Abstract
Objective
Sexual and gender minority (SGM) adolescents report elevated risk for psychopathology. Identifying as a racial/ethnic minority and sexual (SM) or gender minority (GM) may lead to greater stress/discrimination and psychopathology. We examined nonsuicidal self-injury, suicide ideation, and suicide attempts (i.e., self-injurious thoughts and behaviors; SITBs) and depressive symptoms across intersections of sexual orientation, gender, and race/ethnicity.
Method
A large (n = 2,948; 59% GM) sample of adolescents aged 14–18 were recruited online to complete a cross-sectional survey. SGM status, race/ethnicity, and their interactions were used to predict depressive symptoms and SITBs. Associations among race/ethnicity and GM-specific psychosocial factors were assessed.
Results
SM (B = 3.75) and GM (B = 8.81) participants reported higher depressive symptoms and SITB histories (odds ratios [ORs] from 1.92 to 2.43 and 2.87 to 5.44, respectively). Asian participants were less likely to report nonsuicidal self-injury (OR = 0.45) and Latinx participants were more likely to report suicide attempts (OR = 1.50). Although omnibus tests of interactions were largely insignificant, exploratory analyses revealed fewer depressive symptoms (B = −8.40) and SITBs (ORs from −0.95 to −2.05) among Black SM and, at times, Black GM participants. This protective effect may relate to lower self-reported expectations of rejection due to gender.
Conclusions
GM participants reported highest risk for depressive symptoms and SITBs. Contrary to hypotheses, multiple minority identification was not associated with greater psychopathology. Future research, assessing specific sexual and gender identities across diverse samples, is needed to highlight how race impacts psychopathology risk across these identities.
Keywords: sexual minority, gender minority, transgender, nonsuicidal self-injury, suicidal self-injury, adolescence
Sexual minority (SM) adolescents, including those who identify as lesbian, gay, bisexual, queer, or questioning and those who experience attraction to people of the same gender, tend to show elevated risk for psychopathology and self-injurious thoughts and behaviors (SITBs), including nonsuicidal self-injury, suicide ideation, and suicide attempts (Batejan, Jarvi, & Swenson, 2015; King et al., 2008; Marshal et al., 2011). Although there is less research on the topic, gender minority (GM) adolescents, or those who identify with a gender identity that is different from their gender assigned at birth, also show elevated levels of psychopathology and SITBs (Dickey, Reisner, & Juntunen, 2015; Grossman & D’Augelli, 2007; Walls, Kane, & Wisneski, 2010). Providing a framework to understand this elevated risk, the minority stress model (Brooks, 1981; Meyer, 2003) proposes that there are both distal (i.e., objective events, conditions; e.g., daily discrimination) and proximal (i.e., personal and subjective processes; e.g., expectations of rejection) stressors that together increase vulnerability to mental health problems. Indeed, experiences of proximal and distal minority stress (e.g., internalized stigma, concealment, negative societal reactions) are associated with higher levels of depressive symptoms, substance use, and suicide ideation in SM populations (Meyer, 1995; Meyer, 2003). More recent theoretical and empirical research also supports application of this model to GM populations (Breslow et al., 2015; Hendricks & Testa, 2012; Meyer, 2015; Timmins, Rimes, & Rahman, 2017). For example, gender-based discrimination and stigma are associated with higher rates of suicide attempts (Goldblum et al., 2012) and psychological distress among GM-identifying adults (Bockting, Miner, Swinburne Romaine, Hamilton, & Coleman, 2013) and expectations of rejection are associated with stress, anxiety, and situational avoidance (Rood et al., 2016).
Some theories of minority stress posit that belonging to multiple minority groups may lead to unique and more severe experiences of stress and discrimination (e.g., “double jeopardy”; Ferraro & Farmer, 1996). Following this theory, sexual and gender minority (SGM) adolescents who also identify with a racial/ethnic minority group may be expected to experience more psychosocial stressors (e.g., more bullying/discrimination, less familial support) and, consequently, greater experiences of psychopathology and SITBs. Indeed, studies among LGB Black and Latinx adolescents indicate that higher levels of racial- and sexuality-based discrimination, and conflict between sexual and racial minority identities, are related to poorer mental health outcomes (Khan, Ilcisin, & Saxton, 2017; Santos & VanDaalen, 2016; Thoma & Huebner, 2013; Velez, Moradi, & Deblaere, 2015; Szymanski & Meyer, 2008), with similar effects observed among LGB people of color more broadly (Velez, Polihronakis, Watson, & Cox Jr., 2019). Moreover, qualitative studies have shown that, at least among certain intersections of SM and racial/ethnic minority identification, SM-related stressors are compounded by racist discrimination (Bowleg, Huang, Brooks, Black, & Burkholder, 2003).
However, results from direct tests of this theory have been mixed. Several studies of multiple minority stress have demonstrated similar levels of psychological distress when comparing adults identifying as both SM White and SM racial/ethnic minority (Hayes, Chun-Kennedy, Edens, & Locke, 2011; Velez, Watson, Cox Jr., & Flores, 2017). Similar patterns have emerged among adolescents and young adults. In their review of studies comparing mental health outcomes among SM youth (i.e., adolescents and young adults) of color and White SM youth, Toomey, Huynh, Jones, Lee, and Revels-Macalinao (2017) found evidence for higher, lower, and equal rates of psychopathology.
Intersectionality, initially defined by Kimberlé Crenshaw (1989), may be well-suited to make sense of these conflicting findings. Born out of Black feminist and female activists and scholars of color (Moradi & Grzanka, 2017), theories of intersectionality highlight that people often belong to multiple social categories, and that considering these social categories in concert is necessary to understand personal experiences with power, privilege, and discrimination, and to understand the consequences of these experiences (Cole, 2009; Else-Quest & Hyde, 2016). Thus, unlike multiple minority stress, intersectionality would posit that risk for psychopathology and SITBs will vary across intersections of sexuality, gender, and racial/ethnicity. Providing support for this possibility, there is evidence that identifying as SM and Black or Asian is associated with lower likelihood of suicide ideation, planning, and self-harm (Bostwick et al., 2014), whereas identifying as Latinx (e.g., Bostwick et al., 2014; Garofalo, Wolf, Wissow, Woods, & Goodman, 1999) or American Native/Pacific Islander (Bostwick et al., 2014) is associated with greater symptoms of depression and/or past year suicidal behavior. These different patterns parallel research indicating that different racial/ethnic minority groups show differential risk for psychopathology (Brown, Meadows, & Elder, 2007; Cha et al., 2018; Chesin, Moster, & Jeglic, 2013; Van Vorhees et al., 2008).
In testing these types of questions, SM and GM adolescents are often discussed and studied together because sexuality and gender are principal components of identity, and because these adolescents often face similar negative societal stressors (Meyer, Dietrich, & Schwartz, 2008). However, there appear to be key differences in mental health across SM and GM groups. Compared to cisgender heterosexual and SM adolescents (i.e., those whose gender identity matches their gender assigned at birth), GM adolescents and adults may experience higher rates of SITBs and psychopathology compared to cisgender heterosexual and SM adolescents (i.e., Connolly, Zervos, Barone, Johnson, & Joseph, 2016; Eisenberg, Gower, Rider, McMorris, & Coleman, 2019; Grossman & D’Augelli, 2007; King et al., 2008; McKay, Berzofsky, Landwehr, Hsieh, & Smith, 2019; Toomey, Syvertsen, & Shramko, 2018; Walls et al., 2010). However, few studies have demonstrated these discrepancies among SM and GM adolescents within a study sample, with existing studies using relatively small samples including few participants identifying as GM (McKay et al., 2019; Walls et al., 2010) or using broad measurement of GM identity (i.e., “Do you consider yourself transgender, genderqueer, genderfluid, or unsure about your gender identity?”; Eisenberg et al., 2019), which may inadvertently exclude other GM identities (e.g., gender nonbinary). Moreover, very few studies have compared rates and severity of psychopathology among GM adolescents of color (Pinto, Melendez, & Spector, 2008; Ryan, Russell, Huebner, Diaz, & Sanchez, 2010; Santos & VanDaalen, 2016; Velez et al., 2015). Existing research on GM adolescents of color has been preliminary in nature, involving very small samples (Pinto et al., 2008), or examining risk among samples of SMs that also include a small number of GMs (Ryan et al., 2010; Santos & VanDaalen, 2016; Velez et al., 2015).
