Abstract
Human health and animal health are closely intertwined. We share hundreds of diseases with animals, and they are vectors for many diseases that assail humans—but, at the same time, they are essential to many treatments and cures. We discuss in this chapter various aspects of intimate relationship between human and animal health, giving examples of the importance of multidisciplinary studies in understanding these connections and the fundamental aspects of strategies for promoting the health and well-being of both groups.
Keywords: Biotherapy, Folk medicine, Health, Traditional medicine, Wild animals, Zootherapy
Introduction
Humans share the planet with a bewildering variety of other animals and plants, forming an intricate web of interactions. Disturbances that negatively impact the environment or the health of biological organisms will affect the harmonious functioning of their interactions; thus, human health depends on the health of the organisms with which we interact and the environment in which we all live.
The interrelationships between society and nature and the importance of environmental health to human health have become widely acknowledged (Alves and Rosa, 2007, WHO, 2005), drawing attention to the fact that biodiversity losses will have direct or secondary effects on human well-being. Thus, human health must not be considered in isolation, for it depends on the quality of the environment in which we live—for people to be healthy, the environment must be healthy (Alves and Rosa, 2007). The recognition that human, animal, and environmental health are linked generated the “One Health” concept, which is defined by the One Health Commission (2010) as “the collaborative effort of multiple disciplines to obtain optimal health for people, animals, and our environment.” Mi et al. (2016) emphasized that one health seeks to understand the interactions between humans, animals, and environmental factors, and their impacts on health.
Extremely close connections have existed between humans and animals throughout history (Alves, 2012), and we likewise share hundreds of illnesses. Cross-species transmissions and the emergence and eventual evolution of a plethora of infectious pathogens have been observed ever since the establishment of human–animal interfaces (Reperant et al., 2012), with links between human and animal health having profound effects on almost every aspect of our lives.
The links between animals and human health have been substantiated throughout the history of mankind, from causes to cure of human diseases. Seven main aspects should be highlighted when considering this connection: (1) animals as the cause/disseminator of diseases for humans and vice versa; (2) animals as sentinels of human health; (3) the use of animals in traditional medicine systems; (4) animal-assisted therapy; (5) biotherapy; (6) animals as a source of drugs; and (7) use of animals in medical research. These aspects will be briefly discussed in this chapter.
Animals as Cause/Disseminator of Disease in Humans and Vice Versa
Since ancient times, human beings have related the appearance of certain diseases and epidemics to the presence or influence of animals that are considered to presage bad omens, diseases, and death (Ávila-Pires, 1989). This is not surprising, considering that the natural world has a strong influence on the transmission of disease to humans from animals and vice versa, and the perception of more primitive societies therefore certainly reflects daily experiences. As pointed by Wolfe et al. (2007), human hunter/gatherer populations currently suffer, and presumably have suffered for millions of years, from infectious diseases similar or identical to diseases of other wild primate populations.
When an infectious agent responsible for a human disease is also capable of infecting other species, these species may act as reservoirs or vectors for the disease (European Commission, 2011). Arthropods, for example, transmit hundreds of different known infectious and parasitic agents to humans and animals around the world. These vectors include almost all forms of blood-sucking arthropods: mosquitoes, ticks, mites, biting midges, sand flies, kissing bugs, bed bugs, black flies, lice, fleas, and deer and horse flies (Seymour, 1984).
Diseases and infections that are naturally transmitted between animals and humans are known as zoonoses (Bell et al., 1988, Krauss, 2003) and have been known to affect human health throughout history (Kruse et al., 2004). Such diseases have an important impact on public health and economy, and on the conservation of wildlife (Cleaveland et al., 2001). Exposure of humans to zoonoses occurs in different ways, from well-known or well-understood direct transmission routes, such as bites and rabies, to less obvious pathways, the risk factors or potential exposure routes of which are difficult to recognize and are interlinked in a relationship network between human beings, animals, and the environment (Friend, 2006). The most frequent sources of zoonose transmission comprise food and contaminated water, vector insect bites and scratches, or bites from infected animals (Chomel, 2002).
Zoonotic diseases account for approximately 75% of emerging infectious diseases (Chomel et al., 2007, Taylor et al., 2001). A literature search showed that more than 800 human pathogens are zoonotic (Taylor et al., 2001, Woolhouse and Gowtage-Sequeria, 2005). According to Weiss (2001), some of these pathogens may cause serious diseases in wild animals but, in some cases, the animals act as reservoirs, without showing any clinical symptoms (Williams et al., 2002). As mentioned above, zoonoses can be transmitted by direct contact with infected animals, dead or alive, which are used by humans in several ways, including consumption as food or as pets. The consumption of animal products as food or in traditional medicine, for example, facilitates the transmission of serious and widespread zoonoses, such as tuberculosis or rabies (De Smet, 1991, Schnurrenberger and Hubbert, 1981, Still, 2003). Another example deserving mention is avian influenza (Influenza A) viruses; these are responsible for highly contagious acute illness in humans, pigs, horses, marine mammals, and birds, occasionally resulting in devastating epidemics and pandemics (Bengis et al., 2004).
Wild animals constitute an important but poorly known reservoir of emerging infectious diseases, most of which are of zoonotic concern (Pérez, 2009). The trade in wildlife for food consumption, medicines, and as pets, among other uses, involves the capture and sale of billions of animals of incredibly wide varieties of species (Alves et al., 2010a, Alves et al., 2013a, Pérez, 2009, Roldán-Clarà et al., 2014). Wildlife commercialization, both legal and illegal, is considered a significant driver of zoonotic diseases—leading to the introduction of zoonoses and/or foreign diseases that may impact domestic animals and/or native wildlife species (Karesh et al., 2005, Rostal et al., 2012). Hunting and the consumption of bushmeat are important routes for the introduction and transmission of zoonotic diseases (Van Vliet et al., 2017). Any wildlife species harvested for bushmeat could be a potential source of zoonotic diseases that could be transferred during hunting, butchering, or preparation (Karesh and Noble, 2009, Wolfe et al., 2000). Armadillos, for example, are widely hunted as food resources and for medicinal uses, but are natural reservoirs of etiological agents of several zoonotic diseases that affect humans—such as leprosy, trichinosis, coccidioidomycosis (valley fever), Chagas disease, and typhus (Silva et al., 2005). More than 100 occurrences of pulmonary mycosis, for example, were recorded in 40 municipalities in Piauí state in northeastern Brazil (Alves et al., 2016). The exotic pet trade deals with an increasing range of wild animal species, from invertebrates to mammals (Pérez, 2009), and it is believed that epidemics such as SARS (severe acute respiratory syndrome), monkey pox, and avian influenza H5N1 emerged from wildlife markets (Brown, 2004, Burgos and Burgos, 2007, Check, 2004, Karesh et al., 2007, Sleeman, 2006, Warwick et al., 2011).
There is a rising threat from emerging infectious diseases spreading to people and other animals, fueled by human activities ranging from the handling of bushmeat and the trade in exotic animals to the destruction of wild habitat (Lilley et al., 1997, Patz et al., 2000, Walsh et al., 1993). Despite warnings of the potential significance for human disease of changing patterns in their relationship with animals and the natural world, scientists have continued to treat human and animal health as largely independent disciplines, while historians have also neglected this important aspect of human disease (Hardy, 2003). In this sense, it is crucial that the interdependence between animal and humans be considered in the development of new public health practices.
Animal as Sentinels of Human Health
As discussed previously, animals suffer a similar spectrum of disease as humans (Bell et al., 1988, Krauss, 2003) and, therefore, may be sensitive indicators of environmental hazards and provide an early warning system for public health intervention (Reif, 2011). The concept that disease occurrence in nonhuman animal populations (wild and domestic) can serve as a sentinel warning of an environmental threat to human health has a long history (Rabinowitz et al., 2005).
Animals have served in numerous cases as “sentinels” of environmental threats near the living or working environments (Van der Schalie et al., 1999), and humans can, in return, sometimes serve as sentinels for animal health. The potential for animals to serve as sentinels for humans (or vice versa) depends on the type of linkages and contacts between specific animal populations and neighboring humans (Rabinowitz and Conti, 2013). Terrestrial wildlife, companion animals, food production animals, and aquatic animal populations can be monitored as sentinels for environmental impacts caused by pathogens, contaminants, and/or land-use changes (Rabinowitz and Conti, 2013).
Several historical examples illustrate animals’ usefulness as predictors of human illness (Rabinowitz and Conti, 2013, Reif, 2011). In the 1870s, fattened cattle experienced high mortality at a stock show in London’s Smithfield Market associated with a dense industrial fog—a precursor to the air pollution episodes typified by the infamous London Fog of 1952, during which thousands of residents died (Glickman et al., 1991). In the 1950s, recognition of neurobehavioral disturbances in the cat population of Minamata, Japan, preceded a severe episode of neurological disease among local residents caused by consumption of seafood contaminated with methylmercury (Tsuchiya, 1992). Sediments, shellfish, and fish in Minamata Bay became contaminated with mercuric chloride as the result of effluent discharges from a chemical plant. The ataxic “dancing cats of Minamata” were a warning sign. Unfortunately, it was not recognized in time to prevent the human epidemic (Reif, 2011). In 1962, it was cases of lead poisoning in cattle and horses living in the vicinity of a smelter that alerted the Minnesota State Health Department to conduct surveillance for lead exposure in local human populations (Hammond and Aronson, 1964). Another classic example of this is the historic use of canaries by miners to detect the presence of toxic gases in coal mines (Burrell and Seibert, 1916). Dying crows and other birds signaled the appearance and spread of the West Nile virus infection in the Western hemisphere. As the disease spread, monitoring of dead crows was used as a sentinel system for early warning of human disease risk (Julian et al., 2002).
Animal sentinels may potentially be used to address a range of surveillance questions including: (1) detection of a known pathogen in a new area; (2) detection of changes in the prevalence or incidence of a pathogen or disease over time; (3) determining the rates and direction of pathogen spread; (4) testing specific hypotheses about the ecology of a pathogen; and (5) evaluating the efficacy of potential disease control interventions (McCluskey, 2003). Appropriate use of animal sentinels can facilitate the early detection and identification of outbreaks, which is of critical importance both for the success of control and prevention efforts (Chomel, 2003, Kahn, 2006) and for reducing the magnitude of subsequent outbreaks (Ferguson et al., 2005). However, the potential of animal sentinel surveillance can only be fully realized if information sourced from animal populations is acted upon. For example, an Ebola outbreak in central Africa was the result after insufficient preventive health measures were taken despite warnings of an imminent human outbreak being provided from monitoring of Ebola deaths in primate sentinels (Rouquet et al., 2005).
Studies of the effects of environmental exposure on domestic and wild animals can corroborate or inform epidemiologic studies in humans (Reif, 2011). Currently, however, physicians assessing environmental health risks to patients do not routinely include animal sentinel data in their clinical assessments. Public health practitioners are unlikely to respond to mortality events in animals that are not clearly due to West Nile virus or other known zoonoses, such as rabies (Rabinowitz et al., 2005). Reasons for the underuse of animal sentinel data by human health professionals may include limited understanding of the relationships existing between animal, human, and ecosystem health; insufficient knowledge of veterinary medicine; and few institutional protocols to incorporate animal data into public health surveillance (Stephen and Ribble, 2001). Both human and animal health professionals have gained an increasing awareness that disease events in animal populations may have direct relevance to human health (Scotch et al., 2009).
Traditional Medicine
It is known that at the dawn of recorded history humans often ate, or wore on their person, some portion of an animal that was thought to have a healing or protective influence (MacKinney, 1946); this highlights the intertwining of the origin of the medicinal use of faunal elements with their use as food. In the same context, Chemas (2010) remarked that the treatment of illnesses using animal-based remedies is an extremely old practice, the most remote antecedent of which is a carnivore diet, closely followed by the ritual ingestion of deceased persons (e.g., close relatives, warriors) as a means of absorbing their virtues (e.g., courage, virility), and subsequently by a true medicinal use inseparable from magical-religious elements. These observations are in line with the view of nature as providing many things for humankind, including tools for the first attempts at therapeutic intervention (Nakanishi, 1999).
Although plants and plant-derived materials make up the majority of the ingredients used in most traditional medical systems worldwide, whole animals, animal parts, and animal-derived products also constitute important elements of the materia medica (Alakbarli, 2006, Alves et al., 2013b, Alves and Rosa, 2005, Moquin-Tandon, 1861, Scarpa, 1981, Stephenson, 1832, Unnikrishnan, 2004). Products derived from medicinal animals are directly used in the confection of popular remedies and magical items such as charms, amulets, and talismans that are widely sought after in traditional medicinal practices (Alves and Rosa, 2013a, Anyinam, 1995).
The antiquity in the use of medicinal animals and its persistency through times are a testimony to the importance of those therapeutic resources to mankind (Alves et al., 2013b). In modern societies, zootherapy constitutes an important alternative to the many other known therapies practiced worldwide (Alves and Rosa, 2013a). Wild and domestic animals and their by-products (e.g., hooves, skins, bones, feathers, tusks) form important ingredients in the preparation of curative, protective, and preventive medicine (Adeola, 1992, Alves and Alves, 2011, Alves et al., 2012, Ashwell and Walston, 2008, Martinez, 2013, Whiting et al., 2011, Williams et al., 2013).
