Abstract
Antiviral agents are drugs approved by the Food and Drug Administration (FDA) for the treatment or control of viral infections. Available antiviral agents mainly target stages in the viral life cycle. The target stages in the viral life cycle are; viral attachment to host cell, uncoating, synthesis of viral mRNA, translation of mRNA, replication of viral RNA and DNA, maturation of new viral proteins, budding, release of newly synthesized virus, and free virus in body fluids. At least half of available antiviral agents are for the treatment of human immunodeficiency virus (HIV) infections. The others are used mainly for the management of herpesviruses, hepatitis B virus (HBV), hepatitis C virus (HCV), and respiratory viruses.
Antiviral agents can be used for prophylaxis, suppression, preemptive therapy, or treatment of overt disease. Two important factors that can limit the utility of antiviral drugs are toxicity and the development of resistance to the antiviral agent by the virus. In addition, host phenotypic behaviors toward antiviral drugs because of either genomic or epigenetic factors could limit the efficacy of an antiviral agent in an individual. This article summarizes the most relevant pharmacologic and clinical properties of current antiviral agents, and targets for novel antiviral agents.
Keywords: antiviral agents, bioavailability, chemoprophylaxis, drug-resistance efficacy, excretion, half-life, infections, intracellular concentration, metabolism, nucleosides analogue, pharmacokinetics, therapeutic index, treatment, viral life cycle
Keywords: ALT, alanine aminotransferase; CMV, cytomegalovirus; CNS, central nervous system disease; CoV, coronavirus; CPK, creatinine phosphokinase; CSF, cerebrospinal fluid; CYP, cytochrome P450; dATP, deoxyadenosine triphosphate; dGTP, deoxyguanosine triphosphate; EBV, Epstein–Barr virus; FDA, Food and Drug Administration; FEV1, reduced forced expiratory volume; HAART, highly active antiretroviral therapy; HBeAg, hepatitis B e antigen; HBV, hepatitis B virus; HCV, hepatitis C virus; HHV-6, human herpes virus-6; HHV-7, human herpes virus-7; HHV-8, human herpes virus-8; HIV, human immunodeficiency virus; HPMPC, (S)-1-(3-hydroxy-2-phosphonylmethoxypropyl) cytosine; HPV, human papillomavirus; HSE, herpes simplex encephalitis; HSV, herpes simplex virus; IFNs, interferons; MNR, multinucleoside resistance; NA, neuraminidase; NAMs, nucleoside-analog-associated mutations; NK, natural killer; PEG, polyethylene glycol; Pgp, P-glycoprotein; RSV, respiratory syncytial virus; SARS, severe acute respiratory syndrome; SEM, skin, eye, or mouth; SPAG, small-particle aerosol generator; TAMs, thymidine analog resistance mutations; TK, thymidine kinases; UGT, UDP-glucuronosyl transferase; VZV, varicella zoster virus
Defining Statement
Antiviral agents are drugs approved by Food and Drug Administration (FDA) for the treatment or control of viral infections. They target stages in the viral life cycle. An ideal antiviral agent should be effective against both actively replicating and latent viruses; however, most of the available antiviral agents are effective against only replicating viruses.
Introduction
Antiviral agents are drugs approved by the Food and Drug Administration (FDA) for the treatment or control of viral infections. The development of antiviral agents is not trivial as viral replication is intricately linked with the host cell that any antiviral drug that interferes even to a lesser extent with host cell factors may be toxic to the host depending on the duration and dosage used. Available antiviral agents mainly target stages in the viral life cycle. The target stages in the viral life cycle are; viral attachment to host cell, uncoating, synthesis of viral mRNA, translation of mRNA, replication of viral RNA and DNA, maturation of new viral proteins, budding, release of newly synthesized virus, and free virus in body fluids. Antiviral agents used to treat viral diseases are currently limited, and at least half of the available agents are for the treatment of human immunodeficiency virus (HIV) infections. The others are used for the management of herpes simplex virus (HSV), varicella zoster virus (VZV), cytomegalovirus (CMV), hepatitis B virus (HBV), hepatitis C virus (HCV), respiratory syncytial virus (RSV), human papillomavirus (HPV), and influenza virus-related diseases.
Viruses could stay in the cells as episomal form, or are incorporated into host chromosomal DNA without engaging in active viral replication (i.e., viral latency state). An ideal antiviral agent should be effective against both actively replicating and latent viruses; however, most of the available antiviral agents are effective against only replicating viruses. The goals for treating acute viral infections in immunocompetent patients are to reduce the severity of the illness and its complications and to decrease the rate of transmission of the virus. The therapeutic index, or ratio of efficacy to toxicity, must be extremely high in order for the therapy to be acceptable. For chronic viral infections, the goal is to prevent viral damage to visceral organs, and therefore efficacy becomes paramount. Antiviral agents can be used for prophylaxis, suppression, preemptive therapy, or treatment of overt disease. Two important factors that can limit the utility of antiviral drugs are toxicity and the development of resistance to the antiviral agent by the virus. In addition, host phenotypic behaviors toward antiviral drugs because of either genomic or epigenetic factors could limit the efficacy of an antiviral agent in an individual. This article summarizes the most relevant pharmacologic and clinical properties of the available antiviral agents.
Therapeutics for Herpesvirus Infections
There are eight members of the human herpesviridae family: HSV-1, HSV-2, VZV, Epstein–Barr virus (EBV), CMV, human herpes virus-6 (HHV-6), human herpes virus-7 (HHV-7), and human herpes virus-8 (HHV-8). The hallmark of the herpesviruses is their ability to establish latency within the neuronal ganglia of the nervous system or cells of the immune system and reactivate during periods of stress, trauma, or immune suppression.
Acyclovir

Chemistry, mechanism of action, and antiviral activity
Acyclovir [9-(2-hydroxyethoxymethyl) guanine] is a synthetic acyclic purine nucleoside analogue that lacks the 3′-hydroxyl group of nucleosides. Acyclovir is phosphorylated to the active triphosphate metabolite that inhibits viral DNA synthesis (Figure 1). Viral encoded thymidine kinases (TK), present in only herpesvirus-infected cells, catalyze the phophorylation to acyclovir monophosphate. Host cell TK or other kinases cannot phosphorylate acyclovir to its monophosphate metabolite efficiently. Acyclovir is highly selective for cells engaged in active viral replication and does not affect noninfected cells. The monophosphate is subsequently phosphorylated to the di-, and triphosphate by cellular kinases, resulting in acyclovir triphosphate concentrations much higher in HSV-infected than in uninfected cells. Acyclovir triphosphate inhibits viral DNA synthesis by competing with deoxyguanosine triphosphate (dGTP) as a substrate for viral DNA polymerase, as illustrated in Figure 1. Since acyclovir triphosphate lacks the 3′-hydroxyl group required for DNA chain elongation, the growing chain of DNA is terminated. In addition, the incorporated acyclovir can trap viral DNA polymerase and prevent it from initiating other viral DNA replication. The viral polymerase has a greater affinity for acyclovir triphosphate than cellular DNA polymerase, resulting in little incorporation of acyclovir into cellular DNA. In vitro, acyclovir is most active against HSV-1 (average EC50 = 0.04 μg ml−1), HSV-2 (0.10 μg ml−1), and VZV (0.50 μg ml−1). Varicella virus is much less susceptible to acyclovir than is HSV, and hence, higher doses of acyclovir are required in the treatment of VZV infections. EBV TK has poor efficiency to utilize acyclovir as substrate, therefore, higher acyclovir concentrations are required for EBV inhibition. CMV, which lacks a virus-specific TK, is relatively resistant.
Figure 1.

The mechanism of action of acyclovir: (a) activation; (b) inhibition of DNA synthesis and chain termination.
The bioavailability of oral formulations of acyclovir is 15–30%. Peak concentrations of approximately 0.57 and 1.57 μg ml−1 are attained after multidose oral administration of 200 or 800 mg of acyclovir, respectively. Higher plasma acyclovir levels are achieved with intravenous administration. The plasma half-life is 2–3 h in older children and adults with normal renal function and 2.5–5 h in neonates with normal creatinine clearance. The elimination of acyclovir is prolonged in individuals with renal dysfunction, with a half-life of approximately 20 h in persons with end-stage renal disease. Acyclovir is minimally metabolized and approximately 85% is excreted unchanged in the urine via renal tubular secretion and glomerular filtration.
Clinical indications
For most of the clinical indications of acyclovir, valacyclovir and famciclovir are as effective, safe, and convenient alternatives. The clinical applications of valacyclovir and famciclovir are detailed in section ‘Clinical indications’ under ‘Valacyclovir’ and in section Clinical indications under ‘Penciclovir and Famciclovir’, respectively.
Genital herpes
Initial and recurrent episodes of genital HSV infection can be treated with acyclovir, and recurrent episodes can be suppressed with acyclovir. Topical acyclovir is not an effective treatment for genital HSV. Intravenous acyclovir (15 mg kg−1 day−1 in three divided doses for 5–7 days) is the most effective treatment for a first episode of genital herpes and results in a significant reduction in the median duration of viral shedding, pain, and time to complete healing (8 vs. 14 days) but is reserved for patients with systemic complications. Oral therapy (200 mg five times daily) is the standard treatment.
Recurrent genital herpes is less severe and resolves more rapidly than primary infection. Orally administered acyclovir (200 mg five times daily or 400 mg three times daily) for 7–10 days shortens the duration of signs and symptoms, virus shedding, and time to healing by 2, 7, and 4 days, respectively, when initiated within 24 h of onset of symptoms.
Oral acyclovir administration effectively suppresses recurrent genital herpes. Daily administration of acyclovir reduces the frequency of recurrences by up to 80%, and 25–30% of patients have no further recurrences while taking the drug.
Herpes labialis
Topical therapy for HSV-1 mouth or lip infections is of no clinical benefit. Orally administered acyclovir (200 or 400 mg five times daily for 5 days) reduces the time to loss of crust by approximately 1 day (7 vs. 8 days) but does not alter the duration of pain or time to complete healing.
Immunocompromised host
Immunocompromised individuals, such as those infected with HIV or transplant recipients, are afflicted with frequent and severe HSV infections. Clinical benefit from intravenous or oral acyclovir therapy is documented as evidenced by a significantly shorter duration of viral shedding and accelerated lesion healing. Oral acyclovir therapy in high doses in immunocompromised patients with herpes zoster is effective but valaciclovir is superior.
Herpes simplex encephalitis
HSV infection of the brain is the most common cause of sporadic fatal encephalitis in the United States. HSV-1 is predominantly the causative agent of herpes simplex encephalitis (HSE). Acyclovir at a dose of 10 mg kg−1 every 8 h (30 mg kg−1 day−1) for 10–14 days is the therapy of choice and reduces mortality from 70 to 19%. Furthermore, 38% of acyclovir recipients returned to normal neurologic function.
Neonatal HSV infection
Neonatal HSV infection is divided into three clinical categories: skin, eye, or mouth (SEM) disease, central nervous system (CNS) disease, and disseminated (if there is evidence of visceral involvement) HSV disease. The recommended treatment for neonatal herpes infection is 20 mg kg−1 every 8 h of parenteral acyclovir with duration dictated by the extent of disease; 14 days for SEM disease, 21 days for CNS and disseminated disease. For babies with SEM disease, 98% of acyclovir recipients developed normally 2 years after infection. For babies surviving encephalitis and disseminated disease, 43 and 57% of acyclovir recipients, respectively, developed normally.
Varicella
Varicella or chicken pox, is a common, highly contagious illness caused by VZV. It is primarily a disease of early childhood with 90% of cases occurring in children 1–14 years of age. Chicken pox is generally self-limiting in young children and is manifested by fever, mild constitutional symptoms, and an itchy, vesicular rash. The disease is more severe in neonates, adults, and immunocompromised individuals. Oral acyclovir therapy when initiated within 24 h of the onset of the rash reduces the duration of fever, and the number of maximum lesions in immunocompetent children. At present, the clinical importance of acyclovir treatment in otherwise healthy children, in whom chicken pox is self-limiting and results in few complications, remains uncertain. Furthermore, the widely use of the varicella vaccine to protect against VZV will make the use of acyclovir for immunocompetent children with chickenpox obsolete.
Acyclovir therapy of chicken pox in immunocompromised host substantially reduces morbidity and mortality. Intravenous acyclovir treatment (500 mg m−2 of body surface area or 10–12 mg kg−1 every 8 h for 7–10 days) improved the outcome, as evidenced by a reduction of VZV pneumonitis from 45 to <5%. Oral acyclovir therapy is not indicated for immunocompromised host with chicken pox. The bioavailability of valacyclovir makes it an attractive alternative.
Herpes zoster
Herpes zoster or singles is caused by the reactivation of VZV, which resides in a latent state in the sensory ganglia following primary varicella (chicken pox) infection. Acute herpes zoster is a painful, debilitating condition, especially in older adults. The risk of zoster-associated pain persisting after the healing of the rash correlates with increasing age. Intravenous acyclovir therapy of herpes zoster in the normal host produces some acceleration of the healing of the rash, and resolution of pain (both acute neuritis and zoster-associated pain). Oral acyclovir (800 mg five times a day) administration results in accelerated healing of the rash and reduction in the severity of acute neuritis. Oral acyclovir treatment of zoster ophthalmicus reduces the incidence of serious ocular complications such as keratitis and uveitis. Intravenous acyclovir therapy significantly reduces the frequency of cutaneous dissemination and visceral complications of herpes zoster in immunocompromised adults. Acyclovir is the standard therapy at a dose of 10 mg kg−1 (body weight) or 500 mg m−2 (body surface area) every 8 h for 7–10 days.
Resistance
The most common mechanism for conferring acyclovir resistance is mutations in the HSV genome resulting in a deficiency or alteration in viral TK activity. Occasionally, HSV strains are TK altered and maintain the ability to phosphorylate the natural substrate, thymidine, but selectively lose the ability to phosphorylate acyclovir. Mutation of the viral DNA polymerase gene resulting in failure to incorporate the acyclovir triphosphate in progeny DNA molecules is an alternate, but infrequent, mechanism that may result in HSV resistance to acyclovir.
Resistance to acyclovir is uncommon, with prevalence of 0.1–0.4% and 5–6% in immunocompetent and immunocompromised patients, respectively. Acyclovir-resistant isolates of VZV have been identified much less frequently than acyclovir-resistant HSV but have been recovered from marrow transplant recipients and AIDS patients. The acyclovir-resistant VZV isolates all had altered or absent viral TK function but remained susceptible to vidarabine and foscarnet, which do not require viral TK for their activity.
Adverse effect
Acyclovir therapy is associated with few adverse effects. The most common complaints associated with acyclovir therapy include nausea, diarrhea, and headache. Rapid infusions of intravenous acyclovir can result in reversible crystalline nephropathy. A few reports have linked intravenous acyclovir use with CNS disturbances, including agitation, hallucinations, disorientation, tremors, and myoclonus.
Data on outcomes from pregnant mothers exposed to acyclovir during pregnancy showed that the rate of birth defects did not exceed that expected in the general population and the pattern of defects did not differ from those in untreated women.
Valacyclovir

Chemistry, mechanism of action, and antiviral activity
Valacyclovir, is a prodrug of acyclovir (the l-valyl ester of acyclovir). Valacyclovir is rapidly metabolized into acyclovir and valine by the enzyme valacyclovir hydrolase (esterase) found in the brush border of the gastrointestinal tract, and the liver. Valacyclovir provides a high bioavailability of acyclovir, threefold to fivefold higher than that obtained with oral acyclovir, and is equivalent to plasma levels achieved with doses of intravenous acyclovir. The mechanism of action and antiviral activity spectrum of valacyclovir are similar to that as described for acyclovir.
Clinical indications
The antiviral spectrum of valacyclovir encompasses HSV-1, HSV-2, VZV, and CMV. It is effective for treatment of HSV-1 and HSV-2 infections in immunocompetent individuals; initial episode of genital herpes (1 g, twice daily for 10 days); episodic therapy for recurrent herpes labialis (2 g, twice a day for 1 day) and recurrent genital herpes (1 g or 500 mg, twice a day for 3–5 days); and suppression of recurrent genital herpes (1 g or 500 mg, once a day).
For immunocompromised patients, valacyclovir is effective for episodic therapy (1 g, twice a day for >5 days) and suppression of recurrent genital herpes (500 mg, twice a day, or 1 g, once a day). Valacyclovir (1 g, three times daily for 7–10 days) is superior to acyclovir for the reduction of pain associated with shingles.
Resistance
The mechanism of resistance to valacyclovir is similar to that of acyclovir.
Adverse effects
Valacyclovir has similar side effect profile as acyclovir; however, no crystalline nephropathy has been reported with its use.
Cidofovir