In light of potential differences across SM and GM adolescents, and differences across racial and ethnic minority groups, the present study had three aims. First, we sought to compare depression severity and SITB risk across cisgender heterosexual, SM, and GM groups and across racial groups. Second, we sought to examine depressive symptoms and engagement in SITBs among adolescents at intersections of SM, GM, and racial/ethnic identities. Third, given limited prior research examining race/ethnicity within the context of GM identity, the present study also explored whether race/ethnicity is related to expectations of rejection due to gender identity, feelings of congruence between one’s body and gender identity, personal acceptance of gender identity, and disclosure of gender identity to parents/guardians and friends. Because the literature to date is relatively sparse and conflicting, these aims were primarily exploratory in nature and we did not have specific hypotheses. However, if interactions among SGM and racial/ethnic identification result in higher levels of depressive symptoms and endorsement of SITBs, results would support the idea that multiple minority identification is associated with higher levels of risk. On the other hand, if these interactions are not significant, results may suggest that multiple minority stress is not related to risk.
Method
Participants
The present sample included 2,948 adolescents aged 14–18 (M = 15.88; SD = 1.17). Most participants reported that they were assigned female at birth (n = 2,438; 82.69%) and reported they identified as White (n = 1,960; 66.52%). Remaining participants identified as Black (n = 142; 4.86%), Latinx (n = 277; 9.25%), Asian (n = 118; 7.15%), and multiple racial groups (n = 451; 15.57%).
Participants were classified into three groups based on their gender and sexual identities: GM (n = 1,751; 59.40%), SM (n = 633; 21.47%), and cisgender heterosexual (n = 564; 19.13%). Participants were categorized as GM if they identified with any gender other than solely male or female, or if they selected male or female as their current gender identity but indicated a different gender assigned at birth (more details about GM assessment are provided below). Most GM participants reported that they were transmasculine or female to male (n = 914; 52.20%). Remaining participants identified as nonbinary (n = 655; 37.41%), male to female or transfeminine (n = 103; 5.88%), and questioning (n = 79; 4.51%). Participants were categorized as SM if they identified with any sexual orientation other than heterosexual. Most participants identified as bisexual (n = 682; 23.13%), with remaining participants identifying as heterosexual (n = 601; 20.39%), pansexual (n = 565; 19.17%), queer (n = 335; 11.36%), gay (n = 273; 9.26%), lesbian (n = 155; 5.26%), homosexual (n = 36; 1.22%), other (n = 292; 9.91%), and “I do not want to respond” (n = 9; 0.31%).
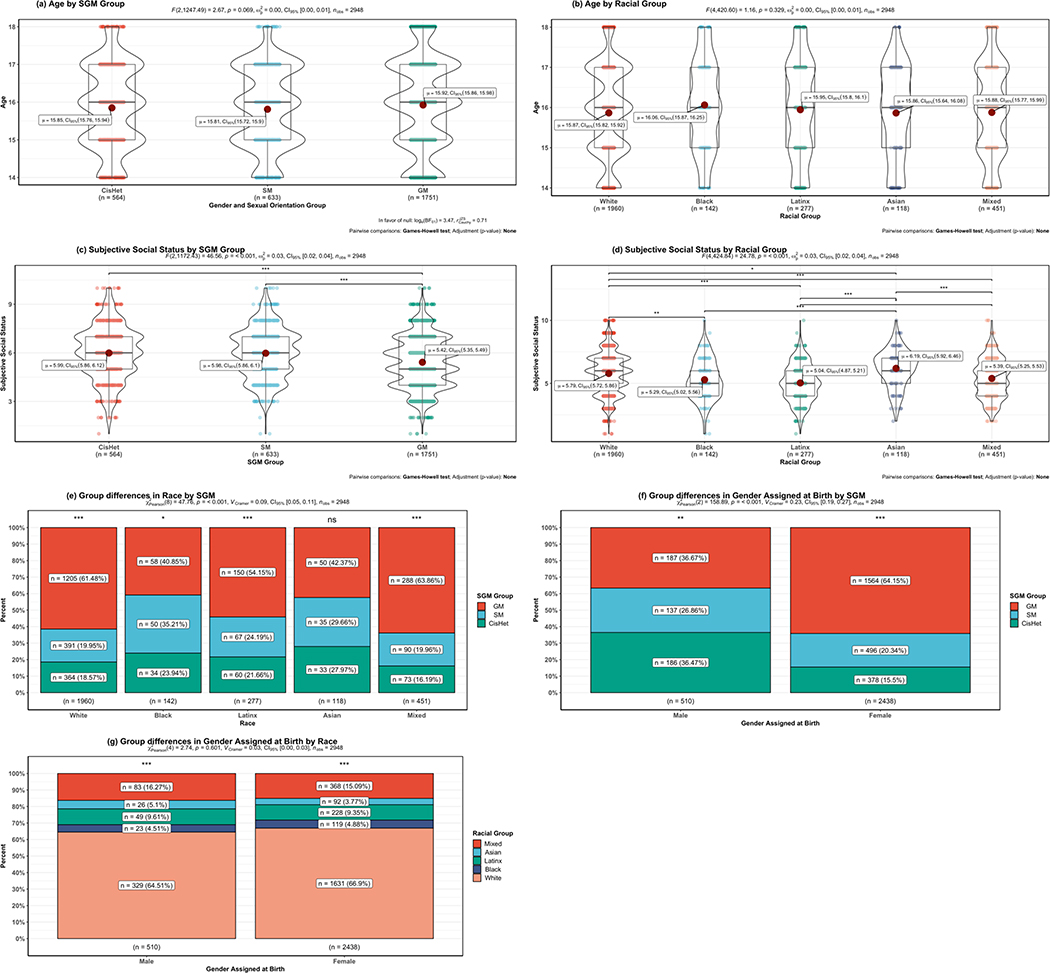
All included participants reported a sexual orientation and gender identity. The vast majority of GM participants (n = 1,700; 97.09%) also identified as SM. Separate GM-SM and GM heterosexual categories were combined into the single GM category because only 51 (2.91%) GM participants identified as heterosexual. More detailed demographic characteristics including differences across SGM and racial groups are listed in Figure 1.
Figure 1.
Demographic Differences Across Groups
Note: SGM = Sexual and Gender Minority. * p < .05; ** p <.01, *** p < .001. Only significant differences between groups are annotated
Procedure
Recruitment
Participants were recruited via paid advertisements on Facebook and Instagram for this cross-sectional study (see Appendix A). One set of advertisements targeted cisgender adolescents using the text, “Teenagers needed for online health study! Click now to participate in research!”; another targeted GM adolescents who listed interests related to transgender topics (e.g., “transgender,” “genderqueer”) using the text, “Are you transgender or genderqueer? Click now to participate in research!” Advertisements were targeted toward racial/ethnic minorities and included images of racially diverse youth to increase participant diversity.
Advertisements were served 377,469 times. After clicking on the advertisement, 8,747 interested participants were presented with study details; 5,642 adolescents assented to participate and began the study. Participants who endorsed SITBs during the study were provided with mental health resources and hotlines. Adolescents were screened out of the survey if they were outside the targeted age range (i.e., younger than 14 or older than 18 years of age; n = 39), and for not identifying as GM and male assigned at birth once we tried to increase those in this demographic (n = 1,958; see Thoma et al., 2019). Participant data was then excluded for evidence of duplicate participation via IP addresses (n = 320), and patterned and inappropriate responses to survey questions (n = 7).
For the current study we excluded participants identifying their race/ethnicity as American Indian (n = 41), other (n = 15), and those who did not indicate their race/ethnicity (n = 16), as the low number of participants across these intersections with SGM precluded meaningful analysis. We also excluded participants identifying as intersex (n = 11); we planned to include gender assigned at birth as a covariate in all analyses, and again, this low number precluded meaningful analysis. Finally, we excluded participants (n = 6) who did not respond to the item assessing subjective social status, as this was another planned covariate in subsequent analyses.
To maximize statistical power, we included all possible participants who completed a given measure. Thus, the sample size in the current study ranged from 1,968 to 2,339 for SITB engagement and depressive symptoms, respectively, and from 1,581 to 1,751 for GM only analyses. Compared to the full sample of 3,318 (including all those who qualified for the original study), participants included in each analysis were not significantly different in terms of race/ethnicity or SGM grouping. However, the final samples included in some analyses showed differences in gender assigned at birth, age, and/or subjective social status. These demographic characteristics are included as covariates in all multivariate analyses. Descriptions of and significant differences between the analyzed sample and the full sample are provided in the “notes” below corresponding figures.
Data collection
This study had a waiver of parental permission to protect participants’ privacy and safety; all study procedures were approved by the University’s Human Research Protection Office. Data were collected anonymously, and questionnaires were completed on a secure server using personal electronic devices. Participants who completed the survey were provided the opportunity to enter a drawing for a $50 electronic gift card.
Measures
Demographic information
Several demographic characteristics were assessed, including age, gender assigned at birth (male, female, intersex), and race/ethnicity (White, Black/African American, Hispanic/Latinx, Asian/Pacific Islander, American Indian/Alaska Native, Other). Participants could select one or more racial/ethnic identities; those who selected multiple racial groups were categorized as “multiracial.” Care was taken to assess sexual and gender identity thoroughly. Participants described their gender identity from the following categories: male, female, transgender, female to male (FTM), male to female (MTF), trans male/trans masculine, trans female/trans feminine, genderqueer, gender expansive, intersex, androgynous, nonbinary, two-spirited, third gender, agender, not sure, and/or other. Participants could select multiple labels. Participants were provided with the following labels to assess sexual orientation: heterosexual, gay, lesbian, bisexual, queer, homosexual, pansexual, other, and “I do not want to respond.”
