Abstract
Background.
Some reports have indicated that, when a cause for Horner syndrome can be determined, it is most often chest and neck tumors and stroke. Others have suggested that Horner syndrome is more frequently caused by surgical procedures in the neck and chest. These differences may be explained by disparate accrual methods. Therefore, we decided to compare the cause of Horner syndrome in cases where the diagnosis was confirmed by apraclonidine testing conducted by ophthalmologists to cases in which the diagnosis was made entirely on clinical grounds mostly by non-ophthalmologists.
Methods.
We applied a new search engine to the inpatient and outpatient electronic medical records text at the University of Michigan Medical Center from 1996 to 2018 for Horner syndrome with and without pharmacologic confirmation via ocular instillation of apraclonidine 0.5%. Among apraclonidine-confirmed cases, 159 met inclusion criteria. Among apraclonidine-unconfirmed cases, over 2,000 cases were identified, so we included only the first 159 cases that met inclusion criteria. In these 318 cases, we documented patient demographics, ophthalmologic features, imaging, underlying cause, and whether the cause was discovered before or after the diagnosis of Horner syndrome.
Results.
In the cohort of 159 apraclonidine-confirmed cases of Horner syndrome, a cause was identified in 97 (61%). Procedures in the neck, chest, skull base, and paraspinal region accounted for most of the identified causes, with cervical carotid dissection the next most common cause. In a cohort of 159 cases of Horner syndrome not tested with apraclonidine because the clinical diagnosis appeared firm, procedures again accounted for the largest percentage, but tumor was the next most common cause. In both groups, when a cause for Horner syndrome could be identified, that cause was nearly always known before the Horner syndrome was identified. However, in an important minority of cases, mostly involving carotid dissection or tumor, the identification of Horner syndrome was critical to the discovery of those conditions.
Conclusions:
The prevalence of causes of Horner syndrome depends on the accrual method. Among pharmacologically-confirmed cases, the cause was often undetermined or due to a preceding neck or chest procedure. Among pharmacologically-unconfirmed cases, a substantial proportion had also been caused by neck and chest procedures, but tumors in that region were also common. When a cause of Horner syndrome was found in both cohorts, it was usually known before the Horner syndrome was discovered, making Horner syndrome an afterthought. However, in an important minority of cases where the cause was not yet known, the identification of Horner syndrome was valuable in leading to important diagnoses like carotid dissection and tumor.
Keywords: Horner syndrome
INTRODUCTION
Horner syndrome classically consists of ptosis, miosis and sometimes anhidrosis. It results from damage to the oculosympathetic pathway, which extends from the hypothalamus to the eye.1 Among the reports that have described the causes and evaluation of Horner syndrome in at least 50 cases,2–8 a 1958 study of 216 patients, based on discharge summaries, found that tumors—often malignant and mostly in the chest and neck—were responsible for over one-third of cases.2 A 1980 study of 450 patients examined in an outpatient ophthalmology clinic4 also found tumor to be the most common identifiable cause. On the other hand, a study of 100 patients examined on an inpatient neurology ward found that stroke accounted for nearly half of the causes.3 A more recent study drawn from the outpatient and inpatient examinations of a single neuro-ophthalmologist5 found that a procedure on the neck and chest was the most commonly identified cause of Horner syndrome, followed by stroke and tumor. These differences in the prevalence of various causes of Horner syndrome might be explained by whether or not the Horner syndrome is pharmacologically-confirmed.
We applied a novel search engine to the inpatient and outpatient electronic medical record text in a single large tertiary care academic center, dividing the cohorts into those with and without pharmacologic confirmation. We used strict definitions of causation.
METHODS
We conducted a retrospective study of patients with Horner syndrome evaluated at the University of Michigan from 1996 to 2018. Because the anisocoria and ptosis may be mild and mimicked by causes other than Horner syndrome (“pseudo-Horner syndrome,”9) we chose as our principal cohort those patients with a positive apraclonidine test, defined as reversal of anisocoria within 30 minutes of instillation of apraclonidine 0.5% in each eye10 (“pharmacologically-confirmed”). In patients with ptosis without anisocoria, we considered the apraclonidine test positive if the pupil in the affected eye dilated and the pupil in the unaffected eye did not. Because the youngest patient in our cohort was 4 years of age, and cocaine is used in our institution only for patients aged under 2 years of age, there are no data in this study on Horner syndrome confirmed with that agent. We also searched the records for patients who were assigned a diagnosis of Horner syndrome without any pharmacologic confirmation (“pharmacologically-unconfirmed”).
