Abstract
Multiple etiological models have been proposed to explain posttraumatic stress disorder (PTSD) and alcohol use disorder (AUD) comorbidity, but the predominant model to date is the “drinking to cope” self-medication model. Despite its popularity, the self-medication model lacks rigorous empirical support due to inconsistencies and methodological limitations, particularly the failure to operationalize drinking to cope with trauma symptoms specifically. The present study sought to measure trauma-related drinking to cope (TRD) in order provide a more specific test of the self-medication model among a representative sample of 1,896 undergraduates with a history of trauma exposure and alcohol use. Using a model building approach in Mplus, a correlated multiple mediator model tested the association between PTSD symptoms and alcohol use problems (AUP) through TRD and DMQ-Cope as moderated by sex. Results indicated that, while accounting for the effects of DMQ-Cope, TRD partially mediated the relation between PTSD symptoms and AUP and that this relationship was stronger for males than for females. With the exception of moderation by sex, results were substantiated using longitudinal data. Findings were consistent with the self-medication model, suggesting that trauma-related drinking to cope motives may serve as a mechanism through which PTSD symptoms influence AUP. TRD may serve as a more specific screening tool for AUP risk among individuals endorsing PTSD symptoms compared to the commonly used DMQ-Cope.
Keywords: Self-Medication, PTSD, Alcohol, Trauma-Related Drinking, Drinking-to-Cope
Posttraumatic stress disorder (PTSD) and alcohol use disorder (AUD) are prevalent, frequently co-occur, and are costly to society (Brown, Stout, & Mueller, 1999a; Kessler, Chiu, Demier, Merikangas, & Walters, 2005; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). High comorbidity of PTSD-AUD constitutes a public health crisis, such that comorbid PTSD-AUD is associated with higher symptom severity (Najavits et al., 1998; Ouimette, Finney, & Moos, 1999), greater service utilization (Brown, Stout, & Mueller, 1999b), poorer treatment prognosis (Blanco et al., 2013; Ipser, Wilson, Akindipe, Sager, & Stein, 2015; Read, Brown, & Kahler, 2004; Shorter, Hsieh, & Kosten, 2015), shorter time to relapse posttreatment (Bonanno, 2004), poorer physical health (Evren et al., 2011), and higher suicidal ideation and attempts (Rojas, Bujarski, Babson, Dutton, & Feldner, 2014). These high-stakes clinical implications warrant increased understanding of factors underlying comorbid PTSD and AUD in order to inform transdiagnostic treatment and prevention efforts.
To that end, consideration of sex differences is imperative with regard to the study and treatment of comorbid PTSD-AUD. A wealth of evidence suggests that females are at substantially higher risk for PTSD than males (Breslau, Davis, Andreski, Federman, & Anthony, 1998; Kessler et al., 1995). Additionally, studies have documented higher rates of risky drinking and AUD in males compared to females (Capraro, 2000; Goldstein, Dawson, Chou, & Grant, 2012), although newer research shows that sex differences in AUD are narrowing and that there have been recent shifts towards more equal levels of consumption (Grant et al., 2015). Findings on sex differences with regard to comorbid PTSD-AUD have been mixed, with a majority of studies demonstrating higher rates in females compared to males (Brady, Grice, Dustan, & Randall, 1993; Brady & Randall, 1999; Kessler et al., 1997; Sonne, Back, Diaz Zuniga, Randall, & Brady, 2003), one study showing higher rates among males compared to females (King, Meehan, Trim, & Chassin, 2006), and a large epidemiologic study demonstrating no sex differences (Goldstein, Dawson, Chou, & Grant, 2012). Thus, it appears most often that the presence of PTSD eliminates some of the sex differences with regard to prevalence of AUD, particularly among women. Given sex differences for both phenotypes, examination of etiologic models should incorporate testing for sex differences.
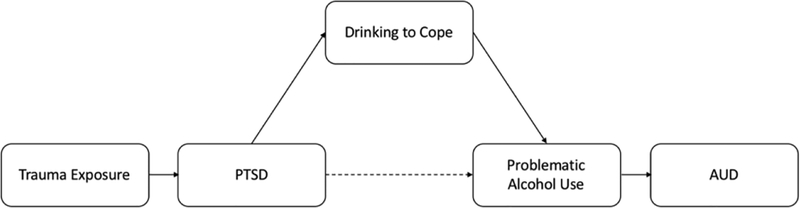
One of the most widely accepted explanations for high comorbidity rates between PTSD and AUD is the self-medication hypothesis. The “drinking to cope” self-medication model is a causal model (see Figure 1) which postulates that individuals with PTSD are more prone to developing problematic drinking behaviors due to a tendency to drink to cope with negative internal experiences (Khantzian, 1999). Examined within a learning-theory framework, the compelling short-term negative reinforcement effects of alcohol may serve to condition the use of alcohol to temporarily alleviate PTSD symptoms and ultimately result in the development of more severe forms of alcohol use (i.e., AUD; Schumm & Chard, 2012).
Figure 1.
Self-Medication Model
Although evidence in support of the self-medication hypothesis exists in piecemeal form (e.g., PTSD onset more commonly precedes AUD onset following trauma than vice versa [Kessler et al., 1995]), methodological limitations have precluded the self-medication model from being extensively studied in a rigorous manner that tests all tenets of the conceptual framework. Instead, the PTSD-AUD self-medication literature to date is largely cross-sectional and functions under multiple assumptions, potentially the most damaging of which is the assumption that drinking to cope with negative affect is synonymous with drinking to cope with PTSD symptoms specifically.
A systematic review of the PTSD-alcohol use self-medication literature (Hawn, Cusack & Amstadter, under second review) demonstrated that, by and large, studies assessed a range of generalized drinking motives, tension-reduction strategies, or alcohol expectancies more broadly to infer trauma-specific drinking to cope rather than assess trauma-related drinking to cope specifically. In fact, the review produced only one measure that assesses alcohol expectancies with regard to PTSD symptoms specifically: the PTSD-Alcohol Expectancies Questionnaire (P-AEQ; Norman, Inaba, Smith, & Brown, 2008). However, the P-AEQ, which has been applied limitedly in the context of the self-medication literature (Hawn et al., under second review), assesses expectations of the effects of alcohol and does not capture drinking motives nor the frequency at which an individual uses alcohol to cope with PTSD symptoms.
The most commonly used assessment with regard to the PTSD-AUD self-medication literature (Hawn et al., under second review) is the drinking to cope subscale of the Drinking Motives Questionnaire—Revised (DMQ-R; Cooper, 1994). The frequency at which the DMQ(-R) is used to infer drinking to cope with PTSD symptoms is problematic because the DMQ-Cope subscale assesses drinking to cope with negative internal experiences generally and is not at all specific to drinking to cope with trauma-related symptoms. Specifically, the subscale asks the frequency at which individuals drink to 1) “forget your worries”; 2) “because it helps you when you feel depressed or nervous”; 3) “to cheer you up when you’re in a bad mood”; 4) “because you feel self-confident or sure of yourself”; 5) “to forget about your problems”. Demonstration of this tendency in the literature to equate general drinking to cope motives with drinking to cope with trauma-related symptoms specifically extends beyond the prevalent use of DMQ-Cope to other measures assessing general coping motives or alcohol expectancies (e.g., Brief COPE [Carver, 1997], Comprehensive Effects of Alcohol [CEOA; Fromme, Stroot, & Kaplan, 1993], Reasons for Drinking Scale [Beseler, Aharonovich, & Hasin, 2011], and subjective measures of self-medication [Sheerin et al., 2016]). To date, it appears that no studies have explicitly examined the extent (i.e., frequency, quantity) of drinking to cope with trauma-related symptoms (e.g., intrusive thoughts, avoidance, anhedonia, hypervigilance) specifically, making this a critical void to fill.
