Abstract
CONTEXT
Women may be at risk for unintended pregnancy if they forgo contraception or use ineffective methods because they erroneously believe they are unlikely to conceive. However, the relationship between perceived susceptibility to pregnancy and contraceptive use is not fully understood.
METHODS
Data collected in 2014–2016 for the Examining Contraceptive Use and Unmet Needs study were used to examine perceived susceptibility to pregnancy among 969 women veterans aged 20–45 who were at risk for unintended pregnancy and received primary care through the U.S. Veterans Administration system. Multivariable logistic regression was used to identify associations between perceived susceptibility to pregnancy (perceived likelihood during one year of unprotected intercourse) and use of any contraceptive at last sex. Multinomial regression models were used to examine method effectiveness among women who used a contraceptive at last sex.
RESULTS
Forty percent of women perceived their susceptibility to pregnancy to be low. Compared with women with high perceived susceptibility to pregnancy, those with low perceived susceptibility were less likely to have used any contraceptive at last sex (86% vs. 96%; adjusted odds ratio, 0.2). Among contraceptive users, women with low perceived susceptibility were less likely than those with high perceived susceptibility to have used a highly effective method (26% vs. 34%; adjusted relative risk ratio, 0.6) or moderately effective method (34% vs. 39%; 0.6) at last sex.
CONCLUSIONS
Identifying and addressing fertility misperceptions among women with low perceived susceptibility to pregnancy could help promote informed decision making about contraception and reduce the risk of unintended pregnancy.
During their reproductive years, women may develop doubts about their ability to become pregnant. For some women, those doubts may reflect medically defined infertility, which is the absence of pregnancy after a year of regular sexual intercourse without contraception.1 In the United States, the prevalence of infertility ranges from 7% to 15%, depending on the estimation approach used.2 However, the proportion of women who fear that they cannot conceive may be much larger. In one nationally representative study, concerns about being able to get pregnant were reported by 40% of women aged 18–40 who were not attempting to conceive and by 70% of women who were trying to do so.3 In a nationally representative telephone survey, 19% of unmarried women aged 18–29 reported believing they were very likely to be infertile; only 41% of these women indicated that this perception was based on information from a doctor.4
Concerns about fertility appear to arise for a variety of reasons, though these reasons are not fully characterized in the literature. Women may begin to question their fertility if they have engaged in unprotected intercourse without becoming pregnant.5–7 Such questioning may be fostered by an overestimation of the likelihood of pregnancy from a single act of unprotected intercourse.8 In some studies, women who were seeking an abortion reported having believed that their fertility was impaired because of their family history4 or because of medical conditions (e.g., polycystic ovarian syndrome or anemia) or treatments;9 other women could not identify a reason for their belief that they were subfecund or infertile.9 While some fertility concerns are certainly well-founded, misconceptions about one’s fertility are common among women who subsequently become pregnant, as seen among 42% of a sample of pregnant women seeking abortion services6 and 42% of another sample of pregnant adolescents.10 Because misperceptions about fertility appear to be common, it is important to understand how they develop, as well as whether and how they influence health behaviors, such as contraceptive use. We lack a full characterization of the relationship between fertility perceptions and contraceptive use among women who do not have an infertility diagnosis and are not trying to become pregnant.
To elucidate the relationship between fertility perceptions and contraceptive use, we used data from a nationally representative survey of women veterans who received primary care within the Department of Veterans Affairs (VA) Healthcare System, the largest integrated health care system in the United States. VA policies specify that comprehensive women’s health care in the VA system includes care from a provider who is competent in contraceptive management and access to contraceptives at low or no cost.11 Women can obtain hormonal contraceptive methods through a VA pharmacy, either in person or by mail, for a fixed copay of $9; no copay is required of women who meet certain eligibility criteria, such as having been discharged from service in Afghanistan or Iraq within the last five years or having been disabled by an injury or illness incurred during active military service. Long-acting reversible contraceptives (IUDs and implants) are available at no cost. If a woman’s primary care provider is not trained to insert long-acting reversible contraceptives, she can obtain a referral to a gynecologist, either on site or at another VA facility or a contracted non-VA facility. Rates of contraceptive use, unmet need for prescription contraceptives and unintended pregnancy among woman veterans are similar to those in the general U.S. population.12
When viewed through the lens of such theoretical models as the health belief model and the theory of reasoned action, fertility perceptions can be regarded as potential antecedents of family planning behaviors. These models posit that an individual’s perception of the likelihood of an outcome can shape preventive health behaviors.13 Women who do not desire to become pregnant may choose to not use contraceptives if they believe that pregnancy is an unlikely outcome.5,6,14 For example, in a recent longitudinal analysis, women aged 25–30 were less likely to use contraceptives if they considered themselves somewhat likely or not very likely (rather than very likely) to get pregnant and have a live birth.15 Our objective was to identify characteristics associated with low perceived susceptibility to pregnancy, and to assess the relationship between perceived susceptibility and current contraceptive use in a sample of women veterans at risk for unintended pregnancy.
