Abstract
Objective
We aim to determine if pelvic incidence (PI) differed between a symptomatic femoroacetabular impingement (FAI) population and a control.
Methods
We retrospectively identified a cohort of symptomatic FAI patients and compared measured PI to a control group.
Results
The PI was significantly lower in the FAI group compared to the control (51.32±1.07 vs. 55.63±1.04; P < 0.01).
Conclusion
The mean PI was significantly decreased in the FAI population compared to a control.
Keywords: Femoroacetabular impingement, Spinopelvic parameters, Pelvic incidence, False profile
1. Introduction
The importance of sagittal balance and its role in normal spine function has been well established.1, 2, 3, 4 Deviations in sagittal balance are thought to cause muscle fatigue, back pain, and degenerative spine conditions.1,2,4 Spinopelvic parameters have been introduced to assist with the objective assessment of sagittal balance in the lumbosacral-pelvic junction. Pelvic incidence (PI) appears to be the main axis of sagittal balance of the spine through its strong influence on lumbar lordosis.5 PI is a fixed angle independent of pelvis orientation in the sagittal plane, and remains constant throughout adulthood.5,6
Femoroacetabular impingement (FAI) has been established as a major cause of non-arthritic hip pain, with bony and soft tissue impingement leading to hip pain and intra-articular damage.7, 8, 9, 10 Progress has been made in the understanding of the pathomechanics of FAI; however, the role of spinopelvic balance and its contribution to the pathology of FAI remains poorly understood.8,10,11 Abnormalities in PI have previously been associated with various spine disorders, with recent authors suggesting abnormalities in PI are also associated with FAI.1,12, 13, 14, 15, 16
PI influences sagittal rotation of the pelvis during standing and gait, leading to increased or decreased acetabular coverage of the femoral heads, and a relative hip impingement or dysplasia, respectively.15,17,18 Despite the association between PI and FAI, investigational studies have been lacking. This may in part be explained by the challenge of obtaining a reliable and accurate measurement of PI with imaging commonly obtained in the evaluation of an FAI patient. Spinopelvic parameters are traditionally measured from a lateral radiograph, with rotational changes in the pelvis altering the measured PI.19,20 This has led authors to investigate the potential use of false profile (FP) radiographs for spinopelvic parameter assessment, with the literature lacking enough evidence to support the accuracy and reliability of this method.20
The purpose of this study was to determine if PI differed between a symptomatic FAI population and that of an asymptomatic control group. Furthermore, we assess the accuracy and reliability of measuring the PI from a FP radiograph in a symptomatic FAI population. We hypothesize that patients with symptomatic FAI have a decreased PI compared to an asymptomatic control, and PI can be determined from a FP radiograph with the use of a corrective formula.
2. Methods
2.1. Patient selection
Following institutional review board approval, we retrospectively identified a consecutive series of patients with symptomatic FAI treated with arthroscopic hip surgery between May 2017 and March 2018 at a single institution. Patient inclusion required a diagnosis of symptomatic and radiographic FAI confirmed by intra-operative findings at the time of surgery. Patients were excluded for having evidence of osteoarthritis on plain radiographs (Tonnis grade of 2 or higher), evidence of a childhood hip pathology (slipped capital femoral epiphysis, developmental dysplasia, and perthes), a history of prior hip or spine surgery, and/or incomplete radiographic assessment (AP pelvis, lateral, and false profile views).
To obtain a control group, we retrospectively identified a consecutive series of patients evaluated in spine clinic between May 2017 and July 2017 with a lateral radiograph and no evidence of symptomatic FAI. Patient inclusion required an assessment of back and/or leg pain, with a lateral radiograph. Patients were excluded for having a history of prior hip or spine surgery, and/or radiographs that do not include visualization of the femoral heads.
Patients in the FAI group were used to determine the accuracy and reliability of measuring PI from a FP radiograph. Patients with FP radiographs where the sacral endplate was obscured were excluded from this analysis.