Chemistry, mechanism of action, and antiviral activity
Cidofovir, (S)-1-(3-hydroxy-2-phosphonylmethoxypropyl) cytosine (HPMPC), is an acyclic phosphonate nucleotide analogue of deoxycytidine monophosphate. Cidofovir has a single phosphate group attached therefore it does not require viral enzymes for conversion to the monophosphate, cellular kinases sequentially phosphorylate the monophosphate to its active triphosphate metabolite. The triphosphate metabolite then serves as a competitive inhibitor of DNA polymerase. The active form of the drug exhibits a 25- to 50-fold greater affinity for the viral DNA polymerase, compared with the cellular DNA polymerase, thereby selectively inhibiting viral replication. Owing to its unique phosphorylation requirements for activation, cidofovir usually maintains activity against acyclovir- and foscarnet-resistant HSV isolates, as well as ganciclovir- and foscarnet-resistant CMV mutants. Cidofovir is less potent than acyclovir in vitro; however, cidofovir persists in cells for prolonged periods, increasing drug activity. In addition, cidofovir produces active metabolites with long half-lives (17–48 h), permitting once weekly dosing. Cidofovir has in vitro activity against VZV, EBV, HHV-6, HHV-8, HPV, polyomaviruses, orthopoxviruses, and adenovirus. Unfortunately, cidofovir concentrates in kidney cells 100 times greater than in other tissues and produces severe proximal convoluted tubule nephrotoxicity when administered systemically. Cidofovir has limited and variable oral bioavailability (2–26%), therefore, it is administered intravenously.
Clinical indication
Cidofovir is licensed for treatment of CMV retinitis and has been used to treat acyclovir-resistant HSV infection. The dosing regimen is 5 mg kg−1 per week during the first 2 weeks, then 5 mg kg−1 every other week, with sufficient hydration and coadministration of oral probenecid to prevent nephrotoxicity. There are anecdotal reports that dividing the 5 mg kg−1 weekly dose into three doses given alternate days in a week may reduce renal toxicity substantially.
Resistance
The development of resistance with clinical use is uncommon; however, mutations in CMV DNA polymerase can mediate altered susceptibility.
Adverse effects
Nephrotoxicity is the principal adverse event associated with systemic administration of cidofovir, occurs in 30–50% of recipients. Other reported side effects include neutropenia, fever, diarrhea, nausea, headache, rash, anterior uveitis, and ocular hypotonia.
Foscarnet

Chemistry, mechanism of action, and antiviral activity
Foscarnet, is an inorganic pyrophosphate analogue of phosphonoacetic acid that inhibits all HHVs, including most ganciclovir-resistant CMV isolate and acyclovir-resistant HSV and VZV strains. It inhibits DNA polymerase by blocking the pyrophosphate-binding site and preventing cleavage of pyrophosphate from deoxynucleotide triphosphates. Unlike acyclovir, which requires activation by a virus-specific TK, foscarnet acts directly on the virus DNA polymerase. Thus, TK-deficient, acyclovir-resistant herpesviruses remain sensitive to foscarnet.
The oral bioavailability of foscarnet is about 20%. The cerebrospinal fluid (CSF) concentration of foscarnet is approximately two-thirds of the plasma level. Renal excretion is the primary route of clearance of foscarnet with >80% of the dose appearing in the urine. Bone sequestration also occurs, resulting in complex plasma elimination.
Clinical indications
The principal indications are CMV retinitis in AIDS patients, and mucocutaneous acyclovir-resistant (viral TK-deficient) or penciclovir-resistant HSV and VZV infections in immunocompromised patients.
Mucocutaneous HSV infections and those caused by VZV in immunocompromised host can be treated with foscarnet at dosages lower than that for the management of CMV retinitis.
Resistance
Isolates of HSV, CMV, and VZV resistant to foscarnet develop both in the laboratory and in the clinical setting. These isolates are all DNA polymerase mutants.
Adverse effects
Foscarnet toxicity includes mainly nephrotoxicity (acute tubular necrosis and interstitial nephritis), metabolic and hematologic abnormalities, and CNS side effects. Patients may develop isolated or combined hypomagnesemia, hypocalcemia, hypokalemia, and hypophosphatemia. CNS side effects include headache, seizures, irritability, tremor, and hallucination. Other reported side effects include fever, rash, painful genital ulcerations, diarrhea, nausea, and vomiting.
Ganciclovir and Valganciclovir


Chemistry, mechanism of action, and antiviral activity
Ganciclovir [9-(1,3-dihydroxy-2-propoxymethyl) guanine] is a nucleoside analogue that differs from acyclovir by having a hydroxymethyl group at the 3′ position of the acyclic side chain. It has 8–20 times greater in vitro activity against CMV, and as active as acyclovir against HSV-1 and HSV-2 and almost as active against VZV. Like acyclovir, the first step of phosphorylation to ganciclovir monophosphate in herpesvirus-infected cells depends on virus-encoded enzymes. In cells infected by HSV-1 or HSV-2, TK catalyzes the phosphorylation of ganciclovir to ganciclovir monophosphate. Because CMV lacks the gene for TK, the enzyme that catalyzes the initial phosphorylation of ganciclovir in CMV-infected cells is the phosphotransferase encoded by UL97 gene. The final phosphorylation steps to the di- and triphosphate is by cellular kinases. Ganciclovir triphosphate serves as a competitive inhibitor of herpes viral DNA polymerase and inhibits the incorporation of guanosine triphosphate into viral DNA. Incorporation of ganciclovir triphosphate into the growing viral chain results in slowing and subsequent cessation of DNA chain elongation. Intracellular ganciclovir triphosphate concentrations are at least tenfold higher in CMV-infected cells than uninfected cells.
The oral bioavailability of ganciclovir is poor (5–7%). Concentrations of ganciclovir in biologic fluids, including aqueous humor and CSF, are less than plasma levels. The plasma elimination half-life is 2–4 h for individuals with normal renal function. The kidney is the major route of clearance of ganciclovir, and therefore, impaired renal function requires adjustment of dosage. The pharmacokinetics of ganciclovir in neonates is similar to that in adults.
Valganciclovir, l-valine ester of ganciclovir, serves as oral prodrug of ganciclovir. Valganciclovir is orally bioavailable (approximately 60%) and is rapidly converted to ganciclovir after absorption. Its mechanism of action and spectrum of activity are similar to that of ganciclovir. Oral valganciclovir can be given in doses that result in serum levels that approximate ganciclovir serum levels achieved with intravenous ganciclovir. Oral valganciclovir is convenient to use and may replace intravenous ganciclovir for initial and maintenance treatment.
Clinical indications
Ganciclovir is approved for treatment and chronic suppression of CMV retinitis in AIDS or other immunocompromised patients, and prophylaxis or preemptive treatment of CMV infection in high-risk transplant recipients. It is also effective for CMV syndromes, including CMV pneumonia, CMV colitis, and gastrointestinal infection in AIDS and transplant patients. In immunocompromised patients, therapy with ganciclovir requires an induction and maintenance phases. The induction dose is 10 mg kg−1 day−1 in two divided doses given for 14–21 days, and a maintenance dose of 5 mg kg−1 day−1 given once daily for 5–7 days per week. Oral valganciclovir dosage is 900 mg twice a day, and 900 mg once a day for induction and maintenance therapy, respectively.
Gancoclovir has been evaluated in the treatment of neonates congenitally infected with CMV. In a phase III randomized controlled trial, ganciclovir therapy (6 mg kg−1 per dose administered twice a day for 6 weeks) protected infants from hearing deterioration beyond one year of life. However, because of the potential toxicity of long-term ganciclovir therapy, additional studies are necessary before a recommendation can be made in the use of ganciclovir for congenital CMV infection.
Resistance
In immunocompromised patients receiving prolong therapy, the prevalence of resistance exceeds 8%. There are two mechanisms of resistance by CMV to ganciclovir: (1) The alteration of the CMV phosphonotransferase (coded by CMV UL97 gene) reduces intracellular phosphorylation of ganciclovir, and (2) mutations in the CMV DNA polymerase (coded by CMV UL54 gene). Resistance is associated with decreased sensitivity up to 20-fold. Occasionally, strains of HSV that are resistant to acyclovir because of TK deficiency are also much less sensitive to ganciclovir.
Adverse effects
The most important side effects of ganciclovir therapy are the development of neutropenia, and thrombocytopenia. Neutropenia occurs in approximately 24–38% of patients. The neutropenia is usually reversible with dosage adjustment of ganciclovir, or withholding of treatment. Thrombocytopenia occurs in 6–19% of patients.
Ganciclovir has gonadal toxicity in animal models, most notably as a potent inhibitor of spermatogenesis. It causes an increased incidence of tumors in the preputial gland of male mice, a finding of unknown significance. As an agent affecting DNA synthesis, ganciclovir has carcinogenic potential.
Penciclovir and Famciclovir


Chemistry, mechanism of action, and antiviral activity
Penciclovir [9-(4-hydroxy-3-hydroxymethylbut-1-yl)] a guanine nucleoside analogue is structurally similar to ganciclovir, differing only be the substitution of a methylene bridge for the ether oxygen in the acyclic ribose part of the molecule. Its metabolism and mechanism of action are similar to those of acyclovir, except that it is not an obligate DNA-chain terminator. The in vitro inhibitory effects of penciclovir on HSV-1, HSV-2, and VZV are similar to those of acyclovir. The oral bioavailability of penciclovir is poor (<5%). Famciclovir, a prodrug of penciclovir with improved bioavailability (approximately 77%), is the diacetyl ester of 6-deoxy penciclovir [9-(4-hydroxy-3-hydroxymethylbut-1-yl)-6-deoxyguanine]. It is well absorbed after oral administration and is rapidly metabolized to penciclovir by deacetylation in the gastrointestinal tract, and liver, after which it is oxidized by the liver at the position 6 of the purine ring. Penciclovir is phosphorylated more efficiently than acyclovir in HSV- and VZV-infected cells. Host cell kinases phosphorylate both penciclovir and acyclovir to a small but comparable extent. The preferential metabolism in HSV- and VZV-infected cells is the major determinant of its antiviral activity. Penciclovir triphosphate has, on average, a tenfold longer intracellular half-life than acyclovir triphosphate in HSV-1-, HSV-2-, and VZV-infected cells after drug removal. Because penciclovir is more stable, it has longer antiviral activity, allowing for less frequent dosing. Both compounds have good activity against HSV-1, HSV-2, and VZV. Penciclovir, like acyclovir, is relatively inactive against CMV and EBV. Penciclovir is active against hepatitis B.
Penciclovir is eliminated rapidly and almost unchanged by active tubular secretion and glomerular filtration by the kidneys. The elimination T 1/2 in healthy subjects is approximately 2 h.
Clinical indications
Famciclovir is available in an oral preparation for treatment of HSV-1, HSV-2, and VZV infections. It is used in the treatment of the following conditions: initial episodes of genital herpes (250 mg, three times a day for 10 days), episodic treatment of recurrent genital herpes (125 mg, twice a day for 5 days), suppression of recurrent genital herpes (250 mg, twice a day), and for shingles (500 mg, every 8 h for 7 days). For immunocompromised patients, famciclovir is efficacious for episodic treatment of recurrent genital herpes (500 mg, twice a day for 7 days). Compared with acyclovir, famciclovir is as effective, safe, and well tolerated in the treatment of HSV infections in HIV-infected individuals. Famciclovir is also at least as effective as acyclovir for ophthalmic zoster and for shingles and acute zoster pain in immunocompromised patients. Compared with valacyclovir, famciclovir is as effective, safe, and convenient in the treatment of zoster.
Penciclovir is available as a 1% cream for topical therapy of mucocutaneous HSV infections, particularly recurrent herpes labialis (cold sores). Topical penciclovir 1% is approved for episodic therapy of herpes labialis and applied every 2 h during waking hours for 4 days. It accelerates lesion healing and resolution of pain by about 1 day. It is available over-the-counter in many countries.
Resistance
HSV and VZV isolates resistant to penciclovir have been identified in the laboratory. Resistance is attributed to alterations or deficiencies of TK and DNA polymerase.
Adverse effects
Therapy with oral famciclovir is well tolerated, being associated only with headache, diarrhea, and nausea. Preclinical studies of famciclovir indicated that chronic administration was tumorigenic (murine mammary tumors) and causes testicular toxicity in other rodents.
Idoxuridine and Trifluorothymidine


Chemistry, mechanism of action, and antiviral activity
Idoxuridine (5-iodo-2′-deoxyuridine), and trifluorothymidine (5-trifluoromethyl-2′-deoxyuridine) are thymidine analogue. When administered systemically, these nucleosides are phosphorylated by both viral and cellular kinases to active triphosphate derivatives, which inhibit both viral and cellular DNA synthesis. Parenteral administration results in potent antiviral activity but also sufficient host cytotoxicity to prevent the systemic use of these drugs. The toxicity of these compounds is not significant when applied topically to the eye in the treatment of HSV keratitis. Both idoxuridine and trifluorothymidine are effective and licensed for treatment of HSV keratitis. Topically applied idoxuridine or trifluorothymidine will penetrate cells of the cornea. Low levels of drugs can be detected in the aqueous humor.
Clinical indications
Trifluorothymidine is the most efficacious of these compounds, and the treatment of choice for HSV keratitis (1 drop of 1% ophthalmic solution instilled in each eye, up to nine times a day). Idoxuridine was the first antiviral compound to receive FDA approval in 1963 for treatment of HSV keratitis.
Resistance
Trifluorothymidine-resistant HSV strains with altered TK substrate specificity have been selected for in vitro. However, clinical significant resistance has not been established.
Adverse effects
The ophthalmic preparation of idoxuridine and trifluorothymidine causes local discomfort, irritation, photophobia, edema of the eyelids, and less commonly, hypersensitivity reactions as well as superficial punctate or epithelial keratopathy.
Vidarabine