Subjective social status
Socioeconomic status was assessed with the MacArthur Scale of Subjective Social Status-Youth Version (Goodman et al., 2001). The measure features a picture of a ladder, and participants were asked to indicate which step of the ladder represents their families’ position in society. This measure has been used in studies of adolescents to assess perceived socioeconomic status (Goodman et al., 2001), and meta-analytic evidence suggests that responses to this item are associated with mental, physical, and self-rated health (Zell, Strickhouser, & Krizan, 2018).
Depressive symptoms
Symptoms of depression were assessed with the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). The CES-D includes twenty items, answered on a 4-point Likert scale, assessing depressive symptoms experienced in the past week, including depressed mood, anhedonia, and hopelessness. Scores on the CES-D were summed across participants; total scores range from 0 to 60. Higher scores indicate more severe depressive symptoms. In studies of adolescents, this measure demonstrates strong internal consistency and reliability (Roberts, Andrews, Lewinsohn, & Hops, 1990). Moreover, this measure has achieved good concurrent validity in racially diverse adolescent samples (Prescott et al., 1998). In the present sample, the CES-D indexed excellent reliability (Cronbach’s alpha = .93).
Self-injurious thoughts and behaviors
Multiple measures were used to assess these behaviors. Lifetime history of suicidal thoughts and attempts were assessed with items from the Youth Risk Behavior Survey (Eaton et al., 2010), the National Longitudinal Study of Adolescent to Adult Health (Harris et al., 2009), and the Ask Suicide-Screening Questions (Horowitz et al., 2013). To assess suicide ideation history, participants were asked, “Have you ever seriously thought about killing yourself?” (0 = no history, 1 = history of suicide ideation). To assess suicide attempt history, participants were asked, “In your lifetime, how many times have you actually tried to kill yourself?” Participants’ continuous responses were dichotomized (0 = no history, 1 = history of one or more suicide attempts). Prior research indicates that these suicide ideation and behavior items have strong convergent and discriminant validity when used with adolescents (May & Klonsky, 2011). Nonsuicidal self-injury was assessed with the question: “In your lifetime, have you ever done anything to purposefully hurt yourself without wanting to die (for example, cutting your skin or burning yourself)?” (0 = no history, 1 = history of nonsuicidal self-injury).
GM-specific psychosocial factors
GM participants completed additional scales to assess five GM-specific psychosocial factors: expectations of rejection, appearance congruence, gender identity acceptance, disclosure of identity to parents/caregivers, and disclosure of identity to friends. Adapting scales assessing expectations of rejection among SM populations, participants were asked about their expectations of rejection due to their gender identities (Mohr & Kendra, 2011; Puckett, Maroney, Levitt, & Horne, 2016). Participants were asked to indicate, from (1) strongly disagree to (6) strongly agree: “I often wonder whether others judge me for my gender identity”; “I can’t feel comfortable knowing that others judge me negatively for my gender identity”; “I think a lot about how my gender identity affects the way people see me”; “I think other people will treat me badly because of my gender identity during the next year.” Paralleling other versions of these scales, items were summed (scores ranging from 4 to 24), with higher scores indicating greater expectations of rejection. In the present sample, this scale demonstrated good reliability (Cronbach’s alpha = .81).
Additionally, participants completed the Transgender Congruence Scale (Kozee, Tylka, & Bauerband, 2012), a 12-item scale assessing the degree to which people feel that their body and appearance match their gender identity (Appearance Congruence, 9 items; Cronbach’s alpha = .88 in the present sample) and their acceptance of their gender identity (Gender Identity Acceptance, 3 items; Cronbach’s alpha = .85 in the present sample). Both subscales are positively related to life satisfaction and negatively related to anxiety and depression (Kozee et al., 2012). Paralleling prior research, average item scores were used, with higher scores indicating greater perceived congruence between participants’ appearance and gender, and greater acceptance of one’s gender identity, on each subscale, respectively.
Finally, participants reported on disclosure of their gender identity to family and peers using the question, “Who knows about your gender identity? Check all that apply.” Options included: parents/primary caregivers, friends, brothers/sisters, other relatives, classmates, teachers, other, and “no one knows about my gender identity.” For the purposes of the present study, we examined disclosure to parents/primary caregivers and friends as two separate outcomes. We examined disclosure to only parents/guardians and friends as participants were most likely to report disclosure to these groups (i.e., 30.2% and 48.3% respectively) and because these represent two groups that are often close supports for adolescents.
Data Analyses
Participants were grouped based on their identified sexual identity, gender, and race/ethnicity. Demographic characteristics of the sample across SGM and racial groups are described in Figure 1. We examined group differences (i.e., SGM status, race/ethnicity) in demographics including age, subjective social status, and gender assigned at birth using One-Way Analysis of Variance (ANOVA) and Chi-Square tests of independence. Unadjusted post-hoc tests were conducted when significant differences were observed. Partial omega squared (ω2ps) and Cramer’s V (V) were used as effect sizes from ANOVAs and Chi-Squared tests, respectively. Although ω2ps is more conservative than partial eta squared, it tends to be less biased when comparing groups including relatively small sample sizes (Albers & Lakens, 2017).
We used multiple linear and multiple logistic regressions to examine the relationships among SGM status, race/ethnicity, and their interaction on depressive symptoms and lifetime histories of nonsuicidal self-injury, suicide ideation, and suicide attempts. For each dependent variable, two models were tested. In the first model, we entered race/ethnicity, SGM status, and relevant covariates (i.e., assigned gender at birth, age, subjective social status). Race and SGM status were dummy coded such that White race and cisgender heterosexual were the reference groups. To facilitate comparisons across SM and GM participants and across all racial groups, estimated marginal means and their 95% confidence intervals (CIs) were estimated, and Holm corrections were used for pairwise comparisons. When appropriate, odds ratios (OR) and their 95% CIs were estimated for significant effects to facilitate effect size interpretation. ORs are described in text, and unstandardized regression coefficients, t/z-values, and p-values are described within study figures.
In the second model, we added interaction terms across all SGM and race/ethnicity identities (see Hayes & Montoya, 2017); given the original dummy codes, White, cisgender heterosexual youth were the reference group for all interactions. We conducted a likelihood ratio test to examine whether interactions improved model fit. Given the relative lack of research examining risk across specific intersections of race/ethnic and SGM identities, we examined and reported simple effects regardless of whether the omnibus interaction improved model fit overall. Because we reported simple effects even in the absence of a significant overall interaction, results should be considered preliminary.
Finally, among GM participants, we examined whether race/ethnicity was significantly associated with GM-specific psychosocial factors using multiple linear and logistic regressions. We tested whether race/ethnicity was associated with disclosure of gender identity to parents and friends (logistic regressions), and with gender identity acceptance, appearance congruence, and expectations of rejection (linear regression). All models included relevant covariates. Analyses were conducted in R using the lmerTest (Bates, Mächler, Bolker, & Walker, 2015), ggplot2 (Wickham, 2011), and ggstatsplot (Patil & Powell, 2018) packages.
Results
Demographic Differences Across Groups
Significant differences in subjective social status, but not age, were observed across SGM and racial/ethnic groups (ω2ps = 0.03). The associations between SGM status and race/ethnicity (V = 0.09) and SGM status and gender assigned at birth (V = 0.23) were also significant. Results of these tests, and unadjusted post-hoc tests probing these effects, are provided in Figure 1.