2.2. Radiographic assessment
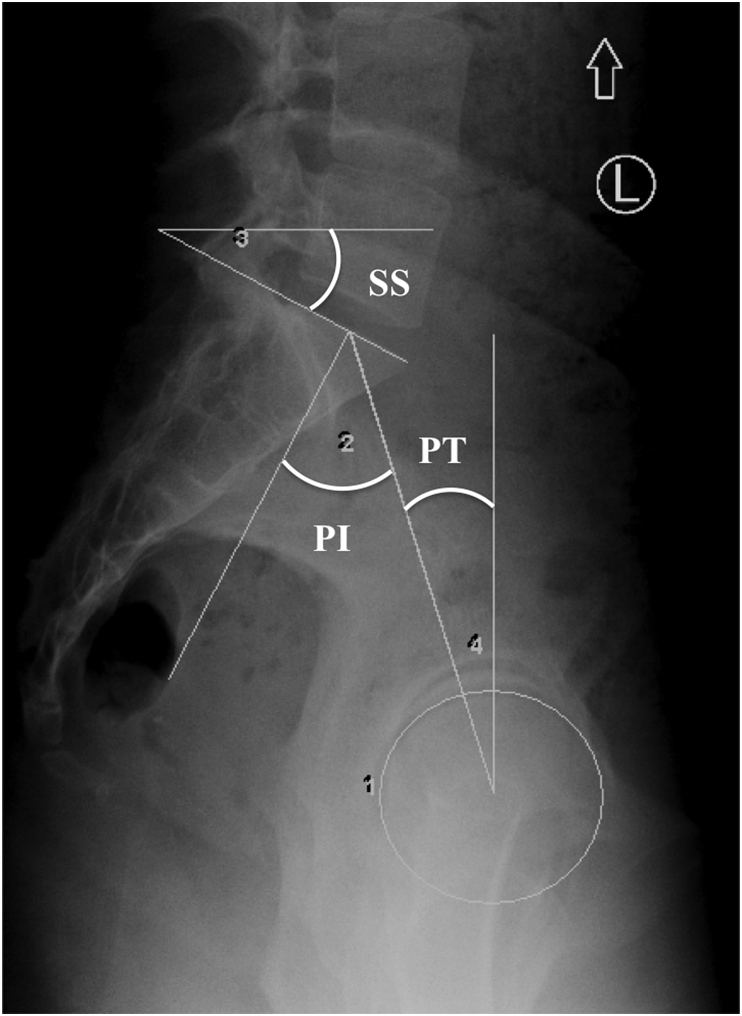
Spinopelvic parameters were measured on a standing lateral radiograph as described by Legaye et al.5 The PI was measured as an angle formed between a line joining the center of the femoral heads to the center of the sacral endplate and a line perpendicular to the sacral endplate. Sacral slope (SS) was measured as an angle formed between a line tangential to the superior endplate of S1 and a line parallel to the horizontal plane. PI is the sum of sacral slope and pelvic tilt (PI = SS + PT).5 Using this equation, the PT was obtained by subtracting the measured SS from the measured PI. Fig. 1 illustrates the radiographic measurement of spinopelvic parameters.
Fig. 1.
Radiographic measurement of spinopelvic parameters including pelvic incidence (PI), sacral slope (SS), and pelvic tilt (PT).
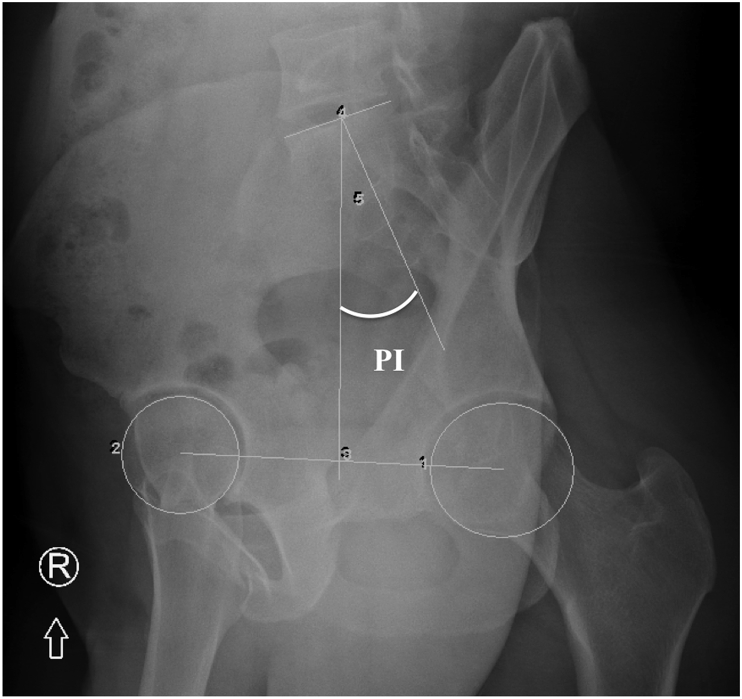
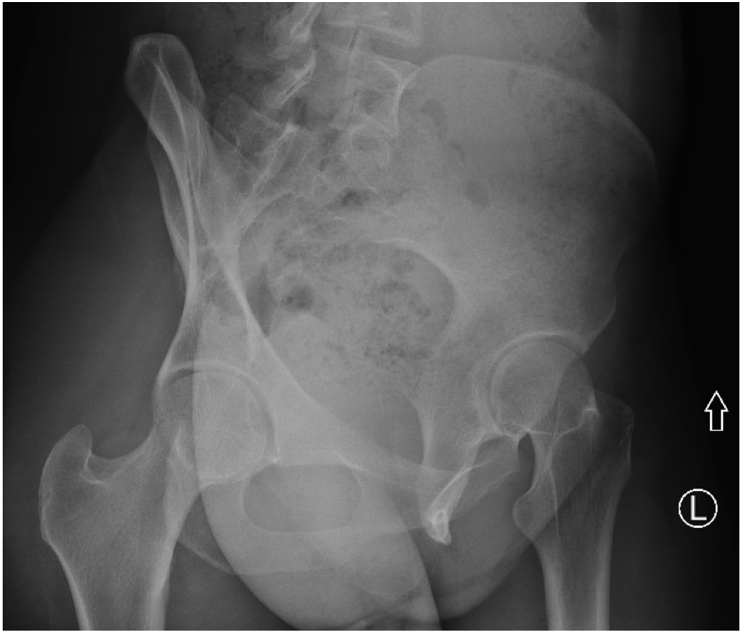
A previously described and validated method was used to measure PI on FP radiographs.20,21 In this method, the PI is measured as an angle formed between a line joining the midpoint between the center of the femoral heads to the center of the sacral endplate and a line perpendicular to the sacral endplate (Fig. 2). FP radiographs where the sacral endplate was obscured as agreed upon by both reviewers were excluded from analysis (Fig. 3). Two senior orthopedic surgery residents obtained radiographic measurements on all patients independently. Table 2 represents the mean from each reviewer's assessment.
Fig. 2.
Radiographic measurement of pelvic incidence (PI) on false profile radiograph of the right hip.
Fig. 3.
False profile radiographic of a left hip illustrating an obscured sacral endplate limiting pelvic incidence (PI) measurement.
Table 2.
