Abstract
BACKGROUND
The opioid epidemic is a national emergency, and it is imperative that all physicians are engaged in reducing exposure. Among dermatologists, dermatologic surgeons prescribe most opioids with the highest rates of prescription occurring in Southern states.
OBJECTIVE
Implement a quality improvement intervention to decrease opioids prescribed and filled to <10% of surgeries performed and have a 0% increase in the amount of patient complaints regarding postoperative pain.
MATERIALS AND METHODS
The number of opioids prescribed and filled in a single surgical facility in Georgia was obtained from the state’s Prescription Drug Monitoring Program before, 1 month after, and 6 months after implementation of the quality improvement initiative. Telephone encounters regarding post-operative pain was also collected at the same specified periods.
RESULTS
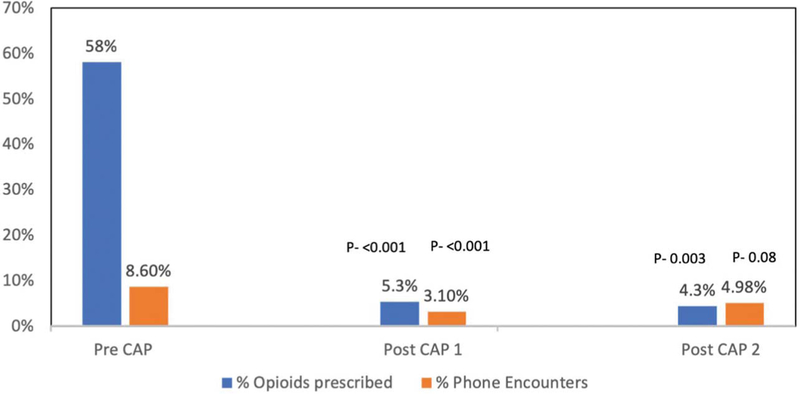
Proportion of opioids prescribed and filled decreased from 58% to 5% at 1-month postintervention and remained low on 6-month follow-up at 4%. There was no increase in postoperative pain complaints. Rather, a decrease in complaints was noted from 8.6% to 3.1% at 1-month postintervention and sustained on 6-month follow-up at 4.9%.
CONCLUSION
Our data support the management of postoperative pain with nonopioid medications.
The opioid epidemic is a national emergency that has spurred public institutions to organize resources and facilitate strategies to combat this largely preventable crisis facing the USpopulation.1 In 2015, the National Survey on Drug Use and Health estimated that 91.8 million (37.8%) US civilian, noninstitutionalized adults used prescription opioids, 11.5 million (4.7%) misused opioids, and 1.9 million (0.8%) were found to have an opioid use disorder.2 Annual prescription opioid overdose deaths rose from 3,442 in 1999 to 17,029 in 2017.3,4 Given this rising epidemic, several key efforts have been launched by federal and state agencies to stem this tide. Efforts include (1) educating the general public and prescribers on opioid risks, (2) increasing funding for treatment of opioid addiction and increased availability of opioid antidotes, (3) developing alternative pain medications, (4)publishing guidelines for safe opioid prescribing,(5)launching requirements for prescriber use of prescription monitoring programs, and (6) enacting legislation to regulate pain clinics.5,6
Opioid prescribing patterns have recently been examined in dermatology. Given the relatively low number of opioids prescribed by dermatologists, there are little published data on the impact that dermatologists may have on the opioid crisis.7 However, it has been demonstrated that even short courses of opioids increase the risk of developing an opioid addiction.8 Among dermatologists prescribing opioids for the Medicare population, the top 1% of prescribers were primarily those in surgical settings, suggesting that acute pain management is the major reason for the prescribing of opioids.7 Dermatologists in southern states were found to prescribe at a higher rate than their cohorts.7 Although there are no published guidelines, systematic reviews assessing acute post-operative pain have found that combination ibuprofen plus acetaminophen is efficacious in adequately controlling postoperative pain.9 Furthermore, in a head-to-head study, initial trial of combination 1000 mg of acetaminophen plus 400 mg of ibuprofen for post-operative pain management was found to be superior at remediating postoperative pain compared with a combination of 325 mg acetaminophen plus 30 mg codeine.10 Based on these and other analyses, recommendations have been to reserve oral opioids as second-line therapy.10,11 The above findings prompted the authors of this study to evaluate the opioid prescribing patterns of a surgical dermatology practice and implement a new protocol with the goal of decreasing the number of opioids prescribed and filled, while effectively managing acute pain in the immediate postsurgical setting.
Materials and Methods
No IRB approval was required as this was a single-center quality improvement intervention analysis.