Impact of Race/Ethnicity, SGM Status, and Their Interaction on Depressive Symptoms and SITBs
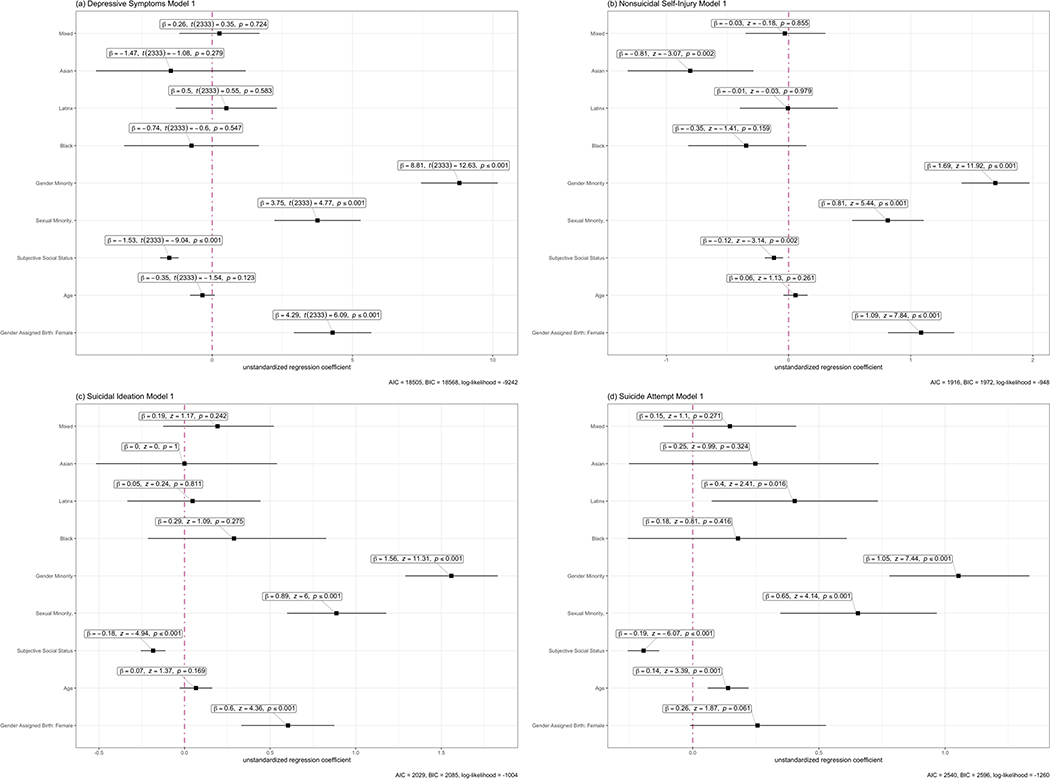
Depressive symptoms model 1
SM (B = 3.75; 95% CI = 2.21 – 5.30), and GM (B = 8.81; 95% CI = 7.44 – 10.18) participants reported, on average, approximately 3 to 9 more depressive symptoms than cisgender heterosexual participants (see Figure 2). Pairwise comparisons indicated that SM participants reported, on average, approximately 5 fewer depressive symptoms that GM participants (B = −5.06; see Supplemental Figure 1). No racial group emerged as significantly different from White (see Figure 2) or from any another racial group (see Supplemental Figure 2).
Figure 2.
Linear and Logistic Regression Models for Mental Health Outcomes
Note: Participants in the depression model included: White (312), Black (29), Latinx (54), Asian (24), Mixed (58); Sexual minority: White (336), Black (42), Latinx (56), Asian (31), Mixed (83); gender minority: White (908), Black (43), Latinx (107), Asian (34), Mixed (222). The 2,343 participants included in this analysis reported significantly higher Subjective social status than the full study sample. Across models of nonsuicidal self-injury, suicide ideation, and suicide attempts, respectively, analyses included: Cisgender heterosexual: White (242, 245, 246), Black (22, 22, 22), Latinx (40, 40, 40), Asian (22, 22, 22), Mixed (47, 47, 47); Sexual minority: White (290, 294, 294), Black (36, 36, 36), Latinx (47, 47, 47), Asian (26, 26, 26), Mixed (65, 65, 65); Gender minority: White (779, 783, 783), Black (39, 39, 39), Latinx (92, 92, 92), Asian (27, 28, 28), Mixed (186, 187, 186). Participants in SITB analyses were significantly more likely to be assigned female at birth, were significantly older, and reported significantly higher Subjective social status than the full study sample.
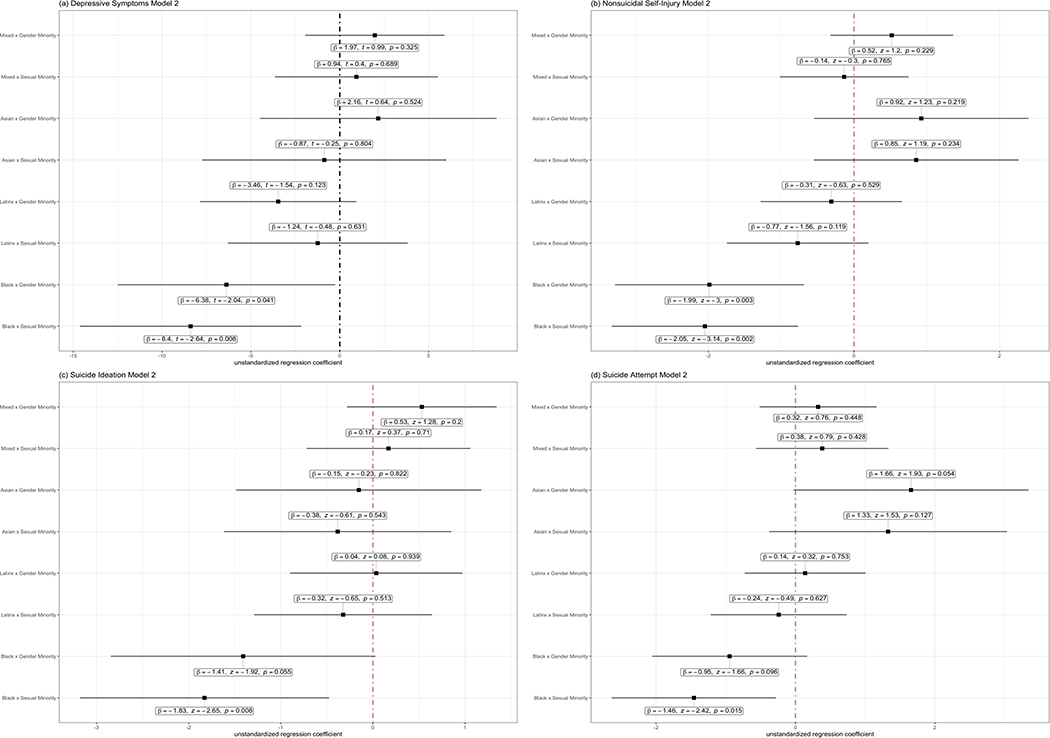
Depressive symptoms model 2
The interaction term between race/ethnicity and SGM statuses did not significantly improve the model (F(8, 2325) = 1.59, p = .12). However, compared to the reference group (i.e., White, cisgender participants), Black and GM (B = −6.38; 95% CI = −12.50 – −0.25) and Black and SM (B = −8.40; 95% CI = −14.63 – −2.16) participants reported, on average approximately 6 to 8 fewer depressive symptoms compared to White cisgender heterosexual participants (see Figure 3).
Figure 3.
Interaction Terms from Linear and Logistic Regression Models for Mental Health Outcomes
Note: Interactions are adjusted for gender assigned at birth, subjective social status, and age. Participants in the depression model included: White (312), Black (29), Latinx (54), Asian (24), Mixed (58); Sexual minority: White (336), Black (42), Latinx (56), Asian (31), Mixed (83); gender minority: White (908), Black (43), Latinx (107), Asian (34), Mixed (222). The 2,343 participants included in this analysis reported significantly higher Subjective social status than the full study sample. Across models of nonsuicidal self-injury, suicide ideation, and suicide attempts, respectively, analyses included: Cisgender heterosexual: White (242, 245, 246), Black (22, 22, 22), Latinx (40, 40, 40), Asian (22, 22, 22), Mixed (47, 47, 47); Sexual minority: White (290, 294, 294), Black (36, 36, 36), Latinx (47, 47, 47), Asian (26, 26, 26), Mixed (65, 65, 65); Gender minority: White (779, 783, 783), Black (39, 39, 39), Latinx (92, 92, 92), Asian (27, 28, 28), Mixed (186, 187, 186). Participants in SITB analyses were significantly more likely to be assigned female at birth, were significantly older, and reported significantly higher Subjective social status than the full study sample.
Nonsuicidal self-injury model 1
Compared to cisgender heterosexual participants, the odds of reporting nonsuicidal self-injury were approximately 2 to 5 times higher among SM (OR = 2.25; 95% CI = 1.68 – 3.02) and GM (OR = 5.44; 95% CI = 4.12 – 7.19) participants (see Figure 2). Pairwise comparisons demonstrated that the odds of reporting nonsuicidal self-injury were approximately 59% lower among SM compared to GM participants (OR = 0.41; see Supplemental Figure 1). Moreover, the odds of reporting nonsuicidal self-injury were approximately 44% lower among Asian compared to White participants (OR = 0.44; 95% CI = 0.27 – 0.75; see Figure 2). Otherwise, no racial category emerged as significantly different from any another (see Supplemental Figure 2).
Nonsuicidal self-injury model 2
The interaction term between race/ethnicity and SGM statuses significantly improved the model (χ2(8, 1937) = 20.82, p < .01). Compared to White cisgender heterosexual participants, the odds of Black GM (OR = 0.14; 95% CI = 0.04 – 0.49) and Black SM (OR = 0.12; 95% CI = 0.03 – 0.45) participants reporting nonsuicidal self-injury were significantly lower (see Figure 3).
