Sir,
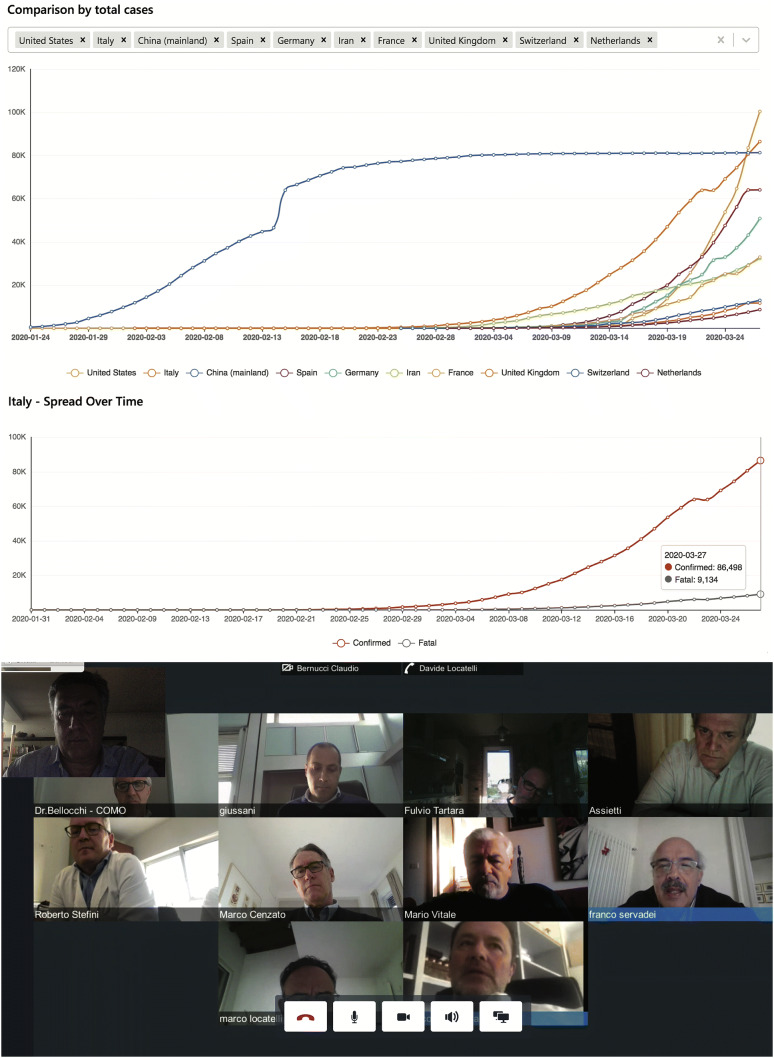
Italy has been hit hard by COVID-19, ranking #2 after the USA when it comes to patients who have been infected by this virus. Surprisingly, in our country we are also seeing an extraordinarily high mortality rate 10.6% (https://bing.com/covid retrieved on March 28th 2020—Fig. 1-top), which has not been explained yet, and may be partially related to the high percentage of elderly people in the Italian population or to the underrepresented figure of the real COVID-19 positive, yet asymptomatic patients/carriers.
Fig. 1.
COVID-19 total cases per country (top) and in Italy (middle); [source: https://bing.com/covid on March 28th 2020]. Snapshot taken during a multidisciplinary neurosurgery/neuro-oncology meeting where ‘Hub and Spoke’ physicians together take part to the teleconference (bottom)
Hospitals workload has become hectic. This poses a threat to the everyday work of a neuro-oncology unit. The main limiting factor is represented by ICU’s, which are stuck, since ∼10% of the patients need intensive care at a certain point [1]. As neurosurgical oncology often demands for ICU admission in the early post-op, it is clear how such an epidemic can affect this neurosurgical subspecialty, on top of others. Besides, neuro-oncological patients may be immunocompromised, presenting the ethical dilemma of having them at the same hospital where COVID-19 patients are. As per the epidemic spreading curves (Fig. 1—middle) it is foreseeable that other countries may experience similar emergency situations in the near future.
