Abstract
Purpose:
This article outlines how current nursing research can utilize technology to advance symptom and self-management science for precision health and provides a roadmap for the development and use of technologies designed for this purpose.
Approach:
At the 2018 annual conference of the National Institute of Nursing Research (NINR) Research Centers, nursing and interdisciplinary scientists discussed the use of technology to support precision health in nursing research projects and programs of study. Key themes derived from the presentations and discussion were summarized to create a proposed roadmap for advancement of technologies to support health and well-being.
Conclusions:
Technology to support precision health must be centered on the user and designed to be desirable, feasible, and viable. The proposed roadmap is composed of five iterative steps for the development, testing, and implementation of technology-based/enhanced self-management interventions. These steps are (a) contextual inquiry, focused on the relationships among humans, and the tools and equipment used in day-today life; (b) value specification, translating end-user values into end-user requirements; (c) design, verifying that the technology/device can be created and developing the prototype(s); (d) operationalization, testing the intervention in a real-world setting; and (e) summative evaluation, collecting and analyzing viability metrics, including process data, to evaluate whether the technology and the intervention have the desired effect.
Clinical Relevance:
Interventions using technology are increasingly popular in precision health. Use of a standard multistep process for the development and testing of technology is essential.
Keywords: National Institute of Nursing Research, nursing research, self-management, symptoms, technology
Nursing science is focused on improving the health and quality of life of individuals, families, and communities (National Institute of Nursing Research [NINR], 2016). Worldwide, over 3.2 billion people are connected to the Internet, and 5 billion people (two thirds of the world’s population) have a mobile phone connection (Sawers, 2017), which presents new possibilities for expanding accessibility to nursing science research, particularly precision health. Precision health “offers the promise of tailoring treatment to individuals based on their genetics, lifestyle, and environment” (Grady, 2017, p. 248). Many of the NINR Research Centers are playing a leading role in advancing nursing science using technology for precision health, and in May 2018, nursing and interdisciplinary scientists gathered to discuss best practices for integrating technology in nursing research. Because opportunities and challenges for the development and application of technology in nursing research are similar across nations, geographical locations, and populations, the topic has international relevance. This article (a) summarizes the state of the science, opportunities and challenges related to the development, and testing and use of technology for precision health across all populations; (b) provides examples of how NINR Research Centers are utilizing technology in research pilot projects; and (c) presents a roadmap for nursing science in the design, testing, and use of technologies to support precision health.
Considerations for Use of Technologies to Support Precision Health
Within the extramural NINR Research Centers, which include Exploratory Centers (P20) and Centers of Excellence (P30), a broad range of technologies to support interventions are being developed to capture, interpret, and deliver health information to individuals in a useful format. However, there are important considerations in using technologies, such as websites, sensors, or mobile apps, to support precision health. Technology itself is not an intervention but serves as the infrastructure through which interventions can be designed and delivered (Marquard, 2018). If this infrastructure (technology) fails, then the intervention may also fail. Therefore, it is important that the technology be rigorously designed and tested prior to full-scale testing in an intervention. Further, the intervention should not be dependent on a specific technology, as technologies tend to rapidly become obsolete (DeVito Dabbs, 2018).
In considering technologies to support precision health, one must identify the need for the technology, its function, and how it supports the theoretical model of the study and intervention. Technology design should be theoretically driven, fit the intervention, and promote use by the individual. Technologies may incorporate innovative tools and data science that customize how disease prevention, detection, and management are approached. These innovative tools may include (a) active systems for physiological monitoring (e.g., wearable technology); (b) passive systems that capture symptom data via online patient portals; and (c) interactive systems that support the exchange of information between the user and healthcare provider.
Models Guiding the Design of User-Centered Technology
It is widely agreed that the individual or end user must be central to the project design in user-centered technology (Bradley, 2010; Gibbons, 2016; Holden et al., 2013; Marquard, 2018; Venkatesh, Thong, & Zu, 2012). There are several models focused on person-centered or user-centered design that provide insight on design features or steps. Marquard (2018) adapted a model to explain how three constructs intersect to identify the needs of the end user (Figure 1). These constructs include (a) human factors, or whether the design is desirable (valued by the users); (b) the business proposition, or whether the design is viable (cost-effective and sustainable); and (c) technology, or whether the design is feasible (able to be designed and created). To assess the applicability of a technology for a specific intervention, the interdisciplinary team of investigators must develop a deep understanding of the end users and their needs. This includes assessing factors that may affect the constructs of desirability, feasibility, and viability, such as the end users’ willingness to use technology, their literacy and language skills, and access to the necessary infrastructure.