We applied the novel Electronic Medical Record Search Engine (EMERSE) of the University of Michigan,11 which extended back to 1996, to locate the terms “Horner,” “Horners,” “Horner’s,” and “apraclonidine” within the text of the electronic medical record system, yielding 495 patients. Of the 495 patients, 336 were excluded because review of records did not confirm a positive apraclonidine test, leaving a study set of 159 patients. The earliest apraclonidine-confirmed case occurred in the year 2005. The 50% cut point for diagnosed cases occurred in 2014.
We used the same search terms without “apraclonidine” and turned up over 2,000 “hits.” Because that number was so large, we decided to limit this cohort to the first 159 cases that documented ptosis and ipsilateral miosis, beginning with the most recently identified cases.
For each of the 159 pharmacologically-confirmed patients, we recorded the sex, age at diagnosis, date of diagnosis, setting in which the initial diagnosis of Horner syndrome was made (outpatient or inpatient), side of Horner syndrome, amount of ptosis, pupil size in dim illumination, imaging modality and its pertinent findings, and cause of the Horner syndrome. For the 159 pharmacologically-unconfirmed patients, we did not record the ophthalmic features because they were sparsely documented, most having been evaluated by non-ophthalmologists. Descriptive statistics were used to describe patient demographics.
Ptosis was recorded as millimeter difference between the two eyes viewed in primary gaze position. Pupil size was recorded in millimeters in the dimmest possible illumination that permitted pupil size measurement; anisocoria was expressed as the difference in pupil size between the two eyes under this condition. Among the 159 apraclonidine-confirmed cases, clinical examination and apraclonidine testing was conducted at the University of Michigan Medical Center under the supervision of the three faculty neuro-ophthalmologists in 158 cases. In one case, we reviewed a reliable record of testing performed elsewhere. Pertinent imaging was conducted or reviewed at our center in 156 cases; for the remaining three cases, the imaging report was available for review. Among the 159 pharmacologically-unconfirmed cases, only 13 had been examined under neuro-ophthalmologic supervision. In the remaining 146 patients, we accepted a record listing of Horner syndrome, acknowledging that ophthalmologic features were rarely documented. As a cause was usually obvious in most such cases, we presumed that the diagnosis of Horner syndrome was reasonable.
We defined the causes of Horner syndrome as follows: 1) Cervical carotid artery dissection: unequivocal evidence of cervical internal carotid luminal tapering on CTA and/or MRI/MRA, or pre-contrast luminal T1 shortening on MRI;12 the imaging evaluation of patients with Horner syndrome has been standard at our institution since 1995, including either CT/CTA or MRI/MRA between the skull base and the mid-thorax when Horner syndrome is the only pertinent clinical abnormality; when an additional clinical abnormality is present to suggest an intracranial lesion, the imaging has extended to the skull vertex; 2) Tumor: mass compressing the paraspinal, thoracic, cervical, or cavernous sinus portions of the oculosympathetic pathway; 3) Post-procedure: new Horner syndrome diagnosed after cranial base/neck/spine/chest/jaw surgery in the region of the oculosympathetic pathway or placement of a central venous catheter into the internal jugular vein; 4) Cavernous sinus lesion: imaging evidence of a lesion within the ipsilateral cavernous sinus with relevant neuro-ophthalmic abnormalities; 5) Cluster headache: episodic ipsilateral periocular headache with at least one other manifestation suggesting trigeminal autonomic cephalalgia13 and no imaging evidence of cervical carotid dissection; 6) Stroke: clinical and imaging evidence of a brain stem or thalamic ischemic or hemorrhagic stroke that could account for Horner syndrome identified at the time of the stroke; 7) Skull fracture in carotid canal: acute onset of Horner syndrome timed with supportive CT evidence within one week of new head trauma, and no imaging evidence of cervical carotid dissection; 8) Congenital Horner syndrome: reliable evidence of Horner syndrome noted on photographs taken in infancy; 9) Longus colli contusion: history of acute neck trauma, imaging evidence of enlarged longus colli muscle compressing cervical oculosympathetic pathway, diagnosis of ipsilateral Horner syndrome within one week of the neck trauma, and no imaging evidence of cervical carotid dissection;14 10) Other trauma: onset of Horner syndrome after neck, spinal, or axillary injury without imaging evidence of carotid dissection.