Chemistry, mechanism of action, and antiviral activity
Vidarabine (vira-A, adenine arabinoside, and 9-d-arabinofuranosyl adenine) is active against HSV, VZV, and CMV. Vidarabine is a purine nucleoside analogue that is phosphorylated intracellularly to its mono-, di-, and triphosphate derivatives. Thus, unlike acyclovir, conversion of vidarabine to its active intracellular derivative does not require viral enzymes at any of the phosphorylation steps. The triphosphate derivative competitively inhibits DNA dependent DNA polymerases of some DNA viruses approximately 40 times more than those of host cells. In addition, vira-A is incorporated into terminal positions of both cellular and viral DNA, thus inhibiting elongation. Viral DNA synthesis is blocked at lower doses of drug than is host cell DNA synthesis, resulting in a relatively selective antiviral effect. However, large doses of vira-A are cytotoxic to dividing host cells.
The use of vidarabine was replaced by acyclovir because of poor solubility and toxicity. It is no longer available as an intravenous formulation. However, vidarabine should be recognized historically as the first antiviral agent licensed in 1977 for systemic treatment.
Clinical indications
Although trifluorothymidine is the antiviral agent of choice for the topical treatment of HSV keratitis, in patients in whom trifluorothymidine cannot be used vidarabine is a suitable alternative. Topical vidarabine is superior to idoxuridine in the treatment of HSV ocular infections.
Resistance
Resistance to vidarabine is conferred by mutations in the viral DNA polymerase gene. The degree of maximal resistance to vidarabine is fourfold, much lower than the 100-fold resistance to acyclovir with similar DNA polymerase resistant mutations. Acyclovir-resistant clinical HSV isolates are always susceptible in vitro to vidarabine.
Adverse effects
Ocular toxicity consists of occasional hyperemia and increased tearing, both of low incidence.
Fomivirsen
Chemistry, mechanism of action, and antiviral activity
Fomivirsen is a 21-nucleotide phosphorothioate oligonucleotide that inhibits CMV replication through an antisense mechanism. Its oligonucleotide sequence (5′-GCG TTT GCT CTT CTT CTT GCG-3′) is complementary to a sequence in mRNA transcripts of the major immediate early region 2 (IE2) of CMV, which encodes for several proteins responsible for the viral gene expression that are essential for the production of infectious viral particles. Binding of fomivirsen to the target mRNA results in inhibition of IE2 protein synthesis, with subsequent inhibition of viral replication. In vitro, fomivirsen inhibits CMV replication in a dose-dependent manner, with a mean IC50 of between 0.03 and 0.2 μmol l−1. Pharmacokinetic assessment of fomivirsen in humans after intraocular administration is limited. In a rabbit model, intraocular administration revealed first-order kinetics with half-life of 62 h. Fomivirsen is cleared from the vitreous in rabbits during the course of 7–10 days by a combination of tissue distribution and metabolism. No systemic absorption has been observed after intravitreal administration in humans.
Clinical indications
Fomivirsen is indicated for use in HIV patients with CMV retinitis who are intolerant of or have contraindication to other treatment for CMV retinitis or in whom the disease is recalcitrant to ganciclovir or cidofovir treatment. It has activity against cidofovir- and ganciclovir-resistant strains of CMV.
Resistance
CMV strains with tenfold decreased susceptibility have been selected in vitro. However, no resistant clinical isolates have been reported.
Adverse effects
Adverse events of fomivirsen are uveitis, including iritis and vitritis, occurring in approximately 25% of patients. These reactions are usually transient or reversible with topical corticosteroids treatment.
New Prospects for Therapy of Herpesvirus Infections
While several classes of compounds are being investigated for the treatment of herpesvirus infections. Some of the compounds that have been the focus of drug discovery in the last decade have been targets of viral encoded enzymes, including inhibitors of ribonucleotide reductase, TK, protease, and DNA polymerase.
Recently, a new compound class of helicase–primase inhibitors, for example, BAY 57-1293, with preclinical pharmacological profile that outperforms the current standard HSV treatment represented by acyclovir, valacyclovir and famciclovir in standard animal models with respect to all parameters of efficacy, has been discovered. This class of compounds bind to two viral targets simultaneously, namely the helicase and primase subunit of the helicase–primase enzyme complex. The helicase–primase complex is essential for the HSV DNA replication process. These compounds have no demonstrable activity against either VZV or CMV.
Therapeutics for Respiratory Virus Infections
Amantadine and Rimantadine


Chemistry, mechanism of action, and antiviral activity
Amantadine (1-adamantanamine hydrochloride) and rimantadine (α-methyl-1-adamantanemethylamine hydrochloride) are symmetric tricyclic amines with narrow spectrum of activity, being useful only against influenza A infections. Rimantadine is fourfold to tenfold more active than amantadine. The mechanism of action of these drugs relates to the influenza A virus M2 protein, an integral transmembrane protein that functions as an ion channel for this virus and is activated by pH. The drop in pH accompanying the hydrogen flux facilitates the dissociation of the M2 protein from the ribonucleoprotein complexes so that the ribonucleoprotein can enter the cell nucleus and initiate replication. By interfering with the function of the M2 protein, amantadine and rimantadine inhibit the acid-mediated dissociation of the matrix protein from the ribonuclear protein complex within endosomes. This event occurs early in the viral replication cycle. The consequences of these drugs are the potentiation of acidic pH-induced conformational changes in the viral hemagglutinin during its intracellular transport.
Absorption of rimantadine is slower compared with that of amantadine. Amantadine is excreted unchanged in the urine by glomerular filtration and, likely, tubular secretion. The plasma elimination T 1/2 is approximately 12–18 h in individuals with normal renal function. However, the elimination T 1/2 increases in the elderly with impaired creatinine clearance. Rimantadine is extensively metabolized following oral administration, with an elimination T 1/2 of 24–36 h. Approximately 15% of the dose is excreted unchanged in the urine.
Clinical indications
Amantadine and rimantadine are licensed both for the chemoprophylaxis and treatment of influenza A infections. Prophylaxis with either drug prevents approximately 50–60% of infections and 70–90% of clinical illnesses caused by type A influenza virus. This degree of prophylactic effectiveness approximates that of inactivated influenza vaccine. Because of a lower incidence of side effects associated with rimantadine, it is used preferentially. Rimantadine can be given to any unimmunized member of the general population who wishes to avoid influenza A, but prophylaxis is especially recommended for control of presumed influenza outbreaks in institutions housing high-risk persons. High-risk individuals include adults and children with chronic disorders of the cardiovascular or pulmonary systems. Prophylaxis also is indicated if the vaccine may be ineffective because the epidemic strain differs substantially from the vaccine strain of influenza A, and for the 2 weeks after vaccination if influenza A already is active in the community.
Amantadine and rimantadine also have been shown to be effective in treatment of influenza A infections in adults and children if treatment is initiated within 48 h of the onset of symptoms. Drug therapy results in reduction in the duration of viral excretion, fever, and other systemic complaints, as well as earlier resumption of normal activities, in comparison with placebo. On average, the duration of illness is shortened by about 1 day. Amantadine and rimantadine are given orally at 200, and 300 mg day−1, respectively.
Resistance
Resistance to amantadine and rimantadine results from point mutations in the RNA sequence encoding for the M2 protein transmembrane domain. Resistance typically appears in the treated subjects within 2–3 days of initiating therapy. About 25–35% of treated patients shed resistant strains by the 5th day of treatment. The clinical significance of isolating resistant strains from the treated subject is not clear; infection and illness in immunocompetent people infected with a drug-resistant virus are similar to those in patients infected with drug-sensitive virus.
Adverse effects
Although the spectrum of adverse events associated with amantadine and rimantadine are qualitatively similar, they are less frequent and less severe with rimantadine. Amantadine is reported to cause side effects in 5–10% of healthy young adults taking the standard adult dose of 200 mg day−1. These side effects are usually mild and cease soon after amantadine is discontinued, although they often disappear with continued use of the drug. CNS side effects, which occur in 5–33% of patients, are most common and include difficulty in thinking, confusion, lightheadedness, hallucinations, anxiety, and insomnia. More severe adverse effects (e.g., mental depression and psychosis) are usually associated with doses exceeding 200 mg daily. About 5% of patients complain of nausea, vomiting, or anorexia. CNS adverse effects associated with rimantadine administration are significantly less; however, rimantadine has been associated with exacerbations of underlying seizure disorders.
Zanamivir and Oseltamivir
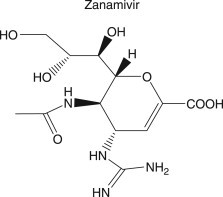

Chemistry, mechanism of action, and antiviral activity
Zanamivir (4-guanidino-2,3-dideoxy-2,3-didehydro-N-acetylneuraminic acid), and oseltamivir [ethyl ester of (3R,4R,5S)-4-scetamido-5-amino-3-(1-ethylpropoxyl)-1-cyclohexane-1-carboxylic acid] are sialic acid analogue that competitively inhibit influenza virus neuraminidase (NA). Influenza virus NA is located on the surface of the virus and is responsible for cleaving terminal sialic acid residues, which are essential for the release of the virus from infected cells, viral aggregation, and spread within the respiratory tract. Influenza NA also decreases viral inactivation by respiratory mucous. The lipophilic side chain of zanamivir and oseltamivir binds to the influenza virus NA, blocking its ability to cleave sialic acid residues. Zanamivir and oseltamivir are effective against both influenza A and influenza B.
Zanamivir has poor oral bioavailability and therefore it is administered by oral inhalation. More than 75% of an orally inhaled dose of zanamivir is deposited in the oropharynx, approximately 13% of this is distributed to the airways and lungs. Local respiratory mucosal concentrations of zanamivir exceeds 1000 ng ml−1 in sputum for 6 h after inhalation (i.e., over and above the concentration required to inhibit influenza A and B viruses). Approximately 10% of inhaled dose is absorbed systemically; peak serum concentrations range from 17 to 142 ng ml−1 within 2 h of administration of a 10 mg dose. The plasma T 1/2 is between 2.5 and 5 h. Systemically absorbed zanamivir is excreted unchanged in the urine. Although serum concentrations of zanamivir increase with decreasing creatinine clearance, no adjustment in dosing is necessary for renal insufficiency because of the limited amount of systemically absorbed drug.
Oseltamivir is an ethyl ester prodrug that, following hydrolysis by hepatic esterases, is converted to the active compound, oseltamivir carboxylate. Approximately 75% of orally administered oseltamivir reaches the systemic circulation in the form of oseltamivir carboxylate. Oseltamivir carboxylate is eliminated unchanged by renal excretion through glomerular filtration and tubular secretion. The elimination T 1/2 of oseltamivir carboxylate is 6–10 h. Serum concentrations of the drug increase in the presence of declining renal function, and dose adjustment is recommended in patients with renal insufficiency.
Clinical indications
Zanamivir and oseltamivir are used for treatment and prevention of influenza A and B infections. Treatment of otherwise healthy adults and children with zanamivir and oseltamivir reduces the duration of symptoms by 0.4 and 1 days, and provides 29–43% relative reduction in the odds of complications when given within 48 h of onset of symptoms. These drugs also significantly diminish viral replication in respiratory secretions. Zanamivir is available as dry powder for inhalation using a breath-activated Diskhaler delivery system. The recommended dose of zanamivir in patients >7 years is 10 mg twice daily for 5 days, while oseltamivir is given at 75 mg twice a day for 5 days.
Inhaled zanamivir, 10 mg once daily given for 4 weeks as seasonal prophylaxis, reduces the likelihood of laboratory confirmed influenza (with or without symptoms) by 34%, influenza disease by 67%, and influenza disease with fever by 84%. Oseltamivir administered for 6 weeks during the peak of influenza season significantly reduces the risk of contracting influenza. The protective efficacy of oseltamivir in preventing culture-proven influenza is about 90%.
Resistance
Viruses resistant to zanamivir and oseltamivir have been generated after in vitro passage in cell culture. Clinical influenza virus isolates with reduced susceptibility to both NA inhibitors have been reported. There are two mechanisms of resistance: mutations in the hemagglutin receptor-binding site, and mutations in the conserved portions of the NA enzyme active site. In general, resistant viruses with mutations in the NA enzyme are thought to have decreased infectivity and fitness and therefore less likely to be transmitted.
Adverse effects
Both NA inhibitors are generally well tolerated. Adverse events following administration of oseltamivir have primarily been gastrointestinal with nausea and vomiting occurring in some patients. Inhalation of zanamivir has resulted in bronchospasm and reduced forced expiratory volume (FEV1). Zanamivir should be used with caution in individuals with reactive airway diseases or chronic obstructive pulmonary diseases.
Ribavirin