Many cultures still employ traditional medicine incorporating animal-derived remedies. Probably the most famous of these are the Chinese, who use animals to treat a variety of ailments. Although less known and less frequently studied, Latin America and Africa both have a long tradition of using their equally varied and rich fauna, including many endangered species, to treat all kinds of ailments (Alves and Rosa, 2013b). Zootherapeutic practices are also found in Europe (Ceríaco, 2013, Quave et al., 2010, Voultsiadou, 2010).
Mammals, fish, reptiles, birds, mollusks, and insects, including many threatened species, are prominently used in traditional medicine (Figure 13.1, Figure 13.2 ) (Alves et al., 2010b, Alves et al., 2008, Alves et al., 2013g, Ferreira et al., 2012, Ferreira et al., 2013, Williams et al., 2013), substantiating the importance of taking into account their harvesting in the context of animal conservation. Many marine (Alves and Dias, 2010, Alves et al., 2013c) and terrestrial invertebrates (Costa-Neto, 2005, Figueirêdo et al., 2015, Kritsky, 1987, Pemberton, 1999) make up part of the therapeutic arsenal of popular medicine (Figure 13.3, Figure 13.4, Figure 13.5 ).
Figure 13.1.

Medicinal animal-derived products (crocodile skulls, antelope horns, and a diversity of carnivore and nonhuman primate skulls) for sale in Benin, West Africa.
Photo credits: Anthony B. Cunningham.
Figure 13.2.

The tegu lizard (Salvator merianae) and boa snake (Boa constrictor), reptiles species often used in Brazilian traditional medicine.
Photo credits: John Philip Medcraft.
Figure 13.3.

Dried starfish for sale in the traditional Chinese medicine market in Chengdu, Sichuan.
Photo credits: Anthony B. Cunningham.
Figure 13.4.

The centipedes (Scolopendra subspinipes), known as wugong in Chinese, widely sold in traditional Chinese medicine markets.
Photo credits: Anthony B. Cunningham.
Figure 13.5.

Examples of raw materials derived from medicinal animals sold in Brazilian cities.
Photo credits: Rômulo R.N. Alves.
Articles and review texts have revealed the high numbers of animal species used in traditional medicinal practices throughout the world (Table 13.1 ). Researchers have reported more than 1500 animal species that have some medicinal use in traditional Chinese medicine (Yinfeng et al., 1997). In Latin America, at least 584 animal species have been reported as being used in traditional medicinal practices (Alves and Alves, 2011). Worldwide, at least 284 reptiles and 47 amphibians (Alves et al., 2013g), 110 primates (Alves et al., 2013e), 108 mammalian carnivores (Alves et al., 2013d), and 266 marine invertebrates (Alves et al., 2013c) are used in popular medicines. Research in 25 African countries has shown that at least 354 bird species are used there in traditional curing practices (Williams et al., 2013) (Table 13.1). Some groups, such as seahorses (Hippocampus spp.) are widely employed for medicinal purposes (Fig. 13.6 ). Rosa et al. (2013) reported that of 48 species recognized as valid by Project Seahorse (2016), 20 species were cited in the literature as having medicinal uses. It is important to point out that the number of animal species used in popular medicinal practices must certainly be larger than what has so far been recorded, as in spite of studies focusing on this theme, many regions have not been closely examined—indicating that further studies will be indispensable to increasing our understanding of the links between the traditional uses of animals and conservation biology, the sustainable management of natural resources, public health policies, and biological prospection (Alves and Rosa, 2006).
Table 13.1.
Richness of Animal Species Used in Traditional Folk Medicine According to Literature
| Animal Group | Number of Medicinal Species | Geographic Coverage | References |
|---|---|---|---|
| Herpetofauna | 331 | Worldwide | Alves et al. (2013g) |
| Primates | 110 | Worldwide | Alves et al. (2013e) |
| Carnivorous mammals | 108 | Worldwide | Alves et al. (2013d) |
| Aquatic mammals | 24 | Worldwide | Alves et al. (2013f) |
| Seahorses | 20 | Worldwide | Rosa et al. (2013) |
| Marine invertebrates | 266 | Worldwide | Alves et al. (2013c) |
| Birds | 354 | Africa (25 countries) | Williams et al. (2013) |
| All taxons combined | 584 | Latin America | Alves and Alves (2011) |
| All taxons combined | 54 | Portugal | Ceríaco (2013) |
| All taxons combined | 109 | India | Mahawar and Jaroli (2008) |
| All taxons combined | 137 | Nigeria | Soewu (2013) |
| All vertebrate groups | 147 | South Africa | Whiting et al. (2013) |
| Mammals | 87 | Benin (West Africa) | Djagoun et al. (2013) |
Figure 13.6.

The longsnout seahorse, Hippocampus reidi (A), species commonly used for medicinal purposes in Brazil, traded in the dried form. Dried seahorse specimens for sale (B–D) in Brazilian cities.
Photo credits: (A) Thelma L.P. Dias, (B and D) Rômulo R.N. Alves, (C) Ierecê L. Rosa.
The world’s animals and plants—including a number of species used in traditional medicine—face threats ranging from habitat loss to the global wildlife trade (Alves and Rosa, 2013a ). There has been an increasing demand for traditional medicines (Alves and Rosa, 2007, Robinson and Zhang, 2011), and the link between traditional medicine and the loss of certain species has become apparent (Alves et al., 2007, Call, 2006). This trend bears important implications for the conservation of the many species of flora and fauna, on which traditional remedies are based (Alves and Rosa, 2013a, Lee, 1999). Unfortunately, whereas the use of traditional remedies used to be a localized practice, the globalization of commerce in combination with the increased popularity of natural approaches to health worldwide has created a level of demand that threatens the survival of many vulnerable species of wildlife (IFAW, 2011). The case of vertebrates threatened by trade for traditional medicine, including rhinos, tigers, bears, pangolins, turtles, seahorses, monkeys, tigers, rhinoceros, and bears is well-known (Fig. 13.7 ).
Figure 13.7.
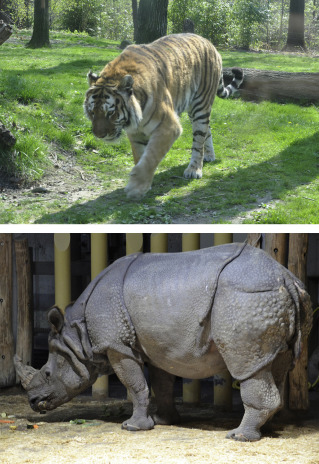
Tigers and rhinos, examples of endangered animals impacted due to use and traffic of their parts for traditional medicines.
Photo credits: Rômulo R.N. Alves.
Medicinal use of fauna represents an additional pressure for many species, and has been indicated as an important cause of population decline. Thus, not only should the use of these animals in popular medicine be considered, but also their exploitation by the pharmaceutical industry (Marques, 1997). As Shaw (2009) points out, any pharmaceutical scientist who is involved in contemporary natural product research has to get involved in, or at the very least become familiar with, global issues of species conservation and/or biodiversity.
Biotherapy
The use of live organisms for treating human and animal illnesses is known as biotherapy (Grassberger et al., 2013). As pointed out by those authors, this is an ancient practice, although it has now attracted the interest of many clinicians, biologists, biochemists, and patient advocates and has emerged as a rapidly advancing multidisciplinary field of medicine. Some of the principal animals used in biotherapy are maggots, leeches, bees, parasitic worms, and fish (Table 13.2 ), giving rise to the fields of maggot therapy, hirudotherapy, apitherapy, helminth therapy, and ichthyotherapy, which will all be briefly discussed below.
Table 13.2.
Animals Species Used in Biotherapy
| Species | References |
|---|---|
| Hirudotherapy | |
| Hirudo medicinalis (Linnaeus, 1758) | Gileva and Mumcuoglu (2013) |
| Hirudo verbana (Carena, 1820) | Van Wingerden and Oosthuizen (1997) and Whitaker et al. (2012) |
| Hirudo michaelseni (Augener, 1936) | Van Wingerden and Oosthuizen (1997) and Whitaker et al. (2012) |
| Poecilobdella granulosa (Savigny, 1822) | Lone et al. (2011) |
| Maggot Therapy | |
| Calliphora vicina (Robineau-Desvoidy, 1830) | Teich and Myers (1986) |
| Chrysomya rufifacies (Macquart, 1842) | Teich and Myers (1986) |
| Lucilia caesar (Linnaeus, 1758) | Baer (1931) and McLellan (1932) |
| Lucilia cuprina (Wiedemann, 1830) | Fine and Alexander (1934) |
| Lucilia illustris (Meigen, 1826) | Lerclercq (1990) |
| Lucilia sericata (Meigen, 1826) | Baer (1931) |
| Phormia regina (Meigen, 1826) | Baer, 1931, Horn et al., 1976, Reames et al., 1988, and Robinson (1933) |
| Protophormia terraenovae (Robineau-Desvoidy, 1830) | Lerclercq (1990) |
| Wohlfahrtia nuba (Wiedemann, 1830) | Grantham-Hill (1933) |
| Musca domestica (Linnaeus, 1758) | Grantham-Hill (1933) |
| Apitherapy | |
| Apis melifera (Linnaeus, 1758) | Kim (2013) |
| Ichthyotherapy | |
| Garra rufa (Heckel, 1843) | Grassberguer and Sherman (2013) |
| Helminth Therapy | |
| Ascaris lumbricoides (Linnaeus, 1758) | Correale and Farez, 2007, Correale and Farez, 2011 |
| Enterobius vermicularis (Linnaeus, 1758) | Correale and Farez, 2007, Correale and Farez, 2011 |
| Hymenolepis diminuta (Rudolphi, 1819) | Correale and Farez, 2007, Correale and Farez, 2011 |
| Hymenolepis nana (Siebold, 1852) | Correale and Farez, 2007, Correale and Farez, 2011 |
| Strongyloides stercoralis (Bavay, 1876) | Correale and Farez, 2007, Correale and Farez, 2011 |
| Trichuris suis (Schrank, 1788) | Fleming et al. (2011) |
| Necator americanus (Stiles, 1902) | Wolff and Broadhurst (2012) |
| Trichuris trichiura (Linnaeus, 1771) | Wolff and Broadhurst (2012) |
Hirudotherapy
The use of medicinal leeches for curative purposes is one of the oldest known practices in medicine (Gileva and Mumcuoglu, 2013) and is called hirudotherapy or leech therapy. Although more than 650 species of leeches have been described, only a few are used for medicinal (therapeutic) purposes. The European medicinal leech, Hirudo medicinalis, is one of the most extensively studied annelids and the most frequently used in modern medical practices (Gileva and Mumcuoglu, 2013). Similar results have also been obtained in some cases with Hirudo verbana and Hirudo michaelseni (Van Wingerden and Oosthuizen, 1997, Whitaker et al., 2012). Medicinal leeches apparently reduce blood coagulation and relieve venous pressure resulting from blood pooling (especially after plastic surgery) and stimulate blood circulation (Godfrey, 1997). Leeches are now applied to treat a wide array of diseases or conditions, including reconstructive plastic surgery; venous, cardiovascular, neurological, gynecological, osteomuscular, and ophthalmologic disorders; periodontal and oral mucosal diseases; and cancer (Gileva and Mumcuoglu, 2013, Gilyova, 2005, Scott, 2002). Specific applications of hirudotherapy can vary in different countries or regions. Hirudotherapy is officially recognized as an alternative therapy for numerous internal diseases including osteoarthritis, phlebitis, hypertension, and glaucoma in some Eastern Europe, Russian, and Asian countries, while American and European practitioners emphasize the value of leeches in microvascular and reconstructive surgery for both pediatric and adult populations (Gilyova, 2005).
Maggot Therapy
One of the most interesting applications of insects as therapeutic agents is maggot therapy, which involves the treatment of superficial or deep wounds with the help of blowfly larvae (Costa-Neto, 2005). This method was accidentally discovered during the World War I and was widely used during the 1930s and 1940s, being indicated for infected wounds that are difficult to heal, such as osteomyelitis, abscesses, burns, wounds on diabetic patients, pressure ulcers, traumatic lesions, tumors, and untreatable gangrene (Martini and Sherman, 2003). The advantages of maggot therapy, also called larval therapy, maggot debridement therapy, and biosurgery, include its profound efficacy in debriding necrotic tissue and its relative safety and simplicity; it is frequently utilized when conventional medical treatments and surgeries are not capable of deterring progressive tissue destruction (Sherman et al., 2013). The therapy treatment consists of applying live, sterile, laboratory raised, blowfly larvae (Diptera: Calliphoridae) to lesions or chronic and/or infected wounds to remove necrotic/infected tissues and promote healing (Martini and Sherman, 2003). The larvae can be applied to a wound in a direct (free-range) or indirect (contained) manner (Gunjegaonkar et al., 2016). Blowfly larvae, Lucilia sericata, are frequently used, although other species have also been employed, such as Lucilia cuprina, Phormia regina, and Calliphora vicina (Sherman et al., 2000). Maggots like those of L. sericata feed on dead tissue where gangrene-causing bacteria thrive. As they eat, they also secrete allantoin, a chemical that inhibits bacterial growth (Costa-Neto, 2005). Medicinal maggots have three actions: they clean wounds by dissolving the dead (necrotic) infected tissue, disinfect the wound by killing bacteria, and stimulate wound healing (Sherman et al., 2000). The larva debride the necrotic tissue using their oral suction apparatus, which liberates digestive enzymes and dissolves the infected tissue; the wound is disinfected through the secretion of antibacterial substances liberated by the larva that activate macrophages, induce wound healing, and stimulate healthy tissue growth (Dallavecchia et al., 2011).