METHODS
Data
We analyzed data collected as part of the Examining Contraceptive Use and Unmet Needs (ECUUN) study, which included a survey of a national random sample of women veterans aged 18–44 who had received primary care within the VA health care system in the previous year. Potentially eligible women were identified through administrative data, and mailed a study packet that included an invitation letter, a study brochure and a postage-paid reply card that they could send to opt out of further communication. Study personnel telephoned women who did not opt out (or who expressed interest) to assess (or confirm) their interest in participating and their eligibility. Women who were interested and eligible provided verbal informed consent over the phone. Of the 8,198 women who were invited to participate, 2,769 were screened, provided consent and enrolled (a 28% response rate), and 2,302 completed the survey (an 83% completion rate). Trained interviewers used computer-assisted telephone interview technology to conduct interviews between April 2014 and January 2016. A $30 honorarium was provided to women for their participation. Institutional review boards at the University of Pittsburgh and VA Pittsburgh approved the study.
Participants were similar to nonparticipants with respect to age, race and ethnicity, marital status, income, history of medical illness, history of mental illness and geographic region; thus, the ECUUN sample can be considered representative of the larger population of women of reproductive age who receive VA care. Additional details about study design and recruitment have been published elsewhere.12
For this analysis, the sample was restricted to the 969 women who were at risk for unintended pregnancy: those who reported having had heterosexual intercourse in the past year, were not pregnant or trying to become pregnant, reported no history of hysterectomy or provider-diagnosed infertility, and were not using male or female sterilization for contraception.
Measures
Our primary independent variable was perceived susceptibility to pregnancy, which was assessed by asking participants to indicate their likelihood of becoming pregnant if they were to have unprotected sex for a year. Response options were very unlikely, unlikely, neither likely nor unlikely, likely, or very likely; the wording of the survey item—“If I am sexually active with a man over the next year and do not use any form of birth control or contraception, I would become pregnant”—was adapted from the Contraceptive Utilities Intention and Knowledge Scale (CUIKS).16 A small number of women (12) told the data collectors that they did not know their likelihood of pregnancy. Because 85% of women, on average, will become pregnant after a year of sexual intercourse without contraception,17 we categorized the responses “likely” or “very likely” as indicating high perceived susceptibility to pregnancy, and all others as indicating low perceived susceptibility.
We created models for two outcomes: the use of any contraceptive at last intercourse, and the effectiveness of the method among women who used one. Methods were classified as highly effective (IUD and implant), moderately effective (pill, patch, ring and injectable) or least effective (barrier methods, fertility awareness methods and withdrawal). If women reported having used more than one method, categorization was according to the most effective method used.
Our analysis also included a number of demographic and health characteristics, which were chosen because of their theoretical or empirical associations with contraceptive use, fertility perceptions or both. The demographic characteristics were age (categorized as 20–29, 30–34, 35–39 or 40–45*), race and ethnicity (white, black, Hispanic or other), marital status (never married; married or living with partner; or divorced, separated or widowed), educational level (had college degree or not), religion (Protestant, Catholic, other Christian, other or none) and annual household income ($0–19,999, $20,000–59,999, or $60,000 or more). Health-related variables were having ever been pregnant, having had a stillbirth, having had a miscarriage, having a history of mental illness (depression, bipolar disorder, posttraumatic stress disorder, schizophrenia, anxiety disorder or panic disorder), having a history of medical illness that could affect contraceptive use (hypertension, thromboembolic disease, coronary artery disease, breast cancer, stroke, liver disease, HIV/AIDS, diabetes, migraine, lupus or seizure disorder) and body mass index (less than 25, 25–30 or greater than 30 kg/m2).
Consistent with standard VA clinical screening items, we classified women as having a history of military sexual trauma if they answered “yes” to either of two questions: “While you were in the military, did you ever receive uninvited and unwanted sexual attention, such as touching, cornering, pressure for sexual favors, or verbal remarks?” or “Did someone ever use force or the threat of force to have sexual contact with you against your will?” We also assessed women’s knowledge of the general likelihood of pregnancy by asking, “If 100 sexually active women of reproductive age did not use any birth control for 1 year, about how many will typically get pregnant?” Women were categorized as having correct knowledge if they selected response option “85” (other options were 3, 20, 50 and don’t know).17
Analysis
We generated descriptive statistics for demographic variables, health characteristics, knowledge of general likelihood of pregnancy and perceived susceptibility to pregnancy. We used chi-squared tests to examine bivariate associations between women’s characteristics and their perceived susceptibility to pregnancy, between perceived susceptibility to pregnancy and contraceptive use at last sex, and between perceived susceptibility and the effectiveness of the method used among women who had used a method.