In order to assess the value of making a diagnosis of Horner syndrome, we divided the cohorts into those in which the cause of Horner syndrome had been discovered before the diagnosis of Horner syndrome (“Cause Discovered Before Diagnosis of Horner Syndrome”) and those in which the cause was not discovered until after the diagnosis of Horner syndrome (“Cause Discovered After Diagnosis of Horner Syndrome”). We further divided the subgroup of patients with “Cause Discovered After Diagnosis of Horner Syndrome” into those in which the examiner had strong clinical clues to the eventually-discovered cause and those that lacked such clues.
If an adequate diagnostic evaluation failed to determine a probable cause of Horner syndrome, we labeled the cases “idiopathic.” If an adequate evaluation had not been performed, or we lacked sufficient information to assign a reasonable cause for Horner syndrome, we considered the cause to be “uncertain.” Cases that were “idiopathic” or “uncertain” were considered to be of “indeterminate” cause. Associations between age, sex, pharmacologic confirmation, and identifying a cause were explored using bivariate logistic regression.
RESULTS
Demographics.
In the pharmacologically-confirmed cohort, there were 80 men and 79 women, ranging in age from 4 to 87 years (median 51, interquartile range [IQR] 34–62). There were only six patients aged 10 years or younger and no patients younger than four years. In the pharmacologically-unconfirmed cohort, there were 73 men and 86 women, ranging in age from 2 to 86 years (median 49, IQR 33–60).
Setting of Horner Diagnosis.
In the pharmacologically-confirmed cases, the diagnosis of Horner syndrome was made on outpatients in 79% of cases, an expected result because testing with apraclonidine is more practical in the outpatient setting. Many of those cases involved neck and chest procedures that had occurred during an inpatient stay. In the pharmacologically-unconfirmed cases, it was not possible to determine reliably whether the diagnosis was first made in the outpatient or inpatient setting.
Ptosis and Anisocoria.
In the pharmacologically-confirmed Horner cohort, 97 (62%) had Horner syndrome on the right side, 59 (38%) on the left side. The amount of ptosis was recorded in 54/159 (34%) patients, ranging from 0.5mm to 4mm (mean 1.7mm). Anisocoria was recorded for 144 (91%) patients, ranging from 0.5mm to 4.5mm (mean 1.6mm). There were 3 patients who had ptosis without anisocoria (carotid dissection—1, cluster headache—1, post-procedure—1). There were 21 patients, or 13% of the entire cohort, who had anisocoria without ptosis (idiopathic—7, post-procedure—4, cluster headache—2, congenital—2, brachial plexus contusion − 1, carotid canal basal skull fracture − 1, metastatic lung squamous cell carcinoma to carotid − 1, uncertain—3). Only three patients described lack of sweating on the ipsilateral face (excision of paraspinal neuroblastoma—1, neck surgery − 1, idiopathic—1).
We have not reported the ophthalmologic features in the pharmacologically-unconfirmed cohort because they were incompletely documented and could not be verified.
Causes.
In the pharmacologically-confirmed cohort, a cause could be determined in 97 (61%) patients (FIGURE 1; TABLE 1). Among the 62 patients in whom no cause could be determined, 51 were considered “idiopathic” and 11 were of “uncertain“ cause.
Figure 1.
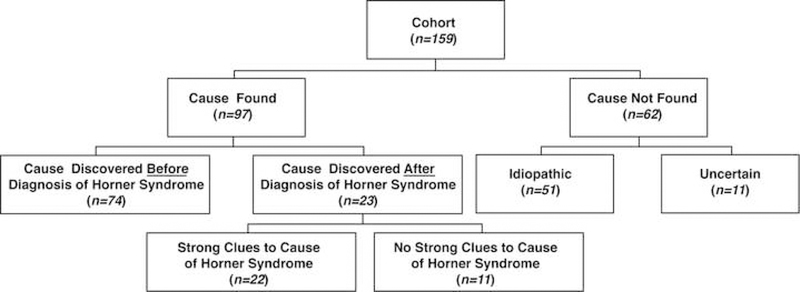
Distribution of 159 Patients with Pharmacologically-Confirmed Horner Syndrome
Table 1.