Chemistry, mechanism of action, and antiviral activity
Ribavirin (α-methyl-1-adamantane methylamine hydrochloride) has antiviral activity against a variety of RNA and DNA viruses. Ribavirin is a nucleoside analogue whose mechanisms of action are poorly understood and probably not the same for all viruses; however, its ability to alter nucleotide pools and the packaging of mRNA appears important. This process is not virus specific, but there is a certain selectivity, in that infected cells produce more mRNA than noninfected cells. A major action is the inhibition by ribavirin-5′-monophosphate of inosine monophosphate dehydrogenase, an enzyme essential for DNA synthesis. This inhibition may have direct effects on the intracellular level of GMP and other nucleotide levels may be altered. The 5′-triphosphate of ribavirin inhibits the formation of the 5′-guanylation capping on the mRNA of vaccinia and Venezuelan equine encephalitis viruses. In addition, the triphosphate is a potent inhibitor of viral mRNA (guanine-7) methyltransferase of vaccinia virus. The capacity of viral mRNA to support protein synthesis is markedly reduced by ribavirin. Ribavirin may inhibit influenza A RNA-dependent RNA polymerase.
Ribavirin can be administered orally (bioavailability of approximately 40–45%) or intravenously. Aerosol administration has become standard for the treatment of RSV infections in children. Oral doses of 600 and 1200 mg result in peak plasma concentrations of 1.3 and 2.5 μg ml−1, respectively. Intravenous dosages of 500 and 1000 mg result in 17 and 24 μg ml−1 plasma concentrations, respectively. Aerosol administration of ribavirin results in plasma levels that are a function of the duration of exposure. Although respiratory secretions will contain milligram quantities of drug, only microgram quantities (0.5–3.5 μg ml−1) can be detected in the plasma.
The kidney is the major route of clearance of drug, accounting for approximately 40%. Hepatic metabolism also contributes to the clearance of ribavirin. Notably, ribavirin triphosphate concentrates in erythrocytes and persists for a month or longer. Likely, the persistence of ribavirin in erythrocytes contributes to its hematopoietic toxicity.
Clinical indications
Respiratory syncytial virus
Ribavirin is licensed for the treatment of carefully selected, hospitalized infants and young children with severe lower respiratory tract infections caused by RSV. Use of aerosolized ribavirin in adults and children with RSV infections reduced the severity of illness and virus shedding. However, placebo controlled trials have failed to demonstrate a consistent decrease in need for mechanical ventilation, duration of stay in intensive care unit, or duration of hospitalization among ribavirin recipients. The use of ribavirin for the treatment of RSV infections is controversial and remains discretionary. The most common adverse events following aerosol administration of ribavirin include bronchospasm and malfunction of ventilator delivery systems. The usual dosage of aerosolized ribavirin is 20 mg ml−1 of drug instilled in a small-particle aerosol generator (SPAG) and administered for 12–22 h day−1 for 3–6 days. To avoid potential exposure of health care workers to ribavirin, special containment delivery system in an isolation room with negative pressure is used.
Hepatitis C
Oral ribavirin in combination with interferon-α (IFN-α) is recommended for hepatitis C infection.
Lassa fever and hemorrhagic fever
Systemic ribavirin has demonstrated efficacy in the management of life-threatening infections caused by Lassa fever and hemorrhagic fever with renal syndrome. Oral ribavirin is recommended for prophylaxis against Lassa fever in exposed contacts.
Resistance
Treatment failures with ribavirin occur in some patients; however, resistance to ribavirin has not been identified as a clinical problem.
Adverse effects
Adverse effects attributable to aerosol therapy with ribavirin of infants with RSV include bronchospasm, pneumothorax in ventilated patients, apnea, cardiac arrest, hypotension, and concomitant digitalis toxicity. Pulmonary function test changes after ribavirin therapy in adults with chronic obstructive pulmonary disease have been noted. Reticulocytosis, rash, and conjunctivitis have been associated with the use of ribavirin aerosol. When given orally or intravenously, transient elevations of serum bilirubin and the occurrence of mild anemia have been reported. Ribavirin has been found to be teratogenic and mutagenic in preclinical testing. Its use is contraindicated in women who are or may become pregnant during exposure to the drug. Concern has been expressed about the risk to persons in the room of infants being treated with ribavirin aerosol, particularly females of childbearing age. Although this risk seems to be minimal with limited exposure, awareness and caution are warranted and, therefore, the establishment of stringent precautions for administration of ribavirin.
New Prospects for Therapy of Respiratory Viruses
While influenza pandemics have long posed a threat to humankind, a threat realized to varying extents in 1918, 1957, and 1968, particular concern has mounted of late due to continued sporadic human cases of H5N1 avian influenza in Southeast Asia, Eastern Europe, and Africa. Amantadine and rimantadine are not recommended for seasonal or avian influenza because circulating influenza A viruses as well as the H5N1 strains affecting humans in Southeast Asia are resistant to these medications. Zanamivir and oseltamivir are the only available options. To expand the antiviral drug arsenal against influenza, researchers have been testing a number of investigational agents, including peramivir and T-705. Although peramivir is a NA inhibitor administered intramuscularly. Preclinical studies in mice and ferrets revealed that the drug could protect 80% or more of animals exposed to pathogenic H5N1 influenza virus compared with 36% of untreated animals. T-705 is a viral RNA polymerase inhibitor in the preclinical testing stage.
The outbreak in 2003 of a novel coronavirus infection, which causes severe acute respiratory syndrome (SARS), underscores the need for antiviral drugs for the control of future SARS outbreaks. New insights into the field of SARS pathogenesis and SARS-coronavirus (CoV) genome structure have revealed novel potential therapeutic targets for antiviral therapy.
Therapeutics for Hepatitis
Interferons
Chemistry, mechanism of action, and antiviral activity
IFNs are glycoprotein cytokines (intercellular messengers) with a complex array of immunomodulating, antineoplastic, and antiviral properties. IFNs are currently classified as α, β, or γ, the natural sources of which, in general, are leukocytes, fibroblasts, and lymphocytes, respectively. Each type of IFN can be produced through recombinant DNA technology. The binding of IFN to the intact cell membrane is the first step in establishing an antiviral effect. IFN binds to the cellular receptors and activates secondary messengers to initiate production of multiple proteins, which are pivotal for the defense of the cell against viruses. The mechanism of action is rather complex. The antiviral effects of IFN include degradation of viral mRNA, inhibition of viral protein synthesis, and prevention of the viral infection of cells. The immunomodulating effects of IFN include enhancement of antigen presentation by HLA I and II to the immune system, activation of natural killer (NK) cells and other immune cells, and increased cytokine production. IFNs are active against a wide spectrum of viruses with RNA viruses being more sensitive than DNA viruses.
IFNs are not orally bioavailable and are administered intramuscularly or subcutaneously (including into a lesion). There appears to be some variability in absorption between each of the three classes of IFN and, importantly, resultant plasma levels. Absorption of IFN-α is more than 80% complete after intramuscular or subcutaneous injection. Plasma levels are dose dependent, peaking 4–8 h after administration and returning to baseline between 18 and 36 h. However, the antiviral activity peaks at 24 h and then slowly decreases to baseline over about 6 days. IFN is eliminated by inactivation in various body fluids and metabolism in a number of organs. Negligible amounts are excreted in the urine unchanged.
IFN-α molecule covalently bonded to polyethylene glycol (PEG) improves the pharmacokinetic profile of IFN markedly. The pegylated forms of IFN-α (Peg-IFN-α) offer a more convenient once weekly instead of daily administration, are licensed for the treatment of hepatitis B and C.
Clinical indications
Hepatitis B
The major goals of therapy for hepatitis B are to prevent progression of the disease to cirrhosis, end stage liver disease or hepatocellular carcinoma. Three generally accepted indications for treatment are: (1) positive test for HBV DNA, (2) positive hepatitis B e antigen (HBeAg), and (3) alanine aminotransferase (ALT) level greater than two times normal. Treatment end points differ in HBeAg positive, and HBeAg negative disease. However, suppression of HBV replication to levels less than 1 × 104 copies per ml (2000 IU ml−1) is regarded as a surrogate of treatment success with a resultant improvement in serum ALT and hepatic necroinflammatory disease.
Hepatitis B DNA polymerase level, a marker of replication, is reduced with standard IFN therapy. Clearance of serum HBeAg and HBV DNA polymerase occurs with treatment (30–40%). The use of pegylated forms of IFN has become common with the convenience of weekly dosing. Genotype and other baseline factors affect the response to PEG-IFN-α2a in HBeAg-positive chronic hepatitis B. Patients with genotypes A and B have a better response in comparison with genotypes C and D patients.
Hepatitis C
The aim of therapy for chronic HCV infection is to decrease and ultimately prevent progressive liver damage leading to cirrhosis, liver failure, or hepatocellular carcinoma. Therapy for chronic HCV infection is indicated in patients with detectable HCV RNA viral load and persistently elevated ALT. Findings of cirrhosis, fibrosis, or even moderate inflammation on liver biopsy support the choice of therapeutic intervention; however, biopsy is not mandatory prior to treatment initiation. Standard IFN, either as monotherapy or in combination with ribavirin, has been used extensively for HCV infections. Combination therapy for 40 weeks resulted in sustained responses in more than 60% of patients. The standard treatment of HCV infection is either PEG-IFN-α2a or PEG-IFN-α2b given alone or in combination with ribavirin. Genotypes 1 and 4 infections are associated with lower sustained virologic response than other HCV genotypes.
Resistance
Resistance to administered IFN has not been documented although neutralizing antibodies to recombinant IFNs have been reported. The clinical importance of this latter observation is unknown.
Adverse effects
Side effects are frequent with IFN (both standard and pegylated) administration and are usually dose limiting. Influenza-like symptoms (i.e., fever, chills, headache, and malaise) commonly occur, but these symptoms usually become less severe with repeated treatments. Leukopenia is the most common hematologic abnormality, occurring in up to 26% of treated patients. Leukopenia is usually modest, not clinically relevant, and reversible upon discontinuation of therapy. Increased ALT levels may also occur as well as nausea, vomiting, and diarrhea. At higher doses of IFN, neurotoxicity is encountered, as manifested by personality changes, confusion, attention deficits, disorientation, and paranoid ideation.
Lamivudine
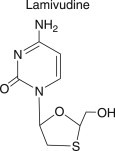
Chemistry, mechanism of action, and antiviral activity
Lamivudine is the (–) enantiomer of a cytidine analogue with sulfur substituted for the 3′ carbon atom in the furanose ring [(–) 2′,3′-dideoxy, 3′-thiacytidine]. It has significant activity in vitro against both HIV-1 and HIV-2 as well as HBV. Lamivudine is phosphorylated to the triphosphate metabolite by cellular kinases. The triphosphate derivative is a competitive inhibitor of the viral reverse transcriptase.
The oral bioavailability in adults is >80% for doses between 0.25 and 8.0 mg kg−1. Peak serum concentrations of 1.5 μg ml−1 are achieved in 1–1.5 h and the plasma T 1/2 is approximately 2–4 h. Lamivudine is eliminated by the kidneys unchanged by both glomerular filtration and tubular excretion, and dosages should be adapted to creatinine clearance.
Clinical indications
Lamivudine is effective as monotherapy for the treatment of chronic HBV infection and in combination with other antiretroviral drugs for treatment of HIV infection. It is the first line drug for the treatment of HBeAg and anti-HBe positive disease. Elevated serum ALT levels have been shown to predict a higher likelihood of HBeAg loss in patients with chronic hepatitis B treated with lamivudine. Lamivudine is administered orally at 100 mg day−1 in the treatment of HBV infections, though the ideal dose could be higher.
Resistance
Resistance to lamivudine monotherapy develops within 6 months of therapy. The incidence of lamivudine resistance is 15–20% per year, with 70% patients becoming resistant after 5 years of treatment. It will be curious to know if lamivudine at higher doses will affect the incidence of resistance. Lamivudine resistance to HBV is conferred through HBV strains with mutations in the viral polymerase, within the catalytic domain (C domain), which includes the YMDD motif (e.g., M204V or M204I), and within the B domain (e.g., L180M or V173L). These mutants have a reduced replication capacity compared with the wild type HBV virus. Lamivudine resistance is managed by sequential treatment with either adefovir or entecavir. However, the advantage of sequential treatment compared to de novo combination therapy is questionable.
Adverse effects
Lamivudine has an extremely favorable toxicity profile. This may be partly because lamivudine does not affect mitochondrial DNA synthesis and its poor inhibition of human DNA polymerases. At the highest doses of 20 mg kg−1 day−1, neutropenia is encountered but at a low frequency.
Adefovir Dipivoxil

Chemistry, mechanism of action, and antiviral activity
Adefovir dipivoxil, bis(pivaloyloxymethyl)ester of 9-(2-phosphonylmethoxyethyl) adenine, is an orally bioavailable prodrug of adefovir, a phosphonate acyclic nucleotide analogue of adenosine monophosphate. Adefovir is monophosphorylated and is not dependent on initial phosphorylation by viral nucleoside kinases to exert its antiviral effect. The phosphorylation to the di- and triphosphate metabolites is by cellular kinases. The triphosphate competes with endogenous deoxyadenosine triphosphate (dATP) in incorporation to the nascent viral DNA resulting in premature termination of viral DNA synthesis due to the lack of a 3′ hydroxyl group. It has activity against HIV, hepadnaviruses and herpesviruses. The bioavailability of adefovir dipivoxil in humans is about 40%. It has a long intracellular half-life of 18 h allowing for a once-daily dose. Clearance of adefovir is by renal excretion. Its pharmacokinetics is substantially altered in subjects with moderate and severe renal impairment.
Clinical indications
The efficacy of adefovir has been assessed in patients with HBeAg positive and negative disease and other settings in the spectrum of chronic hepatitis B infection. At the recommended dose of 10 mg once a day, adefovir resulted in significant improvement when compared with placebo: improvement in liver histology (53% vs. 25%), reduction in HBV DNA (3.52 vs. 0.55 log copies ml−1), normalization of ALT (48% vs. 16%), and HBeAg seroconversion (12% vs. 6%). It is also useful for the treatment of lamivudine-resistant HBV infection.
Resistance
Adefovir resistance occurs in approximately 6% of patients 3 years after adefovir monotherapy. Mutations in the HBV polymerase B domain (A181V/T) and the D domain (N236T) confer resistance to adefovir.
Adverse effects
Nephrotoxicity is the major side effect of higher doses of adefovir. It causes a proximal convoluted tubule lesion characterized by a rise in urea and creatinine. Other dose-related clinical adverse events have been gastrointestinal events, including nausea, anorexia and diarrhea. These are usually mild, intermittent and self-limited without the need for concomitant medications or dose interruption.
Entecavir

Chemistry, mechanism of action, and antiviral activity
Entecavir (2-amino-1,9-dihydro-9-[(1S,3R,4S)-4-hydroxy-3-(hydroxymethyl)-2-methylenecyclopentyl]-6H-purin-6-one), monhydrate is a guanosine nucleoside analogue. Entecavir is efficiently phosphorylated by cellular kinases to the active triphosphate metabolite. It affects three-steps in the replication of HBV: (1) prevent the priming of the HBV reverse transcriptase, (2) prevent reverse transcribing of the HBV pregenomic mRNA, and (3) inhibits DNA-dependent DNA synthesis (i.e., terminating viral DNA synthesis). The HBV polymerase binds preferentially to entecavir triphosphate, and entecavir triphosphate does not affect human mitochondrial DNA synthesis. The effect of entecavir on human cellular polymerase is minimal. Studies prior to approval of entecavir for HBV treatment suggested that entecavir did not have anti-HIV activity at clinical relevant concentrations. However, recent studies have suggested an anti-HIV activity of entecavir at drug concentrations in the low nanomolar range.
Entecavir is well absorbed after oral administration achieving peak plasma concentrations between 0.6–1.5 h. Entecavir is not a substrate of the cytochrome P450 (CYP) enzyme system. It is eliminated primarily in the urine through glomerular filtration and tubular secretion. The mean elimination T 1/2 of entecavir varies from 77 to 149 h in patients with normal function. The intracellular half-life of the triphosphate metabolite in vitro studies is about 15 h.
Clinical indications
Entecavir was approved in March 2005, for the management of adult patients with chronic HBV infection who have active viral replication and/or elevation in liver transaminases or signs of active disease on histological examination. In phase III trials, responses achieved with entecavir surpassed previously published response rates for IFN-α-2b, lamivudine, and adefovir dipivoxil. With recent reports of an anti-HIV activity of entecavir, entecavir monotherapy probably should not be used in individuals with HIV–HBV coinfection who need HBV but not HIV treatment.
Resistance
The prevalence rate of resistance to entecavir in HBV-treatment naive is about 1.2%. However, virologic rebound and resistance have been reported in 43% of lamivudine-resistant patients after 4 year of switching treatment to entecavir. Entecavir resistance requires the following amino acid sequence changes in the reverse transcriptase domain of HBV; M204V/I + L184G, S202I, or M250V.
Adverse effects
Most adverse events in the phase III studies were mild and comprised of headache, upper respiratory tract infections, cough, fatigue, pharyngitis, abdominal pain, and gastrointestinal upset. The most common laboratory abnormality was ALT level greater than five times the upper limit of normal. Monitoring for long-term toxicity is needed.
Telbivudine

Chemistry, mechanism of action, and antiviral activity
Telbivudine (β-l-2′-deoxythymidine) is an l-configured nucleoside with potent and specific activities against HBV and other hepadnaviruses. Telbivudine is a competitive inhibitor of both HBV viral reverse transcriptase and DNA polymerase. Telbivudine is phosphorylated by cellular kinases to the triphosphate metabolite, which competes with naturally occurring thymidine triphosphate for viral DNA elongation. The incorporation of telbivudine into the viral DNA terminates viral DNA chain elongation. In contrast to other nucleoside analogue, such as lamivudine, telbivudine preferentially inhibits anticomplement or second-strand DNA, whereas lamivudine triphosphate preferentially inhibits the complement DNA synthesis.
Preliminary studies have shown a potent inhibition of HBV replication with a safe profile and no effect on mitochondrial metabolism. Telbivudine triphosphate does not inhibit human cellular polymerase α, β, or γ. In addition, telbivudine triphosphate is not a substrate for human DNA polymerase and thus will not induce genotoxicity.
Telbivudine is rapidly absorbed after oral dosing with peak plasma concentration achieved within 1–3 h, the absolute oral bioavailability of telbivudine is not known. Over an 8-h period, telbivudine exhibits an apparent single-phase decline, with T 1/2 of 2.5–5 h. However, a presence of a second, slower elimination phase was observed with intensive sampling in healthy volunteers up to 168 h post-dosing. The second phase starts approximately 16–24 h after dosing, with a long observed terminal-phase T 1/2 of approximately 40 h. The long plasma T 1/2 of telbivudine is consistent with the long intracellular T 1/2 (14 h) of its triphosphate in vitro studies. The elimination T 1/2 of telbivudine increases with renal dysfunction, therefore, dosage reduction of telbivudine is recommended in individuals with renal dysfunction.
Clinical indications
Telbivudine was approved in October 2006 by the FDA for treatment of chronic HBV infection. In clinical trails with primary end point of therapeutic response (a composite of suppression of HBV DNA and either loss of serum HBeAg or ALT normalization) after one year, in HBeAg-positive patients a therapeutic response occurred in 75% of patients treated with telbivudine and 67% of those treated with lamivudine. In HBeAg-negative patients, the response was 75 and 77% for telbivudine and lamivudine, respectively. In the second year of the study, telbivudine was found to be superior to lamivudine. Using the two drugs in combination was no more effective than telbivudine monotherapy.
Resistance
HBeAg-positive, 21.6%, and HBeAg-negative, 8.6%, recipients of telbivudine had HBV DNA rebound that was associated with resistance mutations. Lamivudine-resistance HBV strains have a high level of cross resistance to telbivudine. The mutations in the RT domain of HBV associated with telbivudine resistance are M204I or M204I + L180I/V.
Adverse effects
Most of the adverse effects of telbivudine reported in clinical studies were mild to moderate. The most common were elevated creatinine phosphokinase (CPK), an enzyme present in muscle tissue and a marker for the breakdown of muscle tissue, upper respiratory tract infection, fatigue, headache, abdominal pain, and cough.
Clevudine