Figure 1.
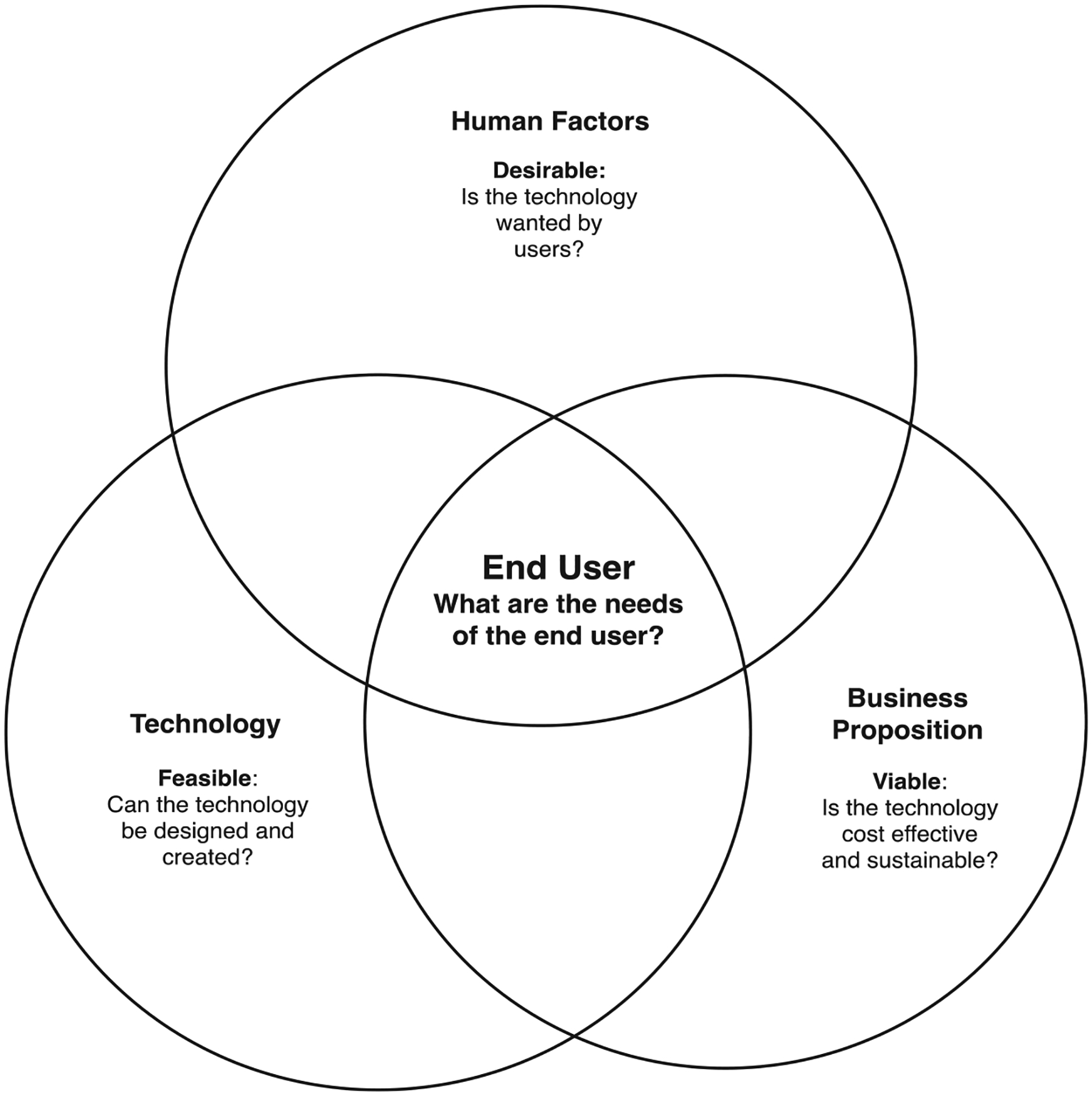
Factors affecting user-centered design (Marquard, 2018)
Other model examples are the Nielsen Norman Group’s Design Thinking Model (Gibbons, 2016) and the Field Guide to Human-Centered Design (IDEO.org, 2015), which describe the process of user-centered design using three phases. The Design Thinking Model (Gibbons, 2016) identifies the phases as (a) understand, (b) explore, and (c) materialize. In The Field Guide to Human-Centered Design (IDEO.org, 2015), the three phases are (a) inspiration, (b) ideation, and (c) implementation. In both cases, the first phase is devoted to understanding the needs of the end user and the problem that the technology should address. Both models suggest participatory design with interviews or other interactive design sessions to help define the need, how the technology may help to fill the need, and stakeholder and end-user preferences for specific characteristics. The second phase in both models includes iterative development of prototypes, testing, obtaining user feedback, and revision of the design. The final phase is planning for large-scale dissemination and implementation.