Provided that the self-medication model is inherently mediational by design, whereby the relationship between PTSD and alcohol use problems is explained at least partially by drinking to cope with trauma-related symptoms (see Figure 1 for review), it would follow that the use of mediational analyses to test its validity is imperative. Surprisingly, however, use of mediational analyses in the PTSD-alcohol self-medication literature as a whole is sparse and has resulted in disparate findings (Hawn et al., under second review). Consistent with the conceptual framework of the self-medication model, several studies have tested the mediating effects of coping motives, using the DMQ-Cope, on the relation between PTSD symptoms and alcohol consumption and/or problems. The majority of these studies have demonstrated support for this model (e.g., Tomaka et al., 2017; Kaysen et al., 2007; McCabe et al., 2018), while some failed to demonstrate support (Delker & Freyed, 2014).
Consideration of other important factors, such as type and frequency of trauma, also regularly differs between studies. Given research on the meaningful differences with regard to PTSD and other outcomes between type (Frans, Rimmö, Åberg, & Fredrikson, 2005) and amount (Cloitre et al., 2009) of trauma experienced, failure to account for trauma exposure could at least partially explain some of the inconsistencies in the self-medication literature.
Study Aims
The present study sought to test the self-medication model using a novel measure of trauma-related drinking to cope (TRD). Aim 1 sought to test whether the relation between PTSD symptoms and AUP was significantly accounted for by the effects of TRD, while accounting for its relationship with DMQ-Cope. Aim 2 sought to investigate whether this self-medication mediation model was moderated by sex. Analyses were conducted both cross-sectionally, using a large sample and comprehensive assessment battery, and longitudinally, using a smaller sample and abbreviated measures. It was hypothesized that TRD would account for the relation between PTSD symptoms and AUP, over and above the effects of DMQ-Cope. Additionally, it was hypothesized that this indirect effect would be stronger for females than males and that this pattern of results would hold across the cross-sectional and confirmatory longitudinal analyses.
Methods
Study Participants and Recruitment
Participants for the present study were recruited from an ongoing cohort study from a large urban university that began in 2011 and includes comprehensive genotyping on all willing participants (Spit for Science [S4S]; NIAAA-R37 AA011408). Individuals were contacted about participating in a spin-off study, Life Events and Alcohol Use (LEAU; P50AA022537, PI: Amstadter, F31AA025820, PI: Hawn), because they met the following study inclusion criteria: had endorsed at least one lifetime traumatic event during a prior S4S survey and reported any lifetime alcohol use on a prior S4S survey. The intention of the LEAU survey was to gather more in-depth information about participant PTSD symptoms, trauma history, and trauma-related drinking to cope. Those expressing an interest in participating in LEAU were emailed a survey link to be completed via REDCap (Harris et al., 2009). The LEAU survey took approximately 20 minutes to complete, after which participants were given the option to collect $20 compensation via cash in person or electronically via Amazon. Of the 1,901 participants who enrolled, 1,848 completed the survey in full (2.8% began but did not complete the entire survey). The present sample (N=1,896) included LEAU participants who had available data on all measures of interest. Of these, 70.18% identified as female. Consistent with the parent study, the LEAU sample was generally representative of the overall university population from which it was recruited with regard to race (49.4% White, 18.9% African-American, 16.3% Asian, 8.0% multi-racial, 6.0% Hispanic/Latino, .6% declined to respond, .4% Pacific Islander, .4% American Indian/Native Alaskan). There were no differences between those in the larger parent study who were and were not included in LEAU on race. However, those included in LEAU were slightly younger (18.46 vs. 18.51, t=4.43, p<.01; Cohens d: .14) and were more likely to be female (70.18% vs. 59.45%; χ2=74.226, p<.001; Cramer’s V: .09). These effects, though significant, were very small and likely not meaningful. All study procedures were approved by the University’s Institutional Review Board.
Study Measures
Trauma Exposure.
Trauma history was obtained in LEAU via the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000), a comprehensive assessment of potentially traumatic events. The TLEQ is a 23-item self-report measure which assesses whether and when participants experienced a range of potentially traumatic events (e.g., natural disaster, assault, accidents, illness/injury) and how many times each traumatic event occurred (i.e., allows for calculation of a comprehensive lifetime trauma count for each participant). The TLEQ has evidenced good test-retest reliability (average of 83% agreement across traumas) and good convergent validity with interview assessments of trauma exposure (Kubany et al., 2000). A lifetime trauma load variable was created by summing the frequency endorsements for each trauma included in the TLEQ. A dichotomous trauma type variable was also created to reflect endorsement status of having ever experienced an interpersonal (i.e., combat, sudden or unexpected death of a loved one, life-threatening or permanently disabling accident experienced by a loved one, robbery, physical assault, witnessing physical assault, threatened with death or serious physical harm, childhood physical abuse, family and domestic violence, childhood sexual abuse, adult sexual assault, unwanted sexual experience, and stalking) or other (i.e., natural disaster, motor vehicle accident, other accident, miscarriage, abortion, life-threatening illness, other) type of trauma.
PTSD.
Presence of PTSD symptoms in the past 30 days was assessed using the PTSD Checklist-5 (PCL-5; Weathers et al., 2013). The PCL-5 is a 20-item questionnaire, corresponding to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) symptom criteria for PTSD. The self-report rating scale is 0–4 for each symptom, ranging from “Not at all” to “Extremely”. The PCL-5 has demonstrated good test-retest reliability (r = .82), and convergent (r’s = .74 to .85) and discriminant (r’s = .31 to .60) validity (Blevins, Weathers, Davis, Witte, & Domino, 2015). Cronbach’s alpha calculated from the LEAU sample suggested excellent internal consistency (.96). A total symptom severity score (range 0–80) was obtained by summing the scores for each of the 20 items.
Alcohol Consumption and Related Consequences.
Participants reported on their past year alcohol use with ordinal frequency and quantity items from the Alcohol Use Disorders Identification Test (AUDIT), which is a 10-item screening measure developed by the World Health Organization to identify individuals with alcohol problems (Babor, De La Fuente, Saunders, & Grant, 1992). The AUDIT assesses alcohol consumption as well as alcohol-related problems (e.g., consequences related to drinking). There is a large body of literature attesting to the psychometric properties of the AUDIT (e.g., Saunders, Aasland, Babor, De la Fuente, & Grant, 1993). The AUDIT evidenced good internal consistency in the LEAU sample (α=.82). The AUDIT total score, which embodies quantity/frequency of alcohol consumption as well as related-problems, was used in the analyses and will heretofore be referred to as alcohol use problems (AUP).
General Drinking to Cope Motives.
General drinking to cope motives were assessed via the 5-item coping subscale of the Drinking Motives Questionnaire-Revised (DMQ-R; Cooper, 1994). Participants are asked to rate the frequency of drinking for each of the listed motives on a 1 to 5 scale, on which 1 equals “almost never/never” and 5 equals “almost always”. The possible range of scores for the DMQ-Cope subscale is 5–25. The DMQ-Cope has demonstrated strong test-retest reliability (ICC=.80; Cheng, Phillips, Zhang, & Wang, 2016) and evidenced good internal consistency within LEAU (α=.88). Response items from the DMQ-Cope measure were summed to create a continuous score.
Trauma-related Drinking to Cope.
