Abstract
Objectives
No prior study has evaluated the prevalence or variability of alcohol withdrawal syndrome (AWS) in general hospitals in the United States (US).
Methods
This retrospective study used secondary data from the Veterans Health Administration (VHA) to estimate the documented prevalence of clinically-recognized AWS among patients engaged in VHA care who were hospitalized during fiscal year 2013. We describe variation in documented inpatient AWS by geographic region, hospital, admitting specialty, and inpatient diagnoses using ICD-9-CM diagnosis and/or procedure codes recorded at hospital admission, transfer, or discharge.
Results
Among 469,082 eligible hospitalizations, the national prevalence of documented inpatient AWS was 5.8% (95% CI 5.2%–6.4%), but there was marked variation by geographic region (4.3%–11.2%), hospital (1.4%–16.1%), admitting specialty (0.7%–19.0%), and comorbid diagnoses (1.3%–38.3%). AWS affected a high proportion of Psychiatric admissions (19.0%, 95% CI 17.5%–20.4%) versus Medical (4.4%, 95% CI 4.0%–4.8%) or Surgical (0.7%, 95% CI 0.6%–0.8%); though by volume, Medical admissions represented the majority of hospitalizations complicated by AWS (n=13,478 Medical versus n=12,305 Psychiatric and n=595 Surgical). Clinically-recognized AWS was also common during hospitalizations involving other alcohol-related disorders (38.3%, 95% CI 35.8%–40.8%), other substance use conditions (19.3%, 95% CI 17.7%–20.9%), attempted suicide (15.3%, 95% CI 13.0%–17.6%), and liver injury (13.9%, 95% CI 12.6%–15.1%).
Conclusions
AWS was commonly recognized and documented during VHA hospitalizations in 2013 but varied considerably across inpatient settings. This clinical variation may in part reflect differences in quality of care and warrants further, more rigorous investigation.
Keywords: Alcohol withdrawal, epidemiology, prevalence, variation, addiction, hospital admission, diagnosis codes
Introduction
Inpatient alcohol withdrawal syndrome (AWS) is a ubiquitous problem in general hospitals linked to poor clinical outcomes. Hospitalized patients with AWS have longer intensive care unit (ICU) and hospital length-of-stay, more frequent hospital-acquired infections and surgical complications, increased risk of sepsis, and higher rates of in-hospital mortality than patients without AWS (Spies et al., 1996b; Spies et al., 1996a; O’Brien et al., 2007; de Wit et al., 2010). Despite significant morbidity and mortality associated with this condition, no prior study has evaluated the prevalence or variability of clinically-recognized AWS in general hospitals across the United States (US).
The purpose of this study was to describe the burden of documented inpatient AWS among patients engaged in care in the Veterans Health Administration (VHA), the largest integrated healthcare system in the US. We estimated the prevalence of clinically-recognized AWS among acute and ICU hospitalizations nationwide in 2013 using diagnostic and/or procedure codes, and described variation by geographic region, hospital, admitting specialty, and commonly occurring or alcohol-related inpatient diagnoses.
Methods
Study data
This retrospective cross-sectional study used a secondary national dataset of veterans engaged in VHA care during 2008 to 2013, as indicated by alcohol screening, required annually for VHA patients since 2004 (Bradley et al., 2006). International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes, dates of hospitalization, hospital facility, and admitting specialty (i.e. “bed section”) were obtained from the Veterans Affairs (VA) Corporate Data Warehouse. The study received approval and waivers of informed consent and HIPAA authorization from the VA Puget Sound Health Care System and University of Washington Institutional Review Boards.
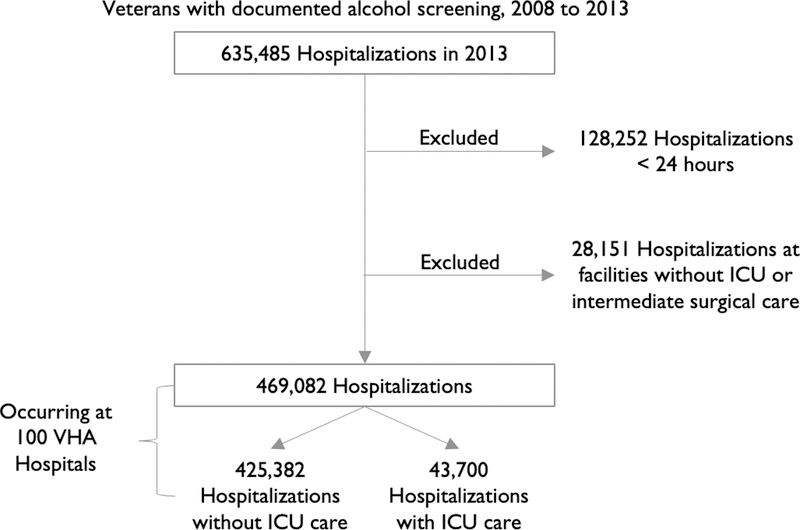
Study sample
The study included all VHA hospitalizations of at least 24-hour-duration at facilities with ICU and intermediate surgical care capabilities during fiscal year 2013 (October 1, 2012 to September 30, 2013). Recurrent hospitalizations by individual patients (approximately 35%) were included to capture the overall burden of AWS in VHA hospitals. Hospitalizations at facilities without ICU or intermediate surgical care were excluded because they are not representative of US general hospitals. Individual hospitalizations lacking acute and/or intensive care services within 10 days of admission were also excluded (e.g. residential or nursing home treatment).