Use of maggot therapy declined with the introduction of modern antibiotics and improvements in surgical debridement, although the use of maggot therapy has been returning due to growing antibiotic resistance and potential adverse effects associated with antibiotic use (Gunjegaonkar et al., 2016). Initially, maggot therapy was used for treating chronic wounds in humans, but was later used with animals as a likewise safe and effective method of curing serious wounds (Munir et al., 2016). Numerous researchers have shown that larval therapy is much more effective at debriding wounds than conventional treatments (Dallavecchia et al., 2011, Sherman et al., 1986). Maggot therapy is commonly used in the United States, Israel, and Europe to treat various types of infected wounds, such as those on the feet of diabetics, postoperative infections, ulcer scabs, and leg ulcers (Ratcliffe et al., 2011, Sherman et al., 2000).
Apitherapy—Bee Venom Therapy
Bee venom therapy is a biotherapeutic medical treatment that uses bee venom to treat numerous illnesses (Kim, 2013). Bee venom has a long history of use as a folk remedy for treating diseases such as arthritis, angiocardiopathy, back pain, musculoskeletal pain, cancerous tumors, multiple sclerosis, and skin diseases, and it is known to promote wound healing (Alqutub et al., 2011, Beck, 1935, Cherniack, 2010, Roy et al., 2015). The use of bee venom is quite ancient, but has attracted growing interest now due to its positive therapeutic results (Moreira, 2012). Bee venom is a colloidal substance that can be dialyzed through membranes and absorbed through the skin (Shimpi et al., 2016); it is composed of approximately 18 active compounds including enzymes, bioamines, and peptides with important biological effects (Yasui, 2012). Bee venom has been reported to have both a central analgesic mechanism and peripheral analgesic action due to its anti-inflammatory action (Shin et al., 2012).
Bee venom can be applied by direct stings from bees (apipuncture or bee sting therapy) or through injections of a venom extract (bee venom therapy)—both requiring the experience of a qualified health professional (Lucache et al., 2015). Bee venom therapy involves the use of the venom produced by Apis melifera, marketed under the names of Apitoxina and Apitox. The venom is applied intradermally, never intravenously, and used for treating various autoimmune diseases, neurological disturbances, and chronic and inflammatory illnesses (Kim, 2013). Apipuncture is a method used by health professionals or licensed practitioners of acupuncture, with the venom being injected by holding a live bee (with forceps) on the affected area of the patient and allowing it to sting that person. Before initiating this type of treatment, however, the patient must be examined for allergic reactions to the venom (Kim, 2013, Yasui, 2012). Bee venom therapy stimulates the immunological system through the hypothalamus, pituitary gland, and suprarenal glands, inducing the body to produce its own curative substances. The efficiency of bee venom therapy has been evaluated in both laboratory and clinical experiments with humans (Yasui, 2012); however, this curative mechanism is not yet well understood, but a series of chemical compounds acting together in the body have been identified (Lucache et al., 2015).
Ichthyotherapy
The term “ichthyotherapy” was proposed in 2006 (Grassberguer and Sherman, 2013) and readily adopted, being defined as an alternative therapy for treating skin diseases with the so-called “doctor fish of Kangal,” Garra rufa (Fig. 13.8 ) (Heckel, 1843) (Grassberguer and Sherman, 2013), a small, freshwater cyprinid fish native to the Middle East (Froese and Pauly, 2016). The use of this species is directed toward treating skin problems such as psoriasis, eczema, dermatitis, acne, calluses, and hardness (Ozcelik and Akyol, 2011). Several underlying mechanisms have been suggested for the observed efficacy of ichthyotherapy. One obvious mechanism is physical contact with the fish, which feeds on desquamating skin, leading to a rapid reduction of superficial skin scales (Grassberguer and Sherman, 2013). G. rufa are toothless fish that consume the dead skin cells of people that they come into direct contact with in the water, without affecting healthy skin (Cabral and Carneiro, 2014). The underlying mechanisms of ichthyotherapy are not yet totally understood, but the most visible effect of exposure to this fish is the removal of excess skin layers, although the dramatic observed reductions in the inflammatory component, especially among patients with psoriasis, suggest additional mechanisms (possibly molecular). More complete biochemical studies will need to be undertaken to identify and characterize the properties of G. rufa in that context (Grassberguer and Sherman, 2013).
Figure 13.8.

“Doctor fish of Kangal,” Garra rufa, fish species used in ichthyotherapy.
Photo credits: Tacyana P.R. Oliveira.
Helminth Therapy
The therapeutic uses of helminths (parasitic worms) have been tested in laboratory trials as new approaches to treating a variety of allergic and autoimmune illnesses (Khan and Fallon, 2013). This type of therapy is called helminth therapy and consists of the inoculation of the patient with specific parasitic intestinal nematodes (helminths). Diseases such as ulcerative colitis, multiple sclerosis, rheumatoid arthritis, Crohn disease, celiac disease, and autism are among the health problems potentially treatable with helminths. A number of such organisms are currently being investigated for their use in therapeutic treatments (see Table 13.2), including Trichuris suis (Fleming et al., 2011), Necator americanus (Elliot et al., 2013), Trichuris trichiura (Correale and Farez, 2011); Hymenolepis diminuta, Ascaris lumbricoides, Strongyloides stercoralis, Enterobius vermicularis, and Hymenolepis nana (Correale and Farez, 2011, Leonardi-Bee et al., 2006).
It is appropriate to note that helminth therapies will probably be increasingly used in developed societies where epidemics of inflammatory disorders are most prevalent, and thus in people never previously exposed to helminths, while the desirable protective effects of helminth infections of humans in field studies have been reported for people in endemic areas (Scrivener et al., 2001). The theory that helminth infection protects against autoimmune diseases can be tested by comparing the prevalence of those diseases in highly helminth-exposed and less- or nonexposed human populations. There is strong evidence that helminth exposure results in changes to the immune system that decrease the risk of developing immune disorders, thereby preventing the onset of immune-mediated diseases that have become common in developed countries (Elliot et al., 2013).
Animal-Assisted Therapy
Another way in which animals can be used to ameliorate human health conditions is through human involvement with living creatures as a form of therapy (Alves et al., 2009). For centuries people have noted that animals can have positive influences on human health and functioning (Nimer and Lundahl, 2007). Florence Nightingale suggested in the 19th century that a bird might be a primary source of pleasure for people confined to their rooms due to medical problems (McConnell, 2002). The use of animals as therapy has intensified now and has received many names, such as animal-assisted therapy, pet therapy, animal-assisted activities, pet-facilitated therapy, pet-assisted therapy, animal-facilitated therapy, animal-assisted interventions, and animal visitation (Connor and Miller, 2000, Fine, 2010, Hooker et al., 2002, Kruger et al., 2006). All of these practices have the common focus of utilizing animals as facilitators for patient recovery and for establishing positive therapies, especially for patients with special needs, children with cognitive or emotional disturbances, and older people (Oliva, 2010).
Both domestic and domesticated animals have found medicinal uses as co-therapists (Silveira, 1998). Among the animals most commonly used for therapeutic purposes are dogs, cats, horses, dolphins, small tame animals such as rabbits and gerbils, and aquarium fish. Typically, reptiles are frowned upon in therapeutic settings because of their high risk of carrying disease or causing injuries to clients, and because of the difficulty of providing those animals with proper care and safe environments. Farm animals are often useful therapy animals, with the most common being llamas and pot-bellied pigs (Chandler, 2012).
Animal-assisted activities can occur in a variety of settings in which people interact with (talk to, pet, groom) companion animals while the animal’s handler is present. Intense attachments can rapidly develop between people and pets during these encounters (Reperant et al., 2012), and researchers have shown that animal-assisted therapies provide numerous positive effects to patient health and can stimulate the development of diverse abilities such as learning, language acquisition, motricity, among others (Oliva, 2010). Contact with animals has proven to be an efficient method for stimulating and helping individuals with mobility problems, mental disabilities, or behavioral problems (Alves and Rosa, 2013b). Animal-assisted therapy can be used, for example, as part of a patient’s physical therapy treatment plan, to decrease anxiety in psychiatric patients and agitation in older adults with dementia (Barker and Dawson, 1998, Batson, 1998). Examples include gradually increasing the number of brush strokes on a dog in order to exercise an impaired hand, and eliciting a relaxation response through horseback riding activities with children with spastic cerebral palsy (McGibbon et al., 1998). Children with autism spectrum disorders were more likely to respond appropriately in therapy sessions involving live dogs than with a stuffed toy dog or a ball (Martin and Farnum, 2002). Some nursing home residents were found to show lower cortisol levels during dog visits than human visits. During and after animal visits, hospitalized patients used fewer analgesics, reporting less pain and less depression, and heart failure patients showed decreased anxiety and epinephrine levels (Beck, 2000, Cole et al., 2007).
Fauna as Source of Drugs
Throughout human history, people have used various natural materials to cure their illnesses and improve their health (Alves and Rosa, 2007). Wildlife not only contributes to traditional medicine but also modern medicine, with natural extracts being used by pharmaceutical companies as raw material for the manufacture of drugs (Rose et al., 2012, Sifuna, 2012). The drugs we use to maintain human health are still predominantly derived from plant and animal species (Fitter, 1986). Historically, while the use of plants as medicines has been extensively recognized, studied, and reviewed, studies on the use of fauna as a source of drugs have only been produced now, and have demonstrated the enormous potential of fauna as a source of natural products and drugs (Alves and Albuquerque, 2013).
Several studies have shown that natural animal resources are highly promising in the search for new products of medicinal or pharmaceutical interest (Alves and Albuquerque, 2013, Chivian, 2002, Dossey, 2010, Fusetani, 2000). This potential is perhaps even greater for animals than for plants, considering that the number of animal species is several times greater (Alves and Albuquerque, 2012). For example, Trowell (2003) points out that there are at least 16 times as many insect species as there are plant species, yet plant chemistry has been studied 7000 times more than insect chemistry, based on a comparison of the amount of research undertaken per species.
Marine animals also represent an exceptional source of bioactive natural products, many of which exhibit structural features not found in terrestrial natural products (Faulkner, 1998, Ireland et al., 1993, Seedhouse, 2010). Drugs have been derived from sharks, sting rays, corals, sea anemones, mollusks, annelids, sponges, sea squirts, sea cucumbers, and horseshoe crabs (Alves and Albuquerque, 2013, Fitter, 1986). Shark liver contains lipids that enhance human resistance to cancer, and the horseshoe crab Limulus not only has a serum that isolates tumor cells and white blood cells from the whole blood of cancer patients, but is also the source of substances used to detect bacterial toxins in human body fluids (Fitter, 1986). Invertebrates are proving to yield increasing numbers of antibiotic agents, blood coagulants and anticoagulants, and neuromuscular, as well as anticancer compounds (Alves and Albuquerque, 2013, Fitter, 1986, Myers, 1979, Seedhouse, 2010). Approximately 2500 new metabolites were reported from a variety of marine organisms during the decade of 1977–87 (Ireland et al., 1993). Already, more than 15,000 natural products have been discovered, and this number continues to grow. While bioprospecting and deep-ocean exploration are in their infancy, the novel biology of the organisms discovered to date and their potential for revolutionizing the medical realm means that scientific interest will be increasingly focused on realizing the potential that exists in the deep ocean. And, inevitably, as a growing body of science reaffirms that deep-sea biodiversity holds major promise for the treatment of human diseases, exploration will surely venture ever deeper in search of untapped resources (Fusetani, 2000, Seedhouse, 2010).
Various terrestrial vertebrates, particularly amphibians and reptiles, have been of great interest in pharmacological studies (Alves and Albuquerque, 2013). One excellent example of successful drug development from a component of snake venom (Bothrops jararaca, Wied, 1824) is that of the inhibitors of angiotensin-converting enzyme. This enzyme is responsible for converting an inactive precursor into the locally active hormone angiotensin, which causes blood vessels to constrict and hence raises blood pressure (Bisset, 1991). Another good example is the work initially conducted by Daly during the 1960s on the skin secretions of dendrobatid frogs from Ecuador, and of other “poison dart” frog species in Central and South America. This work has led to the identification of a number of alkaloid toxins that bind to multiple receptors in the membranes of nerve and muscle cells (Chivian, 2002). The anticarcinogenic activities of Indian monocellate cobra and Russell’s viper venom were studied in carcinoma, sarcoma, and leukemia models. Under in vivo experiments, it was found that the sublethal doses of the Indian Elapidae (monocellate cobra) and Viperidae (Russell’s viper) venom caused cytotoxicity in Ehrlich ascites carcinoma (EAC) cells; it increased the life span of EAC-bearing mice and reinforced its antioxidant system (Debnath et al., 2007). Similarly, antitumor activity of Hydrophidae (Lapemis curtus) venom was also established against EAC in Swiss albino mice in vivo and HeLa and Hep2 tumor cell cultures in vitro (Karthikeyan et al., 2008). Ferreira et al. (2010) evaluated the anti-inflammatory activity of topically administered Tupinambis merianae fat in animal models (male and female Swiss mice––Mus musculus). In this first experimental test of the antiinflammatory activity of T. merianae fat in in vivo models, the authors found that it had significant topical anti-inflammatory activity and reduced inflammation edema in mouse ears caused by croton oil (single and multiple applications), phenol, and arachidonic acid. Similarly, numerous animals produce substances with antimicrobial activities that are effective as defense mechanisms against infections by microorganisms and have synergetic effects when associated with antibiotics (Coutinho et al., 2004)—and researchers have demonstrated positive results in relation to these activities in diverse species (Table 13.3 ).