Causes of Horner Syndrome in 318 Patients with Horner Syndrome
| Cause of Horner Syndrome | Pharmacologically- Confirmed (Percentage of Total) |
Pharmacologically- Unconfirmed (Percentage of Total) |
|---|---|---|
| Indeterminate Cause | 62 (39%) | 15 (9%) |
| Idiopathic | 51 | 0 |
| Uncertain | 11 | 15 |
| Post-Procedure | 34 (21%) | 57 (36%) |
| Surgical | 24 | 33 |
| Central Venous Line | 10 | 24 |
| Carotid Dissection | 14 (9%) | 17 (11%) |
| Spontaneous | 7 | 14 |
| Traumatic | 7 | 3 |
| Trauma | 13 (8%) | 12 (8%) |
| Carotid Canal Basal Skull Fracture | 3 | 0 |
| Brachial Plexus Contusio | 2 | 2 |
| Cavernous Sinus Gunshot Wound | 1 | 0 |
| Cervical Spine Contusion | 1 | 5 |
| Longus Colli Contusion | 1 | 0 |
| Unspecified Neck Trauma | 5 | 5 |
| Cluster Headache | 12 (8%) | 8 (5%) |
| Tumor | 11 (7%) | 28 (18%) |
| Head | 3 | 1 |
| Cervical | 6 | 8 |
| Mediastinal | 2 | 16 |
| Paraspinal | 0 | 3 |
| Stroke | 7 (4%) | 15 (9%) |
| Thalamic Stroke | 4 | 2 |
| Dorsolateral Medullary Infarct | 2 | 12 |
| Superior Cerebellar Artery Infarct | 1 | 1 |
| Infection/Inflammation | 2 (1%) | 0 (0%) |
| Aspergillus Infection of Neck | 1 | 0 |
| Sarcoidosis of Neck | 1 | 0 |
| Carotid-Cavernous Fistula | 2 (1%) | 0 (0%) |
| Congenital Horner Syndrome | 2 (1%) | 7 (4%) |
Among the 97 patients in whom a cause could be found (TABLE 1), Horner syndrome resulted from a procedure in 34 cases. Among those 34 cases, 24 followed surgery (neck—17, thoracic—4, paraspinal—2, cranial base—1) and 10 followed a neck procedure (placement of a central venous catheter—9, scalene block—1). Carotid dissection accounted for 14 patients, of which 7 were unprovoked and 7 were associated with sudden neck strain (motor vehicle accident—4, chiropractic neck manipulation −1, yoga exercises −1, heavy lifting—1).
Trauma was the cause in in 13 cases, including 3 carotid canal skull fractures, 2 brachial plexus contusions, and 1 each of cavernous sinus gunshot wound, cervical spine contusion, and longus colli contusion. Five patients reported neck trauma but had imaging negative for dissection.
Cluster headache was the cause in 12 patients, determined only after carotid imaging was negative. Five of those patients had the classic cluster headache syndrome complex, including episodic periocular pain and nasal and conjunctival congestion; the remaining 7 patients had episodic periocular pain, allowing only a tentative assignment of cause.
Tumor in the oculosympathetic pathway explained 11 cases (cervical paraganglioma—2, neuroendocrine mediastinal tumors—2, anaplastic thyroid cancer—1, cavernous sinus lymphoma—1, cervical lymphoma—1, and 1 each of metastases from lung to carotid artery, nasopharynx to carotid sheath, nasopharynx to cavernous sinus, and periauricular squamous cell carcinoma to cavernous sinus).
Stroke was the cause in only 7 patients (thalamic stroke—4, dorsolateral medullary infarct—2, superior cerebellar artery infarct—1). All strokes had produced multiple neurologic manifestations, among which Horner syndrome was a minor component.
There were two cases each of carotid-cavernous fistula and congenital Horner syndrome, along with a case each of aspergillus infection in the neck and sarcoidosis in the neck.
In the 159 patients with pharmacologically-unconfirmed Horner syndrome, most cases (91%) had an identifiable cause. (Figure 2; Table 1) Among identified causes, procedures still accounted for the highest proportion at 36%. Tumors accounted for 28%, the second highest proportion. All other causes occupied similar proportions as in the pharmacologically-confirmed cases, except that stroke was twice as common, still with under 10% of causes.
Figure 2.