A 4-item trauma-related drinking to cope (TRD) measure was created for and administered as part of the LEAU study. Using the same response options from the DMQ-R, which query frequency of alcohol use on a 1 to 5 Likert scale (1=Almost Never/Never to 5=Almost Always/Always), frequency of alcohol use to cope with symptoms specific to each PTSD cluster (i.e., re-experiencing [e.g., repeated, disturbing dreams of the traumatic event; Item 1], avoidance [e.g., avoiding memories, thoughts, or feelings related to the trauma; Item 2], negative cognitions and mood [e.g., anhedonia; Item 3] , and arousal [e.g., hypervigilance; Item 4]) was assessed. The possible range of scores for the TRD questionnaire is 4–20. Cronbach’s alpha calculated from the LEAU sample suggested the TRD items demonstrated good internal consistency (.88). The psychometric properties of TRD, as well as detailed information about the wording of the four TRD items and the response scale used, have been reported on in detail elsewhere (Hawn, Aggen, Cusack, et al., under review). Response items from the TRD measure were summed to create a continuous score.
Probable PTSD (used in longitudinal analysis).
Participants endorsing any lifetime history of trauma exposure in the S4S Parent study were administered the Primary Care PTSD Screen (PC-PTSD; Prins et al., 2003). The PC-PTSD is a screening instrument with four “Yes/No” items, each representing one of the three Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) (Association & Association, 2000)) PTSD symptom clusters, with avoidance and emotional numbing separated out into two separate items. The newest version of the PC-PTSD (PC-PTSD-5; Prins et al., 2016), which was created to reflect the new Diagnostic and Statistical Manual of Mental Disorders (DSM-5; Association, 2013) criteria for PTSD, was not yet available when the S4S study battery was compiled. PC-PTSD total score, assessed in the S4S parent study prior to enrollment in LEAU (Fall 2014, Spring 2015), was used as the independent (time point 1) variable in the longitudinal analysis of the self-medication model.
AUD (used in longitudinal analysis).
Participants who reported having ever consumed alcohol in the S4S Parent study were asked items related to DSM-5 (Association, 2013) AUD criteria, with some criteria assessed using multiple items. For all but 2 items, response options were “never,” “1–2 times,” or “3 or more times,” which were scored 1, 2, and 3, respectively. These items were then recoded as 0 or 1 to indicate whether the criterion had been met at least once (no or yes) or three or more times (no or yes) in the past year. Items addressing craving and tolerance had response options of “no” and “yes,” coded 0 and 1, respectively. An AUD count variable for symptoms met at least once in the past 12 months was derived. Given that the sample was comprised of emerging adults, a developmental period which typically precedes the average age of onset for a formal AUD (Grant et al., 2015), the AUD count variable for symptoms met at least once (as opposed to three times) in the past year was created in an effort to capture subthreshold alcohol-related consequences. Sum scores were created using a missing data threshold, such that scores were only computed for individuals with data on 6 or more items. Participants were given the option of skipping questions.
Data Analytic Plan
Data checking.
Variables were examined for distributional assumptions prior to analysis. The TRD composite score was significantly skewed (2.68) and kurtotic (7.92) and was therefore log transformed. This score showed improvement in skew (1.78) and kurtosis (2.46), and thus was used as the measure of drinking to cope with trauma-related distress in the analyses. Lifetime trauma load was also skewed (2.52) and kurtotic (12.00) and was log transformed. This score showed improvement in skew (−.218) and kurtosis (−.648) and was used as a covariate in the mediation analyses. In order to reduce non-essential multicollinearity and increase interpretability of findings (Cohen, 2003), all continuous predictors were centered prior to conducting analyses.
Analytic Plan Aim 1: Use of TRD to test the self-medication model.
Hypothesis 1 was that TRD would mediate the effect of PTSD symptoms on AUP symptoms, over and above the effects of DMQ-Cope and study covariates (1a). It was hypothesized that DMQ-Cope would also mediate this relation, over and above study covariates (1b). In order to investigate the outlined study hypotheses, first, mediation analyses testing TRD and DMQ-Cope as independent mediators of the relation between PTSD symptoms and AUP were conducted. Analyses were conducted in Mplus, Version 6.12 (Muthén & Muthén, 2012), using the Model Indirect command. Second, a correlated mediation model was conducted in Mplus in which TRD and DMQ-Cope were both included as mediators and allowed to covary within the same model. This correlated mediation approach was conducted to account for the likely association between TRD and DMQ-Cope.
Hypothesis 2 was that these effects would be stronger for females compared to males. To test this hypothesis, a moderated mediation model, allowing TRD and DMQ-Cope to covary, while sequentially examining these effects for females and then males, was conducted. In order to test for moderated mediation, interactions between PTSD symptoms and sex to predict TRD and DMQ-Cope, and interactions between TRD and DMQ-Cope and sex to predict AUP were estimated in conjunction with the Model Indirect command. Mplus uses the product of coefficients strategy to calculate indirect effects (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; Preacher & Hayes, 2004).
Missing data on endogenous variables was estimated as a function of the observed exogenous variables under the missingness at random assumption (Schafer & Graham, 2002). As including covariates may increase the power of a statistical test by minimizing uncontrolled variability and accounting for variance that would otherwise be thought of as error (Turner et al., 2012), several key covariates (i.e., sex, race, cohort, lifetime trauma load, trauma type) were included in the initial study models. Cohort was included based on previous research using this data demonstrating significant differences in AUP between the cohorts (Bountress et al., under review). Covariates deemed non-significant (p > .05) in the initial model were removed in subsequent models in order to improve model fit and parsimony. Significant covariates retained in the subsequent models included trauma load, trauma type, and sex, accounting for partial variance in TRD; trauma load, trauma type, race, and sex accounting for partial variance in DMQ-Cope; and sex, cohort, and race accounting for partial variance in AUP. The study model was assessed for goodness of fit based on whether the values of the following fit indices are consistent with accepted standards (i.e., Hu, 1999): Comparative Fit Index (CFI): ≥.95, Root Mean Square Error of Approximation (RMSEA) ≤ .06, and Standardized Root Mean Square Residual (SRMR) <.08.
Given the more phenotypically rich LEAU sample was limited by cross-sectional data, the same mediation approach was also applied to data from both LEAU and S4S in order to test the self-medication hypothesis longitudinally (N=899). TRD (1a) and DMQ-Cope (1b), assessed in LEAU (Fall 2016), were regressed onto the maximum endorsed probable PTSD score, calculated using the Primary Care PTSD Screen (PC-PTSD; Prins et al., 2003), assessed in the S4S parent study prior to enrollment in LEAU (Fall 2014, Spring 2015). AUD symptom severity, assessed the Spring following enrollment in LEAU (Spring 2017), was regressed on TRD, DMQ-Cope, and PC-PTSD.
Results
Study Descriptive Statistics and Correlations
Correlational analyses and descriptive statistics are provided in Table 1. Interpretation of sample means as well as differences in the distribution of TRD and other variables among individuals exceeding and not exceeding the PCL-5 and AUDIT cutoff scores are provided in the TRD psychometric paper (Hawn et al., under review). As hypothesized, all constructs included in the full model were significantly associated with one another. Notably, TRD and DMQ-Cope were moderately correlated but not multicollinear (r = .60, p<.001). Moreover, whereas an overwhelming majority (72.96%) of participants in the sample endorsed at least some level of drinking to cope per the DMQ-Cope, only around one-third (34.71%) of participants endorsed at least some level of drinking to cope with trauma-specific symptoms. Similarly, histograms (Figure 2) revealed that DMQ-Cope was normally distributed, unlike the un-transformed TRD measure.
