Abstract
Cholera was a major global scourge in the 19th century, with frequent large-scale epidemics in European cities primarily originating in the Indian subcontinent. John Snow conducted pioneering investigations on cholera epidemics in England and particularly in London in 1854 in which he demonstrated that contaminated water was the key source of the epidemics. His thorough investigation of an epidemic in the Soho district of London led to his conclusion that contaminated water from the Broad Street pump was the source of the disease and, consequently, the removal of the handle led to cessation of the epidemic. He further studied cholera in London homes that were receiving water from two water supply systems; one from the sewage contaminated portion of the Thames River and the other that drew its water upstream from an uncontaminated part of the river. Rates of infection among clients of the distribution system drawing contaminated water far exceeded the, rates among those served by the company whose water intake was from above the contaminated section of the river. This demonstration reinforced the goals of the sanitation movement, which developed sewage drainage systems and water purification systems in cities and towns in the following decades, therewith vastly reducing the threats of cholera, typhoid and many other waterborne diseases. Despite progress being made globally, the public health problems of waterborne disease, including cholera, are by no means gone today, even in high-income countries. The tragic introduction of cholera after the earthquake devastation in Haiti in 2010 resulted in many thousands of cases and deaths from cholera indicating the still-present dangers of diseases spread into disaster situations. Cholera and other waterborne diseases remain some of the heaviest burdens of disease and death in low-income countries, especially after natural disasters or warfare as in Yemen in 2017 and are continuing challenges for global health.
Keywords: John Snow, cholera, contaminated water, the Broad St pump, waterborne disease, cholera epidemics Haiti, Yemen, public health

Dr. John Snow (1813–58). London practicing obstetrician/anesthesiologist who conducted a detailed epidemiologic investigation of London cholera epidemic adjacent to the now famous Broad St. pump.
Courtesy: University of California at Los Angeles (UCLA) School of Public Health. Available at: http://www.ph.ucla.edu/epi/snow/snowcricketarticle.html

The Broad Street Pump, John Snow memorial, Broadwick Street (formerly Broad Street) in, London. In 1854 an epidemic of cholera affected residents of Soho district. Dr. John Snow surveyed deaths reported in the homes mostly near the pump and used it for their drinking water. His documented evidence suggested that contaminated water from this pump was the source of the epidemic; he caused removal of the handle, and the already declining epidemic due to people leaving the area, ceased entirely.
Source: Creative Commons photograph by Justine.

Map of London, 1854. Water-distribution systems, which John Snow investigated comparing cholera cases among consumers of water of two suppliers depending on the site of their water intake from the Thames River.
Courtesy University of California at Los Angeles (UCLA) School of Public Health. Available at: http://www.ph.ucla.edu/epi/snow/snowcricketarticle.html
Background
The 18th–19th centuries brought industrialization and large-scale population migration into cities of Europe including London. One result of this demographic shift was overcrowding in poor housing, served by inadequate or nonexistent public water supplies and waste-disposal systems. In London, the introduction of sewers and flushing toilets directly draining into the Thames led it to becoming an open stinking sewer, due to high tides and strong winds pushing seawater upstream. These conditions resulted in repeated outbreaks of water-borne diseases such as cholera, dysentery, tuberculosis, typhoid fever, influenza, yellow fever, and malaria, and other infectious diseases, as well as the loss of the fishing industry.
Cholera is an acute diarrhea caused by infection with the bacterium, Vibrato cholera. It is endemic in over 50 countries and also the cause of large epidemics. Since 1817, cholera spread rapidly throughout the world largely due to inadvertent transport of bilge water in ships mainly from the Bay of Bengal. The Indian subcontinent has been a long-term focus of cholera and the source of six worldwide epidemics between 1817 and 1923. The seventh cholera pandemic, which began in 1961, affects on an average 3–5 million people annually, with 120,000 deaths with large scale epidemics in Haiti, Yemen and in central Africa in the second decade of the 21st century.
Between 1848 and 1854, a series of cholera outbreaks occurred in London with large-scale loss of life. One epidemic of cholera occurred in the area of Broad Street, Golden Square, in Soho, a poor district of central London with unhygienic industries and housing.
John Snow was born in 1813 in York, England, the first of nine children. His father was a laborer and later a farmer. John saw unsanitary conditions in his hometown with a river contaminated by town sewage. As a medical apprentice from age 14, he experienced a cholera epidemic in a coal-mining village. Snow vowed to resist drink, gambling and marriage, and became a vegetarian. At age 23 he began medical studies and graduated from the University of London in 1844. John Snow, a physician now considered a founding father of modern epidemiology was the personal anesthetist to Queen Victoria and founding member of the London Epidemiological Society. In 1848, Snow was developing his anesthesia practice in the cholera afflicted district when he undertook an independent investigation of the epidemic.
By 1849, about 53,000 cholera deaths were registered for England and Wales. Snow was skeptical of the predominant Miasma Theory, and theorized that the cause of cholera was due to contaminated water as the main form of transmission. In 1854, a cholera epidemic broke out, affecting resident families of tailors and clerks from the shops of nearby Regent Street. The epidemic caused violent diarrhea and very high mortality, with some 600 deaths in one week during September 1854.
The prevailing Miasma Theory was that cholera was caused by airborne transmission of poisonous vapors from foul smells due to poor sanitation. At the same time, the competing Germ Theory that inspired Snow was still an unproven minority opinion in medical circles. Eventually, the foul smells, popularly known at the time as “The Great Stink” from the Thames River flowing past the Houses of Parliament were so severe that the MPs decided to take action. Finally, in 1864 with the plan of Sir Joseph Bazalgette, two enormous sewers were laid along the Thames, diverting the sewage downstream with development of sewage farms to manage the effluent. The system is still in use, but becoming too small to cope with the demands being placed on it as a result of increasing population and land development.
The Report of the Committee on Scientific Inquiries in Relation to the Cholera Epidemic of 1854 concluded that:
“Either in air or water it seems probable that the infection can grow. Often it is not easy to say which of these media may have been the chief scene of poisonous fermentation; for the impurity of one commonly implies the impurity of both; and in considerable parts of the metropolis (where the cholera has severely raged) there is rivalry of foulness between the two.”
When the next cholera epidemic struck London from August to September, 1854, primarily in the Soho area adjacent to Broad Street, Snow investigated it and traced some 600 cholera deaths occurring in a 10-day period. He was struck by the observation that the cases either lived close to or were using the Broad Street pump for drinking water. He also determined that brewery workers and poorhouse residents in the area, both of whom relied on local wells, escaped the epidemic. Snow concluded that access to uncontaminated water prevented them from cholera infection, while users of the Broad Street pump became infected. He persuaded the doubtful civic authorities to remove the handle from the Broad Street pump, and the already subsiding epidemic disappeared within a few days.
As noted in Snow’s report on cholera:
“The most terrible outbreak of cholera … took place (in London) in Broad Street, Golden Square, and the adjoining streets, a few weeks ago … there were upwards of five hundred fatal attacks of cholera in ten days. The mortality … probably equals any that was ever caused in this country, even by the plague; and it was much more sudden, … The mortality would undoubtedly have been much greater had it not been for the flight of the population … in less than six days … the most afflicted streets were deserted by more than three-quarters of their inhabitants.”