Other models may influence the priority of design elements, such as The User Experience Hierarchy of Needs (Bradley, 2010), which is built off of Maslow’s hierarchy of needs. It rests on the assumption that for a technology design to be successful, it must meet basic needs before it can satisfy higher-level needs. The most basic level is functionality, or does the design operate properly and meet the functional requirements. Next is reliability, then usability, including ease of use. Complex concerns such as proficiency or the ability to empower people to do more and better are higher in the model. The highest level of user needs is creativity, the aesthetic beauty or sensori-emotional values, derived from using the technology.
The Consumer Theory of Acceptance and Use of Technology (UTAUT2) is an extension of the Unified Theory of Acceptance and Use of Technology (UTAUT) (Venkatesh, Morris, Davis, & Davis, 2003) and seeks to explain user acceptance of technology. This theory is useful to assess the likelihood of success for new technology. It may also help proactive design of interventions (including training, marketing, etc.) targeted at populations of users that may be less inclined to adopt and use new systems. The UTAUT2 has several mediators of intention and usage of technology: (a) performance expectancy, (b) effort expendancy, (c) social influence, (d) facilitating conditions, (e) hedonic motivation, (f) price value, and (g) habit. The moderators of intention and use behavior include age, gender, and experience (Venkatesh et al., 2012).
For technology that includes interactions between the end user, study team, healthcare providers, and institutions, the Systems Engineering Initiative for Patient Safety (SEIPS) 2.0, captures the complexities of the sociotechnical work system, and the influence of these complexities on processes and outcomes (Holden et al., 2013). The work system includes interactions among the person, technology, organization, internal environment, and tasks. Physical, cognitive, and social/behavioral processes between the end user and study team/healthcare provider drive the outcomes, which can be desirable/undesirable and proximal/distal.
These established models have provided a framework for the technology innovations being tested in the NINR Research Centers. Each model or theory provides a different perspective on developing, testing, and implementing technology that is user centered. These models also suggest techniques that can be used to develop a design focused on user needs and to test and refine the technology.
Testing and Refining Technology to Address User Needs
During the phases of user-centered technology design, a variety of techniques are used to determine user needs, develop and test the technology, and plan for dissemination and implementation. The processes are iterative and include cycling between the process of testing and refining a prototype and gathering user feedback by consulting with heterogeneous groups with diverse backgrounds to address user needs. This iterative nature of user-centered design is essential to optimize use behaviors and data sharing, and to address the evolution in technology platforms that occur over time.
To determine user needs, which may include patients and/or caregivers, and obtain user feedback on the technology, a qualitative approach using semistructured, audio-taped interviews and user observation is considered standard practice, incorporating iterative cycles with potential users to assess the user interface and refine the prototype (Jacob et al., 2013; Kaufman et al., 2003; McCurdie et al., 2012; Snodgrass & Coyne, 1992). This design development approach concentrates on user performance (i.e., ease of use and learning, errors, and efficiency) and satisfaction with program content and functionality (i.e., reports, goal-setting). Human computer interaction literature recommends at least five users, typically a heterogeneous group, for a usability cycle, and two to three cycles to capture the potential breadth of user experiences (Macefield, 2009; Medlock, Wixon, McGee, & Welsh, 2005; Virzi, 1992).
Metrics are used at each stage to quantitatively evaluate stakeholder and end-user experience (see Figure 1). Metrics used to ascertain desirability, the need and usefulness for the technology, should include feedback on whether the technology is valued, and whether there is pleasure and joy in using it. Viability, the cost effectiveness and sustainability of the technology, includes metrics of functionality, trustworthiness, and intent to use. Feasibility, the potential to design and create the technology for the intended purpose, is evaluated with the metrics of usefulness, ease of use, simplicity, and acceptance. Metrics for security practices and adherence to privacy regulations are also of paramount importance to human studies.