We used multivariable logistic regression to model use of any contraceptive, with perceived susceptibility to pregnancy as the primary predictor; results are reported as adjusted odds ratios. Next, we used multivariable multinomial logistic regression to model the relationship between perceived susceptibility to pregnancy and method effectiveness among women who had used a method at last sex. Specifically, we compared use of a highly effective method with use of one of the least effective methods, and use of a moderately effective method with use of one of the least effective methods; results are reported as adjusted relative risk ratios. For all models, we decided a priori to include age, race and ethnicity, and annual household income as covariates. In addition, we included other variables that were associated with low perceived susceptibility in bivariate analyses at the p<.20 level. Because women’s ability to get pregnant declines with age,18 we also tested an interaction between perceived susceptibility and the age category.
RESULTS
Sample Characteristics
The 969 women veterans in the sample were 20–45 years old when they were interviewed; nearly three-fifths were aged 30–39 (Table 1). Slightly more than half were white (52%), while 28% were black, 13% were Hispanic and 7% reported another racial identity (multiracial, Asian, Pacific Islander or Native American). About half of participants were married or living with a partner, and a similar proportion had at least a college degree. Twenty-six percent were Catholic or Protestant, and 41% described themselves as “other Christian.” More than half reported an annual household income between $20,000 and $59,999.
TABLE 1.
Percentage distribution of women veterans aged 20–45, by selected characteristics, according to perceived susceptibility to pregnancy, Examining Contraceptive Use and Unmet Needs study, 2014–2016
| Characteristic | All (N=969) | Perceived susceptibility to pregnancy |
|
|---|---|---|---|
| Low (N=392) | High (N=577) | ||
| Age | ** | ||
| 20–29 | 28.6 | 25.0 | 31.0 |
| 30–34 | 34.3 | 32.1 | 35.7 |
| 35–39 | 23.6 | 26.0 | 22.0 |
| 40–45 | 13.5 | 6.8 | 11.3 |
| Race/ethnicity | |||
| White | 51.8 | 51.0 | 52.3 |
| Black | 27.6 | 28.6 | 26.9 |
| Hispanic | 13.4 | 12.8 | 13.9 |
| Other | 7.2 | 7.7 | 6.9 |
| Marital status‡ | * | ||
| Never married | 25.2 | 28.6 | 22.9 |
| Married/living with partner | 47.5 | 43.0 | 50.6 |
| Divorced/separated/widowed | 27.3 | 28.4 | 26.5 |
| Has college degree | |||
| Yes | 52.6 | 52.6 | 52.7 |
| No | 47.4 | 47.4 | 47.3 |
| Religion‡ | |||
| Protestant | 12.7 | 12.5 | 12.9 |
| Catholic | 13.5 | 12.0 | 14.4 |
| Other Christian | 41.1 | 44.5 | 39.0 |
| Other | 13.0 | 10.7 | 14.6 |
| None | 19.7 | 20.5 | 19.1 |
| Annual household income (US$)‡ | |||
| 0–19,999 | 23.0 | 23.8 | 22.5 |
| 20,000–59,999 | 54.3 | 55.0 | 53.9 |
| ≥60,000 | 22.7 | 21.2 | 23.7 |
| Ever pregnant‡ | *** | ||
| Yes | 71.7 | 62.8 | 77.6 |
| No | 28.3 | 37.2 | 22.4 |
| Ever had stillbirth | |||
| Yes | 0.8 | 0.8 | 0.9 |
| No | 99.2 | 99.2 | 99.1 |
| Ever had miscarriage | |||
| Yes | 22.3 | 21.3 | 23.1 |
| No | 77.7 | 78.7 | 76.9 |
| Knows general likelihood of pregnancy | *** | ||
| Yes | 46.1 | 37.8 | 51.8 |
| No | 53.9 | 62.2 | 48.2 |
| History of mental illness | † | ||
| Yes | 64.8 | 67.4 | 63.1 |
| No | 35.2 | 32.6 | 36.9 |
| History of medical illness | † | ||
| Yes | 50.6 | 53.3 | 48.7 |
| No | 49.4 | 46.7 | 51.3 |
| Body mass index (kg/m2)‡ | |||
| <25 | 34.3 | 31.4 | 36.3 |
| 25–30 | 33.8 | 34.7 | 33.2 |
| >30 | 31.9 | 33.9 | 30.5 |
| History of military sexual trauma | |||
| Yes | 52.5 | 52.0 | 52.9 |
| No | 47.5 | 48.0 | 47.1 |
| Total | 100.0 | 100.0 | 100.0 |
p≤.05.
p≤.01.
p≤.001.
p<.20.
A small number of responses were missing for measures of marital status (one), religion (three), income (12), ever pregnant (two) and body mass index (seven).
Notes: p values indicate differences in distributions between the high and low perceived susceptibility groups and are from chi-squared tests for all measures except “ever had stillbirth,” for which Fisher’s exact test was used because of small cell counts. Percentages may not total 100.0 because of rounding.
Seventy-two percent of participants had been pregnant at least once. Twenty-two percent had experienced a miscarriage, and 1% had had a stillbirth. Only 46% of women correctly identified the general likelihood of getting pregnant in one year.
Substantial proportions of women had a history of mental illness (65%) or a history of a medical illness that could affect contraceptive use (51%). The sample was split almost equally among the three body mass index groups. More than half (53%) of the sample reported having experienced sexual trauma during their time in the military.