Table 13.3.
Examples of Animal Species With Pharmacological Activities
| Species | Activity | References |
|---|---|---|
| Macoma birmanica (Philipi, 1949) | Antibacterial | Adhya et al. (2009) |
| Trionyx sinensis (Wiegmann, 1935) | Antibacterial | Thammasirirak et al. (2006) |
| Amyda cartilaginea (Boddaert, 1770) | Antibacterial | Thammasirirak et al. (2006) |
| Chelonia mydas (Linnaeus, 1758) | Antibacterial | Thammasirirak et al. (2006) |
| Nasutitermes corniger (Motschulsky, 1855) | Modulation of the antibiotic activity | Coutinho et al., 2009, Coutinho et al., 2010 and Chaves et al. (2014) |
| Atta sexdens rubropilosa (Forel, 1908) | Antifungal | Masaro et al. (2001) |
| Squalus acanthias (Linnaeus, 1758) | Antibacterial | Donia and Hamann (2003) |
| Leptodactylus macrosternum (Miranda-Ribeiro, 1926) | Antibacterial | Cabral et al. (2013) |
| Leptodactylus vastus (Adolf Lutz, 1930) | Antibacterial | Cabral et al. (2013) |
| Pseudocanthotermes spiniger | Antibacterial and antifungal | Lamberty et al. (2001) |
| Gallus gallus domesticus (Linnaeus, 1758) | Modulation of the antibiotic activity | Coutinho et al. (2014) |
| Rhinella jimi (Stevaux, 2002) | Modulation of the antibiotic activity | Sales et al. (2015) |
| Rhynocoris marginatus (Fabricius, 1794) | Antibacterial | Sahayaraj et al. (2006) |
| Catamirus brevipennis (Servile) | Antibacterial | Sahayaraj et al. (2006) |
| Tropidurus hispidus (Spix, 1825) | Modulation of the antibiotic activity; antiinflammatory | Santos et al., 2012, Santos et al., 2015 |
| Tropidurus semitaeniatus (Spix, 1825) | Modulation of the antibiotic activity | Santos et al. (2012) |
| Spilotes pullatus (Linnaeus, 1758) | Modulation of the antibiotic activity | Oliveira et al. (2014) |
| Dinoponera australis (Roger, 1861) | Antibacterial | Cologna et al. (2005) |
| Dinoponera quadriceps (Santschi, 1921) | Antibacterial | Cardoso et al. (2010) |
| Boa constrictor (Linnaeus, 1758) | Modulatory of the antibiotic activity; antiinflammatory | Ferreira et al., 2011, Ferreira et al., 2014 |
| Crotalus durissus (Lineu, 1758) | Antiinflammatory | Ferreira et al. (2014) |
| Iguana iguana (Linnaeus, 1758) | Antiinflammatory | Ferreira et al. (2014) |
| Euphractus sexcinctus (Linnaeus, 1758) | Antiinflammatory | Ferreira et al. (2014) |
| Tupinambis merianae (Linnaeus, 1758) | Antiinflammatory | Ferreira et al. (2010) |
| Naja atra (Cantor, 1842) | Antiinflammatory | Zhu et al. (2016) |
There has been increasing attention paid to animals, both vertebrates and invertebrates, as a source for new medicines (Chivian, 2002). Animals have been methodically tested by pharmaceutical companies as sources of drugs for modern medical science (Kunin and Lawton, 1996), and the current percentage of animal sources for producing essential medicines is fairly significant. Of the 252 chemicals selected as essential by the World Health Organization, 11.1% are derived from plants and 8.7% from animals (Marques, 1997). Of the 150 prescription drugs currently in use in the United States of America, 27 have animal origin (World Resources Institute, 2000). Although the potential of faunal biodiversity is well known, a careful strategy is required if species are to be exploited sustainably. One of the main conservation concerns about the exploitation of fauna in the search for bioactive compounds is the possible overharvesting of target organisms (Alves and Albuquerque, 2013). Some taxa with known pharmacological potential are especially susceptible to overexploitation; for example, marine species such as cone shells and mollusks have been overharvested as sources of clinical neuropharmaceuticals (Sukarmi and Sabdono, 2011). Harvesting of reef organisms for the discovery and development of pharmaceuticals is causing increased concern, since it has been perceived by many as unsustainable and a threat to conservation (Hunt and Vincent, 2006, Sukarmi and Sabdono, 2011).
Bioprospecting continues to generate considerable debate (Alves and Albuquerque, 2013), as critics dispute the idea that the commodification of nature will contribute to conservation (Simpson, 1997), or that natural products have a future in the discovery of new drugs (Firn, 2003). Regardless of the perspective adopted, as highlighted by Barrett and Lybbert (2000), the need to conserve precious biodiversity is clear, especially as we begin to appreciate the magnitude of the spiritual, social, and economic services it provides.
Animals in Biomedical Research
In addition to their use in traditional medicine, in biotherapies, and as sources of medicinal drugs, animals are essential to research projects—with both direct and indirect implications for human health. Animal experimentation in the context of scientific research has contributed greatly to the development of medical science and technology, including the development of prophylactic measures and treatments for diseases that affect humans (Chorilli et al., 2009).
Although research using animals intensified during the last century, this technique is known to have been employed since ancient times (Alves, 2012), and animal research has formed the basis for much of the progress in understanding and treating human (and animal) diseases (Schacter, 2006). There are records of experimentation with animals reaching back to ancient Rome, but not until the Renaissance did scholars begin to seriously study how the body works. Leonardo da Vinci (1452–1519) and other artists and anatomists made early anatomical investigations of muscle and bone structure, and William Harvey (1578–1657) discovered the circulation of blood through his experiments with live deer. Much of the live animal experimentation during this period, both in England and France, was based on the view of the French philosopher René Descartes (1596–1650) that animals were incapable of feeling pain. The 19th century French physiologist, Claude Bernard (1813–78) and his teacher, François Magendie (1783–1855), conducted wide-ranging animal experiments, including surgery, the use of drugs, and the removal of body parts from many species (Bishop and Nolen, 2001).
From ancient to modern times, the use of animals in research has become one of the most important ways to better understand aspects of the anatomy, biochemistry, genetics, nutrition and physiology of humans. Additionally, knowledge of the transmission mechanisms and treatment of human diseases are associated with such research. According to Bishop and Nolen (2001), many, if not most, of the spectacular innovations in medical understanding and treatment of today’s human maladies have been based on research using animals.
Animals are used, for example, to develop new surgical techniques; test the efficacy and possible side effects of new drugs; determine the preventative and curative virtues of new medicines against diseases; test the safety of new chemicals used in the food industry; and check the quality of new batches of drugs and medicines (Bowman, 1977, Fitter, 1986). The discovery of antibiotics, analgesics, anesthetics, and antidepressants; the success of organ transplant development; catheterization; cardiac pacemaker and several other surgical techniques; practically all research protocols about safety, toxicity, effectiveness, and quality control of new drugs—all these pass through the use of laboratory animals. Other examples of scientific contributions arising from studies of animals are the discovery of insulin, the development of vaccines against several diseases, and serum production (Fagundes and Taha, 2004). Many drugs used by humans are directly produced from animals, for example, hormones used to overcome problems of fertility in humans are derived from cattle; insulin used to keep diabetics alive comes mainly from the pancreases of cattle and pigs. In addition, many vaccines are produced on animal tissue and on chicken eggs. Measles vaccine, for example, is produced on canine kidney tissue, as well as on eggs (Bowman, 1977).
Approximately 35 million animals are used worldwide in research each year, including dogs, monkeys, and cats, although 90% are laboratory rats, mice, and birds (Bishop and Nolen, 2001). Nonhuman primate species, because of their similarity to humans, are among the principal groups of animals used in biomedical research (Carlsson et al., 2004, Fitter, 1986), which are associated with significant contribution to advances in human health and disease control (Fitter, 1986). A wide variety of nonhuman primate species are used in these studies, involving at least 56 different extant species or subspecies (Carlsson et al., 2004), notably the Asian rhesus monkey Macaca mulatta and the African green or vervet monkey Cercopithecus aethiops (Carlsson et al., 2004, Fitter, 1986). These mammals are important and often essential for research in HIV/AIDS, malaria, cardiovascular diseases, cancers, and hepatitis, and also for the production and testing of drugs and vaccines. Similarly, armadillos have been used in medical research since the mid-1800s (Sharma et al., 2013). Studies involving these mammals have contributed to our knowledge of various infectious diseases, including syphilis and Chagas disease (Sharma et al., 2013, Wicher et al., 1983). However, the nine-banded armadillo Dasypus novemcinctus Linnaeus, 1758 has been most exploited as a model for leprosy (Peña et al., 2008, Scollard, 2008, Sharma et al., 2013) The armadillo is the only animal model in which protection against dissemination of leprosy bacilli or progress of nerve damage can be evaluated. Bacterins of heat-killed Mycobacterium leprae or viable BCG have been shown to protect armadillos against M. leprae challenge or enhance their immunity to the organism (Kirchheimer et al., 1978). Armadillos can also be used for testing new diagnostic candidates because they are the only host in which the true status of infection can be determined, and the long incubation period of leprosy in humans can cause confounding results (Sharma et al., 2013). Another animal group used in medical research experiments are marsupials (Jurgelski, 1984). The opossum, Didelphis virginiana, for example, is used in endocrinological, embryological, anatomical, psychiatric, and neurological research (Wiedorn, 1954).
A dynamic tension exists between support for scientific enquiry, mostly to alleviate human disease and public concern about animal suffering (Bishop and Nolen, 2001). This discussion is not new, however, and as early as the 16th century philosophers were debating the morality of animal experimentation, with their arguments centering on whether animals felt pain and the moral status of animals as living, sentient creatures (Schacter, 2006). Although the discovery of anesthetics and their use in animal experiments might have been expected to somewhat quiet this issue, revulsion at the use and potential misuse of animals for human betterment sustains a significant activism opposed to any use of animals in research (Schacter, 2006).
Conclusions
Humans are animals that live in association with thousands of other animal species and share the same environment and a wide diversity of diseases that can be mutually transmitted. If, on one hand, animals are vectors of human diseases, they are also indispensable for their treatments and cures. Products derived from animals are fundamental ingredients of both traditional remedies and modern drugs; live animals can alert us to approaching epidemics and are protagonists and agents in many therapies, and are fundamental to research efforts that seek to understand human illnesses and test modern medicines. It is therefore clear that human health depends on the health of both animals and our environment, and that health strategies must always take this intricate interdependence into consideration.
