Abstract
Osteoporosis (OP) is a multifactorial disease influenced by genetic, epigenetic, and environmental factors. One of the main causes of the bone homeostasis alteration is inflammation resulting in excessive bone resorption. Long non-coding RNAs (lncRNAs), have a crucial role in regulating many important biological processes in bone, including inflammation. We designed our study to identify lncRNAs misregulated in osteoblast primary cultures derived from OP patients (n = 4), and controls (CTRs, n = 4) with the aim of predicting possible RNA and/or protein targets implicated in this multifactorial disease. We focused on 84 lncRNAs regulating the expression of pro-inflammatory and anti-inflammatory genes and miRNAs. In silico analysis was utilized to predict the interaction of lncRNAs with miRNAs, mRNAs, and proteins targets. Six lncRNAs were significantly down-regulated in OP patients compared to controls: CEP83-AS1, RP11-84C13.1, CTC-487M23.5, GAS5, NCBP2-AS2, and SDCBP2-AS1. Bioinformatic analyses identified HDCA2, PTX3, and FGF2 proteins as downstream targets of CTC-487M23.5, GAS5, and RP11-84C13.1 lncRNAs mediated by the interaction with miRNAs implicated in OP pathogenesis, including miR-21-5p. Altogether, these data open a new regulatory mechanism of gene expression in bone homeostasis and could direct the development of future therapeutic approaches.
Keywords: osteoporosis, epigenetics, long non-coding RNAs, inflammation, bone homeostasis, osteoblast
1. Introduction
Osteoporosis (OP) is characterized by an imbalance in the regulation of bone remodeling between osteoblastic bone formation and osteoclastic bone resorption [1]. Currently OP is viewed as a heterogeneous condition which can occur in any age of life and its etiology is attributed to various endocrine, metabolic, and mechanical factors. Among them, hormonal deficiency plays a fundamental role. Estrogen has a protective effect in bone, due to a direct action on osteoclasts (increasing apoptosis and reducing the receptor activator of nuclear factor-κB ligand (RANKL)-dependent osteoclast formation) and osteoblasts (increasing osteoblast survival and collagens type I production) [2]. Bone homeostasis is important to maintain the coordinated activity between bone-forming osteoblasts and bone-resorbing osteoclasts. Emerging evidence suggests that bone homeostasis imbalance is caused by estrogen deficiency resulting in increased inflammation that results in excessive bone resorption. Osteoporosis is therefore described as an inflammatory disease [2]. In such inflamed situations, pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 stimulate osteoclastogenesis directly. This leads to the recruitment of osteoclast precursor cells into the bone-erosive site and their subsequent differentiation into mature osteoclasts [3].
Numerous genes have been associated with osteoporosis risk and among candidate genes, the vitamin D receptor (VDR) gene, encoding a nuclear hormone receptor, was the first to be proposed as a major susceptibility locus [4]. Recently, genome-wide association studies (GWASs) have identified several osteoporosis-related genes, such as catenin (cadherin-associated protein) beta 1 (CTNNB1), sclerostin (SOST), low-density lipoprotein receptor-related protein 4 (LRP4), LRP5, wingless-type MMTV integration site family, member 4 (WNT4), WNT5B, and AXIN1 [5]. However, genetic factors alone are not sufficient to explain the pathogenesis of osteoporosis. Epigenetic factors represent a link between individual genetic aspects and environmental influences, and they are involved in bone biology and osteoporosis [6]. These mechanisms include post-translational histone modifications, ncRNA-mediated post-transcriptional regulation, and DNA methylation [7]. Several studies showed the importance of miRNAs in controlling bone homeostasis and metabolism. In particular, in a study performed by Weilner et al., authors have found 10 circulating miRNAs deregulated in patients with recent osteoporotic fractures. In total six miRNAs, miR-10a-5p, miR-10b-5p, miR-133b, miR-22-3p, miR-328-3p, and let-7g-5p exhibited significantly different serum levels in response to fracture [8]. Another two studies have profiled the expression of miRNAs in peripheral blood mononuclear cells (PBMCs) from postmenopausal women with low and high bone mineral density (BMD), and they found that miR-503 was markedly reduced and miR-133a significantly increased in OP patients [7]. More recently, much interest has focused on another class of ncRNAs, long non-coding RNAs (lncRNAs) belonging to a novel heterogeneous class of non-protein-coding transcripts with a length of more than 200 nt [1] and with many different functions. LncRNAs can act as decoys by binding to RNA or proteins, they can inhibit or promote transcription through histone and chromatin alteration, alter splicing profiles, or mask miRNA binding sites [9]. LncRNAs have crucial roles in regulating many important biological processes such as cell proliferation, differentiation, migration, and development thus contributing to molecular pathogenesis of different human diseases [1]. To date, studies on the role of lncRNAs in bone biology have been limited. In one study, it was proposed that DANCR (RNA- differentiation antagonizing nonprotein coding RNA) lncRNA regulates expression of the osteogenic regulator Runx2 by recruiting the Polycomb repressive complex component EZH2 to the Runx2 promoter, thereby resulting in suppression of osteogenesis [10]. Runx2 is a member of the RUNX family of transcription factors and encodes for a nuclear protein with a Runt DNA-binding domain and is essential for osteoblast development and bone formation. Runx2 drives pluripotent mesenchymal cells to the osteoblast lineage and increases their maturation and function by regulating the expression of several osteoblast-related extracellular matrix proteins, in particular osteocalcin (OC) [11]. Otto et al. demonstrated that Runx2-deficient mice present a cartilaginous skeleton associated with the absence of osteoblasts, highlighting the major role of Runx2 in bone patterning and endochondral and intramembranous ossification [12]. Additionally, a set of lncRNAs microarray expression data was also generated from a mouse mesenchymal stem cells (MSC) line that was stimulated with BMP2. This study identified 116 lncRNAs that were differentially expressed but no functional characterization was performed to test the requirements for these lncRNAs in osteogenesis [13].
Primary cultures are important tools to provide valuable information about the processes of skeletal development, bone formation, and bone resorption [14]. In this study, we analysed the expression profile of 84 lncRNAs validated or predicted to regulate the expression of genes for acute-phase response, autoimmunity, humoral immune response, inflammatory responses, and innate and adaptive immunity in cultured primary osteoblast cells from OP patients (n = 4) and control (CTR) individuals (n = 4) in order to find a possible regulatory mechanism controlling changes in gene expression in bone homeostasis.