Clevudine was recently approved in South Korea for the treatment of hepatitis B after demonstration of potent anti-hepatitis B activity in phase II and III clinical trials. It is likely to be licensed for hepatitis B treatment in other countries.
Chemistry, mechanism of action, and antiviral activity
Clevudine [1-(2-deoxy-2-fluoro-β-l-arabinofuranosyl) thymidine] is a nucleoside analogue of the unnatural β-l configuration with potent activity against HBV and some activity against EBV. Clevudine is efficiently phosphorylated by cellular kinases to clevudine-triphosphate in target cells. The mechanism of action is mainly inhibition of viral plus-strand DNA synthesis. Preclinical studies revealed that human cellular DNA polymerases α, β, γ, and δ could not utilize the 5′-triphosphate of clevudine as a substrate and, hence, the lack of cytotoxicity. The EC50 of clevudine for HBV inhibition values ranges from 0.02 to 0.84 μmol l−1. Clevudine is well absorbed after oral administration with estimated long half-life of 44–60 h.
Clinical indications
Clevudine is approved for treatment of chronic hepatitis B infection in South Korea. In a randomized, placebo-controlled phase III study in South Korea, chronic HBeAg-positive patients who received 30 mg of clevudine once daily for 24 weeks maintained a 3.73 log10 and 2.02 log10 viral suppression at 34 and 48 weeks, respectively. A unique characteristic of clevudine is the slow rebound of viremia after cessation of treatment.
Resistance
In vitro studies suggest that there may be cross-resistance with lamivudine-resistant HBV mutants. In animal studies resistance occurred in the B domain of the polymerase gene, within 12 months of treatment.
Adverse effects
In clinical trials, clevudine was well tolerated without any serious adverse events reported. Long-term toxicity has to be closely monitored.
Future Prospects
Current antiviral agents either inhibit hepatitis B replication, or invoke an immune response, which may be necessary but not sufficient to effect viral control. Moreover, antiviral resistance remains a concern with long-term therapy, the search for novel agents, and treatment strategies with minimal or no resistance and good long-term safety profile are the focus of ongoing research. Tenofovir, and emtricitabine, licensed for the treatment of HIV infections, also have activity against HBV, but are not yet FDA-approved for this indication. There are a number of new nucleoside and nucleotide analogue in the pipeline; elvucitabine, valtorcitabine, amdoxovir, racivir, MIV 210, β-l-FddC, alamifovir and hepavir B may soon be part of the armamentarium for hepatitis B treatment.
Another challenge is the management of hepatitis B in individuals with HIV coinfection. Appropriate combination regimens for individuals with coinfections are expected in the near future; target treatment of HBV to alter the outcome and take into account the impact of HBV treatment on HIV.
Therapeutics for Papillomavirus
HPVs are small DNA viruses with strict epithelial tropism. HPV infection induces the hyperproliferation of epithelial cells, leading to a broad spectrum of human diseases, ranging from benign warts (self-limiting) to malignant neoplasms. In general, there is no virus-specific effective systemic therapy available. Furthermore, treatment of disease with current therapies has not been shown to reduce the rates of transmission.
The recently FDA-approved quadrivalent prophylactic vaccine (HPV6/11/16/18) has been shown in clinical trials to be effective in preventing high-grade vulval and vaginal lesion associated with HPV 16 and 18. With time, this prophylactic vaccine is expected to reduce the incidence of HPV infections, particularly, infections due to the vaccine types (HPV6, 11, 16, and 18).
Interferon
IFNs have antiproliferative, antiviral, and immunomodulatory properties. IFNs have been administered (mostly IFN-α) topically, systemically, and intralesionally with variable results. They are more effective if used in combination with either local surgery or podophyllotoxin. Several large controlled trials have demonstrated inconsistent clinical benefits of the use of standard IFN-α therapy of condyloma acuminatum (caused by HPV) that was refractory to cytodestructive therapies. Intralesional therapy is painful, systemic therapy is associated with influenza-like symptoms such as fever and myalgia. Furthermore, IFN treatment is expensive and there is limited efficacy.
Imiquimod
This is an immunomodulator approved by the FDA for topical treatment of external and perianal genital warts. It acts as a ligand for Toll-like receptor 7 and activates macrophage and dendritic cells to release IFN α and other proinflammatory cytokines. With imiquimod application, gradual clearance of warts occurs in about 50% of patients over an average of 8–10 weeks. The adverse effects are; application site reactions (irritation, pruritus, flaking, and erosion), and systemic effects including fatigue and influenza-like illness.
Podophyllotoxin
Podophyllotoxin is the main cytotoxic ingredient of podophyllin, a resin used for many years for topical treatment of warts. The exact mechanism of action is unknown. Podophyllotoxin 0.5% solution or gel is similar in effectiveness to imiquimod but may have more adverse effects. Adverse effects include irritation of the adjacent skin, local erosion, ulceration and scarring.
Trichloroacetic acid, podophyllotoxin, and cryotherapy (with liquid nitrogen or a cryprobe) remain the most widely used treatments for external genital warts, but response rate is only 60–70%, and at least 20–30% of responders will have recurrence.
Future Prospects
The current therapies are not targeted antiviral therapies. They result in the physical removal of the lesion or the induction of nonspecific inflammation, thereby inducing a bystander immune response. There is urgent need to develop specific and effective antiviral agents for HPV infections.
Therapeutics for Enteroviral Infections
The enteroviruses include nearly 70 serotypes of closely related pathogens that cause a wide spectrum of human illness, from mild nonspecific fever to common upper respiratory infections, aseptic meningitis, severe myocarditis, encephalitis, and paralytic poliomyelitis. Certain patients, including antibody-deficient individuals, bone marrow recipients, and neonates, may develop potentially life-threatening enterovirus infections for which therapeutic options have been limited. There are case series of the use of immune serum globulin and pleconaril for serious enteroviral infections. Pleconaril failed to secure FDA approval because of its induction of CYP 3A enzyme activity, and the potential for drug interactions, particularly the interference with oral contraceptives.
Pleconaril

Chemistry, mechanism of action, and antiviral activity
Pleconaril (3-{3,5-dimethyl-4-[[3-methyl-5-isoxazolyl}propyl]phenyl]-5[trifluoromethyl]-1,2,4-oxadiazole) exerts its antiviral effect by integrating into a hydrophobic pocket inside the virion, and prevents viral replication by inhibiting viral uncoating and blocking viral attachment to host cell receptors, thus interrupting the infection cycle. The viral capsid structure, which is the target of pleconaril, is relatively conserved among the picornaviruses. Pleconaril has broad spectrum and potent activity against enteroviruses and rhinoviruses.
Pleconaril is 70% bioavailability when given orally. This high level of bioavailability was achieved by the substitution of trifluoromethyl on the oxadiazole ring that reduces its degradation in the liver by enzymes involved in oxidative processes. The metabolic stabilization is reflected in the drug’s long serum half-life (about 6.5 h) after oral dosing. Pleconaril also readily penetrates the blood-brain barrier.
Clinical indications
Common cold
In a phase I trial of pleconaril for treatment of common cold, there was a significant reduction in rhinorrhea of about 1.5 days in those on 400 mg three times daily, and a reduction in a severity score as compared to the placebo. Subsequent trials confirmed a modest reduction in length of symptoms for common cold in patients treated with pleconaril.
Immunocompromised host
Patients with compromised humoral immunity, such as those with agammaglobulinemia, who contract enteroviral infections may develop chronic meningitis and meningoencephalitis, often with a fatal outcome. There are case reports of the efficacy of pleconaril in these patients.
Enteroviral meningitis
For treatment of enteroviral meningitis, two large studies showed a marginal statistical improvement in a clinical score in the pleconaril-treated groups. A subsequent small study of 21 infants with proven enteroviral meningitis in the United States did not have enough power to show unequivocal benefit with pleconaril.
Resistance
Resistance to pleconaril has been reported in some serotypes of enteroviruses, however, the mechanism is not well understood.
Adverse effects
Pleconaril is generally well tolerated. The most common adverse events are headache, diarrhea, and nausea. Long-term use of pleconaril is associated with an increase in menstrual irregularities in women.
Future Prospects
Pleconaril has not been licensed for treatment of enteroviral infections; there is an urgent need to identify alternative drugs that might be effective. There are several investigational compounds; however, none has reached phase I clinical trial. Combinations of drugs are likely to offer the best chance of cure and protection from enterovirus infections in the future.
Anti-HIV Agents
The combination of three or more anti-HIV agents into multidrug regimens, often termed highly active antiretroviral therapy (HAART), can efficiently inhibit HIV viral replication to achieve low or undetectable circulatory HIV-1 levels. This is the start-of-the-art treatment of AIDS or HIV-infected individuals. Drug combinations are, in principle, aimed at obtaining synergism between the compounds, while reducing the likelihood of the development of drug resistance virus, and minimizing toxicity. The available anti-HIV drugs are categorized according the step they target within the HIV viral life cycle (Figure 2); (1) binding inhibitors, for example, coreceptor antagonist (maraviroc); (2) fusion inhibitors (enfuvirtide); (3) reverse transcriptase inhibitors (nucleoside/nucleotide (zidovudine, didanosine, zalcitabine, stavudine, lamivudine, abacavir, emtricitabine, and tenofovir), and non-nucleoside (nevirapine, delavirdine, and efavirenz) analogue); (4) integrase inhibitors (raltegravir); and (5) protease inhibitors (saquinavir, indinavir, ritonavir, nelfinavir, amprenavir, fosamprenavir, lopinavir, atazanavir, tipranavir, and darunavir).
Figure 2.

HIV life cycle showing the stages of intervention of available anti-HIV agents.
Fixed-dose combinations and once-daily dosage forms of many anti-HIV agents are available. There are fixed-dose combinations for zidovudine/lamivudine, zidovudine/lamivudine/abacavir, abacavir/lamivudine, tenofovir/emtricitabine, and tenofovir/emtricitabine/efavirenz.
Coreceptor Antagonist
Maraviroc

Chemistry, mechanism of action, and antiviral activity
Maraviroc (4,4-difluoro-N-{(1S)-3-[exo-3-(3-isopropyl-5-methyl-4H-1,2,4 triazol-4-yl)-8-azabicyclo(3,2,1]oct-8-yl]-1-phenylpropyl}cyclohexanecarboxamide) is the first of the class of CCR5 coreceptor antagonists licensed (August 2007) for HIV treatment. Maraviroc selectively binds to the human chemokine receptor CCR5 present on the cell membrane, preventing the interaction of HIV-1 gp120 and CCR5 necessary for CCR5-tropic HIV-1 to enter cells. It inhibits the replication of CCR5-tropic laboratory strains and primary isolates of HIV-1 in vitro. The mean EC50 for maraviroc against various strains of HIV-1 ranges from 0.1 to 1.25 nmol l−1 (0.05 to 0.64 ng ml−1) in cell culture. Maraviroc was not active against CXCR4-tropic and dual-tropic viruses (EC50 value >10 μmol l−1). The antiviral activity of maraviroc against HIV-2 has not been evaluated.
The absolute bioavailability for 100 and 300 mg doses are 23 and 33%, respectively. Peak plasma concentrations of maraviroc are attained at 0.5–4 h following single oral dose of 1200 mg administered to uninfected volunteers. Maraviroc is bound (approximately 76%) to human plasma proteins. It is principally metabolized by the cytochrome P450 system to metabolites that are essentially inactive against HIV-1. Maraviroc is a substrate of CYP3A and the efflux transporter P-glycoprotein (Pgp), and therefore, its pharmacokinetics are likely to be modulated by inhibitors and inducers of these enzymes/transporters. The terminal half-life in healthy subjects is 14–18 h.
Clinical indications
Maraviroc is approved for use in combination with other anti-HIV agents for the treatment of adults with CCR5-tropic HIV-1, who are treatment-experienced with evidence of viral replication and HIV-1 strains resistant to multiple antiretroviral agents.
Resistance
The resistance profile in treatment-naive and treatment-experienced subjects has not been fully characterized. HIV-1 variants with reduced susceptibility to maraviroc have been selected in cell culture, following serial passage of two CCR5-tropic viruses (CC1/85 and RU570). The maraviroc resistant viruses remained CCR5-tropic with no evidence of a change from a CCR5-tropic virus to a CXCR4-using virus. Two amino acid residue substitutions (Table 1, letter codes of amino acids) in the V3-loop region of the HIV-1 envelope glycoprotein (gp160), A316T and I323V were shown to be necessary for the maraviroc-resistant phenotype in the HIV-1 isolate CC1/85. In the RU570 isolate, a 3-amino acid residue deletion in the V3 loop, ΔQAI (HXB2 positions 315–317), was associated with maraviroc resistance. The clinical relevance of these mutations is not known.
Table 1.
The three-letter and one-letter codes for amino acid residues
| Amino acid | Three-letter code | One-letter code |
|---|---|---|
| Alanine | Ala | A |
| Arginine | Arg | R |
| Asparagine | Asn | N |
| Aspartic acid | Asp | D |
| Cysteine | Cys | C |
| Glutamic acid | Glu | E |
| Glutamine | Gln | Q |
| Glycine | Gly | G |
| Histidine | His | H |
| Isoleucine | Ile | I |
| Leucine | Leu | L |
| Lysine | Lys | K |
| Methionine | Met | M |
| Phenylalanine | Phe | F |
| Proline | Pro | P |
| Serine | Ser | S |
| Threonine | Thr | T |
| Tryptophan | Trp | W |
| Tyrosine | Tyr | Y |
| Valine | Val | V |
Adverse effects
The most common adverse events reported with maraviroc were cough, fever, upper respiratory tract infections, rash, musculoskeletal symptoms, abdominal pain, and dizziness. The product label includes a warning about liver toxicity (hepatoxicity) and a statement about the possibility of heart attacks.
Fusion Inhibitors
Enfuvirtide
Chemistry, mechanism of action, and antiviral activity
Enfuvirtide, a linear 36-amino acid synthetic peptide with the N-terminus acetylated and the C-terminus is a carboxamide, is the first licensed agent in the class of fusion inhibitors. Enfuvirtide interferes with the entry of HIV-1 into cells by inhibiting fusion of viral and cellular membranes (Figure 2). Enfuvirtide binds to the first heptad-repeat (HR1) in the gp41 subunit of the viral envelope glycoprotein and prevents the conformational changes required for the fusion of viral and cellular membranes. The IC50 of enfuvirtide for baseline clinical isolates ranged from 0.089 to 107 nmol l−1 (0.4 to 480 ng ml−1). Enfuvirtide is active against R5, X4, and dual tropic viruses, but has no activity against HIV-2.
Enfuvirtide is administered twice daily by subcutaneous injection. Single-dose vials contain 108 mg of enfuvirtide for the delivery of approximately 90 mg ml−1 when reconstituted. The absolute bioavailability is 84.3 ± 15.5%. Following 90 mg bid dosing of enfuvirtide subcutaneously in combination with other antiretroviral agents in HIV-1 infected subjects, the median T max was 4 h (ranged from 4 to 8 h). Enfuvirtide is catabolized by proteolytic enzymes. It is not metabolized by hepatic CYP450 isoenzyme systems. There are no known clinically significant interactions between enfuvirtide and other medications.
Clinical indications
Enfuvirtide was approved by the FDA in March 2003 for use in adults, and in children aged 6 and older, with advanced HIV infection. Enfuvirtide is used with other anti-HIV agents to treat HIV-1 infection in patients who are treatment-experienced and have detectable viral loads even though they are taking anti-HIV agents.
Resistance
HIV-1 isolates with reduced susceptibility to enfuvirtide have been selected in vitro. Genotypic analysis of these resistant isolates showed mutations that resulted in amino acid substitutions at the enfuvirtide binding HR1 domain positions 36–38 of the HIV-1 envelope glycoprotein gp41. In clinical trials, HIV-1 isolates with reduced susceptibility to enfuvirtide have been recovered from subjects failing enfuvirtide-containing regimen. Most of the isolates with decreased in susceptibility to enfuvirtide of greater than fourfold exhibited genotypic changes in the codons encoding gp41 HR1 domain amino acids 36–45.
HIV-1 clinical isolates resistant to nucleoside analogue reverse transcriptase inhibitors, non-nucleoside analogue reverse transcriptase inhibitors, and protease inhibitors are susceptible to enfuvirtide in cell culture.
Adverse effects
The most common adverse effects of enfuvirtide are injection site reactions. Other symptomatic side effects may include insomnia, headache, dizziness, and nausea. Several cases of hypersensitivity have been described. In phase III studies, bacterial pneumonia was seen at a higher rate in patients who received enfuvirtide than in those who did not receive enfuvirtide. Eosinophilia is the primary laboratory abnormality seen with enfuvirtide administration.
Reverse Transcriptase Inhibitors
Nucleoside/nucleotide reverse transcriptase inhibitors
Zidovudine