Mean spinopelvic parameter measurements.
| Spinopelvic Parameter | FAI | Control | P-value |
|---|---|---|---|
| Pelvic Incidence (lateral) | 51.32±1.07 | 55.63±1.04 | <0.01a |
| Sacral Slope (lateral) | 37.07±0.82 | 36.90±0.99 | 0.90 |
| Pelvic Tilt (lateral) | 14.25±0.76 | 18.72±0.95 | <0.01a |
| Pelvic Incidence (FP) | 34.70±1.75b |
Abbreviations: FAI – Femoroacetabular impingement; FP – False profile.
Indicates statistically significant difference (P < 0.05).
Indicates statistically significant difference (P < 0.05) compared to pelvic incidence (lateral).
Intra- and inter-observer reliability measurements were obtained 6-weeks following initial assessment. For this data, all 26 patients with FP radiographs deemed adequate for PI measurement from the FP view were utilized. Reviewers were blinded to their initial measurements. PI was again measured on each patient's lateral and FP radiograph, and sacral slope from a lateral radiograph, with the results recorded for reliability assessment.
2.3. Statistical analysis
All descriptive and inferential statistics were preformed using R version 3.5.1 (The R Foundation for Statistical Computing, https://www.r-project.org/). Averages were reported as the mean ± standard error of the mean. Two-sample t tests were used for comparing quantitative measurements between the FAI and control group. Chi-square tests were used for categorical variables. Intraclass correlation (ICC) was used to measure the reliability of the two observers. The value of ICC was given along with a 95% confidence interval. PI (lateral) and PI (FP) measurements for each patient were reported as the average measurement from two observers. A scatter plot was developed comparing PI (lateral) and PI (FP) measurements. An estimated regression line was calculated, with best-fit equation reported in Fig. 4.