References
- Adeola M.O. Importance of wild animals and their parts in the culture, religious festivals, and traditional medicine, of Nigeria. Environmental Conservation. 1992;19:125–134. [Google Scholar]
- Adhya M., Singha B., Chatterjee B.P. Purification and characterization of an N-acetylglucosamine specific lectin from marine bivalve Macoma birmanica. Fish & Shellfish Immunology. 2009;27:1–8. doi: 10.1016/j.fsi.2008.11.001. [DOI] [PubMed] [Google Scholar]
- Alakbarli F. Heydar Aliyev Foundation; Baku: 2006. Medical Manuscripts of Azerbaijan. [Google Scholar]
- Alqutub A.N., Masoodi I., Alsayari K., Alomair A. Bee sting therapy-induced hepatotoxicity: a case report. World Journal of Hepatology. 2011;3:268–270. doi: 10.4254/wjh.v3.i10.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves R.R.N. Relationships between fauna and people and the role of ethnozoology in animal conservation. Ethnobiology and Conservation. 2012;1:1–69. [Google Scholar]
- Alves R.R.N., Albuquerque U.P. Ethnobiology and conservation: why do we need a new journal? Ethnobiology and Conservation. 2012;1:1–3. [Google Scholar]
- Alves R.R.N., Albuquerque U.P. Animals as a source of drugs: bioprospecting and biodiversity conservation. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer Heidelberg; 2013. pp. 67–89. [Google Scholar]
- Alves R.R.N., Alves H.N. The faunal drugstore: animal-based remedies used in traditional medicines in Latin America. Journal of Ethnobiology and Ethnomedicine. 2011;7:1–43. doi: 10.1186/1746-4269-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves R.R.N., Dias T.L.P. Usos de invertebrados na medicina popular no Brasil e suas implicações para conservação. Tropical Conservation Science. 2010;3:159–174. [Google Scholar]
- Alves R.R.N., Rosa I.L. Why study the use of animal products in traditional medicines? Journal of Ethnobiology and Ethnomedicine. 2005;1:1–5. doi: 10.1186/1746-4269-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves R.R.N., Rosa I.L. From cnidarians to mammals: the use of animals as remedies in fishing communities in NE Brazil. Journal of Ethnopharmacology. 2006;107:259–276. doi: 10.1016/j.jep.2006.03.007. [DOI] [PubMed] [Google Scholar]
- Alves R.R.N., Rosa I.L. Biodiversity, traditional medicine and public health: where do they meet? Journal of Ethnobiology and Ethnomedicine. 2007;3:1–9. doi: 10.1186/1746-4269-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves R.R.N., Rosa I.L. Springer-Verlag; Berlin Heidelberg: 2013. Animals in Traditional Folk Medicine: Implications for Conservation. [Google Scholar]
- Alves R.R.N., Rosa I.L. Introduction: toward a plural approach to the study of medicinal animals. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer-Verlag; Berlin Heidelberg: 2013. [Google Scholar]
- Alves R.R.N., Rosa I.L., Santana G.G. The role of animal-derived remedies as complementary medicine in Brazil. BioScience. 2007;57:949–955. [Google Scholar]
- Alves R.R.N., Vieira W.L.S., Santana G.G. Reptiles used in traditional folk medicine: conservation implications. Biodiversity and Conservation. 2008;17:2037–2049. [Google Scholar]
- Alves R.R.N., Oliveira M.G.G., Barboza R.R.D., Singh R., Lopez L.C.S. Medicinal animals as therapeutic alternative in a semi-arid region of Northeastern Brazil. Forsch Komplementärmedizin/Research in Complementary Medicine. 2009;16:305–312. doi: 10.1159/000235855. [DOI] [PubMed] [Google Scholar]
- Alves R.R.N., Barboza R.R.D., Souto W.M.S. A global overview of canids used in traditional medicines. Biodiversity and Conservation. 2010;19:1513–1522. [Google Scholar]
- Alves R.R.N., Souto W.M.S., Barboza R.R.D. Primates in traditional folk medicine: a world overview. Mammal Review. 2010;40:155–180. [Google Scholar]
- Alves R.R.N., Rosa I.L., Léo Neto N.A., Voeks R. Animals for the Gods: magical and religious faunal use and trade in Brazil. Human Ecology. 2012;40:751–780. [Google Scholar]
- Alves R.R.N., Lima J.R.F., Araújo H.F. The live bird trade in Brazil and its conservation implications: an overview. Bird Conservation International. 2013;23:53–65. [Google Scholar]
- Alves R.R.N., Medeiros M.F.T., Albuquerque U.P., Rosa I.L. From past to present: medicinal animals in a historical perspective. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer; 2013. pp. 11–23. [Google Scholar]
- Alves R.R.N., Oliveira T.P.R., Rosa I.L., Cunningham A.B. Marine invertebrates in traditional medicines. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer; Berlin: 2013. pp. 263–287. [Google Scholar]
- Alves R.R.N., Pinto L.C.L., Barboza R.R.D., Souto W.M.S., Oliveira R.E.M.C.C., Vieira W.L.S. A global overview of carnivores used in traditional medicines. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer; 2013. pp. 171–206. [Google Scholar]
- Alves R.R.N., Souto W.M.S., Barboza R.R.D., Bezerra D.M.M. Primates in traditional folk medicine: world overview. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer; Berlin: 2013. pp. 135–170. [Google Scholar]
- Alves R.R.N., Souto W.M.S., Oliveira R.E.M.C.C., Barboza R.R.D., Rosa I.L. Aquatic mammals used in traditional folk medicine: a global analysis. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer; Heidelberg: 2013. pp. 241–261. [Google Scholar]
- Alves R.R.N., Vieira W.L.S., Santana G.G., Vieira K.S., Montenegro P.F.G.P. Herpetofauna used in traditional folk medicine: conservation implications. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer-Verlag; Berlin Heidelberg: 2013. pp. 109–133. [Google Scholar]
- Alves R.R.N., Melo M.F., Ferreira F.S., Trovão D.M.B.M., Dias T.L.P., Oliveira J.V., Lucena R.F.P., Barboza R.R.D. Healing with animals in a semiarid northeastern area of Brazil. Environment, Development and Sustainability. 2016;18:1733–1747. [Google Scholar]
- Anyinam C. Ecology and ethnomedicine: exploring links between current environmental crisis and indigenous medical practices. Social Science & Medicine. 1995;40:321–329. doi: 10.1016/0277-9536(94)e0098-d. [DOI] [PubMed] [Google Scholar]
- Ashwell D., Walston N. first ed. TRAFFIC Southeast Asia, Greater Mekong Programme, Ha Noi, Vietnam; 2008. An Overview of the Use and Trade of Plants and Animals in Traditional Medicine Systems in Cambodia. [Google Scholar]
- Ávila-Pires F.D. Zoonoses: hospedeiros e reservatórios. Cadernos de Saúde Pública. 1989;5:82–97. [Google Scholar]
- Baer W.S. The treatment of chronic osteomyelitis with the maggot (larva of the blow fly) The Journal of Bone & Joint Surgery American. 1931;13:438–475. [Google Scholar]
- Barker S.B., Dawson K.S. The effects of animal-assisted therapy on anxiety ratings of hospitalized psychiatric patients. Psychiatric Services. 1998;49:797–801. doi: 10.1176/ps.49.6.797. [DOI] [PubMed] [Google Scholar]
- Barrett C.B., Lybbert T.J. Is bioprospecting a viable strategy for conserving tropical ecosystems? Ecological Economics. 2000;34:293–300. [Google Scholar]
- Batson K. The effect of a therapy dog on socialization and physiological indicators of stress in persons diagnosed. In: Wilson C.C., Turner D.C., editors. Companion Animals in Human Health. Sage; Thousand Oaks: 1998. p. 203. [Google Scholar]
- Beck B.F. D. Appleton-Century Company; 1935. Bee Venom Therapy: Bee Venom, Its Nature, and Its Effect on Arthritic and Rheumatoid Conditions. [Google Scholar]
- Beck A. The use of animals to benefit humans, animal-assisted therapy. In: Fine A.H., editor. The Handbook on Animal Assisted Therapy: Theoretical Foundations and Guidelines for Practice. Academic Press; San Diego: 2000. [Google Scholar]
- Bell J.C., Palmer S.R., Payne J.M. Arnold; London: 1988. The Zoonoses (Infections Transmitted from Animals to Man) [Google Scholar]
- Bengis R.G., Leighton F.A., Fischer J.R., Artois M., Mörner T., Tate C.M. The role of wildlife in emerging and re-emerging zoonoses. Revue Scientifique et Technique, Office International Epizooties. 2004;23:497–511. [PubMed] [Google Scholar]
- Bishop L.J., Nolen A.L. Animals in research and education: ethical issues. Kennedy Institute of Ethics Journal. 2001;11:91–113. doi: 10.1353/ken.2001.0006. [DOI] [PubMed] [Google Scholar]
- Bisset N.G. One man’s poison, another man’s medicine? Journal of Ethnopharmacology. 1991;32:71–81. doi: 10.1016/0378-8741(91)90105-m. [DOI] [PubMed] [Google Scholar]
- Bowman J.C. Edward Arnold.; London: 1977. Animals for Man. [Google Scholar]
- Brown C. Emerging zoonoses and pathogens of public significance—an overview. Revue Scientifique et Technique, Office International Epizooties. 2004;23:435–442. doi: 10.20506/rst.23.2.1495. [DOI] [PubMed] [Google Scholar]
- Burgos S., Burgos S.A. Influence of exotic bird and wildlife trade on avian influenza transmission dynamics: animal-human interface. International Journal of Poultry Science. 2007;6:535–538. [Google Scholar]
- Burrell G.A., Seibert F.M. Bur. Mines, Dep. Inter.; Washington, DC: 1916. Gases Found in Coal Mines. Miners’ Circ. 14. [Google Scholar]
- Cabral H., Carneiro J. O papel da ictioterapia no tratamento da psoríase: relato de caso. Revista Portuguesa de Medicina Geral e Familiar. 2014;30:402–405. [Google Scholar]
- Cabral M.E.S., Dias D.Q., Sales D.L., Oliveira O.P., Teles D.A., Sousa J.G.G., Coutinho H.D.M., Costa J.G.M., Kerntopf M.R., Alves R.R.N. Evaluations of the antimicrobial activities and chemical compositions of body fat from the amphibians Leptodactylus macrosternum Miranda-Ribeiro (1926) and Leptodactylus vastus Adolf Lutz (1930) in Northeastern Brazil. Evidence-Based Complementary and Alternative Medicine. 2013;2013:1–7. doi: 10.1155/2013/913671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Call E. International Fund for Animal Welfare; Massachusetts: 2006. Mending the Web of Life: Chinese Medicine and Species Conservation. [Google Scholar]
- Cardoso J.S., Gonçalves J.M., Fagundes E.N., Costa Neto E.M., Uetanabaro A.P.T. Tratamento de infecções cutâneas com Dinoponera quadriceps: atividade antimicrobiana comprovada. In: Costa-Neto E.M., Alves R.R.N., editors. Zooterapia: Os Animais na Medicina Popular Brasileira. Nupeea; Recife: 2010. pp. 141–157. [Google Scholar]
- Carlsson H.E., Schapiro S.J., Farah I., Hau J. Use of primates in research: a global overview. American Journal of Primatology. 2004;63:225–237. doi: 10.1002/ajp.20054. [DOI] [PubMed] [Google Scholar]
- Ceríaco L.M.P. A review of fauna used in zootherapeutic remedies in Portugal: historical origins, current uses, and implications for conservation. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine. Springer-Verlag; Berlin-Heidelberg: 2013. pp. 317–345. [Google Scholar]
- Chandler C.K. Routledge; New York: 2012. Animal Assisted Therapy in Counseling. [Google Scholar]
- Chaves T.P., Clementino E.L.C., Felismino D.C., Alves R.R.N., Vasconcellos A., Coutinho H.D.M., Medeiros A.C.D. Antibiotic resistance modulation by natural products obtained from Nasutitermes corniger (Motschulsky, 1855) and its nest. Saudi Journal of Biological Sciences. 2014;22:404–408. doi: 10.1016/j.sjbs.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Check E. Health concerns prompt US review of exotic-pet trade. Nature. 2004;427:277. doi: 10.1038/427277a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemas R.C. A zooterapia no âmbito da medicina civilizada. I. Organoterapia humana e animal stricto sensu. In: Costa-Neto E.M., Alves R.R.N., editors. Zooterapia: Os Animais na Medicina Popular Brasileira. first ed. NUPEEA; Recife, PE, Brazil: 2010. pp. 75–102. [Google Scholar]
- Cherniack E.P. Bugs as drugs, part 1: insects: the “new” alternative medicine for the 21st century. Alternative Medicine Review. 2010;15:124–135. [PubMed] [Google Scholar]
- Chivian E. Harvard Medical School; Boston: 2002. Biodiversity: Its Importance to Human Health. [Google Scholar]
- Chomel B.B. Zoonosis bacterianas de aparición reciente. Revista Panamericana de Salud Publica. 2002;11:50–55. [PubMed] [Google Scholar]
- Chomel B.B. Control and prevention of emerging zoonoses. Journal of Veterinary Medical Education. 2003;30:145–147. doi: 10.3138/jvme.30.2.145. [DOI] [PubMed] [Google Scholar]
- Chomel B.B., Belotto A., Meslin F.X. Wildlife, exotic pets, and emerging zoonoses. Emerging Infectious Diseases. 2007;13:6–11. doi: 10.3201/eid1301.060480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorilli M., Michelin D.C., Salgado H.R.N. Animais de laboratório: o camundongo. Revista de Ciências Farmacêuticas Básica e Aplicada. 2009;28:11–23. [Google Scholar]