Chemistry, mechanism of action, and antiviral activity
Zidovudine (3′-azido-2′,3′-dideoxythymidine) is a pyrimidine analogue with an azido group substituting for the 3′ hydroxyl group on the ribose ring. Zidovudine is initially phosphorylated by cellular TK and then to its diphosphate by cellular thymidylate kinase. The triphosphate derivative competitively inhibits HIV reverse transcriptase, and functions as a chain terminator. Zidovudine inhibits HIV-1 at concentrations of approximately 0.013 μg ml−1. In addition, it inhibits a variety of other retroviruses. Synergy has been demonstrated against HIV-1 when zidovudine is combined with didanosine, zalcitabine, lamivudine, nevirapine, delavirdine, saquinavir, indinavir, ritonavir, and other compounds. It was the first drug to be licensed for the treatment of HIV infection, and still is used in combination with other drugs as initial therapy for some patients.
Zidovudine is available in capsule, syrup, and intravenous formulations. Oral bioavailability is approximately 65%. Peak plasma levels are achieved approximately 0.5–1.5 h after treatment. Zidovudine penetrates cerebrospinal fluid, saliva, semen, and breast milk and it crosses the placenta. Drug is predominately metabolized by the liver through the enzyme uridine diphosphoglucuronosyltransferase to its major inactive metabolite 3′-azido-3′-deoxy-5′-O-β-d-glucopyranuronosylthymidine. The elimination T 1/2 is approximately 1 h; however, it is extended in individuals who have altered hepatic function.
Clinical indications
Zidovudine is used in combination with other anti-HIV agents. It is administered orally at 600 mg day−1 (300 mg tablet, twice a day). The single most important usage of zidovudine in the last decade has been the peripartum three-part zidovudine regimen, which has decreased the incidence of transmission of HIV infection from pregnant women to their infants.
Adverse effects
The predominant adverse effect of zidovudine is myelosuppression, as evidenced by neutropenia and anemia, occurring in 16 and 24% of the patients, respectively. Zidovudine has been associated with skeletal and cardiac muscle toxicity, including polymyositis. Nausea, headache, malaise, insomnia, and fatigue are common side effects.
Didanosine

Chemistry, mechanism of action, and antiviral activity
Didanosine (2′,3′-dideoxyinosine) is a purine nucleoside with inhibitory activity against both HIV-1 and HIV-2. Didanosine is activated by intracellular phosphorylation. It is first converted to 2′,3′-dideoxyinsine-5′-monophosphate by 5′nucleotidase and inosine 5′-monophosphate phosphotransferase and subsequently to 2′, 3′-dideoxyadenosine-5′-monophosphate by adenylsuccinate synthetase and lyase. It is then converted to diphosphate by adenylate kinase and subsequently by creatine kinase or phosphoribosyl pyrophosphate synthetase to the triphosphate. The triphosphate metabolite is a competitive inhibitor of HIV reverse transcriptase and a chain terminator. The spectrum of activity of didanosine is enhanced by synergism with zidovudine and stavudine as well as the protease inhibitors.
Didanosine is acid labile and has poor solubility. A buffered tablet results in 20–25% bioavailability. A 300 mg oral dose achieves peak plasma concentrations of 0.5–2.6 μg ml−1 with a T 1/2 of approximately 1.5 h. It is metabolized to hypoxanthine and is cleared primarily by the kidneys.
Clinical indications
Didanosine is used in combination with other anti-HIV agents as part of HAART. It is given as two 100 mg tablets (buffered tablets) twice a day or as one 400 mg capsule (delayed-release capsule) once a day.
Adverse effects
The most significant adverse effect associated with didanosine therapy is the development of peripheral neuropathy (30%) and pancreatitis (10%). Lipoatrophy, lactic acidosis and diabetes have been observed in patients on antiretroviral regimens containing didanosine.
Zalcitabine

Chemistry, mechanism of action, and antiviral activity
Zalcitabine (2′,3′-dideoxycytidine) is a pyrimidine analogue, which is activated by cellular enzymes to its triphosphate derivative. The enzymes responsible for activation of zalcitabine are cell cycle independent, and therefore this offers a theoretical advantage for nondividing cells, specifically dendritic and monocyte/macrophage cells. Zalcitabine inhibits both HIV-1 and HIV-2 at concentrations of approximately 0.03 μmol l−1.
The oral bioavailability following zalcitabine administration is more than 80%. The peak plasma concentrations following an oral dose of 0.03 mg kg−1 range from 0.1 to 0.2 μmol l−1 and the T 1/2 is approximately 20 min. The drug is cleared mainly by the kidneys, and therefore, the presence of renal insufficiency leads to a prolong plasma T 1/2.
Clinical indications
Zalcitabine is used as part of HAART regimen for HIV-1 infections. It is administered orally at 2.25 mg day−1 (one 0.75 mg tablet every 8 h).
Adverse effects
Peripheral neuropathy is the major toxicity associated with zalcitabine administration, occurring in approximately 35% of individuals. Pancreatitis can occur, but does so infrequently. Thrombocytopenia and neutropenia are uncommon (5% and 10%, respectively). Other zalcitabine-related side effects include nausea, vomiting, headache, hepatotoxicity, and cardiomyopathy.
Stavudine

Chemistry, mechanism of action, and antiviral activity
Stavudine (2′,3′-didehydro, 3′-deoxythymidine) is a thymidine analogue with significant activity against HIV-1, having inhibitory concentrations, which range from 0.01 to 4.1 μmol l−1. Its mechanism of action is similar to that of zidovudine.
The oral bioavailability of stavudine is more than 85%. Peak plasma concentrations of approximately 1.2 μg ml−1 are reached within 1 h of dosing at 0.67 mg kg−1 per dose. Stavudine penetrates CSF and breast milk. It is excreted by the kidneys unchanged and, in part, by renal tubular secretion.
Clinical indications
Stavudine is used for HIV infection in combination with other anti-HIV agents. Stavudine is a highly potent inhibitor of HIV-1 replication in vitro. However, its use has been limited by delayed toxicity, notably peripheral neuropathy and myopathy caused by mitochondrial damage. It is administered orally at 80 mg day−1 (one 40 mg capsule every 12 h).
Adverse effects
The principal adverse effect of stavudine therapy is the development of peripheral neuropathy. The development of this complication is related to both dose and duration of therapy. Inhibition of mitochondrial DNA synthesis is proposed to induce depletion of cellular mitochondrial DNA and it is ultimately responsible for the delayed toxicity observed with the use of stavudine and other nucleoside reverse transcriptase inhibitors (NRTIs). Neuropathy tends to appear after 3 months of therapy and resolves slowly with medication discontinuation. Other side effects are uncommon. Fatal and nonfatal pancreatitis have occurred during therapy when stavudine was part of a combination regimen that included didanosine. Redistribution and accumulation of body fat (lipoatrophy) have been observed in patients receiving stavudine as part of their antiretroviral regimen.
Lamivudine
Chemistry, mechanism of action, and antiviral activity
The chemistry and mechanism of action of lamivudine have been described previously in section ‘Lamivudine’ under ‘Therapeutics for Hepatitis’. Lamivudine has significant activity in vitro against both HIV-1 and HIV-2, as well as HBV. Lamivudine is a competitive inhibitor of the viral reverse transcriptase.
Clinical indications
Lamivudine is used in combination with other anti-HIV agents. Lamivudine is given orally at 300 mg day−1 (one 150 mg tablet twice a day, or one 300 mg tablet once a day). It is also formulated in combination with zidovudine, or with zidovudine and abacavir as fixed-dose combination tablet.
Adverse effects
Lamivudine has an extremely favorable toxicity profile. This may largely be attributed to the low affinity of lamivudine for human DNA polymerases, and the lack of active lamivudine metabolites in the mitochondrial compartment of cells. At the highest doses of 20 mg kg−1 day−1, neutropenia is encountered but at a low frequency. In pediatric studies, pancreatitis and peripheral neuropathies have been reported.
Abacavir

Chemistry, mechanism of action, and antiviral activity
Abacavir sulfate, (1S,4R)-4-[2-amino-6-(cyclopropylamino)-9H-purin-9-yl]-2-cyclopentene-1-methanol, is a structural analogue of the purine guanine. The phosphorylation pathway of abacavir differs from that of all other nucleoside analogues. The first step in the conversion of abacavir to its active metabolite, carbovir triphosphate, is phosphorylation to abacavir monophosphate by adenosine phosphotransferase. This step is followed by deamination by a cytosolic enzyme to form carbovir monophosphate, which undergoes two subsequent phosphorylations, to the diphosphate by guanylate kinase and to the triphosphate by nucleoside diphosphate kinase and other enzymes. Carbovir triphosphate competes with endogenous 2′-dGTP for incorporation into the nucleic acid chain, and after incorporation, terminates DNA chain elongation. Abacavir exhibits potent in vitro antiviral activity against wild-type HIV-1 (IC50 4.0 μmol l−1), but this activity is lower than the activity of zidovudine (IC50 0.040 μmol l−1). However, there is no significant difference between the levels of activity of abacavir (IC50 0.26 μmol l−1) and AZT (IC50 0.23 μmol l−1) against clinical isolates of HIV-1.
Abacavir is well absorbed after oral administration with a bioavailability between 76 and 96%. After single or multiple doses, C max is attained after a mean of 0.7–1.7 h, and the mean half-life is 0.8–1.5 h. However, at a dose of 300 mg twice daily as part of a combination regimen, levels of intracellular carbovir triphosphate ranged from <20 to 374 fmol per 106 cells. The intracellular carbovir triphosphate was measurable throughout the 24-h study period, with the highest levels found between 6 and 8 h. This finding suggests a long half-life for carbovir triphosphate within cells. The main route of excretion is renal.
Clinical indications
Abacavir is used in combination with other anti-HIV agents. It is given as a 300 mg tablet twice a day, or two 300 mg tablets once a day. A fixed-dose combination with lamivudine is available (600 mg abacavir, plus 300 mg lamivudine).
Adverse effects
The abacavir hypersensitivity reaction is a potentially fatal syndrome occurring in approximately 5% of HIV-infected patients exposed to this nucleoside analogue after a median of 11 days (range: 1–318 days). Systemic manifestations can include fever, rash, fatigue, and gastrointestinal or respiratory symptoms. Rechallenge with abacavir in individuals presumed to have abacavir hypersensitivity reaction is avoided due to reports of fatal reactions caused by repeated administration of abacavir following a hypersensitivity reaction. The presence of HLA-B*5701 has been associated with elevated odds of developing abacavir hypersensitivity reaction.
Emtricitabine

Chemistry, mechanism of action, and antiviral activity
Emtricitabine, 5-fluoro-1-(2R,5S)-[2-(hydroxymethyl)-1,3-oxathiolan 5-yl]cytosine, is a fluorinated nucleoside analogue of cytosine. Emtricitabine, similar in many ways to lamivudine, has in vitro activity against HIV-1 that is similar to or approximately fourfold to tenfold more potent than that of lamivudine. The EC50 for emtricitabine is in the range of 0.0013–0.64 μmol l−1 (0.0003–0.158 μg ml−1) for laboratory and clinical isolates of HIV-1 in cell culture. Against HIV-2, the EC50 ranges from 0.007 to 1.5 μmol l−1. The cellular enzymes involved in the phosphorylation of emtricitabine are similar to that of lamivudine. The active triphosphate competitively inhibits reverse transcriptase by being incorporated into the viral genome, and causing termination in DNA chain elongation.
The bioavailability of the capsules and oral solution are 93 and 75%, respectively. Emtricitabine is rapidly and extensively absorbed following oral administration with peak plasma concentrations occurring at 1–2 h post dose.
The mean plasma elimination half-life of emtricitabine after a single dose is about 8–10 h in HIV-infected patients. However, after multiple doses of the drug at a dose of 200 mg daily, the intracellular half-life is approximately 39 h. The high intracellular levels of emtricitabine triphosphate achieved are associated with better suppression of plasma HIV RNA. Emtricitabine is not an inhibitor of human CYP450 enzymes. Emtricitabine is eliminated by a combination of glomerular filtration and active tubular secretion.
Clinical indications
Emtricitabine is used with other anti-HIV agents. It is administered orally at a once-daily 200 mg capsule. Emtricitabine is a component of Truvada (a fixed-dose combination of emtricitabine and tenofovir disoproxil fumarate), and Atripla (a fixed-dose combination of efavirenz, emtricitabine, and tenofovir disoproxil fumarate).
Adverse effects
The most common adverse events are headache, diarrhea, nausea, and rash, which are generally of mild to moderate severity. Approximately 1% of patients discontinued participation in clinical trials due to these events.
Tenofovir disoproxil fumarate

Chemistry, mechanism of action, and antiviral activity
Tenofovir disoproxil fumarate is (a prodrug of tenofovir), 9-[(R)-2-[[bis[[(isopropoxycarbonyl)oxy]methoxy]phosphinyl]methoxy]propyl]adenine fumarate (1:1), converted to tenofovir, an acyclic nucleoside phosphonate (nucleotide) analogue of adenosine 5′-monophosphate. Tenofovir disoproxil fumarate requires initial diester hydrolysis for conversion to tenofovir and subsequent phosphorylations by cellular enzymes to form tenofovir triphosphate. Tenofovir triphosphate inhibits the activity of HIV-1 reverse transcriptase by competing with the natural substrate deoxyadenosine 5′-triphosphate and, after incorporation into DNA, by DNA chain termination. Tenofovir triphosphate is a weak inhibitor of mammalian DNA polymerases α, β, and mitochondrial DNA polymerase γ. Tenofovir has antiviral activity in vitro against HIV-1 with IC50 values ranging from 0.5 to 2.2 μmol l−1. The IC50 values of tenofovir against HIV-2 range from 1.6 to 4.9 μmol l−1.
The oral bioavailability of tenofovir in fasting patients is approximately 25%. Following oral administration of a single dose of 300 mg to HIV-1 infected patients, maximum serum concentrations are achieved in 1.0 ± 0.4 h. C max and AUC values are 296 ± 90 ng ml−1 and 2287 ± 685 ng h ml−1, respectively. The oral bioavailability increases when tenofovir is administered after a high-fat meal (40–50% fat). In vitro studies indicate that neither tenofovir disoproxil nor tenofovir are substrates of CYP450 enzymes. Tenofovir is primarily excreted by the kidneys by a combination of glomerular filtration and active tubular secretion. The pharmacokinetics of tenofovir is altered in patients with renal impairment.
Clinical indications
Tenofovir is used in combination with other anti-HIV agents for the treatment of HIV-1 infection. It is administered orally once daily, 300 mg tablet.
Adverse effects
The most common adverse reactions seen in a double-blind comparative controlled study were mild to moderate gastrointestinal events and dizziness. However, the following adverse events have been identified during post-approval use of tenofovir; allergic reaction, hypophosphatemia, lactic acidosis, dyspnea, abdominal pain, increased amylase, pancreatitis, increased liver enzymes, hepatitis, renal insufficiency, renal failure, fanconi syndrome, proximal tubulopathy, proteinuria, increased creatinine, acute tubular necrosis, and nephrogenic diabetes insipidus.
Resistance to nucleoside/nucleotide analogue
Nucleoside analogue-associated mutations (NAMs) develop by at least three pathways: (1) accumulation of zidovudine or thymidine analogue resistance mutations (TAMs), (e.g., 41L, 67N, 70R, 210W, 215Y/F, and 219Q/E); (2) selection of the key 151M mutation, followed by the mutations 62V, 75I, 77L, and 116Y, referred to as the 151 complex; and (3) the 69 insertion complex, consisting of a mutation at codon 69 (typically Ser), followed by an insertion of two or more amino acids (e.g., Ser-Ser, Ser-Arg, or Ser-Gly) and generally accompanied by other NAMs. In clinical isolates, two TAM pathways have been observed: 41L, 210W, 215Y/F and 67N, 70R, 219Q/E/N/R; of these, the 41–210–215 combination is the most prevalent. The cytidine analogue select for the M184V mutation (lamivudine, and emtricitabine), while the K65R is seen with tenofovir selection pressure.
Resistance patterns with earlier nucleoside analogue combinations (zidovudine or stavudine with lamivudine)
The resistance profiles seen with earlier nucleoside analogue combinations are well characterized. With thymidine-based NRTIs (lamivudine/zidovudine or stavudine/lamivudine), the M184V mutation emerges rapidly, whereas TAMs are slower to arise. The use of emtricitabine in place of lamivudine would presumably yield similar results, although clinical data are limited. The M184V mutation has been shown to increase zidovudine susceptibility in the absence or presence of zidovudine resistance mutations and without regard to which TAM combination is present. The M184V mutation may increase sensitivity to tenofovir.
The most commonly observed mutations with zidovudine/didanosine or stavudine/didanosine are TAMs. TAMs and multinucleoside resistance (MNR) mutations (Q151M, T69 insert) are more prevalent in didanosine-containing regimens than in lamivudine-containing regimens.
Resistance patterns with new nucleoside/nucleotide analogue combinations
With abacavir/lamivudine as backbone, the most common mutation selected for is M184V/I followed by the L74V mutation at treatment failure. The K65R is the major mutation selected in vitro by tenofovir alone or in combination with abacavir or lamivudine while abacavir appears to favor L74V and K65R.
In triple-nucleoside/nucleotide regimens (tenofovir/lamivudine/didanosine or tenofovir/lamivudine/abacavir) that lack a thymidine analogue, early treatment failure has been associated with a high frequency of M184V. In addition, 50% of the patients with M184V also harbor the K65R.
Non-nucleoside reverse transcriptase inhibitors
Nevirapine