“There were a few cases of cholera in the neighborhood of Broad Street, Golden Square, in the latter part of August; and the so-called outbreak which commenced in the night of 31 August and the 1st September, was, in all similar instances only a violent increase of the malady. I suspected some contamination of the water of the much-frequented pump in Broad Street … but on examining the water. I found so little impurity in it of an organic nature … I requested … to take a list, at the General Registrar’s Office, of the deaths of cholera, registered during the week ending 2nd September … Eighty-nine deaths from cholera were registered during the week, in the three sub-districts.”
“I found that nearly all the deaths had taken place within a short distance of the pump … With regard to the deaths … there were sixty-one instances in which I was informed that the deceased persons used to drink the water from Broad Street, either constantly or occasionally…”
“The Workhouse in Poland Street is more than three-quarters surrounded by houses in which deaths from cholera occurred, yet out of five hundred and thirty five inmates, only five died of cholera … The Workhouse has a pump-well on the premises, in addition to the supply from the Grand Junction Waterworks, and the inmates never sent to the Broad Street for water. If the mortality in the Workhouse has been equal to that in the streets immediately surrounding it … upward of one hundred persons would have died.”
“There is a brewery in Broad Street, near the pump, and … no brewer’s men were registered as having died of cholera, … above seventy workmen employed in the brewery, none of them had suffered from cholera … at the time the disease prevailed. The men … do not drink water at all …. There is a deep well in the brewery, in addition to the New River water.”
“The result of the inquiry then was that there has been no particular outbreak or increase of cholera, in this part of London, except among the persons who were in the habit of drinking water of the above-mentioned pump-well. I had an interview with the Board of Guardians of St. James parish, … the handle of the pump was removed the following day.”
The cholera epidemic, which was already declining, fell off and disappeared once the pump usage stopped. As a result of this episode, Benjamin Disraeli, together with other members of Parliament, adopted the plan of the Thames Authority and passed legislation forcing the overhaul of London’s water and sewage systems, which after completion, contributed to the nonreturn of cholera.
In the next London cholera epidemic of September to October 1854, the highest rates of cholera occurred in areas of the city where two companies with overlapping water mains supplied homes. One of these—the Lambeth Company—moved its water intake to a less polluted part upstream of the Thames River, while the Southwark and Vauxhall company left its intake in a part of the Thames heavily polluted with sewage.
Again, suspecting water transmission, Snow’s investigation identified cases of mortality from cholera by place of residence and by the two water companies that supplied the homes. During the first four weeks the impure water of Southwark and Vauxhall accounted for fatalities 14 times as great as those of the Lambeth water supply. Snow calculated the cholera rates for a 7-week period in homes supplied by each of the two in possibly the most famous presentation table in epidemiology (Table 5.1 ).
Table 5.1.
Deaths From Cholera Epidemic in Districts of London Supplied by Two Water Companies Over 7 Weeks, 1854
| Water Supply Company | Number of Houses | Deaths From Cholera | Cholera Deaths per 10,000 Houses |
|---|---|---|---|
| Southwark and Vauxhall | 40,046 | 1,263 | 315 |
| Lambeth | 26,107 | 98 | 37 |
| Rest of London | 256,423 | 1,422 | 59 |
Source: Snow J. On the mode of transmission of cholera. London: John Churchill, 1855, pp. 55–98. Part 3, Table IX, Reprinted by UCLA Fielding School of Public Health 2001. Available at: http://www.ph.ucla.edu/epi/snow/snowbook3.html (accessed 26 June 2016).
Homes supplied by the Southwark and Vauxhall Water Company were affected by high cholera death rates, whereas adjacent homes supplied by the Lambeth Company had rates lower than throughout the rest of London. This provided overwhelming epidemiologic support for his hypothesis that the source of the cholera epidemic was the contaminated water from the Thames River, distributed to homes in a large area of south London.
Snow’s pioneering epidemiologic investigation proved the mode of transmission of a waterborne disease that ravaged many parts of the world in the 19th century and still occurs in the 21st century. The V. cholera organism was originally grown in 1854 but was reported in local Italian medical literature and not recognized internationally. International recognition for the definitive identification and growth of the organism during his investigation of an epidemic of cholera in Egypt was given to the eminent German bacteriologist, Robert Koch in 1883. Filipo Pucini was ultimately recognized for the discovery in 1984 when the organism was formally named Vibrio cholerae pucini 1854. Robert Koch was the discoverer of anthrax in 1880, and tuberculosis in 1882, and leader in defining criteria for causation of infectious diseases; he was awarded a Nobel Prize in Medicine in 1905 (see Chapter 7).
The Broad Street pump episode demonstrated that cholera was water-borne and thus the means to prevent it had already been identified almost 30 years before. Snow also established the basic methodology of modern public health for infectious disease investigation and contributed to establishing the validity of the Germ Theory, which was still highly controversial at this time.
With the understanding of the causal relation between microorganisms and diseases at the end of the 19th century, the process for reducing large-scale morbidity and mortality via disinfection was initiated. The first use of chlorine as a disinfectant for water facilities was in 1897 in England. The first use of this method for municipal water facilities in the United States was in Jersey City, New Jersey, and Chicago, Illinois, in 1915. Other cities followed and the use of chlorination as standard treatment for water disinfection rapidly grew. During the 20th century, death rates from waterborne diseases decreased significantly, and although other additional factors contributed to the general improvements in health (such as sanitation, improved quality of life, and nutrition), the improvement of water quality was, without doubt, a major reason. The decline in typhoid fever in the United States between 1900 and 1945 as a result of improved water supply systems and use of chlorination is seen in Figure 5.1 .
Figure 5.1.
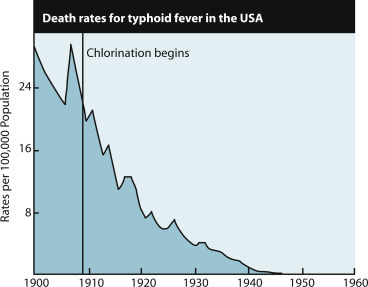
US mortality rates for typhoid fever and water chlorination.
Source: Chlorine Chemistry Council (C3) and Canadian Chlorine Coordinating Committee (C4). Drinking water chlorination: a review of disinfection practices and issues. Adapted from US Centers for Disease Control and Prevention, Summary of Notifiable Diseases, 1997. Available at: http://www.waterandhealth.org/drinkingwater/wp.html (accessed 16 August 2016).
The disinfection of drinking water through both filtration and chlorination processes has been one of the major achievements of public health. Clean water was responsible for nearly half the total mortality reduction in major cities, three-quarters of the infant mortality reduction, and nearly two-thirds of child mortality reduction.
Current Relevance
In 2014, an estimated 3–5 million cases of cholera occurred globally with more than 100,000 deaths, mainly in developing countries without safe drinking water treatment and sanitation.