- Cleaveland S., Laurenson M.K., Taylor L.H. Diseases of humans and their domestic mammals: pathogen characteristics, host range and the risk of emergence. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences. 2001;356:991–999. doi: 10.1098/rstb.2001.0889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole K.M., Gawlinski A., Steers N., Kotlerman J. Animal-assisted therapy in patients hospitalized with heart failure. American Journal of Critical Care. 2007;16:575–585. [PubMed] [Google Scholar]
- Cologna C.T., Barbosa D.B., Santana F.A., Rodovalho C.M., Oliveira L.A., Brandeburgo M.A.M. Convênio CNPq/UFU; Uberlândia: 2005. Estudo da peçonha de Dinoponera australis—Roger, 1861 (Hymenoptera, Ponerinae), V Encontro interno de Iniciação científica. [Google Scholar]
- Connor K., Miller J. Animal-assisted therapy: an in-depth look. Dimensions of Critical Care Nursing. 2000;19:20–26. doi: 10.1097/00003465-200019030-00006. [DOI] [PubMed] [Google Scholar]
- Correale J., Farez M. Association between parasite infection and immune responses in multiple sclerosis. Annals of Neurology. 2007;61:97–108. doi: 10.1002/ana.21067. [DOI] [PubMed] [Google Scholar]
- Correale J., Farez M.F. The impact of parasite infections on the course of multiple sclerosis. Journal of Neuroimmunology. 2011;233:6–11. doi: 10.1016/j.jneuroim.2011.01.002. [DOI] [PubMed] [Google Scholar]
- Costa-Neto E.M. Entomotherapy, or the medicinal use of insects. Journal of Ethnobiology. 2005;25:93–114. [Google Scholar]
- Coutinho H.D.M., Bezerra D.A.C., Lôbo K., Barbosa I.J.F. Atividade antimicrobiana de produtos naturais. Revista Conceitos. 2004;77:77–85. [Google Scholar]
- Coutinho H., Vasconcellos A., Lima M., Almeida-Filho G., Alves R.R.N. Termite usage associated with antibiotic therapy: enhancement of aminoglycoside antibiotic activity by natural products of Nasutitermes corniger (Motschulsky 1855) BMC Complementary and Alternative Medicine. 2009;9:35. doi: 10.1186/1472-6882-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coutinho H.D.M., Vasconcellos A., Freire-Pessôa H.L., Gadelha C.A., Gadelha T.S., Almeida-Filho G.G. Natural products from the termite Nasutitermes corniger lowers aminoglycoside minimum inhibitory concentrations. Pharmacognosy Magazine. 2010;6:1–4. doi: 10.4103/0973-1296.59958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coutinho H., Aquino P., Leite J., Leandro L., Figueredo F., Matias E., Guedes T. Modulação da atividade antibacteriana do tecido adiposo da Gallus gallus domesticus (Linnaeus, 1758)/Modulatory antibacterial activity of body fat from Gallus gallus domesticus (Linnaeus 1758) Comunicata Scientiae. 2014;5:380. [Google Scholar]
- Dallavecchia D.L., Proença B.N., Aguiar Coelho V.M. Biotherapy: an efficient alternative for the treatment of skin lesions. Revista de Pesquisa: Cuidado é Fundamental Online. 2011;3:2071–2087. [Google Scholar]
- De Smet P.A.G.M. Is there any danger in using traditional remedies? Journal of Ethnopharmacology. 1991;32:43–50. doi: 10.1016/0378-8741(91)90102-j. [DOI] [PubMed] [Google Scholar]
- Debnath A., Chatterjee U., Das M., Vedasiromoni J.R., Gomes A. Venom of Indian monocellate cobra and Russell’s viper show anticancer activity in experimental models. Journal of Ethnopharmacology. 2007;111:681–684. doi: 10.1016/j.jep.2006.12.027. [DOI] [PubMed] [Google Scholar]
- Djagoun C.A.M.S., Akpona H.A., Mensah G.A., Nuttman C., Sinsin B. Wild mammals trade for zootherapeutic and mythic purposes in Benin (West Africa): capitalizing species involved, provision sources, and implications for conservation. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer-Verlag; Berlin Heidelberg: 2013. pp. 367–381. [Google Scholar]
- Donia M., Hamann M.T. Marine natural products and their potential applications as anti-infective agents. The Lancet Infectious Diseases. 2003;3:338–348. doi: 10.1016/S1473-3099(03)00655-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dossey A.T. Insects and their chemical weaponry: new potential for drug discovery. Natural Product Reports. 2010;27:1737–1757. doi: 10.1039/c005319h. [DOI] [PubMed] [Google Scholar]
- Elliot D.E., Pritchard D.I., Weinstock J.V. Helminth therapy. In: Grassberger M., Sherman R.A., Gileva O.S., Kim C.M.H., Mumcuoglu K.Y., editors. Biotherapy—History, Principles and Practice: A Practical Guide to the Diagnosis and Treatment of Disease Using Living Organisms. Springer; Dordrecht, The Netherlands: 2013. pp. 177–190. [Google Scholar]
- European Commission . 2011. Biodiversity and Health. [Google Scholar]
- Fagundes D.J., Taha M.O. Modelo animal de doença: critérios de escolha e espécies de animais de uso corrente. Acta Circurgica Brasileira. 2004;19:59–65. [Google Scholar]
- Faulkner D.J. Marine natural products. Natural Product Reports. 1998;15:113–158. doi: 10.1039/a815113y. [DOI] [PubMed] [Google Scholar]
- Ferguson N.M., Cummings D.A.T., Cauchemez S., Fraser C., Riley S., Meeyai A., Iamsirithaworn S., Burke D.S. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437:209–214. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- Ferreira F.S., Brito S.V., Saraiva R.A., Araruna M.K.A., Menezes I.R.A., Costa J.G.M., Coutinho H.D.M., Almeida W.O., Alves R.R.N. Topical anti-inflammatory activity of body fat from the lizard Tupinambis merianae. Journal of Ethnopharmacology. 2010;130:514–520. doi: 10.1016/j.jep.2010.05.041. [DOI] [PubMed] [Google Scholar]
- Ferreira F.S., Silva N.L.G., Matias E.F.F., Brito S.V., Oliveira F.G., Costa J.G.M., Coutinho H.D.M., Almeida W.O., Alves R.R.N. Potentiation of aminoglycoside antibiotic activity using the body fat from the snake Boa constrictor. Revista Brasileira de Farmacognosia. 2011;21:503–509. [Google Scholar]
- Ferreira F.S., Albuquerque U.P., Coutinho H.D.M., Almeida W.O., Alves R.R.N. The trade in medicinal animals in northeastern Brazil. Evidence-based Complementary and Alternative Medicine. 2012;2012:1–20. doi: 10.1155/2012/126938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira F.S., Fernandes-Ferreira H., Leo Neto N., Brito S.V., Alves R.R.N. The trade of medicinal animals in Brazil: current status and perspectives. Biodiversity and Conservation. 2013;22:839–870. [Google Scholar]
- Ferreira F.S., Brito S.V., Sales D.L., Menezes I.R.A., Coutinho H.D.M., Souza E.P., Almeida W.O., Alves R.R.N. Anti-inflammatory potential of zootherapeutics derived from animals used in Brazilian traditional medicine. Pharmaceutical Biology. 2014;52:1403–1410. doi: 10.3109/13880209.2014.894091. [DOI] [PubMed] [Google Scholar]
- Figueirêdo R.E.C.R., Vasconcellos A., Policarpo I.S., Alves R.R.N. Edible and medicinal termites: a global overview. Journal of Ethnobiology and Ethnomedicine. 2015;11:1–7. doi: 10.1186/s13002-015-0016-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine A.H. Academic Press; 2010. Handbook on Animal-assisted Therapy: Theoretical Foundations and Guidelines for Practice. [Google Scholar]
- Fine A., Alexander H. Maggot therapy—technique and clinical application. Journal of Bone and Joint Surgery. 1934;16:572–582. [Google Scholar]
- Firn R.D. Bioprospecting–why is it so unrewarding? Biodiversity and Conservation. 2003;12:207–216. [Google Scholar]
- Fitter R.S.R. Collins; London, London: 1986. Wildlife for Man: How and Why We Should Conserve Our Species. [Google Scholar]
- Fleming J.O., Isaak A., Lee J.E., Luzzio C.C., Carrithers M.D., Cook T.D., Field A.S., Boland J., Fabry Z. Probiotic helminth administration in relapsing–remitting multiple sclerosis: a phase 1 study. Multiple Sclerosis Journal. 2011;17:743–754. doi: 10.1177/1352458511398054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friend M. US Department of the Interior, US Geological Survey; 2006. Disease Emergence and Resurgence: The Wildlife-human Connection. [Google Scholar]
- Froese R., Pauly D. 2016. Garra rufus. [Google Scholar]
- Fusetani N. S Karger Pub; 2000. Drugs from the Sea. [Google Scholar]
- Gileva O.S., Mumcuoglu K.Y. Hirudotherapy. In: Grassberger M., Sherman R.A., Gileva O.S., Kim C.M.H., Mumcuoglu K.Y., editors. Biotherapy-History, Principles and Practice: A Practical Guide to the Diagnosis and Treatment of Disease Using Living Organisms. Springer; Dordrecht, Heidelberg, New York, London: 2013. pp. 31–76. [Google Scholar]
- Gilyova O.S. Modern hirudotherapy–a review. The BeTER LeTTER. 2005;2:1–3. [Google Scholar]
- Glickman L.T., Fairbrother A., Guarino A.M., Bergman H.L., Buck W.B. National Research Council, Committee on Animals as Monitors of Environmental Hazards; Washington, DC: 1991. Animals as Sentinels of Environmental Health Hazards. [Google Scholar]
- Godfrey K. Use of leeches and leech saliva in clinical practice. Nursing Times. 1997;93:62–63. [PubMed] [Google Scholar]
- Grantham-Hill C. Preliminary note on the treatment of infected wounds with the larva of Wohlfartia nuba. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1933;27:93–98. [Google Scholar]
- Grassberger M., Sherman R.A., Gileva O.S., Kim C.M.H., Mumcuoglu K.Y. Springer; 2013. Biotherapy–History, Principles and Practice: A Practical Guide to the Diagnosis and Treatment of Disease Using Living Organism. [Google Scholar]
- Grassberguer M., Sherman R.A. Ichthyotherapy. In: Grassberger M., Sherman R.A., Gileva O.S., Kim C.M.H., Mumcuoglu K.Y., editors. Biotherapy—History, Principles and Practice: A Practical Guide to the Diagnosis and Treatment of Disease Using Living Organisms. Springer Science+Business Media; Dordrecht, The Netherlands: 2013. pp. 147–176. [Google Scholar]
- Gunjegaonkar S.M., Kshirsagar S.S., Bayas J.P. Bio-surgical therapy-overview. International Journal of Pharmacological Research. 2016;6:133–137. [Google Scholar]
- Hammond P.B., Aronson A.L. Lead poisoning in cattle and horses in the vicinity of a smelter. Annals of the New York Academy of Sciences. 1964;111:595–611. doi: 10.1111/j.1749-6632.1964.tb53128.x. [DOI] [PubMed] [Google Scholar]
- Hardy A. Animals, disease, and man: making connections. Perspectives in Biology and Medicine. 2003;46:200–215. doi: 10.1353/pbm.2003.0021. [DOI] [PubMed] [Google Scholar]
- Hooker S.D., Freeman L.H., Stewart P. Pet therapy research: a historical review. Holistic Nursing Practice. 2002;17:17–23. doi: 10.1097/00004650-200210000-00006. [DOI] [PubMed] [Google Scholar]
- Horn K.L., Cobb A.H., Gates G.A. Maggot therapy for subacute mastoiditis. Archives of Otolaryngology. 1976;102:377–379. doi: 10.1001/archotol.1976.00780110089013. [DOI] [PubMed] [Google Scholar]
- Hunt B., Vincent A.C.J. Scale and sustainability of marine bioprospecting for pharmaceuticals. AMBIO: A Journal of the Human Environment. 2006;35:57–64. doi: 10.1579/0044-7447(2006)35[57:sasomb]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- IFAW, I.F.f.A.W. 2011. Traditional Medicine. [Google Scholar]
- Ireland C.M., Copp B.R., Foster M.P., McDonald L.A., Radisky D.C., Swersey J.C. Biomedical potential of marine natural products. Marine Biotechnology. 1993;1:1–43. [Google Scholar]
- Julian K.G., Eidson M., Kipp A.M., Weiss E., Petersen L.R., Miller J.R., Hinten S.R., Marfin A.A. Early season crow mortality as a sentinel for West Nile virus disease in humans, northeastern United States. Vector Borne and Zoonotic Diseases. 2002;2:145–155. doi: 10.1089/15303660260613710. [DOI] [PubMed] [Google Scholar]
- Jurgelski W. The marsupial as a biomedical model. International Journal of Toxicology. 1984;3:343–355. [Google Scholar]
- Kahn L.H. Confronting zoonoses, linking human and veterinary medicine. Emerging Infectious Diseases. 2006;12:556–561. doi: 10.3201/eid1204.050956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karesh W.B., Noble E. The bushmeat trade: increased opportunities for transmission of zoonotic disease. Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine. 2009;76:429–434. doi: 10.1002/msj.20139. [DOI] [PubMed] [Google Scholar]
- Karesh W.B., Cook R.A., Bennett E.L., Newcomb J. Wildlife trade and global disease emergence. Emerging Infectious Diseases. 2005;11:1000–1002. doi: 10.3201/eid1107.050194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karesh W.B., Cook R.A., Gilbert M., Newcomb J. Implications of wildlife trade on the movement of avian influenza and other infectious diseases. Journal of Wildlife Diseases. 2007;43:S55–S59. [Google Scholar]
- Karthikeyan R., Karthigayan S., Sri Balasubashini M., Somasundaram S.T., Balasubramanian T. Inhibition of Hep2 and HeLa cell proliferation in vitro and EAC tumor growth in vivo by Lapemis curtus (Shaw 1802) venom. Toxicon. 2008;51:157–161. doi: 10.1016/j.toxicon.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Khan A.R., Fallon P.G. Helminth therapies: translating the unknown unknowns to known knowns. International Journal for Parasitology. 2013;43:293–299. doi: 10.1016/j.ijpara.2012.12.002. [DOI] [PubMed] [Google Scholar]
