihypertensive medication use was 59.4% (range = 50.2% [Idaho] to 71.2% [Mississippi]). Age-standardized prevalence of antihypertensive medication use was highest in the Southeastern and Appalachian states, as well as the Dakotas (Figure). The age-specific prevalence of antihypertensive medication use also increased with increasing age (Table 2), was highest among blacks (68.1%), was higher among women (64.0%) than among men (56.7%), and did not vary by education or household income level.
Discussion
During 2017, approximately one third (82 million) of U.S. adults reported having hypertension, and an estimated three quarters of those with hypertension (62 million) reported using antihypertensive medication. Age-standardized prevalence of hypertension varied widely by state, remaining highest in the Southeast and among men and blacks. Age-standardized prevalence of antihypertensive medication use also increased with increasing age, was highest among blacks, and was higher among women than among men.
The overall age-standardized self-reported hypertension prevalence of 29.9% was similar to that reported based on 2011–2015 BRFSS data (29.8%) (1) and measured hypertension prevalence of 29% based on data from the 2015–2016 National Health and Nutrition Examination Survey (2). Also consistent with other reports, hypertension prevalence decreased with increasing income (4) and education level (1) and was highest in Southeastern and Appalachian states (1,2). The overall, age-standardized prevalence of antihypertensive medication use (59.6%) was also similar to estimates from the 2011–2015 BRFSS, ranging from 63.0% in 2011 to 61.8% in 2015 (1). Like hypertension prevalence, medication use prevalence was highest in Southeastern and Appalachian states. In the present study, prevalence of medication use was also highest in the Dakotas, despite a midrange prevalence of hypertension in these states. Prevalence of antihypertensive medication use was higher in older age groups, highest among blacks, and higher among women than men. This overall gender difference has been reported previously (1), but the reasons are unclear. Data from Medicare Part D beneficiaries aged ≥65 years suggest that antihypertensive medication nonadherence is similar for men (25.8%) and women (26.7%) (5). More information is needed to examine the relationship between the prevalence of self-reported hypertension and that of antihypertensive medication use.
The findings in this report are subject to at least three limitations. First, data were self-reported. The lack of documented diagnosis of hypertension based on historic blood pressure measurements does not allow for precise assessment of hypertension; however, the results were similar to data from previous reports based on both self-report (1) and measured hypertension (2). Second, low median response rates across states might limit the representativeness of the 2017 BRFSS sample and potentially result in either under- or overestimates of prevalence, although application of sampling weights is likely to reduce some nonresponse bias. Finally, findings are representative of noninstitutionalized civilian persons only and would exclude those living in nursing homes, prisons, and other institutions.
This report provides the most recent state-level surveillance data on prevalence of self-reported hypertension and antihypertensive medication use among persons reporting hypertension. Hypertension prevention and control is a priority of CDC’s state and local funding for heart disease and stroke prevention** and one of the important elements of the Million Hearts initiative (6). CDC has been working closely with states to enhance hypertension management through a strategy of team-based care in which two or more health care providers work collaboratively with each patient. These teams may include doctors, nurses, pharmacists, dietitians, community health workers, and other health care providers. This approach is often multidisciplinary with a team working to educate patients, identify risk factors, provide treatments, and sustain ongoing conversations with patients. This strategy can result in multiple opportunities for intervention for better blood pressure control (7),†† with the ultimate goal of reducing disparities in hypertension awareness, treatment, and control across the United States.
Summary.
What is already known about this topic?
Prevalence of hypertension increases with increasing age and is higher among men than women and among non-Hispanic blacks than among other racial/ethnic groups; prevalence has been consistently higher in the Southeastern and Appalachian regions of the United States.
What is added by this report?
Analysis of 2017 Behavioral Risk Factor Surveillance System data found that approximately one third of U.S. adults reported having hypertension, and an estimated 75% of those reporting having hypertension reported using antihypertensive medication. The prevalence of these factors varied widely by state and was generally highest in the Southeastern and Appalachian states.
What are the implications for public health practice?
A multidisciplinary team-based strategy working to educate patients, maintain dialogue over time, and identify risk factors can provide intervention opportunities for better blood pressure control and could reduce disparities in hypertension awareness, treatment, and control across the United States.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
Footnotes
References
- 1.Fang J, Gillespie C, Ayala C, Loustalot F. Prevalence of self-reported hypertension and antihypertensive medication use among adults aged ≥18 years—United States, 2011–2015. MMWR Morb Mortal Wkly Rep 2018;67:219–24. 10.15585/mmwr.mm6707a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS data brief, no 289. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2017. https://www.cdc.gov/nchs/data/databriefs/db289.pdf [PubMed] [Google Scholar]
- 3.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy people statistical notes, no. 20. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2001. https://www.cdc.gov/nchs/data/statnt/statnt20.pdf [Google Scholar]
- 4.Gillespie CD, Hurvitz KA. Prevalence of hypertension and controlled hypertension—United States, 2007–2010. In: CDC Health Disparities and Inequalities Report—United States, 2013. MMWR Suppl 2013;62(No. Suppl 3). [PubMed] [Google Scholar]
- 5.Ritchey M, Chang A, Powers C, et al. Vital signs: disparities in antihypertensive medication nonadherence among Medicare Part D beneficiaries—United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65:967–76. 10.15585/mmwr.mm6536e1 [DOI] [PubMed] [Google Scholar]
- 6.CDC. Million hearts: strategies to reduce the prevalence of leading cardiovascular disease risk factors—United States, 2011. MMWR Morb Mortal Wkly Rep 2011;60:1248–51. [PubMed] [Google Scholar]
- 7.Kravetz JD, Walsh RF. Team-based hypertension management to improve blood pressure control. J Prim Care Community Health 2016;7:272–5. 10.1177/2150131916645580 [DOI] [PMC free article] [PubMed] [Google Scholar]