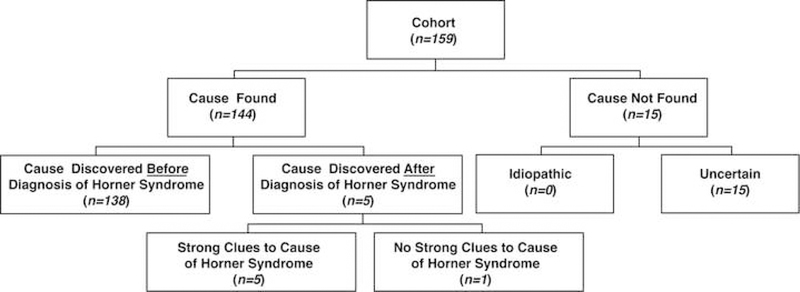
Distribution of 159 Patients with Pharmacologically-Unconfirmed Horner Syndrome
There was no association between age or sex and discovering a cause for Horner syndrome. Patients with pharmacologically-confirmed Horner syndrome had significantly decreased odds of having a cause identified (OR 0.12, 95%CI: 0.06–0.24; P<0.001).
In both cohorts where a cause for Horner syndrome could be identified, it was usually known by the time the Horner syndrome was diagnosed. Furthermore, those with a known cause at the time of diagnosis were less likely to have pharmacologic confirmation (OR 0.17, 95%CI 0.10–0.28; P<0.001). In the pharmacologically-confirmed cohort (TABLE 2), among 97 cases in which a cause could be determined, there were only 23 patients in whom the examiner diagnosing the Horner syndrome did not know its cause. Among them were 12 cluster headaches, 5 carotid dissections, 2 tumors, 2 congenital Horner syndromes, 1 longus colli contusion, and 1 brachial plexus contusion. Clinical clues to the cause were evident in 12 of those 23 patients—5 with a convincing history of cluster headache, 2 with carotid dissection and acute ipsilateral neck pain, 2 with infant photography that showed ptosis and anisocoria, 1 with cavernous sinus lymphoma and an ipsilateral sixth nerve palsy, 1 with severe recent neck injury and imaging evidence of an enlarged longus colli muscle, and 1 with severe shoulder injury and numbness in the ipsilateral arm. There were no clues to the eventually-determined cause in 11 of those 23 patients, including 7 with cluster headache but without a classic pattern, 3 with carotid dissection but no history of new neck pain, and 1 with anaplastic thyroid cancer but no clinical signs apart from the Horner syndrome. Among the 3 carotid dissections without meaningful clinical clues, 1 had presented with unilateral hypersensitivity to touch on the face, 1 had new posterior cervical headache and contralateral blurred vision, and 1 had awakened with periocular pain and non-localizing headache.
Table 2.
Causes of Pharmacologically-Confirmed Horner Syndrome According to Whether Horner Diagnosis Was Made Before or After Cause Was Known
| Cause of Horner Syndrome | Cause Discovered Before Diagnosis of Horner Syndrome (n = 74) |
Cause Discovered After Diagnosis of Horner Syndrome (n = 23) |
|---|---|---|
| Post-Procedure | 34 | 0 |
| Cluster Headache | 0 | 12 |
| Carotid Dissection | 9 | 5 |
| Tumor | 9 | 2 |
| Stroke | 7 | 0 |
| Trauma | 6 | 2 |
| Miscellaneous | 9 | 2 |
In the pharmacologically-unconfirmed cases, there were only 6 cases in which a cause was not known to the examiner making the Horner diagnosis. They consisted of 5 carotid dissections and 1 cervical neuroblastoma. Among the dissections, acute neck pain was always a prominent clue. There were no clues other than Horner syndrome to the neuroblastoma.
The distribution of causes did not vary substantially whether the patient was aged over or under age 50 at the time of Horner syndrome diagnosis.
DISCUSSION
In this retrospective, single-institution study, the distribution of causes of Horner syndrome varied according to the manner in which cases were accrued. In including both apraclonidine-confirmed cases and pharmacologically-unconfirmed cases, this study differs from prior studies, which have included either cases that were confirmed with medications other than apraclonidine or pharmacologically-unconfirmed cases. In our study of 159 pharmacologically-confirmed cases, a cause remained undetermined in nearly half of them, whereas in the 159 pharmacologically-unconfirmed cases, a cause was found in nearly all cases.
Among the identifiable causes in the cohort of pharmacologically-confirmed cases, neck procedures were predominant, followed by cervical carotid dissection and cluster headache. Stroke and tumor accounted for a small proportion of cases. Among the pharmacologically-unconfirmed cases, procedures again accounted for the highest proportion of causes, but tumors in the oculosympathetic pathway were the second most frequent cause. Otherwise the distribution of causes of Horner syndrome did not differ significantly between the two cohorts, except that stroke was a more common cause in the pharmacologically-unconfirmed cases, as expected.