- Kim C.M.H. Apitherapy–bee venom therapy. In: Grassberger M., Sherman R.A., Gileva O.S., Kim C.M.H., Mumcuoglu K.Y., editors. Biotherapy—History, Principles and Practice: A Practical Guide to the Diagnosis and Treatment of Disease Using Living Organisms. Springer Science+Business Media; Dordrecht, The Netherlands: 2013. pp. 77–112. [Google Scholar]
- Kirchheimer W.F., Sanchez R.M., Shannon E.J. Effect of specific vaccine on cell-mediated immunity of armadillos against M. leprae. International Journal of Leprosy and Other Mycobacterial Diseases. 1978;46:353–357. [PubMed] [Google Scholar]
- Krauss H. Zoonoses: infectious diseases transmissible from animals to humans. American Society for Microbiology. 2003 [Google Scholar]
- Kritsky G. Insects in traditional Chinese medicines. Proceedings of the Indiana Academy of Science. 1987;96:289–291. [Google Scholar]
- Kruger K.A., Serpell J.A., Fine A.H. Animal-assisted interventions in mental health: definitions and theoretical foundations. In: Fine A.H., editor. Handbook on Animal-Assisted Therapy: Theoretical Foundations and Guidelines for Practice. Academic Press; California: 2006. pp. 21–38. [Google Scholar]
- Kruse H., Kirkemo A.M., Handeland K. Wildlife as source of zoonotic infections. Emerging Infectious Diseases. 2004;10:2067–2072. doi: 10.3201/eid1012.040707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunin W.E., Lawton J.H. Does biodiversity matter? Evaluating the case for conserving species. In: Gaston K.J., editor. Biodiversity. A Biology of Numbers and Difference Blackwell Science. Oxford; UK: 1996. pp. 367–387. [Google Scholar]
- Lamberty M., Zachary D., Lanot R., Bordereau C., Robert A., Hoffmann J.A., Bulet P. Insect immunity constitutive expression of a cysteine-rich antifungal and a linear antibacterial peptide in a termite insect. Journal of Biological Chemistry. 2001;276:4085–4092. doi: 10.1074/jbc.M002998200. [DOI] [PubMed] [Google Scholar]
- Lee S.K.H. 2nd Australian Symposium on Traditional Medicine and Wildlife Conservation. Australia; Melbourne: 1999. Trade in traditional medicine using endangered species: an international context. [Google Scholar]
- Leonardi-Bee J., Pritchard D., Britton J. Asthma and current intestinal parasite infection: systematic review and meta-analysis. American Journal of Respiratory and Critical Care Medicine. 2006;174:514–523. doi: 10.1164/rccm.200603-331OC. [DOI] [PubMed] [Google Scholar]
- Lerclercq M. Utilisation de larves de dipteres-Maggot Therapy-en medecine: historique et actualite. Bulletin et Annales de la Societe Royale Belge d’Entomologie. 1990;126:41–50. [Google Scholar]
- Lilley B., Lammie P., Dickerson J., Eberhard M. An increase in hookworm infection temporally associated with ecologic change. Emerging Infectious Diseases. 1997;3:391–393. doi: 10.3201/eid0303.970321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lone A.H., Ahmad T., Anwar M., Habib S., Sofi G., Imam H. Leech therapy-a holistic approach of treatment in unani (greeko-arab) medicine. Ancient Science of Life. 2011;31:31–35. [PMC free article] [PubMed] [Google Scholar]
- Lucache B., Albu E., Mungiu O.C. Acupuncture and bee venom therapy in the chronic low back pain: a short review. African Journal of Traditional, Complementary and Alternative Medicines. 2015;12:76–80. [Google Scholar]
- MacKinney L.C. Animal substances in materia medica. Journal of the History of Medicine and Allied Sciences. 1946;1:149–170. doi: 10.1093/jhmas/1.1.149. [DOI] [PubMed] [Google Scholar]
- Mahawar M.M., Jaroli D.P. Traditional zootherapeutic studies in India: a review. Journal of Ethnobiology and Ethnomedicine. 2008;4:17. doi: 10.1186/1746-4269-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques J.G.W. Fauna medicinal: Recurso do ambiente ou ameaça à biodiversidade. Mutum. 1997;1:4. [Google Scholar]
- Martin F., Farnum J. Animal-assisted therapy for children with pervasive developmental disorders. Western Journal of Nursing Research. 2002;24:657–670. doi: 10.1177/019394502320555403. [DOI] [PubMed] [Google Scholar]
- Martinez G.J. Use of fauna in the traditional medicine of native Toba (qom) from the Argentine Gran Chaco region: an ethnozoological and conservationist approach. Ethnobiology and Conservation. 2013;2:1–43. [Google Scholar]
- Martini R.K., Sherman R.A. Terapia de desbridamento com larvas. Journal Brasileiro de Medicina. 2003;85:82–85. [Google Scholar]
- Masaro A.L., Jr., Della Luccia T.M.C., Barbosa L.C.A., Maffia L.A., Morandi M.A.B. Inhibition of the germination of Botrytis cinerea Pers. Fr. conidia by extracts of the mandibular gland of Atta sexdens rubropilosa forel (Hymenoptera: Formicidae) Neotropical Entomology. 2001;30:403–406. [Google Scholar]
- McCluskey B.J. Use of sentinel herds in monitoring and surveillance systems. In: Salman, editor. Animal Disease Surveillance and Survey Systems: Methods Applications. Iowa State Press; Iowa: 2003. pp. 119–133. [Google Scholar]
- McConnell E. Myths & facts…about animal-assisted therapy. Nursing. 2002;32:76. doi: 10.1097/00152193-200203000-00065. [DOI] [PubMed] [Google Scholar]
- McGibbon N.H., Andrade C.K., Widener G., Cintas H.L. Effect of an equine-movement therapy program on gait, energy expenditure, and motor function in children with spastic cerebral palsy: a pilot study. Developmental Medicine & Child Neurology. 1998;40:754–762. doi: 10.1111/j.1469-8749.1998.tb12344.x. [DOI] [PubMed] [Google Scholar]
- McLellan N.W. The maggot treatment of osteomyelitis. Canadian Medical Association Journal. 1932;27:256–260. [PMC free article] [PubMed] [Google Scholar]
- Mi E., Mi E., Jeggo M. Where to now for one health and ecohealth? EcoHealth. 2016;13:12–17. doi: 10.1007/s10393-016-1112-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moquin-Tandon A. Baillière; 1861. Elements of Medical Zoology. [Google Scholar]
- Moreira D.R. Apiterapia no tratamento de patologias. Revista F@pciência. 2012;9:21–29. [Google Scholar]
- Munir T., Malik M.F., Hashim M., Qureshi M.A., Naseem S. Therapeutic applications of blowfly maggots: a review. Journal of Entomology and Zoology Studies. 2016;4(5):33–36. [Google Scholar]
- Myers N. The Sinking Ark: A New Look at the Problem of Disappearing Species. Pergamon Press; New York: 1979. [Google Scholar]
- Nakanishi K. Comprehensive Natural Products Chemistry: Isoprenoids Including Carotenoids and Steroids. 1999. An historical perspective of natural products chemistry. [Google Scholar]
- Nimer J., Lundahl B. Animal-assisted therapy: a meta-analysis. Anthrozoos. 2007;20:225–238. [Google Scholar]
- Oliva V.N.L.S. Terapia assistida por Animais. In: Costa- Neto E.M., Alves R.R.N., editors. Zooterapia: Os Animais na Medicina Popular Brasileira. Nuppea; Recife: 2010. pp. 127–140. [Google Scholar]
- Oliveira O.P., Sales D.L., Dias D.Q., Cabral M.E.S, Araújo Filho J.A., Teles D.A., Sousa J.G.G., Ribeiro S.C., Freitas F.R.D., Coutinho H.D.M., Kerntopf M.R., Costa J.G.M., Alves R.R.N., Almeida W.O. Antimicrobial activity and chemical composition of fixed oil extracted from the body fat of the snake Spilotes pullatus. Pharmaceutical Biology. 2014;52:740–744. doi: 10.3109/13880209.2013.868495. [DOI] [PubMed] [Google Scholar]
- One Health . 2010. One Health Commission. [Google Scholar]
- Ozcelik S., Akyol M. Kangal hot spring with fish (Kangal fishy Health spa) & Psoriasis. La Presse Thermale et Climatique. 2011;148:141–147. [Google Scholar]
- Patz J.A., Graczyk T.K., Geller N., Vittor A.Y. Effects of environmental change on emerging parasitic diseases. International Journal for Parasitology. 2000;30:1395–1405. doi: 10.1016/s0020-7519(00)00141-7. [DOI] [PubMed] [Google Scholar]
- Pemberton R.W. Insects and other arthropods used as drugs in Korean traditional medicine. Journal of Ethnopharmacology. 1999;65:207–216. doi: 10.1016/s0378-8741(98)00209-8. [DOI] [PubMed] [Google Scholar]
- Peña M.T., Adams J.E., Adams L.B., Gillis T.P., Williams D.L., Spencer J.S., Krahenbuhl J.L., Truman R.W. Expression and characterization of recombinant interferon gamma (IFN-γ) from the nine-banded armadillo (Dasypus novemcinctus) and its effect on Mycobacterium leprae-infected macrophages. Cytokine. 2008;43:124–131. doi: 10.1016/j.cyto.2008.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez J.M. Parasites, pests, and pets in a global world: new perspectives and challenges. Journal of Exotic Pet Medicine. 2009;18:248–253. doi: 10.1053/j.jepm.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Project Seahorse . 2016. Why Seahorses? Essential Facts About Seahorses. [Google Scholar]
- Quave C.L., Lohani U., Verde A., Fajardo J., Rivera D., Obón C., Valdes A., Pieroni A. A comparative assessment of zootherapeutic remedies from selected areas in Albania, Italy, Spain and Nepal. Journal of Ethnobiology. 2010;30:92–125. doi: 10.2993/0278-0771-30.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinowitz P., Conti L. Links among human health, animal health, and ecosystem health. Annual Review of Public Health. 2013;34:189–204. doi: 10.1146/annurev-publhealth-031912-114426. [DOI] [PubMed] [Google Scholar]
- Rabinowitz P.M., Gordon Z., Holmes R., Taylor B., Wilcox M., Chudnov D., Nadkarni P., Dein F.J. Animals as sentinels of human environmental health hazards: an evidence-based analysis. EcoHealth. 2005;2:26–37. [Google Scholar]
- Ratcliffe N.A., Mello C.B., Garcia E.S., Butt T.M., Azambuja P. Insect natural products and processes: new treatments for human disease. Insect Biochemistry and Molecular Biology. 2011;41:747–769. doi: 10.1016/j.ibmb.2011.05.007. [DOI] [PubMed] [Google Scholar]
- Reames M.K., Christensen C., Luce E.A. The use of maggots in wound debridement. Annals of Plastic Surgery. 1988;21:388–391. doi: 10.1097/00000637-198810000-00017. [DOI] [PubMed] [Google Scholar]
- Reif J.S. Animal sentinels for environmental and public health. Public Health Reports. 2011;126:50. doi: 10.1177/00333549111260S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reperant L.A., Cornaglia G., Osterhaus A.D.M.E. The importance of understanding the human–animal interface: from early hominins to global citizens. In: Mackenzie J.S., Jeggo M., Daszak M., Richt J.A., editors. One Health: The Human-Animal-Environment Interfaces in Emerging Infectious Diseases. Springer; Heidelberg, New York, Dordrecht, London: 2012. pp. 49–81. [Google Scholar]
- Robinson W. The use of blowfly larvae in the treatment of infected wounds. Annals of the Entomological Society of America. 1933;26:270–276. [Google Scholar]
- Robinson M.M., Zhang X. World Health Organization; Geneva: 2011. The World Medicines Situation 2011–Traditional Medicines: Global Situation, Issues and Challenges. [Google Scholar]
- Roldán-Clarà B., Lopez-Medellín X., Espejel I., Arellano E. Literature review of the use of birds as pets in Latin-America, with a detailed perspective on Mexico. Ethnobiology and Conservation. 2014;3:1–18. [Google Scholar]
- Rosa I.L., Defavari G.R., Alves R.R.N., Oliveira T.P.R. Seahorses in traditional medicines: a global overview. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine. Springer; Berlin: 2013. pp. 207–240. [Google Scholar]
- Rose J., Quave C.L., Islam G. The four-sided triangle of ethics in bioprospecting: pharmaceutical business, international politics, socio-environmental responsibility and the importance of local stakeholders. Ethnobiology and Conservation. 2012;1:1–25. [Google Scholar]
- Rostal M.K., Olival K.J., Loh E.H., Karesh W.B. Wildlife: the need to better understand the linkages. In: Mackenzie J.S., Jeggo M., Daszak P., Richt J.A., editors. One Health: The Human-Animal-Environment Interfaces in Emerging Infectious Diseases. Springer; Berlin Heidelberg: 2012. pp. 101–125. [Google Scholar]
- Rouquet P., Froment J.M., Bermejo M., Kilbourn A., Karesh W., Reed P., Kumulungui B. Wild animal mortality monitoring and human Ebola outbreaks, Gabon and Republic of Congo, 2001–2003. Emerging Infectious Diseases. 2005;11:283–290. doi: 10.3201/eid1102.040533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy S., Saha S., Pal P. Insect natural products as potential source for alternative medicines—a review. World Scientific News. 2015;19:80–94. [Google Scholar]
- Sahayaraj K., Borgio J.F., Muthukumar S., Anandh G.P. Antibacterial activity of Rhynocoris marginatus (Fab.) and Catamirus brevipennis (Servile)(Hemiptera: reduviidae) venomS against human pathogens. Journal of Venomous Animals and Toxins Including Tropical Diseases. 2006;12:487–496. [Google Scholar]
- Sales D.L., Oliveira O.P., Cabral M.E., Dias D.Q., Kerntopf M.R., Coutinho H.D.M., Costa J.G.M., Freitas F.R.D., Ferreira F.S., Alves R.R.N., Almeida W.O. Chemical identification and evaluation of the antimicrobial activity of fixed oil extracted from Rhinella jimi. Pharmaceutical Biology. 2015;53:98–103. doi: 10.3109/13880209.2014.911331. [DOI] [PubMed] [Google Scholar]
