Abstract
Background
Treatment of arrhythmias evoked by accidental or therapeutic hypothermia and rewarming remains challenging. We aim to find an ECG-biomarker that can predict ventricular arrhythmias at temperatures occurring in therapeutic and accidental hypothermia.
Main body
Evaluation of ECG-data from accidental and therapeutic hypothermia patients and experimental data on ECG and ventricular fibrillation (VF) threshold in hypothermic New Zealand White Rabbits. VF threshold was measured in rabbit hearts cooled to moderate (31 °C) and severe (17 °C) hypothermia. QRS-interval divided by corrected QT-interval (QTc) was calculated at same temperatures. Clinical QRS/QTc data were obtained after a systematic literature review. Rabbit QRS/QTc values correlated with risk for VF (correlation coefficient: 0.97). Human QRS/QTc values from hypothermic patients, showed similar correlation with risk for ventricular fibrillation in the experimental data (correlation coefficient: 1.00).
Conclusions
These calculations indicate that QRS/QTc has potential as novel biomarker for predicting risk of hypothermia-induced cardiac arrest. Our findings apply both to victims of accidental hypothermia and to patients undergoing therapeutic hypothermia during surgery or after e.g. cardiac arrest.
Keywords: Hypothermia, Electrophysiology, Ventricular arrhythmias, Therapeutic hypothermia, Cardiac arrest
Background
Accidental hypothermia is a severe condition with high mortality rate, ranging between 25 and 40% in most studies [1]. In young patients succumbing to accidents at sea or harsh weather conditions, many life-years are lost. It is however possible to survive extreme exposure if correct treatment is provided. Hypothermia lowers metabolism and is neuroprotective, allowing survival after accidental cooling down to a core temperature of 13.7 °C [2]. Hypothermic patients are however at grave risk of developing refractory ventricular fibrillation (VF) and cardiac arrest with little chance of successful defibrillation during evacuation and transport to hospital [3]. Such witnessed hypothermic cardiac arrest is termed “rescue collapse” and Frei et al. found an associated mortality rate of 27% [4]. The pathophysiology has been largely unknown and it is therefore challenging to predict arrhythmias and rescue collapse in hypothermic patients, which is related to movement during extrication, mobilisation or transfer [4].
Main text
In a recent study [5], we found that cooling of rabbit hearts to mild-moderate hypothermia (31 °C) alters ventricular repolarisation while transmural conduction remains relatively unchanged. Rabbits were chosen do to the close resemblance to human cardiac electrophysiology [6]. When provoking arrhythmias by electrical stimulation in the rabbit model, we found that this temperature-dependent combination of effects increased risk for VF (decreased VF threshold) in moderate hypothermia and was pro-arrhythmic. Exposure to severe hypothermia (17 °C), conversely, decreased risk for VF as conduction and repolarisation was equally affected. These changes were reflected in QRS and QT-intervals on the ECG. Correcting the QT interval for heart rate reinforced the association between ECG-findings and pro-arrhythmic activity during hypothermia. We found that relative values of QRS-intervals to the corrected QT-interval, correlates with increased risk for ventricular arrhythmia in moderate hypothermia.
Based on these results, we found two biomarkers that correlate highly (correlation coefficient 0.97–0.98) with risk for cardiac arrest in hypothermic hearts, using Bazett’s (QTc) or Fredericia’s (QTf) correction of QT-interval. We find that QRS/QTc emerge as the most available clinical biomarker. It has a comparable correlation (0.97) with VF threshold and is available for calculation from previously published clinical data (Fig. 1).
Fig. 1.