Epidemics of cholera also occur in natural disaster situations, particularly in those areas where sanitation systems break down. A current example of such events is seen in Haiti, where an earthquake in 2010 killed over 200,000 people and displaced over one million persons. This was followed by a massive cholera outbreak 10 months later, with over 665,000 cases and 8,183 deaths. Intensive efforts of the Haitian Ministry of Health together with the Centers for Disease Control (CDC), World Health Organization (WHO), and other international organizations, with massive vaccinations against cholera, prevented thousands of deaths from cholera, but transmission of the disease continued in the following years.
Making matters worse, while Haiti was already struggling with effects of the cholera outbreak since 2010, a major hurricane (Hurricane Matthew) struck in October, 2016. The WHO shipped a million cholera vaccines to Haiti, attempting to minimize the risk of further increases of cases. The UN reports that since the cholera outbreak of 2010 some 780,000 persons have been infected with cholera and 9,145 have died of the disease. Moreover, since the hurricane in 2016, almost 800 new cases arise each week.
The cholera epidemic in Haiti since 2010 has been attributed to importation of the Vibrio bacterium by UN peacekeeper forces from Nepal, still a cholera-endemic country. The sewage contamination in UN peacekeeper camps with poor sanitation spread to nearby camps for displaced homeless Haitians following the earthquake.
Cholera can be imported via travelers from areas still endemic with cholera exposure to street, or other contaminated foods. Cholera and other waterborne diseases remain major global public health problems in the 21st century, particularly in areas of poverty. Both the WHO and the United Nations have recently acknowledged that the Haitian epidemic resulted from entry of the organism into poor hygienic camps by UN troops that were sent in to maintain order. Epidemiologists identified that the cholera strain found in Haiti was the same as one that originated in Nepal, where the disease is still endemic. Improving Haiti’s water and sanitation infrastructure is critical to achieving large health gains and reducing the opportunity for cholera to spread with responsibility attributed to United Nation peacekeeper soldiers from Nepal.
During the 1970s, in the medical and public health professions public health community there was a widespread idea that infectious diseases were gradually going to disappear under the combined influence of hygiene, antibiotics, and vaccines. This false sense of security was shattered with the advent of AIDS in the 1980s, and the subsequent return of diseases previously thought to be under control, such as tuberculosis, malaria, dengue, and plague. The complacency was replaced by a high degree of concern as new infectious diseases continued to arrive, such as HIV in the 1980s, bovine spongiform encephalopathy (BSE) in the 1990s, severe acute respiratory syndrome (SARS) in 2003, Ebola in 2015 and Zika virus in 2016 is now seen as a global public health crisis with few new antibiotics in the pipeline of development, testing, licensure and production. Growing resistance of many organisms to currently available antibiotics and health care associated infections, as well as spread of diseases from tropical areas to temperate zone countries in North America, Europe and other regions such as West Nile Fever, Chikungunya, and Zika. A further concern was the return of old diseases thought to be controlled such as the sexually transmitted diseases, as well as diphtheria and pertussis.
In the early 21st century, the spread of infectious diseases as weapons of terror and even war, including anthrax, came to grip the public and created a whole new spectrum of terrorism. In 2004, another concern came to the fore, with the lack of an influenza vaccine to protect vulnerable people in the population, due to difficulties with production and regulation. In particular, this placed caregivers at high risk of infecting patients or bringing the disease home from the hospital setting.
Today, waterborne disease is given less recognition, as standards of water and sewage treatment are assumed to be part of modern living. However, waterborne enteric disease continues to be among the major killers in many parts of the world, especially among children. Waterborne disease may be so common that it escapes detection in many countries, especially those where hepatitis (especially A and E) is endemic and where incidence of gastroenteritis from shigella, Escherichia coli, rotavirus, and many other enteric infectious agents remains high. Another example is Helicobacter pylori, the cause of chronic peptic ulcer disease and the recognized cause for gastric cancer. Helicobacter, which affects nearly half of the world’s population and is related to poverty and poor hygiene is also waterborne.
In Western industrialized countries, waterborne disease outbreaks have become relatively uncommon due to high levels of water management. Water contamination and enteric disease can also occur from organisms for which routine testing is not currently practiced. For example, testing for rotaviruses (which cause enteric disease) and organisms such as campylobacter and giardia is not routinely done, but water is tested if there is a suspicion of contamination.
In 1999, the CDC reported on achievements of public health during the 20th century in the United States addressing the problem of waterborne disease as follows:
By 1900, however, the incidence of many of these diseases had begun to decline because of public health improvements, implementation of which continued into the 20th century. Local, state, and federal efforts to improve sanitation and hygiene reinforced the concept of collective “public health” action (e.g., to prevent infection by providing clean drinking water). By 1900, 40 of the 45 states had established health departments. The first county health departments were established in 1908. From the 1930s through the 1950s, state and local health departments made substantial progress in disease prevention activities, including sewage disposal, water treatment, food safety, organized solid waste disposal, and public education about hygienic practices (e.g., foodhandling and handwashing). Chlorination and other treatments of drinking water began in the early 1900s and became widespread public health practices, further decreasing the incidence of waterborne diseases.
In 2003, bacterial contamination of the municipal water system in Walkerton, Ontario, Canada resulted in a public health disaster with 7 deaths and 2,300 persons ill. A public inquiry revealed that improper practices and systemic fraudulence by the public utility operators, privatization of municipal water testing, absence of mandatory criteria governing quality of testing, and the lack of provisions for notification of results to multiple authorities all contributed to the crisis. Warnings of significant concerns two years before the outbreak were ineffective as budgetary cuts destroyed the checks and balances needed to ensure municipal water safety.
Safe water also includes ensuring chemical safety through measures such as prevention of lead poisoning from deterioration in distribution systems, such as occurred in Flint, Michigan, in the United States, in 2015. Safe water supply requires exacting physical treatment as well as disinfection, especially of all surface water sources. Effective water management can reduce the burden of gastroenteric disease even in a relatively well-developed country.
Water treatment is one of the fundamentals of preserving public health not only at the sources. Residual chlorine throughout the distribution system prevents secondary contamination from faults in the pipes and leakage of sewage into the system. Many steps are essential for assurance of safe water supplies, including well-organized sanitary and laboratory monitoring by the public health authorities and not only the supplier. Yet waterborne diseases can occur and spread due to error, negligence or as in the case of Haiti unintended consequences of well meant interventions.
Cholera, typhoid fever, dysentery, and hepatitis A and E, and many other bacterial, viral, and parasitic diseases are waterborne diseases, i.e., caused by pathogens transmitted via water supplies. An immensely important public health challenge at the beginning of the 20th century was therefore the improvement and safety of drinking water quality, aiming to significantly reduce illness and death caused by contaminated drinking water.