2. Experimental Section
2.1. Subjects
We enrolled eight individuals who underwent hip surgery in the Orthopedic and Traumatology Department of Policlinico Tor Vergata Hospital. Specifically, we enrolled four consecutive patients (three females and one male) (OP group) who underwent hip arthroplasty for medial hip fractures for low-energy trauma (73.00 ± 3.20 years), and four individuals (44.23 ± 2.77 years) who underwent hip arthroplasty for high-energy hip fractures (two females and two males) (CTR, group) (Table 1). Exclusion criteria were history of cancer, myopathies, or other neuromuscular diseases or chronic administration of corticosteroid for autoimmune diseases (> 1 month), diabetes, alcohol abuse and HBV, HCV, or HIV infections.
Table 1.
Main characteristics of osteoporosis (OP) patients and control (CTR) individuals.
| Clinical Characteristics | OP (n = 4) | CTR (n = 4) |
|---|---|---|
| BMI (kg/m2) | 25.61 ± 1.13 | 27.0 ± 6.0 |
| T Score (L1–L4) | −2.85 ± 0.15 | 0.95 ± 0.01 |
| T Score (neck) | −2.77 ± 0.17 | 0.19 ± 0.05 |
| PASE test | 72.96 ± 24.89 | 100 ± 20.86 |
| Kellgren–Lawrence scale | 0–1 | 0 |
All experiments described in the present study were approved by the ethics committee of Policlinico Tor Vergata (approval reference number #85/12; June, 2017). All experimental procedures were carried out according to The Code of Ethics of the World Medical Association (Declaration of Helsinki). Informed consent was obtained from all patients prior to surgery. Specimens were handled and carried out in accordance with the approved guidelines.
2.2. Human Osteoblast Primary Cell Cultures
Primary cultures of osteoblasts were isolated from the cancellous bone of healthy patients with high-energy femoral fracture and patient affected by osteoporosis. The samples were dissected and treated to obtain a homogeneous population of osteoblasts. Briefly, after dissection, trabecular bone fragments were repeatedly washed in PBS. Then bone fragments were briefly incubated at 37 °C with 1 mg/mL trypsin from porcine pancreas ≥ 60 U/mg (SERVA Electrophoresis GmbH, Heidelberg, Germany) diluted in DPBS. After washing, bone fragments were subjected to repeated digestions with 2.5 mg/mL Collagenase NB 4G Proved grade ≥ 0.18 U/mg (SERVA Electrophoresis GmbH) diluted in DPBS with calcium and magnesium. Supernatant were collected and centrifuged at 310 RCF (Eppendorf, 5804 R) for 5 min. Cell pellets were resuspended in DMEM/F12 (Biowest, Nuaillé, FR) supplemented with 15% FBS, 50 μg/mL gentamicin, and 0.08% Fungizone, penicillin streptomycin (Sigma Chemical Co., St. Louis, MO, USA), and amphotericin B (Biowest), seeded into a 24-well plate and incubated at 37 °C, 5% CO2 until reaching confluence (about 4 weeks). Medium was changed twice a week (Figure 1) [15,16,17]. To assess the quality of each cell purification a fraction of the purified cells was inspected using immunochemistry analysis and morphological inspection. Osteoblast primary cells were observed to be homogeneous and appropriate for osteoblasts and expressing BMP2, RUNX2, and RANK-L. Cells were analyzed for lncRNAs expression at third passage.
Figure 1.
Primary human osteoblast cultures were observed under phase-contrast microscope at 10× field. Scale bar: 500 μm.
2.3. LncRNA Analysis
Total RNA was extracted from osteoblast primary cultures derived by OP (n = 4) and CTR (n = 4), as described [18]. First strand cDNA was synthesized using RT2PreAMP cDNA synthesis kit (QIAGEN, Germany) and pre-amplified with RT2lncRNA PreAMP primer mix (QIAGEN, Hilden, Germany) that contained a specific set of primers to target genes of the human RT2lncRNA inflammatory response and the autoimmunity PCR array (QIAGEN, Hilden, Germany). qRT-PCR was performed using RT2 SYBR® Green qPCR MasterMix (QIAGEN, Hilden, Germany) and RT2lncRNA PCR array human inflammatory response and autoimmunity (QIAGEN, Hilden, Germany) which contains pre-dispensed, laboratory verified, gene-specific primer pairs). The experiment was designed to analyze each sample on a single 96-well plate. The reaction was performed by ABI 7500 Fast Real-Time PCR System (Applied Biosystems, Foster City, CA, USA) with a holding stage at 95 °C for 10 min followed by 40 cycles of each PCR step: 95 °C for 15 s and 60 °C for 1 min. For data analysis, the Ct values were exported to an Excel file and uploaded into the RT2 PCR Array Data Analysis Web Portal at https://www.qiagen.com/dataanalysiscenter. Ct values were normalized based on automatic selection of housekeeping from the full panel on the PCR array. This method automatically selected two optimal reference genes RP11-325K4.3 (ENST00000565861) and RP11-96D1.10 (ENST00000571975) with the most stable expression for the analysis from the full plate on the PCR array. Using the Data Analysis Web Portal, we calculated fold change/regulation with ΔΔCt method, in which ΔCt is calculated between gene of interest and an average of reference genes, followed by ΔΔCt calculations (ΔCt (patient) − ΔCt (control)). Fold change was then calculated using the 2−ΔΔCt formula. The p-values were calculated based on a Student’s t test of the three replicate 2(−ΔCt) values for each gene in the control and OP groups.
2.4. Prediction Methods for lncRNA–RNA Interactions
In silico prediction of lncRNA–mRNA interactions was performed using the database containing the lncRNA–mRNA and lncRNA–lncRNA interactions for 23,898 lncRNAs and 20,185 mRNAs (available at http://rtools.cbrc.jp/cgi-bin/RNARNA/index.pl). In this database, each possible pair of RNAs are ranked according to two interaction energies calculated from the local interaction energies between the two RNA sequences: MinEnergy (adequate for short RNA sequences or for cases in which the strongest local interaction is dominant) and SumEnergy (adequate for long RNA sequences such as lncRNAs and mRNAs and for cases in which several strong interactions exist). The predicted lncRNA–mRNA interactions including these two types of interacting energies were used for the analysis [19].