Dependent variable – Inpatient AWS
Inpatient AWS was defined by primary or secondary ICD-9-CM diagnosis and/or procedure codes indicating recognition and/or treatment of AWS at hospital admission, transfer, or discharge (291.0, 291.3, 291.5, 291.8, 291.81, 94.62, 94.63, 94.68, 94.69) (Timko et al., 2014).
Covariates
Geographic regions were defined by collapsing Veterans Integrated Services Networks into 8 regions across the US. Each hospitalization was classified as Medical, Surgical, or Psychiatric based on the admitting “bed section” (eTable 1, Supplemental Digital Content showing admitting specialty categorization). Hospital “complexity” was determined using the VA Complexity Score (incorporating patient volume/risk, teaching activities, and research) (Rugs et al., 2013). Twenty-one comorbid conditions of interest (not mutually exclusive) were identified using ICD-9-CM codes to estimate prevalence of AWS among common and alcohol-related inpatient diagnoses.
Analyses
We estimated prevalence of documented AWS among VHA hospitalizations nationally and across geographic regions using fixed effects at the regional level and random effects at the hospital-level to account for intraclass correlations. Hospital-level calculations incorporated cluster-robust estimates of variance to account for correlated patient-level data. All analyses were performed using Stata, v14.0 (StataCorp LP, College Station, TX).
Results
Overall, 469,082 hospitalizations at 100 VHA hospitals throughout the US were eligible for this study (Figure 1). These hospitalizations represented 307,984 unique patients: 70.3% with one hospitalization, 18.1% with two hospitalizations, and 11.6% with three or more hospitalizations. The national prevalence of documented inpatient AWS was 5.8% (95% CI 5.2%–6.4%), complicating 26,381 hospitalizations (Table 1) and involving 18,072 unique patients: 75.8% with one hospitalization, 14.2% with two hospitalizations, and 10.0% with three or more hospitalizations complicated by AWS. Prevalence of AWS was highest in New England (11.2%, 95% CI 6.9%–15.5%) and lowest in the Southwest (4.3%, 95% CI 2.8%–5.8%). The prevalence did not vary by facility complexity level (eFigure 1, Supplemental Digital Content demonstrating AWS prevalence by hospital, stratified by facility complexity level). By hospital, prevalence of AWS ranged from 1.4% (95% CI 1.0%–1.9%) to 16.1% (95% CI 13.3%–19.5%) and exceeded 10% at 12 hospitals distributed across 6 of 8 geographical regions. Among hospitalizations requiring ICU care, AWS prevalence was 3.3% (95% CI 2.8%–3.7%) but across hospitals, ranged from 0% to 21.2% (95% CI 14.9%–29.1%). Regional prevalence patterns of AWS among ICU hospitalizations were similar to all hospitalizations.
Figure 1. Flow diagram of Hospitalizations Meeting Inclusion Criteria in the Veterans Health Administration during Fiscal Year 2013.
VHA = Veterans Health Administration
Table 1.