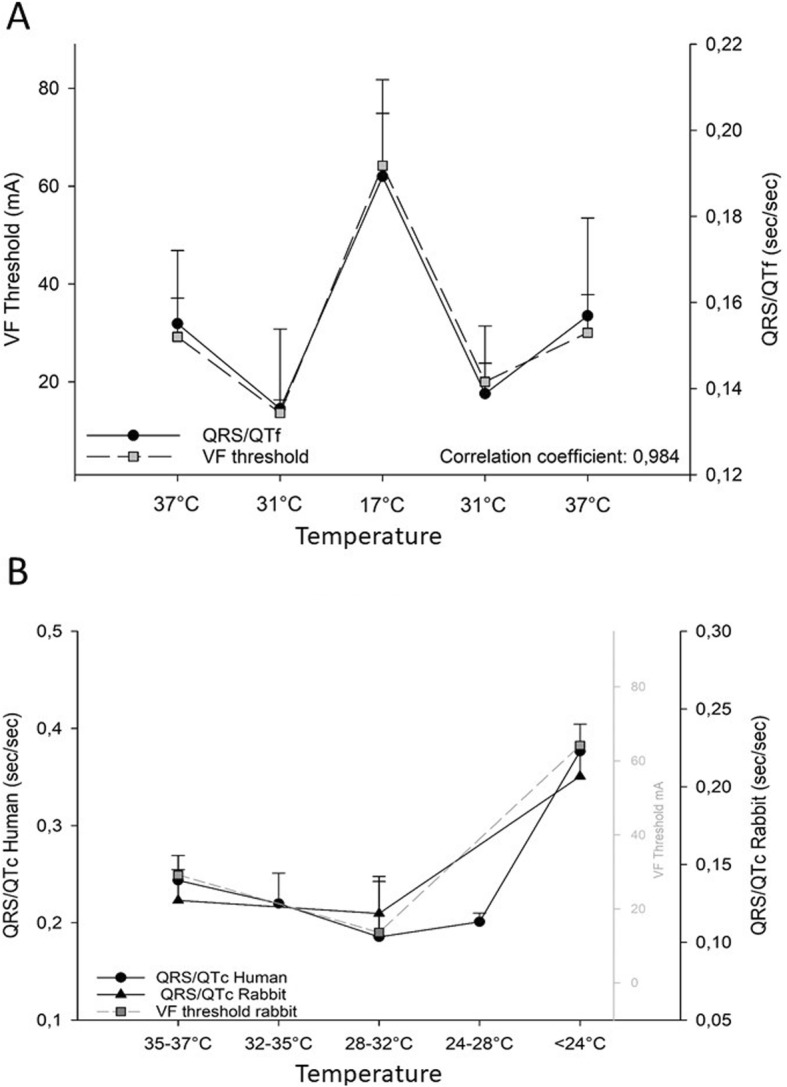
a We have found four potential biomarkers that correlate with risk for cardiac arrest in hypothermic rabbit hearts, calculated from QRS interval relative to Bazett’s (QTc) and Fredericia’s (QTf) correction of QT-interval. QRS/QTf is the most promising experimental biomarker. b QRS/QTc data from the included studies plotted against QRS/QTc and VF threshold values from rabbit. Human data showed high correlation (comparing 37 °C, 28–32 °C and < 24 °C) with both rabbit QRS/QTc (correlation coefficient: 0.97) and rabbit VF threshold (correlation coefficient: 1.00). Human values are given as mean (weighted for number of patients in each study) ± SD between study means weighted for number of patients in each study
To assess the clinical value of QRS/QTc in hypothermic patients, we extracted data from a recently published systematic review article of hypothermia and cardiac electrophysiology [1]. In a total of 8 studies on accidental and therapeutic hypothermia, QRS- and QTc-intervals were listed from patients that could be categorized (Table 1) into normothermia (35–37 °C) and varying degrees of hypothermia: 32–35 °C (mean 33.1 °C), 28–32 °C (mean 30.6 °C), 24–28 °C (mean 26.7 °C), and < 24 °C (mean 23.3 °C). As expected, at the lowest temperatures we found data from few patients, which must be taken account for when assessing QRS/QTc values from < 24 °C and 24–28 °C.
Table 1.