Suicide ideation model 1
Compared to cisgender heterosexual participants, the odds of SM (OR = 2.43; 95% CI = 1.82 – 3.25) and GM participants (OR = 4.75; 95% CI = 3.63 – 6.23) reporting suicide ideation were 2 to 5 times higher (see Figure 2). Pairwise comparisons demonstrated that SM participants were 59% less likely than GM participants to report lifetime suicide ideation (OR = 0.41; see Supplemental Figure 1). No racial group emerged as significantly different from White (see Figure 2) or from any another racial group (see Supplemental Figure 2).
Suicide ideation model 2
The interaction term between race/ethnicity and SGM statuses did not significantly improve the model (χ2(8, 1950) = 10.91, p = .21). Compared to the reference group, Black SM participants were 84% less likely (OR = 0.16; 95% CI = 0.04 – 0.59) to report lifetime suicide ideation (see Figure 3).
Suicide attempt model 1
Compared to cisgender heterosexual participants, SM (OR = 1.92; 95% CI = 1.41 – 2.63) and GM (OR = 2.87; 95% CI = 2.18 – 3.80) participants were approximately 2–3 times more likely to report lifetime suicide attempts (see Figure 2). Pairwise comparisons demonstrated that SM participants were 33% less likely than GM participants to report lifetime suicide attempt(s) (OR = 0.67; see Supplemental Figure 1). The odds of Latinx participants reporting suicide attempts were 1.5 times higher than White participants (OR = 1.50; 95% CI = 1.08 – 2.08). No other racial group emerged as significantly different from White (see Figure 2) or from any another racial group (see Supplemental Figure 1).
Suicide attempt model 2
The interaction term between race/ethnicity and SGM statuses did not significantly improve the model (χ2(8, 1950) = 13.15, p = .11). Compared to White cisgender heterosexual participants, Black SM participants were approximately 77% less likely (OR = 0.23; 95% CI = 0.07 – 0.75) to report lifetime suicide attempts (see Figure 3).
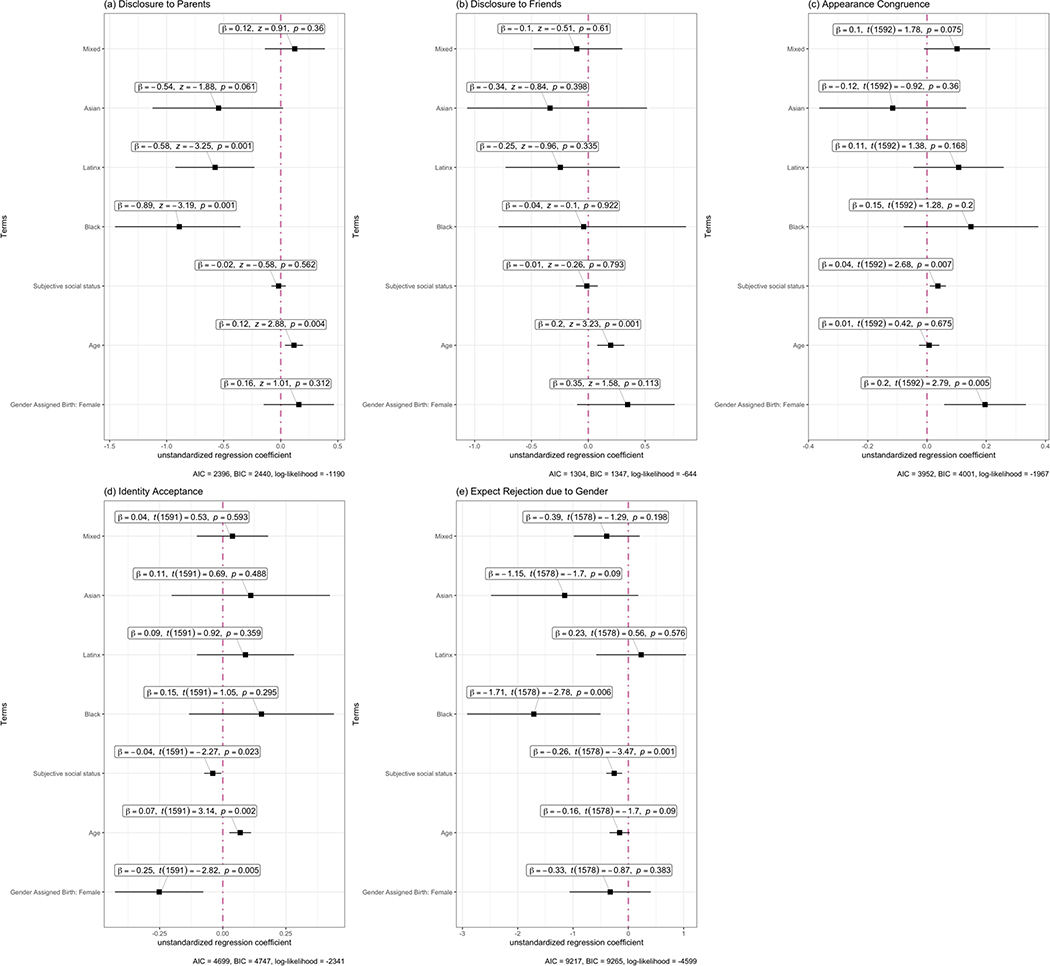
Impact of race/ethnicity on GM-specific psychosocial factors
Race/ethnicity was significantly associated with disclosure of gender identity to parents/guardians. Black (OR = 0.41; 95% CI = 0.23 – 0.70) and Latinx (OR = 0.56; 95% CI = 0.40 – 0.79) participants were approximately half as likely to have told their parents about their gender identities. Race/ethnicity was not significantly associated with disclosure of gender identity to friends. Black participants (B = −1.71; 95% CI = −2.92 – −0.50) reported lower expectations of rejection due to gender identity. Race/ethnicity was not significantly associated with either appearance congruence or identity congruence (see Figure 4).
Figure 4.
Linear and Logistic Regression Models for Gender Minority Psychosocial Stressors
Note: Disclosure to parents, Disclosure to friends, Transgender Congruence Scale Appearance/Identity Congruence, and Expectations of rejection models include: White (1299, 1301, 1098, 1098), Black (66, 66, 53, 53), Latinx (165, 165, 129, 129), Asian (60, 60, 43, 44), Mixed (300, 300, 263, 263).
Discussion
The present study examined the impact of sexual orientation, gender, and racial/ethnic identification on risk for depressive symptoms and SITBs in a large, diverse sample of adolescents. Building on prior research, we examined both sexual and gender identity across different racial groups to better understand how these unique minority identities may interact to confer risk for depressive symptoms and SITB engagement. Additionally, the present study was the first to our knowledge to examine whether race/ethnicity is associated with GM-specific psychosocial factors.
Main Effects of Sexuality, Gender, and Race/Ethnicity
SM and GM participants reported significantly more depressive symptoms and higher rates of all SITBs assessed compared to cisgender heterosexual participants. Post-hoc tests revealed that GMs reported the highest rates of all outcomes assessed. Effect sizes for this difference were moderate to large, with the odds of SITBs ranging from 41–67% higher among GM compared to SM identifying participants. Results parallel and extend preliminary research on this topic (e.g., Connolly et al., 2016; Eisenberg et al., 2019; Grossman & D’Augelli, 2007; King et al., 2008; McKay et al., 2019; Toomey et al., 2018; Walls et al., 2010) by including a large number of GM participants and by using a comprehensive assessment of gender identity. Results suggest that GM adolescents may show unique, and more severe patterns of psychopathology and SITBs, compared to SM and cisgender heterosexual adolescents.
To better understand this elevated risk, we conducted additional post-hoc analyses to examine whether SGM-status was related to differences in family support and bullying/discrimination (see Appendix B for a description of these measures). Results of these analyses indicated higher levels of bullying among GM participants and lower levels of family support among SM and GM participants, compared to cisgender heterosexual participants (see Supplemental Figure 3). Results suggest that SGM adolescents, and particularly GM-identifying adolescents, may experience more frequent and severe stressors across familial and social environments.
Differences in symptoms of depression and rates of SITBs across racial/ethnic groups were largely insignificant with two exceptions: White, compared to Asian, reported twice the odds nonsuicidal self-injury and Latinx compared to White participants reported 1.5 times the odds of having made a suicide attempt. Notably, however, this latter effect did not remain in post-hoc, Holm-corrected analysis when comparing estimated marginal means across each racial group. Lower odds of reporting nonsuicidal self-injury among Asian-identifying participants parallels some (e.g., Chesin et al., 2013), but not all (e.g., Emelianchik-Key, Byrd, & La Guardia, 2016) research on this topic. Additionally, significant differences were not observed among other ethnic groups that had been previously documented. For instance, some prior research reports higher levels of depressive symptoms among Latinx, Asian, and Black/African American youth (i.e., adolescents and young adults), compared to White youth (Brown et al., 2007; Van Voorhees et al., 2008), and lower rates of suicide ideation and attempts among Black adolescents compared to other adolescents (Cha et al., 2018). Future research including larger samples (e.g., thousands) of racial/ethnic minority youth may be necessary to better clarify these discrepancies.