Contextual factors influence the extent to which technology promotes interaction between the individual and his or her health, as well as between the individual and his or her healthcare provider. As noted in the UTAUT2 Model (Venkatesh et al., 2012), mediators that predict end-user behavior (performance expectancy, effort expectancy, social influence, facilitating conditions, hedonic motivation, price value, and habit) and moderators need to be addressed. There are additional moderators of relevance to studies focused on symptom and self-management science, including developmental stage, cognition, health disparities, user costs, and inequality in technology access.
Challenges to Technology Use
To ensure successful technology use, the researcher must have a deep understanding of end-user needs and potential barriers to the use of technology. For example, individuals managing symptoms may encounter technology use challenges due to issues such as altered vision, sensation, and mobility. Researchers have increasingly addressed a variety of health disparity issues related to symptom and self-management science (Bakken & Reame, 2016; Zabler et al., 2018). There are also disparities in access and use of Internet and mobile technology that may be related to individual preferences, age, literacy, race, and language (Bailey et al., 2015; Casillas, Moreno, Grotts, Tseng, & Morales, 2018; Gordon & Hornbrook, 2016). Interventions that are centered on end-user needs must also accommodate language, literacy, and culture, which may add to the methodological complexity of the design, testing, and use of the technology.
Access to the devices and infrastructure is a challenge in the development of technologies for precision health interventions. Devices such as smart phones, tablets, and computers are costly, and access to Internet and cellular networks is not universal. In many rural areas around the world, high speed Internet is not available and cell phone access may not be reliable, leading to rural participants having less access to technologies for personal health (Greenberg, Haney, Blake, Moser & Hesse, 2017). Therefore, research that incorporates technology must be designed with consideration of the factors necessary to optimize access and usability, as well as to ensure adequate documentation and reporting.
Examples of Precision Health Intervention Technologies
The NINR Exploratory Centers (P20) and Centers of Excellence (P30) are each focused on an aspect of nursing science such as symptom management science, self-management science, and populations with complex chronic conditions (2018 P20/P30 Centers). Many of these centers incorporate technology use in the study of precision health. Below we highlight how four of the NINR Research Centers have used technology in their science. Additional examples of technology use may be found on the websites of the NINR Research Centers (see hyperlinks to all NINR Center websites in the Clinical Resources section of this article).
At the P20 UManage Center for Building the Science of Symptom Self-Management (University of Massachusetts Amherst), research teams are developing and applying technology to improve symptom self-management. In one project, researchers incorporated the use of an off-the-shelf actigraph to monitor sleep, a sleep diary, and a peer network to help older individuals learn to improve their sleep hygiene. Use of an off-the-shelf wearable actigraph for sleep management in a population not typically thought of as technologically savvy is a novel application of this technology.
The University of Connecticut School of Nursing’s P20 Center for Accelerating Precision Pain Self-Management is using wearable technology to track health behaviors (physical activity, nutrition, sleep patterns) in patients with painful conditions and to deliver behavior change support and real-time nurse consultation or coaching. The goal of the pilot studies is to improve pain self-management outcomes through reporting real-time summaries of individual physiologic data and achievements toward self-management goals. In addition, nurse consultations focus on assisting individuals with problem solving and integrating self-management skills into daily life.
Researchers at the Center for Transdisciplinary Collaborative Research in Self-Management at the University of Texas, Austin (P30), are using interactive digital games or machine learning to characterize patterns and changes in individual and group self-care-related behavioral data (nutritional, physical activity, stress management, or mental health) that are predictive of distal outcomes in people with chronic illnesses. Following characterization, augmented intelligence algorithms based on a thoughtfully categorized narrative library of key phenotypic characteristics of patients with matching taxonomy (age, gender, acculturation level, level of health literacy, level of depressive symptoms) inform the creation of a more “personalized intervention.” These tools may be used to build community infrastructure for innovative technology-assisted interventions, with the goal of preventing a widening of health disparity gaps in the future.
At the University of Washington’s Center for Innovation in Sleep Self-Management (P30), researchers have applied a user-centered design approach to develop and refine a technology-based sleep self-management intervention design (SMID) for youth. The scientists incorporated intervention materials from a prior web-based intervention for youth with chronic pain that included sleep hygiene education, a self-management focus, direct stakeholder input, and a team of pediatric behavioral sleep experts to develop the SMID. At every phase of the design process, user feedback was incorporated into the next iteration of the intervention.