Table 1.
Correlation Table and Descriptive Statistics of Study Constructs
| Variable | Total Mean (SD) | Females Mean (SD) | Males Mean (SD) | Range | 1 | 2 | 3 | 4 | 5 | SEX t-test | RACE# t-test |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. TRD | 5.27 (2.51) | 5.31 (2.48) | 5.20 (2.59) | 4 – 20 | 1.00 | -- | -- | -- | -- | −1.57 | 1−4 NS |
| 2. DMQ-Cope | 8.63 (4.10) | 8.69 (4.07) | 8.50 (4.19) | 5 – 25 | 0.60*** | 1.00 | -- | -- | -- | −0.90 | 13.07**2−4 NS |
| 3. PTSD | 15.23 (17.03) | 16.74 (17.66) | 11.66 (14.77) | 0 – 80 | 0.56*** | 0.42*** | 1.00 | -- | -- | 4.35*** | 1−4 NS |
| 4. AUP | 7.00 (5.26) | 6.66 (5.06) | 7.86 (5.64) | 0 – 37 | 0.44*** | 0.48*** | 0.22*** | 1.00 | -- | 6.35*** | 14.38***24.18***3−4 NS |
| 5. TRAUMA LOAD | 8.38 (9.18) | 10.38 (9.48) | 7.99 (9.22) | 0 – 94 | 0.35*** | 0.24*** | 0.43*** | 0.19*** | 1.00 | 5.81*** | 1−2.19*25.86***3NS4−2.02* |
Note: TRD = Trauma-related drinking to cope measure; DMQ-Cope = Drinking Motives Questionnaire Coping subscale; PTSD = Posttraumatic stress disorder symptom severity; DSM-5; AUP = Alcohol use problems;
p < .001,
p < .01,
p < .05;
Race was dummy coded to represent
White vs. Black,
White vs. Asian,
White vs. Hispanic/Latino,
White vs. Other; NS = not significant
Figure 2.
TRD and DMQ Histograms
Aim 1: Self-Medication Mediation Models
Examination of TRD and DMQ-Cope separately.
Rows one and two of Table 2 show the results for the independent regression models conducted using TRD and DMQ-Cope as mediators, respectively. There was a significant indirect effect of PTSD symptoms on AUP through TRD, which accounted for 87.97% of the total effect. This model demonstrated good fit to the data (χ2 (10) = 20.928, p = .022; CFI: .991, RMSEA: .024; SRMR: .009). DMQ-Cope was a significant mediator as well, with a significant indirect effect that accounted 83.33% of the total effect. This model also demonstrated good fit to the data (χ2 (6) = 11.851, p = 0.065; CFI: .994; RMSEA: .023; SRMR: .007).
Table 2.
Path coefficients and test statistics for self-medication mediation models
| Total direct effect | Total indirect effect (mediation) | Total effect (indirect + direct) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mediator | Model R2 | β | SE | Ratio | β | SE | Ratio | β | SE | Ratio | Mediated proportion of total effect |
| TRD | 0.242 | −0.035 | 0.025 | −1.407 | 0.256 | 0.016 | 15.900*** | 0.220 | 0.023 | 9.703*** | .8797 |
| DMQ-Cope | 0.271 | 0.036 | 0.022 | 1.604 | 0.180 | 0.013 | 13.416*** | 0.216 | 0.023 | 9.517*** | .8333 |
| Correlated mediation | 0.309 | −0.069 | 0.024 | −2.844** | 0.282 | 0.017 | 16.603*** | 0.214 | 0.023 | 9.331*** | .8034 |
| TRD | 0.334 | - | - | 0.152 | 0.016 | 9.526*** | - | - | - | .4330 | |
| DMQ Cope | 0.195 | - | - | 0.130 | 0.012 | 10.570*** | - | - | - | .3704 | |
| Moderated mediation | 0.307 | −0.063 | 0.024 | −2.609** | 0.410 | 0.029 | 14.183*** | 0.347 | 0.030 | 11.587*** | .8668 |
| TRD | 0.351 | - | - | - | 0.213 | 0.024 | 8.798*** | - | - | - | .4503 |
| DMQ Cope (males) | 0.205 | - | - | - | 0.197 | 0.021 | 9.553*** | - | - | - | .4165 |
| Moderated mediation | 0.307 | −0.064 | 0.024 | −2.676** | 0.239 | 0.017 | 14.216*** | 0.175 | 0.024 | 7.330*** | .7888 |
| TRD | 0.347 | - | - | - | 0.123 | 0.014 | 8.782*** | - | - | - | .4059 |
| DMQ Cope (females) | 0.202 | - | - | - | 0.117 | 0.012 | 9.593*** | - | - | - | .3861 |
Abbreviations: TRD = Trauma-related drinking to cope measure (log transformed); DMQ-Cope = Drinking Motives Questionnaire Coping subscale. Note that the ratio column (Z-score) corresponds to the following p-values: 1.96* (p=0.05); 2.58** (p=0.01); 3.29*** (p=0.001).
Correlated mediation model.
Given that the indirect pathways through TRD and DMQ-Cope were both significant, and that these two constructs were moderately correlated (r = .60), a mediation model was fit which included both constructs and allowed them to correlate. The results of this model are shown in row three of Table 2. The model demonstrated good fit to the data (χ2 (13) = 18.177, p = 0.151; CFI: .998; RMSEA: .014; SRMR: .009). There were significant indirect effects of both TRD and DMQ-Cope. Combined, TRD and DMQ-Cope accounted for 80.34% of the total effect of PTSD symptoms on AUP. A larger proportion of this indirect effect (43.30% of the total effect of PTSD symptoms on AUP) was accounted for by TRD, while a slightly smaller portion (37.04% of the total effect) was attributed to DMQ-Cope. However, the indirect effects of TRD and DMQ-Cope were not statistically distinct, b = .007, p = .325, suggesting that neither mediator accounted for statistically more or less of the total effect compared to the other.
Aim 2: Sex Differences in Self-Medication
Moderated correlated mediation model.
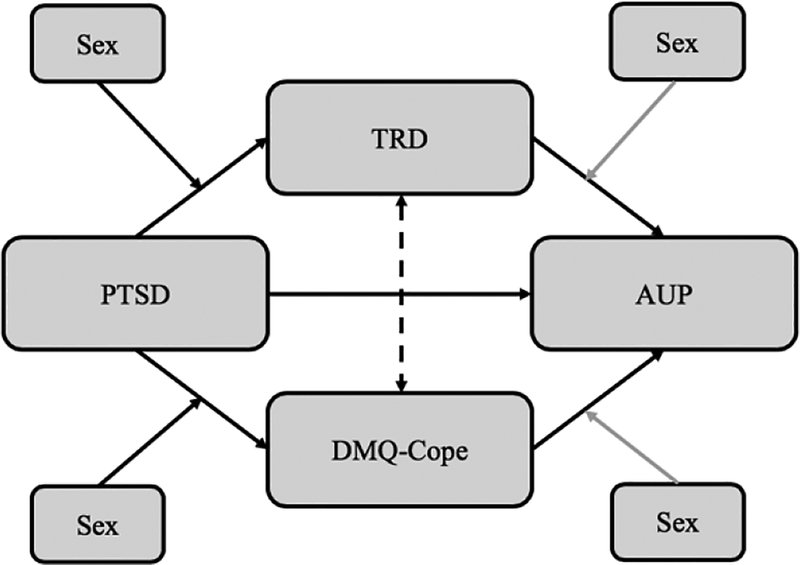
In order to test whether these indirect effects were moderated by sex (Aim 2), a moderated correlated mediation model was conducted, examining the indirect effect for males and then females. These results are shown in rows four and five of Table 2. The model tested whether sex significantly interacted with PTSD symptoms to influence TRD/DMQ-Cope and whether sex significantly interacted with TRD/DMQ-Cope to influence AUP (see Figure 3 for reference). Results showed significant interactions between sex and PTSD symptoms on TRD and DMQ-Cope (p’s < .001) but failed to demonstrate evidence of a significant interaction between sex and TRD or DMQ-Cope on AUP (p’s > .30). The model demonstrated good fit to the data after eliminating the nonsignificant interaction terms (χ2 (14) = 16.462, p = 0.286; CFI: .999; RMSEA: .010; SRMR: .007). Overall, results showed stronger effects of PTSD symptoms on both TRD and DMQ-Cope for males (β = 0.804 and β = 0.565, respectively, p’s < .001) compared to females (β = 0.463 and β = 0.333, p’s < .001). With males set as the reference group, TRD and DMQ-Cope accounted for 45.03% and 41.65% of the total effect, respectively. With females set as the reference group TRD and DMQ-Cope accounted for 40.59% and 38.61% of the total effect, respectively.