Interaction of Sexuality, Gender, and Racial/Ethnic Identification
Findings from the present study did not support the theory that multiple minority identification confers the highest risk for psychopathology. Indeed, no multi-minority group showed higher risk for depressive symptoms, nonsuicidal self-injury, suicide ideation, or suicide attempts compared to White, cisgender, and heterosexual participants. Instead, preliminary results provided partial support for theories of intersectionality, showing varied risk for depressive symptoms and SITBs across intersections of race and SGM identification. Specifically, Black and GM and Black and SM participants reported between 6 and 8 fewer depressive symptoms and reported about 1/7th the odds of nonsuicidal self-injury. Black SM participants reported 1/5th the odds of engaging in suicidal thoughts or behaviors. Although we discuss these potentially provocative results in detail below, it is important to note that these results are inherently preliminary given that the interaction term only improved one model (i.e., the nonsuicidal self-injury model), and given the relatively small number of participants identifying as both Black and SM or GM, also reflected in the wide confidence intervals for observed effects.
These results parallel some prior research on this topic (e.g., Bostwick et al., 2014), indicating that Black SM adolescents may be at lower risk for some forms of psychopathology. Reasons for this protective effect remain largely unclear. That GM and Black participants reported lower levels of expectations of rejection due to their gender identity may be relevant to this lower observed risk. Several unexamined factors could help to explain these findings more fully. For example, there is some evidence that parents prepare racial/ethnic minority, and particularly Black youth (Hughes et al., 2006) to anticipate and to manage discrimination via specific coping strategies and cultural orientation (Neblett, Rivas-Drake, & Umaña-Taylor, 2012). Such parenting styles could provide enhanced coping skills, protecting against additional stigmatization among Black SGM youth when they begin to identify with SGM identities during adolescence.
A related possibility involves stress-related growth. Reframing stressful events as resulting in positive personal or life changes is associated with a wide-range of positive outcomes across both general (Helgeson, Reynolds, & Tomich, 2006) and minority-related stressors (e.g., Cox, Dewaele, Van Houtte, & Vincke, 2010; Wang, Rendina, & Pachankis, 2016). This body of research has been proposed to help explain why Black individuals in the United States might simultaneously experience more stress, but not higher rates of many forms of psychopathology and SITBs compared to their White peers (e.g., Meyer, 2010), and why Black or Latinx and SM people do not report more psychopathology than their White and SM peers (Meyer et al., 2008). Future research should consider testing whether minority-stress related growth or similar constructs (e.g., stress inoculation; Hatzenbuehler, 2009) could help explain the lower risk for psychopathology observed among GM and Black adolescents.
Race/Ethnicity and Transgender-Specific Psychosocial Stressors
Regarding racial differences across GM-specific psychosocial stressors, few effects were observed. This lack of racial/ethnic impact parallels evidence that race/ethnicity does not moderate attitudes toward transgender people in the United States (Norton & Herek, 2013). However, in contrast to these primarily null effects, two significant racial differences emerged. Black and Latinx participants were approximately half as likely to have disclosed their gender identities to their parents/guardians (odds ratios ranging from 0.41 to 0.56). Research directly assessing impacts of race/ethnicity on attitudes toward transgender and gender nonconformity both in and outside of family contexts may shed light on this observed effect. It is worth noting that gender identity disclosure may be both protective and a risk factor in different situations. In terms of positive outcomes, disclosing gender identity to parents/guardians may facilitate gender transition, which has been associated with adaptive mental health functioning (Olson, Durwood, DeMeules, & McLaughlin, 2016). On the other hand, negative parental/guardian reactions to disclosure of gender identity may cause stress and feelings of isolation and rejection. Gender identity disclosure may therefore confer additional risk in certain familial and cultural contexts. This possibility is supported by qualitative research in which Black and lesbian or bisexual women report numerous familial, cultural, and religious factors impacting their decisions for sexual identity disclosure (Bowleg, Burkholder, Teti, & Craig, 2008). More research examining these complex relationships is needed.
Additionally, Black and GM participants reported significantly lower expectations of rejection due to gender identity compared to White participants, with no other significant differences across racial identities emerging among GM participants. However, given lower rates of disclosing gender identity to parents/guardians among Black compared to White participants, Black GM adolescents may still face stigmatization within their own homes.
Limitations, Future Directions, and Conclusions
Findings should be interpreted in light of several limitations. First, 65% of participants were White. Although the sample was quite large and diverse compared to many studies of SGM adolescents, studies including larger samples of diverse youth may result in more reliable estimates of mental health risk across specific intersections of race and SGM identities. Second, 83% of the sample reported that they were assigned female at birth. This sample characteristic is particularly notable in light of intersectionality theories positing that race is a gendered construct (e.g., Thomas, Hacker, & Hoxha, 2011). As a result of this cultural bias, Black individuals may be considered and treated as more masculine, at least in the United States (e.g., Hall, Galinsky, & Phillips, 2015), leading to intersectional invisibility that particularly impacts Black women (Purdie-Vaughns & Eibach, 2008; Thomas, Dovidio, & West, 2014). Yet, for Black participants assigned female at birth, the transition to less feminine gender expression, via non-binary or transgender identification or by SM identification (in some cases), may have led to fewer experiences of gender-based discrimination. Additionally, some evidence indicates SM identification can dampen others’ perceptions of racial minority status (e.g., Petsko & Bodenhausen, 2019). Future research with a larger number of participants assigned male at birth may be better suited to test how intersections of gendered racial groups and SGM identification impact risk.
Third, the sample sizes at some intersections of SGM and race/ethnicity were small, and in the case of depressive symptoms, suicide ideation and suicide attempts, we probed non-significant omnibus interactions. Future studies replicating these results in larger samples are needed to determine the stability of these effects. Fourth, to maintain statistical power, numerous intersections were not assessed, including interactions within specific SM and GM identities, with gender assigned at birth, and with socioeconomic status. Key differences in mental health risk across these intersections may exist. For example, adolescents identifying as gender non-binary or bisexual may show differential risk compared to other GM and SM identities, respectively, when assessed in a sufficiently large sample to probe these intersections.
Fifth, all results were based on cross-sectional, self-report data. Sexual and gender identities can shift and change across development, and participants may have identified differently if assessed at a different time point. Future studies using longitudinal designs will be better suited to look at changes in SM and GM identification, and how such changes impact the limited outcomes assessed here (i.e., depressive symptoms and SITB engagement) alongside a wide range of other important mental and physical health outcomes. Finally, we primarily examined the impact of participant ethnic/racial identification on depressive symptoms and SITBs rather than participant experiences with racism, anti-GM bias, and heterosexism specifically.
The present study provided important insights into associations among sexual and gender minority identity, race/ethnicity, and intersections of both groups on risk for depressive symptoms and SITBs. Results suggest that GM adolescents show higher risk for these outcomes compared to both sexual minority and cisgender heterosexual adolescents. Results do not support the idea that multiple minority identification is universally associated with higher mental health risk, instead indicating that risk varies at different intersections of race/ethnicity and SGM status among adolescents.
Supplementary Material
Public Health Significance Statement.
This study suggests that adolescents identifying as a gender minority are at higher risk for psychopathology compared to those identifying as both sexual minorities and cisgender. Results do not support the idea that multiple minority identification is universally associated with higher mental health risk. Instead, results indicate that this risk varies across intersections of race/ethnicity and sexual and gender minority status. Results should be interpreted with caution in light of study limitations, including broad categorizations of sexual and gender identities.
Acknowledgements
this study was funded by the University of Pittsburgh Central Research Development Fund through an award to the second, third, and final authors. The final author was supported by NIMH grant T32 MH018951.
Appendix A
The data reported in this manuscript were collected as part of a larger data collection. Findings from the larger data collection have been reported in two separate manuscripts. MS 1 (Salk et al., under review) focuses on the feasibility of and sample characteristics obtained from online recruitment targeting sexual and gender minority adolescents. MS 2 (Thoma et al., 2019) presents on disparities in suicide-related outcomes among youth identifying with specific gender minority statuses (trans-female, trans-male, gender-nonbinary across sexes assigned at birth). In contrast, the present manuscript specifically examines risk for depression and self-injurious thoughts and behaviors across sexual and gender minority orientations and risk across intersections of sexual and gender minority orientations and race/ethnicity.