Prevalence of Alcohol Withdrawal Syndrome Among Hospitalizations in the Veterans Health Administration during Fiscal Year 2013: Overall and by Subgroup
| Hospitalizations involving AWS, No. | AWS Prevalence % (95% CI) | |
|---|---|---|
| Overall | 26,381 | 5.8 (5.2–6.4) |
| Geographic Region | ||
| New England | 2,106 | 11.2 (6.9–15.5) |
| Middle Atlantic | 2,081 | 4.6 (3.3–5.8) |
| South Atlantic | 6,099 | 5.3 (4.1–6.4) |
| South | 5,470 | 6.2 (4.7–7.7) |
| Midwest | 5,648 | 6.1 (4.9–7.3) |
| West | 2,442 | 5.9 (4.4–7.4) |
| Northwest | 768 | 5.2 (2.4–8.1) |
| Southwest | 1,767 | 4.3 (2.8–5.8) |
| Facility Complexity Level | ||
| 1a—highest | 13,650 | 5.2 (4.4–5.9) |
| 1b—high | 4,741 | 5.6 (4.4–6.9) |
| 1c—mid-high | 5,191 | 6.8 (5.3–8.2) |
| 2—medium | 2,799 | 6.3 (4.6–7.9) |
| Intensive care | 1,383 | 3.3 (2.8–3.7) |
| Admitting specialty | ||
| Medical | 13,478 | 4.4 (4.0–4.8) |
| Psychiatric | 12,305 | 19.0 (17.5–20.4) |
| Surgical | 598 | 0.7 (0.6–0.8) |
| Diagnoses | ||
| Alcohol-related disorder | 25,039 | 38.3 (35.8–40.8) |
| Other substance use condition | 9,024 | 19.3 (17.7–20.9) |
| Suicide attempt | 204 | 15.3 (13.0–17.6) |
| Liver injury | 7,073 | 13.9 (12.6–15.1) |
| Seizure | 1,870 | 11.9 (10.7–13.1) |
| Mental health disorder | 17,363 | 11.6 (10.6–12.7) |
| Pancreaticobiliary disease | 1,655 | 8.6 (7.7–9.5) |
| Nutrition, electrolyte, or acid-base disorder | 7,949 | 6.5 (5.9–7.2) |
| Gastrointestinal tract disorder | 7,776 | 5.1 (4.6–5.6) |
| Musculoskeletal or soft tissue disorder | 8,339 | 4.8 (4.3–5.3) |
| Trauma | 2,134 | 4.8 (4.3–5.3) |
| Chronic obstructive pulmonary disease | 4,357 | 4.6 (4.1–5.1) |
| Cardiac dysrhythmia | 2,653 | 2.8 (2.5–3.1) |
| Sepsis/shock | 919 | 2.8 (2.5–3.1) |
| Pneumonia | 887 | 2.4 (2.1–2.7) |
| Diabetes mellitus | 3,278 | 2.2 (2.0–2.5) |
| Kidney injury | 2,166 | 1.8 (1.6–2.0) |
| Cerebrovascular disease | 527 | 1.8 (1.6–2.1) |
| Myocardial infarction | 386 | 1.7 (1.5–2.0) |
| Malignancy | 830 | 1.4 (1.2–1.6) |
| Congestive heart failure | 917 | 1.3 (1.1–1.5) |
AWS = Alcohol Withdrawal Syndrome, VHA = Veterans Health Administration
Prevalence estimates are adjusted for intraclass correlations using fixed effects at the regional network-level and random effects at the hospital-level
Inpatient AWS was most prevalent among Psychiatric admissions (19.0%, 95% CI 17.5%–20.4%), followed by Medical admissions (4.4%, 95% CI 4.0%–4.8%) and Surgical admissions (0.7%, 95% CI 0.6%–0.8%). By volume, however, Medical admissions accounted for the greatest number of hospitalizations complicated by AWS (n=13,478 Medical versus n=12,305 Psychiatric and n=598 Surgical). Across VHA hospitals, the documented prevalence of AWS varied substantially among Psychiatric admissions (1.2%–51.8%) and Medical admissions (1.2%–16.3%) but was consistently uncommon among Surgical admissions (0–4.3%) (eFigure 2, Supplemental Digital Content demonstrating AWS prevalence by hospital, stratified by admitting specialty).
Evaluating comorbid inpatient diagnoses, prevalence of AWS was highest in the setting of other alcohol-related disorders (38.3%, 95% CI 35.8%–40.8%), followed by other substance use conditions (19.3%, 95% CI 17.7%–20.9%), attempted suicide (15.3%, 95% CI 13.0%–17.6%), and liver injury (13.9%, 95% CI 12.6%–15.1%). AWS was least prevalent during hospitalizations also complicated by congestive heart failure (1.3%, 95% CI 1.1%–1.5%) and malignancy (1.4%, 95% CI 1.2%–1.6%).
Discussion
This study describes the prevalence of inpatient AWS documented by clinicians during VHA hospitalizations in 2013 using a national cohort of patients engaged in VHA care. AWS was documented during 1 in 17 hospitalizations – more often than myocardial infarction that same year (eTable 2, Supplemental Digital Content showing characteristics of VHA hospitalizations in 2013). However, the overall prevalence at 5.8% masks the wide variation in documented AWS identified across geographic regions (4.3%–11.2%), hospitals (1.4%–16.1%), admitting specialties (0.7%–19.0%), and comorbid inpatient diagnoses (1.3%–38.3%).