Figure 3.
Moderated Correlated Mediation; Note: PTSD=Posttraumatic stress disorder symptom severity; TRD=Trauma related drinking to cope; DMQ-Cope=Drinking motives questionnaire coping subscale; AUP=Alcohol use problems.
Longitudinal model.
A longitudinal model was conducted incorporating data from the S4S parent study. Maximum endorsed PC-PTSD score prior to LEAU enrollment was the time point 1 predictor variable, TRD and DMQ-Cope assessed in LEAU were included as time point 2 mediator variables, and AUD criterion count (AUDIT total not available) assessed following LEAU participation was the time point 3 outcome variable. AUD criterion count assessed at time point 1 was included as a covariate in the model to control for prior symptoms of AUD. Because PC-PTSD was multicollinear (r = .90) with the PC-PTSD X Sex interaction term in the moderated mediation model, the standard errors of the model parameter estimates could not be computed and we were therefore unable to test the moderating effects of sex in the longitudinal model. These results suggest that the PC-PTSD X Sex interaction term did not provide information over and above the main effects of PC-PTSD and sex. Consistent with findings using the cross-sectional data, both TRD (β = 0.021, p = 0.025) and DMQ-Cope (β = 0.067, p < .001) significantly mediated the relation between PTSD symptoms and AUD criterion count. However, unlike the models conducted using the more comprehensive cross-sectional data, results of the correlated mediation model suggested that DMQ-Cope accounted for a significantly (b = −0.076, p = 0.012) larger proportion of the total effect (43.51%) than TRD (13.64%). The best fitting model (χ2 (6) = 7.832, p = 0.251; CFI: .998; RMSEA: .018; SRMR: .014) accounted for the effect of AUD criterion count assessed at time point 1 on the variance in TRD (β = 0.163, p < .001), DMQ-Cope (β = 0.121, p = .001), and AUD at time 3 (β = 0.333, p < .001). Significant covariates retained in the longitudinal model included race (accounting for partial variance in both DMQ-Cope and AUD) and sex (accounting for partial variance in AUD).
Discussion
Overview of findings
The self-medication model is the most predominantly used model to explain PTSD-AUD comorbidity, although the current literature to date has limitations (e.g., lack of trauma-specific drinking to cope measures, failing to employ a mediational statistical design, purely cross-sectional data). This study attempted to address these limitations and in doing so produced three main findings. First, findings demonstrated evidence for TRD as a distinct measure of drinking to cope motives in the context of PTSD symptoms. Second, results showed general support for the self-medication model. There were demonstrated unique effects of both general drinking to cope motives (DMQ-Cope) and drinking motives related to coping with trauma-related symptoms specifically (TRD) on the relation between PTSD symptoms and AUP. Third, results showed evidence for key sex differences with respect to the self-medication model, such that males with high levels of PTSD symptoms were more likely to drink to cope with trauma-related distress than females.
TRD as it relates to other variables
The present study sought to fill a notable gap in the literature by testing the self-medication model using a novel measure of drinking to cope with trauma-related symptoms specifically (TRD). This was done via modification of a prolific measure of general drinking to cope (DMQ-Cope; Cooper, 1994) in order to query the frequency of alcohol use to cope with symptoms specific to each PTSD cluster (i.e., re-experiencing, avoidance, negative cognitions and mood, and arousal; Hawn et al., under review]). TRD was significantly associated with PTSD symptom severity, alcohol use severity, and DMQ-Cope. Notably, TRD and DMQ-Cope were moderately correlated but not multicollinear, suggesting that, as expected, they are associated yet distinct constructs. The stark contrast between the rate at which participants endorsed DMQ-Cope versus TRD belies arguably one of the most common assumptions in the self-medication literature to date: that drinking to cope with negative affect is synonymous with drinking to cope with trauma-related symptoms specifically. As such, it is plausible that much of the research to date has overestimated the relation between drinking to cope and PTSD.
Support for the self-medication hypothesis
Cross-sectionally.
Results from the mediation models were consistent with the self-medication hypothesis, such that TRD explained a significant proportion of the relation between PTSD symptoms and AUP, even when accounting for the indirect effect of DMQ-Cope within the same model. The unique variance accounted by both TRD and DMQ-Cope in the model provides evidence that these are associated, yet separate constructs. The significant mediating effect of DMQ-Cope on the relation between PTSD and AUP in the present sample is consistent with prior research demonstrating support for DMQ-Cope as a mediator between PTSD and problematic drinking (Kaysen et al., 2007; McCabe et al., 2018; Tomaka et al., 2017). This prior research, in combination with the novel TRD findings, provides iterative support for the self-medication model. Further, present findings demonstrating a unique effect of TRD on PTSD-AUP comorbidity above and beyond DMQ-Cope support the use of a specific measure of trauma-specific drinking motives moving forward.
Longitudinally.
Given the basic causal premise of the self-medication model, the present study sought to substantiate the primary analyses longitudinally. Findings were generally consistent with those generated in the primary correlated mediation model. However, the moderation by sex could not be replicated due to poor model fit and multicollinearity between the PC-PTSD and moderator variables. Similar to the cross-sectional analyses, the overall model was significant and both TRD and DMQ-Cope accounted for significant proportions of the variance between PC-PTSD and AUD. However, unlike the cross-sectional analyses in which the proportion accounted for by DMQ-Cope and TRD did not differ, the proportion accounted for by DMQ-Cope was significantly higher than that accounted for by TRD in the longitudinal model. This finding could potentially be an artifact of our sample, given that college-age predates the average onset of AUD (Grant et al., 2015). For instance, given the sample was comprised of emerging adults, a developmental period which typically precedes the average age of onset for a formal AUD (Grant et al., 2015), it is possible that the AUDIT total score used in the cross-sectional analyses, which captures alcohol consumption and related problems, provided a more developmentally appropriate depiction of alcohol use problems, as opposed to the AUD criterion count used in the longitudinal analysis. Furthermore, differences in magnitude of effects seen between the cross-sectional and longitudinal analyses could be a product of either phenotypic strength (i.e., the cross-sectional analyses included comprehensive and validated measures of PTSD symptoms and alcohol use, whereas the longitudinal analysis included the brief PC-PTSD screen and a summation of items meant to reflect various AUD criteria) or methodological rigor (i.e., the ability to test these relationships temporally in the longitudinal sample). Another notable potential limitation of the supplemental longitudinal analyses is possible overlap between time point 2 (TRD/DMQ-Cope) and time point 3 (AUD). AUD at time point 3 was assessed in the Spring of 2017 and queried symptoms experienced in the past 12 months. TRD at time point 2 was assessed in the Fall of 2016, potentially confounding the temporal precedent of TRD before AUD. Future studies using other samples and more comprehensive measures of PTSD symptomatology should test the mediational effects of TRD within a longitudinal framework, as such research would ultimately decrease bias that accompanies cross-sectional approaches to mediation (Maxwell & Cole, 2007) and provide further validated empirical support for the self-medication model.