Chemistry, mechanism of action, and antiviral activity
Nevirapine (11-cyclopropyl-5,11-dihydro-4-methyl-6H-dipyrido[3,2-b:2′,3′-e]; [1,4]diazepin-6-one) is a reverse transcriptase inhibitor of HIV-1. However, its mechanism of action is different from nucleoside analogue. It binds to a hydrophobic pocket adjacent to the active site of the reverse transcriptase and causes conformational changes that affect replication. Nevirapine has a bioavailability of approximately 65%. Peak serum concentration of 3.4 μg ml−1 is achieved approximately 4 h after a 400 mg oral dose. Nevirapine is metabolized by liver microsomes to hydroxymethyl-nevirapine.
Clinical indications
Nevirapine is used in combination with other anti-HIV agents. It is administered orally at 200 mg day−1 for the first 14 days (one 200 mg tablet per day), then 400 mg day−1 (two daily 200 mg tablets). Single-dose nevirapine is used widely in resource-limited settings to prevent mother-to-child transmission of HIV infection.
Adverse effects
The most common adverse effects include the development of a nonpruritic rash in as many as 50% of patients who received 400 mg day−1. In addition, fever, myalgias, headache, nausea, vomiting, fatigue, and diarrhea have also been associated with administration of drug.
Resistance
Changes in two sets of amino acid residues (100–110 and 180–190) in the reverse transcriptase gene confer resistance to nevirapine. Nevirapine monotherapy is associated with resistance most frequently appearing at codon 181.
Delavirdine

Chemistry, mechanism of action, and antiviral activity
Delavirdine (1-[5-methanesulfonamido-1H-indol-2-yl-carbonyl]-4-[3-(1-methylethylamino) pyridinyl] piperazine) is a second-generation bis (heteroaryl) piperazine licensed for the treatment of HIV infection. Its mechanism of action is similar to that of nevirapine. It is absorbed rapidly when given orally with bioavailabilty of >60%. Delavirdine is metabolized by the liver with an elimination T 1/2 of approximately 1.4 h. It has an inhibitory concentration against HIV-1 of approximately 0.25 μmol l−1. Inhibitory concentrations for human DNA polymerases are significantly higher.
Clinical indications
Delavirdine is used in combination with other anti-HIV agents. It is administered at 1200 mg day−1 (two 200 mg tablets three times a day).
Adverse effects
Delavirdine administration is associated with a maculopapular rash. Other side effects are less common.
Resistance
Delavirdine resistance can be generated rapidly both in vitro and in vivo with the codon change identified at 236, resulting in an increase and susceptibility to >60 μmol l−1. Delavirdine resistance can be conferred by mutations at codons 181 and 188, as seen with other non-nucleoside analogue.
Efavirenz

Chemistry, mechanism of action, and antiviral activity
Efavirenz [(S)-6-chloro-4-(cyclopropylethynyl)-1,4-dihydro-4 (trifluoromethyl)-2H-3,1-benzoxazin-2-one] is a non-NRTI that can be administered once daily. Activity is mediated predominately by noncompetitive inhibition of HIV-1 reverse transcriptase. HIV-2 reverse transcriptase, and human cellular DNA polymerases α, β, γ, and δ are not inhibited by efavirenz. The 90–95% inhibitory concentration of efavirenz is approximately 1.7–25 nmol l−1.
Clinical indications
Efavirenz is used in combination with other antiretroviral agents for the treatment of HIV-1 infection. Combination therapy has resulted in a 150-fold or greater decrease in HIV-1 RNA levels.
Adverse effects
The most common adverse events are skin rash (25%), which is associated with blistering, moist desquamation, or ulceration (1%). In addition, delusions and inappropriate behavior have been reported in 1 or 2 patients per 1000.
Resistance
Resistance to efavirenz is caused by mutation in the reverse transcriptase gene as with other non-nucleoside analogue, and appears rapidly.
Integrase Inhibitors
Raltegravir

Chemistry, mechanism of action, and antiviral activity
Raltegravir, a structural analogue of a class of compounds with a distinct diketo acid moiety, is a novel HIV-1 integrase inhibitor with potent in vitro activity against HIV-1 (IC95 of 33 nmol l−1) in the presence of 50% human serum. It is active against a wide range of wild-type and multidrug-resistant HIV-1 clinical isolates and has potent activity against viruses that use CCR5 and/or CXCR4 coreceptors for entry.
Raltegravir is absorbed rapidly, with median T max values in the fasting state of about 1 h; plasma concentrations decrease from C max in a biphasic manner, with a half-life of approximately 1 h for the initial (α) phase and an apparent half-life of approximately 7–12 h for the terminal (β) phase. The pharmacokinetic data for raltegravir are supportive of twice daily administration. It is metabolized by hepatic glucuronidation and has no effect on CYP3A4. Approximately 7–14% of the raltegravir dose is excreted unchanged in urine.
Clinical indications
Raltegravir received priority approval from the FDA (October 2007) for treatment of HIV-1 infection in combination with other antiretroviral agents in treatment-experienced patients with evidence of HIV-1 replication despite ongoing antiretroviral therapy. The dosage of raltegravir is 400 mg administered orally, twice daily with or without food.
Adverse effects
Side effects (mostly mild to moderate) were seen with similar frequency in the raltegravir and placebo arms; the rate of serious adverse events was less than 3% across arms. No lipid abnormalities have been reported so far with raltegravir.
Resistance
In 9 of 41 patients failing raltegravir, no mutations were detected; while in 32 of 41 patients, three mutational patterns were described (N155H, Q148K/R/H, and, rarely, Y143R/C). The clinical implications of these findings are unknown.
Protease Inhibitors
Protease inhibitors are used in combination with other anti-HIV agents for treatment of HIV infection. They are a potent component of HAART regimens. Protease inhibitors are used in combination with ritonavir as the boosting protease inhibitor. The concept of boosting involves pharmacokinetic drug interactions; currently available protease inhibitors are metabolized in the liver by the cytochrome P450 3A4 (CYP3A4) enzyme system. Ritonavir is the most powerful enzyme inhibitor in the protease inhibitor class. The combination with ritonavir allows the boosted protease inhibitor to maintain prolonged blood levels. This allows for decreased dosage, and reduces a three times a day schedule to a twice daily or even a once daily regimen.
Long-term HAART containing protease inhibitors has been most strongly associated with syndromes characterized by dyslipidemia, peripheral lipodystrophy, and insulin resistance.
Saquinavir

Chemistry, mechanism of action, and antiviral activity
Saquinavir (cis-N-tert-butyl-decahydro-2[2(R)-hydroxy-4-phenyl-3-(S)-([N-(2 quinolycarbonyl)-Lasparginyl] amino butyl)-4aS, 8aS]-isoquinoline-3[S]-carboxyamide methanesulfonate) is a hydroxyethylamine-derived peptidomimetic HIV protease inhibitor. Saquinavir inhibits HIV-1 and HIV-2 at concentrations of 10 nmol l−1 and is synergistic with other nucleoside analogue as well as selected protease inhibitors.
Oral bioavailability is approximately 30% with extensive hepatic metabolism. Peak plasma concentrations of 35 mg μl−1 are obtained following a 600 mg dose.
The clinical efficacy of saquinavir is limited by poor oral bioavailability but improved formulation (soft-gel capsule) enhances efficacy. Saquinavir is boosted with 100 mg twice a day of ritonavir to improve its bioavailabilty and efficacy even against saquinavir-resistant HIV strains.
Adverse effects
Adverse effects are minimal with no dose-limiting toxicities. Abdominal discomfort, including diarrhea and nausea, has been reported infrequently.
Resistance
Mutations at codon sites 90 and 48 of the protease gene result in approximately a 30-fold decrease in susceptibility to saquinavir.
Indinavir
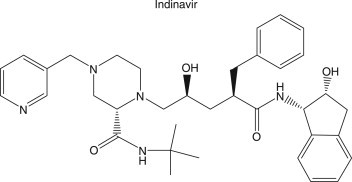
Chemistry, mechanism of action, and antiviral activity
Indinavir {N-[2(R)-hydroxy-1(S)-indanyl]-5-[2(S)-(1,1-dimethylethlaminocarbonyl)-4-(pyridin-3-yl) methylpiperazin-1-yl]-4[S]-hydroxy-2[R]-phenylmethyl pentanamide} is a peptidomimetic HIV-1 and HIV-2 protease inhibitor. At concentrations of 100 nmol l−1, indinavir inhibits 90% of HIV isolates. Indinavir is rapidly absorbed with a bioavailability of 60% and achieves peak plasma concentrations of 12 μmol l−1 after a 800 mg oral dose.
Adverse effects
Although indinavir is well tolerated, commonly encountered adverse effects include indirect hyperbilirubinemia (10%) and nephrolithiasis (5%).
Resistance
Indinavir resistance develops rapidly with monotherapy and occurs at multiple sites. The extent of resistance is directly related to the number of codon changes in the HIV protease gene. Codon 82 is a common mutation in indinavir-resistant HIV isolates.
Ritonavir

Chemistry, mechanism of action, and antiviral activity
Ritonavir (10-hydroxy-2-methyl-5[1-methylethyl]-1[2-(1-methylethyl)-4-thiazo lyl]-3,6,dioxo-8,11-bis[phenylmethyl]-2,4,7,12-tetra azatridecan-13-oic-acid, 5 thiazolylmethylester, [5S-(5R, 8R,10R, 11R)]) is an HIV protease inhibitor with activity in vitro against HIV-1 laboratory strains (0.02–0.15 μmol l−1). It is synergistic when administered with nucleoside analogue. Oral bioavailability is approximately 80%, with peak plasma levels of approximately 1.8 μmol l−1 after 400 mg administered every 12 h. The plasma half-life is approximately 3 h.
Adverse effects
Adverse effects include nausea, diarrhea, and headache, but all occur at a low frequency.
Resistance
Ritonavir has cross-resistance to indinavir. Mutations at codon 82 are the most common.
Nelfinavir

Chemistry, mechanism of action, and antiviral activity
Nelfinavir [3S-(3R, 4aR, 8aR, 22′S, 3′S)]-2-[2″-hydroxy-3′-phenylthiomethyl-4′-aza-5′-ox-o-5′-(2″methyl-3′-hydroxyphenyl)pentyl]-decahydroiso-quinoline-3-N-(tert-butyl-carboxamide methanesulfonic acid salt) is another peptidomimetic HIV protease inhibitor. Inhibitory concentrations of HIV-1 are in the range of 20–50 nmol l−1. It has anti-HIV-2 activity. Nelfinavir is orally bioavailable at approximately 40%, achieving peak plasma concentrations of 2 or 3 mg following a 800 mg dose every 24 h. The drug is metabolized by hepatic microsomes.
Adverse effects
Nelfinavir is well tolerated with mild gastrointestinal complication reported.
Resistance
Cross-resistance to other protease inhibitors, particularly saquinavir, indinavir, or ritonavir, is not common. The most frequently demonstrated site of mutation is at codon 30.
Amprenavir

Chemistry, mechanism of action, and antiviral activity
Amprenavir is a hydroxyethylamine sulfonamide peptidomimetric with a structure identified as (3S)-tetrahydro-3-furyl N-(1S,2R)-3-(4-amino-N isobutylbenzenesulfonamido)-1-benzyl-2-hydroxypropylcarbamate. It is active at a concentration of 10–20 nmol l−1. The oral bioavailability is >70% and peak plasma concentrations of 6.2–10 μg ml−1 are achieved after dosages of 600–1200 mg. The plasma half-life is 7–10 h. CSF concentrations are significant. Amprenavir is metabolized in the liver by the cytochrome P450 3A4 (CYP3A4) enzyme system.
Adverse effects
The most common adverse events are gastrointestinal events (nausea, vomiting, diarrhea, and abdominal pain/discomfort), which are mild to moderate in severity. Also, skin rash can occur in patients on amprenavir.
Resistance
Genotypic analysis of isolates from treatment-naive patients failing amprenavir-containing regimens showed mutations in the HIV-1 protease gene resulting in amino acid substitutions primarily at positions V32I, M46I/L, I47V, I50V, I54L/M, and I84V, as well as mutations in the p7/p1 and p1/p6 Gag and Gag-Pol polyprotein cleavage sites.
Fosamprenavir

Chemistry, mechanism of action, and antiviral activity
Fosamprenavir, a prodrug of amprenavir [(3S)-tetrahydrofuran-3-yl (1S,2R)-3-[[(4-aminophenyl) sulfonyl](isobutyl) amino]-1 benzyl-2-(phosphonooxy) propylcarbamate monocalcium salt], is an inhibitor of human HIV protease. Fosamprenavir is rapidly hydrolyzed to amprenavir by enzymes in the gut epithelium. After administration of a single dose of fosamprenavir to HIV-1-infected patients, the peak concentration occurs between 1.5 and 4 h (median 2.5 h). Amprenavir is metabolized in the liver by the cytochrome P450 3A4 (CYP3A4) enzyme system. The plasma elimination half-life of amprenavir is approximately 7.7 h.
Adverse effects
Side effects profile is similar to that of amprenavir.
Resistance
Fosamprenavir selects for amprenavir-associated mutations on treatment failure, though, at a much lower incidence.
Lopinavir

Chemistry, mechanism of action, and antiviral activity
Lopinavir [N-(4(S)-(2-(2,6-dimethylphenoxy)-acetylamino)-3(S)-hydroxy-5-phenyl-1(S)-benzylpentyl)-3-methyl-2(S)-(2-oxo(1,3-diazaperhydroinyl)butanamin)] is an inhibitor of the HIV protease, prevents cleavage of the Gag-Pol polyprotein, resulting in the production of immature, noninfectious viral particles. It is coformulated with ritonavir at 4:1 ratio (Kaletra). In the presence of 50% human serum, the mean EC50 values of lopinavir against HIV-1 laboratory strains ranges from 65 to 289 nmol l−1 (0.04–0.18 μg ml−1). It has some activity against HIV-2 strains. Lopinavir peak plasma concentration occurs approximately 4 h after administration. Lopinavir is metabolized by CYP3A, and ritonavir inhibits the metabolism of lopinavir, thereby increasing the plasma levels of lopinavir.
Adverse effects
Most common adverse events are nausea, diarrhea, increased cholesterol and triglycerides, and lipodystrophy.
Resistance
Virologic response to lopinavir/ritonavir has been shown to be affected by the presence of three or more of the following amino acid substitutions in protease at baseline: L10F/I/R/V, K20M/N/R, L24I, L33F, M36I, I47V,G48V, I54L/T/V, V82A/C/F/S/T, and I84V.
Atazanavir

Chemistry, mechanism of action, and antiviral activity
Atazanavir [(3S,8S,9S,12S)-3,12-Bis(1,1-dimethylethyl)-8-hydroxy-4,11-dioxo-9 (phenylmethyl)-6-[[4-(2-pyridinyl)phenyl]methyl]-2,5,6,10,13-pentaazatetradecanedioic acid dimethyl ester, sulfate (1:1)] is an azapeptide inhibitor of HIV-1 protease. Atazanavir exhibits anti-HIV-1 activity with an EC50 in the absence of human serum of 2–5 nmol l−1 against a variety of laboratory and clinical HIV-1 isolates in vitro.
Atazanavir is rapidly absorbed with a T max of approximately 2.5 h. Atazanavir is metabolized in the liver by the cytochrome P450 3A4 (CYP3A4) enzyme system. The mean elimination half-life of atazanavir in healthy volunteers and HIV-infected adult patients is approximately 7 h.
Adverse effects
The most common adverse event in patients is the asymptomatic elevations in indirect (unconjugated) bilirubin related to inhibition of UDP-glucuronosyl transferase (UGT). The hyperbilirubinemia is reversible upon discontinuation of atazanavir. Atazanavir may cause abnormal electrocardiogram findings, increased serum glucose, and lipodystrophy in some patients.
Resistance
HIV-1 isolates with a decreased susceptibility to atazanavir have been selected in vitro and obtained from patients treated with atazanavir or atazanavir/ritonavir. The mutations associated with resistance to atazanavir are I50L, N88S, I84V, A71V, and M46I. Atazanavir-resistant clinical isolates from treatment-naive harbored the I50L mutation (after an average of 50 weeks of atazanavir therapy), often, in combination with an A71V mutation. However, the viral isolates with the I50L mutation are phenotypically resistant to atazanavir but show in vitro susceptibility to other protease inhibitors (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir).
Tipranavir