2.5. Prediction Methods for lncRNA–RNA Binding Protein (RBP) Interactions
RBP and lncRNA interactions were predicted using the NPInter v3.0 (https://www.bioinfo.org/NPInter/index.htm), a database which contains experimentally-verified interaction between ncRNA (excluding tRNA and rRNA) and other biomolecules (proteins, mRNA, miRNA, and genomic DNAs) [20].
2.6. Prediction Methods for lncRNA–miRNA Interactions
In silico prediction of lncRNA–miRNA interactions was performed using DIANA-LncBase v2 [21] (www.microrna.gr/LncBase), a database of experimentally-supported and in silico-predicted miRNA recognition elements (MREs) on lncRNAs, identified with the DIANA-microT algorithm. For assessment of miRNA regulatory roles in bone homeostasis and osteoporosis pathways and the identification of miRNA-target genes implicated in these pathways, we performed a functional characterization using DIANA-miRPath v3.0 [22] (http://www.microrna.gr/miRPathv3) and DIANA-TarBase v8.0 [23] (http://carolina.imis.athena-innovation.gr/diana_tools/web/index.php?r=tarbasev8%2Findex), respectively.
3. Results
3.1. Clinical Evaluation and In Vitro Study of Human Osteoblast Primary Cell Cultures
The OP group included four patients (three females and one male) with fragility hip fracture, T-score ≤ −2.5 S.D. and Kellgren−Lawrence (K–L) score from 0 to 1; while four control individuals (two females and two males) were characterized by a T-score ≥ −1.0 S.D. and K–L score from 0 to 1 (Table 1). Osteoblasts from the cancellous bone of OP and control (CTR) individuals were isolated and cultured in vitro (Figure 1), as described in the Methods section, for lncRNAs expression analysis.
3.2. Expression Profile of lncRNAs
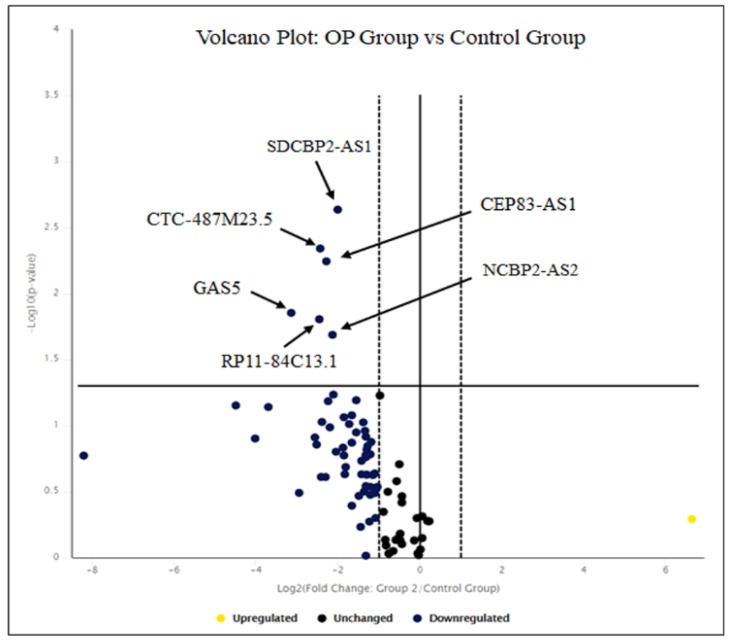
In order to evaluate the expression levels of lncRNAs in osteoblast primary cells from OP patients vs. CTRs, we analyzed 84 lncRNAs, validated or predicted to regulate the expression of pro-inflammatory and anti-inflammatory genes and microRNAs (https://www.qiagen.com/us/shop/assay-technologies/realtime-pcr-and-rt-pcr-reagents/rt2-lncrna-pcr-arrays?catno=-rt-pcr-reagents/rt2-lncrna-pcr-arrays?catno=LAHS-004Z#geneglobe). We selected significant changes (p < 0.05) that were at least two-fold up- or down-regulated as compared to controls. We identified six lncRNAs that were significantly down-regulated in OP patients compared to CTRs: CEP83 antisense RNA 1 (CEP83-AS1 and NR_027035) fold-regulation = −8.75 (p = 0.014), RP11-84C13.1 (ENST00000603357) fold regulation= −5.44 (p = 0.016), CTC-487M23.5 (ENST00000602872) fold-regulation = −5.39 (p = 0.004), growth arrest-specific 5 (GAS5 and NR_002578) fold-regulation= −4.86 (p = 0.006), hypothetical LOC152217 (NCBP2-AS2 and NR_024388) fold-regulation= −4.34 (p = 0.02), SDCBP2 antisense RNA 1 (SDCBP2-AS1 and ENST00000446423) fold-regulation= −4.00 (p = 0.002) (Table 2 and Figure 2).
Table 2.
Differentially-expressed long non-coding RNAs in OP patients vs. CTRs.
| Long Non-Coding RNAs (LncRNAs) | Fold-Regulation | p-Value |
|---|---|---|
| CEP83-AS1 | −8.75 ↓ down | 0.014 |
| RP11-84C13.1 | −5.44 ↓ down | 0.015 |
| CTC-487M23.5 | −5.39 ↓ down | 0.004 |
| GAS5 | −4.86 ↓ down | 0.006 |
| NCBP2-AS2 | −4.34 ↓ down | 0.020 |
| SDCBP2-AS1 | −4.00 ↓ down | 0.002 |
Fold-regulation represents fold-change results in a biologically meaningful way. Fold-change values greater than one indicate a positive- or an up-regulation, and the fold-regulation is equal to the fold-change. Fold-change values less than one indicate a negative- or down-regulation, and the fold-regulation is the negative inverse of the fold-change. The p-values were calculated based on a Student’s t-test of the three replicate 2(−ΔCt) values for each gene in the control group and OP group [24]. ↓: down-regulation.
Figure 2.
Volcano plot of LncRNAs levels in OP vs. CTRs. The Volcano plot shows the significant lncRNAs that we found down-regulated in osteoblast cell lines on the left (down-regulated) and above the solid vertical line (statistically significant), according to significant p-value and fold-regulation change. The solid vertical line represents no change in gene expression (log2 (1) = 0). The dotted lines represent a selected threshold or boundary for fold change. The default setting is 2. The solid vertical line represents a selected threshold for the p-value and statistical significance. The default setting is 0.05. Statistical significance versus fold-change is shown on the y- and x-axes, respectively [24].