Appendix B
Psychosocial Factors
To assess family support, participants indicated the degree to which they felt supported by their family using a 4-item, Likert-type (i.e., 1 [strongly disagree] to 5 [strongly agree]) scale. Items included: “Most of the time, my parent(s) are warm and loving toward me;” “Overall, I am satisfied with my relationship with my parent(s);” “When I do something wrong that is important, my parent(s) talk about it with me and help me to understand why it is wrong;” and “I am satisfied with the way my parent(s) and I communicate with each other.” Items were summed, with higher scores indicating higher family support. In the present sample, this scale demonstrated excellent reliability (Cronbach’s alpha = 0.90).
Regarding bullying, participants answered four questions assessing how often they felt they had been teased or bullied in the past month, using a scale from (1) never to (4) many times. Specifically, participants were asked: “In the past six months, how often have you been teased or bullied?;” “In the past six months, how often have you been hit or beaten up?;” “In the past six months, how often have you been treated rudely or unfairly?;” and “In the past six months, how often has someone called you bad names?” Items were averaged to produce a single bullying score, with higher scores indicating higher levels of bullying. In the present sample, this scale demonstrated acceptable reliability (Cronbach’s alpha = 0.78).
References
- Batejan KL, Jarvi SM, & Swenson LP (2015). Sexual orientation and non-suicidal self-injury: A meta-analytic review. Archives of Suicide Research, 19(2), 131–150. doi: 10.1080/13811118.2014.957450 [DOI] [PubMed] [Google Scholar]
- Bates D, Mächler M, Bolker B, & Walker S (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1). doi: 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, & Coleman E (2013). Stigma, mental health, and resilience in an online sample of the US transgender population. American Journal of Public Health, 103(5), 943–951. doi: 10.2105/AJPH.2013.301241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick WB, Meyer I, Aranda F, Russell S, Hughes T, Birkett M, & Mustanski B (2014). Mental health and suicidality among racially/ethnically diverse sexual minority youths. American Journal of Public Health, 104(6), 1129–1136. doi: 10.2105/AJPH.2013.301749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L, Huang J, Brooks K, Black A, & Burkholder G (2003). Triple jeopardy and beyond: Multiple minority stress and resilience among Black lesbians. Journal of Lesbian Studies, 7, 87–108. doi: 10.1300/J155v07n04_06 [DOI] [PubMed] [Google Scholar]
- Bowleg L, Burkholder G, Teti M, & Craig ML (2008). The complexities of outness: Psychosocial predictors of coming out to others among Black lesbian and bisexual women. Journal of LGBT Health Research, 4(4), 153–166. doi: 10.1080/15574090903167422 [DOI] [PubMed] [Google Scholar]
- Breslow AS, Brewster ME, Velez BL, Wong S, Geiger E, & Soderstrom B (2015). Resilience and collective action: Exploring buffers against minority stress for transgender individuals. Psychology of Sexual Orientation and Gender Diversity, 2(3), 253–265. doi: 10.1037/sgd0000117 [DOI] [Google Scholar]
- Brooks VR (1981). Minority stress and lesbian women. Lexington, MA: Lexington Books. [Google Scholar]
- Brown JS, Meadows SO, & Elder GH (2007). Race-ethnic inequality and psychological distress: Depressive symptoms from adolescence to young adulthood. Developmental Psychology, 43(6), 1295–1311. doi: 10.1037/0012-1649.43.6.1295 [DOI] [PubMed] [Google Scholar]
- Cha CB, Franz PJ, M Guzmán E, Glenn CR, Kleiman EM, & Nock MK (2018). Annual Research Review: Suicide among youth - epidemiology, (potential) etiology, and treatment. Journal of Child Psychology and Psychiatry, 59(4), 460–482. doi: 10.1111/jcpp.12831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesin MS, Moster AN, & Jeglic EL (2013). Non-suicidal self-injury among ethnically and racially diverse emerging adults: Do factors unique to the minority experience matter? Current Psychology, 32(4), 318–328. doi: 10.1007/s12144-013-9185-2 [DOI] [Google Scholar]
- Cole ER (2009). Intersectionality and research in psychology. American Psychologist, 64(3), 170–180. doi: 10.1037/a0014564 [DOI] [PubMed] [Google Scholar]
- Connolly MD, Zervos MJ, Barone CJ II, Johnson CC, & Joseph CLM (2016). The mental health of transgender youth: Advances in understanding. Journal of Adolescent Health, 59(5), 489–495. doi: 10.1016/j.jadohealth.2016.06.012 [DOI] [PubMed] [Google Scholar]
- Cox N, Dewaele A, Van Houtte M, & Vincke J (2010). Stress-related growth, coming out, and internalized homonegativity in lesbian, gay, and bisexual youth. An examination of stress-related growth within the minority stress model. Journal of Homosexuality, 58(1), 117–137. doi: 10.1037/sgd0000117 [DOI] [PubMed] [Google Scholar]
- Dickey LM, Reisner SL, & Juntunen CL (2015). Non-suicidal self-injury in a large online sample of transgender adults. Professional Psychology: Research and Practice, 46(1), 3–11. doi: 10.1037/a0038803 [DOI] [Google Scholar]
- Eaton KD, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, … Wechsler H (2010). Youth risk behavior surveillance — United States, 2009. Center for Disease Controls and Prevention, 59(SS05), 1–142. [PubMed] [Google Scholar]
- Eisenberg ME, Gower AL, Rider GN, McMorris BJ, & Coleman E (2019). At the intersection of sexual orientation and gender identity: Variations in emotional distress and bullying experience in a large population-based sample of U.S. adolescents. Journal of LGBT Youth, 16(3), 235–254. doi: 10.1080/19361653.2019.1567435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Else-Quest NM, & Hyde JS (2016). Intersectionality in quantitative psychological research: I. Theoretical and epistemological issues. Psychology of Women Quarterly, 40(2), 155–170. doi: 10.1177/0361684316629797 [DOI] [Google Scholar]
- Emelianchik-Key K, Byrd RJ, & La Guardia AC (2016). Adolescent non-suicidal self-injury: Analysis of the youth risk behavior survey. The Professional Counselor, 6(1), 61–75. doi: 10.15241/kk.6.1.61 [DOI] [Google Scholar]
- Ferraro KF, & Farmer MM (1996). Double jeopardy to health hypothesis for African Americans: Analysis and critique. Journal of Health and Social Behavior, 37(1), 27–43. doi: 10.2307/2137229 [DOI] [PubMed] [Google Scholar]
- Garofalo R, Wolf RC, Wissow LS, Woods ER, & Goodman E (1999). Sexual orientation and risk of suicide attempts among a representative sample of youth. Archives of Pediatrics and Adolescent Medicine, 153(5), 487–493. doi: 10.1001/archpedi.153.5.487 [DOI] [PubMed] [Google Scholar]
- Goldblum P, Testa RJ, Pflum S, Hendricks ML, Bradford J, & Bongar B (2012). The relationship between gender-based victimization and suicide attempts in transgender people. Professional Psychology: Research and Practice, 43(5), 468–474. doi: 10.1037/a0029605 [DOI] [Google Scholar]
- Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P, and Udry JR 2009. The National Longitudinal Study of Adolescent to Adult Health: Research Design [WWW document]. URL: http://www.cpc.unc.edu/projects/addhealth/design.