Four prior studies have estimated the prevalence of inpatient AWS using single-center samples (Foy and Kay, 1995; Marik and Mohedin, 1996; Spies et al., 1996b; Spies et al., 1996c; Maldonado et al., 2014); the only study conducted in a general hospital setting (in Australia) reported 8% prevalence of AWS (Foy and Kay, 1995). Our results are generally consistent with these prior reports, but we estimated clinically-recognized and documented prevalence of AWS in a sample drawn from 100 hospitals throughout the US, which allowed for assessment of variation across inpatient settings.
This study found marked variation in the documented prevalence of inpatient AWS. On one extreme, the observed variation could only reflect differences in diagnostic coding practices (across providers, admitting services, hospitals, and regions). More likely, the results of this study also represent variation in true disease prevalence and clinical practices that warrant further investigation using more rigorous methods. Prior studies indicate there are regional differences in alcohol consumption and AUD (Karlamangla et al., 2006), thus true incidence of inpatient AWS may vary by geographic region. Variable documentation of AWS could also reflect differences in clinical recognition, prophylaxis, and/or hospital admitting rules, which may meaningfully impact patient outcomes. Although inpatient AWS is often considered a secondary complication of “primary” medical/surgical issues prompting hospitalization (Maldonado et al., 2014), for health systems like the VHA, reliable recognition of AWS among inpatients could improve management of AWS and trigger systematic engagement in addiction treatment after discharge (Timko et al., 2014).
Limitations
The true disease prevalence of inpatient AWS in this study remains unknown. Clinical documentation is an imperfect representation of disease – particularly diagnostic codes designed for billing rather than patient care, which introduce variation due to heterogenous coding practices. Unfortunately, no viable alternative methods for identifying cases of AWS in large administrative datasets currently exist – there are no validated biomarkers or operational definitions for AWS among inpatients.
Diagnostic codes likely underestimate the true prevalence of inpatient AWS for a number of reasons. Patients who receive AWS prophylaxis may not manifest signs/symptoms of AWS. AWS that occurs amidst competing physiologic abnormalities (e.g. due to sepsis, blood loss during surgery, or sedation used for mechanical ventilation) may go unrecognized by clinicians. Even when recognized, under-coding of AWS may result from accidental omission, particularly during hospitalizations involving multiple competing diagnoses that require documentation. Finally, clinicians may hesitate to document diagnoses like AWS that result in stigmatization. To increase sensitivity, we identified ICD-9-CM codes for AWS at multiple points during the course of hospitalizations (at admission, transfer, and discharge), but for the reasons above, our results likely represent conservative estimates of inpatient AWS prevalence.
The results of this study, drawn from VHA data collected in 2013, may not reflect current inpatient AWS prevalence due to changes in the veteran population (e.g. more women). Moreover, ICD-9-CM codes have been superseded by ICD-10, which limits generalizability of our results to current diagnostic coding practices. While significant attention is devoted to AWS in patients undergoing emergency surgery (Spies et al., 1996a; Spies et al., 1996b; de Wit et al., 2010), the majority of surgeries at VHA hospitals are elective (Kessler et al., 2011). Our results do not generalize to non-veteran inpatient populations given the relatively older, predominantly male population served by the VHA. Acknowledging these limitations, large secondary clinical datasets like the one used in this study are an important source of information, particularly regarding clinical variation that may impact quality of care (Mulley, 2009). As the largest integrated healthcare system in the US, the VHA is a particularly rich source of data, with over 100 facilities of varying complexity representing all regions of the country and providers from diverse training backgrounds.
Conclusions
In the VHA, AWS was common during hospitalizations in 2013 but variably documented across inpatient settings. Given known associations between AWS, poor clinical outcomes, and increased healthcare costs (Spies et al., 1996b; Spies et al., 1996a; O’Brien et al., 2007; de Wit et al., 2010; Clark et al., 2013), these findings signal a need for greater understanding of factors that contribute to variation in clinical-recognition and documentation of AWS, and the impact on quality of care.
Supplementary Material
Acknowledgments
Funding:
VA Puget Sound Health Care System Research & Development Associate Chief of Staff (ACOS) Pilot Grant Program, the Center of Excellence for Substance Abuse Treatment & Education (CESATE), and K24AA022128
Footnotes
Conflicts of Interest:
None
Contributor Information
Tessa L Steel, University of Washington, Division of Pulmonary, Critical Care, & Sleep Medicine, Seattle-Denver Center of Innovation (COIN), VA Puget Sound Health Care System, Seattle Division, 1660 South Columbian Way S-152, Seattle, WA 98108.