3.3. Bioinformatic Analysis and Target Prediction
In order to investigate a possible role of the six lncRNAs differentially expressed in primary osteoblasts from OP patients, we perform a bioinformatic analysis using different web-based target prediction tools for mRNAs, proteins, or miRNA targets.
First, we identified putative lncRNA–mRNA interactions using a database that contains all the predicted RNA−RNA interactions along with the following information: MinEnergy and SumEnergy [19] (http://rtools.cbrc.jp/cgi-bin/RNARNA/index.pl). The top five predicted RNA targets according to both MinEnergy and SumEnergy interaction are reported in Table 3. This analysis did not uncover any RNA molecule interacting with CEP83 antisense RNA 1 (head to head) lncRNA.
Table 3.
List of interaction between lncRNAs and putative mRNAs.
| List of mRNAs Interacting with lncRNAs | |||||
|---|---|---|---|---|---|
| LncRNA | mRNA | Ensemble ID | MinEnergy | Location | SumEnergy |
|
CEP83-AS1
(ENST00000623122) |
- | - | - | - | - |
|
CTC-487M23.5
(ENST00000602872) |
AGO3 | ENST00000373191 | −63.2 | UTR3 | −2550.9 |
| RBM28 | ENST00000223073 | −62.5 | UTR3 | −2038.0 | |
| PDK1 | ENST00000282077 | −71.3 | UTR3 | −1994.5 | |
| PPM1L | ENST00000498165 | −72.6 | UTR3 | −1622.0 | |
| HDAC2 | ENST00000519065 | −56.2 | UTR3 | −1573.2 | |
|
GAS5
(ENST00000450589) |
SOD2 | ENST00000538183 | −40.8 | UTR3 | −1798.0 |
| FGFR1OP | ENST00000366847 | −38.2 | UTR3 | −1508.2 | |
| NOS1 | ENST00000317775 | −47.2 | UTR3 | −1380.6 | |
| EIF4E | ENST00000450253 | −42.2 | UTR3 | −1298.0 | |
| LRRC27 | ENST00000392638 | −42.9 | UTR3 | −1002.8 | |
|
RP11-84C13.1
(ENST00000603357) |
IGFN1 | ENST00000335211 | −39.1 | CDS | −2316.5 |
| RYR2 | ENST00000366574 | −40.3 | CDS | −1848.3 | |
| CCDC88A | ENST00000436346 | −35.2 | UTR5 | −1688.0 | |
| CACNG8 | ENST00000270458 | −37.9 | UTR3 | −1488.5 | |
| RYR3 | ENST00000389232 | −40.4 | CDS | −1469.4 | |
|
NCBP2-AS2
(ENST00000602845) |
SMAD2 | ENST00000402690 | −34.5 | UTR5 | −1363.4 |
| PTPN14 | ENST00000366956 | −28.7 | CDS | −1249.8 | |
| LRP1 | ENST00000243077 | −31.0 | CDS | −1132.5 | |
| PTPN4 | ENST00000263708 | −28.5 | CDS | −1056.9 | |
| IGSF10 | ENST00000282466 | −29.0 | CDS | −1056.2 | |
|
SDCBP2-AS1
(ENST00000446423) |
ASXL2 | ENST00000435504 | −38.9 | CDS | −4456.0 |
| CBL | ENST00000264033 | −37.5 | UTR3 | −3988.8 | |
| HIVEP3 | ENST00000372584 | −38.1 | CDS | −3670.8 | |
| HDAC9 | ENST00000406451 | −38.9 | CDS | −3554.0 | |
| ROCK1 | ENST00000399799 | −39.0 | UTR5 | −3065.6 | |
(-): no mRNA interaction found.
We then searched for lncRNA–protein interactions with the aim of identifying proteins implicated in the pathogenic mechanism of osteoporosis. This in silico analysis was performed through the NPInter v3.0 database and disclosed only two protein targets potentially related to bone homeostasis: HNRNPC [25] interacting with GAS5 and ADAR1 [26] interacting with SDCBP2-AS1 lncRNA.
We also used DIANA-LncBase v2 tools to identify miRNAs targeted by the six lncRNAs deregulated in osteoblast cell lines. This analysis revealed that CTC-487M23.5, GAS5, and RP11-84C13.1 lncRNAs potentially bind only one miRNA each: hsa-miR-136-3p (Pr. Score 0.451), hsa-miR-21-5p (Pr. Score 0.382), and hsa-miR-576-3p (Pr. Score 0.408), respectively (Table 4). Conversely, NCBP2-AS2 and SDCBP2-AS1 lncRNAs interact with multiple miRNAs, including miR-497~195 cluster, hsa-miR-103a-3p, hsa-miR-23a-3p, hsa-miR-24-2-5p, and hsa-miR-23b-3p which have been already associated with the inhibition of osteoblastogenesis (through the downregulation of multiple BMP-responsive genes), regulation of osteoblast differentiation (by directly targeting Runx2), and suppression of osteogenesis and bone formation by targeting most of the known signaling pathways involved in osteoblast biology [27,28].
Table 4.
List of interactions between lncRNAs and putative miRNA-targeted proteins and pathways.
| List of miRNAs Interacting with lncRNA | ||||
|---|---|---|---|---|
| LncRNA | miRNA | Pr.Score* | KEGG Pathways | Gene Target |
|
CEP83-AS1
(ENST00000623122) |
- | - | - | - |
|
CTC-487M23.5
(ENST00000602872) |
hsa-miR-136-3p | 0.451 | ECM-receptor interaction | THBS2 |
| PPP1CB | ||||
| PDGFC | ||||
|
GAS5
(ENST00000450589) |
hsa-miR-21-5p | 0.382 | Hippo signaling pathway FoxO signaling pathway | PDCD4 |
| PTX3 | ||||
|
RP11-84C13.1
(ENST00000603357) |
hsa-miR-576-3p | 0.408 | Hippo signaling pathway FoxO signaling pathway | FGF2 |
| FRS2 | ||||
| PTPN11 | ||||
|
NCBP2-AS2
(ENST00000602845) |
hsa-miR-103a-3p | 0.734 | Hippo signaling pathway FoxO signaling pathway Wnt signaling pathway TGF-β signaling pathway mTOR signaling pathway HIF-1 signaling pathway AMPK signaling pathway Insulin signaling pathway TNF signaling pathway | Runx2 |
| hsa-miR-497-5p | 0.799 | BMP | ||
| hsa-miR-195-5p | 0.662 | |||
| hsa-miR-23a-3p | 0.417 | Runx2/SATB2 | ||
| hsa-miR-24-2-5p | 0.497 | |||
| hsa-miR-23b-3p | 0.418 | SMAD | ||
| hsa-let-7d-3p | 0.391 | Collagens | ||
|
SDCBP2-AS1
(ENST00000446423) |
hsa-miR-2116-3p | 0.545 | FoxO signaling pathway TGF-β signaling pathway | |
| hsa-miR-532-3p | 0.558 | |||
| hsa-miR-150-5p | 0.644 | |||
* Pr. Score (or miTG score) is a general score for the predicted interaction, the closer to 1, the greater the confidence. The higher miTG score corresponds to a high probability of targeting [21] (-): no miRNA and gene interaction found.