In a total of 8 studies [1] on accidental and therapeutic hypothermia, QRS- and QTc-intervals were published from patients that could be categorized into normothermia and varying degrees of hypothermia. Human values are given as mean (weighted for number of patients)
| Temperature | QRS mean (sec) | QTc mean (sec) | QRS/QTc | QTc/QRS | Patients n= | Included studies n= |
|---|---|---|---|---|---|---|
| 35–37 °C | 0,114 | 0,468 | 0,244 | 4,11 | 371 | 5 |
| 32–35 °C | 0,113 | 0,515 | 0,220 | 4,56 | 282 | 5 |
| 28–32 °C | 0,097 | 0,520 | 0,187 | 5,36 | 156 | 4 |
| 24–28 °C | 0,114 | 0,565 | 0,201 | 4,96 | 20 | 2 |
| < 24 °C | 0,160 | 0,425 | 0,389 | 2,66 | 2 | 1 |
In Fig. 1 we present QRS/QTc data from the included clinical studies plotted against QRS/QTc and VF threshold values from rabbit. Human data showed high correlation with both rabbit QRS/QTc (correlation coefficient: 0.97) and rabbit VF threshold (correlation coefficient: 1.00). This implies that QRS/QTc could predict risk for VF at different temperatures in hypothermic patients. As rescue collapse contributes to the high mortality rate in accidental hypothermia [4], prediction of VF risk could be of high clinical value. This would be relevant also in the in-hospital setting, where QRS/QTc could have a role in assessing safety of therapeutic hypothermia treatment. The inverse calculation; QTc/QRS could be an even more easily accessible clinical marker, relating higher values with higher risk for VF during hypothermia.
Conclusion
We believe that these calculations, as we have applied on preclinical and clinical data, have potential as novel biomarkers for predicting risk of hypothermia-induced cardiac arrest. QTc/QRS or QRS/QTc could easily be tested in the clinic, and have potential to be implemented in guidelines to predict rescue collapse and ease further clinical research into pharmacological prevention of this condition. Our findings apply both to victims of accidental hypothermia and to patients undergoing therapeutic hypothermia during surgery or after e.g. cardiac arrest, where a biomarker used for risk assessment would be of high value.
Acknowledgements
We thank A. Rankin and M. Dunne for technical assistance.
Declarations
All experiments from which data were used in this study, were undertaken in accordance with the United Kingdom Animals (Scientific Procedures) Act of 1986 and conform to the Guide for the Care and Use of Laboratory Animals published by the National Institutes of Health (NIH Publication No. 85–23, revised 1996).
Authors’ contributions
ESD analyzed the data, ESD, GS, RM and TT interpreted the data and wrote the manuscript. The authors read and approved the final manuscript.
Funding
This work was supported by a grant from the Northern Norwegian Health Authority [HNF1337–17 to ESD].
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Erik Sveberg Dietrichs, Email: erik.sveberg.dietrichs@uit.no.
Torkjel Tveita, Email: torkjel.tveita@uit.no.
Rachel Myles, Email: Rachel.myles@glasgow.ac.uk.
Godfrey Smith, Email: godfrey.smith@glasgow.ac.uk.
References
- 1.Dietrichs ES, Tveita T, Smith G. Hypothermia and cardiac electrophysiology: a systematic review of clinical and experimental data. Cardiovasc Res. 2019;115:501–509. doi: 10.1093/cvr/cvy305. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert M, Busund R, Skagseth A, et al. Resuscitation from accidental hypothermia of 13.7 degrees C with circulatory arrest. Lancet. 2000;355:375–376. doi: 10.1016/S0140-6736(00)01021-7. [DOI] [PubMed] [Google Scholar]
- 3.Khorsandi M, Dougherty S, Young N, et al. Extracorporeal life support for refractory cardiac arrest from accidental hypothermia: a 10-year experience in Edinburgh. J Emerg Med. 2017;52:160–168. doi: 10.1016/j.jemermed.2016.10.043. [DOI] [PubMed] [Google Scholar]
- 4.Frei C, Darocha T, Debaty G, et al. Clinical characteristics and outcomes of witnessed hypothermic cardiac arrest: a systematic review on rescue collapse. Resuscitation. 2019;137:41–48. doi: 10.1016/j.resuscitation.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Dietrichs ES, McGlynn K, Allan A, Connolly A, Bishop M, Burton F, Kettlewell S, Myles R, Tveita T, Smith GL. Moderate but not severe hypothermia causes pro-arrhythmic changes in cardiac electrophysiology. Cardiovasc Res. 2020:cvz309. 10.1093/cvr/cvz309. Online ahead of print. [DOI] [PMC free article] [PubMed]
- 6.Edwards AG, Louch WE. Species-Dependent Mechanisms of Cardiac Arrhythmia: A Cellular Focus. Clin Med Insights Cardiol. 2017;11:1179546816686061. 10.1177/1179546816686061. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.