Our study’s finding that the cause among apraclonidine-confirmed Horner syndrome cases was indeterminate in 39% conforms to the 40% found in the 450-patient study by Maloney et al,4 where pharmacologic confirmation was with topical epinephrine and cocaine (TABLE 3). It is much less than the 73% undetermined rate among 112 outpatient Horner syndrome cases confirmed with cocaine and hydroxyamphetamine testing by Sadaka et al.7 Notably, a study of 52 inpatients and outpatients with topical cocaine-confirmed Horner syndrome drawn from the case records of a single neuro-ophthalmologist5 found that only 16% were of indeterminate origin.
Table 3.
Causes of Horner Syndrome in Major Published Studies
| Cause of Horner Syndrome |
Our Study (Pharmacologically Confirmed) (n = 159) |
Our Study (Pharmacologically Unconfirmed) (n = 159) |
Giles et al2 (1958) (n = 216) |
Keane3 (1979) (n = 100) |
Maloney et al4 (1980) (n = 450) |
Almog et al5 (2010) (n = 52) |
Sadaka et al6 (2017) (n = 132) |
|---|---|---|---|---|---|---|---|
| Undetermined | 39% | 9% | 24% | 8% | 40% | 17% | 78% |
| Post Procedure | 21% | 36% | 19% | 5% | 10% | 24% | 3% |
| Carotid Dissection | 9% | 11% | 0% | 0% | 0% | 7% | 2% |
| Trauma | 8% | 8% | 6% | 6% | 4% | 8% | 1% |
| Cluster Headache | 8% | 5% | 0% | 2% | 12% | 0% | 8% |
| Tumor | 7% | 18% | 36% | 23% | 13% | 16% | 5% |
| Stroke | 4% | 9% | 5% | 48% | 3% | 16% | 1% |
| Miscellaneous | 3% | 0% | 4% | 7% | 15% | 8% | 2% |
| Congenital | 1% | 4% | 6% | 0% | 3% | 2% | 0% |
As for pharmacologically-unconfirmed Horner syndrome, our finding that a cause remained undetermined in only 15% differs little from the 24% found in the 216 inpatient cases studied by Giles et al.2 A study of 100 neurology inpatients with a pharmacologically-unconfirmed diagnosis of Horner syndrome made by a single neurologist3 found that only 9% of cases were of indeterminate cause. We surmise that when a diagnosis of Horner syndrome is made without pharmacologic confirmation, it is often based on a cause identified in inpatients. By contrast, when the Horner diagnosis depends on pharmacologic confirmation, as occurs often in outpatients, its cause will often remain unknown.
Carotid dissection was the second most common identifiable cause of Horner syndrome in our study. That diagnosis does not appear in the older reports, probably because it only became feasible in the era of modern non-invasive vascular imaging. We presume that carotid dissection caused Horner syndrome in some of the cases attributed in earlier reports to neck trauma. Two recent reports8,15 mention carotid dissection as the explanation for 40%8 and 18%15 of identifiable causes of Horner syndrome.
Cluster headache accounted for about 10% of causes in our study, as it did in the studies of Sadaka et al.7 and Maloney et al.,4 but not in other studies. We acknowledge that this diagnosis must be made with caution because it depends heavily on patient report. We did not assign cluster headache as a diagnosis unless carotid imaging was negative and the patient had periodic headache with at least a suggestion of other trigeminal autonomic symptoms.
Stroke was an infrequent cause of Horner syndrome in our study. It was the major cause in the 1979 report of 100 patients by Keane,3 but that was based on his observations as a neurologist consulting on patients in an inpatient neurology ward. Other studies,2,4–8 which draw less on neurologic inpatients, have found stroke to be an infrequent cause, explainable by the fact that Horner syndrome is a minor aspect of stroke, not necessary to its diagnosis, and not responsible for symptoms. Therefore, it often goes undocumented.
Trauma, mostly to the neck, accounted for an important proportion of Horner syndrome in our study, as it has in other studies. Previous reports do not often specify the nature of trauma or the site of impact.2,3 Most of the patients in those reports had not undergone definitive vascular imaging. We suspect that many had undetected carotid dissection. Our study included 9 patients with neck trauma and negative carotid artery imaging in whom we presume the mechanism was contusion of the Horner fibers adjacent to the carotid wall.