A Roadmap for Technology Use in Precision Health
Through the experiences gained from NINR Center research projects and analysis of the present state and issues on the use of technology for precision health, a roadmap of best practices for the coordinated advancement of nursing science was created. The roadmap for technology use in precision health was based on the key themes arising during presentations and discussion at the gathering in May 2018. The proposed roadmap is composed of five iterative steps for the development, testing, and implementation of technology-based/enhanced self-management interventions and is guided by the University of Twente’s Centre for eHealth and Wellbeing Research (CeHRes) Roadmap (Reblin et al., 2017) and contextualized within the Nursing Science Precision Health (NSPH) Translational Model (Hickey et al., 2019). The incorporation of the NSPH Model (Hickey et al., 2019) served as an important element for nursing science. The NSPH Model was developed to explicate methods for the characterization of genotype or other biomarkers, phenotype, and environment, as well as precision in intervention target discovery, design, and delivery. In this model, precision is characterized as four constructs (measurement, phenotype, genotype or biomarkers, and intervention) and is enabled by an information and data science infrastructure that includes the use of technology (Hickey et al., 2019). The approach provides theoretical linkages between the intervention and technology use in each step, and is designed to support end users, caregivers, and healthcare providers. While the new NINR Centers roadmap for technology use in precision health emanates from symptom science and self-management, its constructs can be applied more broadly to technology design and use in many other areas of nursing science.
Step 1, contextual inquiry, focuses on the relationships among humans, and the tools and equipment used in day-to-day life. Contextual inquiry targets what problems deemed important to the end user should be addressed, and whether the type of personalized technology is wanted. The goals are to acquire a deep understanding of the target population’s attitudes, beliefs, and needs, including “technology readiness,” and verify potential solutions for which the technology is being designed. The first step is to assemble an interdisciplinary team of collaborators, including nurses, engineers, computer and other scientists, as well as technology designers. During this first phase, the interdisciplinary research team explores the literature to identify gaps specific to end users and the potential technology, and the nursing science focus.
The next step in this phase is to identify end users, including individuals, families, and healthcare providers, representative of a diverse pool of possible users, taking into consideration the issues of health disparities, culture, and literacy. The team would then identify end-user specific needs (i.e., how technology can aid in the design of interventions to facilitate patient or caregiver–provider communication and reduce symptom burden) and then collect iterative feedback through focus groups or interviews using participatory design sessions that engage end users. One strategy to guide this process is “design thinking,” which is a user-centered process that provides an organizational framework, leverages collective expertise, and encourages innovation (Gibbons, 2016; Joe, Chaudhuri, Le, Thompson, & Demiris, 2015). Data from focus groups should be analyzed using qualitative research techniques to establish themes, including individual values related to technology, to guide the next step of the roadmap.
In Step 2, value specification, end-user values are translated into end-user requirements. The goal of this step is to understand how the technology should be personalized. The activities begin with a second round of focus groups to collect more detailed and purpose-driven data. These data clearly define user needs, technology requirements, and feature specifications, as well as end-user constraints such as performance expectancy, effort expectancy, social influence, technology anxiety, behavioral intention (to adopt and maintain use), and resistance to change. UTAUT2 is an excellent model to guide this process (Venkatesh et al., 2012). The next part of this phase is to identify system level constraints, such as availability or appropriateness of resources or expertise, for intervention development and costs.
The purpose of Step 3, design, is to verify that the technology or device can be created (i.e., resources are available, costs are aligned with budget) and to develop the prototype(s) using technology design concepts that conform to user values and the exact technical specifications. The design requirements depend on the modality. For example, an Internet intervention will have design features very different from those of a tablet- or phone-based app. The design should be intuitive so that it “thinks” the same way as the end user, uses support systems currently in existence (such as where end users will access the tool or intervention), and contains human-centered design features that mimic end-user characteristics specific to geography, capabilities, and access. The Hierarchy of Needs design is one model to effectively guide this activity (Bradley, 2010).
Step 3 establishes the information architecture so that information is tailored and meaningful to the end users and evaluates system level functionality, including user-friendliness, feasibility of use in the environment, responsiveness, and costs including hardware and software, and technology support needs (e.g., management of data portals). During this phase, the team creates and tests a prototype with the goal of obtaining end-user feedback to assess the effectiveness and efficiency of the prototype. The meaning that the end users attach to a technology and its uses can vary widely. These factors are critical to understanding and establishing predictors of use and achievement of intended behaviors. The Consumer Acceptance component of the UTAUT2 model is an example of a quantitative approach that could guide this process (Venkatesh et al., 2012).