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135(5), 707–730. doi: 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA, & Tomich PL (2006). A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology, 74(5), 797–816. doi: 10.1037/0022-006X.74.5.797 [DOI] [PubMed] [Google Scholar]
- Hendricks ML, & Testa RJ (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients: An adaptation of the Minority Stress Model. Professional Psychology: Research and Practice, 43(5), 460–467. doi: 10.1037/a0029597 [DOI] [Google Scholar]
- Khan M, Ilcisin M, & Saxton K (2017). Multifactorial discrimination as a fundamental cause of mental health inequities. International Journal for Equity in Health, 16(1), 43. doi: 10.1186/s12939-017-0532-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, & Nazareth I (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8(1), 70. doi: 10.1186/1471-244X-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozee HB, Tylka TL, & Bauerband LA (2012). Measuring transgender individuals’ comfort with gender identity and appearance: Development and validation of the transgender congruence scale. Psychology of Women Quarterly, 36(2), 179–196. doi: 10.1177/0361684312442161 [DOI] [Google Scholar]
- Lenth RV (2016). Least-squares means: The R package lsmeans. Journal of Statistical Software, 69(1). doi: 10.18637/jss.v069.i01 [DOI] [Google Scholar]
- Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J,… Brent DA (2011). Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review. The Journal of Adolescent Health, 49(2), 115–123. doi: 10.1016/j.jadohealth.2011.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- May A, & Klonsky ED (2011). Validity of suicidality items from the youth risk behavior survey in a high school sample. Assessment, 18(3), 379–381. doi: 10.1177/1073191110374285 [DOI] [PubMed] [Google Scholar]
- McKay T, Berzofsky M, Landwehr J, Hsieh P, & Smith A (2019). Suicide etiology in youth: Differences and similarities by sexual and gender minority status. Children and Youth Services Review, 102, 79–90. doi: 10.1016/j.childyouth.2019.03.039 [DOI] [Google Scholar]
- Meyer IH (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36(1), 38–56. doi: 10.2307/2137286 [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. doi: 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Dietrich J, & Schwartz S (2008). Lifetime prevalence of mental disorders and suicide attempts in diverse lesbian, gay, and bisexual populations. American Journal of Public Health, 98(6), 1004–1006. doi: 10.2105/AJPH.2006.096826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2010). Identity, stress, and resilience in lesbians, gay men, and bisexuals of color. The Counseling Psychologist, 38(3), 442–454. doi: 10.1177/0011000009351601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2015). Resilience in the study of minority stress and health of sexual and gender minorities. Psychology of Sexual Orientation and Gender Diversity, 2(3), 209–213. doi: 10.1037/sgd0000132 [DOI] [Google Scholar]
- Mohr JJ, & Kendra MS (2011). Revision and extension of a multidimensional measure of sexual minority identity: The lesbian, gay, and bisexual identity scale. Journal of Counseling Psychology, 58(2), 234–245. doi: 10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- Moradi B, & Grzanka PR (2017). Using intersectionality responsibly: Toward critical epistemology, structural analysis, and social justice activism. Journal of Counseling Psychology, 64(5), 500–513. doi: 10.1037/cou0000203 [DOI] [PubMed] [Google Scholar]
- Neblett EW Jr., Rivas-Drake D, & Umaña-Taylor AJ (2012). The promise of racial and ethnic protective factors in promoting ethnic minority youth development. Child Development Perspectives, 6(3), 295–303. doi: 10.1111/j.1750-8606.2012.00239.x [DOI] [Google Scholar]
- Norton AT, & Herek GM (2013). Heterosexuals’ attitudes toward transgender people: Findings from a national probability sample of US adults. Sex Roles, 68(11–12), 738–753. doi: 10.1007/s11199-011-0110-6 [DOI] [Google Scholar]
- Olson KR, Durwood L, DeMeules M, & McLaughlin KA (2016). Mental health of transgender children who are supported in their identities. Pediatrics, 137(3), e20153223. doi: 10.1542/peds.2015-3223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patil I (2018). ggstatsplot: “ggplot2” Based Plots with Statistical Details. CRAN. Retrieved from https://cran.r-project.org/web/packages/ggstatsplot/index.html
- Pinto RM, Melendez RM, & Spector AY (2008). Male-to-female transgender individuals building social support and capital from within a gender-focused network. Journal of Gay & Lesbian Social Services, 20(3), 203–220. doi: 10.1080/10538720802235179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescott CA, McArdle JJ, Hishinuma ES, Johnson RC, Miyamoto RH, Andrade NN,… Carlton BS (1998). Prediction of major depression and dysthymia from CES-D scores among ethnic minority adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 37(5), 495–503. doi: 10.1097/00004583-199805000-00012 [DOI] [PubMed] [Google Scholar]
- Puckett JA, Maroney MR, Levitt HM, & Horne SG (2016). Relations between gender expression, minority stress, and mental health in cisgender sexual minority women and men. Psychology of Sexual Orientation and Gender Diversity, 3(4), 489. doi: 10.1037/sgd0000201 [DOI] [Google Scholar]
- R Core Team. (2019). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from https://www.R-project.org/ [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Roberts RE, Andrews JA, Lewinsohn PM, & Hops H (1990). Assessment of depression in adolescents using the Center for Epidemiologic Studies depression scale. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 2(2), 122–128. doi: 10.1037/1040-3590.2.2.122 [DOI] [Google Scholar]
- Rood BA, Reisner SL, Surace FI, Puckett JA, Maroney MR, & Pantalone DW (2016). Expecting rejection: Understanding the minority stress experiences of transgender and gender-nonconforming individuals. Transgender Health, 1(1), 151–164. doi: 10.1089/trgh.2016.0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan C, Russell ST, Huebner D, Diaz R, & Sanchez J (2010). Family acceptance in adolescence and the health of LGBT young adults. Journal of Child and Adolescent Psychiatric Nursing, 23(4), 205–213. doi: 10.1111/j.1744-6171.2010.00246.x [DOI] [PubMed] [Google Scholar]
- Salk RH, Thoma BC, & Choukas-Bradley S (Under Review). The Gender Minority Youth Study: Overview of Methods and Social Media Recruitment of a Nationwide Sample of U.S. Cisgender and Transgender Adolescents. [DOI] [PMC free article] [PubMed]
- Santos CE, & VanDaalen RA (2016). The associations of sexual and ethnic-racial identity commitment, conflicts in allegiances, and mental health among lesbian, gay, and bisexual racial and ethnic minority adults. Journal of Counseling Psychology, 63(6), 668–676. doi: 10.1037/cou0000170 [DOI] [PubMed] [Google Scholar]
- Szymanski DM, & Meyer D (2008). Racism and heterosexism as correlates of psychological distress in African American sexual minority women. Journal of LGBT Issues in Counseling, 2(2), 94–108. doi: 10.1080/15538600802125423 [DOI] [Google Scholar]
- Thoma BC, & Huebner DM (2013). Health consequences of racist and antigay discrimination for multiple minority adolescents. Cultural Diversity & Ethnic Minority Psychology, 19(4), 404–414. doi: 10.1037/a0031739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoma BC, Salk RH, Choukas-Bradley S, Goldstein TR, Levine MD, & Marshal MP (2019). Suicidality disparities between transgender and cisgender adolescents. Pediatrics, 144(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas AJ, Hacker JD, & Hoxha D (2011). Gendered racial identity of Black young women. Sex Roles, 64(7–8), 530–542. doi: 10.1007/s11199-011-9939-y [DOI] [Google Scholar]
- Thomas EL, Dovidio JF, & West TV (2014). Lost in the categorical shuffle: Evidence for the social non-prototypicality of Black women. Cultural Diversity and Ethnic Minority Psychology, 20(3), 370–376. doi: 10.1037/a0035096 [DOI] [PubMed] [Google Scholar]
- Timmins L, Rimes KA, & Rahman Q (2017). Minority stressors and psychological distress in transgender individuals. Psychology of Sexual Orientation and Gender Diversity, 4(3), 328. doi: 10.1037/sgd0000237 [DOI] [Google Scholar]
- Toomey RB, Huynh VW, Jones SK, Lee S, & Revels-Macalinao M (2017). Sexual minority youth of color: A content analysis and critical review of the literature. Journal of Gay & Lesbian Mental Health, 21(1), 3–31. doi: 10.1080/19359705.2016.1217499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toomey RB, Syvertsen AK, & Shramko M (2018). Transgender Adolescent Suicide Behavior. Pediatrics, 142(4), e20174218. doi: 10.1542/peds.2017-4218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees BW, Paunesku D, Kuwabara SA, Basu A, Gollan J, Hankin BL,… Reinecke M (2008). Protective and vulnerability factors predicting new-onset depressive episode in a representative of U.S. adolescents. Journal of Adolescent Health, 42(6), 605–616. doi: 10.1016/j.jadohealth.2007.11.135 [DOI] [PubMed] [Google Scholar]
- Velez BL, Moradi B, & Deblaere C (2015). Multiple oppressions and the mental health of sexual minority Latina/o individuals. The Counseling Psychologist, 43(1), 7–38. doi: 10.1177/0011000014542836 [DOI] [Google Scholar]
- Velez B, Watson L, Cox R Jr., & Flores M (2017). Minority Stress and Racial or Ethnic Minority Status: A Test of the Greater Risk Perspective. Psychology of Sexual Orientation and Gender Diversity, 4. doi: 10.1037/sgd0000226 [DOI] [Google Scholar]
- Velez BL, Polihronakis CJ, Watson LB, & Cox R Jr. (2019). Heterosexism, racism, and the mental health of sexual minority people of color. The Counseling Psychologist, 47(1), 129–159. doi: 10.1177/0011000019828309 [DOI] [Google Scholar]
- Walls NE, Kane SB, & Wisneski H (2010). Gay—Straight Alliances and School Experiences of Sexual Minority Youth. Youth & Society, 41(3), 307–332. doi: 10.1177/0044118X09334957 [DOI] [Google Scholar]
- Wang K, Rendina HJ, & Pachankis JE (2016). Looking on the bright side of stigma: How stress-related growth facilitates adaptive coping among gay and bisexual men. Journal of Gay & Lesbian Mental Health, 20(4), 363–375. doi: 10.1080/19359705.2016.1175396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham H (2011). ggplot2. Wiley Interdisciplinary Reviews: Computational Statistics, 3(2), 180–185. doi: 10.1002/wics.147 [DOI] [Google Scholar]
- Zell E, Strickhouser JE, & Krizan Z (2018). Subjective social status and health: A meta-analysis of community and society ladders. Health Psychology, 37(10), 979–987. doi: 10.1037/hea0000667 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.