Inclusion of covariates.
In addition to testing the veracity of our conceptual model within a longitudinal framework, another notable strength of the present study is the inclusion of potentially relevant factors, such as cohort, sex, race, lifetime trauma load, and trauma type. The final models demonstrated significant effects of trauma load, trauma type and sex on both TRD and DMQ-Cope. Interestingly, however, whereas race was retained as a significant covariate accounting for the effects of DMQ-Cope, it did not significantly account for partial variance in TRD. Future research examining the influence of race on generalized drinking motives but not trauma-specific drinking motives warrants further examination. Of note, we included all potentially traumatic events assessed in the TLEQ in our calculations of trauma load and trauma type. The possibility that some events endorsed on the TLEQ may not constitute a traumatic event, as defined by the DSM-5, is a potential limitation. That said, the TLEQ is a comprehensive assessment of potentially traumatic events that has demonstrated good reliability, as well as convergent validity with interview assessments of trauma exposure (Kubany et al., 2000). Failure to account for important confounds likely contributes to the inconsistency of the self-medication literature and may result in misleading or skewed findings. Despite the inclusion of many relevant covariates in the model, future studies should extend additional risk factors to include other psychiatric conditions, including panic disorder, major depression and social phobia (McFarlane, 1998).
Important sex considerations
The present study also found significant, albeit small, sex effects with regard to the self-medication model. Despite the absence of significant mean differences in TRD or DMQ-Cope between males and females, findings suggested that, in the presence of high PTSD symptoms, males are drinking more to cope with their PTSD symptoms compared to their female counter parts. This finding was contrary to study hypothesis, which assumed that females may be more likely to drink to cope with trauma-related symptoms given their higher rates of PTSD symptoms compared to males (Breslau et al., 1998; Kessler et al., 1995). Our finding that males drank more to cope with PTSD symptoms in the presence of high PTSD could potentially explain the limited research demonstrating higher rates of PTSD-AUD comorbidity among males compared to females (King et al., 2006), however, the overall literature on sex differences with regard to PTSD-AUD comorbidity is inconsistent (Brady et al., 1993; Brady & Randall, 1999; Goldstein et al., 2012b; Kessler et al., 1997; Sonne et al., 2003). Given the mixed literature on this topic to date, we offer this as one potential thread to add to still forming tapestry. With regard to clinical utility, these findings suggest that assessing for TRD among males may be particularly critical in identifying individuals at potential risk of “self-medicating” through the use of alcohol. The presence of significant sex effects with regard to self-medication in the present study could potentially be explained by gender differences in coping strategies (e.g., avoidant coping versus emotion-focused coping). However, the literature on this topic is also mixed and seems to depend on how coping is defined and measured (Eaton & Bradley, 2008). Additionally, it is noteworthy that the present study sample was large and the sex effects demonstrated in the moderated correlated mediation model were relatively small. There is much left to be unveiled with regard to sex differences in the context of the self-medication model, creating a valuable direction for future research.
Clinical implications
The present findings incite a need for change in the current self-medication literature, which up until now, has as a whole been operating under the assumption that general drinking to cope is synonymous with drinking to cope with trauma-specific symptoms. Given evidence for the misuse of this broad application, increased use of measures that assess PTSD-symptom-specific alcohol expectancy (P-AEQ; Norman et al., 2008) and creation of measures that assess PTSD-symptom-specific alcohol motives and frequency (i.e., TRD) are warranted. Resolution of this misconception has important clinical implications, particularly given the overwhelming rates of PTSD-AUD comorbidity and related public health outcomes (Brown et al., 1999a; Kessler et al., 2005; Kessler et al., 1995). Creation of a gold standard measure for self-reported trauma-specific drinking to cope would serve not only to improve methodology by generating reliability and validity, but also could be useful in targeting individuals with PTSD who may be at increased risk for AUD and therefore lead to improvements in treatment and prevention efforts.
Additional future directions
Given that TRD did not fully mediate the effect between PTSD symptoms and alcohol use severity reinforces that there are likely multiple pathways through which trauma may influence drinking patterns which are likely not mutually exclusive and that the self-medication model is not the “silver bullet”, warranting the need for investigation into additional models of comorbidity to inform clinical intervention. Moreover, given evidence for moderate overlap in genetic variance between PTSD and AUD (Sartor et al., 2011; Xian et al., 2000), genetically informed research surrounding the self-medication model is warranted. Investigations into the shared genetic risk and biological underpinnings of comorbid PTSD and AUD would help to further elucidate common etiological pathways underlying PTSD, AUD, and intermediate trauma-specific drinking to cope, which is imperative to the development of effective prevention and treatment programs.
Acknowledgments
Spit for Science has been supported by Virginia Commonwealth University, P20 AA017828, R37AA011408, K02AA018755, and P50 AA022537 from the National Institute on Alcohol Abuse and Alcoholism, and UL1RR031990 from the National Center for Research Resources and National Institutes of Health Roadmap for Medical Research. Sage Hawn’s time is currently funded by NIAAA F31 AA025820-01. Dr. Amstadter’s time is supported by NIAAA K02 AA023239. Dr. Sheerin’s time is supported by K01-AA025692. We would like to thank the Spit for Science participants for making this study a success, as well as the many University faculty, students, and staff who contributed to the design and implementation of the project.
Footnotes
Findings from this data have been disseminated via local (i.e., 22nd Annual Research Symposium and Exhibit in Richmond, VA, in April 2018) and international (i.e., International Society for Traumatic Stress Studies in Washington, DC, in November 2018) conferences.