The difference in the prevalence of tumor among pharmacologically-confirmed and pharmacologically-unconfirmed Horner syndrome in our study is striking but easily explainable by accrual methods. Tumors accounted for 5% of identifiable causes among our pharmacologically-confirmed cases, yet 28% in pharmacologically-unconfirmed cases. In other reported pharmacologically-confirmed cohorts, Sadaka et al.7 found only 5% were tumors, but Maloney et al4 found 13% and Almog et al5 found 16%. By contrast, in the pharmacologically-unconfirmed cohort of Giles et al,2 tumor accounted for 36% of Horner cases.
When a cause could be determined in our cohorts, the examiner making the diagnosis of Horner syndrome already knew that cause in most cases, making the Horner diagnosis often an afterthought. Almog et al5 found this phenomenon in 62% of cases, but other reports have not emphasized this important point. In our two cohorts, there were 29 cases in which the diagnosis of Horner syndrome triggered the investigation leading to a cause for Horner syndrome, of which 12 had no localizing clues. Among them were three acute carotid dissections without recent neck pain or trauma and two tumors—an anaplastic thyroid cancer and a cervical neuroblastoma.
We acknowledge limitations of our study. It was retrospective, so that data were originally gathered as part of a clinical rather than a research assessment. The measurement of pupil size may not have been accurate, given that pupillometry was not used. Evaluation of Horner syndrome at the time of diagnosis was sometimes inadequate to determine a definite cause. The data were drawn from just one institution, including only a small number of children. Inclusion of more children might have altered the causation prevalence. We acknowledge that the diagnosis of Horner syndrome might have been incorrect in some of the patients who did not undergo apraclonidine testing. We further acknowledge that the prevalence of causes might have been biased because the imaging protocol did not always include the intracranial space or the orbit and the sensitivity of imaging improved over the study period.
However, our study has strengths. The cohort is one of the largest reported to date. Cases were accrued via a search that detected all text mentions of Horner syndrome with and without pharmacologic confirmation, allowing a broader inclusion than studies dependent on personal files or discharge diagnoses. For pharmacologic confirmation, we relied on topical apraclonidine, a now more commonly-used pharmacologic indicator of Horner syndrome than cocaine, epinephrine, or hydroxyamphetamine, which were used in prior studies. We employed strict definitions of all causes. Cases mostly belonged to the modern era of neuroimaging in which a reliable diagnosis of carotid dissection could be made. Unlike some earlier studies, we did not use “isolated Horner syndrome” as a select group. Instead, we separated out the subgroup in which the diagnosis of Horner syndrome preceded the discovery of its cause because it is there that the Horner diagnosis adds most value.
Based on this study and others, the following profile of adult Horner syndrome emerges:
-
1)
When the diagnosis of Horner syndrome is based on pharmacologic confirmation, it is often an isolated abnormality and a definite cause will often not be found even in the face of adequate investigation.
-
2)
When a cause for Horner syndrome is found, our study suggests that it will most often be a procedure damaging the oculosympathetic pathway and it will almost always be known before the diagnosis of Horner syndrome is made, making Horner syndrome frequently a clinical afterthought.
-
3)
If the cause is not known at the time of Horner syndrome diagnosis, carotid dissection may be the cause even if acute neck or face pain is not described.
-
4)
Cluster headache is a setting for Horner syndrome, but diagnosis is always uncertain and should not be made without ruling out carotid dissection.16
-
5)
Tumors account for an important proportion of causes; if a tumor has not already been identified at the time of Horner diagnosis, appropriate imaging is justified.
-
6)
Horner syndrome may be common in medullary stroke, but is probably not documented because the ophthalmic manifestations are minor compared to the neurologic manifestations.
-
7)
Miscellaneous causes will account for some cases of Horner syndrome; they may not be apparent at the time of Horner diagnosis and are important to uncover.
-
8)
Horner syndrome will usually display a combination of ptosis and miosis, but miosis may occur without ptosis, with the understanding that small amounts of ptosis can be easily overlooked.
In this profile, there are management implications. When Horner syndrome follows a procedure or stroke that could have damaged the oculosympathetic pathway, there is no need for further evaluation. Where the cause is not yet known, localization to the central, preganglionic, or postganglionic segment of the oculosympathetic pathway by pupil reactions to topical adrenergic agents is not sufficiently accurate to be useful.10 Clinical clues will be more useful, as they were in some of our cases.6 When there are such clinically localizing clues, they should be conveyed to the interpreting radiologist because some lesions may have subtle imaging signs, as was the case in our single patient with longus colli contusion. Even so, Horner syndrome diagnosed without a known preceding cause will often be an isolated abnormality without clinically localizing clues. It should then trigger non-targeted imaging from the skull base to the high thoracic region, using CT/CTA or MRI/MRA 17 with emphasis on discovering carotid dissection and tumors, acknowledging that the yield will be low.10,18,19
Acknowledgments
No funding was received for this work.