In 1991, V. cholera O1 apparently arrived in a cargo ship from China whose sewage was spread into the harbor of Lima, Peru. It contaminated shellfish, popular among the local population, and therewith created a local epidemic that continued to spread in Central and South America between 1991 and 1994. The Pan American Health Organization (PAHO) reported a total of over one million cases and almost 10,000 deaths (case-fatality rate: 0.9%) from countries in the western hemisphere in this period. In southern Asia, an epidemic caused by a newly recognized strain of V. cholera, which began in late 1992, then spread to several areas of Central America, Brazil, and Argentina. In 2011, 58 countries from all continents reported a cumulative total of 589,854 cholera cases, representing an increase of 85 percent from 2010, with the greatest proportion of cases in Haiti and the African continent. In 2014, 55 percent of all reported cholera cases were from Africa and 15% from the Americas, the latter clearly resulting from the Haiti outbreak that started in 2010. The case fatality rate for cholera increased by 47 percent from 2013 compared to 2014. In 2014, a case fatality rate of 1.17 percent represented 190,549 cases and 2,231 deaths, mainly in Afghanistan, Democratic Republic of Congo (DRC), Ghana, Haiti, and Nigeria.
Waterborne disease outbreaks reported in the United States between 1920 and 2002, included at least 1,870 events associated with drinking water, an average of 22.5 per year, with 883,806 illnesses, for an average of 10,648 cases per year. Of more recent cases, just over half of the outbreaks had no organisms that were specifically identified but were epidemiologically identified as viral in origin. In addition to the disease outbreaks, these waterborne organisms constitute a special risk of death for persons with compromised immune systems, including cancer patients being treated with chemotherapy, HIV-positive persons, and patients being treated with immunosuppressants. Outbreaks of waterborne giardia and cryptosporidium in the United States raised concerns, because these organisms are not efficiently eliminated by standard water treatment.
Ethical Issues
The principal ethical issue is implementation of existing technology of public health globally to save human lives now being lost to waterborne and other diarrheal diseases. Diarrheal disease caused by contaminated water, food, or transmission from person to person can be caused by many bacteria, viruses, and parasites. Together, these are the second leading cause of death in children under 5 years of age, killing some 760,000 children every year. The most serious complication of severe diarrheal disease in young children results from dehydration due to the loss of fluids and salts necessary for survival. Dehydration is mostly treatable with oral rehydration solutions (ORS), one of the great public health innovations of the past half century, now used globally. Children most at risk are those that have been previously malnourished or with impaired immunity. Prevention includes access to safe drinking water; improved sanitation; handwashing with soap; exclusive breastfeeding for the first six months of life; good personal and food hygiene; health education about how infections spread; and rotavirus vaccination.
Clearly, the issues related to control of infectious diseases are not gone, nor are they likely to be without major new breakthroughs in vaccine production and new modes of treatment. But control of waterborne enteric diseases continues to depend on well-tested and effective traditional means of infectious disease control. Public health organizations require strong emphasis on monitoring of water security, adequate waste disposal systems, disease reporting systems, training of health workers and the public, and strong laboratory capacity and support.
Other causes of diarrheal disease morbidity are no less important. Rotavirus is a major cause of disease and death among children up to age five years, even in high- and medium-income countries. But the burden is mainly on low-income populations especially in low-income countries led by India, Nigeria, Pakistan, and sub-Saharan African countries. Oral rotavirus vaccines introduced in the industrialized world in 2006 have had a great impact in the United States, reducing hospitalizations for severe rotavirus by as much as 80 percent. Rotavirus globally is estimated by the WHO to cause annually approximately 111 million episodes of gastroenteritis, 25 million clinic visits, two million hospitalizations, and 352,000–592,000 deaths (median 440,000 deaths) in children up to five years of age.
Rotavirus causes severe acute gastroenteritis with diarrhea and vomiting, primarily in infants and young children. The oral vaccine has been introduced in 90 countries by the end of 2016, with global child coverage estimated at 25 percent, having been adopted in most high- and many medium-income countries and gradually introduced in low-income countries. Adoption of rotavirus vaccine in routine national immunization programs resulted in reduction of over 85 percent of rotavirus hospitalizations in Belgium, and similar reductions in hospitalizations for rotavirus-induced diarrheal conditions showed the high effectiveness of the rotavirus vaccines (over 85%). In many countries, the vaccine is only partially reimbursed on a per-prescription basis. A systematic review of ecological studies from eight countries reported a 49–89 percent decline in laboratory-confirmed rotavirus hospital admissions in children less than five years old within two years of vaccine introduction. Increasing the use of rotavirus vaccine with proven efficacy and cost effectiveness, along with efforts to improve access to safe water supplies, improved food and sewage management, and personal hygiene will continue to reduce the burden of disease and death in the vulnerable child population where sanitation is still poor. Clean sanitary facilities in homes supported by safe public sewage collection and treatment systems are essential for prevention of enteric infections. A World Bank data base review of percentage of homes with access to improved sanitary faclities with change between 1990 and 2015 showed high income countries such as the US, Canada, UK, Netherlands and Australia with 99–100% in both years. China increased from 48 to 77 percent, and India from 17 to 40 percent. Global coverage increased from 53 to 67 percent.
Meeting the goal of clean, safe drinking/potable water requires implementing a multibarrier approach that includes: protecting source water from contamination, appropriately treating raw source water, especially surface water, and ensuring safe distribution of treated water to the consumers. While chlorination is a mainstay in protecting water supplies, filtration and coagulation are equally important. Filtration, coagulation, and disinfection of water are the optimal combination known to date, where chlorination kills or inactivates bacteria and viruses and filtration completes the action of eliminating pathogens in particles and eliminating parasitic protozoa.
Wastewater includes water with human waste, food scraps, oils, soaps, and chemicals from homes, from industry, and from storm runoff. Untreated wastewater discharged to nature can damage the environment and groundwater, making treatment essential. Nature copes well with small amounts, but can be overwhelmed by large amounts of untreated wastewater and sewage. Treatment plants reduce pollutants in wastewater to a level nature can handle. Government regulation of business, industry, and local authorities is a vital part of modern public health. Business and industry are legally accountable, but not well enforced, for ensuring their wastewater runoff is within accepted standards. Use of wastewater for irrigation after extensive treatment for irrigation is part of modern water economies and within supervised standards for field and orchard crops and even in vegetables and other ground crops, including for newly emerging pathogens and chemicals.
Chemical disinfectants in water treatment and sewage usually can result in the formation of chemical byproducts. However, the risks to health from these byproducts are extremely small in comparison to the risks associated with inadequate disinfection. Disinfection efficacy should not be compromised in attempting to control such byproducts. The main advantage of chlorine-based water disinfection over other methods (such as ozone and UV radiation) is its long-lasting effect; its presence also prevents the regrowth of microorganisms, thereby protecting clean water throughout the distribution system. Chlorine as a disinfectant is also easily monitored and controlled as a drinking-water disinfectant, and frequent monitoring is recommended wherever chlorination is practiced.
Private water supplies, such as wells, used by millions of people even in high-income countries are not government regulated or well protected. Contamination by animal excretions and agricultural runoff are of serious concern. These sources of water can be made safe by fencing and hard surrounding platform along with regular use of household chlorine (5.25%) bleach. Potential contaminants include microorganisms of human and animal waste products. Chemical contaminants from natural and man-made sources can be equally hazardous.