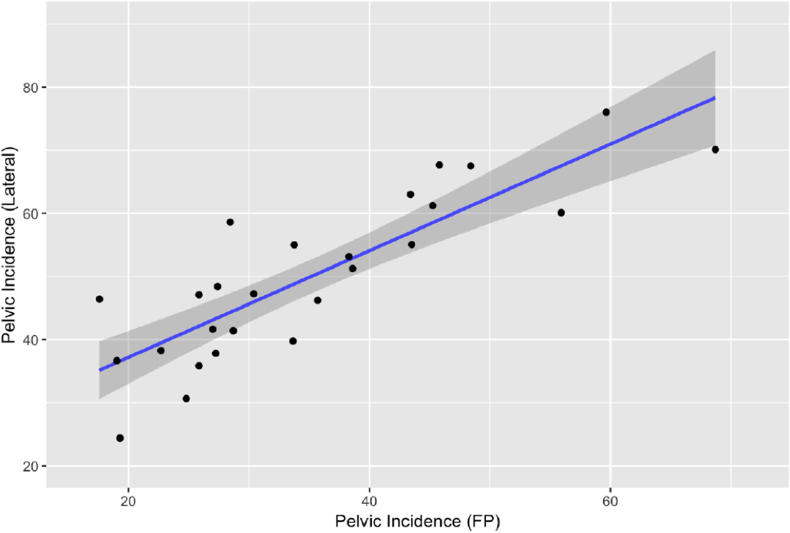
Fig. 4.
Correlation between pelvic incidence measured on false profile and lateral radiographs
a Correlation coefficient: 0.84. b Best fit equation: PILateral = 20.29 + 0.84PIFP.
3. Results
One hundred twenty-three consecutive patients were considered for analysis in the symptomatic FAI group. Twenty-three patients were excluded leaving 100 patients for evaluation of spinopelvic parameter measurements. Of these 100 patients, 26 had FP radiographs with non-obscured sacral endplates allowing for PI measurement allowing for the sub analysis of Pelvic Incidence (FP). One hundred fourteen consecutive patients were considered for analysis in the control group. Thirty-four patients were excluded leaving 80 patients for evaluation. There were significantly more females in the FAI group, which was significantly younger than the control group (P < 0.01). See Table 1.
Table 1.
Demographics.
| Variable | FAI | Control | P-value |
|---|---|---|---|
| Number of Patients | 100 | 80 | |
| Sex (% Female) | 60.00±4.90 | 37.50±5.40 | <0.01a |
| Mean Age (Years) | 39.00±1.30 | 50.77±1.77 | <0.01a |
Abbreviations: FAI – Femoroacetabular impingement.
Indicates statistically significant difference (P < 0.05).
The mean PI measured on a lateral radiograph was significantly lower in the symptomatic FAI group compared to the control group (51.32±1.07 vs. 55.63±1.04; P < 0.01). Similarly, the mean PT was significantly lower in the FAI group (P < 0.01). There was no significant difference between mean SS (P = 0.90). The mean PI as measured from a FP radiograph was 34.70±1.75, which was 16.62° less than PI as measured from a lateral radiograph (P < 0.01) (Table 2).
There was a strong linear correlation between measured PI (lateral) and PI (FP), with a correlation coefficient of 0.84. PI (lateral) and PI (FP) measurements were linearly associated, with a regression line shown in Fig. 4. PI (lateral) measurements can thus be estimated utilizing PI (FP) measurements and the given regression equation: PILateral = 20.29 + 0.84PIFP (R2 = 0.72, P < 0.01).
The intra-observer correlation agreement for PI (lateral) showed excellent reliability for both reviewers (kappa = 0.98 and kappa = 0.98; respectively). Similar results were seen for the intra-observer correlation agreement for PI (FP) (kappa = 0.96 and kappa = 0.95; respectively). The inter-observer correlation agreement for PI (lateral) and PI (FP) showed excellent reliability (kappa = 0.96 and kappa = 0.97; respectively). See Table 3.
Table 3.