In Step 4, operationalization, the intervention is used in a real-world setting. End users are taught to use the technology, a plan for adoption is developed, and workflow (i.e., length of training, questions asked, problems encountered) is evaluated. In this step, a feasibility trial is conducted with a small number of stakeholders. This step incorporates the explore phase outlined in Nielsen Norman Group’s Design Thinking Model (Gibbons, 2016) and the ideation phase from The Field Guide to Human-Centered Design (IDEO.org, 2015).
In Step 5, summative evaluation, collection of viability metrics, including the analysis of process data, is a major priority. To accomplish these goals, patterns of technology use and the intervention for which the technology was developed (e.g., how long it takes to use the technology-based intervention) and whether the technology and the intervention have the desired effect are measured. A fourth round of end-user feedback via qualitative (open-ended survey questions) and quantitative approaches to determine desirability, expectancy, and credibility of the intervention is then conducted. The Credibility/Expectancy Questionnaire is an example of a useful instrument to assess these concepts (Devilly & Borkovec, 2000; Kazdin, 1979). Based on these findings, the technology and the intervention are refined with respect to scalability, equitable allocation, and accessibility. Benchmarks for success are established at this step. Once the technology-based intervention development outcomes are achieved, design of a business model where cost effectiveness and sustainability are assessed, and exploration of adaption of the technology and intervention for other populations occur. Finally, a pilot study is conducted to establish preliminary outcomes on clinical feasibility and efficacy as well as clinical validity when applicable.
Ensuring that the theoretical underpinnings, selection of appropriate technology design, incorporation of end-user feedback, and the tailoring interventions are all reflective of the culture and health-literacy of the intended users are critical elements of intervention development. Interventions that are developed within frameworks that encourage the involvement of end users in the process, such as the CeHRes Roadmap, will be more suited for personalized use, better tailored for implementation in the intended environment or social context, and more likely to show evidence of efficacy. Well-developed interventions can make important contributions to improving individual and family health. If individuals, families, and healthcare providers have positive experiences with technology-based interventions, they may be more likely to adopt or recommend them in the future.
Discussion
The integration and advancement of technologies to support precision health provides an opportunity to collectively expand the field of nursing science. Many of the pilot studies from the current NINR Research Centers are integrating machine learning algorithms to identify phenotypes through pattern recognition, application rules to automate instant responses during data collection, or data visualization to disseminate customized data back to the end user. These methods can promote end-user engagement and provide the means to tailor interventions to the needs of the end user.
When conducting research using existing technology, scientists should report specific information on the model or version used, usage by participants, and settings used in the study to assist with identifying end-user use behaviors. For studies that develop technologies to support precision health, several additional details are needed to enhance rigor and reproducibility, including explication of theoretical underpinnings in the choice of technology, population focus, populations involved in the participatory design sessions and a summary of findings, application of user-centered models, and processes of testing and refining the technology.
The opportunity to develop and design user-centered technologies to support precision health can be enhanced using this new roadmap. The steps of the NINR Centers roadmap (contextual inquiry, value specification, design, operationalization, and summative evaluation) provide a foundation for the personalization of technology. In addition, the roadmap provides the steps to enhance data capture over time to advance phenotyping or to deliver nurse-driven self-management interventions. Finally, the innovative use of technology to support precision health may provide opportunities for increasing accessibility to highly effective and precisely targeted options for care that are tailored to the needs of diverse individuals across different settings.
Conclusions
The NINR Research Centers provide a unique contribution to the design and use of technologies in the support of precision health. Technology use to characterize symptom phenotypes and identify biomarkers, as well as to deliver tailored interventions across a wide array of conditions, are currently in use. Technology can be a powerful tool when designed within a user-centered framework. To optimize how technologies are used to support nursing science, the theoretical linkage between an intervention and technology use must be explicit, with transparency in the methods used during user-centered design, testing, and evaluation. Best practices for engaging minority and underserved populations and increasing access to these technologies should also be incorporated to prevent widening health disparities.
While the incorporation of technology to enhance self- and symptom-management has exponentially increased, it is critical that data to support its use in clinical practice be rigorous and reproducible. As outlined in this article, the use of a standard multistep process for the development and testing of technology is essential and relevant to nursing research being conducted around the globe. Nurse scientists and their interdisciplinary teams can use this roadmap in the development of novel technologies or in the application of existing technologies. Overall, the support of precision health and delivery of personalized interventions that improve health and well-being are goals that are consistent with nursing science and precision health.
Clinical Resources.