Cholera continues to spread across many countries with dramatic consequences, overwhelming stretched health systems and diverting resources from other crucial prevention-oriented programs. Global priority for increasing safe water supply as part of the MDGs did achieve its targets of increasing access to safe water, but cholera itself has not been a topic of major priority in global health.
The UN report on MDGs indicates that the global target of halving the proportion of people without access to improved sources of water was met five years ahead of schedule. Between 1990 and 2015, 2.6 billion people gained access to improved drinking water sources. Worldwide 2.1 billion people have gained access to improved sanitation. Despite progress, 2.4 billion are still using unimproved sanitation facilities, including 946 million people still practicing open defecation.
However, WHO reestablished a Global Task Force on Cholera Control in 2012 to increase the visibility of cholera as an important global public health challenge. This emphasizes disseminating information about cholera prevention and control and conducting advocacy and resource mobilization activities to support cholera prevention and control at national, regional, and global levels with participation by the international community of donors and public health professionals.
Cholera can appear in disaster situations such as in severe floods, and other natural calamities including earthquakes, tsunamis, and floods, as well as manmade catastrophes including civil wars and refugee situations as well.
In the second decade of the 21st century, major epidemics of cholera are wreaking havoc in man-made and natural disaster settings. In post-hurricane Haiti as a result of imported vibrio by UN peacekeeper forces and recklessly poor sanitation, contamination of water used by a displaced persons’ camp in 2010 resulted in a devastating cholera epidemic persisting for years. This has killed more than 11,000 people and left more than 880,000 infected by June 2017. A deadly cholera epidemic is raging in war torn Yemen with over 200,000 cases and 1,500 deaths reported by WHO. Cholera is also rampant in strife-torn East Africa with Red Cross reports of 51,000 cholera cases in Somalia and nearly 5,000 in South Sudan associated with famine, poor supply of food aid in a vicious tragedy mainly of man-made causes.
Economic Issues
In 1993 in the United States contamination of water sources with the parasite cryptosporidium caused major waterborne disease outbreaks in Milwaukee, Wisconsin and elsewhere. The Milwaukee outbreak was the largest reported waterborne disease outbreak in US history, with approximately 403,000 ill persons with 4,400 hospitalizations. Attack rates were as high as 50 percent in some parts of the city. Cryptosporidium is transmitted from person to person and from animals to humans, but can also be transmitted in swimming pools and community waters. Cryptosporidium was reportedly present in 65–87 percent of surface water samples tested in the United States. The total cost of illness in this outbreak was calculated at $96.3 million: $31.7 million in medical costs and $64.6 million in productivity losses.
Giardia lamblia is another parasite that can be transmitted in inadequately filtered surface water and for which chlorination is inadequate to disinfect. In the period 2011–12, in the United States 32 drinking water-associated outbreaks were reported, with at least 431 cases of illness, 102 hospitalizations, and 14 deaths. Legionella was responsible for 66 percent of these outbreaks and 26 percent of illnesses; other bacteria and viruses accounted for 16 percent of outbreaks and 53 percent of illnesses.
Helicobacter pylori as the major cause of acute and chronic peptic ulcer disease (PUD) and gastric cancer is known to be related to hygienic conditions including water safety, and is thought to be prevalent in more than half the world population with a high economic impact on health systems. One of the important measures for its control is water security, especially for low- and medium-income countries (see Chapter 22).
Prevention of waterborne diseases requires high standards for community, food, and personal hygiene, sanitation including garbage disposal, supply and treatment of safe drinking water, and prohibiting the use of raw or partially treated sewage for irrigation of crops. Sanitation, particularly the filtration and chlorination of drinking water, prohibiting the use of raw or partially treated sewage for the irrigation of ground crops. Crucial treatment for diarrhea is prompt fluid therapy with sugar electrolytes in large volumes to replace all fluid loss with oral rehydration therapy (ORT). Using this form of treatment can successfully treat up to 80 percent of cholera cases. Tetracycline shortens the duration of the disease, and chemoprophylaxis for contacts following stool samples may help in reducing its spread. A vaccine is also available, which can help to control outbreaks. Rehydration is a cornerstone of treatment and can reduce the fatality rate to less than one percent.
Cholera and its burden on a country serve as indicators of poverty and inadequate social infrastructure and development. It persists as a major public health challenge in developing countries that lack fundamental sanitary infrastructure, with effective public health systems capable of providing clean, safe water. Due to unsanitary living conditions, these populations and communities are at high risk of major cholera outbreaks as well as other diarrheal diseases.
Cholera infection still endemic in more than 50 countries is caused by V. cholera O1 (99% of cases worldwide), which produces a toxin causing severe watery diarrhea that can be rapidly fatal without treatment of dehydration. Globally, gastroenteric infections kill some three million children per year and must remain one of the high priority issues in international aid for the coming decades. Even industrialized countries with proper sanitation and water supply systems face the risks of waterborne disease outbreaks, since these can occur due to malfunctions and human error in monitoring water supply and safety, as the examples of Milwaukee and Walkerton, Canada, in 2003 showed.
The United Nations 1966 International Covenant on Economic, Social and Cultural Rights (ICESCR) confirmed the right to water in international law, noting that such a right is “indispensable for leading a life in human dignity” and “a prerequisite for the realization of other human rights.” This international commitment was reaffirmed in 2002 that: The “human right to water entitles everyone to sufficient, safe, acceptable, physically accessible and affordable water for personal and domestic uses” (see Box 5.1 ). This right is implicit in the rights to health, housing, food, life, and dignity enshrined in other international conventions, such as the International Bill of Human Rights and the Convention on the Rights of the Child. The focus is explicitly on the responsibilities of governments for delivering clean water and adequate sanitation services to all.
Box 5.1. United Nations: Human Rights to Water and Sanitation.
Sufficient and continuous water supply for personal and domestic uses; the WHO estimates this should be 50–100 liters per person daily.
Safe, i.e., free from microorganisms, chemical substances, and radiological hazards that threaten health.
Acceptable in color, taste, and odor.
Physically accessible, i.e., within 1,000 meters of the home and collection time not to exceed 30 minutes, and safe for gender privacy.
Affordable for all and costs should not exceed three percent of household income.
Source: United Nations. Available at: http://www.un.org/waterforlifedecade/human_right_to_water.shtml (accessed 14 November 2016).
The global initiative of the Millennium Development Goals (MDGs) from 2001 to 2015 was a consensus-combined effort of 140 countries to achieve reduced poverty, improved education and health of women and children, and improved access to sanitation, as well as control of diseases such as malaria, HIV, and TB. The MDGs included a specific goal to increase access to safe water supplies. Since 2011, the WHO Global Task Force on Cholera Control has also worked to support the design and implementation of global strategies to contribute to capacity development for cholera prevention and control.
Between 1990 and 2015, progress was made so that 1.9 billion people gained access to piped drinking water and 2.1 billion people gained access to improved sanitation. After the MDGs the UN created Sustainable Development Goals (SDGs), which incorporate many of the MDG goals and an agenda for global sustainable development until 2030. Among the 17 goals, number six is on “clean water and sanitation,” and other goals are likely to seek to contribute to prevention and control of waterborne diseases (e.g., Goal 3: Good Health and Well-being).