Intra-observer and inter-observer reliability.
| Spinopelvic Parameter | Reviewer 1 Intra-observer Reliability (95% CI) | Reviewer 2 Intra-observer Reliability (95% CI) | Inter-observer Reliability (95% CI) |
|---|---|---|---|
| Pelvic Incidence (lateral) | 0.98 (0.95, 0.99)a | 0.98 (0.97, 0.99)a | 0.96 (0.16, 0.99)a |
| Pelvic Incidence (FP) | 0.96 (0.91, 0.98)a | 0.95 (0.88, 0.98)a | 0.97 (0.93, 0.99)a |
| Sacral Slope (lateral) | 0.97 (0.93, 0.99)a | 0.95 (0.90, 0.98)a | 0.97 (0.87, 0.99)a |
Abbreviations: FAI – Femoroacetabular impingement; FP – False profile; 95% CI – 95% confidence interval.
Indicates excellent reliability (kappa >0.75).
4. Discussion
In this study, we found a significantly lower PI in the symptomatic FAI group compared to the control group (51.32±1.07 vs. 55.63±1.04; P < 0.01). Our results are in agreement with data published by previous authors.14,22 Hellman et al. found a significantly lower mean PI in a cohort of 60 symptomatic FAI patients compared to a historical control (49.30 vs. 55.0; P < 0.01).14 Weinberg et al. reported a mean PI of 46.7 in 25 patients with mixed FAI, which was significantly lower than the mean PI of their control group at 56.1 (P = 0.01).22
This data suggests there may be a relationship between decreased PI and symptomatic FAI. Gebhart et al. assessed PI and hip morphology in 40 cadaveric specimens and found decreased PI to be associated with cam and pincer deformities.16 However, many studies have also reported a high incidence of bony abnormalities associated with FAI in asymptomatic populations.23, 24, 25, 26, 27, 28
Hellman et al. theorized the association between symptomatic FAI and decreased PI may be a consequence of restricted spinopelvic motion.14 They suggest that with a low PI, patients are unable to increase their pelvic tilt with leg flexion compared to someone with a normal PI. Thus resulting in less dynamic acetabular anteversion, leading to anterior impingement, and smaller limits of terminal hip motion. Considering this, patients with bony deformities characteristic of FAI may be more prone to symptoms when they have a decreased PI since restricted spinopelvic motion may decrease a patients’ ability to compensate for their hip pathoanatomy. Furthermore, some believe that cam and pincer deformities are actually the result of repetitive stress from impingement, similar to what a hip with a decreased PI is subjected to.
The clinical significance of these findings remains unknown due to a lack of investigational studies on spinopelvic parameters in symptomatic FAI populations. This, in part, is due to the challenge of obtaining an accurate and reliable radiographic assessment of PI utilizing imaging commonly obtained in the evaluation of FAI patients. Investigating the potential use of FP radiographs to accurately and reliably measure spinopelvic parameters may help to resolve this issue. Tyrakowski et al. found that measured PI can be influenced by coronal rotation of the pelvis, determining 30° to be the maximal angle of rotation for reliable PI measurement.21 Janusz et al. found measured PI to be accurate at up to 20° of coronal rotation, with the sacral endplates insufficiently visualized past this degree of rotation.19 Li et al. reported increased rotation from a lateral view results in greater error in measuring PI; however, PI can be measured accurately at up to 25° of coronal rotation.20
While previous authors have reported no significant difference between measured PI (lateral) and PI (FP) in radiological pelvic phantoms, mathematical models, and cadaveric specimens rotated up to 30°, our clinical data suggests these findings may be more difficult to apply in a clinical setting.20,21 Only 26 of the 100 patients in the symptomatic FAI cohort (26%) had FP views where the sacral endplate was not obscured as seen in Fig. 3, allowing for PI measurement. In these patients, we found excellent intra-observer and inter-observer reliability measuring PI from FP radiographs (Table 3). Contrary to previous studies, the mean measured PI (FP) was significantly less than mean PI (lateral) (Table 2).
The contradiction between reported measurements in radiological pelvic phantoms, mathematical models, and cadaveric specimens could in part be explained by the less than ideal circumstances seen in clinical practice. Difficulties faced in the clinical setting include slight variations in the degree of coronal rotation of the FP radiographs, limb length discrepancies, and pelvic obliquity. Despite a significant difference between the mean PI (lateral) and PI (FP), these measurements were found to be linearly associated with excellent correlation (Fig. 4). Recognizing this, a regression line was determined with a best-fit equation as follows: PILateral = 20.29 + 0.84PIFP (Fig. 4). We believe that use of our corrective equation may provide a more accurate assessment of PI when measured off a FP view in the clinical setting.