Center for Accelerating Precision Pain Self-Management, University of Connecticut. https://cappsm.nursing.uconn.edu
Center for Complexity and Self-Management of Chronic Disease (CSCD), University of Michigan. http://www.socr.umich.edu/CSCD/
Center for Innovation in Sleep Self-Management, University of Washington. https://nursing.uw.edu/research/programs/sleep-research/
Center for Transdisciplinary Collaborative Research in Self-Management Science, University of Texas, Austin. http://nursing.utexas.edu/tcrss/
Northeastern Center for Technology in Support of Self-Management and Health, Northeastern University. http://www.northeastern.edu/nucare/
Omics Associated with Self-Management Interventions for Symptoms (OASIS) Center, University of Maryland, Baltimore. http://www.nursing.umaryland.edu/research/oasis/
Precision in Symptom Self-Management (PriSSM), Columbia University. http://nursing.columbia.edu/research/precision-symptom-self-management-prissm-center
Self-Management Science Center at the University of Wisconsin, University of Wisconsin-Milwaukee. https://uwm.edu/nursing/about/centers-institutes/self-management/
SMART Center II, Case Western University. https://nursing.case.edu/research/centers/smart/
Symptom Self-Management Center, Medical University of South Carolina. http://academicdepartments.musc.edu/nursing/initiatives/researchoffice/ssmc.htm
UManage Center for Building the Science of Self-Management, University of Massachusetts, Amherst. https://www.umass.edu/nursing/UManage-Center
Yale Center for Sleep Disturbance in Acute and Chronic Conditions, Yale University. http://sleep.yale.edu/yale-center-sleep-disturbance
Acknowledgment
The Centers are supported by the National Institute of Nursing Research: P20 NR014126, P20 NR015320, P20 NR015331, P20 NR015339, P30 NR015326, P30 NR015335, P20 NR016575, P20 NR016599, P20 NR016605, P30 NR016585, P30 NR016587, P30 NR016579.
References
- Bailey SC, O’Conor R, Bojarski EA, Mullen R, Patzer RE, Vicencio D, … Wolf MS (2015). Literacy disparities in patient access and health-related use of internet and mobile technologies. Health Expectations, 18(6), 3079–3087. 10.1111/hex.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakken S, & Reame N (2016). The promise and potential perils of big data for advancing symptom management research in populations at risk for health disparities. Annual Review of Nursing Research, 34, 247–260. 10.1891/0739-6686.34.247 [DOI] [PubMed] [Google Scholar]
- Bradley S (2010). Designing for a hierarchy of needs. Smashing Magazine, April(26). Retrieved from https://www.smashingmagazine.com/2010/04/designing-for-a-hierarchy-of-needs/ [Google Scholar]
- Casillas A, Moreno G, Grotts J, Tseng CH, & Morales LS (2018). A digital language divide? The relationship between internet medication refills and medication adherence among limited English proficient (LEP) patients. Journal of Racial & Ethnic Health Disparities, 5(6), 1373–1380. 10.1007/s40615-018-0487-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devilly GJ, & Borkovec TD (2000). Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavioral Therapy and Experimental Psychiatry, 31(2), 73–86. 10.1016/S0005-7916(00)00012-4 [DOI] [PubMed] [Google Scholar]
- DeVito Dabbs A (2018, May 1). The design and development of personalized precision health technology Lecture presented at NINR Center Directors’ Meeting. Bethesda, MD. [Google Scholar]
- Gibbons S (2016). Design thinking 101. Retrieved from https://www.nngroup.com/articles/design-thinking/
- Gordon NP, & Hornbrook MC (2016). Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: A database and survey study of seniors in a large health plan. Journal of Medical Internet Research, 18(3), e50 10.2196/jmir.5105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady P (2017). Advancing science, improving lives: NINR’s new strategic plan and the future of nursing science. Journal of Nursing Scholarship, 49(3), 247–248. 10.1111/jnu.12286 [DOI] [PubMed] [Google Scholar]