Conclusion
Policy initiatives are essential to support the development and implementation of global strategies for policy and capacity development for cholera prevention locally, nationally, and globally. This is meant to promote donor support, technical exchange, coordination, and cooperation on cholera-related activities; to strengthen countries’ policies and capacity to prevent and control cholera; to disseminate technical guidelines and operational manuals; and to support development of a research agenda with emphasis on evaluating innovative approaches to cholera prevention and control in affected countries.
Snow’s brilliant, game-changing studies of cholera in 1854 earned him the title “the father of modern epidemiology.” His work led directly to steps taken to improve water safety in London, setting new standards for other urban centers across the industrialized world, resulting in cholera, typhoid, and other enteric infectious diseases largely disappearing in many countries and saving of millions of lives over the years. Yet cholera, along with many other waterborne diseases, remains a serious challenge to public health with severe health, economic, and social effects globally particularly on the poorest populations, especially those in developing countries or in disaster situations in the 21st century.
The potential to relieve suffering and death from cholera, and other gastroenteric infections from contaminated water (and food) resulting from John Snow’s work, is still far from being fully achieved. But his contribution has saved millions of lives. Improving sanitation and reducing poverty are still closely linked issues in public health today in both industrialized and developing countries. The WHO has called for recognition of cholera as a Neglected Tropical Disease and promotes its prevention and control globally. But clearly cholera and its many brother waterborne diseases are real and present dangers in a globalized world with millions traveling for business, tourism, and migration. John Snow pointed the way, and the modern world needs to apply lessons learned from this case.
The WHO Global Task Force on Cholera Control, and WHO work to:
-
1.
Support the design and implementation of global strategies to contribute to capacity development for cholera prevention and control globally;
-
2.
Provide a forum for technical exchange, coordination, and cooperation on cholera-related activities to strengthen countries’ capacity to prevent and control cholera;
-
3.
Support countries for the implementation of effective cholera control strategies and monitoring of progress;
-
4.
Disseminate technical guidelines and operational manuals;
-
5.
Support the development of a research agenda with emphasis on evaluating innovative approaches to cholera prevention and control in affected countries;
-
6.
Increase the visibility of cholera as an important global public health problem through the dissemination of information about cholera prevention and control, and
-
7.
Conduct advocacy and resource mobilization activities to support cholera prevention and control at national, regional, and global levels.
Recommendations
The following recommendations represent key lines of action highlighting the Millennium Development Goals and the follow-up Sustainable Development Goals recommended actions for increased access to safe water supplies and preventive care for diarrheal disease which despite progress with MDGs are still one of the leading causes of death under age 5 globally.
-
1.
Continued global health efforts of the WHO and UN and other international agencies should expand efforts to improve safe water, improved sanitary home facilities and safe community sewage management in low- and medium-income countries.
-
2.
Control and elimination of cholera and other microbiological causes of severe diarrheal disease must be given high priority on the global health agenda with training and improved safety of water sources and distribution systems.
-
3.
Research to develop effective vaccines that can be introduced to routine vaccination programs such as has successfully occurred with rotavirus vaccine should be of high priority of public private partnerships working to advance global health.
-
4.
Funding assistance to low-income countries and poor regions of middle- and high-income countries and donors should include resources for the essential water infrastructure and monitoring systems and training of monitoring and laboratory personnel.
-
5.
Education for public health workers, political leaders, and the general public should stress the multiple interventions needed to ensure the quality and quality of safe drinking water, improved home sanitary facilities and community sewage systems, as fundamental to public health especially for preparation in disaster situations.
Student Review Questions
-
1.
How did the emptying of raw sewage into the Thames River contribute to the cholera epidemics of the 1850s?
-
2.
What were the alternative explanations for the London cholera epidemics at the time of the mid-19th century epidemics?
-
3.
What were the characteristics of the cholera epidemics discovered by Snow in his investigation that led to him identify water as the vehicle for transmission of the disease?
-
4.
What is the state of waterborne gastroenteric disease in the total burden of disease globally at the present time?
-
5.
How did cholera become established in Haiti following the earthquake and hurricane in 2004 and 2016? What happened as a result of the presence of United Nations troops contaminating local sewage near a refugee camp?
-
6.
What are the key prevention measures of waterborne diseases crucial to public health?
-
7.
What are the key components for assuring safety of community water supplies?
-
8.
How are cryptosporidium, shigellosis, rotavirus, and Helicobacter pylori related to cholera?
-
9.
What are the differences between proof of association and proof of causation in epidemiology? Explain which applied to John Snow's studies?
-
10.
What are the advantages and disadvantages of chlorine disinfection of community and household water supplies?
Recommended Readings
- 1.Anderson C. Cholera epidemic traced to risk miscalculation. Nature. 1991;354:255. doi: 10.1038/354255a0. [DOI] [PubMed] [Google Scholar]
- 2.Albert M.J., Neira M. The role of food in the epidemiology of cholera. World Health Stat Q. 1997;50(1–2):111–118. Abstract available at: http://www.ncbi.nlm.nih.gov/pubmed/9282393 (accessed 29 June 2016) [PubMed] [Google Scholar]
- 3.Ali M., Nelson A.R., Lopez A.L., Sack D.A. Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis. 2015;9(6):e0003832. doi: 10.1371/journal.pntd.0003832. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4455997/pdf/pntd.0003832.pdf (accessed 20 August 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benedict K.M., Reses H., Vigar M., Roth D.M., Roberts V.A., Mattioli M. Surveillance for waterborne disease outbreaks associated with drinking water — United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2017;66:1216–1221. doi: 10.15585/mmwr.mm6644a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beer K.D., Gargano J.W., Roberts V.A., Hill V.A., Garrison L.E., Kutty P.K. Surveillance for waterborne disease outbreaks associated with drinking water—United States, 2011–2012. Morb Mortal Wkly Rep. 2015;64(31):842–848. doi: 10.15585/mmwr.mm6431a2. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6431a2.htm (accessed 26 June 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Update: Vibrio cholerae 01—Western Hemisphere, 1991–1994, and V. cholerae 0139—Asia, 1994. Morb Mortal Wkly Rep. 1995;44(11):215–219. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/00036609.htm (accessed 4 July 2016) [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention Achievements in public health, 1900–1999: control of infectious diseases. Morb Mortal Wkly Rep. 1999;48(29):621–629. Available at: http://www.cdc.gov/mmwr/pdf/wk/mm4829.pdf (accessed 29 June 2016) [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention A century of U.S. water chlorination and treatment: one of the ten greatest public health achievements of the 20th century. Morb Mortal Wkly Rep. 1999;48(29):621–629. Available at: http://www.cdc.gov/healthywater/drinking/history.html (accessed 17 August 2016) [Google Scholar]
- 9.Centers for Disease Control and Prevention Cholera epidemic associated with raw vegetables—Lusaka, Zambia, 2003–2004. Morb Mortal Wkly Rep. 2004;53(34):783–786. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5334a2.htm (accessed 29 June 2016) [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention 150th anniversary of John Snow and the pump handle. Morb Mortal Wkly Rep. 2004;53(34):783. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5334a1.htm (accessed 4 July 2017) [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Haiti cholera outbreak: cholera in Haiti one year later, 2011. Available at: https://www.cdc.gov/cholera/haiti/haiti-one-year-later.html (accessed 26 June 2016).