Contributor Information
Sage E. Hawn, Virginia Institute for Psychiatric and Behavioral Genetics and Virginia Commonwealth University
Kaitlin E. Bountress, Virginia Institute for Psychiatric and Behavioral Genetics
Christina M. Sheerin, Virginia Institute for Psychiatric and Behavioral Genetics, Spit for Science Working Group
Danielle M. Dick, Virginia Commonwealth University
Ananda B. Amstadter, Virginia Institute for Psychiatric and Behavioral Genetics and Virginia Commonwealth University
References
- Agabio R, Campesi I, Pisanu C, Gessa GL, & Franconi F (2016). Sex differences in substance use disorders: focus on side effects. Addict Biol, 21(5), 1030–1042. doi: 10.1111/adb.12395 [DOI] [PubMed] [Google Scholar]
- Agabio R, Pisanu C, Luigi Gessa G, & Franconi F (2017). Sex differences in alcohol use disorder. Current Medicinal Chemistry, 24(24), 2661–2670. [DOI] [PubMed] [Google Scholar]
- Arnedt JT, Rohsenow DJ, Almeida AB, Hunt SK, Gokhale M, Gottlieb DJ, & Howland J (2011). Sleep following alcohol intoxication in healthy, young adults: effects of sex and family history of alcoholism. Alcohol Clin Exp Res, 35(5), 870–878. doi: 10.1111/j.1530-0277.2010.01417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association, A. P., & Association, A. P. (2000). DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision. Washington, DC: American Psychiatric Association, 75. [Google Scholar]
- Association, A. P. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Babor TF, De La Fuente J, Saunders J, & Grant M (1992). Audit The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Health Care. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Benjet C, Bromet E, Karam E, Kessler R, McLaughlin K, Ruscio A, … Hill E (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beseler CL, Aharonovich E, & Hasin DS (2011). The enduring influence of drinking motives on alcohol consumption after fateful trauma. Alcohol Clin Exp Res, 35(5), 1004–1010. doi: 10.1111/j.1530-0277.2010.01431.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Brady K, Perez-Fuentes G, Okuda M, & Wang S (2013). Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: results from National Epidemiological Survey on Alcohol and Related Conditions. Drug Alcohol Depend, 132(3), 630–638. doi: 10.1016/j.drugalcdep.2013.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for DSM- 5 (PCL- 5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. [DOI] [PubMed] [Google Scholar]
- Blumenthal H, Leen-Feldner EW, Knapp AA, Badour CL, & Boals A (2015). Traumatic event exposure and alcohol use expectancies among adolescents. Journal of Child & Adolescent Substance Abuse, 24(6), 337–343. doi: 10.1080/1067828X.2013.839407 [DOI] [Google Scholar]
- Bonanno GA (2004). Loss, trauma, and human resilience. Have we underestimated the human capacity to thrive after extremely aversive events?. American Psychologist, 59, 20–28. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379. [DOI] [PubMed] [Google Scholar]
- Brady KT, Grice DE, Dustan L, & Randall C (1993). Gender differences in substance use disorders. Am J Psychiatry, 150(11), 1707–1711. doi: 10.1176/ajp.150.11.1707 [DOI] [PubMed] [Google Scholar]
- Brady KT, & Randall CL (1999). Gender differences in substance use disorders. Psychiatr Clin North Am, 22(2), 241–252. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis G, Andreski P, Federman B, & Anthony JC (1998). Epidemiological findings on posttraumatic stress disorder and co-morbid disorders in the general population Adversity, stress, and psychopathology (pp. 319–328). London, Oxford: University Press. [Google Scholar]
- Brown PJ, Stout RL, & Mueller T (1999a). Substance use disorder and posttraumatic stress disorder comorbidity: Addiction and psychiatric treatment rates. Psychology of Addicitive Behaviors, 13(2), 115–122. [Google Scholar]
- Brown PJ, Stout RL, & Mueller T (1999b). Substance use disorder and posttraumatic stress disorder comorbidity: Addiction and psychiatric treatment rates. Psychology of Addictive Behaviors, 13(2), 115–122. [Google Scholar]
- Capraro RL (2000). Why college men drink: Alcohol, adventure, and the paradox of masculinity. Journal of American College Health, 48(6), 307–315. [DOI] [PubMed] [Google Scholar]
- Carver CS (1997). You want to Measure Coping But Your Protocol’s Too Long: Consider the Brief COPE. Int J Behav Med, 4(1), 92–100. [DOI] [PubMed] [Google Scholar]
- Cheng HG, Phillips MR, Zhang Y, & Wang Z (2016). Psychometric properties of the D rinking M otives Q uestionnaire- R evised among community- dwelling current drinkers in the N ingxia autonomous region of C hina. Drug and Alcohol Review, 35(4), 433–441. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stolbach BC, Herman JL, Kolk B. v. d., Pynoos R, Wang J, & Petkova E (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West S, & Aiken L (2003). Applied multiple regression/correlation analysis for the behavioral sciences. Mahwah, NJ: Erlbaum. [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment, 6(2), 117. [Google Scholar]
- Delker BC, & Freyd JJ (2014). From betrayal to the bottle: Investigating possible pathways from trauma to problematic substance use. Journal of Traumatic Stress, 27(5), 576–584. [DOI] [PubMed] [Google Scholar]
- Dick DM, Nasim A, Edwards AC, Salvatore JE, Cho SB, Adkins A, … Clifford J (2014). Spit for Science: launching a longitudinal study of genetic and environmental influences on substance use and emotional health at a large US university. Frontiers in genetics, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon LJ, Leen-Feldner EW, Ham LS, Feldner MT, & Lewis SF (2009). Alcohol use motives among traumatic event-exposed, treatment-seeking adolescents: Associations with posttraumatic stress. Addictive Behaviors, 34(12), 1065–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton RJ, & Bradley G (2008). The role of gender and negative affectivity in stressor appraisal and coping selection. International Journal of Stress Management, 15(1), 94. [Google Scholar]
- Evren C, Sar V, Dalbudak E, Cetin R, Durkaya M, Evren B, & Celik S (2011). Lifetime PTSD and quality of life among alcohol-dependent men: impact of childhood emotional abuse and dissociation. Psychiatry Research, 186, 85–90. [DOI] [PubMed] [Google Scholar]
- Foa EB (1995). Posttraumatic stress diagnostic scale (PDS). Minneapolis: National Computer Systems. [Google Scholar]
- Fossos N, Kaysen D, Neighbors C, Lindgren KP, & Hove MC (2011). Coping motives as a mediator of the relationship between sexual coercion and problem drinking in college students. Addictive Behaviors, 36(10), 1001–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frans Ö, Rimmö PA, Åberg L, & Fredrikson M (2005). Trauma exposure and posttraumatic stress disorder in the general population. Acta Psychiatrica Scandinavica, 111(4), 291–290. [DOI] [PubMed] [Google Scholar]
- Fromme K, Stroot EA, & Kaplan D (1993). Comprehensive effects of alcohol: Development and psychometric assessment of a new expectancy questionnaire. Psychological assessment, 5(1), 19. [Google Scholar]
- Goldstein RB, Dawson DA, Chou SP, & Grant BF (2012a). Sex differences in prevalence and comorbidity of alcohol and drug use disorders: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Stud Alcohol Drugs, 73(6), 938–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Dawson DA, Chou SP, & Grant BF (2012b). Sex differences in prevalence and comorbidity of alcohol and drug use disorders: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Stud Alcohol Drugs, 73(6), 938–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, … Fan A (2017). Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA psychiatry, 74(9), 911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, … Huang B (2015). Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA psychiatry, 72(8), 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant VV, Stewart SH, O’Connor RM, Blackwell E, & Conrod PJ (2007). Psychometric evaluation of the five-factor Modified Drinking Motives Questionnaire—Revised in undergraduates. Addictive Behaviors, 32(11), 2611–2632. [DOI] [PubMed] [Google Scholar]