When asked to estimate their likelihood of becoming pregnant if they were to have unprotected sex for a year, 17% of participants said they were very unlikely, 10% said they were unlikely, 1% did not know, 12% said they were neither unlikely nor likely, 12% said they were likely and 48% said they were very likely (not shown). Thus, by our definition, 40% of the sample perceived their susceptibility to pregnancy as low and 60% as high. The two perceived susceptibility groups differed by age and marital status, and women with low perceived susceptibility were less likely than those with high perceived susceptibility to have ever been pregnant (63% vs. 78%) and to know the general likelihood of getting pregnant (38% vs. 52%). No differences between groups were evident for the other characteristics.
Contraceptive Use
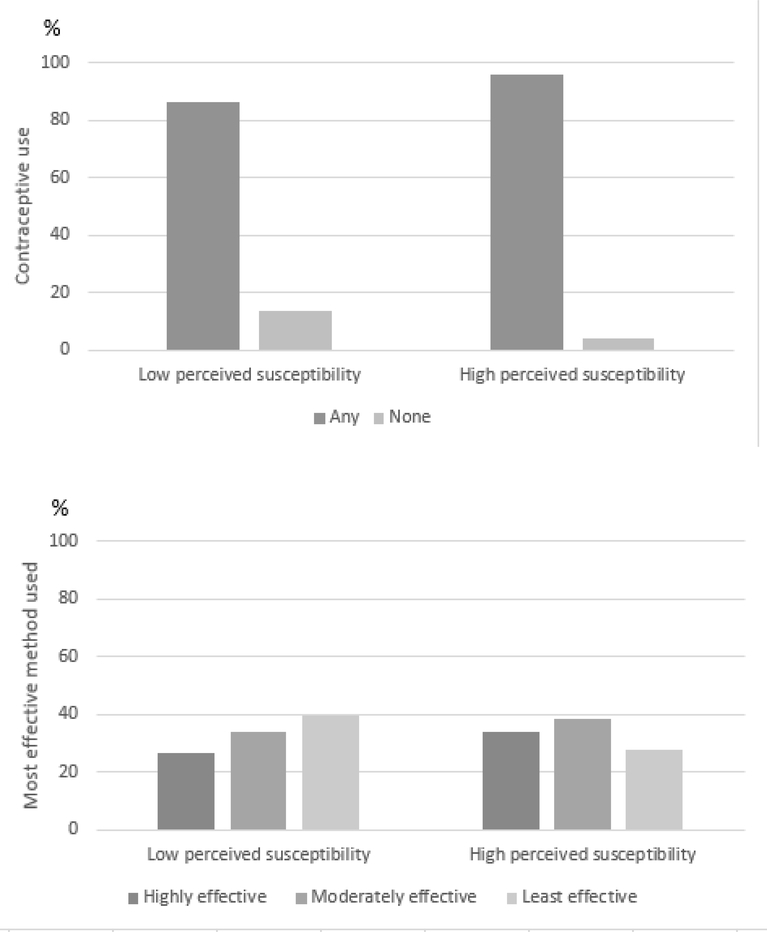
Ninety-two percent of the women had used some form of contraceptive at last intercourse, while 8% had not (not shown). Contraceptive use differed significantly by perceived susceptibility to pregnancy: At last sex, 86% of women with low perceived susceptibility had used contraceptives, compared with 96% of women with high perceived susceptibility (Figure 1). Of those who had used any type of contraceptive, 31% had used a highly effective method, 37% a moderately effective method and 32% one of the least effective methods. This distribution differed by women’s perceived susceptibility to pregnancy, such that 40% of those with low perceived susceptibility, but only 28% of those with high perceived susceptibility, had used one of the least effective methods; conversely, use of a highly effective method was reported by 34% of women with high perceived susceptibility, but only 26% of those with low perceived susceptibility.
FIGURE 1. Percentage distribution of women veterans aged 20–45, by use of any contraceptive at last intercourse; and percentage distribution of contraceptive users, by effectiveness of method used at last sex—all by perceived susceptibility to pregnancy.
Note: Use of any contraceptive and effectiveness of method used both differed between low and high perceived susceptibility groups at p<.001.
In multivariable analyses (Table 2), women veterans with low perceived susceptibility to pregnancy were less likely than those with high perceived susceptibility to have used any contraceptive at last sex (adjusted odds ratio, 0.2). There was no interaction between perceived susceptibility and age (not shown). No other variables were associated with use of any contraceptive.
TABLE 2.