Finally, DIANA-miRPath v3.0 and DIANA-TarBase v8.0 have been queried to understand the regulatory role of miRNAs into biological processes and pathways through the identification of targeted proteins. As shown in Table 4, the downregulation of CTC-487M23.5, GAS5, RP11-84C13.1, NCBP2-AS2, and SDCBP2-AS1 could interfere with bone homeostasis deregulating different KEEG pathway such as Hippo, Wnt and FoxO signaling related to bone formation and resorption. Unfortunately, we were not able to identify any CEP83-AS1 protein interactors.
4. Discussion
LncRNAs are very versatile regulators and they can play different roles in the nucleus and in the cytoplasm through various mechanisms. LncRNAs control the epigenetic state of genes and regulate both transcriptional (when they bind 3’UTR of mRNAs) and translation level (by base pairing at different sites in the coding and untranslated regions of mRNAs). Moreover, lncRNAs also have the ability to compete for miRNA-binding and to act as ‘sponges’ or ‘decoys’ for miRNAs, thus leading to enhanced translations of targeted transcripts [29,30]. Although the functional roles of miRNAs in osteoporosis have been extensively investigated [7,31,32], the role of lncRNAs in bone homeostasis and their underlying mechanism remains undefined [33]. Osteoporosis is not typically considered an immunological disorder albeit there are overlapping pathways between bone biology and biology of inflammation [34]. Emerging clinical and molecular studies suggest that inflammation exerts significant influence on bone turnover, inducing osteoporosis. Numerous pro-inflammatory cytokines have been implicated in the regulation of osteoblasts and osteoclasts, and a shift towards an activated immune profile has been hypothesized as an important risk factor [35]. In this paper, we report results of a pilot study to determine the expression profile of lncRNAs regulating pro-inflammatory and anti-inflammatory genes and miRNAs in osteoblast primary cells from OP patients vs. controls. Six lncRNAs were significantly down-regulated in OP patients and in silico bioinformatics analysis highlighted several predicted lncRNA targets (either miRNAs or mRNAs) implicated in bone homeostasis (Table 3 and Table 4). Our expression analysis showed the down-regulation in OP cells of GAS5 lncRNA, whose role is well established in literature. GAS5 lncRNA has been reported to be a key control element during growth, differentiation, and development in mammalian species. In a recent study, the role of GAS5 in growth plate chondrocytes [36], bone marrow mesenchymal stem cells (BMSCs) [37], and human multipotential mesenchymal stem cells (hMSCs) [38] was demonstrated and this could suggest a role of GAS5 in bone homeostasis. GAS5 is predicted to negatively regulate hsa-miR-21-5p which also regulates osteoclast formation and differentiation through a positive feedback loop involving c-Fos/miR-21/PDCD4 (programed cell death 4) [31]. Furthermore, miR-21-5p was highly expressed in bone tissue obtained from osteoporosis patients [39,40]. One of putative targets of hsa-miR-21-5p is PTX3 mRNA. Pentraxin 3 (PTX3) gene encodes for the prototypic long pentraxin, which is released in response to primary pro-inflammatory stimuli and represents an essential player in tuning inflammation [41,42,43]. It has been proposed that PTX3 elevation during bone inflammatory conditions promotes RANKL production and favors osteoclastogenic potential by osteoblasts, implying its involvement in bone resorption [44]. In a recent study, Scimeca et al., demonstrated the down-regulation of PTX3 at both transcription and translation levels in OP osteoblast cell lines [45]. It is possible therefore to speculate that PTX3 decrease is a downstream effect, mediated by miR-21-5p, caused by the downregulation of GAS5 lncRNA in osteoblasts from OP patients (Figure 3A) [29,30].
Figure 3.
Hypothetical pathogenetic mechanisms emerging from this study. (A) Growth arrest-specific 5 (GAS5) lncRNA masks miR-21-5p binding sites, (B) CTC-487M23.5 lncRNA inhibits the translation of HDAC2 mRNA, (C) NCPB2-AS2 lncRNA masks miRNA binding sites implicated in osteoblast differentiation, and (D) RP11-84C13.1 lncRNA masks miR-576-3p binding sites. ↑ and ↑: increase; ↓: decrease;  : no repression;
: no repression;  : repression.
: repression.
Moreover, bioinformatics analysis predicted the CTC-487M23.5 lncRNA binding with the 3’UTR of HDAC2 mRNA. HDAC2, the major enzymes for histone deacetylation, is a key positive regulator during receptor activator of nuclear factor-κB ligand (RANKL) and its overexpression leads to osteoclastogenesis and bone resorption. In particular, HDAC2 activates Akt thus suppressing FoxO1 transcription resulting in enhanced osteoclastogenesis [46]. Further functional studies are needed to demonstrate the CTC-487M23.5 lncRNA/HDAC2 mRNA interaction and its effect on the stability and translation of HDAC2 mRNA (Figure 3B).