Lombardy is the Italian region which has been most heavily affected by this epidemic. The C. Besta Neurological Institute has a long-standing tradition as a national large-volume center mainly committed to neuro-oncology; it does not have an A&E Dept.; so far, we managed to keep it as a COVID-19-free hospital, enforcing a strict control policy for all admitted patients, relatives, and visitors. Because of these peculiar features, in an effort to preserve the availability of ICU beds for COVID-19 patients as much as possible, the C. Besta Institute has been designated as the regional centralizing neurosurgery HUB for neuro-oncology [2], while all other Centers’ activity has been progressively quenched, according to a Hub and Spoke organizational scheme. This operative network became effective on March 16th, allowing SPOKE neurosurgical équipes from Lombardy to come to our Institute and to operate themselves on their patients. We provide them with the entire neuro-oncological infrastructure, taking care of patients before admission (pre-op studies), during hospitalization (including radiation and oncological therapy inpatient assessment, when appropriate), and at discharge (either home or rehab). In the first three weeks of HUB implementation, despite the expected decrease of global activity as compared to normal times, we managed to take care of all the neuro-oncology patients that were referred to our Institute and deemed urgent (not amenable to be postponed). In particular, we have seen 159 brain tumor out-patients, operated on 67 patients (18 operated by SPOKE neurosurgical équipes at our Institute), and delivered in-hospital chemotherapy to 27 patients. Of course, the main challenge was represented by maintaining the Hub as a COVID-19-free Hospital. The algorithm that served to this purpose was based on a tight control of admissions, early recognition of any signs or symptoms of infection, and a rigid protection for any health professionals. More specifically, all patients were deeply screened with body temperature, O2 saturation, C-reactive protein, transamineses levels, complete cell blood count, chest radiography, pharyngeal SARS-CoV-2 swab, and a thorough interview. In case of SARS-CoV-2 positivity, surgical indication was re-discussed, based on some preliminary unpublished data (Fontanella et al.—manuscript in preparation), suggesting a higher risk of morbidity and lethality. So far, this new paradigm has worked smoothly, implementing a new way of close interaction via weekly teleconferences (Fig. 1—bottom). Neurosurgeons and neuro-oncologists collaborated with great sense of responsibility and respect and this resulted in a high level of patient satisfaction.
All in all, we are learning a lot from this terrible experience and, as neuro-oncological surgeons and neuro-oncologists, we are striving to continue providing our patients with the best possible standard of care. We hope that our Hub and Spoke model may serve as an example to other neuro-oncological units/institutes all over the world, should they face similar difficult circumstances. Neuro-oncology may be regarded as a niche subspecialty but its function is vital to the community and must be kept going despite everything, for the sake of patients. Maybe this new networking system—which optimizes resources in neurosurgical oncology and neuro-oncology—may serve as an example in the setting of possible future emergency scenarios, or even in non-emergency settings, especially within the landscape of public and universalistic health systems.
Funding
Not applicable.
Compliance with ethical standards
Conflict of interest
All the authors declared that they have no conflict of inerest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Francesco DiMeco, Email: francesco.dimeco@istituto-besta.it.
the ‘Hub and Spoke’ Lombardy Neurosurgery Group:
Marco Locatelli, Marco Benazzo, Giannantonio Spena, Claudio Bernucci, Erik Sganzerla, Marcello Egidi, Diego Spagnoli, Carlo Giussani, Michele Incerti, Giorgio Lorusso, Roberto Stefini, Roberto Assietti, Silvio Bellocchi, Maurizio Fornari, Miran Skrap, Fulvio Tartara, Mario Vitale, Paolo Ferroli, Angelo Franzini, Antonio Silvani, Marco Fontanella, and Marco Cenzato
References
- 1.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA; 2020 doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 2.Cenzato M, DiMeco F, Fontanella M, Locatelli D, Servadei F (2020) Neurosurgery in the Storm of Covid 19: Suggestions from Lombardy Region. J Neurosurg, Italy (ex malo bonum) (in press) [DOI] [PMC free article] [PubMed]