Footnotes
There is no conflict of interest to disclose.
References
- 1.Walton KA, Buono LM. Horner syndrome. Curr Opin Ophthalmol 2003;14:357–363 [DOI] [PubMed] [Google Scholar]
- 2.Giles CL, Henderson JW. Horner’s syndrome: an analysis of 216 cases. Am J Ophthalmol 1958;46:289–296. [DOI] [PubMed] [Google Scholar]
- 3.Keane JR. Oculosympathetic paresis. Analysis of 100 hospitalized patients. Arch Neurol 1979;36:13–15. [DOI] [PubMed] [Google Scholar]
- 4.Maloney WF, Younge BR, Moyer NJ. Evaluation of the causes and accuracy of pharmacologic localization in Horner’s syndrome. Am J Ophthalmol 1980;90:394–402 [DOI] [PubMed] [Google Scholar]
- 5.Almog Y, Gepstein R, Kesler A. Diagnostic value of imaging in Horner syndrome in adults. J Neuroophthalmol 2010;30:7–11. [DOI] [PubMed] [Google Scholar]
- 6.Gao Z, Crompton JL. Horner Syndrome: A Practical Approach to Investigation and Management. Asia Pac J Ophthalmol 2012;1:175–179. [DOI] [PubMed] [Google Scholar]
- 7.Sadaka A, Schockman SL, Golnik KC. Evaluation of Horner Syndrome in the MRI Era. J Neuroophthalmol 2017;37:268–272 [DOI] [PubMed] [Google Scholar]
- 8.Beebe JD, Kardon RH, Thurtell MJ. The Yield of Diagnostic Imaging in Patients with Isolated Horner Syndrome. Neurol Clin 2017;35:145–151. [DOI] [PubMed] [Google Scholar]
- 9.Thompson BM, Corbett JJ, Kline LB, Thompson HS. Pseudo-Horner’s Syndrome. Arch Neurol 1982;39:108–111. [DOI] [PubMed] [Google Scholar]
- 10.Davagnanam I, Fraser CL, Miszkiel K, Daniel CS, Plant GT. Adult Horner’s syndrome: a combined clinical, pharmacological, and imaging algorithm. Eye 2013;27:291–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hanauer DA, Mei Q, Law J, Khanna R, Zheng K. Supporting information retrieval from electronic health records: A report of University of Michigan’s nine-year experience in developing and using the Electronic Medical Record Search Engine (EMERSE). J Biomed Inform 2015;55:290–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel RR, Adam R, Maldjian C, Lincoln CM, Yuen A, Arneja A. Cervical Carotid Artery Dissection: Current Review of Diagnosis and Treatment. Cardiol Rev 2012;20:145–152 [DOI] [PubMed] [Google Scholar]
- 13.Headache Classification Subcommittee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2013;33:629–808 [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim M, Parmar H, Yang L. Horner syndrome associated with contusion of the longus colli muscle simulating a tumor. J Neuroophthalmol 2010;30:70–72. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y, Morgan ML, Barros Palau AE, Yalamanchili S, Lee AG. Evaluation and neuroimaging of the Horner syndrome. Can J Ophthalmol 2015;50:107–111. [DOI] [PubMed] [Google Scholar]
- 16.Rigamonti A, Iurlaro S, Reganati P, Zilioli A, Agostoni E. Cluster headache and internal carotid artery dissection: two cases and review of the literature. Headache 2008;48:467–470. [DOI] [PubMed] [Google Scholar]
- 17.Trobe JD. The evaluation of Horner syndrome. J Neuroophthalmol 2010;30:1–2. [DOI] [PubMed] [Google Scholar]
- 18.Digre KB, Smoker WR, Johnston P, Tryhus MR, Thompson HS, Cox TA, Yuh WT. Selective MR imaging approach for evaluation of patients with Horner’s syndrome. AJNR Am J Neuroradiol 1992;13:223–227. [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Moosa A, Eggenberger E. Neuroimaging yield in isolated Horner syndrome. Curr Opin Ophthalmol 2011. Nov;22:468–471. [DOI] [PubMed] [Google Scholar]