- 12.Centers for Disease Control and Prevention. Cholera in Haiti, 2014. Available at: http://www.cdc.gov/cholera/haiti/index.html (accessed 26 June 2016).
- 13.Centers for Disease Control and Prevention. Water treatment, community water treatment, 2015. Available at: http://www.cdc.gov/healthywater/drinking/public/water_treatment.html (accessed 26 June 2016).
- 14.Chin C.S., Sorenson J., Harris J.B., Robins W.P., Charles R.C., Jean-Charles R.R. The origin of the Haitian cholera outbreak strain. N Engl J Med. 2011;364(1):33–42. doi: 10.1056/NEJMoa1012928. Available at: http://www.nejm.org/doi/full/10.1056/NEJMoa1012928 (accessed 15 August 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chlorine Chemistry Council and Canadian Chlorine Coordinating Committee. Water quality and health. Drinking water chlorination, a review of disinfection practices and issues. Available at: http://www.waterandhealth.org/drinkingwater/wp.html (accessed 16 August 2016).
- 16.Corso P.S., Kramer M.H., Blair K.A., Addin D.G., Davis J.P., Haddix A.C. Cost of illness in the 1993 waterborne Cryptosporidium outbreak, Milwaukee, Wisconsin. Emerg Infect Dis. 2003;9(4):426–431. doi: 10.3201/eid0904.020417. Available at: http://wwwnc.cdc.gov/eid/article/9/4/02-0417_article (accessed 26 June 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Craun M.F., Craun G.F., Calderon R.L., Beach M.J. Waterborne outbreaks reported in the United States. J. Water Health. 2006;4(Suppl. 2):19–30. doi: 10.2166/wh.2006.016. Abstract available at: http://www.ncbi.nlm.nih.gov/pubmed/16895084 (accessed 26 June 2016) [DOI] [PubMed] [Google Scholar]
- 18.Crockett C.S. The role of wastewater treatment in protecting water supplies against emerging pathogens. Water Environ Res. 2007;79(3):221–232. doi: 10.2175/106143006x111952. Abstract available at: http://www.ncbi.nlm.nih.gov/pubmed/17469654 (accessed 20 August 2016) [DOI] [PubMed] [Google Scholar]
- 19.Crump J.A., Mintz E.D. Global trends in typhoid and paratyphoid fever. Clin Infect Dis. 2010;50(2):241–246. doi: 10.1086/649541. Available at: http://cid.oxfordjournals.org/content/50/2/241.long (accessed 17 August 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cutler D., Miller G. The role of public health improvements in health advances: the twentieth-century United States. Demography. 2005;42(1):1–22. doi: 10.1353/dem.2005.0002. Available at: http://www.ncbi.nlm.nih.gov/pubmed/15782893. [DOI] [PubMed] [Google Scholar]
- 21.Department of Epidemiology, Fielding School of Public Health, University of California at Los Angeles (UCLA). John Snow. Available at: http://www.ph.ucla.edu/epi/snow.html (accessed 5 July 2017).
- 22.Esrey S.A., Potash J.B., Roberts L., Shiff C. Effects of improved water supply on ascariasis, diarrhoea, dracunculiasis, hookworm infection, schistosomiasis, and trachoma. Bull World Health Organ. 1991;69:609–621. Available at: http://apps.who.int/iris/bitstream/10665/48164/1/bulletin_1991_69%285%29_609-621.pdf (accessed 12 November 2016) [PMC free article] [PubMed] [Google Scholar]
- 23.Frerichs R.R., Keim P.S., Barrais R., Piarroux R. Nepalese origin of cholera epidemic in Haiti. Clin Microbiol Infect. 2012;18(6):E158–E163. doi: 10.1111/j.1469-0691.2012.03841.x. Available at: http://www.sciencedirect.com/science/article/pii/S1198743X14641343 (accessed 14 November 2016) [DOI] [PubMed] [Google Scholar]
- 24.George G., Rotich J., Kigen H., Catherine K., Waweru B., Boru W. Notes from the field: ongoing cholera outbreak—Kenya, 2014–2016. Morb Mortal Wkly Rep. 2016;65:68–69. doi: 10.15585/mmwr.mm6503a7. [DOI] [PubMed] [Google Scholar]
- 25.Harris J.B., LaRocque R.C., Qadri F., Ryan E.T., Calderwood S.B. Cholera. Lancet. 2012;379(9835):2466–2476. doi: 10.1016/S0140-6736(12)60436-X.V. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.History of the Thames 1999–2016. Available at: http://www.riverthames.co.uk/history.htm (accessed 15 July 2016).
- 27.Hrudey S.E., Payment P., Huck P.M., Gillam R.W., Hrudey E.J. A fatal waterborne disease epidemic in Walkerton, Ontario: comparison with other waterborne outbreaks in the developed world. Water Sci Technol. 2003;47(3):7–14. Available at: http://www.ncbi.nlm.nih.gov/pubmed/12638998 (accessed 26 June 2016) [PubMed] [Google Scholar]
- 28.Hurst C.J. Presence of enteric viruses in freshwater and their removal by the conventional drinking water treatment process. Bull World Health Organ. 1991;69:113–119. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2393205/pdf/bullwho00046-0120.pdf (accessed 26 June 2016) [PMC free article] [PubMed] [Google Scholar]
- 29.Katz JM. UN admits role in Cholera epidemic in Haiti. Available at: https://www.nytimes.com/2016/08/18/world/americas/united-nations-haiti-cholera.html?_r=1 (accessed 19 August 2016).
- 30.MacKenzie W.R., Hoxie N.J., Proctor M.E., Gradus M.S., Blair K.A., Peterson D.E. A massive outbreak in Milwaukee of cryptosporidium infection transmitted through the public water supply system. N Engl J Med. 1994;331:161–167. doi: 10.1056/NEJM199407213310304. Available at: http://www.nejm.org/doi/pdf/10.1056/NEJM199407213310304 (accessed 25 June 2016) [DOI] [PubMed] [Google Scholar]
- 31.Morris J.G. Cholera—modern pandemic disease of ancient lineage. Emerg Infect Dis. 2011;17:2099–2104. doi: 10.3201/eid1711.111109. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3310593/ (accessed 16 August 2012) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paneth N., Vinten-Johansen P., Brody H., Rip M. A rivalry of foulness: official and unofficial investigations of the London cholera epidemic of 1854. Am J Public Health. 1998;88:1545–1553. doi: 10.2105/ajph.88.10.1545. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1508470/pdf/amjph00022-0105.pdf (accessed 4 July 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Piarroux R., Barrais R., Faucher B., Haus R., Piarroux M., Gaudart J. Understanding the cholera epidemic, Haiti. Emerg Infect Dis. 2011;17(7):1161–1168. doi: 10.3201/eid1707.110059. Available at: http://wwwnc.cdc.gov/eid/article/17/7/11-0059_article#r32 (accessed 26 June 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reuters Health News. U.N. remarks on Haiti cholera a “groundbreaking” step to justice, say lawyers, August 18, 2016. Available at: http://www.reuters.com/article/us-haiti-cholera-idUSKCN10T209 (accessed 13 November 2016).