Carol A Malte, Center of Excellence in Substance Addiction Treatment and Education, VA Puget Sound Health Care System, Seattle Division, 1660 South Columbian Way S-152, Seattle, WA 98108.
Katharine A Bradley, Kaiser Permanente Washington Health Research Institute, 1730 Minor Ave, Suite 1600, Seattle, WA 98101.
Sharukh Lokhandwala, University of Washington, Division of Pulmonary, Critical Care, & Sleep Medicine, Harborview Medical Center, 325 9th Ave, Campus Box 359762, Seattle, WA 98104.
Catherine L Hough, University of Washington, Division of Pulmonary, Critical Care, & Sleep Medicine, Harborview Medical Center, 325 9th Ave, Campus Box 359762, Seattle, WA 98104.
Eric J Hawkins, Center of Excellence in Substance Addiction Treatment and Education, Seattle-Denver Center of Innovation (COIN), University of Washington, Department of Psychiatry and Behavioral Sciences, VA Puget Sound Health Care System, Seattle Division, 1660 South Columbian Way S-152, Seattle, WA 98108.
REFERENCES
- Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am J Managed Care. 2006;12(10):597–606. [PubMed] [Google Scholar]
- Clark BJ, Keniston A, Douglas IS, et al. Healthcare Utilization in Medical Intensive Care Unit Survivors with Alcohol Withdrawal. Alcohol Clin Exp Res. 2013;37(9):1536–1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit M, Jones DG, Sessler CN, Zilberberg MD, Weaver MF. Alcohol-use disorders in the critically ill patient. Chest. 2010;138(4):994–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foy A, Kay J. The incidence of alcohol-related problems and the risk of alcohol withdrawal in a general hospital population. Drug Alcohol Rev. 1995;14(1):49–54. [DOI] [PubMed] [Google Scholar]
- Karlamangla AS, Zhou K, Reuben DB, Greendale GA, Moore AA. Longitudinal trajectories of heavy drinking in adults in the United States of America. Addiction. 2006;101:91–99. [DOI] [PubMed] [Google Scholar]
- Kessler CS, Bhandarkar S, Casey P, Tenner A. Predicting patient patterns in veterans administration emergency departments. West J Emerg Medicine. 2011;12(2):204–207. [PMC free article] [PubMed] [Google Scholar]
- Maldonado JR, Sher Y, Ashouri JF, et al. The “Prediction of Alcohol Withdrawal Severity Scale” (PAWSS): systematic literature review and pilot study of a new scale for the prediction of complicated alcohol withdrawal syndrome. Alcohol. 2014;48(4):375–390. [DOI] [PubMed] [Google Scholar]
- Marik P, Mohedin B. Alcohol-related Admissions to an Inner City Hospital Intensive Care Unit. Alcohol Alcoholism. 1996;31(4):393–396. [DOI] [PubMed] [Google Scholar]
- Mulley AG. Inconvenient truths about supplier induced demand and unwarranted variation in medical practice. BMJ. 2009;339:b4073. [DOI] [PubMed] [Google Scholar]
- O’Brien JM, Lu B, Ali NA, et al. Alcohol dependence is independently associated with sepsis, septic shock, and hospital mortality among adult intensive care unit patients. Crit Care Med. 2007;35(2):345–350. [DOI] [PubMed] [Google Scholar]
- Rugs D, Toyinbo P, Patel N, et al. Processes and Outcomes of the Veterans Health Administration Safe Patient Handling Program: Study Protocol. JMIR Res Protoc. 2013;2(2):e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spies C, Dubisz N, Neumann T, et al. Therapy of alcohol withdrawal syndrome in intensive care unit patients following trauma: results of a prospective, randomized trial. Crit Care Med. 1996a;24(3):414–422. [DOI] [PubMed] [Google Scholar]
- Spies C, Neuner B, Neumann T, et al. Intercurrent complications in chronic alcoholic men admitted to the intensive care unit following trauma. Intensive care medicine. 1996b;22(4):286–293. [DOI] [PubMed] [Google Scholar]
- Spies C, Nordmann A, Brummer G, et al. Intensive care unit stay is prolonged in chronic alcoholic men following tumor resection of the upper digestive tract. Acta Anaesth Scand. 1996c;40(6):649–656. [DOI] [PubMed] [Google Scholar]
- Timko C, Bonn-Miller MO, McKellar J, Ilgen M. Detoxification History and 2-Year Outcomes of Substance Use Disorder Treatment and Mutual-Help Group Participation. J Drug Issues. 2014;44(1):4–21. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.