Another interesting result is the interaction between NCBP2-AS2 and several miRNAs deregulated in osteoporosis such as members of the miR-497∼195 cluster (associated with the inhibition of osteoblastogenesis), miR-103a (regulating osteoblast differentiation), and miR-23a/-27a/24-2 cluster (controlling osteogenesis) [28,39]. Thus, NCBP2-AS2 lncRNA could indirectly regulate osteogenesis and bone formation through interaction with this set of miRNAs by targeting most of the known signaling pathways involved in bone homeostasis. For example, Wnt/β-catenin signaling is indispensable for osteoblastogenesis, and loss or gain of function of this pathway is associated with a profound decrease or increase of bone mass, FoxOs were found to be crucial for bone mass homeostasis even though they are not bone specific transcription factors, and the Hippo pathway is involved in regulating bone-forming osteoblasts during bone development and remodeling [47,48] (Figure 3C). Interestingly, bioinformatic analysis also reveals that miR-103a and miR-23a/27a/24-2 clusters putatively interact with RUNX2, important regulatory factors involved in skeletal gene expression and osteoblastic differentiation [11]. Recent findings suggest that stabilized Runx2 induces Wnt signaling and enhances aerobic glycolysis in osteoblasts [49]. Moreover, Haxaire et al., [11] demonstrated that overexpression of Runx2 in experimental animals strongly induced RANKL, but depleted beta-catenin, reducing bone mass and bone volume. However, if the overexpression of Runx2 was performed in the presence of lithium chloride (an inhibitor of the beta-catenin degrading enzyme GSK-3 beta) osteoblasts could differentiate and bone volume was restored (described in a recent review by Kovács et al.) [50].
Finally, we found that RP11-84C13.1 lncRNA interacts with hsa-miR-576-3p. This miRNA is implicated in the regulation of viral infection and inflammation [51]. Bioinformatic analysis reveals that one of hsa-miR-576-3p targets is fibroblast growth factor 2 (FGF2) mRNA. FGF2 protein is expressed in the majority of cells and tissues including limb bud, chondrocyte and osteoblast cells, and it was experimentally demonstrated that deletion of Fgf2 in mice leads to decreased bone mass, bone formation, and mineralization [52] (Figure 3D).
In conclusion, although the present findings require confirmation in larger samples, our study has documented for the first time the deregulation of six lncRNAs in primary osteoblasts from OP patients with a potential involvement in inflammation and bone homeostasis. Moreover, an in silico search for lncRNA targets uncovered several mRNAs and proteins representing novel potential biomarkers for this debilitating disease. Additional experiments on the functional and physiological role of these lncRNAs and their putative interactions are needed in order to understand the pathogenic mechanism of OP and to develop personalized therapeutic approaches for bone resorption.
Abbreviations
| OP | Osteoporosis |
| CTR | Control |
| lncRNAs | Long non-coding RNAs |
| miRNAs | Micro-RNAs |
| PASE | Physical Activity Scale for the Elderly |
| Pr. Score | Prediction Score |
Author Contributions
F.C., U.T., and A.B. conceived and designed the research; F.C., M.M., V.V.V, A.M.R., and G.D’A. performed the experiments; F.C., M.S., M.C., G.N., A.O., V.T., U.T., and A.B. participated in data acquisition and curation; M.S. and V.V.V. provided help for using software and bioinformatics analysis; F.C., U.T., and A.B. wrote the original draft; M.S., U.T., and A.B. improved and revised this manuscript; U.T. and A.B. obtained funds. All authors have read and agreed to the published version of the manuscript.
Funding
This research was financed by the Italian Ministry of Education, University and Research (MIUR), PRIN 2015 Prot. #201528E7CM.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Valdés-Flores M., Casas-Avila L., de León-Suárez V.P., Falcón-Ramírez E. Genetics and Osteoporosis. In: Dionyssiotis Y., editor. Osteoporosis. InTech; London, UK: 2012. p. 33. [Google Scholar]
- 2.Mac I., Alcorta-sevillano N., Rodr C.I. Osteoporosis and the Potential of Cell-Based Therapeutic Strategies. Int. J. Mol. Sci. 2020;21:1653. doi: 10.3390/ijms21051653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gordon J.A.R., Montecino M.A., Aqeilan R.I., Janet L., Stein G.S., Lian J.B. Epigenetic Pathways Regulating Bone Homeostasis: Potential Targeting for Intervention of Skeletal Disorders. Curr. Osteoporos. Rep. 2014;12:496–506. doi: 10.1007/s11914-014-0240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Urano T., Inoue S. Genetics of osteoporosis. Biochem. Biophys. Res. Commun. 2014;452:287–293. doi: 10.1016/j.bbrc.2014.07.141. [DOI] [PubMed] [Google Scholar]
- 5.Richards J.B., Zheng H.-F., Spector T.D. Genetics of osteoporosis from genome-wide association studies: Advances and challenges. Nat. Rev. Genet. 2012;13:576–588. doi: 10.1038/nrg3228. [DOI] [PubMed] [Google Scholar]
- 6.Marini F., Cianferotti L., Brandi M., Marini F., Cianferotti L., Brandi M.L. Epigenetic Mechanisms in Bone Biology and Osteoporosis: Can They Drive Therapeutic Choices? Int. J. Mol. Sci. 2016;17:1329. doi: 10.3390/ijms17081329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vrtačnik P., Marc J., Ostanek B. Epigenetic mechanisms in bone. Clin. Chem. Lab. Med. 2014;52:589–608. doi: 10.1515/cclm-2013-0770. [DOI] [PubMed] [Google Scholar]