Aim
The goal of this study was to decrease the proportion of opioids prescribed and filled to less than 10% of surgeries performed and have a 0% increase in the amount of patient complaints regarding postoperative pain.
Facility Postoperative Protocol
Before implementation of the quality improvement intervention, the standard protocol for pain management for each surgical case was to instruct patients to take acetaminophen over-the-counter (OTC).Patients were also asked during the surgical encounter whether they would like a prescription for opioids and if so, were prescribed opioids. Tylenol with codeine was prescribed 97% of the time and Norco the rest of the time, and this was per provider discretion. Patients were also called on same day as procedure to assess for adequate postoperative pain control. Given that most surgical sites were closed with absorbable sutures, no face-to-face follow-up visit was scheduled. However, the facility maintained an open-door policy in which patients were allowed to walk-in to discuss pain control if they desired. In the majority of cases, pain complaints were managed over the phone.
Data Collection
To assess the number of opioids prescribed to and filled by patients, the facility reviewed the state of Georgia’s Prescription Drug Monitoring Program (PDMP) registry and retrospectively counted the number of opioid prescriptions filled from February 1 to March 15, 2018. The number of surgeries (Mohs micrographic surgery [MMS] and standard excision) performed was also collected during the same time frame. Patient-initiated telephone encounters regarding postoperative pain were used as a proxy measure for uncontrolled postoperative pain. A review of telephone encounters was conducted during the same time frame, and the encounter was included as a patient complaint if it was documented that the patient used the words “pain, discomfort, burning, stinging, or uncomfortable” and the staff used the words “Tylenol, ibuprofen, codeine, or Norco.” On March 19, 2018, the facility implemented a new pain management protocol in the form of a quality improvement intervention denoted as a Corrective Action Plan (CAP). For any patient who underwent MMS or standard excision, and who had no existing contraindications, instructions were provided to take acetaminophen 1,000 mg and ibuprofen 400 mg immediately after surgery, and every 8 hours as needed for pain. Patients receiving anticoagulants or anti-platelets at the time of surgery and those with a history of gastrointestinal bleeding or renal dysfunction were instructed to take acetaminophen 1 gm without ibuprofen. Only patients who specifically asked for opioids citing prior lack of adequate pain control on combination NSAIDS/acetaminophen were prescribed opioids. Once the CAP was implemented, the same data detailed above were again collected from March 19, 2018, to April 27, 2018, for a total of 30 days. To ensure sustained improvement in the opioid prescribing pattern of the facility, the same data were again collected 6 months later from October 15, 2018, to November 23, 2018, for a total of 30 days.
Statistical Analysis
The total number of opioids prescribed and filled and the telephone encounters relating to postoperative pain were expressed as a percentage of the total number of surgeries performed during this timeframe. The proportion of opioid prescriptions filled and postoperative telephone calls at each time frame after intervention were compared with preintervention proportions using χ2 tests. p < .05 was considered significant in 2-sided tests.
Results
Before implementation of the CAP, 349 surgeries were performed between February 1, 2018, and March 15, 2018, and 58% of surgical patients during that time received and filled an opioid prescription (Figure 1). Thirty (8.6%) surgical patients called complaining of postoperative pain (Figure 1). After the CAP was implemented, 5% (p < .001) of the 323 patients who underwent surgery received and filled an opioid prescription and 3.1% (p<.001) called about postoperative pain (Figure 1). During the 6-month follow-up period, 4% (p = .003) of the 281 patients who underwent surgery received and filled an opioid prescription and 4.9% (p = .08) called regarding postoperative pain (Figure 1).
Figure 1.
Proportion of opioids prescribed and filled and telephone encounters at each time point. Pre CAP depicts the percent of opioids prescribed and filled and postoperative phone encounters regarding pain before the implementation of the new protocol. Post CAP depicts the proportion of opioids prescribed and filled and telephone encounters regarding pain shortly after the intervention was implemented. On follow-up, 6 months later, the proportion of opioids prescribed and filled and telephone encounters regarding postoperative pain remained similar.
The facility met its a priori goal of having a 0% increase in postoperative pain complaints, and in fact noted a 64% relative decrease in number of post-operative phone calls regarding pain after implementation of the CAP, and 53% relative decrease during the 6-month follow-up period. There were 2 postoperative complications noted, an instance of hemorrhage before implementation of the CAP and a hematoma formation after the CAP was implemented.