Adjusted odds ratios (and 95% confidence intervals) from logistic regression analysis examining relationship between selected characteristics and use of any contraceptive at last intercourse among women veterans at risk for unintended pregnancy; and relative risk ratios (and 95% confidence intervals) from multinominal logistic regression analyses examining method effectiveness among those who had used a method at last sex
| Characteristic | Any contraceptive use | Highly effective vs. least effective method | Moderately effective vs. least effective method |
|---|---|---|---|
| Perceived susceptibility to pregnancy | |||
| High (ref) | 1.00 | 1.00 | 1.00 |
| Low | 0.24 (0.14–0.42)*** | 0.62 (0.43–0.89)* | 0.59 (0.41–0.83)** |
| Age | ** | ||
| 20–29 (ref) | 1.00 | 1.00 | 1.00 |
| 30–34 | 1.83 (0.87–3.88) | 0.85 (0.53–1.36) | 1.11 (0.72–1.72) |
| 35–39 | 0.85 (0.41–1.77) | 0.61 (0.37–1.03) | 0.49 (0.30–0.82)** |
| 40–45 | 0.67 (0.30–1.49) | 0.47 (0.25–0.88)* | 0.59 (0.33–1.07) |
| Race/ethnicity | * | ||
| White (ref) | 1.00 | 1.00 | 1.00 |
| Black | 0.79 (0.43–1.44) | 0.68 (0.44–1.04) | 0.77 (0.51–1.16) |
| Hispanic | 0.67 (0.32–1.37) | 0.42 (0.24–0.74)** | 0.60 (0.37–0.99)* |
| Other | 1.30 (0.43–3.92) | 0.72 (0.37–1.37) | 0.53 (0.27–1.04) |
| Marital status | ** | ||
| Never married (ref) | 1.00 | 1.00 | 1.00 |
| Married/living with partner | 0.64 (0.31–1.29) | 1.95 (1.21–3.14)** | 1.61 (1.03–2.53)* |
| Divorced/separated/widowed | 1.13 (0.52–2.44) | 1.04 (0.63–1.72) | 1.40 (0.88–2.23) |
| Annual household income (US$) | ** | ||
| 0–19,999 (ref) | 1.00 | 1.00 | 1.00 |
| 20,000–59,999 | 1.59 (0.84–3.02) | 2.07 (1.31–3.27)** | 1.64 (1.08–2.50)* |
| ≥60,000 | 1.13 (0.52–2.48) | 1.71 (0.95–3.08) | 1.61 (0.93–2.79) |
| Ever pregnant | |||
| No (ref) | 1.00 | 1.00 | 1.00 |
| Yes | 0.55 (0.29–1.08) | 1.20 (0.76–1.89) | 0.58 (0.39–0.88)** |
| Knows general likelihood of pregnancy | |||
| No (ref) | 1.00 | 1.00 | 1.00 |
| Yes | 1.09 (0.65–1.80) | 1.31 (0.92–1.87) | 0.98 (0.70–1.38) |
| History of mental illness | |||
| No (ref) | 1.00 | 1.00 | 1.00 |
| Yes | 0.68 (0.39–1.21) | 1.18 (0.81–1.73) | 0.98 (0.69–1.41) |
| History of medical illness | |||
| No (ref) | 1.00 | 1.00 | 1.00 |
| Yes | 0.99 (0.58–1.67) | 1.24 (0.86–1.78) | 1.04 (0.73–1.47) |
p<.05.
p<.01.
p<.001.
Notes: The logistic regression analysis included 954 women for whom data on all variables were available; the multinomial analysis included 881contraceptive users for whom data on all variables were available. Asterisks that follow odds ratios and confidence intervals indicate level of significance for differences between the relevant subgroup and the reference group; asterisks that do not follow odds ratios and confidence intervals indicate level of significance for differences among all subgroups for that variable.
In the multinomial model of contraceptive effectiveness, women with low perceived susceptibility to pregnancy were less likely than women with high perceived susceptibility to have used a highly effective method rather than one of the least effective methods (adjusted relative risk ratio, 0.6). Similarly, low perceived susceptibility was associated with a reduced likelihood of using a moderately effective method rather than a least effective one (0.6)
Other associations were also evident in the multinomial model. Use of a highly effective contraceptive method, rather than a least effective one, was less likely among women aged 40–45 than among those aged 20–29 (adjusted relative risk ratio, 0.5), as well as among Hispanic women than among white women (0.4); such use was more likely among women who were married or living with a partner than among never-married (2.0), and among women with a household income of $20,000–59,999 than among those with a lower income (2.1).
Use of a moderately effective contraceptive method, rather than one of the least effective methods, was less likely among women aged 35–39 than among those aged 20–29 (relative risk ratio, 0.5), among Hispanic women than among white women (0.6), and among women who had ever been pregnant than among those who had not (0.6). Use of a moderately effective method was more likely among women who were married or living with a partner than among never-married women (1.6), and among women with a household income of $20,000–59,999 than among those whose income was lower (1.6).
DISCUSSION
In this sample of nearly 1,000 women veterans who had received primary care through the VA, two-fifths thought their susceptibility to pregnancy was low. Despite not desiring to become pregnant, women with low perceived susceptibility were more likely to have not used contraceptives at last sex—and, if they had used contraceptives, to have used one of the least effective methods—than women with high perceived susceptibility to pregnancy. Our findings suggest that a woman’s beliefs about her ability to become pregnant may be an important and often unrecognized determinant of contraceptive behaviors that appear discordant with pregnancy intentions or goals.