- 8.Weilner S., Skalicky S., Salzer B., Keider V., Wagner M., Hildner F., Gabriel C., Dovjak P., Pietschmann P., Grillari-Voglauer R., et al. Differentially circulating miRNAs after recent osteoporotic fractures can influence osteogenic differentiation. Bone. 2015;79:43–51. doi: 10.1016/j.bone.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 9.Santoro M., Nociti V., Lucchini M., De Fino C., Losavio F.A., Mirabella M. Expression Profile of Long Non-Coding RNAs in Serum of Patients with Multiple Sclerosis. J. Mol. Neurosci. 2016;59:18–23. doi: 10.1007/s12031-016-0741-8. [DOI] [PubMed] [Google Scholar]
- 10.Zhu L., Xu P.C. Downregulated LncRNA-ANCR promotes osteoblast differentiation by targeting EZH2 and regulating Runx2 expression. Biochem. Biophys. Res. Commun. 2013;432:612–617. doi: 10.1016/j.bbrc.2013.02.036. [DOI] [PubMed] [Google Scholar]
- 11.Haxaire C., Haÿ E., Geoffroy V. Runx2 Controls Bone Resorption through the Down-Regulation of the Wnt Pathway in Osteoblasts. Am. J. Pathol. 2016;186:1598–1609. doi: 10.1016/j.ajpath.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 12.Otto F., Thornell A.P., Crompton T., Denzel A., Gilmour K.C., Rosewell I.R., Stamp G.W.H., Beddington R.S.P., Mundlos S., Olsen B.R., et al. Cbfa1, a Candidate Gene for Cleidocranial Dysplasia Syndrome, Is Essential for Osteoblast Differentiation and Bone Development. Cell. 1997;89:765–771. doi: 10.1016/S0092-8674(00)80259-7. [DOI] [PubMed] [Google Scholar]
- 13.Huynh N.P.T.T., Anderson B.A., Guilak F., McAlinden A. Emerging roles for long noncoding RNAs in skeletal biology and disease. Connect. Tissue Res. 2017;58:116–141. doi: 10.1080/03008207.2016.1194406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kartsogiannis V., Ng K.W. Cell lines and primary cell cultures in the study of bone cell biology. Mol. Cell. Endocrinol. 2004;228:79–102. doi: 10.1016/j.mce.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Wergedal J.E., Baylink D.J. Characterization of Cells Isolated and Cultured from Human Bone. Exp. Biol. Med. 1984;176:60–69. doi: 10.3181/00379727-176-41843. [DOI] [PubMed] [Google Scholar]
- 16.Wong G., Cohn D.V. Separation of parathyroid hormone and calcitonin-sensitive cells from non-responsive bone cells. Nature. 1974;252:713–715. doi: 10.1038/252713a0. [DOI] [PubMed] [Google Scholar]
- 17.Robey P.G., Termine J.D. Human bone cells in vitro. Calcif. Tissue Int. 1985;37:453–460. doi: 10.1007/BF02557826. [DOI] [PubMed] [Google Scholar]
- 18.Anastasiadou E., Garg N., Bigi R., Yadav S., Campese A.F., Lapenta C., Spada M., Cuomo L., Botta A., Belardelli F., et al. Epstein-Barr virus infection induces miR-21 in terminally differentiated malignant B cells. Int. J. Cancer. 2015;137:1491–1497. doi: 10.1002/ijc.29489. [DOI] [PubMed] [Google Scholar]
- 19.Terai G., Iwakiri J., Kameda T., Hamada M., Asai K. Comprehensive prediction of lncRNA-RNA interactions in human transcriptome. BMC Genomics. 2016;17:12. doi: 10.1186/s12864-015-2307-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hao Y., Wu W., Li H., Yuan J., Luo J., Zhao Y., Chen R. NPInter v3.0: An upgraded database of noncoding RNA-associated interactions. Database. 2016;2016:1–9. doi: 10.1093/database/baw057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paraskevopoulou M.D., Vlachos I.S., Karagkouni D., Georgakilas G., Kanellos I., Vergoulis T., Zagganas K., Tsanakas P., Floros E., Dalamagas T., et al. DIANA-LncBase v2: Indexing microRNA targets on non-coding transcripts. Nucleic Acids Res. 2016;44:D231–D238. doi: 10.1093/nar/gkv1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vlachos I.S., Zagganas K., Paraskevopoulou M.D., Georgakilas G., Karagkouni D., Vergoulis T., Dalamagas T., Hatzigeorgiou A.G. DIANA-miRPath v3.0: Deciphering microRNA function with experimental support. Nucleic Acids Res. 2015;43:W460–W466. doi: 10.1093/nar/gkv403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karagkouni D., Paraskevopoulou M.D., Chatzopoulos S., Vlachos I.S., Tastsoglou S., Kanellos I., Papadimitriou D., Kavakiotis I., Maniou S., Skoufos G., et al. DIANA-TarBase v8: A decade-long collection of experimentally supported miRNA-gene interactions. Nucleic Acids Res. 2018;46:D239–D245. doi: 10.1093/nar/gkx1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qiagen . Handbook. Hilden, Germany: 2015. [(accessed on 10 February 2020)]. RT2 Profiler PCR Array Data Analysis v3.5 Handbook; p. 24. Available online: https://geneglobe.qiagen.com/it/product-groups/rt2-lncrna-qpcr-assays. [Google Scholar]
- 25.Lisse T.S., Vadivel K., Bajaj S.P., Zhou R., Chun R.F., Hewison M., Adams J.S. The heterodimeric structure of heterogeneous nuclear ribonucleoprotein C1/C2 dictates 1,25-dihydroxyvitamin D-directed transcriptional events in osteoblasts. Bone Res. 2014;2:1–11. doi: 10.1038/boneres.2014.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu S., Sharma R., Nie D., Jiao H., Im H.J., Lai Y., Zhao Z., Zhu K., Fan J., Chen D., et al. ADAR1 ablation decreases bone mass by impairing osteoblast function in mice. Gene. 2013;513:101–110. doi: 10.1016/j.gene.2012.10.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gennari L., Bianciardi S., Merlotti D. MicroRNAs in bone diseases. Osteoporos. Int. 2017;28:1191–1213. doi: 10.1007/s00198-016-3847-5. [DOI] [PubMed] [Google Scholar]
- 28.Ell B., Kang Y. MicroRNAs as regulators of bone homeostasis and bone metastasis. Bonekey Rep. 2014;3:1–9. doi: 10.1038/bonekey.2014.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deng K., Wang H., Guo X., Xia J. The cross talk between long, non-coding RNAs and microRNAs in gastric cancer. Acta Biochim. Biophys. Sin. (Shanghai) 2015;48:111–116. doi: 10.1093/abbs/gmv120. [DOI] [PubMed] [Google Scholar]