These results may have many clinical implications. There appears to be an association between decreased PI and symptomatic FAI, which may prove to be a predictive factor for future symptomatic impingement in asymptomatic patients. Our data supports the idea that PI can be reliably measured from FP radiographs where the sacral endplate can be accurately identified, allowing for retrospective analysis of PI in previous FAI cohorts. Future retrospective and prospective analysis is required to determine the clinical significance of decreased PI, for instance, as a predictor of treatment failure, or risk for developing contralateral symptoms. The ability to measure PI from FP radiographs allows for the assessment of spinopelvic parameters from imaging routinely obtained in the work up of FAI, limiting the need for additional radiographs and radiation exposure.
This study is not without limitation. Our study design was retrospective in nature, limiting the level of evidence. There was a significant difference in percent female and mean age between the symptomatic FAI group and the control. While PI does not change with age, some authors have suggested a potential difference between sexes, which may represent a confounding variable in our data. Due to obscured sacral endplates in many of the FP radiographs, many patients had to be excluded from our analysis, increasing the likelihood of selection bias. Last, despite finding a significant difference in PI between a symptomatic FAI population and control, the clinical significance of this difference remains unknown.
5. Conclusion
Mean PI was significantly decreased in our symptomatic FAI population compared to our control group, suggesting an association between these findings. There is excellent inter- and intra-observer reliability in PI measurements obtained from FP radiographs in the clinical setting; however, these measurements deviated significantly from those obtained from lateral radiographs. Despite these differences, there is a strong linear correlation between measured PI (lateral) and PI (FP) allowing for a corrective equation to be utilized to accurately determine PI from FP radiographs in the clinical setting.
References
- 1.Glassman S.D., Berven S., Bridwell K., Horton W., Dimar J.R. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 2.Glassman S.D., Bridwell K., Dimar J.R., Horton W., Berven S., Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 3.Lazennec J.Y., Ramare S., Arafati N. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson R.P., McManus A.C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine. 1994;19:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 5.Legaye J., Duval-Beaupere G., Hecquet J., Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mac-Thiong J.M., Berthonnaud E., Dimar J.R., 2nd, Betz R.R., Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine. 2004;29:1642–1647. doi: 10.1097/01.brs.0000132312.78469.7b. [DOI] [PubMed] [Google Scholar]
- 7.Nepple J.J., Prather H., Trousdale R.T. Clinical diagnosis of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21(Suppl 1):S16–S19. doi: 10.5435/JAAOS-21-07-S16. [DOI] [PubMed] [Google Scholar]
- 8.Bedi A., Kelly B.T. Femoroacetabular impingement. J Bone Jt Surg Am Vol. 2013;95:82–92. doi: 10.2106/JBJS.K.01219. [DOI] [PubMed] [Google Scholar]
- 9.Frank J.S., Gambacorta P.L., Eisner E.A. Hip pathology in the adolescent athlete. J Am Acad Orthop Surg. 2013;21:665–674. doi: 10.5435/JAAOS-21-11-665. [DOI] [PubMed] [Google Scholar]
- 10.Ganz R., Parvizi J., Beck M., Leunig M., Notzli H., Siebenrock K.A. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 11.Leunig M., Beaule P.E., Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616–622. doi: 10.1007/s11999-008-0646-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roussouly P., Gollogly S., Berthonnaud E., Labelle H., Weidenbaum M. Sagittal alignment of the spine and pelvis in the presence of L5-s1 isthmic lysis and low-grade spondylolisthesis. Spine. 2006;31:2484–2490. doi: 10.1097/01.brs.0000239155.37261.69. [DOI] [PubMed] [Google Scholar]