Discussion
In this quality improvement intervention, we analyze whether decreasing the number of opioids prescribed and filled for postoperative pain management could be done without having an effect on number of postoperative pain complaints. Our findings suggest that a pain management protocol that primarily focuses on the utilization of OTC analgesics, specifically acetaminophen and ibuprofen, leads to even better postoperative pain control given the decrease in number of phone calls regarding pain we noted after intervention. This supports previous data that the combination of acetaminophen and ibuprofen is far superior in the management of postoperative pain than either acetaminophen alone or acetaminophen plus codeine.10
The high number of telephone encounters noted before the intervention could be due to data that 25% of MMS patients do not actually take their prescribed opioids and of those that do, only 41% of the course is completed.12 However, in a study assessing factors related to patient-initiated communication after MMS, 17.2% of 1,531 patients initiated communication, and of these, 11.4% called regarding postoperative pain.13 Therefore, the proportion of pain-related phone encounters (8.6%) noted before implementation of our protocol is similar to previously published data. Procedure complexity was not collected during study period; however, the charges for surgical services between the 3 measurement periods did not vary, showing that case complexity did not play a role in our results.
Our data are encouraging for other surgical practices hoping to reduce the number of opioids prescribed postoperatively. They may use this framework to implement the same quality improvement intervention with some reassurance that they can achieve adequate postoperative pain control with nonopioid medications alone, or at least as the initial approach.
Limitations
This was a single-center quality improvement intervention; therefore, results may not be generalizable. However, the large number of procedures completed during each measured time frame as well as the sustained improvement noted 6 months later lends to some generalizability. In addition, the practice is referral-based; therefore, all the patients treated originate from multiple sites across the state of Georgia lending to some heterogeneity in regard to the demographics, medical, and socioeconomic status of the patient population.
Procedure complexity and timing between surgeries and phone encounters were not collected. However, the duration between surgical procedures and phone encounters was negligible as per anecdotal experience; patient-initiated phone calls were usually within 1 to 2 days postoperatively.
Conclusions
Overall, our study suggests that postoperative pain in the dermatologic setting may be managed with acetaminophen and ibuprofen, lending further support to previous data. We therefore propose to make this a guideline for all dermatologic surgeries.
Footnotes
The authors have indicated no significant interest with commercial supporters.
References
- 1.Gostin LO, Hodge JG, Noe SA. Reframing the opioid epidemic as a national emergency. JAMA 2017;318:1539–40. [DOI] [PubMed] [Google Scholar]
- 2.Han B, Compton WM, Blanco C, Crane E, et al. Prescription opioid use, misuse, and use disorders in U.S. Adults: 2015 national Survey on Drug use and Health. Ann Intern Med 2017;167:293–301. [DOI] [PubMed] [Google Scholar]
- 3.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy, Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse. 4 Trends in opioid use, harms, and treatment In: Phillips JK, Ford MA, Bonnie RJ, editors. Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. Washington (DC): National Academies Press (US); 2017. Available at: https://www.ncbi.nlm.nih.gov/books/NBK458661/. Accessed March 24, 2019 [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple Cause of Death 1999–2017 on CDC WONDER Online Database, Released December 2018. [Google Scholar]
- 5.Wickramatilake S, Zur J, Mulvaney-Day N, Klimo MC, et al. How states are tackling the opioid crisis. Public Health Rep 2017;132:171–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Califf RM, Woodcock J, Ostroff S. A proactive response to prescription opioid abuse. N Engl J Med 2016;374:1480–5. [DOI] [PubMed] [Google Scholar]
- 7.Cao S, Karmouta R, Li DG, Din RS, et al. Opioid prescribing patterns and complications in the dermatology Medicare population. JAMA Dermatol 2018;154:317–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017;66:265–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ong CKS, Seymour RA, Lirk P, Merry AF. Combining paracetamol(acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg 2010;110:1170–9. [DOI] [PubMed] [Google Scholar]
- 10.Sniezek PJ, Brodland DG, Zitelli JA. A randomized controlled trial comparing acetaminophen, acetaminophen and ibuprofen, and acetaminophen and codeine for postoperative pain relief after Mohs surgery and cutaneous reconstruction. Dermatol Surg 2011;37: 1007–13. [DOI] [PubMed] [Google Scholar]
- 11.Glass JS, Hardy CL, Meeks NM, Carroll BT. Acute pain management in dermatology: risk assessment and treatment. J Am Acad Dermatol 2015;73:543–60. [DOI] [PubMed] [Google Scholar]
- 12.Harris K, Curtis J, Larsen B, Calder S, et al. Opioid pain medication use after dermatologic surgery: a prospective observational study of 212 dermatologic surgery patients. JAMA Dermatol 2013;149: 317–21. [DOI] [PubMed] [Google Scholar]
- 13.Chitgopeker P, Sidey K, Aronson A, Hammel J, et al. Factors associated with patient-initiated communication after Mohs micrographic surgery. Dermatol Surg 2019;45:234–43. [DOI] [PubMed] [Google Scholar]