- 35.Rosen G. A history of public health. Expanded edition. The Johns Hopkins University Press; Baltimore, MD: 1993. [Google Scholar]
- 36.Sabbe M., Berger N., Blommaert A., Ogunjimi B., Grammens B., Callens M. Sustained low rotavirus activity and hospitalisation rates in the post-vaccination era in Belgium, 2007 to 2014. Euro Surveill. 2016;21(27):pii=30273. doi: 10.2807/1560-7917.ES.2016.21.27.30273. Available at: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=22518 (accessed 8 July 2016) [DOI] [PubMed] [Google Scholar]
- 37.Salvadori M.I., Sontroop J., Garg A.X., Moist L.M., Suri R.S., Clark W.F. Factors that led to the Walkerton tragedy. Kidney Int Suppl. 2009;112:S33–S34. doi: 10.1038/ki.2008.616. Available at: http://www.kidney-international.org/article/S0085-2538(15)53612-0/pdf (accessed 16 August 2016) [DOI] [PubMed] [Google Scholar]
- 38.Schoenen D. Role of disinfection in suppressing the spread of pathogens with drinking water: possibilities and limitations. Water Res. 2002;36(15):3874–3888. doi: 10.1016/s0043-1354(02)00076-3. Abstract available at: http://www.ncbi.nlm.nih.gov/pubmed/12369533 (accessed 29 June 2016) [DOI] [PubMed] [Google Scholar]
- 39.Snow J. Snow on cholera. The Commonwealth Fund; New York: 1936. On the mode of transmission of cholera, 1855. Reprinted by UCLA Fielding School of Public Health 2001. Available at: http://www.ph.ucla.edu/epi/snow/snowbook2.html (accessed 4 July 2016) [Google Scholar]
- 40.Tappero J.W., Tauxe R.V. Lessons learned during public health response to cholera epidemic in Haiti and the Dominican Republic. Emerg Infect Dis. 2011;17(11):2087–2093. doi: 10.3201/eid1711.110827. Available at: http://www.medscape.com/viewarticle/754871_7 (accessed 13 November 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tulchinsky T.H., Burla E., Clayman M., Sadik C., Brown A., Goldberger S. Safety of community drinking-water and outbreaks of waterborne enteric disease outbreak: Israel, 1976–97. Bull World Health Organ. 2001;78:1466–1473. Abstract available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2560668/pdf/11196499.pdf (accessed 29 June 2016) [PMC free article] [PubMed] [Google Scholar]
- 42.United Nations, Department of Economic and Social Affairs (UNDESA), International decade for action: water for life, 2005–2015, Available at: http://www.un.org/waterforlifedecade/scarcity.shtml (accessed 16 August 2016).
- 43.United Nations Development Programme . Water governance for poverty reduction, 2004. United Nation; New York: 2004. Available at: http://www.undp.org/content/dam/aplaws/publication/en/publications/environment-energy/www-ee-library/water-governance/water-governance-for-poverty-reduction/UNDP_Water%20Governance%20for%20Poverty%20Reduction.pdf (accessed 14 November 2016) [Google Scholar]
- 44.United Nations. The Millennium Development Goals report 2015. Available at: http://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf (accessed 28 June 2016).
- 45.United Nations. Report of the Special Rapporteur on extreme poverty and human rights. General Assembly, August, 2016. New York: United Nations, 2016. Available at: http://chrgj.org/wp-content/uploads/2016/08/G-A7140823.pdf (accessed 12 November 2016).
- 46.Vachon D. Father of modern epidemiology: John Snow. University of California, Los Angeles (UCLA); Los Angeles, CA: 2005. Available at: http://www.ph.ucla.edu/epi/snow/fatherofepidemiology.html (accessed 25 June 2016) [Google Scholar]
- 47.Vinten-Johansen P., Brody H., Paneth N., Rachman S., Rip M. Cholera, chloroform, and the science of medicine: a life of John Snow. Oxford University Press; New York: 2003. Book review in: NEJM. 2004;350:90–91. Available at: http://www.nejm.org/doi/full/10.1056/NEJM200401013500122 (accessed 26 June 2016) [Google Scholar]
- 48.World Health Organization Cholera 2015. Wkly Epidemiol Rec. 2016;91(40):433–440. Available at: http://apps.who.int/iris/bitstream/10665/250142/1/WER9138.pdf (accessed 15 November 2016) [PubMed] [Google Scholar]
- 49.World Health Organization . Guidelines for drinking-water quality. 4th edition. WHO; Geneva, Switzerland: 2011. Available at: http://apps.who.int/iris/bitstream/10665/44584/1/9789241548151_eng.pdf http://www.who.int/water_sanitation_health/publications/2011/dwq_guidelines/en/ (accessed 29 June 2016) [Google Scholar]
- 50.World Health Organization Epidemic focus cholera: the genie that escaped. Wkly Epidemiol Rec. 2016;91(23):297–304. Available at: http://www.who.int/wer/2016/wer9123.pdf?ua=1 (accessed 4 July 2016) [PubMed] [Google Scholar]
- 51.World Health Organization. Diarrhoeal disease: fact sheet updated May 2017. Available at: http://www.who.int/mediacentre/factsheets/fs330/en/ (accessed 26 June 2016).
- 52.World Health Organization. Cholera: fact sheet, updated October 2016. Available at: http://www.who.int/mediacentre/factsheets/fs107/en/ (accessed 14 November 2016).
- 53.World Health Organization. Rotavirus, June 3, 2016. Available at: http://www.who.int/immunization/diseases/rotavirus/en/ (accessed 26 June 2016).
- 54.World Health Organization. Estimated rotavirus deaths for children under 5 years of age: 2013, 215,000. Available at: http://www.who.int/immunization/monitoring_surveillance/burden/estimates/rotavirus/en/ (accessed 26 June 2016).
- 55.World Health Organization. The Global Task Force on Cholera Control. Available at: http://www.who.int/cholera/task_force/en/ (accessed 21 August 2016).
- 56.World Health Organization. Number of reported cholera cases. Available at: http://www.who.int/gho/epidemic_diseases/cholera/cases_text/en/ (accessed 15 October 2016).
- 57.Yen C., Tate J.E., Patel M.M., Parahar U.D. Rotavirus vaccines: update on global impact and future priorities. Hum Vaccin. 2011;7(12):1282–1290. doi: 10.4161/hv.7.12.18321. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3338930/ (accessed 5 July 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zeng M., Mao X.H., Li J.X., Tong W.D., Wang B., Zhang Y.J. Efficacy, safety, and immunogenicity of an oral recombinant Helicobacter pylori vaccine in children in China: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2015;386(10002):1457–1464. doi: 10.1016/S0140-6736(15)60310-5. [DOI] [PubMed] [Google Scholar]