- 30.Rashid F., Shah A., Shan G. Long Non-coding RNAs in the Cytoplasm. Genom. Proteom. Bioinform. 2016;14:73–80. doi: 10.1016/j.gpb.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang P., Xiong Q., Ge W., Zhang L. The role of MicroRNAs in osteoclasts and osteoporosis. RNA Biol. 2014;11:1355–1363. doi: 10.1080/15476286.2014.996462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Panach L., Mifsut D., Tarín J.J., Cano A., García-Pérez M.Á. Serum Circulating MicroRNAs as Biomarkers of Osteoporotic Fracture. Calcif. Tissue Int. 2015;97:495–505. doi: 10.1007/s00223-015-0036-z. [DOI] [PubMed] [Google Scholar]
- 33.Wu Q.Y., Li X., Miao Z.N., Ye J.X., Wang B., Zhang F., Xu R.S., Jiang D.L., Zhao M.D., Yuan F.L. Long Non-coding RNAs: A new regulatory code for osteoporosis. Front. Endocrinol. (Lausanne) 2018;9:1–8. doi: 10.3389/fendo.2018.00587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brincat S.D., Borg M., Camilleri G., Calleja-Agius J. The role of cytokines in postmenopausal osteoporosis. Minerva Ginecol. 2014;66:391–407. [PubMed] [Google Scholar]
- 35.Ginaldi L., Cristina M., Benedetto D., De Martinis M. Osteoporosis, inflammation and ageing. Immun. Ageing. 2005;2:1–5. doi: 10.1186/1742-4933-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Song J., Ahn C., Chun C.H., Jin E.J. A long non-coding RNA, GAS5, plays a critical role in the regulation of miR-21 during osteoarthritis. J. Orthop. Res. 2014;32:1628–1635. doi: 10.1002/jor.22718. [DOI] [PubMed] [Google Scholar]
- 37.Wang X., Zhao D., Zhu Y., Dong Y., Liu Y. Long non-coding RNA GAS5 promotes osteogenic differentiation of bone marrow mesenchymal stem cells by regulating the miR-135a-5p/FOXO1 pathway. Mol. Cell. Endocrinol. 2019;496:110534. doi: 10.1016/j.mce.2019.110534. [DOI] [PubMed] [Google Scholar]
- 38.Feng J., Wang J.X., Li C.H. LncRNA GAS5 overexpression alleviates the development of osteoporosis through promoting osteogenic differentiation of MSCs via targeting microRNA-498 to regulate RUNX2. Eur. Rev. Med. Pharmacol. Sci. 2019;23:7757–7765. doi: 10.26355/eurrev_201909_18985. [DOI] [PubMed] [Google Scholar]
- 39.Kelch S., Balmayor E.R., Seeliger C., Vester H., Kirschke J.S., Van Griensven M. MiRNAs in bone tissue correlate to bone mineral density and circulating miRNAs are gender independent in osteoporotic patients. Sci. Rep. 2017;7:1–12. doi: 10.1038/s41598-017-16113-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seeliger C., Karpinski K., Haug A.T., Vester H., Schmitt A., Bauer J.S., Van Griensven M. Five freely circulating miRNAs and bone tissue miRNAs are associated with osteoporotic fractures. J. Bone Miner. Res. 2014;29:1718–1728. doi: 10.1002/jbmr.2175. [DOI] [PubMed] [Google Scholar]
- 41.Doni A., Garlanda C., Mantovani A. Innate immunity, hemostasis and matrix remodeling: PTX3 as a link. Semin. Immunol. 2016;28:570–577. doi: 10.1016/j.smim.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grčević D., Sironi M., Valentino S., Deban L., Cvija H., Inforzato A., Kovačić N., Katavić V., Kelava T., Kalajzić I., et al. The long pentraxin 3 plays a role in bone turnover and repair. Front. Immunol. 2018;9:9. doi: 10.3389/fimmu.2018.00417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Parente R., Sobacchi C., Bottazzi B., Mantovani A., Grčevic D., Inforzato A. The Long Pentraxin PTX3 in Bone Homeostasis and Pathology. Front. Immunol. 2019;10:1–9. doi: 10.3389/fimmu.2019.02628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee E.-J., Song D.-H., Kim Y.-J., Choi B., Chung Y.-H., Kim S.-M., Koh J.-M., Yoon S.-Y., Song Y., Kang S.-W., et al. PTX3 Stimulates Osteoclastogenesis by Increasing Osteoblast RANKL Production. J. Cell. Physiol. 2014;229:1744–1752. doi: 10.1002/jcp.24626. [DOI] [PubMed] [Google Scholar]
- 45.Scimeca M., Salustri A., Bonanno E., Nardozi D., Rao C., Piccirilli E., Feola M., Tancredi V., Rinaldi A., Iolascon G., et al. Impairment of PTX3 expression in osteoblasts: A key element for osteoporosis. Cell Death Dis. 2017;8:e3125. doi: 10.1038/cddis.2017.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dou C., Li N., Ding N., Liu C., Yang X., Kang F., Cao Z., Quan H., Hou T., Xu J., et al. HDAC2 regulates FoxO1 during RANKL-induced osteoclastogenesis. Am. J. Physiol. Cell Physiol. 2016;310:C780–C787. doi: 10.1152/ajpcell.00351.2015. [DOI] [PubMed] [Google Scholar]
- 47.Pan J.X., Xiong L., Zhao K., Zeng P., Wang B., Tang F.L., Sun D., Guo H.H., Yang X., Cui S., et al. YAP promotes osteogenesis and suppresses adipogenic differentiation by regulating β-catenin signaling. Bone Res. 2018;6:18. doi: 10.1038/s41413-018-0018-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Iyer S., Ambrogini E., Bartell S.M., Han L., Roberson P.K., De Cabo R., Jilka R.L., Weinstein R.S., O’Brien C.A., Manolagas S.C., et al. FOXOs attenuate bone formation by suppressing Wnt signaling. J. Clin. Investig. 2013;123:3409–3419. doi: 10.1172/JCI68049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee W.C., Guntur A.R., Long F., Rosen C.J. Energy metabolism of the osteoblast: Implications for osteoporosis. Endocr. Rev. 2017;38:255–266. doi: 10.1210/er.2017-00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kovács B., Vajda E., Nagy E.E. Regulatory effects and interactions of the Wnt and OPG-RANKL-RANK signaling at the bone-cartilage interface in osteoarthritis. Int. J. Mol. Sci. 2019;20:4653. doi: 10.3390/ijms20184653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yarbrough M.L., Zhang K., Sakthivel R., Forst C.V., Posner B.A., Barber G.N., White M.A., Fontoura B.M.A. Primate-specific miR-576-3p sets host defense signalling threshold. Nat. Commun. 2014;5:1–10. doi: 10.1038/ncomms5963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Su N., Jin M., Chen L. Role of FGF/FGFR signaling in skeletal development and homeostasis: Learning from mouse models. Bone Res. 2014;2:1–24. doi: 10.1038/boneres.2014.3. [DOI] [PMC free article] [PubMed] [Google Scholar]