- Grayson CE, & Nolen-Hoeksema S (2005). Motives to Drink as Mediators Between Childhood Sexual Assault and Alcohol Problems in Adult Women. J Trauma Stress, 18(2), 137–145. doi: 10.1002/jts.20021 [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Cusack SE, & Amstadter AB (under second review). A systematic review of the self-medication hypothesis in the context of posttraumatic stress disorder and comorbid problematic alcohol use. Journal of Traumatic Stress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Aggen SH, Cusack SE, Spit for Science Working Group, Dick DM, & Amstadter AB (under review). Examination of a novel measure of trauma-related drinking to cope. Journal of Consulting and Clinical Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Sheerin CM, Webb BT, Peterson RE, Do EK, Dick D, … Amstadter AB (2018). Replication of the Interaction of PRKG1 and Trauma Exposure on Alcohol Misuse in an Independent African American Sample. Journal of Traumatic Stress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LB, P.M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Ipser JC, Wilson D, Akindipe TO, Sager C, & Stein DJ (2015). Pharmacotherapy for anxiety and comorbid alcohol use disorders. Cochrane Database Syst Rev, 1(CD007505). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Dillworth TM, Simpson T, Waldrop A, Larimer ME, & Resick PA (2007). Domestic violence and alcohol use: Trauma-related symptoms and motives for drinking. Addictive Behaviors, 32(6), 1272–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demier O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, & Anthony JC (1997). Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry, 54, 313–321. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ (1999). Treating addiction as a human process. Northvale, NJ: Jason Aronson. [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM- IV and DSM- 5 criteria. Journal of Traumatic Stress, 26(5), 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Meehan BT, Trim RS, & Chassin L (2006). Marker or mediator? The effects of adolescent substance use on young adult educational attainment. Addiction, 101, 1730–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, & Burns K (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychological Assessment, 12(2), 210. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological methods, 7(1), 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, & Cole DA (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological methods, 12(1), 23. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Fields JA, Monahan CJ, & Bracken KL (2015). Drinking motives among heavy-drinking veterans with and without posttraumatic stress disorder. Addiction research & theory, 23(2), 148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AC (1998). Epidemiological evidence about the relationship between PTSD and alcohol abuse: the nature of the association. Addict Behav, 23(6), 813–825. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus Version 7 user’s guide. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Najavits LM, Gastfriend DR, Barber JP, Reif S, Muenz LR, Blaine J, … Weiss RD (1998). Cocaine dependence with and without PTSD among subjects in the national institute on drug abuse collaborative cocaine treatment study. American Journal of Psychiatry, 155(2), 214–219. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, & Hilt L (2006). Possible contributors to the gender differences in alcohol use and problems. J Gen Psychol, 133(4), 357–374. doi: 10.3200/genp.133.4.357-374 [DOI] [PubMed] [Google Scholar]
- Norman SB, Inaba RK, Smith TL, & Brown SA (2008). Development of the PTSD-alcohol expectancy questionnaire. Addict Behav, 33(6), 841–847. [DOI] [PubMed] [Google Scholar]
- O’Hare T, & Sherrer M (2011). Drinking motives as mediators between PTSD symptom severity and alcohol consumption in persons with severe mental illnesses. Addictive Behaviors, 36(5), 465–469. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Finney JW, & Moos RH (1999). Two-year posttreatment functioning and coping of substance abuse patients with posttraumatic stress disorder. Psychology of Addictive Behaviors, 13, 105–114. [Google Scholar]
- Park CL, & Levenson MR (2002). Drinking to cope among college students: prevalence, problems and coping processes. Journal of Studies on Alcohol, 63(4), 486–497. [DOI] [PubMed] [Google Scholar]
- Peters EN, Khondkaryan E, & Sullivan TP (2012). Associations between expectancies of alcohol and drug use, severity of partner violence, and posttraumatic stress among women. J Interpers Violence, 27(11), 2108–2127. doi: 10.1177/0886260511432151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior research methods, instruments, & computers, 36(4), 717–731. [DOI] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron R, Hugleshofer D, Shaw-Hegwar J, … Sheikh JI (2003). The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry, 9(1), 9–14. doi: 10.1185/135525703125002360 [DOI] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, … Leyva YE (2016). The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Brown PJ, & Kahler CW (2004). Substance use and posttraumatic stress disorders: symtpom interplay and effects on outcome. Addictive Behaviors, 29(8), 1665–1672. [DOI] [PubMed] [Google Scholar]
- Rojas SM, Bujarski S, Babson KA, Dutton CE, & Feldner MT (2014). Understanding PTSD comorbidity and suicidal behavior: associations among histories of alcohol dependence, major depressive disorder, and suicidal ideation and attempts. Journal of Anxiety Disorders, 28 318–325. [DOI] [PubMed] [Google Scholar]
- Sartor CE, McCutcheon VV, Pommer NE, Nelson EC, Grant JD, Duncan AE, … Heath AC (2011). Common genetic and environmental contributions to posttraumatic stress disorder and alcohol dependence in young women. Psychological Medicine, 41(7), 1497–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption- II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: our view of the state of the art. Psychol Methods, 7(2), 147–177. [PubMed] [Google Scholar]
- Schumm JA, & Chard KM (2012). Alcohol and stress in the military. Alcohol Res, 34(4), 401–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheerin C, Berenz EC, Knudsen GP, Reichborn-Kjennerud T, Kendler KS, Aggen SH, & Amstadter AB (2016). A population-based study of help seeking and self-medication among trauma-exposed individuals. Psychol Addict Behav, 30(7), 771–777. doi: 10.1037/adb0000185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorter D, Hsieh J, & Kosten TR (2015). Pharmacologic management of comorbid posttraumatic stress disorder and addictions. American Journal of Addictions, 24, 705–712. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Stappenbeck CA, Luterek JA, Lehavot K, & Kaysen DL (2014). Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology, 123(1), 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonne SC, Back SE, Diaz Zuniga C, Randall CL, & Brady KT (2003). Gender differences in individuals with comorbid alcohol dependence and post-traumatic stress disorder. Am J Addict, 12(5), 412–423. [PubMed] [Google Scholar]
- Stappenbeck CA, Bedard-Gilligan M, Lee CM, & Kaysen D (2013). Drinking motives for self and others predict alcohol use and consequences among college women: The moderating effects of PTSD. Addictive Behaviors, 38(3), 1831–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Pihl RO, Conrod PJ, & Dongier M (1998). Functional associations among trauma, PTSD, and substance-related disorders. Addictive Behaviors, 23, 797–812. [DOI] [PubMed] [Google Scholar]
- Tomaka J, Magoc D, Morales- Monks SM, & Reyes AC (2017). Posttraumatic Stress Symptoms and Alcohol- Related Outcomes Among Municipal Firefighters. Journal of Traumatic Stress, 30(4), 416–424. [DOI] [PubMed] [Google Scholar]
- Turner EL, Perel P, Clayton T, Edwards P, Hernandez AV, Roberts I, … Steyerberg EW (2012). Covariate adjustment increased power in randomized controlled trials: an example in traumatic brain injury. J Clin Epidemiol, 65(5), 474–481. doi: 10.1016/j.jclinepi.2011.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, & Starzynski LL (2005). Trauma exposure, posttraumatic stress disorder and problem drinking in sexual assault survivors. J Stud Alcohol, 66(5), 610–619. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Relyea M, Peter-Hagene L, & Vasquez AL (2013). Trauma histories, substance use coping, PTSD, and problem substance use among sexual assault victims. Addictive Behaviors, 38(6), 2219–2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vik PW, Islam-Zwart KA, & Ruge LN (2008). Application of the PTSD-alcohol expectancy questionnaire (P-AEQ) to sexually assaulted college women. Addict Res Theory, 16(6), 585–594. doi: 10.1080/16066350701867273 [DOI] [Google Scholar]
- Waldrop AE, Back SE, Verduin ML, & Brady KT (2007). Triggers for cocaine and alcohol use in the presence and absence of posttraumatic stress disorder. Addictive Behaviors, 32(3), 634–639. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Keane T, Palmieri P, Marx B, & Schnurr P (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Weiss DS (2007). The impact of event scale: revised Cross-cultural assessment of psychological trauma and PTSD (pp. 219–238): Springer. [Google Scholar]
- Xian H, Chantarujikapong SI, Shrerrer JF, Eisen SA, Lyons MJ, Goldberg J, … True W (2000). Genetic and environmental influences on posttraumatic stress disorder, alcohol, and drug dependence in twin pairs. Drug and Alcohol Dependence, 61(1), 95–102. [DOI] [PubMed] [Google Scholar]