Chemistry, mechanism of action, and antiviral activity
Tipranavir [2-Pyridinesulfonamide, N-[3-[(1R)-1-[(6R)-5,6-dihydro-4-hydroxy-2-oxo-6-(2-phenylethyl)-6-propyl-2H-pyran-3-yl]propyl]phenyl]-5-(trifluoromethyl)] is a nonpeptidic HIV protease inhibitor belonging to the class of 4-hydroxy-5,6-dihydro-2-pyrone sulfonamides. Tipranavir inhibits the replication of laboratory strains of HIV-1 and clinical isolates in vitro, with EC50 ranging from 0.03 to 0.07 μmol l−1 (18–42 ng ml−1).
The effective mean elimination half-life of tipranavir/ritonavir in healthy volunteers and HIV-infected adult patients is approximately 4.8 and 6.0 h, respectively, at steady state following a dose of 500/200 mg twice daily with a light meal. Tipranavir is predominantly metabolized by the CYP 3A4 enzyme system.
Tipranavir, coadministered with 200 mg of ritonavir, is used in combination with other anti-HIV agents for the treatment of HIV-1 infected adult who are highly treatment-experienced with evidence of viral replication, or have HIV-1 strains resistant to multiple protease inhibitors. Response rates are reduced if five or more protease inhibitor-associated mutations are present at baseline and patients are not given concomitant enfuvirtide with tipranavir/ritonavir.
Adverse effects
Adverse events include rash, increased cholesterol, increased triglycerides, lipodystrophy, and hepatitis. There have been reports of both fatal and nonfatal intracranial hemorrhage with the use of tipranavir/ritonavir. Tipranavir/ritonavir should be used with caution in patients who may be at risk of increased bleeding from trauma, surgery or other medical conditions, or who are receiving medications known to increase the risk of bleeding such as antiplatelet agents or anticoagulants.
Resistance
HIV-1 isolates that were 87-fold resistant to tipranavir were selected in vitro by 9 months and contained 10 protease mutations that developed in the following order: L33F, I84V, K45I, I13V, V32I, V82L, M36I, A71V, L10F, and I54V/T. In clinical trials tipranavir had less than fourfold decreased susceptibility against 90% of HIV-1 isolates resistant to amprenavir, atazanavir, indinavir, lopinavir, nelfinavir, ritonavir, or saquinavir. Tipranavir-resistant viruses selected for in vitro have decreased susceptibility to the protease inhibitors amprenavir, atazanavir, indinavir, lopinavir, nelfinavir, and ritonavir but remain sensitive to saquinavir.
Darunavir

Chemistry, mechanism of action, and antiviral activity
Darunavir, in the form of darunavir ethanolate, has the following chemical name: [(1S,2R)-3-[[(4-aminophenyl)sulfonyl](2-methylpropyl)amino]-2-hydroxy-1-(phenylmethyl) propyl]-carbamic acid (3R,3aS,6aR)-hexahydrofuro[2,3-b]furan-3-yl ester monoethanolate. It is an inhibitor of the HIV protease. Darunavir exhibits activity against laboratory strains and clinical isolates of HIV-1 and laboratory strains of HIV-2 with median EC50 values ranging from 1.2 to 8.5 nmol l−1 (0.7–5.0 ng ml−1). Darunavir, coadministered with 100 mg ritonavir twice daily, was absorbed following oral administration with a T max of approximately 2.5–4 h. The absolute oral bioavailability of a single 600 mg dose of darunavir alone and after coadministration with 100 mg ritonavir twice daily was 37 and 82%, respectively. Darunavir is primarily metabolized by CYP3A. Ritonavir inhibits CYP3A, thereby increasing the plasma concentrations of darunavir when given in combination.
Darunavir, coadministered with 100 mg ritonavir, and with other anti-HIV agents, is indicated for the treatment of HIV infection in antiretroviral treatment-experienced adult patients, such as those with HIV-1 strains resistant to more than one protease inhibitor.
Adverse effects
The most common treatment-emergent adverse events (>10%) reported in the de novo subjects, regardless of causality or frequency, were diarrhea, nausea, headache, and nasopharyngitis. Other side effects are increased triglycerides, increased cholesterol, lipodystrophy, increased glucose, and increased liver enzyme levels.
Resistance
Darunavir-resistant virus derived in cell culture from wild-type HIV had 6- to 21-fold decreased susceptibility to darunavir and harbored three to six of the following amino acid substitutions S37N/D, R41E/S/T, K55Q, K70E, A71T, T74S, V77I, or I85V in the protease. In phase IIb trial, the amino acid substitution V32I developed on darunavir/ritonavir (600/100 mg twice a day) in greater than 30% of virologic failure isolates and substitutions at amino acid position I54 developed in greater than 20% of virologic failure isolates. Other substitutions that developed in 10–20% of darunavir/ritonavir virologic failure isolates occurred at amino acid positions I15, L33, I47, G73, and L89.
Future Prospects in HIV Therapeutics
The simplification of HAART regimens has been a high priority for many years. As the number of effective drugs increases, so does the number of possible effective regimens. The trend toward fixed-dose combinations and once-daily dosage forms of many antiretroviral drugs has provided welcome relief to patients. Not only is their medication burden simplified, but as a consequence of improved adherence to therapy, they should experience better control of HIV and thus reduced morbidity.
New drug discovery strategies attempt at circumventing the current drug resistant problem by focusing on either novel targets or new compounds capable of suppressing HIV strains that are resistant to current inhibitors. There are several nucleoside analogues in preclinical and clinical studies. Notably are the novel 4′-substituted thymidine analogues with potent antiviral activity and less cytotoxic. An example is the recently discovered 2′,3′-didehydro-3′-deoxy-4′-ethynylthymidine, structurally related to stavudine, is a more potent inhibitor of HIV-1 replication and is much less inhibitory to mitochondrial DNA synthesis and cell growth in cell cultures than its progenitor stavudine. The triphosphate metabolite accumulates in cells much longer than stavudine, and exerts persistent antiviral activity even after removal of drug from culture. It also has a unique resistance profile when compared to other thymidine analogues and maintains activity against multidrug resistant HIV strains. It is currently in preclinical studies with phase I and II clinical trials anticipated in 2008. Other new NRTIs in phase II clinical trials are MIV-310, SPD754, and L-d4FC. A new non-nucleoside analogue in phase II trials is TMC125, it appears to have potent antiviral activity in treatment-experienced patients with resistance mutations to this drug class or in patients who are treatment naive. There is increasing number of compounds discovered as anti-HIV agents targeted at virtually any step in the replicative cycle of the virus and novel targets in development.
Summary
It is anticipated that new and effective treatments for viral infections will be available with the advent of modern and improved technology, based on molecular biology, combinatorial chemistry, and computer-aided design of compounds with greater specificity targeting on viral life cycle.
See also:
HIV/AIDS; Hepatitis Viruses; Herpesviruses; Influenza; Respiratory Viruses; Retroviruses; Virus Infection
Glossary
- alanine aminotransferase
An enzyme found in the liver and blood serum, the concentration of which is often elevated in cases of liver damage.
- antiretroviral agent
Any drug used in treating patients with human immunodeficiency virus (HIV) infection.
- antiviral resistance
The developed resistance of a virus to a specific drug.
- bilirubin
A greenish compound formed in the liver from the degradation of the hemoglobin from degraded red blood cells.
- bioavailability
The property of a drug to be absorbed and distributed within the body in a way that preserves its useful characteristics; for example, it is not broken down, inactivated, or made insoluble.
- chemoprophylaxis
Preventive treatment with chemical agents such as drugs.
- codon
A triplet of three consecutive nucleotide components in the linear genetic code in DNA or messenger RNA, which designates a specific amino acid in the linear sequence of a protein molecule.
- creatinine
An end product of energy metabolism found in the blood in uniform concentration, which is excreted by the kidney at a constant rate. Alterations of this rate are considered an indication of kidney malfunction.
- cytokine
One of a variety of proteins which has a regulatory effect on a cell.
- drug resistance
Decreased susceptibility to antiviral usually due to changes in the amino acid residues of target enzyme. For example, a substitution of valine for methionine at residue 184 of the reverse transcriptase enzyme of HIV confers resistance to lamivudine (M184V mutation, see Table 1 for letter codes of amino acids).
- EC50
Concentration of a drug that produces a 50% effect, for example, in virus yield.
- hemagglutinin
Specific glycoprotein molecules on the surface of some viruses, which have the property of binding to the surface of the red blood cells of some animal species. Because there are multiple binding sites, one virus can bind to two red cells causing them to clump (agglutinate).
- hepatotoxicity
Liver toxicity.
- interferon
Any group of glycoproteins with antiviral activity.
- lipoatrophy
Redistribution/accumulation of body fat including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and ‘cushingoid appearance’ observed in some patients receiving antiviral agents for HIV treatment.
- maintenance therapy
Drug treatment given for a long time to maintain its effect after the condition has been controlled or to prevent recurrence.
- monotherapy
Treatment with a single drug, contrasted with combination therapies with more than one drug at the same time.
- mutations
Changes to the base pair sequence of the genetic material of an organism.
- nephrolithiasis
The presence of kidney stones.
- nephrotoxicity
Kidney toxicity.
- neuraminidase
An enzyme, present on the surface of some viruses, which catalyzes the cleavage of a sugar derivative called neuraminic acid.
- peptidomimetic
A molecule having properties similar to those of a peptide or short protein.
- pharmacokinetic
Refers to the rates and efficiency of uptake, distribution, and disposition of a drug in the body.
- phase III
The final stage in testing of a new drug, after determination of its safety and effectiveness, in which it is tested on a broad range, and large population of patients for comparison to existing treatments and to test for rare complications.
- placebo
An agent used as a ‘control’ in tests of drugs. The placebo is an agent without the specific effects of the drug under test and is used to determine to what extent any observed effects of the drug are due to psychological effects or expectations. It is usually given to some patients while the test drug is given to others, but neither group knows which agent it is receiving (the so-called ‘blind’ design).
- prodrug
A drug that is given in a form that is inactive and must be metabolized in the body to the active form.
- prophylaxis
Prevention.
- protease
An enzyme that catalyzes the cleavage of proteins. In the case of HIV, a virus-specific protease is needed to cleave some of the virus coat proteins into their final, active form.
- protease inhibitor
A substance that inhibits the action of protease enzyme.
- replication cycle
The series of steps that a virus or cell goes through to multiply.
- shingles
Eruptive rash, usually in a girdle (L. cingulus; hence ‘shingles’) distribution on the trunk, resulting from infection with varicella zoster virus.
- T1/2
The time for reduction of some observed quantity, for example, the blood concentration of a drug, by 50%.
- teratogenesis
Production of fetal abnormalities by some agent.
- therapeutic index
The numerical ratio of the concentration needed to achieve a desired effect in 50% of the patients and the concentration that produces unacceptable toxicity in 50% of the patients.
- thymidine kinase
An enzyme that catalyzes the transfer of a phosphoryl group from a donor such as adenosine triphosphate to the sugar (deoxyribose) component of the thymidine molecule, a building block of DNA.
- viremia
The presence of virus in the bloodstream.
- virion
A complete virus, including the coat and nucleic acid core.
Acknowledgments
Work performed and reported by the authors was supported by Public Health Service grant AI-38204 from NIAID.
Portion of the current article were reproduced from the previous edition, written by Richard Whitley.
Further Reading
- Arvin A.M. Antiviral therapy for varicella and herpes zoster. Seminars in Pediatric Infectious Diseases. 2002;13(1):12–21. doi: 10.1053/spid.2002.29753. [DOI] [PubMed] [Google Scholar]
- Balfour H.H., Jr. Antivirals (non-AIDS) The New England Journal of Medicine. 1999;340:1255–1268. doi: 10.1056/NEJM199904223401608. [DOI] [PubMed] [Google Scholar]
- Cheng Y.C., Ying C.X., Leung C.H., Li Y. New targets and inhibitors of HBV replication to combat drug resistance. Journal of Clinical Virology. 2005;34(S1):S147–S150. doi: 10.1016/s1386-6532(05)80026-5. [DOI] [PubMed] [Google Scholar]
- De Clercq E. Antiviral drugs in current clinical use. Journal of Clinical Virology. 2004;30:115–133. doi: 10.1016/j.jcv.2004.02.009. [DOI] [PubMed] [Google Scholar]
- Desmond R.A., Accortt N.A., Talley L., Villano S.A., Soong S.J., Whitley R.J. Enteroviral meningitis: Natural history and outcome of pleconaril therapy. Antimicrobial Agents and Chemotherapy. 2006;50(7):2409–2414. doi: 10.1128/AAC.00227-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dusheiko G., Antonakopoulos N. Current treatment of hepatitis B. Gut. 2008;57(1):105–124. doi: 10.1136/gut.2005.077891. [DOI] [PubMed] [Google Scholar]
- Dworkin R.H., Johnson R.W., Breuer J. Recommendations for the management of herpes zoster. Clinical Infectious Diseases. 2007;44:S1–S26. doi: 10.1086/510206. [DOI] [PubMed] [Google Scholar]
- Jefferson T.O., Demicheli V., Di Pietrantonj C., Jones M., Rivetti D. Neuraminidase inhibitors for preventing and treating influenza in healthy adults. Cochrane Database of Systematic Reviews. 2006 doi: 10.1002/14651858.CD001265.pub2. Issue 3, Art. No.: CD001265. [DOI] [PubMed] [Google Scholar]
- Kleymann G., Fischer R., Betz U.A.K. New helicase-primase inhibitor as drug candidates for the treatment of herpes simplex disease. Nature Medicine. 2002;8(4):392–398. doi: 10.1038/nm0402-392. [DOI] [PubMed] [Google Scholar]
- McMahon M.A., Jilek B.S., Brennan T.P. The HBV drug entecavir – effects on HIV-1 replication and resistance. The New England Journal of Medicine. 2007;356:2614–2621. doi: 10.1056/NEJMoa067710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paintsil E., Dutschman G.E., Rong H. Intracellular metabolism and persistence of the anti-human immunodeficiency virus activity of 2′,3′-didehydro-3′-deoxy-4′-ethynylthymidine, a novel thymidine analog. Antimicrobial Agents and Chemotherapy. 2007;51(11):3870–3879. doi: 10.1128/AAC.00692-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka H., Haraguchii K., Kumamoto H., Baba M., Cheng Y.C. 4′-Ethynylstavudine (4′-Ed4t) has potent anti-HIV-1 activity with reduced toxicity and shows a unique activity profile against drug-resistant mutants. Antiviral Chemistry & Chemotherapy. 2005;16(4):217–221. doi: 10.1177/095632020501600402. [DOI] [PubMed] [Google Scholar]
- Whitley R.J. Antiviral agents. In: Lederberg J., editor. 2nd edn. vol. 2. Academic Press; San Diego: 2000. (Encyclopedia of Microbiology). [Google Scholar]
- Whitley R.J., Kimberlin D.W. Herpes simplex: Encephalisits children and adolescents. Seminars in Pediatric Infectious Diseases. 2005;16(1):17–23. doi: 10.1053/j.spid.2004.09.007. [DOI] [PubMed] [Google Scholar]
- Wu J.J., Pang K.R., Huang D.B. Advances in antiviral therapy. Dermatologic Clinics. 2005;23:313–322. doi: 10.1016/j.det.2004.09.001. [DOI] [PubMed] [Google Scholar]