As Lundsberg et al. found,3 we determined that the proportion of women who expressed doubts about their fertility was greater in our sample than that observed in other population-based studies.4,15,19 The variation in levels of perceived susceptibility may be due to differences in survey items or study populations (our sample of veterans skewed older than the civilian population). Like Gemmill,15 we found that low perceived susceptibility to pregnancy was more common among women without a prior pregnancy than among women who had been pregnant before. Nonetheless, we note that almost two-thirds of the women with low perceived susceptibility in our sample had previously had a pregnancy. Other studies have suggested that Hispanic ethnicity and lower socioeconomic status are associated with greater fertility concerns,4,15 but such associations were not seen in our sample.
The relationship we saw between low perceived susceptibility and contraceptive use was consistent with findings from other subpopulations.5,6,8,14 By documenting this association among women veterans who receive care through the VA, we show that the trend persists even in an integrated health care system where all women should have access to low- or no-cost contraceptives and contraceptive counseling. Our findings are consistent with Gemmill’s recent analysis of data from the National Longitudinal Survey of Youth, in which women who doubted their biological ability to have a child (encompassing both conception and having a live birth) were more likely than other women to forgo contraception in the following year.15 Our study expanded upon Gemmill’s in several significant ways. First, the age range was wider in our sample (20–45 vs. 25–30), and unlike Gemmill we excluded women who were trying to get pregnant or had an infertility diagnosis. In addition, our survey question did not combine perceived susceptibility to pregnancy with perceived ability to have a pregnancy resulting in a live birth. Although Gemmill found a significant bivariate association between history of miscarriage or stillbirth and a woman’s perception of her ability to become pregnant and have a live birth, we did not find associations between either history of miscarriage or history of stillbirth and perceived susceptibility to pregnancy. The absence of this association in our study leads us to suspect that women may conceptualize their ability to get pregnant as distinct from their ability to have a live birth, such that concerns about not being fertile and concerns about pregnancy loss may have distinctly different relationships with prospective contraceptive use. However, this was not our primary research question, and more research is needed to understand the distal influence of pregnancy loss on perceptions and behaviors related to unintended pregnancy prevention. Our study makes a distinct contribution to the literature in isolating women’s attitudes toward becoming pregnant from their attitudes about pregnancy outcomes.
Low perceived susceptibility to pregnancy is common, is potentially modifiable and may disrupt women’s ability to achieve their reproductive goals. For this reason, low perceived susceptibility needs to be assessed both when family planning services are delivered and in research studies assessing factors that influence contraceptive decision making. A woman who believes she cannot get pregnant may consider discussions about contraception or pregnancy planning irrelevant, adding another dimension to the growing literature about why women may not view pregnancy planning as salient.7 If such a woman has an unintended pregnancy, she has missed the opportunity to optimize her health before conceiving, which is particularly worrisome for women veterans and other populations that have high rates of medical illness, mental illness and use of medications (e.g., statins) that can cause birth defects.20 Further research could evaluate the best approaches for efficiently assessing perceived susceptibility to pregnancy in the clinical encounter and addressing any misconceptions. Patient-centered reproductive goals counseling may include screening for low perceived susceptibility to pregnancy, exploring reasons for these beliefs in a nonjudgmental manner, and offering fertility counseling or evaluation where appropriate.
According to the American College of Obstetricians and Gynecologists, a fertility evaluation is appropriate for women aged 35 or younger who have been trying to get pregnant for a year, for women older than 35 who have been trying for six months and for women older than 40 within six months of trying.1 At VA facilities, fertility evaluation and limited treatments are available for all veterans, although assisted reproductive technology and in vitro fertilization are available only for selected veterans with service-related disability that contributes to infertility.21 Whether coverage of fertility evaluations and care is adequate, accessible and equitable in the VA or other health care systems is a separate and important question that deserves attention.
Some women may truly have undiagnosed infertility, while others may have concerns that can be addressed with other resources, such as information that establishes more realistic expectations about the general likelihood of pregnancy. In our study, women veterans who incorrectly identified the general likelihood of pregnancy were more likely to have low perceived susceptibility to pregnancy than were women who knew that typically 85 out of 100 women would become pregnant after a year of sexual activity without contraceptives. We noted that almost half of the women veterans in this sample underestimated the general likelihood of pregnancy. However, in our multivariable analysis, knowledge of the general likelihood of pregnancy was not associated with contraceptive use, a finding that contrasts with results of previous studies. For example, Foster et al. found that women who thought the risk of conception from one year of unprotected intercourse was 75% or less were more likely than other women to express willingness to have unprotected sex in the next three months,6 and Biggs and Foster found that women who thought the risk was 70% or less had an elevated likelihood of having had unprotected intercourse in the last three months.22 However, it is unclear whether providing education about typical pregnancy rates would affect contraceptive behaviors, because women may put more credence in personal experiences or beliefs than in information from health care providers.23–26 We note that educational attainment was not associated with perceived susceptibility to pregnancy among our participants; more than half of our sample had a college degree, suggesting that these issues affect women who are highly educated.