- Greenberg AJ, Haney D, Blake KD, Moser RP, & Hesse BW (2017). Differences in access to and use of electronic personal health information between rural and urban residents in the United States. Journal of Rural Health, 34(Suppl. 1), s30–s38. 10.1111/jrh.12228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey K, Bakken S, Byrne M, Bailey D, Demiris G, & Grady P (2019). Precision health: Advancing symptom and self-management science. Nursing Outlook, 67(4), 462–475. 10.1016/j.outlook.2019.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, & Rivera-Rodriguez AJ (2013). SEIPS 2.0: A human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics, 56(11), 1669–1686. 10.1080/00140139.2013.838643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IDEO.org. (2015). The field guide to human-centered design. Retrieved from http://www.designkit.org/resources/1
- Jacob E, Pavlish C, Duran J, Stinson J, Lewis MA, & Zeltzer L (2013). Facilitating pediatric patient-provider communications using wireless technology in children and adolescents with sickle cell disease. Journal of Pediatric Health Care, 27(4), 284–292. 10.1016/j.pedhc.2012.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe J, Chaudhuri S, Le T, Thompson H, & Demiris G (2015). The use of think-aloud and instant data analysis in evaluation research: Exemplar and lessons learned. Journal of Biomedical Informatics, 56, 284–291. 10.1016/j.jbi.2015.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman DR, Patel VL, Hilliman C, Morin PC, Pevzner J, Weinstock RS, … Starren J (2003). Usability in the real world: Assessing medical information technologies in patients’ homes. Journal of Biomedical Informatics, 36(1–2), 45–60. 10.1016/S1532-0464(03)00056-X [DOI] [PubMed] [Google Scholar]
- Kazdin AE (1979). Therapy outcome questions requiring control of credibility and treatment-generated expectancies. Behavior Therapy, 10(1), 81–93. 10.1016/S0005-7894(79)80011-8 [DOI] [Google Scholar]
- Macefield R (2009). How to specify the participant group size for usability studies: A practitioner’s guide. Journal of Usability Studies, 5(1), 34–45. Retrieved from http://uxpajournal.org/wp-content/uploads/sites/8/pdf/JUS_Macefield_Nov2009.pdf [Google Scholar]
- Marquard J (2018, May 1). Opportunities for personalized precision health technology use in health monitoring Lecture presented at NINR Center Directors’ Meeting, Bethesda, MD. [Google Scholar]
- McCurdie T, Taneva S, Casselman M, Yeung M, McDaniel C, Ho W, & Cafazzo J (2012). mHealth consumer apps: The case for user-centered design. Biomedical Instrumentation & Technology, 46(Suppl. 2), 49–56. 10.2345/0899-8205-46.s2.49 [DOI] [PubMed] [Google Scholar]
- Medlock MC, Wixon D, McGee M, & Welsh D (2005). The rapid iterative test and evaluation method: Better products in less time In Bias RG & Mayhew DJ (Eds.), Cost-justifying usability (2nd ed, pp. 489–517). San Francisco: Morgan Kaufmann. [Google Scholar]
- National Institute of Nursing Research. (2016). The NINR strategic plan: Advancing science, improving lives. Bethesda, MD: National Institutes of Health Publication; https://www.ninr.nih.gov/sites/files/docs/NINR_StratPlan2016_reduced.pdf [Google Scholar]
- Reblin M, Wu YP, Pok J, Kane L, Colman H, Cohen AL, … Agutter J (2017). Development of the electronic social network assessment program using the Center for eHealth and Wellbeing research roadmap. JMIR Human Factors, 4(3), e23 10.2196/humanfactors.7845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawers P (2017, June 13). 5 billion people now have a mobile phone connection, according to GSMA data. Retrieved from https://venturebeat.com/2017/06/13/5-billion-people-now-have-a-mobile-phone-connection-according-to-gsma-data/ [Google Scholar]
- Snodgrass A, & Coyne R (1992). Models, metaphors and the hermeneutics of designing. Design Issues, 9(1), 56–74. 10.2307/1511599 [DOI] [Google Scholar]
- Venkatesh V, Morris MG, Davis GB, & Davis FD (2003). User acceptance of information technology: Toward a unified view. MIS Quarterly, 27(3), 425–478. 10.2307/30036540 [DOI] [Google Scholar]
- Venkatesh V, Thong J, & Zu X (2012). Consumer acceptance and use of information technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Quarterly, 36(1), 157–178. 10.2307/41410412 [DOI] [Google Scholar]
- Virzi RA (1992). Refining the test phase of usability evaluation: How many subjects is enough? Human Factors, 34(4), 457–468. 10.1177/001872089203400407 [DOI] [Google Scholar]
- Zabler B, Tsai PY, Fendrich M, Cho Y, Taani MH, & Schiffman R (2018). Effect of a nurse case management intervention for hypertension self-management in low-income African Americans. Contemporary Clinical Trials, 71, 199–204. 10.1016/j.cct.2018.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]