- Santos I.J.M., Coutinho H.D.M., Ferreira Matias E.F., Costa J.G.M., Alves R.R.N., Almeida W.O. Antimicrobial activity of natural products from the skins of the semiarid living lizards Ameiva ameiva (Linnaeus, 1758) and Tropidurus hispidus (Spix, 1825) Journal of Arid Environments. 2012;76:138–141. [Google Scholar]
- Santos I.J.M., Leite G.O., Costa J.G.M., Alves R.R.N., Campos A.R., Menezes I.R.A., Freita F.R.V., Nunes M.J.H., Almeida W.O. Topical anti-inflammatory activity of oil from Tropidurus hispidus (Spix, 1825) Evidence-Based Complementary and Alternative Medicine. 2015;2015 doi: 10.1155/2015/140247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarpa A. Pre-scientific medicines: their extent and value. Social Science & Medicine. 1981;15A:317–326. doi: 10.1016/0271-7123(81)90061-4. [DOI] [PubMed] [Google Scholar]
- Schacter B.Z. Greenwood Publishing Group; 2006. The New Medicines: How Drugs Are Created, Approved, Marketed, and Sold. [Google Scholar]
- Schnurrenberger P.R., Hubbert W.T. Iowa State University Press; Ames, IA: 1981. An Outline of the Zoonoses. [Google Scholar]
- Scollard D.M. The biology of nerve injury in leprosy. Leprosy Review. 2008;79:242–253. [PubMed] [Google Scholar]
- Scotch M., Odofin L., Rabinowitz P. Linkages between animal and human health sentinel data. BMC Veterinary Research. 2009;5:15. doi: 10.1186/1746-6148-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott K. Is hirudin a potential therapeutic agent for arthritis? Annals of the Rheumatic Diseases. 2002;61:561–562. doi: 10.1136/ard.61.6.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scrivener S., Yemaneberhan H., Zebenigus M., Tilahun D., Girma S., Ali S., McElroy P., Custovic A., Woodcock A., Pritchard D. Independent effects of intestinal parasite infection and domestic allergen exposure on risk of wheeze in Ethiopia: a nested case-control study. The Lancet. 2001;358:1493–1499. doi: 10.1016/S0140-6736(01)06579-5. [DOI] [PubMed] [Google Scholar]
- Seedhouse E. Springer; 2010. Ocean Outpost: The Future of Humans Living Underwater. [Google Scholar]
- Seymour C. Arthropod vectors of human disease in the United States. Clinical Microbiology Newsletter. 1984;6:85–89. [Google Scholar]
- Sharma R., Lahiri R., Scollard D.M., Pena M., Williams D.L., Adams L.B., Figarola J., Truman R.W. The armadillo: a model for the neuropathy of leprosy and potentially other neurodegenerative diseases. Disease Models and Mechanisms. 2013;6:19–24. doi: 10.1242/dmm.010215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw C. Advancing drug discovery with reptile and amphibian venom peptides: venom-based medicines. The Biochemical Society. 2009;31:34–37. [Google Scholar]
- Sherman R.A., Wyle F., Vulpe M. Maggot therapy for treating pressure ulcers in spinal cord injury patients. The Journal of Spinal Cord Medicine. 1986;18:71–74. doi: 10.1080/10790268.1995.11719382. [DOI] [PubMed] [Google Scholar]
- Sherman R.A., Hall M.J.R., Thomas S. Medicinal maggots: an ancient remedy for some contemporary afflictions. Annual Review of Entomology. 2000;45:55–81. doi: 10.1146/annurev.ento.45.1.55. [DOI] [PubMed] [Google Scholar]
- Sherman R.A., Mumcuoglu K.Y., Grassberger M., Tantawi T.I. Maggot therapy. In: Grassberger M., Sherman R.A., Gileva O.S., Kim C.M.H., Mumcuoglu K.Y., editors. Biotherapy-History, Principles and Practice: A Practical Guide to the Diagnosis and Treatment of Disease Using Living Organisms. Springer Science+Business Media; Dordrecht, The Netherlands: 2013. pp. 5–29. [Google Scholar]
- Shimpi R., Chaudhari P., Deshmukh R., Devare S., Bagad Y., Bhurat M. A review: phamacotherapeutics of bee venom. World Journal of Pharmacy and Pharmaceutical Sciences. 2016;5:656–667. [Google Scholar]
- Shin B.C., Kong J.C., Park T.Y., Yang C.Y., Kang K.W., Choi S. Bee venom acupuncture for chronic low back pain: a randomised, sham-controlled, triple-blind clinical trial. European Journal of Integrative Medicine. 2012;4:e271–e280. [Google Scholar]
- Sifuna N. The future of traditional customary uses of wildlife in modern Africa: a case study of Kenya and Botswana. Journal of Biophysical Chemistry. 2012;2:31–38. [Google Scholar]
- Silva E., Rosa P., Arruda M., Rúbio E. Determination of duffy phenotype of red blood cells in Dasypus novemcinctus and Cabassous sp. Brazilian Journal of Biology. 2005;65:555–557. doi: 10.1590/s1519-69842005000300022. [DOI] [PubMed] [Google Scholar]
- Silveira N. Editora Leo Christiano; São Paulo, Brasil: 1998. Gatos, a emoção de lidar. [Google Scholar]
- Simpson R.D. Biodiversity prospecting: shopping the wilds is not the key to conservation. Resources. 1997;126:12–15. [Google Scholar]
- Sleeman J. Wildlife zoonoses for the veterinary practitioner. Journal of Exotic Pet Medicine. 2006;15:25–32. [Google Scholar]
- Soewu D.A. Zootherapy and biodiversity conservation in Nigeria. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer-Verlag; Berlin Heidelberg: 2013. pp. 347–365. [Google Scholar]
- Stephen C., Ribble C. Death, disease and deformity; using outbreaks in animals as sentinels for emerging environmental health risks. Global Change & Human Health. 2001;2:108–117. [Google Scholar]
- Stephenson J. John Wilson; 1832. Medical Zoology, and Mineralogy; or Illustrations and Descriptions of the Animals and Minerals Employed in Medicine, and of the Preparations Derived from Them: Including Also an Account of Animal and Mineral Poisons. [PMC free article] [PubMed] [Google Scholar]
- Still J. Use of animal products in traditional Chinese medicine: environmental impact and health hazards. Complementary Therapies in Medicine. 2003;11:118–122. doi: 10.1016/s0965-2299(03)00055-4. [DOI] [PubMed] [Google Scholar]
- Sukarmi S., Sabdono A. Ethical perspectives of sustainable use of reef’s invertebrates as a source of marine natural products. Journal of Coastal Development. 2011;11:97–103. [Google Scholar]
- Taylor L.H., Latham S.M., Mark E.J. Risk factors for human disease emergence. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences. 2001;356:983–989. doi: 10.1098/rstb.2001.0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teich S., Myers R.A. Maggot therapy for severe skin infections. Southern Medical Journal. 1986;79:1153–1155. doi: 10.1097/00007611-198609000-00029. [DOI] [PubMed] [Google Scholar]
- Thammasirirak S., Ponkham P., Preecharram S., Khanchanuan R., Phonyothee P., Daduang S., Srisomsap C., Araki T., Svasti J. Purification, characterization and comparison of reptile lysozymes. Comparative Biochemistry and Physiology Part C: Toxicology & Pharmacology. 2006;143:209–217. doi: 10.1016/j.cbpc.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Trowell S. Drugs from bugs: the promise of pharmaceutical entomology. Futurist. 2003;37:17–19. [Google Scholar]
- Tsuchiya K. Historical perspectives in occupational medicine. The discovery of the causal agent of minamata disease. American Journal of Industrial Medicine. 1992;21:275–280. doi: 10.1002/ajim.4700210215. [DOI] [PubMed] [Google Scholar]
- Unnikrishnan E. 2004. Materia Medica of the Local Health Traditions of Payyannur Centre for Development Studies. [Google Scholar]
- Van der Schalie W.H., Gardner H.S., Jr., Bantle J.A., De Rosa C.T., Finch R.A., Reif J.S., Reuter R.H., Backer L.C., Burger J., Folmar L.C. Animals as sentinels of human health hazards of environmental chemicals. Environmental Health Perspectives. 1999;107:309–315. doi: 10.1289/ehp.99107309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Vliet N., Moreno J., Gómez J., Zhou W., Fa J.E., Golden C., Alves R.R.N., Nasi R. Bushmeat and human health: assessing the evidence in tropical and sub-tropical forests. Ethnobiology and Conservation. 2017;6:1–45. [Google Scholar]
- Van Wingerden J.J., Oosthuizen J.H. Use of the local leech Hirudo michaelseni in reconstructive plastic and hand surgery. South African Journal of Surgery (Suid-Afrikaanse tydskrif vir chirurgie) 1997;35:29–31. [PubMed] [Google Scholar]
- Voultsiadou E. Therapeutic properties and uses of marine invertebrates in the ancient Greek world and early Byzantium. Journal of Ethnopharmacology. 2010;130:237–247. doi: 10.1016/j.jep.2010.04.041. [DOI] [PubMed] [Google Scholar]
- Walsh J.F., Molyneux D.H., Birley M.H. Deforestation: effects on vector-borne disease. Parasitology. 1993;106:S55–S75. doi: 10.1017/s0031182000086121. [DOI] [PubMed] [Google Scholar]
- Warwick C., Lindley S., Steedman C. How to handle pets: a guide to the complexities of enforcing animal welfare and disease control. Environmental Health News. 2011;8(18–19) [Google Scholar]
- Weiss R.A. The Leeuwenhoek lecture 2001. Animal origins of human infectious disease. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences. 2001;356:957–977. doi: 10.1098/rstb.2001.0838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker I.S., Oboumarzouk O., Rozen W.M., Naderi N., Balasubramanian S.P., Azzopardi E.A., Kon M. The efficacy of medicinal leeches in plastic and reconstructive surgery: a systematic review of 277 reported clinical cases. Microsurgery. 2012;32:240–250. doi: 10.1002/micr.20971. [DOI] [PubMed] [Google Scholar]
- Whiting M.J., Williams V.L., Hibbitts T.J. Animals traded for traditional medicine at the Faraday market in South Africa: species diversity and conservation implications. Journal of Zoology. 2011;284:84–96. [Google Scholar]
- Whiting M.J., Williams V.L., Hibbitts T.J. Animals traded for traditional medicine at the Faraday market in South Africa: species diversity and conservation implications. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer-Verlag; Berlin Heidelberg: 2013. pp. 421–473. [Google Scholar]
- WHO . first ed. WHO; Geneva, Switzerland: 2005. Ecosystems and Human Well-Being : Health Synthesis : A Report of the Millennium Ecosystem Assessment. [Google Scholar]
- Wicher K., Kalinka C., Walsh G.P. Attempt to infect the nine-banded armadillo with Treponema pallidum. International Archives of Allergy and Immunology. 1983;70:285–287. doi: 10.1159/000233336. [DOI] [PubMed] [Google Scholar]
- Wiedorn W.S. A new experimental animal for psychiatric research: the opossum, Didelphis virginiana. Science. 1954;119:360–361. doi: 10.1126/science.119.3090.360. [DOI] [PubMed] [Google Scholar]
- Williams E.S., Yuill T., Artois M., Fischer J., Haigh S.A. Emerging infectious diseases in wildlife. Revue Scientifique et Technique, Office International des Epizooties. 2002;21:139–158. doi: 10.20506/rst.21.1.1327. [DOI] [PubMed] [Google Scholar]
- Williams V.L., Cunningham A.B., Bruyns R.K., Kemp A.C. Birds of a feather: quantitative assessments of the diversity and levels of threat to birds used in African traditional medicine. In: Alves R.R.N., Rosa I.L., editors. Animals in Traditional Folk Medicine: Implications for Conservation. Springer; 2013. pp. 383–420. [Google Scholar]
- Wolfe N.D., Eitel M.N., Gockowski J., Muchaal P.K., Nolte C., Prosser A.T., Torimiro J.N., Weise S.F., Burke D.S. Deforestation, hunting and the ecology of microbial emergence. Global Change & Human Health. 2000;1:10–25. [Google Scholar]
- Wolfe N.D., Dunavan C.P., Diamond J. Origins of major human infectious diseases. Nature. 2007;477:279–283. doi: 10.1038/nature05775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff M.J., Broadhurst M.J. Helminthic therapy: improving mucosal barrier function. Trends in Parasitology. 2012;28:187–194. doi: 10.1016/j.pt.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolhouse M.E., Gowtage-Sequeria S. Host range and emerging and reemerging pathogens. Emerging Infections Diseases. 2005;11:1842–1847. doi: 10.3201/eid1112.050997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Resources Institute, W.R.R . World Resources Institute; Washington, DC: 2000. People and Ecosystems the Fraying Web of Life; p. 389. [Google Scholar]
- Yasui A.M. Universidade Federal Rural do Rio de Janeiro; Seropédica: 2012. Avaliação da toxicidade e da resposta cutânea local induzidas por doses diluídas de veneno de abelha em cães. [Google Scholar]
- Yinfeng G., Xueying Z., Yan C., Di W., Sung W. China Council for International Cooperation on Environment and Development; 1997. Sustainability of Wildlife Use in Traditional Chinese Medicine, Conserving China’s Biodiversity: Reports of the Biodiversity Working Group (BWG) pp. 190–220. [Google Scholar]
- Zhu Q., Huang J., Wang S., Qin Z., Lin F. Cobrotoxin extracted from Naja atra venom relieves arthritis symptoms through anti-inflammation and immunosuppression effects in rat arthritis model. Journal of Ethnopharmacology. 2016:1–9. doi: 10.1016/j.jep.2016.11.009. [DOI] [PubMed] [Google Scholar]