Future work is needed to grapple with how to optimize the process of correcting misperceptions about typical fertility while not being dismissive of women’s experiences and understanding of their fertility. Regardless of whether education about the general likelihood of pregnancy changes women’s contraceptive behavior, it is nonetheless important—and potentially empowering—to provide women with accurate and meaningful information relevant to their health goals.
Limitations
Although this study provides new information about women’s fertility perceptions and contraceptive use, we acknowledge certain limitations. It is challenging to compare data across studies because no validated or standard assessment of fertility perceptions exists. We used an item from CUIKS to query perceived susceptibility to pregnancy, an approach that may not be comparable to other assessments in the literature, particularly those using survey items that inquire about both becoming pregnant and having a live birth.15 Because our data were cross-sectional, they cannot establish a causal relationship between measures; we recommend the use of longitudinal data collection, such as the design used by Gemmill,15 to test whether low perceived susceptibility is an antecedent to future contraceptive decision making, and if interventions that modify perceived susceptibility can increase concordance between childbearing goals and contraceptive use. Longitudinal data collection would also provide insight into the potential bidirectional or cyclical relationship between these constructs, since it is possible that not becoming pregnant after unprotected intercourse causes some women to believe they have low susceptibility even before they have met the age-specific temporal criteria for infertility. We also note that although we did not find an interaction between age and perceived susceptibility, we may not have had sufficient statistical power to detect such an interaction, and a larger sample size could clarify if the variation in the point estimates is actually statistically significant.
Our use of the ECUUN data set permits us to generalize to the population of women veterans who use the VA health care system, an important and growing population, as well as to gain insight into behavioral factors that are relevant to all women of reproductive age. In a previous analysis, characteristics of ECUUN participants were compared with age-specific estimates for women aged 20–44 with at least a high school education (or the equivalent) who had participated in the 2011–2013 National Survey of Family Growth.12 That analysis showed that high proportions of women in the ECUUN sample belonged to racial and ethnic minority groups, or had a history of medical illness, mental illness or military sexual trauma, so findings from this sample of women veterans may be generalizable to some vulnerable populations. However, because more than half of women in the ECUUN sample had at least a college degree and an income of $20,000–59,999, we caution against generalizing to women with less education or financial resources. Furthermore, since all ECUUN participants have access to the VA health care system, findings cannot be generalized to women without health insurance. Stronger inferences about perceived susceptibility to pregnancy among nonveterans would require additional investigation with a broader nationally representative sample.
Conclusions
Women veterans who are sexually active but do not want to become pregnant have an elevated likelihood of not using contraceptives or of using one of the least effective methods if they perceive that they are unlikely to become pregnant. Low perceived susceptibility to pregnancy appears to be an important construct related to family planning behaviors and may be a promising target for interventions to help women align contraceptive use with their childbearing goals. Future work should explore whether the provision of fertility assessments in health care encounters and comprehensive sex education can alter women’s perceived susceptibility to pregnancy and subsequent contraceptive choices.
Acknowledgments
The ECUUN study was supported by a grant from the U.S. Department of Veterans Affairs (IIR 12–124). The authors were supported by grants from the U.S. Department of Veterans Affairs (CDA 14-41) and the National Center for Advancing Translational Sciences (TL1TR001858). In addition, Laura Britton received support during manuscript preparation as a Hillman Scholar in Nursing Innovation and a Jonas Nurse Leader Scholar. The content of this article is solely the responsibility of the authors and does not represent the official views of the Department of Veterans Affairs, the United States Government or the National Institutes of Health.
Footnotes
No women aged 18–19 met our eligibility criteria, and several women who were aged 44 at enrollment were aged 45 at the time they were interviewed.
Contributor Information
Laura E. Britton, Columbia University School of Nursing, New York.
Colleen P. Judge-Golden, University of Pittsburgh School of Medicine, Pittsburgh.
Tierney E. Wolgemuth, University of Pittsburgh School of Medicine, Pittsburgh.
Xinhua Zhao, Center for Health Equity Research and Promotion, VA Pittsburgh Healthcare System.
Maria K. Mor, Biostatistics and Informatics Core, Center for Health Equity Research and Promotion, VA Pittsburgh Healthcare System; Department of Biostatistics, Graduate School of Public Health, University of Pittsburgh.
Lisa S. Callegari, Seattle-Denver Center of Innovation for Veteran-Centered and Value-Driven Care, VA Puget Sound, Seattle; Departments of Obstetrics & Gynecology and Health Services, University of Washington.
Sonya Borrero, Center for Health Equity Research and Promotion, VA Pittsburgh Healthcare System; Department of Medicine, University of Pittsburgh.
REFERENCES
- 1.American College of Obstetricians and Gynecologists, Treating infertility, 2017, https://www.acog.org/Patients/FAQs/Treating-Infertility.