- 13.La Maida G.A., Zottarelli L., Mineo G.V., Misaggi B. Sagittal balance in adolescent idiopathic scoliosis: radiographic study of spino-pelvic compensation after surgery. Eur Spine J. 2013;22(Suppl 6):S859–S867. doi: 10.1007/s00586-013-3018-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hellman M.D., Haughom B.D., Brown N.M., Fillingham Y.A., Philippon M.J., Nho S.J. Femoroacetabular impingement and pelvic incidence: radiographic comparison to an asymptomatic control. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc North Am Int. Arthrosc Assoc. 2017;33:545–550. doi: 10.1016/j.arthro.2016.08.033. [DOI] [PubMed] [Google Scholar]
- 15.Morris W.Z., Fowers C.A., Yuh R.T., Gebhart J.J., Salata M.J., Liu R.W. Decreasing pelvic incidence is associated with greater risk of cam morphology. Bone Joint Res. 2016;5:387–392. doi: 10.1302/2046-3758.59.BJR-2016-0028.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gebhart J.J., Streit J.J., Bedi A., Bush-Joseph C.A., Nho S.J., Salata M.J. Correlation of pelvic incidence with cam and pincer lesions. Am J Sports Med. 2014;42:2649–2653. doi: 10.1177/0363546514548019. [DOI] [PubMed] [Google Scholar]
- 17.DiGioia A.M., Hafez M.A., Jaramaz B., Levison T.J., Moody J.E. Functional pelvic orientation measured from lateral standing and sitting radiographs. Clin Orthop Relat Res. 2006;453:272–276. doi: 10.1097/01.blo.0000238862.92356.45. [DOI] [PubMed] [Google Scholar]
- 18.Ross J.R., Tannenbaum E.P., Nepple J.J., Kelly B.T., Larson C.M., Bedi A. Functional acetabular orientation varies between supine and standing radiographs: implications for treatment of femoroacetabular impingement. Clin Orthop Relat Res. 2015;473:1267–1273. doi: 10.1007/s11999-014-4104-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janusz P., Tyrakowski M., Monsef J.B., Siemionow K. Influence of lower limbs discrepancy and pelvic coronal rotation on pelvic incidence, pelvic tilt and sacral slope. Eur Spine J. 2016;25:3622–3629. doi: 10.1007/s00586-016-4458-8. [DOI] [PubMed] [Google Scholar]
- 20.Li R.T., Liu R.W., Neral M. Use of the false-profile radiographic view to measure pelvic incidence. Am J Sports Med. 2018;46:2089–2095. doi: 10.1177/0363546518780938. [DOI] [PubMed] [Google Scholar]
- 21.Tyrakowski M., Wojtera-Tyrakowska D., Siemionow K. Influence of pelvic rotation on pelvic incidence, pelvic tilt, and sacral slope. Spine. 2014;39:E1276–E1283. doi: 10.1097/BRS.0000000000000532. [DOI] [PubMed] [Google Scholar]
- 22.Weinberg D.S., Gebhart J.J., Liu R.W., Salata M.J. Radiographic signs of femoroacetabular impingement are associated with decreased pelvic incidence. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc North Am Int. Arthrosc Assoc. 2016;32:806–813. doi: 10.1016/j.arthro.2015.11.047. [DOI] [PubMed] [Google Scholar]
- 23.Laborie L.B., Lehmann T.G., Engesaeter I.O., Eastwood D.M., Engesaeter L.B., Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502. doi: 10.1148/radiol.11102354. [DOI] [PubMed] [Google Scholar]
- 24.Hack K., Di Primio G., Rakhra K., Beaule P.E. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg. 2010;92:2436–2444. doi: 10.2106/JBJS.J.01280. American volume. [DOI] [PubMed] [Google Scholar]
- 25.Reichenbach S., Juni P., Werlen S. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res. 2010;62:1319–1327. doi: 10.1002/acr.20198. [DOI] [PubMed] [Google Scholar]
- 26.Jung K.A., Restrepo C., Hellman M., AbdelSalam H., Morrison W., Parvizi J. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg. 2011;93:1303–1307. doi: 10.1302/0301-620X.93B10.26433. British volume. [DOI] [PubMed] [Google Scholar]
- 27.Kang A.C., Gooding A.J., Coates M.H., Goh T.D., Armour P., Rietveld J. Computed tomography assessment of hip joints in asymptomatic individuals in relation to femoroacetabular impingement. Am J Sports Med. 2010;38:1160–1165. doi: 10.1177/0363546509358320. [DOI] [PubMed] [Google Scholar]
- 28.Chakraverty J.K., Sullivan C., Gan C., Narayanaswamy S., Kamath S. Cam and pincer femoroacetabular impingement: CT findings of features resembling femoroacetabular impingement in a young population without symptoms. AJR Am J Roentgenol. 2013;200:389–395. doi: 10.2214/AJR.12.8546. [DOI] [PubMed] [Google Scholar]