- 2.Thoma ME et al. , Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach, Fertility and Sterility, 2013, 99(5):1324–1331.e1, 10.1016/j.fertnstert.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lundsberg LS et al. , Knowledge, attitudes, and practices regarding conception and fertility: a population-based survey among reproductive-age United States women, Fertility and Sterility, 2014, 101(3):767–774, 10.1016/j.fertnstert.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Polis CB and Zabin LS, Missed conceptions or misconceptions: perceived infertility among unmarried young adults in the United States, Perspectives on Sexual and Reproductive Health, 2012, 44(1):30–38, 10.1363/4403012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nettleman MD et al. , Reasons for unprotected intercourse: analysis of the PRAMS survey, Contraception, 2007, 75(5):361–366, 10.1016/j.contraception.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 6.Foster DG et al. , Attitudes toward unprotected intercourse and risk of pregnancy among women seeking abortion, Women’s Health Issues, 2012, 22(2):e149–e155, 10.1016/j.whi.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Borrero S et al. , “It just happens”: a qualitative study exploring low-income women’s perspectives on pregnancy intention and planning, Contraception, 2015, 91(2):150–156, 10.1016/j.contraception.2014.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biggs MA, Karasek D and Foster DG, Unprotected intercourse among women wanting to avoid pregnancy: attitudes, behaviors, and beliefs, Women’s Health Issues, 2012, 22(3):e311–e318, 10.1016/j.whi.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Frohwirth L, Moore AM and Maniaci R, Perceptions of susceptibility to pregnancy among U.S. women obtaining abortions, Social Science & Medicine, 2013, 99:18–26, 10.1016/j.socscimed.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 10.White E et al. , Fear of inability to conceive in pregnant adolescents, Obstetrics & Gynecology, 2006, 108(6):1411–1416, 10.1097/01.AOG.0000240137.99609.2e. [DOI] [PubMed] [Google Scholar]
- 11.Frayne S et al. , Sourcebook: Women Veterans in the Veterans Health Administration, Volume 3: Sociodemographics, Utilization, Costs of Care, and Health Profile, Washington, DC: Veterans Administration, 2014. [Google Scholar]
- 12.Borrero S et al. , Unintended pregnancy and contraceptive use among women veterans: The ECUUN study, Journal of General Internal Medicine, 2017, 32(8):900–908, 10.1007/s11606-017-4049-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinstein ND, Testing four competing theories of health-protective behavior, Health Psychology, 1993, 12(4):324–333. [DOI] [PubMed] [Google Scholar]
- 14.Masinter LM, Feinglass J and Simon MA, Pregnancy intention and use of contraception among Hispanic women in the United States: data from the National Survey of Family Growth, 2006–2010, Journal of Women’s Health and Law, 2013, 22(10):862–870, 10.1089/jwh.2013.4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gemmill A, Perceived subfecundity and contraceptive use among young adult U.S. women, Perspectives on Sexual and Reproductive Health, 2018, 50(3):119–127, 10.1363/psrh.12072. [DOI] [PubMed] [Google Scholar]
- 16.Davis CM et al. , eds., Handbook of Sexuality-Related Measures, Thousand Oaks, CA: SAGE Publications, 1998. [Google Scholar]
- 17.Hatcher RA et al. , Contraceptive Technology, 21st ed., New York: Ayer Company Publishers, 2018. [Google Scholar]
- 18.Wesselink AK et al. , Age and fecundability in a North American preconception cohort study, American Journal of Obstetrics & Gynecology, 2017, 217(6):667.e1–667.e8, 10.1016/j.ajog.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention, Key statistics from the National Survey of Family Growth, 2017, https://www.cdc.gov/nchs/nsfg/key_statistics.htm.
- 20.Schwarz EB et al. , Provision of potentially teratogenic medications to female veterans of childbearing age, Medical Care, 2010, 48(9):834–842, 10.1097/MLR.0b013e3181e57946. [DOI] [PubMed] [Google Scholar]
- 21.Veterans Health Administration, Infertility Evaluation and Treatment: Veterans Health Directive 1332, 2017, https://www.va.gov/VHAPUBLICATIONS/ViewPublication.asp?pub_ID=5431.
- 22.Biggs MA and Foster DG, Misunderstanding the risk of conception from unprotected and protected sex, Women’s Health Issues, 2013, 23(1):e47–e53, 10.1016/j.whi.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Carter MW et al. , A qualitative study of contraceptive understanding among young adults, Contraception, 2012, 86(5):543–550, 10.1016/j.contraception.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 24.Gilliam ML et al. , Concerns about contraceptive side effects among young Latinas: a focus-group approach, Contraception, 2004, 70(4):299–305, 10.1016/j.contraception.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 25.Yee L and Simon M, The role of the social network in contraceptive decision-making among young, African American and Latina women, Journal of Adolescent Health, 2010, 47(4):374–380, 10.1016/j.jadohealth.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guendelman S et al. , Perceptions of hormonal contraceptive safety and side effects among low-income Latina and non-Latina women, Maternal and Child Health Journal, 2000, 4(4):233–239, 10.1023/A:1026643621387. [DOI] [PubMed] [Google Scholar]